Unlocking the Secrets of Knee Joint Unloading: A Systematic Review and Biomechanical Study of the Invasive and Non-Invasive Methods and Their Influence on Knee Joint Loading
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Strategy
2.1.1. Search Strategy
2.1.2. Study Selection
2.1.3. Procedure Classification
2.1.4. Data Collection and Extraction
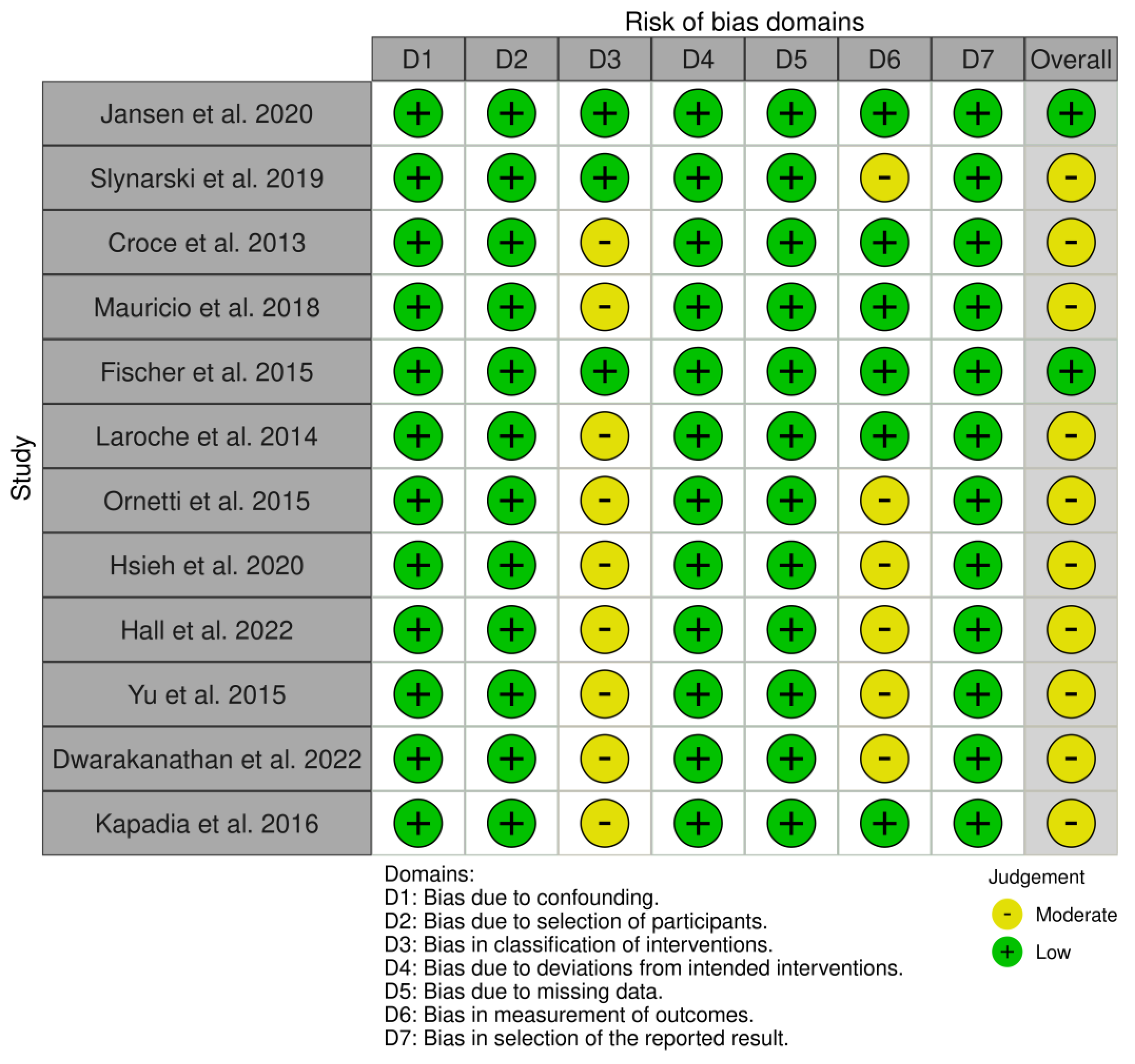
2.1.5. Risk of Bias Assessment
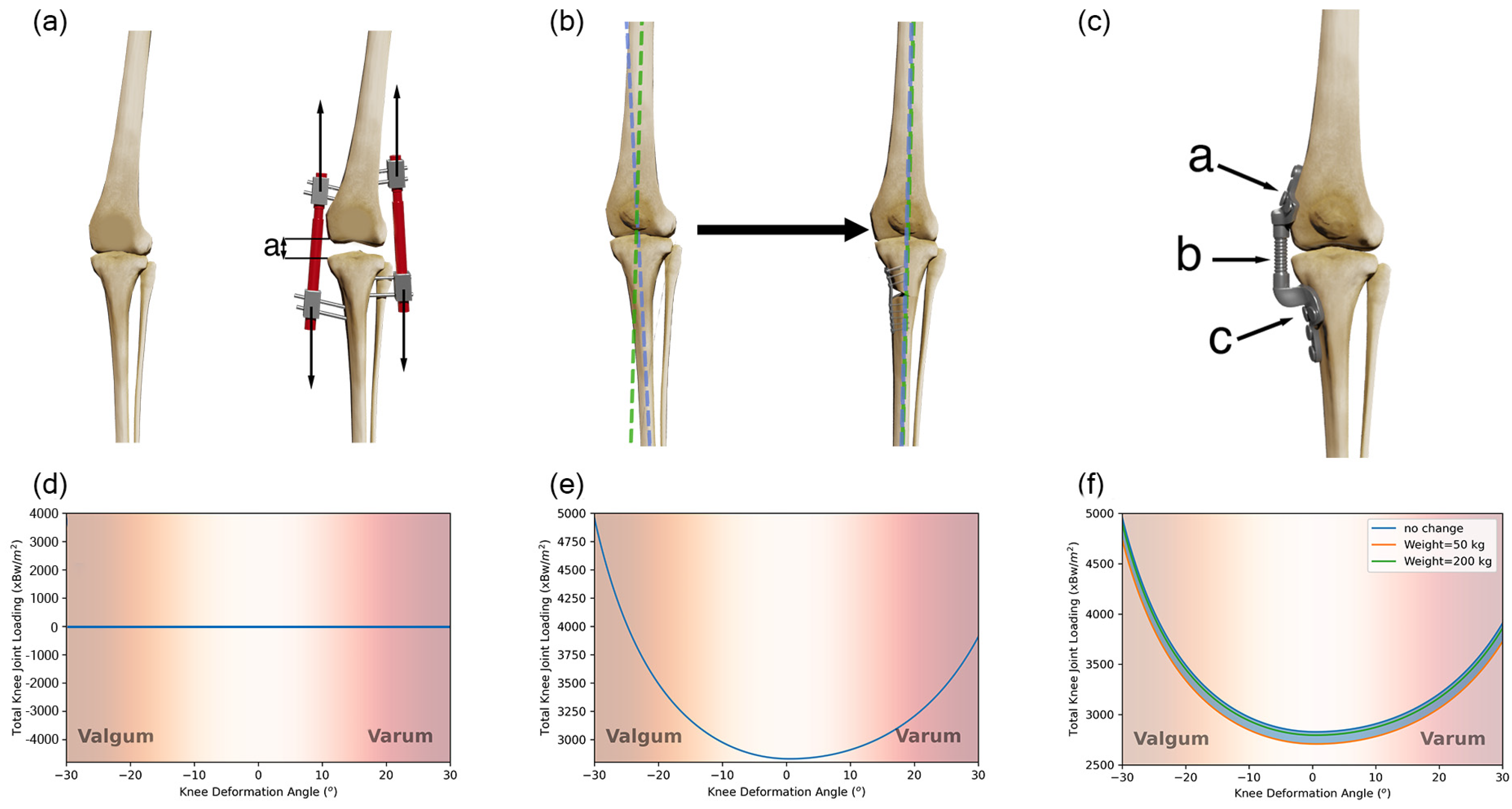
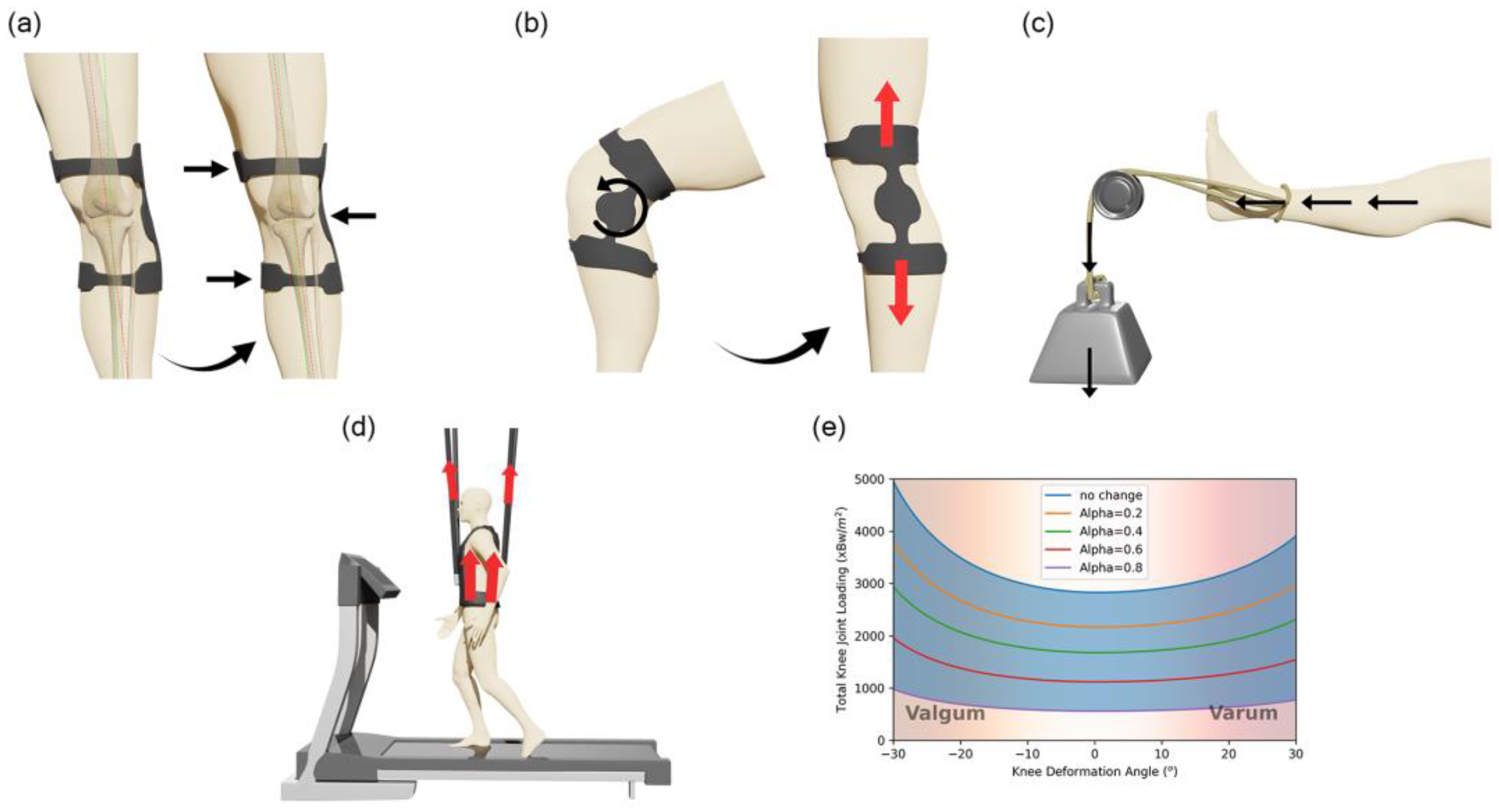
2.2. Biomechanical Model
3. Results
3.1. Search Results
3.2. Risk of Bias
3.3. Invasive Methods
3.3.1. Knee Joint Distraction
3.3.2. High Tibial Osteotomy
3.3.3. Implantable Shock Absorber
3.4. Non-Invasive Methods
3.4.1. Knee Unloader Brace
3.4.2. Distraction Rotation Knee Brace
3.4.3. Physical Therapy
4. Discussion
4.1. Efficiency of Invasive Methods
4.2. Efficiency of Non-Invasive Methods
5. Limitations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| OA | Osteoarthritis |
| TKA | Total Knee Arthroplasty |
| KJD | Knee Joint Distraction |
| HTO | High Tibial Osteotomy |
| ISA | Implantable Shock Absorber |
| KUB | Knee Unloading Brace |
| DRKB | Distraction Rotation Knee Brace |
| PT | Physical Therapy |
| JSW | Joint Space Width |
| CT | Cartilage Thickness |
| WOMAC | Western Ontario and McMaster Universities Osteoarthritis Index |
| KOOS | Total Knee injury and Osteoarthritis Outcome Score system |
| GV | Gait velocity |
| PKAM | Peak Knee Adduction Moment |
| RTS | Time to Return to Sports |
| RTW | Time to Return to Work |
| GRF | Ground Reaction Force |
| VAS | Visual Analogue Scale |
Appendix A

References
- Maquet, P.G.J. Biomechanics of the Knee; Springer: Berlin/Heidelberg, Germany, 1984. [Google Scholar] [CrossRef]
- Bijlsma, J.W.; Berenbaum, F.; Lafeber, F.P. Osteoarthritis: An update with relevance for clinical practice. Lancet 2011, 377, 2115–2126. [Google Scholar] [CrossRef]
- Albright A. A National Public Health Agenda for Osteoarthritis: 2020 Update. Osteoarthritis Action Alliance Arthritis Foundation Centers for Disease Control and Prevention. 2020. pp. 1–28. Available online: https://www.arthritis.org/getmedia/7b7cb13b-7075-4173-be6e-38ec475952b2/OA-Agenda-CDC-2020-R3.pdf (accessed on 11 February 2024).
- Hochberg, M.C.; Cisternas, M.G.; Watkins-Castillo, S.I. ‘Osteoarthritis’, The burden of Musculoskeletal Diseases in the United States, 4th ed. Available online: https://www.boneandjointburden.org/fourth-edition/iiib10/osteoarthritis (accessed on 24 March 2021).
- Bonnin, M.; Chambat, P. (Eds.) Osteoarthrisis of the knee. In Approche Pratique en Orthopédie–Traumatologie; Springer: Paris, France, 2008. [Google Scholar]
- Rodriguez-Merchan, E.C.; De La Corte-Rodriguez, H. The role of orthoses in knee osteoarthritis. Hosp. Pract. 2019, 47, 1–5. [Google Scholar] [CrossRef]
- Aboulenain, S.; Saber, A.Y. Primary Osteoarthritis. StatPearls. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557808/ (accessed on 20 May 2021).
- Jackson, B.D.; Teichtahl, A.J.; Morris, M.E.; Wluka, A.E.; Davis, S.R.; Cicuttini, F.M. The effect of the knee adduction moment on tibial cartilage volume and bone size in healthy women. Rheumatology 2003, 43, 311–314. [Google Scholar] [CrossRef]
- Rodríguez-Merchán, E.C.; Gómez-Cardero, P. Comprehensive Treatment of Knee Osteoarthritis. In Recent Advances; Springer International Publishing: Cham, Switzerland, 2020. [Google Scholar]
- Bayliss, L.E.; Culliford, D.; Monk, A.P.; Glyn-Jones, S.; Prieto-Alhambra, D.; Judge, A.; Cooper, C.; Carr, A.J.; Arden, N.K.; Beard, D.J.; et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: A population-based cohort study. Lancet 2017, 389, 1424–1430. [Google Scholar] [CrossRef]
- Takahashi, T.; Baboolal, T.G.; Lamb, J.; Hamilton, T.W.; Pandit, H.G. Is Knee Joint Distraction a Viable Treatment Option for Knee OA?—A Literature Review and Meta-Analysis. J. Knee Surg. 2019, 32, 788–795. [Google Scholar] [CrossRef]
- Rahmatullah Bin Abd Razak, H.; Campos, J.P.; Khakha, R.S.; Wilson, A.J.; van Heerwaarden, R.J. Role of joint distraction in osteoarthritis of the knee: Basic science, principles and outcomes. J. Clin. Orthop. Trauma 2022, 24, 101723. [Google Scholar] [CrossRef]
- Liu, X.; Chen, Z.; Gao, Y.; Zhang, J.; Jin, Z. High Tibial Osteotomy: Review of Techniques and Biomechanics. J. Healthc. Eng. 2019, 2019, 8363128. [Google Scholar] [CrossRef]
- Block, J.; Stiebel, M.; Miller, L. Post-traumatic knee osteoarthritis in the young patient: Therapeutic dilemmas and emerging technologies. Open Access J. Sports Med. 2014, 5, 73–79. [Google Scholar] [CrossRef]
- Mistry, D.A.; Chandratreya, A.; Lee, P.Y.F. An Update on Unloading Knee Braces in the Treatment of Unicompartmental Knee Osteoarthritis from the Last 10 Years: A Literature Review. Surg. J. 2018, 04, e110–e118. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- WOMAC Survey Form. Western Ontario and McMaster Universities Osteoarthritis Index|RehabMeasures Database. Available online: https://www.sralab.org/sites/default/files/2017-07/New_patient_Hip_WOMAC.PD_.pdf (accessed on 14 June 2024).
- Theiler, R.; Spielberger, J.; Bischoff, H.; Bellamy, N.; Huber, J.; Kroesen, S. Clinical evaluation of the WOMAC 3.0 OA Index in numeric rating scale format using a computerized touch screen version. Osteoarthr. Cartil. 2002, 10, 479–481. [Google Scholar] [CrossRef]
- Roos, E.M.; Lohmander, L.S. The Knee injury and Osteoarthritis Outcome Score (KOOS): From joint injury to osteoarthritis. Health Qual. Life Outcomes 2003, 1, 64. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Erdemir, A. Open Knee: Open Source Modeling and Simulation in Knee Biomechanics. J. Knee Surg. 2015, 29, 107–116. [Google Scholar] [CrossRef]
- Chokhandre, S.; Schwartz, A.; Klonowski, E.; Landis, B.; Erdemir, A. Open Knee(s): A Free and Open Source Library of Specimen-Specific Models and Related Digital Assets for Finite Element Analysis of the Knee Joint. Ann. Biomed. Eng. 2023, 51, 10–23. [Google Scholar] [CrossRef]
- Marieswaran, M.; Sikidar, A.; Goel, A.; Joshi, D.; Kalyanasundaram, D. An extended OpenSim knee model for analysis of strains of connective tissues. Biomed. Eng. Online 2018, 17, 42. [Google Scholar] [CrossRef]
- Xu, H.; Bloswick, D.; Merryweather, A. An improved OpenSim gait model with multiple degrees of freedom knee joint and knee ligaments. Comput. Methods Biomech. Biomed. Eng. 2015, 18, 1217–1224. [Google Scholar] [CrossRef]
- Arnold, E.M.; Ward, S.R.; Lieber, R.L.; Delp, S.L. A Model of the Lower Limb for Analysis of Human Movement. Ann. Biomed. Eng. 2010, 38, 269–279. [Google Scholar] [CrossRef]
- Guess, T.M.; Razu, S. Loading of the medial meniscus in the ACL deficient knee: A multibody computational study. Med. Eng. Phys. 2017, 41, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Razu, S.S.; Kuroki, K.; Cook, J.L.; Guess, T.M. Function of the Anterior Intermeniscal Ligament. J. Knee Surg. 2018, 31, 068–074. [Google Scholar] [CrossRef]
- Minns, R. Rorces at the knee joint: Anatomical considerations. J. Biomech. 1981, 14, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Kettelkamp, D.B.; Chao, E.Y.M. A Method for Quantitative Analysis of Medial and Lateral Compression Forces at the Knee During Standing. Clin. Orthop. Relat. Res. 1972, 83, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Maquet, P.G.; Pelzer, G.A. Evolution of the maximum stress in osteo-arthritis of the knee. J. Biomech. 1977, 10, 107–117. [Google Scholar] [CrossRef]
- Asseln, M.; Eschweiler, J.; Trepczynski, A.; Damm, P.; Radermacher, K.; Masani, K. Evaluation and validation of 2D biomechanical models of the knee for radiograph-based preoperative planning in total knee arthroplasty. PLoS ONE 2020, 15, e0227272. [Google Scholar] [CrossRef]
- Schmidt, A.M.; Stockton, D.J.; Hunt, M.A.; Yung, A.; Masri, B.A.; Wilson, D.R. Reliability of tibiofemoral contact area and centroid location in upright, open MRI. BMC Musculoskelet. Disord. 2020, 21, 795. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Jansen, M.P.; Besselink, N.J.; van Heerwaarden, R.J.; Custers, R.J.H.; Emans, P.J.; Spruijt, S.; Mastbergen, S.C.; Lafeber, F.P.J.G. Knee Joint Distraction Compared with High Tibial Osteotomy and Total Knee Arthroplasty: Two-Year Clinical, Radiographic, and Biochemical Marker Outcomes of Two Randomized Controlled Trials. Cartilage 2021, 12, 181–191. [Google Scholar] [CrossRef]
- Diduch, D.R.; Crawford, D.C.; Ranawat, A.S.; Victor, J.; Flanigan, D.C. Implantable Shock Absorber Provides Superior Pain Relief and Functional Improvement Compared with High Tibial Osteotomy in Patients with Mild-to-Moderate Medial Knee Osteoarthritis: A 2-Year Report. Cartilage 2023, 14, 152–163. [Google Scholar] [CrossRef]
- van Outeren, M.; Waarsing, J.; Brouwer, R.; Verhaar, J.; Reijman, M.; Bierma-Zeinstra, S. Is a high tibial osteotomy (HTO) superior to non-surgical treatment in patients with varus malaligned medial knee osteoarthritis (OA)? A propensity matched study using 2 randomized controlled trial (RCT) datasets. Osteoarthr. Cartil. 2017, 25, 1988–1993. [Google Scholar] [CrossRef] [PubMed]
- Jansen, M.; Maschek, S.; Van Heerwaarden, R.; Mastbergen, S.; Wirth, W.; Lafeber, F.; Eckstein, F. Knee joint distraction is more efficient in rebuilding cartilage thickness in the more affected compartment than high tibial osteotomy in patients with knee osteoarthritis. Osteoarthr. Cartil. 2019, 27, S330–S331. [Google Scholar] [CrossRef]
- van der Woude, J.A.D.; Wiegant, K.; van Heerwaarden, R.J.; Spruijt, S.; van Roermund, P.M.; Custers, R.J.H.; Mastbergen, S.C.; Lafeber, F.P.J.G. Knee joint distraction compared with high tibial osteotomy: A randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 876–886. [Google Scholar] [CrossRef]
- van der Woude, J.A.D.; Wiegant, K.; van Heerwaarden, R.J.; Spruijt, S.; Emans, P.J.; Mastbergen, S.C.; Lafeber, F.P.J.G. Knee joint distraction compared with total knee arthroplasty. Bone Jt. J. 2017, 99-B, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Jansen, M.P.; Mastbergen, S.C.; van Heerwaarden, R.J.; Spruijt, S.; van Empelen, M.D.; Kester, E.C.; Lafeber, F.P.J.G.; Custers, R.J.H.; Farouk, O. Knee joint distraction in regular care for treatment of knee osteoarthritis: A comparison with clinical trial data. PLoS ONE 2020, 15, e0227975. [Google Scholar] [CrossRef]
- Hoorntje, A.; Kuijer, P.P.F.M.; Koenraadt, K.L.M.; Waterval-Witjes, S.; Kerkhoffs, G.M.M.J.; Mastbergen, S.C.; Marijnissen, A.C.A.; Jansen, M.P.; van Geenen, R.C.I. Return to Sport and Work after Randomization for Knee Distraction versus High Tibial Osteotomy: Is There a Difference? J. Knee Surg. 2022, 35, 949–958. [Google Scholar] [CrossRef]
- Slynarski, K.; Walawski, J.; Smigielski, R.; van der Merwe, W. Two-Year Results of the PHANTOM High Flex Trial: A Single-Arm Study on the Atlas Unicompartmental Knee System Load Absorber in Patients with Medial Compartment Osteoarthritis of the Knee. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2019, 12, 117954411987717. [Google Scholar] [CrossRef]
- Della Croce, U.; Crapanzano, F.; Li, L.; Kasi, P.K.; Patritti, B.L.; Mancinelli, C.; Hunter, D.J.; Stamenović, D.; Harvey, W.F.; Bonato, P. A Preliminary Assessment of a Novel Pneumatic Unloading Knee Brace on the Gait Mechanics of Patients with Knee Osteoarthritis. PM&R 2013, 5, 816–824. [Google Scholar] [CrossRef]
- Mauricio, E.; Sliepen, M.; Rosenbaum, D. Acute effects of different orthotic interventions on knee loading parameters in knee osteoarthritis patients with varus malalignment. Knee 2018, 25, 825–833. [Google Scholar] [CrossRef]
- Fischer, A.G.; Wolf, A. Assessment of the effects of body weight unloading on overground gait biomechanical parameters. Clin. Biomech. 2015, 30, 454–461. [Google Scholar] [CrossRef]
- Laroche, D.; Morisset, C.; Fortunet, C.; Gremeaux, V.; Maillefert, J.-F.; Ornetti, P. Biomechanical effectiveness of a distraction–rotation knee brace in medial knee osteoarthritis: Preliminary results. Knee 2014, 21, 710–716. [Google Scholar] [CrossRef]
- Ornetti, P.; Fortunet, C.; Morisset, C.; Gremeaux, V.; Maillefert, J.; Casillas, J.; Laroche, D. Clinical effectiveness and safety of a distraction-rotation knee brace for medial knee osteoarthritis. Ann. Phys. Rehabil. Med. 2015, 58, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, L.-F.; Lin, Y.-T.; Wang, C.-P.; Liu, Y.-F.; Tsai, C.-T. Comparison of the effect of Western-made unloading knee brace with physical therapy in Asian patients with medial compartment knee osteoarthritis—A preliminary report. J. Formos. Med. Assoc. 2020, 119, 319–326. [Google Scholar] [CrossRef]
- Duivenvoorden, T.; van Raaij, T.M.; Horemans, H.L.D.; Brouwer, R.W.; Bos, K.P.; Bierma-Zeinstra, S.M.A.; Verhaar, J.A.N.; Reijman, M. Do Laterally Wedged Insoles or Valgus Braces Unload the Medial Compartment of the Knee in Patients with Osteoarthritis? Clin. Orthop. Relat. Res. 2015, 473, 265–274. [Google Scholar] [CrossRef]
- Ebert, J.R.; Hambly, K.; Joss, B.; Ackland, T.R.; Donnelly, C.J. Does an Unloader Brace Reduce Knee Loading in Normally Aligned Knees? Clin. Orthop. Relat. Res. 2014, 472, 915–922. [Google Scholar] [CrossRef]
- Hall, M.; Starkey, S.; Hinman, R.S.; Diamond, L.E.; Lenton, G.K.; Knox, G.; Pizzolato, C.; Saxby, D.J.; Abdelbasset, W.K. Effect of a valgus brace on medial tibiofemoral joint contact force in knee osteoarthritis with varus malalignment: A within-participant cross-over randomised study with an uncontrolled observational longitudinal follow-up. PLoS ONE 2022, 17, e0257171. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.P.; Williams, M.; Eyles, J.P.; Chen, J.S.; Makovey, J.; Hunter, D.J. Effectiveness of knee bracing in osteoarthritis: Pragmatic trial in a multidisciplinary clinic. Int. J. Rheum. Dis. 2016, 19, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Khademi-Kalantari, K.; Aghdam, S.M.; Baghban, A.A.; Rezayi, M.; Rahimi, A.; Naimee, S. Effects of non-surgical joint distraction in the treatment of severe knee osteoarthritis. J. Bodyw. Mov. Ther. 2014, 18, 533–539. [Google Scholar] [CrossRef]
- Konopka, J.A.; Finlay, A.K.; Eckstein, F.; Dragoo, J.L. Effects of unloader bracing on clinical outcomes and articular cartilage regeneration following microfracture of isolated chondral defects: A randomized trial. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2889–2898. [Google Scholar] [CrossRef]
- Dwarakanathan, R.; Mohanty, R.K.; Sahoo, S.; Prasad, S. Efficacy of unloader knee orthosis and lateral wedge insole on static balance in medial knee osteoarthritis. J. Orthop. Trauma Rehabil. 2022, 29, 221049172210952. [Google Scholar] [CrossRef]
- Kapadia, B.H.; Cherian, J.J.; Starr, R.; Chughtai, M.; Harwin, S.F.; Bhave, A.; Mont, M.A. Gait Using Pneumatic Brace for End-Stage Knee Osteoarthritis. J. Knee Surg. 2016, 29, 218–223. [Google Scholar] [CrossRef]
- Van Egmond, N.; Van Grinsven, S.; Van Loon, C.J. Is There a Difference in Outcome Between Two Types of Valgus Unloading Braces? A Randomized Controlled Trial. Acta Orthop. Belg. 2017, 83, 690–699. [Google Scholar] [PubMed]
- Abdel-Aal, N.M.; Ibrahim, A.H.; Kotb, M.M.; Hussein, A.A.; Hussein, H.M. Mechanical traction from different knee joint angles in patients with knee osteoarthritis: A randomized controlled trial. Clin. Rehabil. 2022, 36, 1083–1096. [Google Scholar] [CrossRef]
- Petersen, W.; Ellermann, A.; Henning, J.; Nehrer, S.; Rembitzki, I.V.; Fritz, J.; Becher, C.; Albasini, A.; Zinser, W.; Laute, V.; et al. Non-operative treatment of unicompartmental osteoarthritis of the knee: A prospective randomized trial with two different braces—Ankle–foot orthosis versus knee unloader brace. Arch. Orthop. Trauma Surg. 2019, 139, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Hjartarson, H.F.; Toksvig-Larsen, S. The clinical effect of an unloader brace on patients with osteoarthritis of the knee, a randomized placebo controlled trial with one year follow up. BMC Musculoskelet. Disord. 2018, 19, 341. [Google Scholar] [CrossRef] [PubMed]
- Robert-Lachaine, X.; Dessery, Y.; Belzile, É.L.; Turmel, S.; Corbeil, P. Three-month efficacy of three knee braces in the treatment of medial knee osteoarthritis in a randomized crossover trial. J. Orthop. Res. 2020, 38, 2262–2271. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- van Heerwaarden, R.J.; Verra, W. Knee joint distraction in the treatment of severe osteoarthritis. Arthroskopie 2020, 33, 10–14. [Google Scholar] [CrossRef]
- Intema, F.; Van Roermund, P.M.; Marijnissen, A.C.A.; Cotofana, S.; Eckstein, F.; Castelein, R.M.; Bijlsma, J.W.J.; Mastbergen, S.C.; Lafeber, F.P.J.G. Tissue structure modification in knee osteoarthritis by use of joint distraction: An open 1-year pilot study. Ann. Rheum. Dis. 2011, 70, 1441–1446. [Google Scholar] [CrossRef]
- Jansen, M.P.; Maschek, S.; van Heerwaarden, R.J.; Mastbergen, S.C.; Wirth, W.; Lafeber, F.P.J.G.; Eckstein, F. Changes in Cartilage Thickness and Denuded Bone Area after Knee Joint Distraction and High Tibial Osteotomy—Post-Hoc Analyses of Two Randomized Controlled Trials. J. Clin. Med. 2021, 10, 368. [Google Scholar] [CrossRef]
- Lee, D.C.; Byun, S.J. High Tibial Osteotomy. Knee Surg. Relat. Res. 2012, 24, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Slynarski, K.; Lipinski, L. Treating Early Knee Osteoarthritis with the Atlas® Unicompartmental Knee System in a 26-Year-Old Ex-Professional Basketball Player: A Case Study. Case Rep. Orthop. 2017, 2017, 5020619. [Google Scholar] [CrossRef]
- Clifford, A.G.; Gabriel, S.M.; Connell, O.; Lowe, D.; Miller, L.E.; Block, J. The KineSpring® Knee Implant System: An implantable joint-unloading prosthesis for treatment of medial knee osteoarthritis. Med. Dev. 2013, 6, 69–76. [Google Scholar] [CrossRef]
- Block, J.; London, N.J.; Smith; Miller, L. Bridging the osteoarthritis treatment gap with the KineSpring Knee Implant System: Early evidence in 100 patients with 1-year minimum follow-up. Orthop. Res. Rev. 2013, 5, 65–73. [Google Scholar] [CrossRef][Green Version]
- Walpole, S.C.; Prieto-Merino, D.; Edwards, P.; Cleland, J.; Stevens, G.; Roberts, I. The weight of nations: An estimation of adult human biomass. BMC Public Health 2012, 12, 439. [Google Scholar] [CrossRef]
- Ramsey, D.K.; Russell, M.E. Unloader Braces for Medial Compartment Knee Osteoarthritis: Implications on Mediating Progression. Sports Health 2009, 1, 416–426. [Google Scholar] [CrossRef]
- Murphy, D.P.; Webster, J.B.; Lovegreen, W.; Simoncini, A. Lower Limb Orthoses. In Braddom’s Physical Medicine and Rehabilitation; Elsevier: Amsterdam, The Netherlands, 2021; pp. 229–247. [Google Scholar] [CrossRef]
- Hryvniak, D.; Wilder, R.P.; Jenkins, J.; Statuta, S.M. Therapeutic Exercise. In Braddom’s Physical Medicine and Rehabilitation; Elsevier: Amsterdam, The Netherlands, 2021; pp. 291–315. [Google Scholar] [CrossRef]
- Atchison, J.W.; Tolchin, R.B.; Ross, B.S.; Eubanks, J.E. Manipulation, Traction, and Massage. In Braddom’s Physical Medicine and Rehabilitation; Elsevier: Amsterdam, The Netherlands, 2021; pp. 316–337. [Google Scholar] [CrossRef]
- Goh, E.L.; Lou, W.C.N.; Chidambaram, S.; Ma, S. The role of joint distraction in the treatment of knee osteoarthritis: A systematic review and quantitative analysis. Orthop. Res. Rev. 2019, 11, 79–92. [Google Scholar] [CrossRef]
- Jansen, M.P.; Boymans, T.A.; Custers, R.J.; Van Geenen, R.C.; Van Heerwaarden, R.J.; Huizinga, M.R.; Nellensteijn, J.M.; Sollie, R.; Spruijt, S.; Mastbergen, S.C. Knee Joint Distraction as Treatment for Osteoarthritis Results in Clinical and Structural Benefit: A Systematic Review and Meta-Analysis of the Limited Number of Studies and Patients Available. Cartilage 2021, 13, 1113S–1123S. [Google Scholar] [CrossRef] [PubMed]
- Cerejo, R.; Dunlop, D.D.; Cahue, S.; Channin, D.; Song, J.; Sharma, L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002, 46, 2632–2636. [Google Scholar] [CrossRef]
- Otsuki, S.; Nakajima, M.; Okamoto, Y.; Oda, S.; Hoshiyama, Y.; Iida, G.; Neo, M. Correlation between varus knee malalignment and patellofemoral osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 176–181. [Google Scholar] [CrossRef]
- Coakley, A.; McNicholas, M.; Biant, L.; Tawy, G. A systematic review of outcomes of high tibial osteotomy for the valgus knee. Knee 2023, 40, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Sabzevari, S.; Ebrahimpour, A.; Roudi, M.K.; Kachooei, A.R. High Tibial Osteotomy: A Systematic Review and Current Concept. Arch. Bone Jt. Surg. 2016, 4, 204–212. [Google Scholar]
- Hayes, D.A.; Waller, C.S.; Li, C.S.; Vannabouathong, C.; Sprague, S.; Bhandari, M. Safety and Feasibility of a KineSpring Knee System for the Treatment of Osteoarthritis: A Case Series. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2015, 8, 47–54. [Google Scholar] [CrossRef]
- Richardson, J.B. The Treatment of Medial Compartmental Knee Osteoarthritis (OA) Symptoms with the KineSpringTM Unicompartmental Knee Arthroplasty (UKA) System. Available online: https://doi.org/10.1186/ISRCTN63048529 (accessed on 18 July 2024).
- Pareek, A.; Parkes, C.W.; Gomoll, A.H.; Krych, A.J. Improved 2-Year Freedom from Arthroplasty in Patients with High-Risk SIFK Scores and Medial Knee Osteoarthritis Treated with an Implantable Shock Absorber versus Non-Operative Care. Cartilage 2023, 14, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Chughtai, M.; Bhave, A.; Khan, S.Z.; Khlopas, A.; Ali, O.; Harwin, S.F.; Mont, M.A. Clinical Outcomes of a Pneumatic Unloader Brace for Kellgren–Lawrence Grades 3 to 4 Osteoarthritis: A Minimum 1-Year Follow-Up Study. J. Knee Surg. 2016, 29, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Barati, K.; Kamyab, M.; Takamjani, I.E.; Bidari, S.; Parnianpour, M. Effect of equipping an unloader knee orthosis with vibrators on pain, function, stiffness, and knee adduction moment in people with knee osteoarthritis: A pilot randomized trial. Gait Posture 2023, 99, 83–89. [Google Scholar] [CrossRef]
- Oliveira, S.; Andrade, R.; Valente, C.; Espregueira-Mendes, J.; Silva, F.; Hinckel, B.B.; Carvalho, Ó.; Leal, A. Mechanical-based therapies may reduce pain and disability in some patients with knee osteoarthritis: A systematic review with meta-analysis. Knee 2022, 37, 28–46. [Google Scholar] [CrossRef]
- Oliveira, S.; Andrade, R.; Hinckel, B.B.; Silva, F.; Espregueira-Mendes, J.; Carvalho, Ó.; Leal, A. In Vitro and In Vivo Effects of Light Therapy on Cartilage Regeneration for Knee Osteoarthritis: A Systematic Review. Cartilage 2021, 13, 1700S–1719S. [Google Scholar] [CrossRef]
- Petersen, W.; Ellermann, A.; Zantop, T.; Rembitzki, I.V.; Semsch, H.; Liebau, C.; Best, R. Biomechanical effect of unloader braces for medial osteoarthritis of the knee: A systematic review (CRD 42015026136). Arch. Orthop. Trauma Surg. 2016, 136, 649–656. [Google Scholar] [CrossRef]
- Raposo, F.; Ramos, M.; Cruz, A.L. Effects of exercise on knee osteoarthritis: A systematic review. Musculoskelet. Care 2021, 19, 399–435. [Google Scholar] [CrossRef]
- Mo, L.; Jiang, B.; Mei, T.; Zhou, D. Exercise Therapy for Knee Osteoarthritis: A Systematic Review and Network Meta-analysis. Orthop. J. Sports Med. 2023, 11, 232596712311727. [Google Scholar] [CrossRef] [PubMed]
- Jamtvedt, G.; Dahm, K.T.; Christie, A.; Moe, R.H.; Haavardsholm, E.; Holm, I.; Hagen, K.B. Physical Therapy Interventions for Patients with Osteoarthritis of the Knee: An Overview of Systematic Reviews. Phys. Ther. 2008, 88, 123–136. [Google Scholar] [CrossRef]
- Holder, J.; van Drongelen, S.; Uhlrich, S.D.; Herrmann, E.; Meurer, A.; Stief, F. Peak knee joint moments accurately predict medial and lateral knee contact forces in patients with valgus malalignment. Sci. Rep. 2023, 13, 2870. [Google Scholar] [CrossRef] [PubMed]
- Manal, K.; Gardinier, E.; Buchanan, T.; Snyder-Mackler, L. A more informed evaluation of medial compartment loading: The combined use of the knee adduction and flexor moments. Osteoarthr. Cartil. 2015, 23, 1107–1111. [Google Scholar] [CrossRef]
- Creaby, M. It’s not all about the knee adduction moment: The role of the knee flexion moment in medial knee joint loading. Osteoarthr. Cartil. 2015, 23, 1038–1040. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, N.; Silva, F.S.; Carvalho, Ó.; Leal, A. The effect that Lower Limb orthoses have on cartilage on patients with knee osteoarthritis: A narrative review. Prosthet. Orthot. Int. 2022, 47, 466–476. [Google Scholar] [CrossRef] [PubMed]
- Kattan, A.E.; AlHemsi, H.B.; AlKhawashki, A.M.; AlFadel, F.B.; Almoosa, S.M.; Mokhtar, A.M.; Alasmari, B.A. Patient Compliance with Physical Therapy Following Orthopedic Surgery and Its Outcomes. Cureus 2023, 15, e37217. [Google Scholar] [CrossRef]
- Davies, G.; Yeomans, D.; Tolkien, Z.; Kreis, I.A.; Potter, S.; Gardiner, M.D.; Jain, A.; Henderson, J.; Blazeby, J.M. Methods for assessment of patient adherence to removable orthoses used after surgery or trauma to the appendicular skeleton: A systematic review. Trials 2020, 21, 507. [Google Scholar] [CrossRef]
- Cinthuja, P.; Krishnamoorthy, N.; Shivapatham, G. Effective interventions to improve long-term physiotherapy exercise adherence among patients with lower limb osteoarthritis. A systematic review. BMC Musculoskelet. Disord. 2022, 23, 147. [Google Scholar] [CrossRef]
- Thirumaran, A.J.; Deveza, L.A.; Atukorala, I.; Hunter, D.J. Assessment of Pain in Osteoarthritis of the Knee. J. Pers. Med. 2023, 13, 1139. [Google Scholar] [CrossRef]


| Ref. | Experimental | Comparator | Population | Patients | Outcome | Follow-Up | Result |
|---|---|---|---|---|---|---|---|
| [36] | KJD | HTO | Mild and Severe Knee OA Patients | 18 | JSW | 2 years | 0.22 |
| KJD | TKA | 18 | JSW | 0.15 | |||
| HTO | KJD | 33 | JSW | −0.47 | |||
| [37] | ISA | HTO | Mild Symptomatic Knee OA | 73 | WOMAC (Total) | 2 years | 46.2 |
| HTO | ISA | 65 | WOMAC (Total) | 33 | |||
| [38] | KUB | Regular Care | Mild Symptomatic Knee OA | 30 | VAS (Pain) | 1 year | −0.1 |
| HTO (Open Wedge) | HTO (Closed Wedge) | 83 | 0 | ||||
| [39] | KJD | TKA | Mild and Severe Knee OA Patients | 20 | WOMAC (Total) | 2 years | 38.9 |
| KOOS | 28.7 | ||||||
| JSW | 0.99 | ||||||
| VAS (Pain) | −3.19 | ||||||
| KJD | HTO | 23 | WOMAC (Total) | 26.8 | |||
| KOOS | 21.6 | ||||||
| JSW | 0.83 | ||||||
| VAS (Pain) | −2.14 | ||||||
| HTO | KJD | 46 | WOMAC (Total) | 34.4 | |||
| KOOS | 30 | ||||||
| JSW | 0.88 | ||||||
| VAS (Pain) | −3.85 | ||||||
| [40] | KJD | HTO | Mild and Severe Knee OA Patients | 23 | JSW | 1 year | 0.5 |
| WOMAC (Total) | 18 | ||||||
| KOOS (Total) | 17 | ||||||
| HTO | KJD | 46 | JSW | 0.2 | |||
| WOMAC (Total) | 29 | ||||||
| KOOS (Total) | 19 | ||||||
| [41] | KJD | TKA | Severe Knee OA Patients | 20 | JSW | 1 year | 1.9 |
| WOMAC (Total) | 30 | ||||||
| KOOS (Total) | 27 | ||||||
| VAS (Pain) | -3.6 | ||||||
| [42] | KJD | KJD | Mild and Severe Knee OA Patients | 84 | WOMAC (Total) | 6 Weeks | 22.2 |
| KJD | KJD | 62 | WOMAC (Total) | 28.3 | |||
| [43] | KJD | HTO | Knee OA Patients that Underwent KJD or HTO | 16 | RTS | 1 year | 0.79 |
| RTW | 0.94 | ||||||
| HTO | HTO | 35 | RTS | 0.8 | |||
| RTW | 0.97 | ||||||
| [44] | ISA | - | Patients with Knee OA that Underwent ISA Surgery | 26 | WOMAC (Pain) | 2 years | 38.5 |
| 26 | WOMAC (Function) | 29.5 | |||||
| [45] | KUB | PKUB | Knee OA Patients | 14 | PKAM | No Follow-up | −0.82 |
| PKUB | KUB | 14 | PKAM | −0.75 | |||
| [46] | KUB | Regular Care | Medial Knee OA Patients | 52 | PKAM | No Follow-up | −0.02 |
| [47] | PT | Regular Care | Healthy Patients | 10 | GV | No Follow-up | 0.03 |
| [48] | DRKB | Regular Care | Symptomatic Medial Knee OA | 20 | VAS (Pain) | 5 weeks | −3.3 |
| WOMAC (Total) | 20.66666667 | ||||||
| GV | 0.1 | ||||||
| PKAM | 0.018 | ||||||
| [49] | DRKB | - | Medial Knee OA Patients | 20 | KOOS | 52 weeks | 13.62 |
| VAS (Pain) | −25 | ||||||
| GV | 0.1 | ||||||
| [50] | KUB | PT | Severe knee OA Patients | 20 | Pain (VAS) | 1 year | −2.3 |
| PT | KUB | 21 | Pain (VAS) | −2.3 | |||
| [51] | KUB | LWI | Medial Knee OA Patients | 20 | PKAM | No Follow-up | 0.05 |
| GRF | 0 | ||||||
| PKAM | 6 months | 0.01 | |||||
| GRF | 0.02 | ||||||
| [52] | KUB | Regular Care | Healthy Patients | 20 | PKAM | No Follow-up | 0.015 |
| GV | 0.02 | ||||||
| [53] | KUB | Regular Care | Medial Radiographic Knee OA and Varus Malalignment | 30 | GV | 8 weeks | 0.05 |
| 30 | KOOS | 21.64 | |||||
| [54] | KUB | Regular Care | Symptomatic, Radiographic Knee OA | 50 | Pain (VAS) | 52 weeks | −1.34 |
| 86 | Pain (VAS) | −1.36 | |||||
| [55] | PT | Regular Care | Severe Knee OA Patients | 40 | KOOS (Total) | 1 month | 19.92 |
| [56] | KUB | Regular Care | Patients who Underwent Microfracture | 24 | Cartilage Thickness (MRI) | 24 months | 0.4 |
| KOOS (Total) | 17.8 | ||||||
| [57] | KUB | Lateral Wedge Insole | Medial Knee OA Patients | 33 | GV | 6 months | 0.06 |
| KOOS (Total) | 29.22 | ||||||
| [58] | PKUB | Regular Care | Knee OA Patients | 24 | GV | 3 months | 0.093 |
| [59] | KUB | KUB | Medial Knee OA Patients | 50 | WOMAC (Total) | 12 Weeks | 16.3 |
| KUB | KUB | 50 | WOMAC (Total) | 10.5 | |||
| [60] | PT | Regular care | Knee OA Patients | 120 | VAS (Pain) | 4 weeks | −2.3 |
| WOMAC (Total) | 6.17 | ||||||
| [61] | KUB | AFO | Medial Knee OA Patients | 62 | KOOS (Function) | 6 months | 10.6 |
| [62] | KUB | Placebo | Knee OA Patients | 74 | KOOS (Total) | 52 weeks | 8.92 |
| [63] | KUB | KUB | Medial Knee OA Patients | 7 | KOOS (Total) | 3 months | 9 |
| KUB | KUB | 7 | 7.2 | ||||
| KUB | KUB | 7 | 13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, N.A.T.C.; Arieira, A.; Hinckel, B.; Silva, F.S.; Carvalho, Ó.; Leal, A. Unlocking the Secrets of Knee Joint Unloading: A Systematic Review and Biomechanical Study of the Invasive and Non-Invasive Methods and Their Influence on Knee Joint Loading. Rheumato 2025, 5, 8. https://doi.org/10.3390/rheumato5030008
Fernandes NATC, Arieira A, Hinckel B, Silva FS, Carvalho Ó, Leal A. Unlocking the Secrets of Knee Joint Unloading: A Systematic Review and Biomechanical Study of the Invasive and Non-Invasive Methods and Their Influence on Knee Joint Loading. Rheumato. 2025; 5(3):8. https://doi.org/10.3390/rheumato5030008
Chicago/Turabian StyleFernandes, Nuno A. T. C., Ana Arieira, Betina Hinckel, Filipe Samuel Silva, Óscar Carvalho, and Ana Leal. 2025. "Unlocking the Secrets of Knee Joint Unloading: A Systematic Review and Biomechanical Study of the Invasive and Non-Invasive Methods and Their Influence on Knee Joint Loading" Rheumato 5, no. 3: 8. https://doi.org/10.3390/rheumato5030008
APA StyleFernandes, N. A. T. C., Arieira, A., Hinckel, B., Silva, F. S., Carvalho, Ó., & Leal, A. (2025). Unlocking the Secrets of Knee Joint Unloading: A Systematic Review and Biomechanical Study of the Invasive and Non-Invasive Methods and Their Influence on Knee Joint Loading. Rheumato, 5(3), 8. https://doi.org/10.3390/rheumato5030008









