Abstract
We experience life and interact with others in a multitude of ways. The term ‘neurodivergence’ refers to variations from what is considered typical or normal. Neurodivergence influences an individual’s behaviour in social situations and is associated with atypical emotional responses. This can precipitate inequity and rejection. Neurodivergent females are especially prone to many physical and psychological health issues, and musculoskeletal disorders account for a significant proportion of these. Research and education into neurodivergent conditions in females should inform the reassessment of clinicians’ present approach to those who present with multiple unexplained symptoms. Obtaining official confirmation of a neurodivergent condition improves access to support services and helps them and their family better understand themselves and the challenges they face. This commentary highlights the increased risk of developing rheumatological disease for females with neurodivergent conditions and suggests how clinicians might increase their awareness of this.
Keywords:
neurodivergence; autism; ADHD; hypermobility; rheumatoid arthritis; osteoporosis; fibromyalgia 1. Key Lessons
- Neurodivergent conditions are under-recognised among females who often present differently to males.
- Neurodivergent females are at an increased risk of developing a wide range of rheumatological disorders.
- These include fibromyalgia, hypermobility, rheumatoid arthritis, osteoporosis and connective tissue disease.
2. What Is Neurodivergence?
While ‘neurodiversity’ represents the wide variation in the approach people take when communicating and socialising [1], the term ‘neurodivergence’ relates more specifically to differences in mental or neurological functioning from the standard norm. This includes autism, attention deficit hyperactivity disorder (ADHD) and Tourette’s syndrome, and there is evidence that a milder form of the same trend accounts for dyslexia and dyspraxia [2]. Social isolation and self-harm are common among females with these conditions, and their physical symptoms are often a reflection of their inner anguish. If we are to better respond to the clinical needs of females with neurodivergent conditions, we need to improve our understanding of their way of thinking and behaving. Their ability to describe their feelings may differ significantly from that of people with normal neurodevelopment (neurotypicals). They might struggle to verbalise their symptoms in a logical or consistent manner, and they may find it hard to deal with persistent questions that try to disentangle what may sometimes seem like a jumble of symptoms without a form timeline. Their expectations of a clinical consultation may often differ to that of the clinician, but it is important that doctors recognise this. We should concentrate on the issues that neurodivergent people describe, rather than the problems that they are [3]. Obtaining official confirmation of a neurodivergent condition improves access to support services and helps them and their family better understand themselves and the challenges they face. This commentary highlights the increased prevalence of rheumatological disease in females with neurodivergent conditions, describes these associations and suggests how rheumatologists can help.
3. The Link between Female Neurodivergence and Heightened Healthcare Needs
Although neurodivergent conditions have been perceived as being the province of males, recent evidence has emerged over the last 10 years that challenges this assumption [4]. The estimated prevalence of autism in the population was often quoted at about 1% with a 4:1 male to female ratio, but this is now thought to represent an underestimate of the true prevalence [4]. It appears that although females often receive their diagnosis later in life, ADHD and autism may be much more prevalent among females than has been appreciated. This may be due to their ability to camouflage their difficulties in order to avoid social rejection or alienation. Because of this, they are more prone to internalise their concerns, resulting in a suppression of their natural tendencies. Such behaviour can trigger intense anxiety, obsession and anger, which may manifest itself in a variety of clinical expressions. They often exhibit heightened sensitivity to emotional and sensory stimuli and find that this makes them feel increased muscle tension and tenderness, producing distress and discomfort [5]. This may be combined with difficulty in making and maintaining close contact with others, leading to a sense of isolation or abandonment. Frequently, this can cause them to feel misunderstood and to lose faith in their own ability, and to lose confidence in other people’s ability and willingness to support them. Autonomic hypersensitivity can be associated with emotional instability and produce a perceived lack of object constancy [6]. Fatigue, muscle tenderness and despair may become evident over time, precipitating a referral to mental health services, a pain team or a rheumatologist.
Autistic people die younger, and they are more prone than their neurotypical peers to a wide range of disorders during their lifetimes [7,8]. A recent review of the literature defined these disorders [9]. Suicide is a major concern among younger neurodivergent females, and the propensity towards developing vascular diseases and diabetes appears to be both increased and accelerated in older females. The mechanisms may include a decrease in physical activity due to fatigue or social anxiety, an increased body mass index, and higher levels of tobacco and alcohol consumption [9]. Masking may contribute to delays in the diagnosis of an underlying neurodivergent condition in females, and such emotional suppression could contribute to the silent progression of these diseases.
Neurodivergent females appear to have worse healthcare outcomes if they have experienced significant adverse experiences during childhood. Females are at a greater risk in this regard, and this might explain their increased use of healthcare resources [10]. A recent review explored the issues described by autistic females with regards to accessing medical care and identified impaired executive function, poor communication and hypersensitivity as all being contributory [11]. Failure of healthcare workers to appreciate these problems led to lower levels of satisfaction and worsening healthcare outcomes [12]. Surprisingly little literature exists specifically on the needs of females with neurodivergent conditions, despite dysfunction of every organ system being listed among the many disorders they report. However, it is established that autistic females are over-represented among all women who seek support for many medical disorders, and it appears that this is especially true for musculoskeletal conditions.
4. The Musculoskeletal Healthcare Needs of Neurodivergent Females
Although data on the prevalence of neurodivergence among patients presenting with rheumatic disease are hard to find, we have calculated that 12% of patients seen in our secondary care rheumatological service are neurodivergent. We discuss the most frequent associations between neurodivergence and rheumatic disease in this section.
Hypermobility spectrum disorders include Ehlers–Danlos (EDS) and these are strongly related to the presence of neurodivergence, especially in females [13]. A reduced sense of balance and poor coordination are often additional features and add to the risk of injury, dislocation or fracture. Formal assessment of the extent of hypermobility using Beighton’s test is recommended to quantify joint laxity, which tends to reduce over time. Teaching proprioceptive exercises and the practice of non-weightbearing exercises such as swimming or cycling can be very helpful, especially when allied to the provision of supportive physiotherapy and joint care techniques. A minority of patients are at risk of vascular complications associated with more severe forms of EDS and may need to be referred to a Clinical Geneticist for further investigation.
Chronic musculoskeletal pain with tenderness to touch and profound fatigue may lead to the suspicion of fibromyalgia in females. This is supported by the presence of autonomic hypersensitivity, which may manifest as postural orthostatic tachycardia syndrome, irritable bowel or recurrent headache. Patients often report trouble sleeping and complain of brain fog. Many such women have features of a neurodivergent condition [14] and there is often also a family history of autism, ADHD and fibromyalgia [15,16]. It appears that hypermobility is also often associated with this symptom complex, and it has been proposed that hypermobility mediates the relationship between fibromyalgia and neurodivergence. Pain clinics report that a significant number of their clientele are females with neurodivergent features, and one report suggested that 77% of young women with autism or ADHD had already manifested features of chronic pain by the age of 27 [17].
Systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) are among the auto-immune disorders reported with greater frequency in the first-degree relatives of neurodivergent females [18]. In general, there is also an increased prevalence of auto-immune conditions among the mothers of neurodivergent women. In addition to maternal auto-immune thyroid disease, both RA [19] and SLE [20,21] are recorded with greater frequency in mothers of neurodivergent female offspring. While maternal RA is associated with a generalised increase in the risk of autism among progeny, maternal SLE is linked to an increased risk for autism only among Caucasian women [22]. The chances of developing both autism and ADHD appear to be increased among the offspring of mothers with RA [23]. Raynaud’s phenomenon may predict or herald the development of a systemic rheumatological auto-immune disorder in neurodivergent female offspring of a mother with auto-immune disease and can be exacerbated by stimulants prescribed for concomitant ADHD [24].
Children with autism exhibit lower bone mineral density across all sites when compared to neurotypical controls [25]. Osteoporosis is reported in females with ADHD and this may be in part a consequence of prescribed stimulants [26]. Bone loss, or reduced bone formation, along with poor balance due to impaired proprioception, causes a much-inflated fracture risk at the hip, spine and forearm in autistic females at all ages. Their odds ratio for hip fractures increases from 8.1 in girls to 24.8 in adult autistic females [27]. Other factors that may contribute to this increased fracture risk include vitamin D deficiency and intestinal dysbiosis from restrictive eating disorders in adolescence.
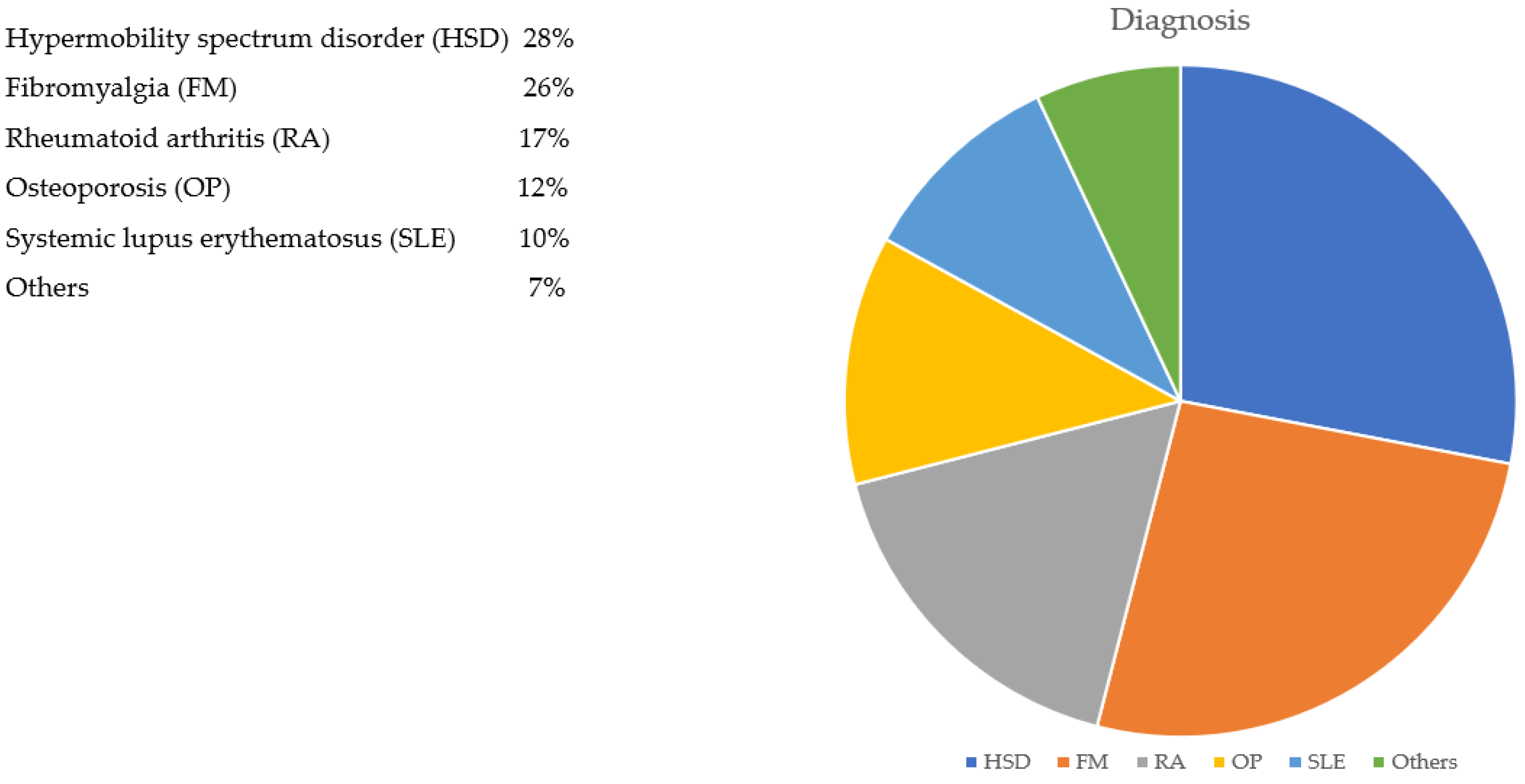
Hormonal factors contribute to the over-representation of neurodivergent females among patients with rheumatic disease. There is substantial evidence that hormones influence both physical and mental symptom expression in neurodivergent females [28], and this is particularly prevalent in perimenopausal women with ADHD [29]. Additionally, the expression of symptoms in both autism and ADHD varies significantly with the time of the month between the menarche and the menopause [30]. Table 1 shows the estimated prevalence of neurodivergence in some common musculoskeletal conditions, while Figure 1 shows the commonest rheumatic diseases diagnosed in neurodivergent females attending rheumatological clinics.

Table 1.
An illustration of the estimated prevalence of neurodivergence in some common musculoskeletal conditions.

Figure 1.
To show the commonest rheumatological diseases diagnosed in 100 neurodivergent females attending hospital clinics.
5. Therapeutic Challenges
Doctors have been slow to recognise the physical features that neurodivergent conditions can manifest in females. Not all females with autism or ADHD are aware of their condition, and those that are neurodivergent may choose not to disclose this. Historically, a label of psychosomatic illness has often been applied to females who exhibit these features, with the concept that such patients can be hard to help. It is time we re-evaluated this approach and adopted a less judgemental attitude. Consistency and continuity of care are important ways to build trust, which neurodivergent people often struggle to achieve. If a diagnosis of a neurodivergent condition is suspected, access to appropriate multidisciplinary support may be appreciated whilst avoiding multiple unnecessary cross-referrals.
A careful explanation of the diagnosis and its relationship to other aspects of the individual’s symptomatology is especially important for neurodivergent females. They need to feel believed and validated in their symptomatology. Even if their condition proves difficult to treat, it is vital that they feel understood and supported both within the consultation and subsequently. Counselling and psychological support may assist such individuals by encouraging them to learn how to share their symptoms and psychosocial challenges in an open and non-combative manner with those who wish to help and support them. Sharing their story with healthcare professionals can be daunting for neurodivergent people because of the variability in their emotional expression, and there is a risk that the full extent of their issues is underestimated as a consequence. In secondary care consultations, sharing the story verbatim in a letter to the primary care physician is helpful, and it is essential that the patient also receives a copy. This also helps to avoid misunderstanding and to ensure that agreed-upon therapeutic plans are followed through with. Obtaining consent for the involvement of other members of the multi-disciplinary team is important where this is proposed. Sharing selective and relevant information on the patient’s condition with specialist nurses, physiotherapists or occupational therapists requires the patient’s knowledge and consent and will likely improve the effectiveness of the intervention.
Many neurodivergent females describe difficulty in tolerating medication. Sensory sensitivities may make them unduly prone to side effects and they may experience these at lower doses than neurotypical women. There are also increased concerns about the potential for addiction in autistic individuals [31]. Starting with a low dose and titrating slowly upwards is generally a good rule. Certain categories of analgesics, such as opiates, also appear to be less effective in, or poorly tolerated by, autistic females, while other agents, including cannabinoids, used off-licence are frequently reported as being useful in relieving pain and distress [32]. It is unclear as to whether these issues are gender-specific in the context of neurodivergence but clinicians observe these issues more often among females. We may need to reconsider our definition of pain in the setting of neurodivergence, given that functional magnetic resonance imaging demonstrates different cerebral responses in neurodivergent females compared to their neurotypical peers. Likewise, immunomodulators may be effective at lower-than-usual doses in neurodivergent females and consensus between the rheumatologist and patient is essential to ensure effective compliance with drug therapy. Access to a helpline is much appreciated by neurodivergent females, especially if there is the option to use email rather than insistence on a telephone call.
Within a rheumatological setting, it is important for clinicians to acquire an appreciation of the range of common disorders experienced by neurodivergent females. The art of ‘learning to listen’ remains an essential tool in diagnoses. Neurodivergent people can feel uncomfortable if they are not given enough time to share their concerns, and an open unhurried dialogue is more likely to facilitate a diagnosis. If patients are encouraged to share their lived experience, it becomes easier for the clinician to ’join the dots’, which may allow the diagnosis of a neurodivergent condition to surface from what may have previously appeared to be a random collection of unrelated symptoms. Likewise, it is essential that clinicians are aware of the broad range of rheumatic conditions commonly experienced by neurodivergent females. If we are to become more effective at managing these conditions, breaking down barriers between services for physical and mental health would be a great help. This may allow the relationship between the limbic, endocrine and immune systems in neurodivergent individuals to be better understood, and clinicians to become more adept at managing their patients with neurodivergent conditions [33].
6. How Patients and the Public Contributed to this Article
Two of the authors of this paper have lived experience of female neurodivergence, and two authors work in the provision of healthcare delivery to females with neurodivergent conditions. Females with autism and/or ADHD specifically requested that we emphasise and explain their medical needs to rheumatologists to improve their access to effective healthcare.
Author Contributions
Conceptualization, R.M. and C.K.; methodology, C.K.; software, all; validation, R.T. and R.M.; writing—original draft preparation, C.K.; writing, R.M. and R.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Singer, J. Odd People in The Birth of Community Amongst People on the “Autistic Spectrum”: A Personal Exploration of a New Social Movement Based on Neurological Diversity. Bachelor’s Thesis, Faculty of Humanities and Social Science, University of Technology, Sydney, Australia, 1998. [Google Scholar]
- Koi, P. Genetics on the neurodiversity spectrum: Genetic, phenotypic and endophenotypic continua in autism and ADHD. Stud. Hist. Philos. Sci. 2021, 89, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Stenning, A.; Rosqvist, H.B. Neurodiversity studies: Mapping out possibilities of a new critical paradigm. Disabil. Soc. 2021, 36, 1532–1537. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Adamo, N.; Ásgeirsdóttir, B.B.; Branney, P.; Beckett, M.; Colley, W.; Cubbin, S.; Deeley, Q.; Farrag, E.; Gudjonsson, G.; et al. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry 2020, 20, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Rynkiewicz, A.; Schuller, B.; Marchi, E.; Piana, S.; Camurri, A.; Lassalle, A.; Baron-Cohen, S. An investigation of the ‘female camouflage effect’ in autism using a computerized ADOS-2 and a test of sex/gender differences. Mol. Autism 2016, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, D.; Lindström, E.; Bingefors, K.; Lewander, T.; Ekselius, L. Gender differences of axis I and II comorbidity in subjects diagnosed with attention-deficit hyperactivity disorder as adults. Acta Neuropsychiatr. 2013, 25, 165–174. [Google Scholar] [PubMed]
- Hirvikoski, T.; Mittendorfer-Rutz, E.; Boman, M.; Larsson, H.; Lichtenstein, P.; Bölte, S. Premature mortality in autism spectrum disorder. Br. J. Psychiatry 2016, 208, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Hand, B.N.; Angell, A.M.; Harris, L.; Carpenter, L.A. Prevalence of physical and mental health conditions in Medicare-enrolled, autistic older adults. Autism 2020, 24, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Weir, E.; Allison, C.; Warrier, V.; Baron-Cohen, S. Increased prevalence of non-communicable physical health conditions among autistic adults. Autism 2021, 25, 681–694. [Google Scholar] [CrossRef]
- Weiss, J.A.; Isaacs, B.; Diepstra, H.; Wilton, A.S.; Brown, H.K.; McGarry, C.; Lunsky, Y. Health Concerns and Health Service Utilization in a Population Cohort of Young Adults with Autism Spectrum Disorder. J. Autism Dev. Disord. 2018, 48, 36–44. [Google Scholar] [CrossRef]
- Mason, D.; Ingham, B.; Urbanowicz, A.; Michael, C.; Birtles, H.; Woodbury-Smith, M.; Brown, T.; James, I.; Scarlett, C.; Nicolaidis, C.; et al. A Systematic Review of What Barriers and Facilitators Prevent and Enable Physical Healthcare Services Access for Autistic Adults. J. Autism Dev. Disord. 2019, 49, 3387–3400. [Google Scholar] [CrossRef]
- Nicolaidis, C.; Raymaker, D.; McDonald, K.; Dern, S.; Boisclair, W.C.; Ashkenazy, E.; Baggs, A. Comparison of Healthcare Experiences in Autistic and Non-Autistic Adults: A Cross-Sectional Online Survey Facilitated by an Academic-Community Partnership. J. Gen. Intern. Med. 2013, 28, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Eccles, J.; Iodice, V.; Dowell, N.; Owens, A.; Hughes, L.; Skipper, S.; Lycette, Y.; Humphries, K.; Harrison, N.; Mathias, C.; et al. Joint hypermobility and autonomic hyperactivity: Relevance to neurodevelopmental disorders. J. Neurol. Neurosurg. Psychiatry 2014, 85, e3. [Google Scholar] [CrossRef]
- Casanova, E.L.; Baeza-Velasco, C.; Buchanan, C.B.; Casanova, M.F. The Relationship between Autism and Ehlers-Danlos Syndromes/Hypermobility Spectrum Disorders. J. Pers. Med. 2020, 10, 260. [Google Scholar] [CrossRef] [PubMed]
- Reyero, F.; Ponce, G.; Rodriguez-Jimenez, R.; Fernandez-Dapica, P.; Taboada, D.; Martin, V.; Navio, M.; Jimenez-Arriero, M.; Hoenicka, J.; Palomo, T. High frequency of childhood ADHD history in women with fibromyalgia. Eur. Psychiatry 2011, 26, 482–483. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.; Martin, R.; Saravanan, V. The Links between Fibromyalgia, Hypermobility and Neurodivergence. Touch Reviews 15 March 2022. Available online: https://www.touchimmunology.com/fibromyalgia/journal-articles/the-links-between-fibromyalgia-hypermobility-and-neurodivergence/ (accessed on 3 May 2023).
- Asztély, K.; Kopp, S.; Gillberg, C.; Waern, M.; Bergman, S. Chronic Pain and Health-Related Quality of Life in Women with Autism and/or ADHD: A Prospective Longitudinal Study. J. Pain Res. 2019, 12, 2925–2932. [Google Scholar] [CrossRef] [PubMed]
- Comi, A.M.; Zimmerman, A.W.; Frye, V.H.; Law, P.A.; Peeden, J.N. Familial Clustering of Autoimmune Disorders and Evaluation of Medical Risk Factors in Autism. J. Child Neurol. 1999, 14, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.-K.; Cheng, Y.-S.; Chen, I.-W.; Chiu, H.-J.; Chung, W.; Tzang, R.-F.; Fan, H.-Y.; Lee, C.-W.; Hung, K.-C. Impact of parental rheumatoid arthritis on risk of autism spectrum disorders in offspring: A systematic review and meta-analysis. Front. Med. 2022, 9, 1052806. [Google Scholar] [CrossRef]
- Dalsgaard, S. More Evidence Linking Autoimmune Diseases to Attention-Deficit/Hyperactivity Disorder. JAMA Pediatr. 2021, 175, e205502. [Google Scholar] [CrossRef]
- Li, D.-J.; Tsai, C.-S.; Hsiao, R.C.; Chen, Y.-L.; Yen, C.-F. Associations between Allergic and Autoimmune Diseases with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder within Families: A Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 4503. [Google Scholar] [CrossRef]
- Zhu, Z.; Tang, S.; Deng, X.; Wang, Y. Maternal Systemic Lupus Erythematosus, Rheumatoid Arthritis, and Risk for Autism Spectrum Disorders in Offspring: A Meta-analysis. J. Autism Dev. Disord. 2020, 50, 2852–2859. [Google Scholar] [CrossRef]
- Chiu, H.-J.; Sun, C.-K.; Tsai, S.-J.; Bai, Y.-M.; Hung, K.-C.; Hsu, J.-W.; Huang, K.-L.; Su, T.-P.; Chen, T.-J.; Sun, A.; et al. A nationwide study of the risks of major mental disorders among the offspring of parents with rheumatoid arthritis. Sci. Rep. 2022, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Umair, H.M.; Sandler, R.D.; Alunno, A.; Matucci-Cerinic, M.; Hughes, M. Association between central nervous system stimulants used to treat attention deficit hyperactivity disorder (ADHD) and Raynaud’s phenomenon: A scoping review. Semin. Arthritis Rheum. 2021, 51, 1200–1204. [Google Scholar] [CrossRef] [PubMed]
- Abadi, M.R.H.; Neumeyer, A.; Misra, M.; Kontulainen, S. Bone health in children and youth with ASD: A systematic review and meta-analysis. Osteoporos. Int. 2021, 32, 1679–1691. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.T.; Walick, K.S.; Rivera, J.C. Preliminary Evidence of an Association between ADHD Medications and Diminished Bone Health in Children and Adolescents. J. Pediatr. Orthop. 2017, 37, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Neumeyer, A.M.; O’rourke, J.A.; Massa, A.; Lee, H.; Lawson, E.A.; McDougle, C.J.; Misra, M. Brief report: Bone fractures in children and adults with autism spectrum disorders. J. Autism Dev. Disord. 2015, 45, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.; Eisenlohr-Moul, T.; Martel, M.M. Reproductive steroids and ADHD symptoms across the menstrual cycle. Psychoneuroendocrinology 2018, 88, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Dorani, F.; Bijlenga, D.; Beekman, A.T.; van Someren, E.J.; Kooij, J.S. Prevalence of hormone-related mood disorder symptoms in women with ADHD. J. Psychiatr. Res. 2021, 133, 10–15. [Google Scholar] [CrossRef]
- Quinn, P.O.; Madhoo, M. A Review of Attention-Deficit/Hyperactivity Disorder in Women and Girls. Prim. Care Companion J. Clin. Psychiatry 2014, 16, pcc.13r01596. [Google Scholar] [CrossRef]
- Butwicka, A.; Långström, N.; Larsson, H.; Lundström, S.; Serlachius, E.; Almqvist, C.; Frisén, L.; Lichtenstein, P. Increased risk for substance use-related problems in autism spectrum disorders: A population-based cohort study. J. Autism Dev. Disord. 2017, 47, 80–89. [Google Scholar] [CrossRef]
- Hill, K.P. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: A clinical review. JAMA 2015, 313, 2474–2483. [Google Scholar] [CrossRef]
- Zerbo, O.; Massolo, M.L.; Qian, Y.; Croen, L.A. A study of physician knowledge and experience with Autism in adults in a large integrated healthcare system. J. Autism Dev. Disord. 2015, 45, 4002–4014. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).