Exploring Dietary Patterns and Their Associations with Obesity in School-Aged Children in Croatia: A Cross-Sectional CroCOSI Study
Abstract
1. Introduction
2. Materials and Methods
- Measurement of Body Weight and Height
- Determination of Nutritional Status
- Assessment of Dietary Patterns
- Association of dietary patterns with childhood obesity
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| FFQ | Food frequency questionnaire |
| PCA | Principal component analysis |
| DP | Dietary pattern |
| M | Mean |
| SD | Standard deviation |
| MDN | Median |
| MIN | Minimum |
| MAX | Maximum |
References
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; USDA: Washington, DC, USA, 2020.
- Craig, L.C.A.; McNeill, G.; Macdiarmid, J.I.; Masson, L.F.; Holmes, B.A. Dietary patterns of school-age children in Scotland: Association with socio-economic indicators, physical activity and obesity. Br. J. Nutr. 2010, 103, 319–334. [Google Scholar] [CrossRef]
- Liberali, R.; Kupek, E.; Assis, M.A.A.D. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Cribb, V.; Emmett, P.; Northstone, K. Dietary patterns throughout childhood and associations with nutrient intakes. Public Health Nutr. 2013, 16, 1801–1809. [Google Scholar] [CrossRef] [PubMed]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef]
- Warkentin, S.; Stratakis, N.; Fabbri, L.; Wright, J.; Yang, T.C.; Bryant, M.; Heude, B.; Slama, R.; Montazeri, P.; Vafeiadi, M.; et al. Dietary patterns among European children and their association with adiposity-related outcomes: A multi-country study. Int. J. Obes. 2025, 49, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Tognon, G.; Moreno, L.A.; Mouratidou, T.; Veidebaum, T.; Molnár, D.; Russo, P.; Siani, A.; Akhandaf, Y.; Krogh, V.; Tornaritis, M.; et al. Adherence to a Mediterranean-like dietary pattern in children from eight European countries. The IDEFICS study. Int. J. Obes. 2014, 38 (Suppl. S2), S108–S114. [Google Scholar] [CrossRef]
- Garrido-Miguel, M.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Rodríguez-Artalejo, F.; Moreno, L.A.; Ruiz, J.R.; Ahrens, W.; Martínez-Vizcaíno, V. Prevalence and Trends of Overweight and Obesity in European Children from 1999 to 2016: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019, 173, e192430. [Google Scholar] [CrossRef] [PubMed]
- Musić Milanović, S.; Križan, H.; Lang Morović, M.; Meštrić, S.; Šlaus, N.; Pezo, A. Europska Inicijativa Praćenja Debljine u Djece, Hrvatska 2021./2022. (CroCOSI); Hrvatski zavod za javno zdravstvo: Zagreb, Croatia, 2024.
- Emmett, P.M.; Jones, L.R.; Northstone, K. Dietary patterns in the Avon Longitudinal Study of Parents and Children. Nutr. Rev. 2015, 73, 207–230. [Google Scholar] [CrossRef]
- Rundle, A.G.; Factor-Litvak, P.; Suglia, S.F.; Susser, E.S.; Kezios, K.L.; Lovasi, G.S.; Cirillo, P.M.; Cohn, B.A.; Link, B.G. Tracking of Obesity in Childhood into Adulthood: Effects on Body Mass Index and Fat Mass Index at Age 50. Child. Obes. 2020, 16, 226–233. [Google Scholar] [CrossRef]
- Ambrosini, G.L. Childhood dietary patterns and later obesity: A review of the evidence. Proc. Nutr. Soc. 2014, 73, 137–146. [Google Scholar] [CrossRef]
- Martínez-González, M.Á.; Martín-Calvo, N. The major European dietary patterns and metabolic syndrome. Rev. Endocr. Metab. Disord. 2013, 14, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Breda, J.; McColl, K.; Buoncristiano, M.; Williams, J.; Abdrakhmanova, S.; Abdurrahmonova, Z.; Ahrens, W.; Akhmedova, D.; Bakacs, M.; Boer, J.M.A.; et al. Methodology and implementation of the WHO European Childhood Obesity Surveillance Initiative (COSI). Obes. Rev. 2021, 22, e13215. [Google Scholar] [CrossRef]
- De Onis, M. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Andridge, R.R.; Little, R.J.A. A Review of Hot Deck Imputation for Survey Non-response. Int. Stat. Rev. 2010, 78, 40–64. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Costello, A.B.; Osborne, J. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 7. [Google Scholar] [CrossRef]
- Nasreddine, L.; Shatila, H.; Itani, L.; Hwalla, N.; Jomaa, L.; Naja, F. A traditional dietary pattern is associated with lower odds of overweight and obesity among preschool children in Lebanon: A cross-sectional study. Eur. J. Nutr. 2019, 58, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Bahreynian, M.; Paknahad, Z.; Maracy, M.R. Major Dietary Patterns and Their Associations with Overweight and Obesity Among Iranian Children. Int. J. Prev. Med. 2013, 4, 448. [Google Scholar]
- Lioret, S.; Touvier, M.; Lafay, L.; Volatier, J.-L.; Maire, B. Dietary and Physical Activity Patterns in French Children Are Related to Overweight and Socioeconomic Status. J. Nutr. 2008, 138, 101–107. [Google Scholar] [CrossRef]
- Rutayisire, E.; Wu, X.; Huang, K.; Tao, S.; Chen, Y.; Wang, S.; Tao, F. Dietary patterns are not associated with overweight and obesity in a sample of 8900 Chinese preschool children from four cities. J. Nutr. Sci. 2018, 7, e24. [Google Scholar] [CrossRef]
- Kelishadi, R.; Heshmat, R.; Mansourian, M.; Motlagh, M.E.; Ziaodini, H.; Taheri, M.; Ahadi, Z.; Aminaee, T.; Goodarzi, A.; Mansourian, M.; et al. Association of dietary patterns with continuous metabolic syndrome in children and adolescents; a nationwide propensity score-matched analysis: The CASPIAN-V study. Diabetol. Metab. Syndr. 2018, 10, 52. [Google Scholar] [CrossRef] [PubMed]
- Oellingrath, I.M.; Svendsen, M.V.; Brantsæter, A.L. Eating patterns and overweight in 9- to 10-year-old children in Telemark County, Norway: A cross-sectional study. Eur. J. Clin. Nutr. 2010, 64, 1272–1279. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Panagiotakos, D.; Psarra, G.; Sidossis, L.S. Recommended dairy intake is associated with healthy dietary habits, better physical fitness, less obesity and a healthier lifestyle profile in school age children. Br. J. Nutr. 2022, 128, 2046–2053. [Google Scholar] [CrossRef] [PubMed]
- Monzani, A.; Ricotti, R.; Caputo, M.; Solito, A.; Archero, F.; Bellone, S.; Prodam, F. A Systematic Review of the Association of Skipping Breakfast with Weight and Cardiometabolic Risk Factors in Children and Adolescents. What Should We Better Investigate in the Future? Nutrients 2019, 11, 387. [Google Scholar] [CrossRef]
- Wang, K.; Niu, Y.; Lu, Z.; Duo, B.; Effah, C.Y.; Guan, L. The effect of breakfast on childhood obesity: A systematic review and meta-analysis. Front. Nutr. 2023, 10, 1222536. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.; Chan, D.; Lau, W.; Lo, D.; Li, L.; Woo, J. A Cross-sectional Study to Examine the Association Between Dietary Patterns and Risk of Overweight and Obesity in Hong Kong Chinese Adolescents Aged 10–12 Years. J. Am. Coll. Nutr. 2014, 33, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; Li, Y.; Liu, A.; Zhang, Q.; Hu, X.; Du, S.; Ma, J.; Xu, G.; Li, Y.; Guo, H.; et al. Dietary Pattern and Its Association with the Prevalence of Obesity and Related Cardiometabolic Risk Factors among Chinese Children. PLoS ONE 2012, 7, e43183. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.E.; Marshall, J.R.; Sechrest, L. Invited Commentary: Factor Analysis and the Search for Objectivity. Am. J. Epidemiol. 1998, 148, 17–19. [Google Scholar] [CrossRef]
- Nanayakkara, J.; Margerison, C.; Booth, A.O.; Worsley, A.; Aydin, G. Parents face several barriers in providing a healthy school lunch for their primary school children: A survey of Victorian (Australian) parents. Health Promot. J. Austr. 2024, 35, 1116–1127. [Google Scholar] [CrossRef]
- Korkalo, L.; Vepsäläinen, H.; Ray, C.; Skaffari, E.; Lehto, R.; Hauta-alus, H.H.; Nissinen, K.; Meinilä, J.; Roos, E.; Erkkola, M. Parents’ Reports of Preschoolers’ Diets: Relative Validity of a Food Frequency Questionnaire and Dietary Patterns. Nutrients 2019, 11, 159. [Google Scholar] [CrossRef]
- Mills, V.C.; Skidmore, P.M.L.; Watson, E.O.; Taylor, R.W.; Fleming, E.A.; Heath, A.-L.M. Relative Validity and Reproducibility of a Food Frequency Questionnaire for Identifying the Dietary Patterns of Toddlers in New Zealand. J. Acad. Nutr. Diet. 2015, 115, 551–558. [Google Scholar] [CrossRef] [PubMed]
| Parameters | M | SD | MDN | MIN | MAX |
|---|---|---|---|---|---|
| Total | |||||
| Body weight (kg) | 33.94 | 8.32 | 32.10 | 17.81 | 92.81 |
| Body height (cm) | 137.57 | 7.01 | 137.45 | 115.25 | 173.45 |
| BMI-for-age | 0.56 | 1.32 | 0.46 | −4.79 | 4.99 |
| Children without obesity | |||||
| Body weight (kg) | 31.41 | 5.46 | 30.80 | 17.81 | 52.31 |
| Body height (cm) | 136.75 | 6.79 | 136.75 | 115.25 | 166.65 |
| BMI-for-age | 0.17 | 1.01 | 0.21 | −4.79 | 2.00 |
| Children with obesity | |||||
| Body weight (kg) | 47.61 | 7.80 | 46.50 | 31.71 | 92.81 |
| Body height (cm) | 141.31 | 7.02 | 140.97 | 122.75 | 173.45 |
| BMI-for-age | 2.70 | 0.57 | 2.56 | 2.01 | 4.99 |
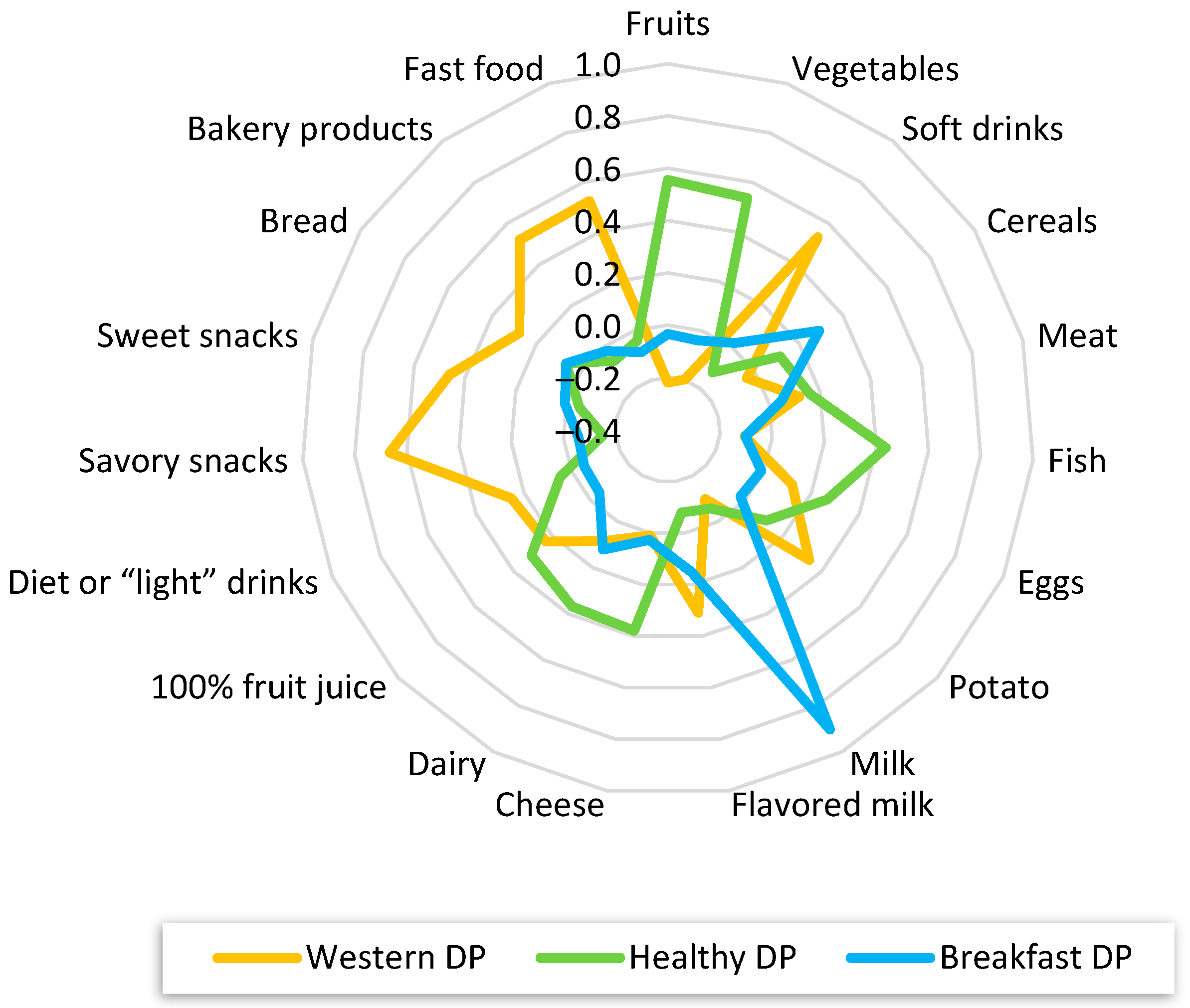
| Missing (%) | Western Dietary Pattern | Healthy Dietary Pattern | Breakfast Dietary Pattern | |
|---|---|---|---|---|
| Fruits | 0.64 | −0.220 | 0.556 | −0.034 |
| Vegetables | 0.71 | −0.196 | 0.536 | −0.039 |
| Soft drinks | 0.57 | 0.532 | −0.122 | 0.020 |
| Cereals | 1.36 | −0.039 | 0.113 | 0.292 |
| Meat | 0.98 | 0.118 | 0.160 | 0.049 |
| Fish | 1.14 | −0.105 | 0.436 | −0.102 |
| Eggs | 1.03 | 0.119 | 0.265 | −0.009 |
| Potato | 1.25 | 0.335 | 0.113 | −0.023 |
| Milk | 1.41 | −0.099 | −0.058 | 0.902 |
| Flavored milk | 2.69 | 0.309 | −0.079 | 0.152 |
| Cheese | 2.64 | 0.010 | 0.379 | 0.027 |
| Dairy | 1.28 | 0.082 | 0.369 | 0.121 |
| 100% fruit juice | 4.62 | 0.232 | 0.309 | −0.045 |
| Diet or “light” drinks | 1.96 | 0.253 | 0.050 | −0.051 |
| Savory snacks | 1.39 | 0.667 | −0.151 | −0.058 |
| Sweet snacks | 1.03 | 0.460 | −0.051 | 0.006 |
| Bread | 1.93 | 0.277 | 0.064 | 0.063 |
| Bakery products | 1.25 | 0.521 | −0.066 | −0.018 |
| Fast food | 1.02 | 0.525 | −0.040 | −0.087 |
| Variance explained by each factor (%) | 10.7 | 7.10 | 5.10 | |
| Cumulative variance (%) | 10.7 | 17.80 | 22.90 |
| Children Without Obesity N (%) | Children with Obesity N (%) | Total N (%) | |
|---|---|---|---|
| Western DP | 1344 (28.40) | 291 (33.22) | 1635 (29.15) |
| Healthy DP | 1514 (32.00) | 243 (27.74) | 1757 (31.33) |
| Breakfast DP | 1874 (39.60) | 342 (39.04) | 2216 (39.52) |
| Coefficient | OR | CI (95%) | p | |
|---|---|---|---|---|
| Western DP | −0.008 | 1.00 | (0.98–1.00) | 0.11 |
| Healthy DP | −0.012 | 0.988 | (0.98–0.99) | 0.045 |
| Breakfast DP | −0.035 | 0.966 | (0.95–0.99) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasanović, J.; Križan, H.; Šatalić, Z.; Musić Milanović, S. Exploring Dietary Patterns and Their Associations with Obesity in School-Aged Children in Croatia: A Cross-Sectional CroCOSI Study. Dietetics 2025, 4, 26. https://doi.org/10.3390/dietetics4030026
Hasanović J, Križan H, Šatalić Z, Musić Milanović S. Exploring Dietary Patterns and Their Associations with Obesity in School-Aged Children in Croatia: A Cross-Sectional CroCOSI Study. Dietetics. 2025; 4(3):26. https://doi.org/10.3390/dietetics4030026
Chicago/Turabian StyleHasanović, Jasmina, Helena Križan, Zvonimir Šatalić, and Sanja Musić Milanović. 2025. "Exploring Dietary Patterns and Their Associations with Obesity in School-Aged Children in Croatia: A Cross-Sectional CroCOSI Study" Dietetics 4, no. 3: 26. https://doi.org/10.3390/dietetics4030026
APA StyleHasanović, J., Križan, H., Šatalić, Z., & Musić Milanović, S. (2025). Exploring Dietary Patterns and Their Associations with Obesity in School-Aged Children in Croatia: A Cross-Sectional CroCOSI Study. Dietetics, 4(3), 26. https://doi.org/10.3390/dietetics4030026








