Abstract
Restricting food intake before consuming alcohol due to weight concerns or to increase alcohol’s intoxicating effects (food and alcohol disturbance, FAD) is a recognised problem in young American college students, but there is less evidence about whether middle-aged and older adults are also engaging in FAD behaviours. A cross-sectional survey of FAD and potential alcohol problems using validated measures (Compensatory Eating and Behaviours in Response to Alcohol Consumption, CEBRACS; Alcohol Use Disorders Identification Test, AUDIT-C) was administered online and in two universities in the north of England to adults aged ≥ 18 years old who had consumed ≥ one alcoholic beverage within the previous month. Most of the 488 participants were ≥25 years (73%) and not university students (72%). Overall, 69% of participants engaged in at least one FAD behaviour in the previous 3 months. The youngest age group (18–24 years) was significantly less likely than the oldest age group (53+ years) to never engage in FAD behaviours: alcohol effects OR (CI) 0.05 (0.02, 0.13); bulimia 0.08 (0.01, 0.67); and restriction 0.21 (0.08, 0.52). Nevertheless, 47% of the oldest age group engaged in at least one FAD-related behaviour, and student status was not associated with FAD behaviours, except for alcohol effects. FAD behaviours were engaged in by most alcohol consumers in this study, including middle- and older-aged adults, and non-students.
1. Introduction
Alcohol consumption, especially heavy episodic drinking (binge drinking), is associated with being a student [1,2], and drinking may be perceived as the social norm, with participating in a heavy drinking culture as important for social acceptance [3,4]. Despite this association with youth, alcohol consumption in middle and older-aged adults, including frequency of consumption, high intakes, and binge drinking, is of concern [5,6,7,8,9], with increasing alcohol use associated with increasing age. For example, in the UK, 31% of 16–24-year-olds drink weekly compared with 59% of 55–64-year-olds. Furthermore, while 62% of those aged 16–24 years drank in the past year, this rose to 85% among 55–74-year-olds [8]. Drinking alcohol, even at low levels, is associated with an increased risk of cardiovascular disease (CVD) and other non-communicable diseases (NCDs), including dementia, some cancers [10,11], and increased risk for depression and suicide [12]. Risks to health increase with increasing age [13], particularly as older people are more vulnerable to the physiological effects of alcohol, even from amounts considered light or moderate for younger generations [14].
Food and alcohol disturbance (FAD), also known as “drunkorexia” [15], encompasses behaviours associated with compensating for the dietary energy in alcohol due to weight concerns, such as restricting food intake, exercising, purging, and diuretic use, and/or restricting food intake prior to and during drinking to enhance the intoxicating effects of alcohol [16]. Behaviours associated with FAD are indicative of disordered eating and alcohol misuse [17,18]. FAD in college/university students is positively associated with higher alcohol intakes and heavy episodic drinking [19,20,21,22,23,24,25]. It is also positively associated with alcohol-related harms, such as memory loss, getting into a physical fight, being injured, having unprotected sex, and being taken advantage of sexually [21], as well as resulting in higher scores on the Rutgers Alcohol Problem Index (RAPI) [24,26,27,28], a measure of adolescent problem drinking that includes items relating to harm [26].
Estimates of FAD prevalence are complicated by how FAD is conceptualised (i.e., weight concern only or including the intoxication effects), which is also reflected in the different measures used. Much of the research has been conducted with college and university students, especially in the USA. For example, Shepherd et al. [29] reviewed FAD in American college students and found that of 36 quantitative studies, half used single-item measures, and one-third did not measure motivations and behaviours associated with enhancing intoxication. Many studies did not report the prevalence, but of those that did, the prevalence ranged from 11% to 56%. In those that used the validated Compensatory Eating and Behaviours in Response to Alcohol Consumption Scale (CEBRACS) [30], which measures behaviours associated with weight concern and intoxication motivations before, during, and after consuming alcohol, the prevalence was similar across studies (40% to 56%) [19,25,31,32,33]. The limited number of studies involving non-American university students have revealed similar findings [23,27,31,34]. There is less evidence about the prevalence of FAD in non-students and older people, but recent studies from Australia [35], USA [36,37], and UK [34,37] indicate that people older than college age and non-students are engaging in FAD behaviours (measured using CEBRACS) with a similar or higher prevalence [34,36], particularly among high-risk drinkers and excessive exercisers [35], as well as identifying that FAD also affects specific groups, such as women who drink to cope with the challenges of parenting [37]. In light of the relatively little evidence compared with American college/university students on engagement with FAD in middle and older-aged adults, especially in the UK, and the concerning levels of alcohol consumption by middle-aged and older adults, this study sought to explore whether UK adults across a range of ages are engaging with alcohol-related behaviours associated with weight concern and with enhancing the intoxicating effects of alcohol.
2. Materials and Methods
2.1. Study Design
A cross-sectional survey using a convenience sample was carried out in the UK using validated measures of FAD behaviours (CEBRACS) [30] and alcohol use [Alcohol Use Disorders Identification Test (AUDIT-C)] [38].
2.2. Participants
The inclusion criteria for participation were to be aged at least 18 years, with no upper age limit, and to have consumed at least one alcoholic beverage within the previous month, with no limit on the quantity or frequency of alcohol consumed. Those who never consume alcohol were excluded from participation. A sample size calculation estimated that 369 participants would be required based on a 40% prevalence of FAD (defined as engaging in at least one FAD behaviour) with a 95% CI of ±10% [39]. We based this calculation on the prevalence in American college students, as measured using CEBRACS [19,25,31,32,33].
2.3. Measures
2.3.1. FAD Behaviours
CEBRACS was used to measure the frequency of behaviours engaged in during the past 3 months before, during, and after alcohol consumption to compensate for the energy in alcohol, or to become intoxicated more quickly [30]. CEBRACS contains 21 items, scored from 1 (Never) to 5 (Almost all the time), comprising four subscales: alcohol effects (7 items, behaviours designed to either become more intoxicated or to become intoxicated faster by eating less); bulimia (6 items, using laxatives, diuretics, and vomiting, as a means to make up for the energy in alcohol); dietary restraint and exercise (6 items, exercising, consuming low-calorie foods or alcoholic drinks, or eating less); and restriction (2 items, missing meals or skipping an entire day or more of meals). Because CEBRACS was developed and validated in an American sample, cognitive interviews [40] were conducted with six participants to ensure UK respondents’ comprehension of the measure’s items, resulting in the addition of a brief explanation of the term diuretics and examples of low-calorie alcoholic drinks.
2.3.2. Alcohol Use
Alcohol use was measured using the UK version of AUDIT-C [38]. Three items measure the frequency of alcohol consumption (Never to ≥4 times/week), the number of units consumed on a typical day (1–2 to ≥10), and the frequency of consuming 6 units of alcohol if female and 8 units of alcohol if male on a single occasion during the last year (never to daily or almost daily). A score of 0–4 indicates a low risk of alcohol dependency, 5–7 increasing risk, 8–10 higher risk, and 11–12 possible alcohol dependency [38]. To aid respondents in answering, an image showing the UK definition of alcohol units was included [41].
2.3.3. Demographics
The demographic information collected was self-identified gender, age group, and whether respondents were students.
2.4. Procedure
Data were collected between February and August 2019 through an online survey platform (eSurv.org), advertised using social media platforms (Instagram, LinkedIn, and Facebook) and a university staff email newsletter, or face-to-face using a paper version of the measures. The latter took place in several locations in the north of England, including at two universities. For the online version, the first page of the survey was a participant information sheet with a consent statement that participants endorsed before being allowed to progress to the measures. For the paper-based version, potential participants, such as students, friends, acquaintances, and work colleagues, were approached by one of two researchers (J.K. or R.B.). The researchers checked that the inclusion criteria were met, provided a verbal explanation of what participation involved and a copy of the participant information sheet, and obtained verbal informed consent before participants self-completed the measures.
2.5. Statistical Analysis
Data were analysed using SPSS (Version 25.0. Armonk, NY, USA: IBM Corp). The CEBRACS measure showed acceptable to excellent internal reliability: CEBRACS total, α = 0.917; alcohol effects, α = 0.966; bulimia, α = 0.750; dietary restraint and exercise, α = 0.868; restriction, α = 0.631. Scores for CEBRACS and its subscales were calculated by summing the responses for the items that make up these measures (see Supplementary Materials). These scores were positively skewed, with a high percentage of respondents choosing “Never” for the FAD behaviours. Therefore, for the purposes of analysis, these highly skewed variables were recoded to create ordinal variables with three categories of “Never”, “Rarely”, and “Regularly”, based on the frequency of performing the relevant behaviours [25]. For example, for the subscale alcohol effects, which has 7 items, the score can range between 7 and 35. This was recoded as Never if the score was 7 (i.e., the equivalent of choosing Never for each item), as Rarely for a score between 8 and 14 (equivalent of choosing Rarely for ≥1 item), and as Regularly for scores ≥ 15 (equivalent of choosing Sometimes, Often or Almost all the time for each item).
The score for AUDIT-C was used to categorise participants into alcohol risk categories. The association between age group and AUDIT-C risk category was examined using a chi-square test for independence, with p values calculated from the adjusted standardised residuals and applying a Bonferroni correction (p < 0.003). Differences in the AUDIT-C score between age groups were assessed using one-way ANOVA, with the Tukey post hoc test.
To examine the relationship between age and FAD behaviours (FAD prevalence, calculated from the CEBRACS total score, and the CEBRACS subscales alcohol effects, bulimia, dietary restraint and exercise, and restriction), cumulative odds ordinal regression with proportional odds analyses were conducted. Alcohol use (AUDIT-C risk category), gender, and student status were entered as control variables. Linear regression, with dummy variables created for the binary variables gender and student status, produced variable inflation factors (VIF) below 1.5 for all variables, indicating no multicollinearity. A chi-square test was used to examine the predictive ability of the age group to predict never engaging in FAD behaviours. Pseudo R2 values (Nagelkerke) are reported to indicate the proportion of variance in FAD behaviours that is explained by the model. The test of parallel lines was used to evaluate whether the odds were equal at each threshold.
3. Results
3.1. Participant Characteristics
Of the initial 504 respondents, three were excluded for not meeting the inclusion criterion of consuming alcohol, six did not indicate their age, and a further seven had missing responses for CEBRACS, resulting in a final sample of 488 respondents. The age groups 53–59 years (n = 42) and 60+ years (n = 26) were combined into one group (53+ years) for the purposes of analysis.
Most participants completed the online version of the measures (n = 410, 84%). The majority of participants were female (see Table 1); there was no difference in age group by gender (χ2 (5, n = 482) = 6.88, p = 0.230, phi 0.119); younger participants were significantly more likely to be students than older participants (χ2 (5, n = 477) = 193.22, p < 0.001, phi 0.636).

Table 1.
Characteristics of the participants (n = 488).
3.2. Alcohol Use
The mean (SD) AUDIT-C score was 6.0 (2.4), with two-thirds (n = 324, 69%) at increased risk of alcohol dependency (i.e., score ≥ 5) (see Table 2). Women scored significantly lower (M = 5.7, SD = 2.3) than men (M = 6.6, SD = 2.7; t (178) = −3.131, p = 0.002); students scored significantly higher than non-students (M = 6.6, SD = 2.4 vs. M = 5.7, SD = 2.4; t (460) = −3.463, p = 0.001). There was a statistically significant difference in AUDIT-C score across the age groups F (5, 466) = 5.834, p < 0.001 (Table 2). There was also a significant association between age group and AUDIT-C risk category (χ2 (10, n = 472) = 28.69, p = 0.001, Cramer’s V = 0.174), with fewer 18–24-year-olds in the low-risk category and more in the highest risk group than expected, more 25–31-year-olds than expected in the low-risk category, and fewer of the oldest group (53+ years) in the highest risk category. However, this was only statistically significant at the Bonferroni adjusted significance level for the 18–24-year-olds in the highest AUDIT-C risk category (p = 0.000145).

Table 2.
Number (n) and percentage (%) of participants for risk of alcohol dependency for the whole sample and by age group.
3.3. Alcohol-Related Compensatory Behaviours
Two-thirds of participants reported engaging in at least one of the alcohol-related compensatory behaviours (Figure 1). Eating less and exercising to compensate for the energy in alcohol (dietary restraint and exercise) was engaged in rarely by 31% and regularly by 29% of participants. This contrasts with behaviours associated with bulimia, where 87% never engaged in these behaviours.
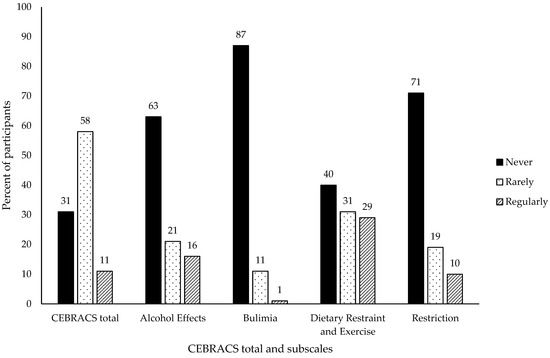
Figure 1.
Percentage of participants reporting engaging “never”, “rarely”, and “regularly” in FAD behaviours for the whole sample.
3.4. Relationship Between Age and FAD Behaviours
The ordinal regression models provided a significant improvement over the baseline intercept-only model for FAD prevalence (χ2 (9) = 118.79, p < 0.001), alcohol effects (χ2 (9) = 193.18, p < 0.001), bulimia (χ2 (9) = 45.44, p < 0.001), dietary restraint and exercise (χ2 (9) = 59.41, p < 0.001), and restriction (χ2 (9) = 85.70, p < 0.001). Goodness of fit was assessed using the Pearson chi-square statistic; the observed data were consistent with the fitted model for FAD prevalence (χ2 (97) = 81.58, p = 0.774), alcohol effects (χ2 (99) = 80.57, p = 0.912), bulimia (χ2 (97) = 74.51, p = 0.956), dietary restraint and exercise (χ2 (99) = 82.96, p = 0.877), and restriction (χ2 (99) = 81.55, p = 0.899). The model provided a significant improvement over the baseline intercept-only model for FAD prevalence (χ2 (9) = 118.79, p < 0.001), alcohol effects (χ2 (9) = 193.18, p < 0.001), bulimia (χ2 (9) = 45.44, p < 0.001), dietary restraint and exercise (χ2 (9) = 59.41, p < 0.001), and restriction (χ2 (9) = 85.70, p < 0.001).
FAD behaviours were engaged in by all age groups, although less frequently by the older age groups (see Figure 2a–e and Table 3). Compared with the oldest age group, the youngest age group were seven times less likely to have never engaged in FAD behaviours, 20 times less likely to have never engaged in restrictive behaviours designed to enhance the intoxication effect of alcohol (alcohol effects), 12 times less likely to have never used diuretics, laxatives or vomited to compensate for the energy in alcohol (bulimia), and nearly five times less likely to have never skipped at least one meal before drinking or not eaten at all for at least one day after drinking to compensate for the energy in alcohol (restriction). The exception to this pattern was for dietary restraint and exercise, with the 25–31 year and 32–38 year age groups significantly less likely to have never engaged in these behaviours compared with those aged ≥ 53 years.
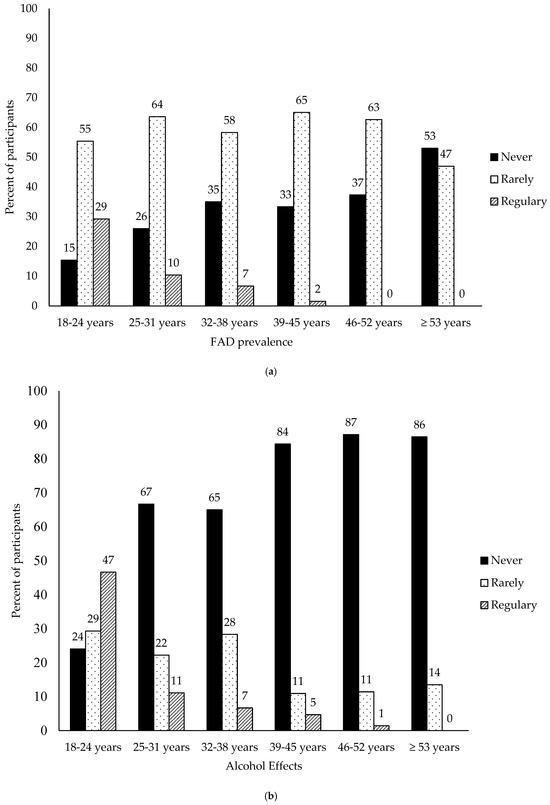
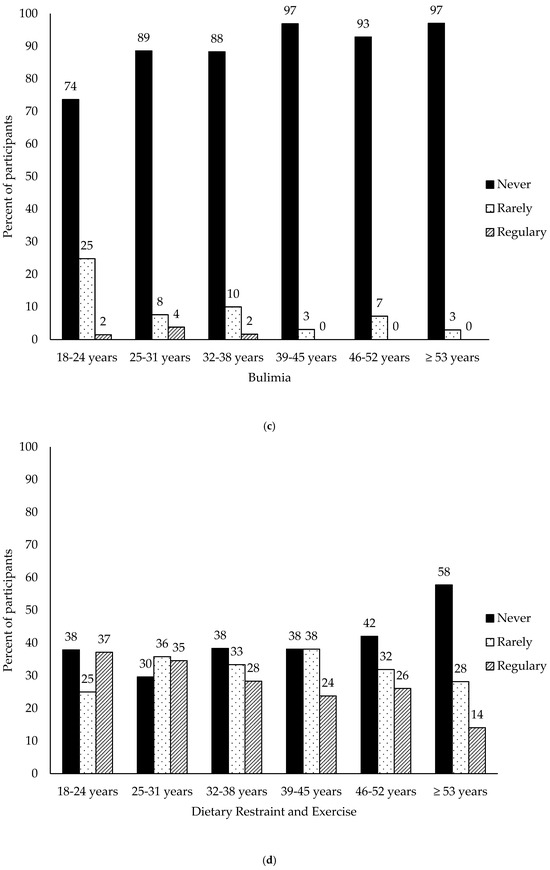
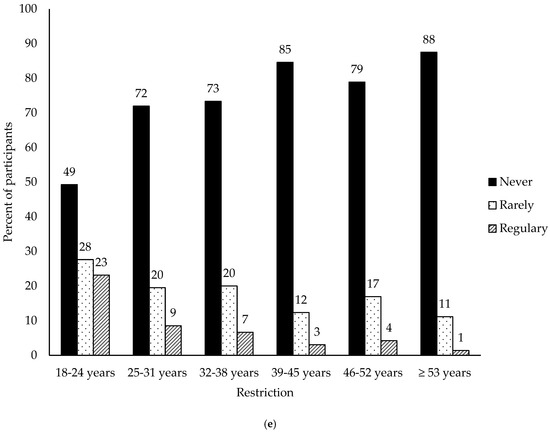
Figure 2.
(a) Percentage of participants reporting engaging in FAD behaviours “never”, “rarely” and “regularly” by age group. (b) Percentage of participants reporting engaging in restrictive behaviours to enhance intoxication “never”, “rarely”, and “regularly” (alcohol effects) by age group. (c) Percentage of participants using laxatives, diuretics, and vomiting “never”, “rarely”, and “regularly” (bulimia) by age group. (d) Percentage of participants exercising, consuming low-calorie foods or alcoholic drinks, or eating less (dietary restraint and exercise) “never”, “rarely”, and “regularly” by age group. (e) Percentage of participants missing meals or skipping an entire day (restriction) “never”, “rarely”, and “regularly” by age group.

Table 3.
Ordinal logistic regression models for ‘never’ engaging in FAD behaviours for CEBRACS Total and CEBRACS subscales alcohol effects, bulimia, dietary restraint and exercise, and restriction.
Women were less likely to never engage in FAD behaviours than men, except for alcohol effects and bulimia. There was no difference in the likelihood of never engaging in FAD behaviours by student status, except for alcohol effects—students were less likely than non-students to never restrict food intake before and during drinking to increase intoxication. Alcohol consumption was also associated with engaging in FAD behaviours, with those at low risk for alcohol problems more likely to never engage in FAD behaviours.
4. Discussion
Most research about FAD has been undertaken with young college/university students in the USA [17,22,29,36,42], with relatively few studies investigating older age groups or from the UK [34,35,36,37,43]. This study sought to contribute to the evidence base by recruiting a UK sample of alcohol consumers aged at least 18 years old with no upper age limit, including non-students as well as students, to examine the prevalence of engagement with FAD, conceptualised as restriction due to weight concern and restriction due to intoxication effects, across a range of age groups. We found that two-thirds of participants had engaged in at least one FAD behaviour during the previous 3 months, with the younger age groups more likely than the older age groups to engage in FAD behaviours, especially compared with the oldest group (53+ years). Even so, we found that 47% of the oldest age group reported engaging in at least one FAD-related behaviour. The most notable difference between age groups was in restricting food intake for the purposes of enhancing alcohol intoxication (alcohol effects), with 47% of the youngest age group reporting that they regularly restricted food intake prior to or during drinking to enhance the effects of alcohol compared with no one in the oldest age group.
Although engaging in FAD-related behaviours was more likely in the younger age groups, we found no association with student status, except for alcohol effects: non-students were 1.8 times more likely than students to never engage in FAD behaviours associated with restricting to enhance intoxication. The youngest age group was significantly more likely to also be students, but the likelihood of never engaging in behaviours associated with alcohol effects was 20 times less likely compared with the oldest age group, suggesting that youth rather than student status predicted restricting food intake to enhance intoxication from alcohol. Our findings are consistent with a UK study of young adults (18–25 years) that compared current students with previous students and non-students and found no significant differences between the groups [34]. As most of the research in this area has been conducted with university students, there is relatively little information about adults older than the traditional student age. However, Australian researchers Moeck and Thomas [35], using Amazon Mechanical Turk (MTurk) to recruit a broader age range of adults (18–76 years, mean 39 years), found that 64% of their participants had engaged in at least one FAD behaviour in the previous 3 months, similar to the 69% in our study. Mean total CEBRACS scores were similar (see Supplementary Table S1), although considerably lower than Hill and Nolan [36], who also used MTurk to recruit a non-student sample of American women (mean age 37 years), as well as recruiting a sample of female college students (mean age 19 years). The mean score was 33.04 (11.75) for their undergraduate sample, comparable with the score for our 18–24 years-old participants of 36.8 (14.6), but it was 53.79 (21.21) for the older participants recruited via MTurk, whereas in our study total scores for the older age groups were all lower than for the 18–24 years-old age group. Their MTurk sample scores for the CEBRACS subscales were also considerably higher than those of our female participants. Hill and Mazurek’s investigation of FAD in USA and UK mothers used Prolific to recruit a comparable sample size (n = 466) with a broad age range (23–70 years; mean 40 years) [37]. Their CEBRACS subscale scores are similar to our female participants’ scores. The variation in FAD prevalence and CEBRACS scores between the different studies mean that it is not clear whether middle to older aged adults engage in FAD behaviours more or less than younger adults, but it is clear that engagement with FAD behaviours is not exclusive to young university/college students.
FAD was associated with alcohol intake, especially potentially problematic drinking. Those with alcohol consumption patterns that indicated a low risk of harm were between three and five times less likely to engage in FAD behaviours compared with those at the highest risk. To some extent, this is not surprising, as those who drink more frequently will have more opportunities to compensate for the energy in alcohol. However, restricting food intake prior to and during drinking, whether for weight concern issues or to get drunk more quickly, puts consumers at greater risk of alcohol-related harm. The absorption of alcohol will be quicker for those “drinking on an empty stomach”, increasing the risk of reaching a dangerous stage of alcohol intoxication [44]. In university students, restricting food intake before drinking has been found to be associated with an increased risk of alcohol-related harm [21,24,27,28]. Our findings that 76% of the youngest age group rarely or regularly restrict food intake to feel the effects of alcohol faster is therefore particularly concerning.
Our findings relating to the prevalence of engaging in FAD behaviours are consistent with the literature, which tends to conceptualise FAD as pathological (whether disordered eating or alcohol misuse), but with no diagnostic criteria [45], “prevalence” tends to be reported, as we have here, as “ever engaging” in at least one FAD related behaviour. It seems likely that this definition, especially if it does not differentiate between the different behaviours associated with FAD, overestimates the number of people for whom FAD is pathological.
Strengths and Limitations
Although we were successful in recruiting a range of ages of UK adults, with three-quarters of the sample older than the traditional student age, the reliance on convenience sampling and how participants were recruited likely introduces selection bias and limits the generalisability of the findings. Although we did not collect information on the highest level of education, the sampling strategy probably resulted in a sample with relatively higher educational attainment and income compared with the UK general population. Despite our aim to recruit a sample with a wide age range, the number in the oldest age groups was relatively small. In common with much of the research in this area, most of our participants were female, limiting the generalisability to men, although a systematic review of gender differences, measured using validated scales, showed no differences in motivations or behaviours between women and men [46]. Although we used validated measures of FAD behaviours and alcohol use, they are reliant on self-reported behaviours and may be susceptible to socially desirable reporting and memory issues [47,48]. We found that FAD engagement was associated with a higher risk for alcohol behaviours; as problematic alcohol use and eating disorders have been shown to co-occur [49,50], a measure of disordered eating and information about the family history of disordered eating would be useful for a more comprehensive assessment.
The cross-sectional study design is also a limitation. Without longitudinal follow-up, it is unclear whether the differences between age groups will continue, with the youngest age group continuing to exhibit higher engagement with FAD behaviours, or if increasing age will bring their behaviours into line with the middle- and older-age groups. With trends indicating a reduction in adolescents’ alcohol consumption [51], it might be expected that younger adults’ engagement with FAD might also reduce.
These limitations suggest avenues for future research, such as recruitment strategies designed to recruit representative samples of those aged over 50 years, as we know their patterns of alcohol consumption are of concern. The risks of harm associated with alcohol consumption increase with increasing age [52], but there is a lack of research focussing on the harm associated with FAD in older age groups. It would be interesting to explore whether the type of alcohol-related harms associated with FAD experienced by younger age groups [21,24,27,28] are shared by those in older age groups.
5. Conclusions
Although engaging in FAD behaviours was more common in university-aged young people, middle-aged and older UK adults were also engaging in FAD behaviours. Some of the behaviours associated with FAD are clearly detrimental to health, such as purging and missing meals. For others, such as exercising before or after drinking alcohol to compensate for the energy in alcohol, it is not so clear cut. With the increasing prevalence of overweight and obesity [53,54,55], it could be argued that if people are going to drink alcohol, taking steps to compensate for the energy in alcohol could be considered beneficial to health. Indeed, increasing the public’s awareness of the energy content of alcohol is part of some Governments’ obesity prevention strategies [56]. However, the intention of these policies is to reduce energy intake by deterring people from consuming alcohol rather than restricting food intake to allow for higher alcohol consumption. A potential unintended consequence of such public health campaigns is that they could increase the frequency with which people engage in potentially damaging FAD behaviours if they choose alcohol over food [57]. The findings from this study suggest that people from all age groups may be making that choice, potentially putting their health at risk.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/dietetics4020019/s1, Table S1: CEBRACS total and CEBRACS subscale scores for the whole sample and by age group, gender, and student status.
Author Contributions
Conceptualisation J.B., H.R.M., J.K. and R.B.; methodology J.B., H.R.M., J.K. and R.B.; investigation J.B., H.R.M., J.K. and R.B.; formal analysis J.B.; visualisation J.B.; writing—original draft preparation J.B. and H.R.M.; writing—review and editing J.B., H.R.M., J.K. and R.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Undergraduate Faculty of Health and Social Care Research Ethics Sub-Committee of Edge Hill University (UGRAD116, 15 February 2019) and the School of Applied Sciences Research Integrity and Ethics Committee at the University of Huddersfield (SAS-SREIC 4.1.19-4).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Dataset available upon request from the authors.
Acknowledgments
The authors thank all those participants who contributed to this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| FAD | food and alcohol disturbance |
| CEBRACs | Compensatory Eating and Behaviours in Response to Alcohol Consumption Scale |
| AUDIT-C | Alcohol Use Disorders Identification Test |
References
- Krieger, H.; Young, C.M.; Anthenien, A.M.; Neighbors, C. The epidemiology of binge drinking among college-age individuals in the United States. Alcohol Res. Curr. Rev. 2018, 39, 23–30. [Google Scholar]
- Ranker, L.R.; Lipson, S.K. Prevalence of heavy episodic drinking and alcohol use disorder diagnosis among US college students: Results from the national Healthy Minds Study. Addict. Behav. 2022, 135, 107452. [Google Scholar] [CrossRef]
- Gambles, N.; Porcellato, L.; Fleming, K.M.; Quigg, Z. “If You Don’t Drink at University, You’re Going to Struggle to Make Friends” Prospective Students’ Perceptions around Alcohol Use at Universities in the United Kingdom. Subst. Use Misuse 2022, 57, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Mathes Winnicki, B.M.; Hinds, Z.; Newberger, N.G.; Livingston, N.A. Prospective associations between perceived social connection and alcohol use: A scoping review. Addict. Res. Theory 2023, 31, 250–259. [Google Scholar] [CrossRef]
- Miller, M.; Mojica-Perez, Y.; Livingston, M.; Kuntsche, E.; Wright, C.J.; Kuntsche, S. The who and what of women’s drinking: Examining risky drinking and associated socio-demographic factors among women aged 40–65 years in Australia. Drug Alcohol Rev. 2022, 41, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhang, Y.; Wu, C. Alcohol consumption and associated factors among middle-aged and older adults: Results from China Health and Retirement Longitudinal Study. BMC Public Health 2022, 22, 322. [Google Scholar] [CrossRef]
- Grucza, R.A.; Sher, K.J.; Kerr, W.C.; Krauss, M.J.; Lui, C.K.; McDowell, Y.E.; Hartz, S.; Virdi, G.; Bierut, L.J. Trends in Adult Alcohol Use and Binge Drinking in the Early 21st-Century United States: A Meta-Analysis of 6 National Survey Series. Alcohol. Clin. Exp. Res. 2018, 42, 1939–1950. [Google Scholar] [CrossRef]
- National Statistics. Health Survey for England, 2021 Part 1. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2021/part-3-drinking-alcohol (accessed on 28 July 2023).
- Kepner, W.E.; Han, B.H.; Nguyen, D.; Han, S.S.; Lopez, F.A.; Palamar, J.J. Past-month binge drinking and cannabis use among middle-aged and older adults in the United States, 2015–2019. Alcohol 2023, 107, 32–37. [Google Scholar] [CrossRef]
- Rehm, J.; Shield, K.D. Alcohol use and cancer in the European Union. Eur. Addict. Res. 2021, 27, 1–8. [Google Scholar] [CrossRef]
- Room, R.; Babor, T.; Rehm, J. Alcohol and public health. Lancet 2005, 365, 519–530. [Google Scholar] [CrossRef]
- Hallett, J.; Howat, P.M.; Maycock, B.R.; McManus, A.; Kypri, K.; Dhaliwal, S.S. Undergraduate student drinking and related harms at an Australian university: Web-based survey of a large random sample. BMC Public Health 2012, 12, 37. [Google Scholar] [CrossRef]
- O’Connell, H.; Chin, A.-V.; Cunningham, C.; Lawlor, B. Alcohol use disorders in elderly people–redefining an age old problem in old age. BMJ 2003, 327, 664–667. [Google Scholar] [CrossRef]
- Gargiulo, G.; Testa, G.; Cacciatore, F.; Mazzella, F.; Galizia, G.; Della-Morte, D.; Langellotto, A.; Pirozzi, G.; Ferro, G.; Ferrara, N.; et al. Moderate alcohol consumption predicts long-term mortality in elderly subjects with chronic heart failure. J. Nutr. Health Aging 2013, 17, 480–485. [Google Scholar] [CrossRef]
- Kershaw, S. Starving Themselves, Cocktail in Hand. The New York Times, 2 March 2008. Available online: https://www.nytimes.com/2008/03/02/fashion/02drunk.html (accessed on 29 January 2025).
- Choquette, E.M.; Rancourt, D.; Kevin Thompson, J. From fad to FAD: A theoretical formulation and proposed name change for “drunkorexia” to food and alcohol disturbance (FAD). Int. J. Eat. Disord. 2018, 51, 831–834. [Google Scholar] [CrossRef] [PubMed]
- Simons, R.M.; Hansen, J.M.; Simons, J.S.; Hovrud, L.; Hahn, A.M. Drunkorexia: Normative behavior or gateway to alcohol and eating pathology? Addict. Behav. 2021, 112, 106577. [Google Scholar] [CrossRef] [PubMed]
- Hunt, T.K.; Forbush, K.T. Is “drunkorexia” an eating disorder, substance use disorder, or both? Eat. Behav. 2016, 22, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Bryant, J.B.; Darkes, J.; Rahal, C. College Students’ Compensatory Eating and Behaviors in Response to Alcohol Consumption. J. Am. Coll. Health 2012, 60, 350–356. [Google Scholar] [CrossRef]
- Burke, S.C.; Cremeens, J.; Vail-Smith, K.; Woolsey, C. Drunkorexia: Calorie Restriction Prior to Alcohol Consumption Among College Freshman. J. Alcohol Drug Educ. 2010, 54, 17–34. [Google Scholar]
- Giles, S.M.; Champion, H.; Sutfin, E.L.; McCoy, T.P.; Wagoner, K. Calorie restriction on drinking days: An examination of drinking consequences among college students. J. Am. Coll. Health 2009, 57, 603–610. [Google Scholar] [CrossRef]
- Hill, E.M.; Ruark, R. An examination of the role of social comparison orientation and social norms in drunkorexia engagement. Addict. Behav. 2022, 124, 107107. [Google Scholar] [CrossRef]
- Knight, A.; Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Simpson, S. Drunkorexia: An Empirical Investigation among Australian Female University Students. Aust. Psychol. 2017, 52, 414–423. [Google Scholar] [CrossRef]
- Landry, A.S.; Madson, M.B.; Mohn, R.S.; Nicholson, B.C. Development and psychometric evaluation of the college eating and drinking behaviors scale in US college students. Int. J. Ment. Health Addict. 2017, 15, 485–492. [Google Scholar] [CrossRef]
- Peralta, R.L.; Barr, P.B. Gender orientation and alcohol-related weight control behavior among male and female college students. J. Am. Coll. Health 2017, 65, 229–242. [Google Scholar] [CrossRef]
- White, H.R.; Labouvie, E.W. Towards the assessment of adolescent problem drinking. J. Stud. Alcohol 1989, 50, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Roosen, K.M.; Mills, J.S. Exploring the motives and mental health correlates of intentional food restriction prior to alcohol use in university students. J. Health Psychol. 2015, 20, 875–886. [Google Scholar] [CrossRef]
- Tuazon, V.E.; Travis, S.P.; Honderich, E.M.; Williams, A.E.; Menefee, S.E.; Gressard, C.F. Drunkorexia: An exploratory investigation of college students with alcohol-related infractions. J. Coll. Couns. 2019, 22, 13–26. [Google Scholar] [CrossRef]
- Shepherd, C.B.; Berry, K.A.; Ye, X.; Li, K. Food and alcohol disturbance among US college students: A mixed methods scoping review. J. Am. Coll. Health 2021, 71, 1715–1731. [Google Scholar] [CrossRef]
- Rahal, C.J.; Bryant, J.B.; Darkes, J.; Menzel, J.E.; Thompson, J.K. Development and validation of the Compensatory Eating and Behaviors in Response to Alcohol Consumption Scale (CEBRACS). Eat. Behav. 2012, 13, 83–87. [Google Scholar] [CrossRef]
- Choquette, E.M.; Ordaz, D.L.; Melioli, T.; Delage, B.; Chabrol, H.; Rodgers, R.; Thompson, J.K. Food and Alcohol Disturbance (FAD) in the US and France: Nationality and gender effects and relations to drive for thinness and alcohol use. Eat. Behav. 2018, 31, 113–119. [Google Scholar] [CrossRef]
- Palermo, M.; Choquette, E.M.; Ahlich, E.; Rancourt, D. Food and alcohol disturbance by athlete status: The roles of drive for thinness, drive for muscularity, and sex. J. Am. Coll. Health 2021, 69, 905–912. [Google Scholar] [CrossRef]
- Peralta, R.L.; Schnellinger, R.P.; Wade, J.M.; Barr, P.B.; Carter, J.R. The association between Food and Alcohol Disturbance (FAD), race, and ethnic identity belonging. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2019, 24, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Griffin, B.L.; Vogt, K.S. Drunkorexia: Is it really “just” a university lifestyle choice? Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2020, 26, 2021–2031. [Google Scholar] [CrossRef]
- Moeck, E.K.; Thomas, N.A. Food and alcohol disturbance in a broad age-range adult sample. Eat. Behav. 2021, 41, 101510. [Google Scholar] [CrossRef]
- Hill, E.M.; Nolan, M.T. Examining eating disorder-related social comparison orientation and body dissatisfaction in the relationship between fit ideal internalization and drunkorexia engagement. Eat. Behav. 2021, 41, 101480. [Google Scholar] [CrossRef] [PubMed]
- Hill, E.M.; Mazurek, M.E. Problematic alcohol use and food and alcohol disturbance in mothers: Examining the role of stress, body dissatisfaction, and wine-mom-consistent drinking. Alcohol 2023, 113, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Alcohol Use Screening Tests. Available online: https://www.gov.uk/government/publications/alcohol-use-screening-tests (accessed on 11 December 2018).
- Eng, J. Sample size estimation: How many individuals should be studied? Radiology 2003, 227, 309–313. [Google Scholar] [CrossRef]
- Peterson, C.H.; Peterson, N.A.; Powell, K.G. Cognitive Interviewing for Item Development: Validity Evidence Based on Content and Response Processes. Meas. Eval. Couns. Dev. 2017, 50, 217–223. [Google Scholar] [CrossRef]
- NHS England. Alcohol Units; National Health Services England: London, UK, 2019. [Google Scholar]
- Hill, E.M.; Lego, J.E. Examining the role of body esteem and sensation seeking in drunkorexia behaviors. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2020, 25, 1507–1513. [Google Scholar] [CrossRef]
- Vogt, K.S.; Harper, M.; Griffin, B.L. “… because I’m so drunk at the time, the last thing I’m going to think about is calories”: Strengthening the argument for Drunkorexia as a food and alcohol disturbance, evidence from a qualitative study. Br. J. Health Psychol. 2022, 27, 1188–1208. [Google Scholar] [CrossRef]
- Jones, A.W.; Jönsson, K. Food-induced lowering of blood-ethanol profiles and increased rate of elimination immediately after a meal. J. Forensic Sci. 1994, 39, 1084–1093. [Google Scholar] [CrossRef]
- Thompson-Memmer, C.; Glassman, T.; Diehr, A. Drunkorexia: A new term and diagnostic criteria. J. Am. Coll. Health 2019, 67, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Speed, S.; Ward, R.M.; Haus, L.; Branscum, P.; Barrios, V.; Budd, K.M.; Lemons, K.; Humenay, E. A systematic review of common drunkorexia measures: Examining gender differences across scales. Am. J. Health Educ. 2022, 53, 342–359. [Google Scholar] [CrossRef]
- Davis, C.G.; Thake, J.; Vilhena, N. Social desirability biases in self-reported alcohol consumption and harms. Addict. Behav. 2010, 35, 302–311. [Google Scholar] [CrossRef] [PubMed]
- McKenna, H.; Treanor, C.; O’Reilly, D.; Donnelly, M. Evaluation of the psychometric properties of self-reported measures of alcohol consumption: A COSMIN systematic review. Subst. Abus. Treat. Prev. Policy 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, L.D.S.; de Souza, A.P.L.; Ferreira, I.M.S.; Lima, D.W.d.C.; Pessa, R.P. Binge eating and alcohol consumption: An integrative review. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2021, 26, 759–769. [Google Scholar] [CrossRef]
- Bogusz, K.; Kopera, M.; Jakubczyk, A.; Trucco, E.M.; Kucharska, K.; Walenda, A.; Wojnar, M. Prevalence of alcohol use disorder among individuals who binge eat: A systematic review and meta-analysis. Addiction 2021, 116, 18–31. [Google Scholar] [CrossRef]
- Loy, J.K.; Seitz, N.-N.; Bye, E.K.; Raitasalo, K.; Soellner, R.; Törrönen, J.; Kraus, L. Trends in alcohol consumption among adolescents in Europe: Do changes occur in concert? Drug Alcohol Depend. 2021, 228, 109020. [Google Scholar] [CrossRef]
- White, A.M.; Orosz, A.; Powell, P.A.; Koob, G.F. Alcohol and aging–an area of increasing concern. Alcohol 2023, 107, 19–27. [Google Scholar] [CrossRef]
- Okati-Aliabad, H.; Ansari-Moghaddam, A.; Kargar, S.; Jabbari, N. Prevalence of Obesity and Overweight Among Adults in the Middle East Countries from 2000 to 2020: A Systematic Review and Meta-Analysis. J. Obes. 2022, 2022, 8074837. [Google Scholar] [CrossRef]
- Stival, C.; Lugo, A.; Odone, A.; van den Brandt, P.A.; Fernandez, E.; Tigova, O.; Soriano, J.B.; López, M.J.; Scaglioni, S.; Gallus, S.; et al. Prevalence and correlates of overweight and obesity in 12 European Countries in 2017–2018. Obes. Facts 2022, 15, 655–665. [Google Scholar] [CrossRef]
- Hu, K.; Staiano, A.E. Trends in obesity prevalence among children and adolescents aged 2 to 19 years in the US from 2011 to 2020. JAMA Pediatr. 2022, 176, 1037–1039. [Google Scholar] [CrossRef] [PubMed]
- Jané-Llopis, E.; Kokole, D.; Neufeld, M.; Hasan, O.S.M.; Rehm, J. What Is the Current Alcohol Labelling Practice in the WHO European Region and What Are Barriers and Facilitators to Development and Implementation of Alcohol Labelling Policy? World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Robinson, E.; Boyland, E.; Evans, R.; Finlay, A.; Halsall, L.; Humphreys, G.; Langfield, T.; McFarland-Lesser, I.; Patel, Z.; Jones, A. Energy labelling of alcoholic drinks: An important or inconsequential obesity policy? Obes. Sci. Pract. 2023, 9, 75–86. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).