1. Introduction
In 2005, the Danish Health Authority published Cancer Plan II, which aims to strengthen cancer prevention and improve the basis for Danish cancer patients to be offered assessment and treatment that are initiated early, experienced coherently by patients and have high international professional quality. The plan contains professional recommendations in several areas where a strengthened effort is deemed necessary [
1].
Surgery is the treatment that has the best chance of leading to a cure for most cancers including renal cell carcinoma (RCC), and the quality of cancer surgery is therefore of decisive importance for the treatment outcome. Analyses of treatment outcomes in the form of survival show that for a number of operable cancers, survival was lower in Denmark than in the other Nordic countries, especially in the first months after diagnosis. It is estimated that strengthening cancer surgery could contribute to improving treatment outcomes, and the evaluation of Cancer Plan I has pointed to a need to optimize cancer surgery.
A large number of international studies have shown that several factors are important for cancer surgery and quality, including the time of surgery in relation to the stage of the disease, a sufficiently large number of operations per surgeon and per patient, whether multidisciplinary cooperation has been established, training/further training of the surgeon and the entire team and compliance with clinical guidelines [
2]. Cancer Plan II describes these [
1].
Multidisciplinary team conferences play a deciding role for treatment of renal cancer patients. Variations such as frequency, participation and guideline adherence may affect patient outcome. Studies have shown that MDT provides (1) better care coordination and outcomes, (2) reduced unexpected hospital admissions, and (3) shortened hospital stays.
2. Multidisciplinary Team Meetings (MDMs)
Calman–Hine was the first comprehensive cancer report to be produced in the UK, and set out principles for cancer care and clinical organizations for service delivery [
3]. It advocated a change from a generalist model (e.g., care given by general surgeons and physicians) that was supported by specialists to a fully specialist service. MDM conferences have become an important part of Danish cancer treatment since Cancer Plan II and with the establishment of the DMCGs [
4].
With the multidisciplinary aspects of the treatment courses, the patient is ensured a treatment offer at the highest evidence-based level. The MDM Committee under DMCG.dk has been established to investigate, monitor and promote the development of the MDT conferences.
3. Clinical Quality Improvement and Indicator Sets in the Danish Healthcare Quality Institute's Clinical Quality Registers
DMCG.dk was founded in 2004 and is the association of Danish Multidisciplinary Cancer Groups, whose main task is to promote cancer treatment in Denmark [
4,
5]. For each register, a professional steering group has been established to determine what the content should be—including the individual indicators and standards (quality goals) [
6].
Darenca is the DMCG for RCC. The group consist of five urologists, three oncologists, one epidemiologist, two pathologists, two diagnostic imaging specialists, one genetic representative and one patient representative. The Darenca group met several times during the year to prepare an annual report at the end of the year, which is sent to all hospitals, hospital management, politicians and the Danish Health Authority. The annual report is finalized with members from Darenca and three from the Danish Healthcare Quality Institute—a Chief data manager, an epidemiologist and a statistician.
The clinical quality registers allow for uniform national monitoring across the country [
6]. The target group and purpose of use are crucial for how frequently and how data should be analyzed and knowledge communicated. The overall thinking in the work is an improvement model with the following elements: (a) set goals (standard), (b) establish measurement (indicator), (c) select change (intervention), (d) test change, and (e) assessment (audit). The efforts are focused on creating national consensus on quality and challenges in the current disease area, and on measuring, assessing and reporting results [
7].
4. The 2024 Darenca Report
The annual report includes two patient populations: (A) patients with newly diagnosed histologically or cytologically verified RCC (Patient Population 1) and (B) all surgically treated patients with histologically verified kidney cancer (Patient Population 2) [
8]. Population 1 is based on extracts from the National Registry of Pathology (NRP), while Population 2 is based on extracts from both the National Patient Register (NPR) and the NRP. The register Darencadata includes all persons with a first-time diagnosis of renal cancer in Denmark since August 2010 [
7].
An overview of the current indicators is shown in
Table 1. Here is a brief summary of the results from the annual report from Darenca with national, regional and hospital-based data for the diagnosis and treatment of RCC in Denmark, which was published in January 2025 [
8]. The register includes over 13,000 new cases of RCC in Denmark from its inception on 1 August 2010 to 31 July 2024, of which 1035 occurred in the period from 1 August 2023 to 31 July 2024. Patients with newly diagnosed RCC are identified using the National Register of Pathology (LRP). Thus, only patients with histologically or cytologically verified RCC are included in the register. This is unique to Denmark, as in some countries patients are also included where the diagnosis is based solely on imaging.
The incidence rates of RCC have shown an increasing trend in most countries over the past 10 years, which has also been the case in Denmark [
2]. In the current report, the age-standardized incidence is 16.9 per 100,000 inhabitants. Survival after RCC is increasing in Denmark and is above international levels. The observed 1-year survival was 91% for the period 1 August 2022–31 July 2024. The observed 5-year survival was correspondingly 71%, increasing compared to 68% and 63% in the two previous periods. At the same time, there has been an increase in the proportion of patients with T1 tumors during the period, and this higher proportion will positively affect survival. However, it is seen from supplementary analyses that survival is also increasing for patients with stage III and IV (TNM-EAU guideline) as a sign of improved treatment options for patients with locally advanced and metastatic disease. The treatment of RCC is primarily surgical, and surgical treatment continues to move towards an increased proportion of kidney-preserving procedures. During the current period, 939 patients have received surgical treatment (operation or ablation). Of these, 54% are unchanged kidney-preserving procedures. The postoperative morbidity in the form of reoperation and complications is 4% and the proportion of patients who die within 30 days after surgery is <1% (Clavien–Dindo I-V). Morbidity and mortality are at international level. There is some variation between the departments in the proportion of complications, which should be an area of focus for the departments and for Darenca. The proportion of patients with T1a tumors who receive nephrectomy rather than kidney-preserving treatment is currently 13%, which is slightly higher than the last two years (10%). The Central Denmark Region has had a particularly positive development over the last five-year period for this indicator. Nationally, nephrectomies have been performed laparoscopically, including robot-assisted procedures, in 85%, with some variation between departments (
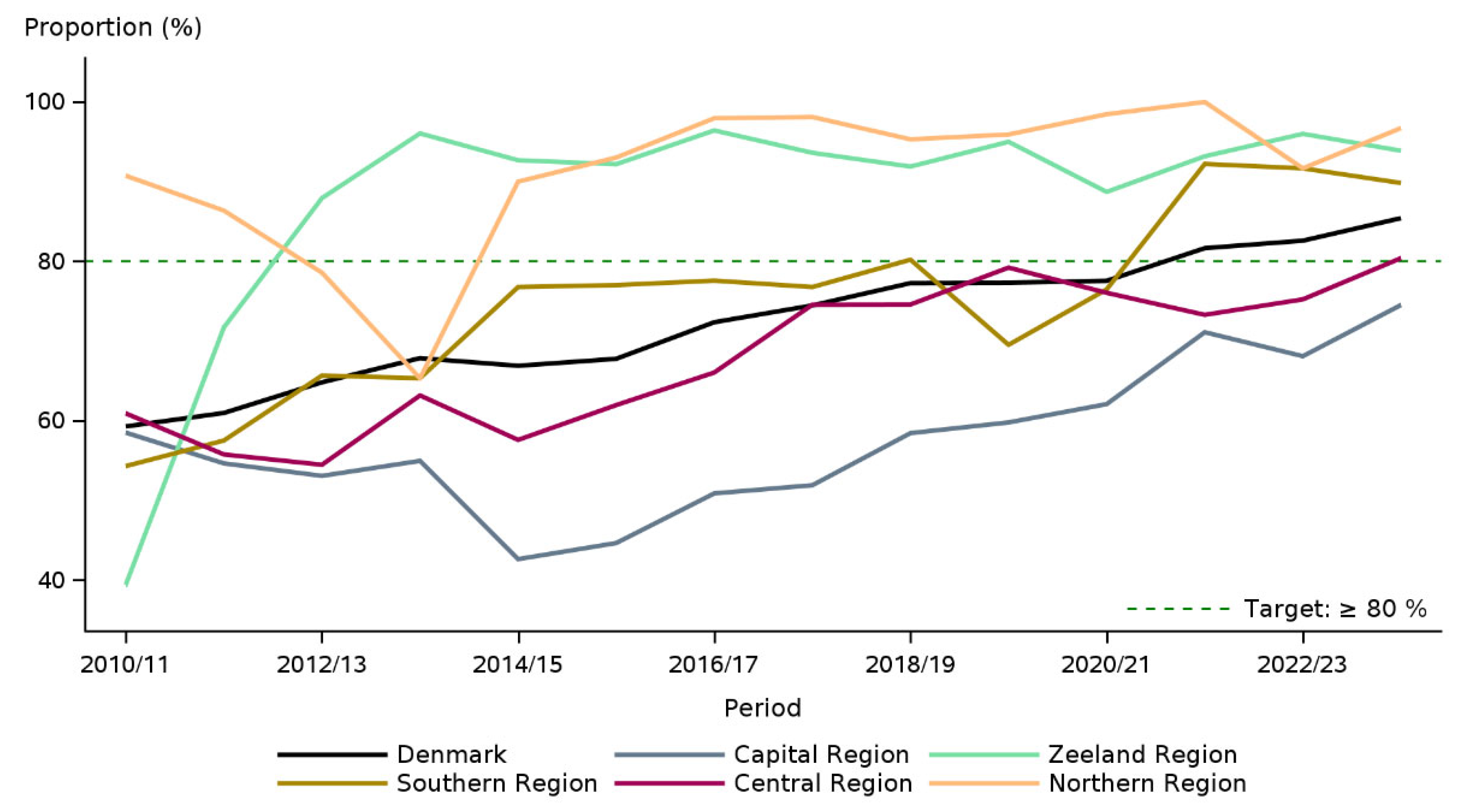
Figure 1).
The indicator result has raised from 65% to now over 80% over a five-year period. Differences in results are still observed, with the Capital Region and Central Denmark Region having the lowest results, but all regions have shown an increasing trend in the proportion receiving minimally invasive surgery, with the Capital Region in particular having improved results.
The proportion of endoscopically or ablatively treated patients who are discharged within 3 days of the procedure is 89%, also with some departmental variation, where two centers are lower than the rest of the country, and the steering group calls for this to be a focus area for the departments in collaboration with Darenca. A dialog will be ongoing to clarify the reasons why the development at one department has not been on level with the rest of the country, including whether there are challenges as a result of extensive restructuring of the specialty in the Region of Southern Denmark. We think that the MDM is the key point where the decision is made about the treatment that is deemed best for the individual patient along with the annual report from the whole country. In relation to the fact that this is the first time this indicator has been included, it is reassuring to see that 71% of the patients had registered MDT in the period 90 days before to 90 days after the time of diagnosis. However, regional differences from 54% to 98% are currently seen, and this will be a focus area where registration practices for MDM procedures to the National Patient Register should be prioritized. However, it is important to point out that only 8% have missing or unclassifiable stage reports of (c)TNM stage to the National Patient Register (LPR), which is a clear improvement compared to last year's reporting.
5. Conclusions
Through systematic work with data-driven quality improvement, interdisciplinary collaboration, cancer patient pathways, and the introduction of new treatments, we have observed a uniform treatment and increased survival in patients with kidney cancer over the last 5 years.
Author Contributions
Conceptualization, methodology, investigation, data curation, writing—original draft preparation, supervision L.L.; methodology, L.L., H.L., E.H.I.; formal analysis, H.L. and E.H.I.; data curation, H.L., E.H.I.; writing—original draft preparation, LL.; writing—review and editing, L.L., M.N., N.F., A.K.M.D. and E.H.I.; supervision, L.L. and M.N.; project administration, L.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board.
Informed Consent Statement
Not applicable.
Data Availability Statement
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DMCG | Danish Multidisciplinary Cancer Groups |
| RCC | Renal Cell Carcinoma |
| LRP | National Registry of Pathology |
| NRP | National Registry of Patients |
References
- Kraeftplan II. Sundhedsstyrelsens Anbefalinger til Forbedringer af Indsatsen på Kræftområdet. June 2005. Available online: https://www.dmcg.dk/siteassets/dmcg---om/dmcg---grundlaggelse-og-historie/kraeftplanii.pdf (accessed on 17 August 2025).
- EAU Guidelines on Renal Cell Carcinoma. Available online: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Renal-Cell-Carcinoma-2024.pdf (accessed on 17 August 2025).
- Haward, R.A. The Calman-Hine report: A personal retrospective on the UK's first comprehensive policy on cancer services. Lancet Oncol. 2006, 4, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Sundhedsdatastyrelsen. Kliniske Kvalitetsdatabaser. København: Sundhedsdatastyrelsen. 2021. Available online: https://sundhedsdatastyrelsen.dk/data-og-registre/kliniske-kvalitetsdatabaser (accessed on 17 August 2025).
- Nørgaard, M.; Johnsen, S.P. How can the research potential of the clinical quality databases be maximized? The Danish experience. J. Intern. Med. 2016, 2, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, H.T.; Pedersen, L.; Jørgensen, J.; Ehrenstein, V. Danish clinical quality databases—An important and untapped resource for clinical research. Clin. Epidemiol. 2016, 8, 425–427. [Google Scholar] [CrossRef] [PubMed]
- Danckert, B.; Horsbøl, T.A.; Andersen, O.; Dalton, S.O.; Christensen, J.; Rasted, M.; Petersen, A.; Nørgaard, M.; Azawi, N.; Lund, L.; et al. Registrations of Patients with Renal Cell Carcinoma in the Nationwide Danish Renal Cancer Database versus the Danish Cancer Registry: Data Quality, Completeness and Survival (DaRenCa Study-3). Clin. Epidemiol. 2020, 12, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Dansk Renal Cancer Database (DaRenCaData). Available online: https://www.sundk.dk/media/xgnaeoaz/darencadata_aarsrapport-2024.pdf (accessed on 17 August 2025).
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).