1.1. CARDIAC » Adult Congenital
1.1.1. Surgical Correction of Tetralogy of Fallot in Adults: A Retrospective Analysis of Recent Experience
Kamran Ahmadov, Kamran Musayev, Ilkin Osmanov, Fahreddin Alekberov and Murad Bayramli
Department of Cardiovascular Surgery, Merkezi Klinika, Baku, Azerbaijan
BACKGROUND AND AIM: To report our experience with surgical correction of Tetralogy of Fallot (TOF) in adults.
METHOD: We retrospectively analyzed our results of adults with TOF who underwent surgical correction between 2020 and 2024. The cohort consisted of 15 patients, with a mean age of 28 years (range: 17–48 years). Mean cardiopulmonary bypass and aortic cross-clamp times were 103 and 66 min, respectively. Mean ICU was 3 days (range 2–4 days).
RESULTS: No mortality was observed during the study period. Mean hospital stay was 6 days (range 5–8 days). Additionally, there were no cases with major adverse cardiac and cerebrovascular events (MACCE).
CONCLUSIONS: Surgical correction of TOF can be safely performed in adults, with favorable outcomes in terms of mortality and MACCE. Our experience highlights the feasibility and safety of this procedure in the adult population.
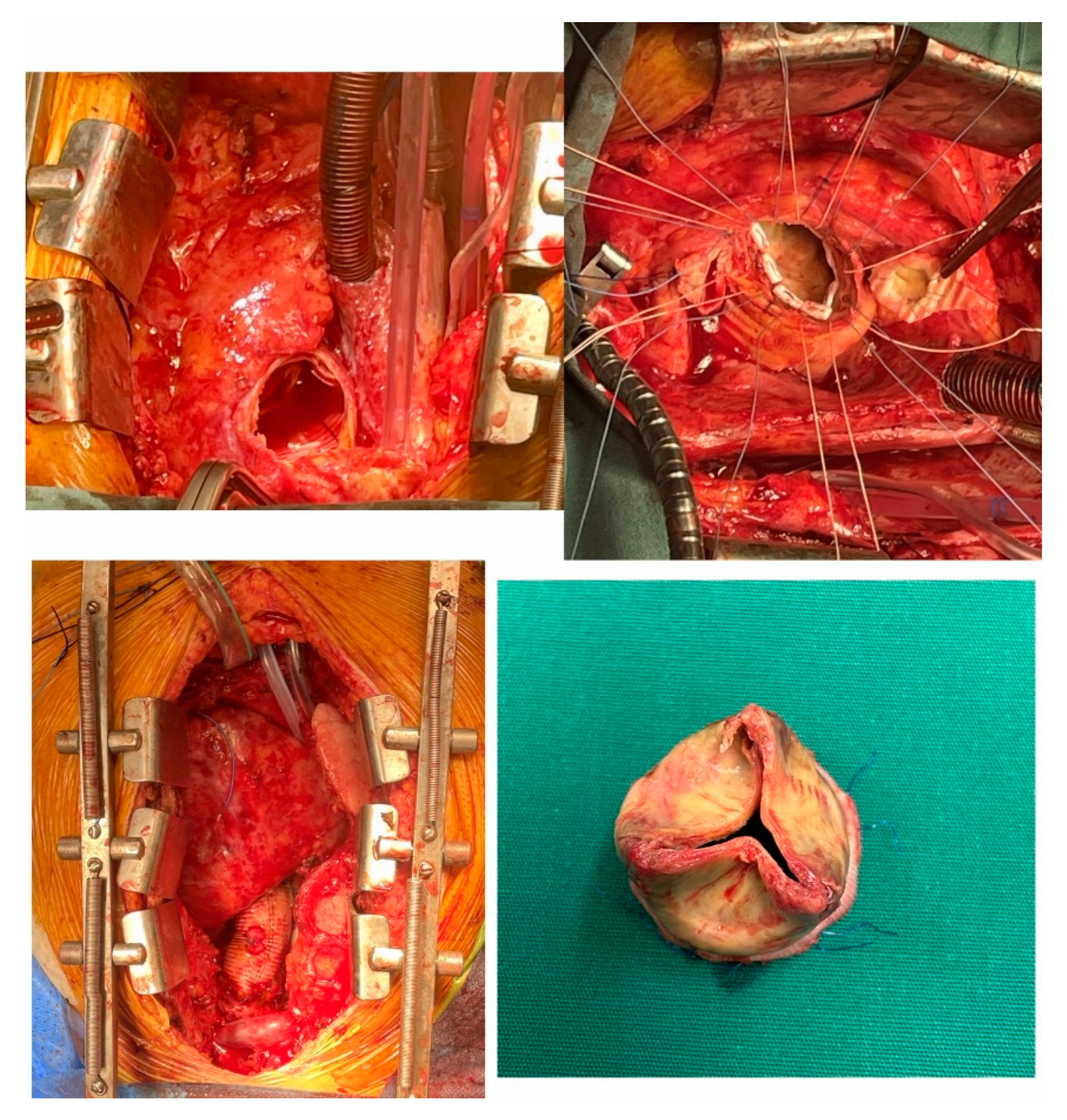
1.1.2. The First Cone Surgery Performed in Adult Ebstein Anomaly in Turkey
Erdoğan Ibrişim, Kadir Burhan Karadem and Dinçer Uysal
Department of Cardiovascular Surgery, Suleyman Demirel University, Isparta, Turkey
Ebstein’s disease is a rare congenital anomaly that occurs in one in 200.00 live births. Treatment of disease, repair, or replacement of the tricuspid valve prevents advanced insufficiency of the tricuspid valve. Plication of the atrialized ventricle, annular construction of tricuspid valve, closure of the defect to eliminate the right-left shunt. Cone operation is the most physiological and reliable of all methods. Valvular replacement and not using ring provide an advantage. Cone adulthood the first operation carried out with success in Turkey. We think that the frequent use of Cone method will have a positive effect to decrease the mortality, morbidity, and survival time in these cases.
1.1.3. Incidental Finding of Undiagnosed Aortic Coarctation in a 63-Year-Old Man Revealed by a Poly-Trauma
Wafa Id El Mouden, Wassim Beladel, Mehdi Barrajaa and Mohamed El Minaoui
Department of Cardiology, University Hospital Agadir, Medical School of Medicine & Pharmacy Ibn Zohr University, Agadir, Morocco
Aortic Coarctation is a narrowing of the aorta beyond the left subclavian artery, with an incidence ranging from 5% to 8% of all congenital cardiac defects. This anomaly is usually detected at birth by systematic palpation of the femoral pulses, but can also be diagnosed later, in both older children and adults.
We illustrate this fact with a case of a 63-year-old patient undergoing treatment for hypertension for four years. The diagnosis of coarctation of the aorta was established following a thoracic CT scan as part of the lesion assessment for poly-trauma following a road traffic accident.
While Coarctation of the Aorta is uncommon in adults, it should be included in the diagnostic evaluation for secondary hypertension, especially in individuals with a history of congenital heart disease. Better control of blood pressure, earlier repair and trans-catheter intervention may provide good results in this case.
No case of coarctation of the aorta in the context of poly-trauma has been cited in the literature, adult and elderly patients with uncorrected coarctation generally have a low survival rate, and the management strategies for such cases are controversial, especially when it is associated to other pathologies.
In the light of our findings, we recommend a thorough physical examination for all patients with suspected coarctation of the aorta, including upper and lower extremities blood pressure measurements.
1.1.4. Modified Central Shunt (Aasim’s Shunt) Procedure via Upper Mini Sternotomy in Teenage Patients with Complex Cyanotic Congenital Heart Disease and Hypoplastic Pulmonary Vasculature
BACKGROUND: Grown up children with complex cyanotic congenital heart disease and hypoplastic pulmonary vasculature are not amenable to biventricular total correction surgery in our setup. In this study we present our experience with such patients undergoing modified central shunt (Aasim’s Shunt) via upper ministernotomy access.
METHODS: We studied 6 patients (4 males, 2 females), 13 years to 19 years of age, with hypoplastic pulmonary arteries who underwent modified central shunt procedure between 2018 and 2023. Patient’s preoperative, operative, postoperative and demographic data were recorded.
RESULTS: Patients were operated as the first-step palliation. No mortality was observed. The median follow-up after the procedure is 12 months (range 6 months to 18 months).
CONCLUSIONS: The central shunts increase oxygen saturation and improve quality of life with potential for pulmonary arteries development. Low morbidity, low mortality, good survival rate and less technical difficulty of this procedure make it a better option for treatment of complex cyanotic congenital heart disease patients, having hypoplastic pulmonary vasculature.
1.1.5. Perioperative Management and Hemostatic Control of Antiphospholipid Syndrome in Cardiac Valvular and Septal Defect Surgery
Tanees Akhter, Ahson Memon, Malik Shafqat Hasan and Imran Ali
Department of cardiothoracic surgery, Tabba heart institute, Karachi, Pakistan
BACKGROUND: Individuals with Antiphospholipid syndrome (APS) often have heart valve anomalies, however, experience with valve replacement in such individuals with a considerably large ASD is limited. We offer a case of a mitral valve replacement and an ASD closure in a patient with this disease at our institute.
CASE PRESENTATION: A 29 year old female, married, APS positive, with no other comorbids, presented in the OPD for an elective ASD (Atrial Septal Defect) repair and mitral valve replacement. Her TEE (Transesophageal echocardiography) showed a bileaflet mitral valve prolapse causing severe eccentric mid to late systolic mitral regurgitation with multiple regurgitation jets and systolic flow reversal in left upper and left lower pulmonary veins. Mitral annulus measured 33 mm and a large ASD measuring 48 mm in diameter with predominantly left to right shunt was detected.
She was given clearance for surgery after being reviewed by a multidisciplinary team and successfully operated on, on the 23rd of November 2023, via a median sternotomy, on cardiopulmonary bypass and with an intricately managed anticoagulation process.
CONCLUSIONS: This case highlights the special perioperative difficulties that APS patients undergoing on pump cardiac surgery face, especially with regard to ASD closure. We have demonstrated, that although rare, such a condition may arise in some patients that have APS and can be, through correct risk assessment and management, surgically corrected.
1.1.6. Application of Reimplantation Technique in the Patient Who Had Anomalous Aortic Origin of the Right Coronary Artery and Aberrant Right Subclavian Artery
Ebubekir Sönmez, Izatullah Jalalzai, Eyüp Serhat Çalık and Ümit Arslan
Department of Cardiovascular Surgery, Atatürk University Medical Faculty, Erzurum, Türkiye
BACKGROUND: A rare congenital cardiac anomaly known as Anomalous Aortic Origin of the Right Coronary Artery (AAORCA) usually affects the right coronary artery (RCA) originating from the left sinüs of valsalva. Although AAORCA can cause angina, syncope, palpitations, and sudden cardiac death, most patients remain asymptomatic. Here, we present a rare case of a 42 year-old man who had AAORCA with an aberrant right subclavian artery. As a treatment, he underwent reimplantation of the right coronary artery to the aorta and right subclavien artery to right common carotid artery.
CASE PRESENTATION: A 42-year-old man presented with a history of angina. Beside blood tests and holter effor, to exclude any possibaly ischemic heart disease, coronary CT was ordered which reported that the RCA originated from the left sinus of Valsalva, indicating AAORCA. The RCA passed through the pulmonary artery and ascending aorta. At the same time aberrant right subclavian artery (ARCA) existence is revealed in the CT. ARCA is traveled posterior of esophagus. Operation was planned and we performed a reimplantation of the RCA and ARCA.
AAORCA, a rare congenital abnormality, can cause sudden cardiac death. Symptomatic patients should be treated surgically, while asymptomatic patients should be managed clinically, with secondary prevention through platelet antiaggregants and cholesterol reducers.
1.1.7. Retroaortic Innominate Vein with Right Aortic Arch in an Adult Patient with Previous Tetralogy of Fallot Repair
David C. Cistulli, Mathew Doyle and Benjamin M. Robinson
Department of Cardiothoracic Surgery, Royal Prince Alfred Hospital, Camperdown, NSW, Australia
BACKGROUND: Retroaortic innominate vein is a very rare congenital abnormality, with only a few case reports in the literature. When combined with right aortic arch and Tetralogy of Fallot, there is just one previous case report of this abnormality. We present a such case in a patient undergoing redo cardiac surgery.
CASE: A 43 year old female was referred to our Cardiothoracic Surgery service for tricuspid valve replacement and closure of patent foramen ovale in the context of worsening right ventricular function. This was on a background of previous Tetralogy of Fallot repair at 11 months old, which involved several revisions including Melody pulmonary valve insertion 10 years prior to referral. Pre-operative imaging demonstrated the unique combination of retroaortic innominate vein with a right aortic arch. Intra-operatively, special care was taken to identify where the innominate vein joined the right brachiocephalic vein. This was important for insertion and snaring the superior vena cava cannula below this junction, to ensure sufficient drainage of the innominate vein.
1.1.8. Unrepaired Persistent Truncus Arteriosus Typ4 in a 52 Years Old Woman Patient
INTRODUCTION: Truncus arteriosus (PAVSD) is a congenital defect that occurs as a result of incomplete septasia of great arteries and VSD. The common coronal arteria provides systemic, pulmonary and coronary perfusion. This pathology presents with severe heart failure, arrhythmia and right heart failure.
CLINICAL CASE: A 52-year-old woman applied to our clinic with chest pain, abdominal ascites, and arrhytmmia (NYHA III f.s). He has a physical work limitation since his childhood. She was not under regular cardiologist monitoring and did not receive regular treatment.
Physical examination: On the right, the breath sounds decrease on the lungs, on the left, wet wheezing is heard in the lower denominator. Core tones: increased, holosystolic sound is heard. Jugular venous distention+ and grade II ascites are observed in the abdomen. Their fingers are rod-shaped, and cyanosis is observed at the fingertips and around the mouth.
Hb-15.2, HCT-52.3, RBC-7,09, WBC-7.44, PLT-250
creatine—0.9 mg/dL, urea—54 mg/dL, TSH—10.84 mIU/mL, CRP—7.7 mg/L,
ECG: Atrial fibrillation, taxisystolic form.
ECHO: Biventrikulyar dilatation and hypertrophy, biatrial dilatation
PSAX: Pulmonary valve and artery could not be visualized
A5C: Overriding aorta, perimembranous VSD (−20 mm)
Primary Diagnosis: Pulmonary atresia? Truncus arteriosus? Heart Failure NHYA III. Atrial Fibrillation. Hypothyreoidism.
CT Angiography: CAT, which appeared by overriding IVS. RCA—originates from the right anterior part of the truncal sinus, LCA—originates from the left posterior part of the truncal sinus. Mapcas 4 mm on the right, 9 mm, 14 mm on the left.
CT: Undercirculation on the right side, Overcirculation on the left side
Clinical diagnosis:
A consultation was held with the cardiosurgeon. It was deemed inoperable and conservative treatment was prescribed.
Medical treatment: Rivaroxaban 20 mq × 1, Diqoksin 0.25 mq × 1, Verospirone 50 mg × 2, Furosemide 2 mL/20 mq × 2
RESULT: The patient was clinically relatively stabilized and conservative treatment was recommended, with subsequent follow-up checks recommended.
1.4. CARDIAC » Aortic Valve and Aortic Root Surgery
1.4.1. Aortic Stone Wars in a Case of Familial Hypercholesterolemia
Zied Ben Ayed 1, Imen Gabsi 1, Aiman Ghrab 1, Rahma Kallel 2, Walid Trigui 1 and Imed Frikha 1
- 1
Department of CardioVascular and Thoracic Surgery, Habib Bourguiba University Hospital, Sfax, Tunisia
- 2
Department of Cardiology, Mohamed Ben Sassi Hospital, Gabes, Tunisia
BACKGROUND AND AIM: Familial hypercholesterolemia (FH) is a genetic disorder characterized by high levels of low-density lipoprotein cholesterol (LDL-C) that predispose affected individuals to early-onset atherosclerotic cardiovascular disease (ASCVD).
This case report describes a patient with FH who presented with severe ASCVD.
METHOD: A 28-year-old male with a medical history of familial hypercholesterolemia, treated with atorvastatin and ezetimibe, and type 2 diabetes mellitus, treated with insulin, came to the emergency department with dyspnea and chest pain.
The patient had a family history of FH, and his older brother also had FH and early-onset CAD.
The examination revealed a harsh systolic ejection murmur, best heard at the right second intercostal space, radiating to the carotids, and a mild diastolic murmur.
Additionally, xanthomas on the elbows and knees were noted.
The patient had LVH and left ventricular dysfunction with an ejection fraction (LVEF) of 45%.
Coronary angiography revealed significant stenosis in all three major coronary arteries, and the CT-Scan showed a porcelain aorta with significant stenosis in its initial part.
RESULTS: The patient underwent a complex surgery that consisted of several components, including aortic valve replacement, aortic annulus enlargement, aortic root enlargement, and triple CABG.
The patient’s condition improved significantly following surgery, as indicated by an echocardiogram that showed a 65% increase in LVEF, no wall-motion abnormalities, and successful surgical intervention.
The patient had a smooth postoperative recovery, and subsequent CT scans revealed good flow in the coronary bypass grafts without any signs of residual stenosis in the aorta.
CONCLUSIONS: The challenges of managing FH are highlighted in this case report, which describes a complex surgical procedure performed on a 28-year-old male with FH who presented with multiple cardiovascular complications.
This case emphasizes the importance of genetic counseling and screening of family members of affected individuals to facilitate early diagnosis and treatment of FH.
1.4.2. Does Thrombocytopenia Exist Following Sutureless Aortic Valve Replacement (SU-AVR): An Institutional Experience of 178 Patients
Mustafa Mert Ozgur 1, Halil Ibrahim Bulut 2, Barıs Gurel 1, Mehmet Aksut 1, Tanıl Ozer 1, Ahmet Mirza Ozdemir 1, Hakan Hancer 1 and Kaan Kirali 1
- 1
Department of Cardiovascular Surgery, Koşuyolu High Specialization Training and Research Hospital, Istanbul, Türkiye
- 2
Cerrahpasa School of Medicine, Istanbul University Cerrahpasa, Istanbul, Turkey
BACKGROUND AND AIM: Sutureless Aortic Valves (Su-AVR) have been intricately designed to optimize the effectiveness of valve replacement surgery, placing a primary emphasis on minimizing invasiveness and shortening implantation time. Despite advancements, thrombocytopenia following sutureless aortic valve replacement remains a relatively obscure concern that requires further clarification. This study stands as the most extensive and largest registered assessment of thrombocytopenia following Su-AVR within the Turkish patient population, known for its tendency towards anemia in comparison to Western populations.
METHOD: From January 2015 to July 2023, a total of 178 individuals meeting the inclusion criteria were included in the analysis. The platelet count for each patient was evaluated one year post-operation at the same hospital.
RESULTS: The cohort, with a mean age of 70.1 ± 10.7 years, displayed minimal variations in valvular functions among individuals. Remarkably, there were no instances of aortic complications, structural heart complications, or prolonged bleeding within the cohort. Despite relatively high average EuroScore II values at 9.6 ± 3.5%, the 30-day survival rate stood at 94.4%, the 1-year survival rate at 80%, and the overall mortality rate at 60 months reached 66%. Additionally, complications associated with expandable valves, including paravalvular leak, stroke, and transient ischemic attack (TIA), were observed to be less than 5% at the 1-year clinical follow-up. The mean platelet count preoperatively was 236.7 ± 81.5, and at the postoperative 12th month, it was 222.2 ± 88.6, with this difference not reaching statistical significance (p = 0.109). Importantly, there was no occurrence of new-onset thrombocytopenia in any of the patients.
CONCLUSIONS: In conclusion, SU-AVR emerges as a safe procedure with respect to thrombocytopenia, and it yields satisfactory clinical results in the examined parameters.
1.4.3. Sex-Related Differences in Outcomes After Bioprosthetic and Mechanical Aortic Valve Replacement: A Report from the National Registry
Milos Matkovic 1, Igor Zivkovic 2, Slobodan Micovic 2, Ilija Bilbija1, Petar Milacic 2, Nemanja Aleksic 1, Nemanja Milosevic 2, Svetozar Putnik 1
- 1
Department for Cardiac Surgery, University Clinical Centre of Serbia, Belgrade, Serbia
- 2
Department for Cardiac Surgery, Institute for Cardiovascular Diseases Dedinje, Belgrade, Serbia
BACKGROUND AND AIM: Limited data are available for SAVR gender-based procedural and outcome differences. This study aimed to determine whether there are baseline, practice patterns and outcomes differences of SAVR by sex.
METHOD: An observational study with data derived from the National SAVR Registry. All consecutive patients with isolated AVR with at least 3 years follow-up were divided into 4 groups according to their sex and the type of implanted prosthesis. According to the statistical analysis plan, the primary outcome of the present study was all-cause mortality at 3 years. The prespecified subgroup analyses were (1) the EACTS Guideline age-defined threshold for a mechanical prosthesis (<65 years of age) and (2) the presence of patient-prosthesis mismatch (PPM).
RESULTS: Female patients (n = 517) were older (67.2 + 9.3 vs. 64.4 + 12.2 years, p < 0.001) and had greater body mass index (2.23 + 7.2 vs. 2.01 + 0.2 m2, p < 0.005) than male patients (n = 732). Also, they had higher EUROscore values (1.85 + 1.5 vs. 1.78 + 1.9 p < 0.005) and lower EF (51.8 + 13.5 vs. 57.7 + 10.8%, p < 0.001). In subgroup of patients who received mechanical prosthesis females had a higher rate of PPM than male patents (9.1 vs. 2.2%, p < 0.001). No significant difference was seen between males and females for 3-year mortality risk (14.6% vs. 14.1%, p = 0.87). Males who underwent bioprosthetic SAVR had a significantly higher mortality risk than those who received mechanical valve prostheses HR = 0.54 (95% CI 0.36–0.81, p = 0.003). The mortality difference favoring mechanical prostheses was particularly observed in patients aged <65, HR 0.25 (95% CI 0.11–0.68, p = 0.005).
CONCLUSIONS: Females were older and had worse clinical risk profiles at index hospitalization for SAVR. No significant difference was seen between males and females for 3-year mortality risk. Further prospective studies, including international data-sharing, are needed to comprehensively assess sex-related differences in SAVR.
1.4.4. Patient-Prosthesis Mismatch After Surgical Aortic Valve Replacement with Biological Prosthesis—Sutureless vs. Non-Sutureless Valve
- 1
Department for Cardiac Surgery, University Clinical Center of Serbia, Belgrade, Serbia
- 2
Department for Cardiac Surgery, Institute for cardiovascular diseases ‘’Dedinje”, Belgrade, Serbia
BACKGROUND AND AIM: Patient-prosthesis mismatch (PPM) may impair functional capacity and survival after aortic valve replacement. The aim was to investigate the impact of PPMon survival in mid-term follow-up (up to 36 months) in patients who underwent surgical AVR with implantation of biological valves (sutureless and other stented bioprosthesis).
METHOD: An observational study was performed using the data derived from the national registry of surgical AVR. All patients with isolated AVR and biological prosthesis implanted have been enrolled in the study and were divided into two groups, according to the type of prosthesis implanted into sutureless and non-sutureless group. All groups were than divided into PPM and no-PPM groups according to the presence of PPM.
RESULTS: The total of 426 patients who underwent surgical AVR have been enrolled in the study (96 patients in sutureless and 330 patients in the non-sutureless group). In the sutureless group female gender was much more frequent compared to the other group (63 (67.1%) vs. 126 (38.6%), p = 0.001). The rate of PPM was also similar between groups 52 (55.3%) vs. 208 (63.8%) pts, p = 0.136. Survival compared for overall AVR cohort with biological valves with and without PPM was lower in the PPM group (81.1% vs. 90.7%, p = 0.001, HR 2.11 (95% CI 1.18–3.75)). Further analysis within the sutureless group revealed lower survival in the PPM group compared to non-PPM group (25.5 months vs. 34.5 months, p = 0.002, HR 7.09 (95% CI 1.62–31.25)). However, in the non-sutureless group the difference in survival in PPM and non-PPM group was not observed (30.6 months vs. 32.2 months, p = 0.219, HR 1.49 (95% CI 0.78–2.89)).
CONCLUSIONS: If the risk of PPM after the implantation of a sutureless biological prosthesis is suspected, prospective strategies to avoid PPM at the time of the operation are warranted. Aortic root enlargement with other type of biological prosthesis may be considered as alternative.
1.4.5. Evaluation of Short and Mid-Term Results of Patients Who Had Aortic Valve Neocuspidization with the Ozaki Technique
Elgin Hacızade 1, Kubilay Karabacak 2, Murat Kadan 2, Emre Kubat 2, Gökhan Erol 2, Tayfun Özdem 2 and Tuna Demirkıran 2
- 1
Gülhane Training and Research Hospital, Main Clinical Hospital of the Ministry of Defense of Azerbaijan
- 2
Gülhane Training and Research Hospital
BACKGROUND AND AIM: The gold standard treatment for severe AVD has always been aortic valve replacement (AVR), which involves the substitution of the native aortic valve with a biological or mechanical prosthesis. The Ozaki procedure is now gaining popularity in cardiac surgery centers around the world. This study aimed to present the first 85 patients with midterm experience of the AVNeo procedure of a single center.
METHOD: Pre- and post-operative data of patients who were surgically treated with aortic valve neocuspidization technique in our clinic due to aortic valve stenosis and insufficiency were obtained by scanning retrospectively from the file or automation system. In our research, the data of the series of 85 patients who applied this technique in our clinic from November 2019 until January 2023 will be evaluated. Preoperative data of patients, operative and postoperative data were collected and evaluated.
RESULTS: The mean age of patients was 58.9 ± 13.4 aged years and 48 (56.5) of them were men. The mean follow-up period of 85 patients who underwent the AVNeo technique was 19.3 ± 10.5 months. Preoperative echocardiographic findings showed us Peak aortic gradient (mmHg) was 87.32 ± 27.6, the Mean aortic gradient was 54.4 ± 18.3, and the aortic valve area (mm2) was 1.13 ± 0.33. The mean aortic cross-clamp time in our clinical series was 118.3 ± 32.3, while the cardiopulmonary bypass time was 154.5 ± 45.4 min.
CONCLUSIONS: In conclusion, the AVNeo procedure is a feasible technique for all kinds of aortic pathologies. In the AVNeo procedure, there is no prosthetic stent ring, and the glutaraldehyde-fixed autologous pericardium is directly sutured into the native aortic annulus. This technique also has much better hemodynamic results as it does not change the anatomical structure of the annulus and the commissures thus allowing normal physiological annular movements and Dynamics without reducing the valve’s functional area.
1.4.6. Medium Term Outcomes from Perceval Aortic Valve Replacement in Aotearoa New Zealand
Navneet Singh and Parma Nand
Department of Cardiothoracic Surgery, Auckland City Hospital, Auckland, New Zealand
BACKGROUND AND AIM: The Perceval bioprosthesis is a contemporary sutureless technology utilised for surgical aortic valve replacement (AVR). Perceval valves allow for AVR with reduced cross-clamp and cardiopulmonary bypass times, which correlates with improved postoperative patient morbidity and mortality. However, there is a paucity of literature reporting the medium-term outcomes from Perceval AVR in indigenous populations. We aimed to investigate the mid-term outcomes from Perceval AVR at our single centre with a significant indigenous population (Maori/Pacific).
METHOD: All consecutive patients undergoing Perceval AVR (during isolated or combined procedures) at our unit from March 2011 to August 2021 were retrospectively analysed from a prospectively-collected database. Data are presented as mean +/− standard deviation.
RESULTS: Across the 10-year study period, 145 patients (mean age: 73.2 years; males: 71.7%; indigenous Maori/Pacific ethnicity: 18.3%; mean EuroSCORE II: 3.78%) underwent Perceval AVR. The most common indication for surgery was aortic stenosis (82.5%). The operative caseload was complex, with only 27.6% of patients undergoing first-time isolated AVR. The mean cross-clamp and cardiopulmonary bypass times were 74.7 +/− 40.6 and 111.3 +/− 63.6 min respectively. Latest follow-up transthoracic echocardiography (performed at a mean of 2.2 +/− 1.7 years postoperatively) revealed that 96% of patients had either none or only trivial paravalvular/transvalvular leaks. 30-day mortality and stroke rates were 6.2% and 2.1% respectively. Medium-term survival rates across 5 year and 9.5 year follow-up were 70% and 55% respectively. There was only one reoperation on the aortic valve.
CONCLUSIONS: Across an older indigenous patient population undergoing complex cardiac surgery, Perceval AVR facilitates short cross-clamp times with excellent medium-term prosthetic valvular function. Medium-term (5-year) survival is acceptable.
1.4.7. Single Center Experience in the Aortic Valve Sparing Procedure
Stefan Stankovic, Igor Zivkovic, Petar Milacic, Petar Vukovic and Slobodan Micovic
Department of Cardiac Surgery, Institute for Cardiovascular diseases Dedinje, Belgrade, Serbia
BACKGROUND AND AIM: Aortic valve-sparing surgeries using David 1 re-implantation technique avoid the requirement of lifelong anticoagulation therapy in patients with an aortic root aneurysm. This retrospective study evaluated clinical and echocardiographic results of aortic valve-sparing procedure to repair aortic root aneurysms. We used both the department’s database and follow-up data.
METHOD: This retrospective analysis included 90 patients who had an aortic valve-sparing procedure between October 2014 and April 2021. Patients in this study had enlarged aortic roots and ascending aortas, with or without aortic regurgitation (AR). The research excluded patients with ascending aorta aneurysms and aortic stenosis, as well as those hospitalized for acute aortic dissection. During the follow-up period, patients were evaluated clinically and with an echocardiogram. The average follow-up was 25.5 months.
RESULTS: Among 90 adults undergoing aortic root replacement using David 1 procedure, the mean age was 52.4 ± 12.5 years, and most were men (82.4%). The aortic root aneurysm was associated with bicuspid aortic valve (BAV) in 30 (34.4%) patients. Concomitant procedures were performed in 17 (18.9%) patients. Median aortic cross clamp time was 112.9 ± 20.9 min. Tubular graft was used in 77 (85.6%) and Valsalva graft in 13 (14.4%) patients. Postoperatively, aortic valve insufficiency was trivial/none in 71 (78.9%) and mild in 19 (21.1%) patients. There were 3 (3.3%) in hospital deaths and 4 late deaths, after discharge. A 1 (1.1%) patient required aortic valve replacement after discharge. During the period of 2 years 82 (91.1%) patients were alive and free from aortic valve reoperation.
CONCLUSIONS: Aortic valve-sparing procedures result in excellent function of the reimplanted aortic valves, and significant left ventricle reverse remodeling following the surgery. The medium-term follow-up revealed patients’ great satisfaction with treatment results.
1.4.8. “Comparison of AVR via Conventional Full Sternotomy vs. Upper Mini-Sternotomy” Our Experience in MTI-HMC, Khyber Pakhtunkhwa, Pakistan
BACKGROUND AND AIM: Aortic valve replacement (AVR) for severe symptomatic aortic valve pathology is one of the common cardiac surgical procedures with excellent long-term outcomes. In this study we looked for outcomes like re-openings, requirements for blood transfusions, sterna wound infection, faster recovery, intensive care unit (ICU) stay and short term mortality until post-operative safe discharge from.
METHOD: We reviewed the medical records of all patients who underwent AVR surgery at our Department and 96 patients were identified. Outcomes between minimally invasive AVR group and AVR through full sternotomy group were compared.
RESULTS: Mini-sternotomy AVR procedure was done in 52 patients while conventional sternotomy AVR procedure was done in 44 patients. The mean age was 40 +/− 16 in the mini-AVR group compared to 45 +/− 18 conventional AVR group. No in-hospital mortality happened in mini-AVR group and it was associated with shorter ICU stay, faster recovery, less ventilation time, decreased requirement for blood transfusions and shorter hospital stay. Only one (1) in-hospital mortality happened in conventional AVR group. One (1) reopening happened and there was no sternal wound infection requiring re-admissions in mini-AVR group.
CONCLUSIONS: We conclude that AVR via upper mini-sternotomy is a superior modality than conventional sternotomy AVR in our experience.
1.4.9. The Aortic Root Pathologies and Surgical Management: Insights from a Single Center’s Experience
Muhammad Aasim and Raheel Khan
Department of Cardiac Surgery, Hayatabad Medical Complex, Peshawar, Pakistan
BACKGROUND AND AIM: Aortic root replacement is a complicated surgical procedure which has undergone many considerable technical improvements with time. We analyzed the results of surgical procedures for Aortic Root pathologies performed at our cardiac surgery department performed by a single consultant cardiac surgeon (Dr. M. Aasim).
METHOD: Between 2018 and 2023; Twenty seven (27) patients underwent aortic root surgery. Twenty two (22) patients were male and 5 females; their mean age was 49 +/− 20 years. Diagnosis was aortic dissection in 7 patients (Acute 2, chronic 5), aneurysm of ascending aorta in 13 patients, and Marfan syndrome in 7 patients. Nineteen (19) patients had aortic root replacement using the “modified Bental techniques”. Two (2) patients were treated using the aortic valve sparing techniques with “Dacron graft”, and 5 using aortic root enlargement. One (1) of the patients was treated using PTFE graft wrapping like the “modified personalized external aortic root support (PEARS) procedure”. Follow-up time ranges from 1 month to 5 years.
RESULTS: There was one (1) in-hospital death. One patient presented to CCU with bleeding complication within three (3) months. In remaining 25/27 patients’ good quality of life and freedom from complications is observed in follow ups.
CONCLUSIONS: The less mortality and satisfying results show that aortic root surgery is a low risk and useful treatment. Surgical procedures on the aortic root have mostly changed the quality of life in patients and extended their lifespan. These procedures will continue to grow with better graft/prosthetic material, improved valves and improvements in the surgical techniques.
1.4.10. Aortic Valve Neocuspidization with the Ozaki Procedure: Mid-Term Results
Djordje Radosav Krstic, Slobodan Micovic, Milan Cirkovic, Igor Zivkovic and Petar Milacic
Department of Cardiac Surgery, Dedinje Cardiovascular Institute, Belgrade, Serbia
BACKGROUND AND AIM: Aortic valve illnesses are the most common type of valve disease. Conventional aortic valve replacement remains the gold standard. Neocuspidization of the aortic valve using autologous pericardium is other surgical option for these individuals. The Ozaki technique produces hemodynamic values similar to a native aortic valve, therefore lifelong anticoagulant medication is not required in these individuals.
METHOD: The prospective observation research was carried out at the institution between March 2019 and March 2023. A total of 34 patients were included. We operated on patients with isolated aortic stenosis or insufficiency. A freshly made autologous pericardium was used for the neo aortic valve. Our study excluded patients with aortic valve endocarditis and those who required urgent surgery. There was no infective endocarditis among our patients. The follow-up consisted of clinical and echocardiographic (neo aortic valve function) examinations.
RESULTS: A total of 34 people were operated on using the Ozaki method. 50% of the participants were male, with an average age of 66.27 ± 5.7 SD years. Aortic stenosis was a reason for surgery in the 30 patients (88.2%) with severe aortic stenosis and 4 (11.8%) with severe aortic regurgitation. The average preoperative aortic valve gradient was 71 ± 15 SD mmHg. The cardiopulmonary bypass and cross-clamp duration were 91 and 108 min, respectively. There was no significant postoperative aortic regurgitation, and the control echo showed a mean aortic valve preasure of 11 ± 4 SD mmHg. The typical ICU and hospital stay were two and eight days, respectively. The average follow-up time is 38 months.
CONCLUSIONS: The Ozaki method is an effective alternative to surgical aortic valve therapy, particularly in individuals with a small aortic anulus. The midterm follow-up showed excellent outcomes.
1.4.11. Mid-Term Results of Ozaki Procedure—Azerbaijan Experience
Kamran Ahmadov and Kamran Musayev
Department of Cardiovascular Surgery, Merkezi Klinika, Baku, Azerbaijan
BACKGROUND AND AIM: We aimed to report outcomes of the Ozaki procedure, reconstructing aortic valve leaflets with autologous pericardium in Azerbaijan.
METHOD: In a retrospective analysis, 40 patients underwent aortic valve reconstruction (Ozaki procedure) between August 2018 and June 2023. Divided into two groups (Group A and B), patients in Group A followed Ozaki’s technique, while Group B received an additional commissure reinforcement technique. Mean ages were 63 and 65 years for Groups A and B, respectively.
RESULTS: Patients had aortic stenosis or a combination of aortic stenosis and aortic regurgitation. Preoperative echocardiography revealed peak and mean pressure gradients of 84 ± 34.6 mmHg and 50.5 ± 23 mmHg. Cardiopulmonary bypass and aortic cross-clamp times were 142/115 min and 144/107 min for Groups A and B, respectively. No in-hospital mortalities or pacemaker implantations occurred. None presented with aortic stenosis. No significant increase in aortic gradients during follow-up was noted, and no reoperations were required. Four patients in Group A developed mild aortic regurgitation during follow-up, while in Group B, aortic regurgitation was no more than minimal. Median follow-up periods were 56 and 20 months for Groups A and B, respectively. Our study showed 100% freedom from major adverse valve-related events.
CONCLUSIONS: Since Ozaki and colleagues introduced aortic valve reconstruction with autologous pericardium, it gained popularity. Mid-term Ozaki procedure results demonstrated favorable outcomes regarding mortality, valve gradients, and freedom from adverse valve-related events. However, some studies indicated slightly elevated valve regurgitation recurrence post-Ozaki procedure. Our proposed additional commissural reinforcement technique showed reduced aortic valve regurgitation during follow-up. Long-term results will follow.
1.4.12. Evaluation of the Durability of the Aortic Valve Bioprosthesis Resilia Inspiris in the Centers of Paris Public Assistance: ENDURANCE Registry
Michele D’alonzo 1, Pierre Demondion 2, Paul Achouh 3, Jean Louis De Brux 4, Pascal Leprince 2, Thierry Folliguet 1 and Antonio Fiore 1
- 1
Department of Cardiac Surgery, Hôpital Henri Mondor, Assistance Publique-Hôpitaux de Paris, Creteil, France
- 2
Department of Cardio-Thoracic Surgery, Hôpital Pitié-Salpêtrière Hospital, Assistance Publique-Hôpitaux de Paris, Paris, France
- 3
Department of Cardiac and Vascular Surgery, Hôpital Européen Georges-Pompidou, Assistance Publique-Hôpitaux de Paris, Paris, France
- 4
Department of Cardiac Surgery, The Scientific Committee of the EPICARD Registry, Angers University Hospital, Angers, France
BACKGROUND AND AIM: The prevailing approach in contemporary surgical management of aortic valve pathology is progressively leaning towards the adoption of biological prostheses. The novel Inspiris Resilia stands out as a promising solution for reducing the risk of structural valve deterioration. This study examines outcomes concerning hemodynamic performance and complications after its implantation.
METHOD: In this prospective, observational, multicenter registry all consecutive patients who underwent isolated or concomitant surgical aortic valve replacement were enrolled. Transthoracic echocardiography was performed preoperatively, at discharge and after one year of surgery. The primary endpoints were to report mortality and hemodynamic performance of this innovative bioprostheses.
RESULTS: A total of 1208 patients were included. The mean age was 63.2 ± 9.9 years (76.5% male). Most interventions were elective, with a median EuroSCORE II of 2.29%. Active endocarditis was the indication for 14.7% patients while concomitant procedures were done in 49.8% of cases.
Hospital mortality was 1.9% while one-year survival rate was 94.6%. Within 30 days, adverse events were limited: 30 patients (2.5%) required permanent pacemaker implantation; 33 patients (2.7%) experienced a stroke and only 3 patients (0.2%) showed significant paravalvular leak at discharge.
Mean pressure gradient decreased from 45.6 ± 18.2 mmHg preoperatively to 10.6 ± 4.5 mmHg at discharge and remained stable at 1-year echocardiographic control. The mean effective orifice area at last follow-up was 2.34 ± 0.56 cm2. Severe patient-prosthesis mismatch was present in 9 patients, only one patient experienced early stage 3 structural deterioration (VARC-3).
CONCLUSIONS: Our study demonstrates encouraging results in terms of safety and efficacy, with excellent one-year survival rates and good hemodynamic performance. Long-term studies are necessary to assess valve durability and its advantages in percutaneous valve-in-valve procedures.
1.4.13. Risk Factors Associated with Adverse Outcomes for Sternal Re-Entry for Surgical Aortic Valve Replacement
Philemon Gukop 1, Pouya Youssefi 1, Justin Nowell 1, Rajan Sharma 1, Robin Kanagasabay 1 and Marjan Jahangiri 2
- 1
Department of Cardiothoracic Surgery, St George’s University Hospital NHS, London, UK
- 2
St. George’s Hospital, University London, London, UK
BACKGROUND AND AIM: Sternal re-entry for cardiac surgery is associated with morbidity and mortality of up to 10% in some series. It is essential to identify risk factors associated with adverse outcomes of re-sternotomy for aortic valve replacement. This would guide patient selection for re-sternotomy to improve outcomes
Aim/OBJECTIVE: To identify factors associated with adverse outcomes for sternal re-entry for Aortic valve replacement (AVR)
METHOD: Retrospective data analysis on 178 consecutive patients who had sternal re-entry for AVR in a single centre between 2010 to 2018. Relevant data collected from patient’s records.
Univariate and multivariate regression analysis of significant variables that predict death was done.
Significant Results presented as 95% CI with odd ratio and
p-value and Kaplan-Meier’s (KM) survival curves (
Table 1).
p-value < 0.05 is significant.
CONCLUSIONS: Risk factors for Adverse outcomes for sternal re-entry for AVR include previous CABG, Active endocarditis and end organs failure requiring support.
Such patients should be pre-optimised or offered appropriate alternative treatment to improve outcomes.
1.4.14. Early and Mid-Term Results According to Valve Dimensions in Patients Undergoing Transcatheter Aortic Valve Implantation
Şennur Kızılağaç, Emrah Oğuz, Hakan Posacıoğlu, Anıl Ziya Apaydın, Ümit Kahraman, Ayşen Yaprak Engin, Irem Demiray and Mustafa Özbaran
Department of Cardiovasculer Surgery, Ege University, Izmir, Turkey
BACKGROUND AND AIM: This study aims to analyze the early and mid-term clinical results of patients diagnosed with severe aortic stenosis who underwent Transcatheter Aortic Valve Implantation (TAVI) operation using a 34-gauge valve and valves of different sizes.
METHOD: Retrospectively, a total of 152 patients who underwent TAVI surgery at Ege University Faculty of Medicine Cardiovascular Surgery Department between January 2018 and August 2023 were included in the study. In the study, patient data were obtained through file scanning and current patient records. The data obtained in the study were analyzed in the SPSS analysis program.
RESULTS: As a result of our study, it was seen that the average age of patients with 34 mm valves (Group A) was significantly younger than patients with valves smaller than 34 mm (Group B), and advanced age was found to be a risk factor in patients who developed early mortality. Operation times were similar in both groups. It was observed that patients who received 34 mm valves needed temporary and permanent pacemakers in the postoperative period. Permanent KPM implantation was evaluated as an important reason for the increase in intensive care unit stays. No significant difference was detected between the two groups in terms of PVL at the first and last postoperative follow-ups. Short and mid-term mortality occurred at levels similar to the both of this group.
CONCLUSIONS: In our study, the results obtained from both groups were similar, the complications in patients with 34 mm valves were low, intensive care and hospital stays were not long, and short and medium term mortality occurred at levels similar to the other group, indicating that the 34 mm valve can be used safely in suitable patients. This suggests that patients in the implanted group should be carefully monitored for conduction disorders due to increased KPM rates.
1.4.15. Midterm Results of Bentall Procedures
Elvin Mamiyev 1, Ümit Kahraman 2, Ayşen Yaprak Engin 2, Anıl Ziya Apaydın 2, Serkan Ertugay 2, Osman Nuri Tuncer 2, Yüksel Atay 2 and Mustafa Özbaran 2
- 1
Department of Cardiovascular Surgery, Liv Bona Dea Hospital, Baku, Azerbaijan
- 2
Department of Cardiovascular Surgery, Ege University, Izmir, Türkiye
BACKGROUND AND AIM: The aim of this study is to analyze perioperative risk factors for midterm complications and mortality after Bentall procedures.
METHOD: Between 2016–2022, 85 patients who underwent Bentall procedure and discharged were included. The data including demographics, comorbidities, preoperative echocardiographic findings, operative data, length of stay in the hospital and intensive care unit, postoperative early complication after discharge were analyzed. The patients were divided into two groups in terms of midterm complications; patients with midterm complications (group W, n = 24) and patients without midterm complications (group WO, n = 61) which were defined as graft infection, valve dysfunction, endocarditis, hemorrhage.
RESULTS: Preoperative characteristics were comparable except higher preoperative creatinine (p = 0.020), CRP levels (p = 0.008), and lower hemoglobin levels (=0.047) in Group W. Having additional procedures was significantly more common in Group W (p = 0.017 and p = 0.026). Femoral cannulation was more common compared to antegrad cannulations in Group W (p = 0.019). As early complications, cerebrovascular events with rates of 25% to 3.27% (p = 0.006) and arrythmia with the rates of 45.8% to 34.4% (p = 0.001) were observed in Group W and WO respectively. In group W, 4.7% had graft infection, 2.4% had valve dysfunction, 4.7% had endocarditis, 5.9% had tamponade, 3.5% had hemorrhage. Having a complication (p = 0.04) and each of the complications other than tamponade (CVE p = 0.025, graft infection p = 0.011, valve dysfunction p = 0.044, endocarditis p = 0.001, hemorrhage p = 0.041, arrythmia p = 0.033) were found related with midterm mortality. In ROC analyses, diameter of ascending aorta (p = 0.029), diameter of sinuses of Valsalva (p = 0.047), duration of cardiac ischemia (p = 0.027), duration of cardiopulmonary bypass (p = 0.034), femoral cannulation (p = 0.032) was found related with midterm mortality (4.7% and 1.2% respectively for groups W and WO).
CONCLUSIONS: Larger aneurysms may complicate the operations both with longer procedures and alternative cannulation sites. It should be kept in mind that femoral cannulation may bring early and late complications.
1.4.16. Aortic Valve Replacement with Right Anterior Mini-Thoracotomy: A Less Invasive Method Even for Sutured Valves
Ulku Kafa Kulacoglu, Taner Iyigun, Isa Can, Timucin Aksu and Mehmet Ali Dala
Department of Cardiovascular Surgery, Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Training and Research Hospital, Istanbul, Turkiye
BACKGROUND AND AIM: Minimally-invasive valve surgery is becoming more popular when compared with a standard median sternotomy as surgical trauma is decreased. The aim of our study is to present our clinical experience regarding the results of patients who underwent isolated aortic valve replacement, including sutured valves, via the right anterior mini thoracotomy technique.
METHOD: This study is a retrospective observational cohort study consisting of data from 30 patients who underwent isolated aortic valve replacement surgery using the right anterior thoracotomy method between February 2020–November 2023. All surgeries were performed using conventional surgical equipment. In 27 patients, peripheral cannulation and in 4 patients, vacuum–assisted (40–60 mmHg) central cannulation was performed. Subluxations of 2nd or 3rd ribs were performed for better surgical exposure. Delnido cardioplegia in 28 patients, and isothermic blood cardioplegia in 2 patients have been used. 22 mechanical valves, 7 biological valves and 1 sutureless valves were implanted.
RESULTS: We observed that post-operative intensive care unit staying was 1.3 days in average (1–3 days) and hospital staying was 8.6 days in average (5–15 days) with this technique. Average Cardio-pulmonary bypass (CPB) duration was 143.6 min (86–271 min) and cross-clamping duration was 93.6 min (45–162 min). No mortality has occurred in 30 days follow-up.
CONCLUSIONS: In selected patients, right anterior thoracotomy is a safe method due to its longer operative time as well as minimal surgical trauma, with good cosmetic results, and shorter hospital stay. Another advantage of this technique is; the surgery can be performed without any necessity for special surgical equipment even on sutured aortic valves.
1.4.17. Frequency of Aortic Root Enlargement to Prevent PPM in Patients Undergone Aortic Valve Replacement in Peshawar Institute of Cardiology
Muhammad Nisar, Aamir Iqbal and Abdul Nasir
Peshawar Institute of Cardiology, Peshawar, Pakistan
BACKGROUND AND AIM: The implantation of a prosthetic valve, that is too small due to a small aortic annulus can complicate aortic valve replacement and cause patient prosthetic mismatch. To prevent this, aortic root enlargement is effective surgical technique. Because of technical difficulty and complication, it’s not much popular among cardiac surgeons but due to large number of patients undergoing AVR with small aortic annulus, this procedure is essential for cardiac surgeons.
Aim of this study is to determine the frequency of aortic root enlargement in males and females undergoing aortic valve replacement.
METHOD: This retrospective empirical groundwork was carried out at Peshawar institute of cardiology, included (n = 76) adults, who underwent isolated AVR, AVR + ARE, AVR + CABG and AVR + MVR. Data was extracted through electronic medical record (EMR) and by using SPSS version 26.0 the data was evaluated.
RESULTS: The mean age of the patients (37.53 ± 15.589), mean BMI (24.9125 ± 5.07249), mean BSA (1.9607 ± 2.28518). Etiology showed rheumatic heart disease 48.7% to be the most prevalent one. Frequency and percentage of AVR + ARE was (9, 11.8%) respectively. Mean by-pass and cross-clamp time (mins) for other valvular surgeries and AVR + ARE (161.9254 ± 64.08737), (189.3333 ± 77.83155) (128.9701 ± 51.88857), (154.7778 ± 69.11906). Mean hospital stay (days) (6.52 ± 2.003), (5.4444 ± 1.74005) and ICU stay (days) (1.99 ± 0.945), (1.4444 ± 0.72648). The
Table 2 shows that females are more likely undergo for aortic root enlargement compared to males.
CONCLUSIONS: Although ARE is not a widely followed procedure due to the contradictory evidence from previous literature. However experienced surgeons follow it to relieve the patient from patient prosthesis mismatch. Due to high frequency of small aortic annulus in our population making this procedure essential to prevent PPM but in spite of that long term follow up and good sample size is needed in future to better analyze the long-term effects of aortic root enlargement procedures.
1.4.18. Remodeling Patterns and Evolution of Transvalvular Gradients in Aortic Stenosis Patients: A Comparison Between TAVI and SAVR with Biological Prostheses
Grigore Tinică, Andrei Țăruș, Mihail Enache, Silivu Paul Stoleriu and Alberto Emanuel Bacușcă
Department of Cardiovascular Surgery, Cardiovascular Diseases Institute “George I.M. Georgescu”, Grigore T. Popa University of Medicine and Pharmacy, Iasi, Romania
BACKGROUND AND AIM: Aortic stenosis (AS) is the most prevalent heart valve disease in the Western world and is associated with a poor prognosis after the onset of symptoms. Its prevalence is rising rapidly as a consequence of the aging population. Restoring the aortic valve function by treatment with either SAVR or TAVR aims to increase the aortic valve area, lower aortic valve gradients, reverse left ventricular hypertrophy, and reduce mortality. Our objective was to delve into the intricacies of LV mass alterations post-TAVI and SAVR, examining the factors impacting these shifts. To our knowledge, this study represents the inaugural endeavor of its kind documented in Romania.
METHOD: Conducted retrospectively, this study examined 315 patients treated from December 2014 to December 2022, dividing them into surgical and transcatheter treatment cohorts. Baseline and six-month follow-up clinical and echocardiographic data were gathered. Statistical analysis evaluated group disparities and factors predicting reduction in LV mass.
RESULTS: TAVI was associated with a faster recovery with a shorter ICU stay and a lower need of inotrope medication, but also with a higher rate of permanent pacing and a reduced LV mass regression and remodeling. The reduction in atrial volume was more pronounced in the TAVI group compared to the SAVR group. The reduction in both maximal and mean gradients and LV mass index following SAVR surpassed those observed after TAVI. Preoperative LVMi and mean pressure gradient positively correlated with LVM reduction, while TAVI negatively impacted it.
CONCLUSIONS: Both TAVI and SAVR procedures offer advantages in decreasing left ventricular mass, albeit with SAVR demonstrating superior efficacy. Identifying predictors of LV mass reduction is pivotal for enhancing treatment approaches, underscoring the importance of considering early valve replacement to prevent irreversible LV hypertrophy.
1.4.19. Perceval Sutureless Redo Aortic Valve Replacement Inside Patch-Reconstructed Aortic Roots for Infective Endocarditis: A Case Series
Navneet Singh, Parma Nand
Department of Cardiothoracic Surgery, Auckland City Hospital, Auckland, New Zealand
BACKGROUND: We highlight the novel use of the Perceval sutureless bioprosthesis in a new context; that is, for redo aortic valve replacement inside reconstructed neo-aortic roots following debridement of infected root abscesses.
CASE: We have used Perceval valves in this context in five cases. As an example of one of our cases, a 67-year-old obese male had a history significant for St Jude aortic valve replacement in 2015 for aortic stenosis. The patient subsequently presented in 2022 with Staphyloccus epidermidis endocarditis. Transoesophageal echocardiography revealed a large 1.8 cm vegetation on the prosthetic aortic valve leaflets. This was causing obstruction to disc motion. The vegetation was adherent to the aortomitral curtain and was associated with an aortic root abscess that extended posteriorly and into the base of the anterior mitral leaflet. The patient developed complete heart block and embolic strokes. He proceeded urgently to theatre.
A redo median sternotomy was undertaken with central cannulation for cardiopulmonary bypass. The St Jude valve was removed. A 3 × 2 cm aortic root abscess was debrided and the root and aortomitral curtain reconstructed using bovine pericardium. A large size Perceval valve was implanted in an intra-annular position in the neo-aortic root, with the guiding sutures tied down to provide further security to the valve seating. The patient had an unremarkable postoperative course.
We report the first known successful implantation of the Perceval sutureless bioprosthesis for redo aortic valve replacement inside a patch-reconstructed neo-aortic root for prosthetic valve infective endocarditis involving a large root abscess. Of note, we have used the Perceval valve in four other similar cases. This highlights the value of sutureless valves in hostile aortic roots with fragile tissues demanding minimal suturing.
1.4.20. A Novel Perspective: Employing Right Vertical Infra-Axillary Mini-Thoracotomy for Interventions on Aortic Root or Ascending Aorta
Ahmet Arif Ağlar and Ahmet Yavuz Balci
Department of Cardiovascular Surgery, Medistate Kavacik Hospital, Istanbul, Turkiye
OBJECTIVE: The popularity of minimally invasive techniques for the ascending aorta is on the rise, commonly employing incisions such as mini-sternotomy and right anterior mini-thoracotomy. Our research presents a novel and secure method for managing ascending aorta and/or aortic root pathologies, implemented through a right infra-axillary vertical mini-thoracotomy.
METHODS: Three patients diagnosed with ascending aortic aneurysm underwent surgery, with the first procedure taking place in April 2023 and utilizing a right infra-axillary vertical mini-thoracotomy. The primary selection criteria took into account four excluding factors: a history of prior cardiac surgery, a diagnosis of endocarditis, the presence of pathology necessitating intervention in the aortic arch, and the need for coronary artey bypass grafting. The surgical interventions involved the Bentall procedure with bioprosthetic aortic valve for one patient, supracoronary ascending aortic replacement for another, and aortic valve replacement + supracoronary ascending aortic replacement for the third patient. The infra-axillary mini-thoracotomy was performed through a 8-cm vertical skin incision centering the right fourth intercostal space on the anterior axillary line.
RESULTS: The average age of the cases was 48.3 ± 11.46, and all three were male. The mean length of hospital stay is 7.6 ± 1.6 days. The average follow-up duration is 4.6 months. No morbidity or mortality was observed.
CONCLUSIONS: Utilizing a minimally invasive approach through a right vertical infra-axillary mini-thoracotomy can serve as a secure alternative to the standard procedure for interventions on the ascending aorta and aortic root, with or without aortic valve involvement. This approach is considered safe for selected patients with ascending aortic and/or complex aortic root pathologies.
1.4.21. Simultaneous Coronary Bypass and Patent Foramen Ovale Closure with Removal of Lamble’s Excrescences on Aortic Valve
Zeki Temìztürk, Abdussamet Asaroğlu, Burak Balcı, Mehmed Yanartaş and Nihan Kayalar
Başakşehir Çam and Sakura City Hospital, Cardiovascular Surgery Clinic, Istanbul, Turke
OBJECTIVE: Lambl’s Excrescences are rare cardiac structures described as fine, mobile, filiform fronds that typically occur at sites of valve closure, and are believed to result from minor endothelial damage due to valve wear and tear. We aimed to discuss our treatment approach in an asymptomatic Lamble’s excresences patient who will undergo open heart surgery.
METHODS: Patient was a 73 years old female who presented with shortness of breath. She had normal sinus rhythm and her neurological examination was normal. Transosephageal echocardiography showed patent foramen ovale (PFO) and multiple fibrillar structures on all cusps of aortic valve and the most probable diagnosis was Lamble’s excresences. A coronary angiogram revealed 3 vessel coronary disease requiring coronary bypass grafting. The operation included 3 vessel CABG, PFO closure and removal of lambl’s excresences from the aortic valve.
RESULTS: As a result of the excision material sent for pathology examination, the diagnosis of Lambl’s Excrescences was confirmed. (picture 1). The patient was discharged after an uneventful postoperative period.
DISCUSSION: Currently, there is no common consensus on the treatment of Lambl’s Excrescences. The reports on coincidental detection or diagnosis in asymptomatic patients are very scarce and concomitant removal along with other cardiac surgeries is extremely rare. Although our patient was asymptomatic, due to the presence of multiple mobile structures we performed resection of Lambl’s Excrescences to confirm the diagnosis and to prevent the possible risk of postoperative embolism and cerbrovascular events.
CONCLUSION: In patients who will undergo other cardiac operations, we suggest that coincidental Lambl’s Excrescences should be removed especially if they are multiple and mobile. This adds little risk to the operation and may prevent postoperative emboli. Further studies and more cases will help to establish a better consensus on the treatment strategies.
1.4.22. Management of a Patient with an Atheromatous Penetrating Aortic Ulcer (PAU) Rupture
Timuçin Sabuncu, Raksana Mahmudova, Anıl Cankurt, Ismail Yolcu and Oktay Peker
Department of Cardiovascular Surgery, Hacettepe University, Ankara, Turkey
A 74-year-old female patient who applied to the emergency room with complaints of chest pain, cough and shortness of breath; the patient’s history, revealed that, she applied to the emergency room with similar complaints 6 months ago; but there were no abnormal evidence were found in the examinations at that time.
In laboratory tests; Hb 10.3 g/dL, leukocytes: 13.2/mm3, platelets: 452,000/mm3, creatinine: 0.57 mg/dL, glucose: 191 mg/dL, procalcitonin: 0.38 ng/mL, CRP: 52.8 mg/L, Troponin-I: 20 ng/mL, BNP: 35.4 pg/mL. COVID Ag test (−), arterial blood gas sampling pH: 7.39, lactate: 3.9 mmol/L.
Echocardiography revealed a fibrinous pericardial effusion with a thickness of 16 mm in the infracardium, 19 mm in the lateral wall, and 19 mm in the vicinity of the apex. Moderate mitral regurgitation and moderate-severe tricuspid regurgitation were observed. Pulmonary artery pressure was measured as 45 mmHg.
The cardiovascular surgery department was consulted after triple rule out CTA showed excess contrast filling, compatible with intramural hematoma and 2 ulcerated plaques in the ascending aorta with accompanying hemopericardium.
The patient was taken to surgery. CPB initiated with femoral artery and vein cannulation. Sternotomy was performed. Pericardium was opened. Hemorrhagic pericardial fluid was aspirated. It was observed that the heart and aorta were covered with hematoma. The hematoma was drained. The penetrating ulcerative segment in the ascending aorta was resected from the sinutubular junction to the beginning of the arch, and the ascending aorta was replaced with a 28 mm diameter tubular dacron graft.
In the postoperative period, diabetes insipidus and polyuria clinic were observed. Patient consulted with the department of endocrinology and recommended follow-up with fluid replacement. The patient, who had no other problems in the postoperative period, was discharged with full recovery on the 8th postoperative day. The patient, who was examined on the 45th postoperative day, is being followed without any problems.
1.4.23. Clinical Case of Interrupted Aortic Arch and Critical Aortic Stenosis in Adult
Kirill V. Mershin 1, Nikita P. Myakin 1, Yuliya V. Cherkashina 1, Gamid M. Kurbanov 1, Vilnur V. Gazizov 1, Elina E. Vlasova 1, Evgenii A. Tabakian 1, Grigorii A. Shiryaev 2, Maksim A. Khabarov 1, Dmitrii V. Petrovskii 1, Renat S. Akchurin 1 and Andrey A. Shiryaev 1
- 1
Cardiovascular Surgery Department, FSBI NMRCC Named After Academician E.I. Chazov of the MH of the RF, Moscow, Russia
- 2
Tomography Department, FSBI NMRCC Named After Academician E.I. Chazov of the MH of the RF, Moscow, Russia
BACKGROUND: Interrupted aortic arch (IAA) is a rare congenital anomaly of aorta with limited number of case reported. Loss of communication between the arch and descending aorta is often associated with other congenital heart defects such as bicuspid aortic valve (AV). Our report demonstrates the surgical approach and hospital postoperative result in patient with critical aortic stenosis and previously unknown IAA.
METHODS: A 58-year-old female was admitted in cardiovascular department for AV replacement in FSBI NMRCC named fater academitian E.I. Chazov in November 2023. She had no known growth and development abnormalities. She had the history of arterial hypertension since youth, two pregnancies followed by non-complicated childbirths and two healthy children. Dyspnea has appeared in 2022 and has worsened in May 2023; at the same time angina pectoris and the lower extremities swealing were noted. Transthoracic echo has revealed critical aortic stenosis and AV replacement was recommended. The additional examination has detected unsuspected IAA. The patient showed no lower extremity ischemia, no serious chronic kidney disease, and it was concluded that there was sufficient collateral blood flow to the lower part of the body. The cardiac team analyzed the examination data including the difference between the upper and lower extremities arterial pressures at rest and during exercise. Based on this, a decision was made to perform isolated aortic stenosis correction by mechanical valve replacement with additional lower body perfusin through femoral canula. In the postoperative period a 3rd degree AV block developed and a permanent pacemaker was implanted. Patient was mobilized in standard terms and was discharged on 12th day.
CONCLUSIONS: Based on this case of patients with IAA and critical aortic valve stenosis, isolated surgical aortic valve replacement with additional lower body perfusion can be chosen.
1.4.24. Recurrent Cardiac Papillary Fibroelastoma with Multiple Organ Embolism—Is It Really Benign?: A Case Report
- 1
Başakşehir Çam and Sakura City Hospital, Istanbul, Turkey
- 2
Bayındır Söğütözü Hospital, Ankara, Turkey
A 50-year-old female patient was admitted to an external center with the complaint of pain in her leg and embolectomy was performed. She was referred to us after a 12 × 12 mm mass was detected at the level of the aortic valve. There was no abnormality in her examination. Due to sudden onset of pain, femoral embolectomy was performed. She was then operated, and a fragile, lobulated mass extending over the aortic valve noncoronary leaflet was removed. No dysfunction was observed in the aortic valve. Fibrous material was detected in the pathology report. After the femoral embolectomy, the material sent to pathology was also found to be fibrinous material. The patient did not develop any complications, and was discharged.
Two years later, a solid mass of 10 × 9 mm was detected in the left leaflet of the aortic valve of the patient who developed dyspnea. Ejection fraction: 40%, moderate aortic regurgitation, and a maximum gradient of 27 mmHg in the aortic valve were detected. On computed tomography of the abdomen, there was an ischemic lesion area of embolism and infarct areas in the right kidney. There were ischemic areas in the upper pole posterior and lower pole of the left kidney. An infarct area due to embolism was detected in the posterosuperior part of the spleen.
It was decided to re-operate the patient. There was a 1 × 1 × 0.5 cm rough, hard mass on the right aortic leaflet with a broad base, extending between the right and left leaflets, and restricting the movement of both leaflets. The mass was excised together with the dysfunctional aortic valve. The aortic root was enlarged with the Nick technique using and a 23 St. Jude mechanical valve was implanted. In the pathology report, it was observed that fibrous connective tissue was formed in the blood-fibrin association. She was extubated on time and discharged.
1.4.25. Floating Thrombus on the Junction Between Ascending Aorta and Aortic Arch: To Operate or Not to Operate?
Estelle Démoulin 1, Tomasz Nalecz 1, Raoul Schorer 2, Ariane Lepot 2, Bernhard Walder 2, Christoph Huber 1 and Mustafa Cikirikcioglu 1
- 1
Division of Cardiovascular Surgery, Department of Surgery, University Hospitals and Faculty of Medicine, Geneva, Switzerland
- 2
Division of Anaesthesiology, Department of Anaesthesiology, Intensive Care and Pharmacology, University Hospitals and Faculty of Medicine, Geneva, Switzerland
BACKGROUND AND AIM: Floating aortic thrombi represent a rare yet potentially life-threatening pathology. Current literature delineates varied treatment modalities (surgical resection vs. anticoagulation or fibrinolytic therapy) contingent upon patient operability and overall condition. We present our approach to preoperative preparation, timing, and surgical technique in a patient harboring a floating aortic thrombus located at the junction of the ascending aorta and aortic arch.
Patient and METHODS: A 59 year-old male presented with abdominal pain and vomiting to our emergency department. Abdominal imaging revealed mesenteric ischemia and intestinal necrosis, necessitating emergency laparotomy with resection of a long segment of the jejunum. Subsequent detailed postoperative evaluation in the intermediate care unit raised suspicion of acute neurologic syndrome, prompting cranial and full-body CT imaging to ascertain the source of recent cerebral and mesenteric embolization. Imaging revealed a floating aortic thrombus at the junction of the ascending aorta and aortic arch. A multidisciplinary discussion ensued to determine optimal treatment to forestall further morbid and lethal embolization. Emergency MRI excluded hemorrhagic transformation and perioperative bleeding risk, allowing cardiac surgery. Surgical intervention comprised median sternotomy, deep circulatory arrest with anterograde cerebral perfusion, aortotomy without cross-clamping, resection of the floating thrombus and atheromatous ascending aorta, minor curve of the aortic arch, and hemiarch replacement with a Dacron graft. Seventy hours after admission the patient left the intensive care unit with an excellent recovery. Postoperative investigations confirmed hepatocellular carcinoma, elucidating the patient’s heightened propensity for clot formation.
CONCLUSIONS: This case underscores life-threatening danger of floating thrombi in the ascending aorta. Timely diagnosis and surgical intervention are imperative to avoid embolic sequelae and disability. Early multidisciplinary collaboration and vigilant perioperative monitored care are paramount in effectively managing these complex cases. An international register for these rare cases is warranted to refine diagnostic and therapeutic approaches including patient-relevant outcomes.
1.4.26. Performing Bentall Operation via Left Thoracotomy: An Unusual Case
Seçil Öztürk Küçüker, Irem Iris Kan, Atıf Yolgösteren and Mustafa Tok
Department of Cardiovascular Surgery, Bursa Uludag University, Bursa, Turkey
A 46-year-old female patient with a known history of hypertension and diabetes mellitus was admitted to our hospital for pain in her left arm. She had pectus excavatum in physical examination, and her peripheral pulses were palpable. In upper extremity CT angiography, a bilateral subclavian artery aneurysm was detected. Coil embolization was applied to the right subclavian artery, and a stent was placed in the left subclavian artery. Thoracal, abdominal, and pelvic CT angiographies were done to exclude any other accompanying aneurysms. A sinus valsalva aneurysm with a diameter of 59 mm was detected.
Since the patient had pectus excavatum deformity and the heart was located more to the left than usual, performing a Bentall procedure by a left thoracotomy was considered in the surgical approach of this patient. The operation was performed by cannulating the left femoral artery and vein.
The patient was extubated on the postoperative second day and was discharged from the intensive care unit on the postoperative fifth day. On the ninth postoperative day, the patient had the symptoms of cardiac tamponade and was re-operated. Early extubation was performed after re-operation. Eight hours after the second operation, the cardiac tamponade recurred, requiring a third operation. Again, early extubation was performed, and the patient was discharged after being hospitalized for two days in the intensive care unit and 11 days in the ward.
In the literature, the Bentall surgeries performed by thoracotomy are scarcely found, and almost all of these cases were performed using a right-sided approach. As a general notion of medicine, we should treat the patient, not the disease. The approach to the patient may differ according to other co-existent medical conditions. Considering the patient’s anatomical features, a left thoracotomy was more suitable in our case.
1.5. CARDIAC » Atrioventricular Valve (Mitral/Tricuspid) Surgery
1.5.1. Early and Mid Term Results of Repair of Mitral Valve by Transapical Neochorda Implantation on Beating Heart
Furkan Burak Akyol 1, Emre Kubat 1, Gökhan Erol 1, Murat Kadan 1, Kubilay Karabacak 1, Tayfun Özdem 1, Tuna Demirkıran 1 and Cengiz Bolcal 2
- 1
Department of Cardiovascular Surgery, Gülhane School of Medicine, Health Sciences University, Ankara, Turkey
- 2
Department of Cardiovascular Surgery, Memorial Hospital, Ankara, Turkey
BACKGROUND AND AIM: Transapical beating heart neochord implantation is one of the latest techniques. Gulhane Training and Research Hospital has been applied this technique to 31 patients and has the largest case series in the country. There are approximately 1000 cases around the world, therefore investigating the results of this technique are limited. In this study, we aimed to analyse the epidemiological, biochemical and radiological results of the patients who underwent this surgery retrospectively and assess the morbidity and the mortality rates of the patients.
METHOD: In our study, 31 patients who underwent transapical beating heart neochord implantation were included. Demographic data, comorbidities, stages of heart failure, preoperative echocardiographic measurements, preoperative risk assessment, operative characteristics, postoperative outcome, postoperative follow-up data of the 31 patients who underwent neochord implantation with NeoChord DS1000 device were extracted and analysed retrospectively.
RESULTS: 87.1% of the patients were male. Mean age was 57.1 ± 14 and mean BMI was 25.7 ± 3.6. The most frequent comorbidities were HT (35.5%), DM (16.1%), AF (16.1%) and CHF (13%). Mean operative time was 122.2 (±14.3) min and the number of implanted chordae were betven 2 and 7. Almost all patients (96.8%) were discharged with grade 1 or less MR. 17% of the patients had mean or higher MR on the first postoperative year. One of these patients had 3rd grade MR due to implanted posterior chordae rupture and was operated. 38% of the remaining 29 patients had mean of higher MR on longer follow up examinations.
CONCLUSIONS: This study in which we analysed the results of the patients who underwent mitral valve repair using NeoChord technique shows that we have success, morbidity and mortality rates similar to the existing literature. These results of our first experience with this technique which was showed to have acceptable morbidity and mortality rates even in learning process, were assuring and similar to the literature. However, longer follow up data and larger studies are needed.
1.5.2. Clinical Outcomes of Patients Presented with Mitral Valve Endocarditis Undergoing Surgery: A Long-Term Single Centre Study
Ali Haddad 1, Alexandros Merkourios Dimitriou 2, Gina El Gabry 2, Aydin Demircioglu 3, Lena Van Brakel 2, Ilir Balaj 2, Matthias Thielmann 2, Markus Kamler 2, Thorsten Brenner 1, Payam Akhyari 2 and Sharaf Eldin Shehada 2
- 1
Department of Anesthesiology and Intensive Care Medicine, University Hospital Essen, University Duisburg-Essen, Essen, Germany
- 2
Department of Thoracic and Cardiovascular Surgery, West German Heart and Vascular Centre, University Hospital Essen, University Duisburg-Essen, Essen, Germany
- 3
Institute of Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, University Duisburg-Essen, Essen, Germany
BACKGROUND AND AIM: Management of patients presenting with mitral valve endocarditis (MVE) is complicated and associated with high morbidity and mortality. We evaluate patients with MVE who underwent surgery in our department and analyze factors that predicted early and late mortality.
METHOD: A retrospective cohort evaluating 171 consecutive patients presented with MVE undergoing cardiac surgery in our department between 01/2010–12/2020. Endpoints are early and long-term survival outcomes. Multivariate analysis was used to define predictors of mortality.
RESULTS: Mean age was 61.4 ± 13.2 y; male (61.4%). One third of patients presented with previous cerebrovascular event (35.7%), 20% had previous cardiac surgery, 51.9% had renal failure and 25.4% had sepsis. Mean logistic EuroScore was 24.9 ± 20.6% and Mean STS-PROMM was 24.9 ± 20.6%. Majority of patients (59.6%) underwent urgent/emergent surgery and half of them (50.9%) required concomitant procedure. Postoperative results showed low cardiac output syndrome (LCOS) in 19.6%, cardiopulmonary resuscitation (CPR) in 5.4%, need for dialysis in 19%, sepsis in 13.6%, revision for bleeding in 12.5% and 30-day mortality in 18.7%. Late outcomes reported one-year and overall mortality in 21.1% and 35.7% of patients respectively. Multivariate analysis reported preoperative renal failure (odds ratio (OR), 1.16; 95% confidence interval (CI), 1.061 to 1.269; p = 0.001), non-elective surgery (OR, 1.162; 95% CI, 1.037 to 1.302; p = 0.009), postoperative LCOS (OR, 1.265; 95% CI, 1.146 to 1.398; p < 0.001), revision for bleeding (OR, 1.151; 95% CI, 1.043 to 1.27; p = 0.005), sepsis (OR, 1.27; 95% CI, 1.157 to 1.394; p < 0.001), dialysis (OR, 1.121; 95% CI, 1.005 to 1.25; p = 0.041) as strong predictors of early-mortality.
CONCLUSIONS: Outcomes of patients with MVE undergoing cardiac surgery report high mortality as expected by risk scores. The risk increases significantly in patients presented with preoperative renal failure undergoing non-elective surgery, concomitant procedure and those who required revision for bleeding, developed postoperative renal failure, LCOS or sepsis.
1.5.3. Tricuspid Valve Replacement: Not a Metallic Touch
Mehmet Cahit Sarıcaoğlu 1, Yusuf Çorbacıoğlu 1,2, Nur Dikmen 1, Ali Ihsan Hasde 1, Mustafa Bahadır Inan 1 and Ahmet Ruchan Akar 1
- 1
Department of Cardiovascular Surgery, Ankara University, Ankara, Turkey
- 2
Department of Cardiovascular Surgery, Gaziantep City Hospital, Gaziantep, Turkey
BACKGROUND AND AIM: The debate concerning the optimal type and patients of tricuspid position continues. We analyzed the short and long-term results of biological prostheses in patients who underwent isolated or combined tricuspid valve replacement, at our cardiac surgical centre in capital of Turkey.
METHOD: From September 2009 to May 2022, 74 patients underwent tricuspid valve replacement. Patients were divided into an isolated group or a combined group according to whether their surgery was combined with a left heart valve or aortic surgery. Mechanical tricuspid valve replacement was excluded and 33 patients underwent bioprosthetic tricuspid valve replacement (isolated group: 21 vs. combined group: 12). We reviewed preoperative characteristics and analysed operative data, outcomes and mortality in combined or ITVR groups.
RESULTS: Thirty-three patients underwent ITVR, mean age 54.1 ± 15.9 years, 55% female and mean BMI 26.22 kg/m2. Mean logistic EuroSCORE-STS score was 10.1–9.4 for combined group and 6.4–4.5% for isolated group. Etiologies were functional insufficiency (45%), endocarditis (36%), degenerative (3%), rheumatic (3%) and congenital (3%). Postoperative complications were: need for transfusional support (45.6%), inotropic support longer than 48 h (38.2%), prolonged invasive ventilation over 24 h (35.3%), new onset of atrial fibrillation (12.1%), duplication or postoperative creatinine over 2 mg/dL (5.9%), dialysis (9.1%), stroke (3%), intra-aortic balloon pump (6%), permanent pacemaker implantation (3%) and sepsis (3%). Post operative short-term mortality in the combined group was higher (n = 9, 4%) than that in the isolated group (n = 4, 3%).
CONCLUSIONS: Every decision regarding tricuspid valve prostheses should be individualized, but according to recent research, in isolated tricuspid valve surgery, biological prostheses replacement may be an optimal choice for patients.
1.5.4. Novel Paired-Ring Sizer Accurately Predicts Changes in Leaflet Coaptation Length: Validation in Cadaveric Swine Heart Model
BACKGROUND AND AIM: A novel “paired-ring” mitral annuloplasty ring sizing device/technique was introduced at AATS Mitral Conclave 2023 as proof-of-concept and is now approved for first-in-human trial at our institution. This technique has the potential to dramatically improve ring selection during valve repair procedures by allowing the surgeon to predict/preview coaptation length (CL) prior to ring implantation. The sizer can be designed to function in conjunction with any commercially available annuloplasty ring/band (across all sizes). The presented prototype corresponds specifically with the Physio-2 ring.
METHOD: Cadaveric swine hearts (n = 8) were used to validate ring sizing method/device performance. For each procedure, an ink mark was placed on the anterior mitral leaflet as an initial reference point. Saline pressure test was used to distend the left ventricle. Distance from the ink mark to the exact point of anterior leaflet coaptation was measured to establish a baseline point of reference. Paired-ring sizer was used to produce a moderate downsizing of the annulus. The left ventricle was distended with saline. Distance from the reference ink mark to the (new) point of anterior leaflet coaptation was measured under the temporary influence of the sizer. The difference between the two measurements represents the potential increase in CL as predicted by the sizer. The sizer was removed and a corresponding (size) Physio-2 ring implanted in standard fashion. “Predicted” and “actual” CLs were compared.
RESULTS: A moderate increase in CL was achieved (2.0–5.5 mm) in seven hearts, and no change in one heart (because it was too small). Initial “predicted” CLs corresponded well (≤0.5 mm difference) with final “actual” CLs in all 8 hearts.
CONCLUSIONS: Functionality of a novel paired-ring mitral sizing device and method were validated using a cadaveric swine heart model. CL changes predicted by the sizer corresponded accurately with CL produced by its corresponding commercially available annuloplasty ring implant.
1.5.5. Short-Term Outcomes of a Novel Technique: Ozaki Procedure with Right Vertical Infra-Axillary Mini-Thoracotomy
Ahmet Arif Ağlar and Ahmet Yavuz Balci
Department of Cardiovascular Surgery, Medistate Kavacik Hospital, Istanbul, Turkiye
BACKGROUND AND AIM: The Ozaki procedure, known for its notable mid-term outcomes in aortic valve reconstruction, traditionally necessitates conventional sternotomy. While there are limited reports on the viability of mini-sternotomy for the Ozaki procedure, there is a lack of studies on the mini-thoracotomy approach. This study aims to disclose the short-term outcomes associated with the Ozaki technique when applied with the right vertical infra-axillary mini-thoracotomy approach.
METHOD: We conducted a retrospective analysis on eight consecutive patients (5 males and 3 females) who underwent the Ozaki procedure using right vertical infra-axillary mini-thoracotomy between October 2020 and August 2023. Surgical indications for aortic valve intervention included severe aortic stenosis in seven patients and severe aortic regurgitation in one patient. Furthermore, one patient underwent an additional procedure, specifically tricuspid DeVega annuloplasty.
RESULTS: The Ozaki procedure with mini-thoracotomy was successfully performed in all patients. The mean age was 68.6 ± 10.9 years. The overall duration of follow-up was 18 ± 10.5 months. Postoperative echocardiographic assessment showed a mean peak pressure gradient of 18 ± 8.9 mmHg at discharge, and 12.6 ± 5.4 mmHg at last follow-ups. In follow-ups, aortic regurgitation was not observed in 5 patients, while it was mildly observed in 3 patients. There was no mortality and morbidity. In one case, endocarditis manifested in the neo-aortic valve four months after the operation, necessitating the aortic valve replacement (AVR) with mechanical prosthesis.
CONCLUSIONS: The Ozaki procedure utilizing right vertical infra-axillary mini-thoracotomy demonstrated favorable feasibility, hemodynamic performance, and safety in the short-term. Extended follow-up is required to assess its midterm to long-term outcomes.
1.5.6. Does Modified del Nido Cardioplegia Enhance Minimally Invasive Atrio-Ventricular (A-V) Valve Surgery?
- 1
Cardiothoracic Unit, Department of Surgery, Universiti Malaya Medical Centre, Kuala Lumpur, Malaysia
- 2
Faculty of Medicine, Universiti Malaya, Kuala Lumpur, Malaysia
- 3
Cardiothoracic Unit, Kpj Damansara Specialist Hospital 2, Kuala Lumpur, Malaysia
BACKGROUND AND AIM: We investigate the efficacy of modified del Nido solution (DNS) with intermittent blood cardioplegia (IBC) in patients who underwent minimally invasive A-V valve surgeries.
METHOD: A two-year single-centre, single-surgeon retrospective cohort study was conducted. We excluded aortic and pulmonary valve surgeries as well as cases requiring sternotomy, Maze procedure and Left Atrial Appendage (LAA) ligation. The controls were similar cases using IBC. The modified DNS was made using our formulation. Primary outcomes were operating time and number of extra repair procedures. Secondary outcomes were severity assessed by post-operative follow-up echocardiograms.
RESULTS: Between January 2022 and December 2023, 38 adult patients who underwent MIS A-V valve surgeries were included. DNS was used for 14 patients while IBC was used for 24 patients. There were 18 cases of mitral valve repair, 9 cases of mitral valve replacement, 9 cases of mitral valve replacement and tricuspid annuloplasty, and 2 others. In general, the DNS group demonstrated shorter cardiopulmonary bypass time (177.07 ± 35.40 vs. 193.58 ± 43.72 min) and shorter aortic cross-clamp time (117.38 ± 26.71 vs. 130.66 ± 41.81 min). Despite a shorter operating time, the DNS group had slightly more additional procedures with the mitral repair technique. During one-month follow-up echocardiogram, only one patient in DNS group showed increase in severity compared to three in the IBC group.
CONCLUSIONS: Modified DNC is a safe and effective alternative to IBC for MIS A-V valve surgeries. It provides minimal interruption to the surgeons during the surgeries.
1.5.7. Time to Change Traditional Way of Warfarin Management in Developing World? 1 Year Follow-Up of Patients Undergone Mechanical Valve Replacement in Newly Established Cardiac Center
Muhammad Tariq and Aamir Iqbal
Cardiac Surgery Department, Peshawar Institute of Cardiology, Peshawar, Pakistan
BACKGROUND AND AIM: Due to the higher prevalence of rheumatic heart disease in underdeveloped nations, mechanical heart valves remain the preferred choice for younger patients, exposing them to an increased risk of thromboembolism and bleeding complications. The main aim of the study was to investigate the complications and mortality rates linked to mechanical heart valve replacement in patients within a developing country at 1 year.
METHOD: This retrospective observational study was conducted on the patients presented AVR, MVR and DVR at the Cardiac Surgery Department of Peshawar Institute of Cardiology (PIC). The data of 258 patients was collected between a period of two years i.e., from Jan 2021 till Dec 2022 (
Table 3).
RESULTS: Out of 258 patients, 39 (15%) were readmitted for issues including pericardial effusion, pleural effusion, bleeding, endocarditis, hemorrhagic stroke, stuck valve. The in-hospital mortality rate was 2.7%, and the 1-year mortality rate was 10.3%, with 14 cases (51.86%) attributed to warfarin-related complications. The number of INR tests conducted after discharge within one year was 8.34 ± 8.268. Additionally, the number of consultations for INR management in one year was reported as 2.53 ± 3.715.
CONCLUSIONS: According to our findings, warfarin-related complications significantly contribute to mortality and morbidity among patients with mechanical valves in developing countries. Given this, it’s imperative for new cardiac centers in these regions to adopt more innovative strategies like establishing warfarin clinic, self-testing device, remote cardiac centers to decrease complications.
1.5.8. Management and Midterm Results of Acute Type A Aortic Dissection
- 1
Department of Cardiovascular Surgery, EGE Hospital, Baku, Azerbaijan
- 2
Department of Cardiovascular Surgery, Central Clinic Hospital, Baku, Azerbaijan
- 3
Department of Cardiovascular Surgery, Central Customs Hospital, Baku, Azerbaijan
BACKGROUND AND AIM: The best surgical management of acute type A aortic dissection remains controversial. The purpose of this study was to clarify our experience with management of acute type A aortic dissection and report our midterm results.
METHOD: Between October 2016 and March 2022, 48 patients patients with acute type A aortic dissection underwent emergency surgery in our center. Following the prompt diagnosis with computer tomography and echocardiography, emergency surgical central repair with predominantly axillary cannulation (87.5%) was performed. The mean follow-up was 4.3 +/− 1.8 years.
RESULTS: Mean age was 45 +/− 17 years, 89.6% were men. On admission, 20.8% (n = 10) of patients had cardiac tamponade. The incidence of cardiogenic shock were presented in 37.5% (n = 18) of patients. 6% of patients had bicuspid aortic valve, 27% had Marfan syndrome. Performed concomitant procedures included: 5% (n = 10) coronary artery bypass grafting, 1% (n = 10) repair of coarctation of aorta, 1% (n = 10) repair of atrial septum defect. Aortic valve were preserved in 54.2% (n = 10) of patients. 41 patients had an ascending aorta and 4 patients had partial arch replacement. Total circulatory arrest was used in 45 patients (93.8%), with mean time 4.4 +/− 3.8 min. There were 5 (10.4%) in-hospital deaths. Neurological complications presented in 29.2% (n = 14), with postoperative stroke in 10.4% (n = 5) of patients. Preoperative cardiogenic shock and renal failure are the independent risk factors for poor outcome (p < 0.001). Discharged patients had overall survival of 71.4% at 5 years.
CONCLUSIONS: Prompt diagnosis, following by emergent central repair with preferably axillary cannulation provides satisfactory results for patients with acute type A aortic dissection. Mid-term prognosis after surviving the operation is good.
1.5.9. Endoscopic Minimally Invasive Approach Versus Median Sternotomy for Multiple Valve Surgery: A Propensity-Matched Analysis
Saad Salamate 1, Farhad Bakhtiary 1, Ali Bayram 2, Miriam Silaschi 1, Ömür Akhavuz 1, Mirko Doss 2, Sami Sirat 2 and Ali El Sayed Ahmad 1
- 1
Departement of Cardiac Surgery, University Hospital Bonn, Bonn, Germany
- 2
Department of Cardiac Surgery, Helios Hospital Siegburg, Siegburg, Germany
BACKGROUND AND AIM: Endoscopic minimally invasive valve surgery is a promising alternative to valve surgery through median sternotomy. Our study aims at comparing the short-term outcomes of patients undergoing endoscopic minimally invasive multiple concomi-tant valve surgeries (MIMVS) with median sternotomy (MS).
METHOD: Demographic, clinical, and procedural data of all consecutive patients who under-went multiple valve surgeries at two institutions in Germany from March of 2017 to March of 2023 were retrospectively collected. Patients were divided into two groups: MIMVS versus MS and their out-comes were compared before and after propensity score matching. Primary endpoint was the incidence of 30-day mortality.
RESULTS: 317 patients were included in the study, 112 patients in each group were matched 1:1. MIMVS was performed on 123 patients. Within the unmatched patients, 30-day mortality rates were 7.3% for MIMVS versus 14.4% for MS (p = 0.055), 8% vs. 12.5% after matching (p = 0.28). Median blood transfusion in the MIMVS group was 0 [0–3] vs. 1 [0–4] in the MS group both before (p = 0.014) and after (p = 0.002) matching. MIMVS was associated with similar cardiopulmonary bypass time 105.5 [79.8–124] versus 98 [68.8–130.3] min and aortic cross clamping times 70 [53–80.3] versus 63.5 [46–90.3] min (p-values 0.9 and 0.76 respectively). Median hospital and intensive care stays were similar between both groups (2 [1–4] vs. 2 [1–5] days, p = 0.36, and 12 [8–17] vs. 12.5 [9–21] days, p = 0.38).
CONCLUSIONS: In our experience, endoscopic minimally invasive multiple valve surgeries through right anterior mini-thoracotomy is as feasible, safe, and effective as medial ster-notomy in select patients.
1.5.10. Surgical Valve Thrombectomy in Mechanical Valve Thrombosis: A Series About 21 Cases
Sami Bouchenafa, Ahmed Zaki Boukli Hacene, Boukri Hamouda, Redha Djilali Sayah, Tarek Hamdi, Mohammed Ould Abderrahmane, Makhlouf Amir, Abdelkader Boukhors, Mohammed Bensaber, Nour El Houda Draou, Linda Zebirate and Mohammed Atbi
Departement of Cardiac Surgery, EHU Hospital, Oran, Algeria
BACKGROUND AND AIM: Mechanical valve thrombosis (MVT) is a severe complication of heart valve replacement. In this study we presented our surgical experience of valve thrombectomy for thrombosed mechanical valves
METHOD: Between October 2010 to January 2022, 59 patients were operated for mechanical valve thrombosis. Only patients who underwent surgical valve thrombectomy were studied. Preoperative, operative and postoperative data were collected and analyzed.
RESULTS: Among these 59 patients with mechanical valve thrombosis, 21 (34.4%) patients had surgical valve thrombectomy. In this study 18 patients (85.7%) were women. The mean age was 36.3 ± 11.7 years. The site of thrombosis was the mitral valve in all patients. The most common clinical sign was dyspnea III-IV 19 patients (90.5%). The interval between the first replacement and thrombosis was 37.6 ± 18.4 months. INR < 2 in 17 patients (81%). The mean CPB and cross-clamp time were 57.6 ± 29.8 and 33.1 ± 18.4 min respectively. The mean of mechanical ventilation was 6.5 ± 1.3 h. Mean ICU stay of patients was 1.5 ± 0.5 day and mean hospital stay of patients was 12.1 ± 3.4 days. Early mortality (30 days) was 01 death (4.8%).
CONCLUSIONS: Valve thrombosis is a serious complication. Early diagnosis and urgent surgery give good results. Surgical valve thrombectomy with re-establishment of valve motion is an effective alternative when the thrombus is fresh and early. Effective anticoagulation is the best means of prevention
1.5.11. The Effect of Preoperative Milrinone Infusion in Mitral Valve Surgery
Wajiha Arshad, Musfireh Siddiqeh, Muhammad Azam, Alifa Sabir and Sahab Ahmad
Department of Cardiac Surgery, Rawalpindi Institute of Cardiology, Rawalpindi, Pakistan
BACKGROUND AND AIM: Milrinone is a type III phosphodiesterase inhibitor that increases intracellular concentration of cyclic adenosine monophosphate (cAMP) in the vascular smooth muscle cell and cardiomyocyte. The effects of intravenous milrinone include pulmonary vasodilatation, systemic vasodilatation and produce positive inotropic effects by slowing the hydrolysis of cyclic adenosine monophosphate in the myocardium.
The aim of this study is to determine the effects of IV milrinone infusion in the terms of post operative arrhythmias, right heart failure and duration of ICU stay.
METHOD: This is a single centre retrospective observational study of the 61 consecutive patients operated for Mitral valve surgery either due to mitral regurgitation or mitral stenosis at Rawalpindi Institute of Cardiology from 2022–2023. IV milrinone infusion was started at least 12 h before the surgery and its effects were observed post operatively.
RESULTS: A total of consecutive 61 patients were added in this study, among them 29 (47.54%) were females and 32 (52.45%) were male. 35 patients (57.377%) underwent isolated Mitral Valve surgery and remaining 26 (42.622%) underwent combined procedure including mitral valve surgery and other cardiac procedure. Mean age of the patient was 39.18. Total of 08 patients (13.11%) experienced arrhythmias. Mean hours of ICU stay were 88.114. Only 01 patient (1.63%) died of right heart failure.
CONCLUSIONS: Milrinone provides adequate cardiac performance, causing a greater reduction in post operative arrhythmias, inotropic support, and right heart failure.
1.5.12. Thromboaspiration of a Left-Sided Bioprosthesis Valve Thrombosis by a Mini-Invasive Access: The Lausanne Novel Procedure—A Safer Pioneering Procedure to Alleviate the Risks of Redo Surgery, Thrombolysis and AngioVac-System
Ziyad Gunga, Eric Eeckhout and Matthias Kirsch
Cardiac Surgery Department, Lausanne University Hospital (CHUV), Switzerland
INTRODUCTION: Left-sided bioprosthetic valve thrombosis is considered a relatively rare but life-threatening clinical entity. Is conventional redo on-pump surgery the only way to remove a thrombus resistant to well-conducted anticoagulant? We present a novel procedure via a minimally invasive access to treat such a pathology.
MATERIAL AND METHODS: Case Presentation: A 54-year old male patient underwent mitral valve replacement with a 33-mm bioprosthesis (BP) The post-operative follow-up at 2 months highlighted a motile mass pedunculated to the bioprosthesis. The patient was asymptomatic. A broad spectrum empiric antibiotherapy was initiated for 3 weeks conjointly with a therapeutic-dose anticoagulation with heparin. The echocardiographic control showed no alteration in size after 3 weeks. Because of its bulky nature (18 × 11 mm), hypermobility, resistance to anticoagulation and the neurological threat, we were urged to devise a way to remove the thrombus via a minimally invasive access, as per the patient’s desire.
RESULTS: Patient is placed supine with an intubation by a double lumen tube. A cerebral protection system, Sentinel®, is used to protect against embolic material. A 3.5 cm transverse incision was made, and the intercostal space opened. Two apical concentric pursestring sutures were realized. The apex was punctured with a needle and a soft guidewire was inserted antegrade. A 14 Fr Occlutech delivery set System with an adjustable tip was inserted with its dilatator. The proximal part of the Occlutech® was connected to a pediatric extracorporeal circuit and the aspirated blood, filtered and returned back via the left femoral vein. The patient was discharged at day 3. The echocardiography after 1 year did not show any relapse.
CONCLUSIONS: Thromboaspiration of a left sided valve thrombosis via a trans-apical mini-invasive approach can be an excellent alternative for patients who are reluctant to surgery or for a thrombus resistant to anticoagulation.
1.5.13. Transaxillary Mitral Valve Repair and Atrial Septal Deffect Closure
Allaa Subhi Abdel Majeed and Yad Nuaman Othman
Sulaimaniyah Cardiac Hospital, Sulaimaniyah, Iraq
Iraqi Cardiothoracic Society, Kurdistan Cardiothoracic Society, Baghdad, Iraq
Mitral valve disease is no longer an irreparable condition with the advancement in surgical techniques in the last decades.
Minimal invasive cardiac surgery along with mitral valve repair has become a popular option in advanced centers especially for young females who fit the intervention criteria.
This 38 year old single unmarried female patient referred to our department with severe mitral regurgitation associated with exertional dyspnea.
After discussion of management plan the decision were made to go through minimal invasive approach.
Through right transaxillary vertical 5 cm incision and femoral cardiopulmonary bypass we found incidentally an atrial septal defect.
Through left atrial approach direct vision mitral valve repair and ASD secundum closure done.
In post-operative follow up sessions patient symptoms get relieved and get back to her normal lifestyle.
In conclusion young age patients with such a crippling conditions demand us to choose safest and less invasive intervention if possible.
Such procedures considered as one of the favorable options for females in reproductive age, therefore we try to offer it for a wide variety of our patients.
Though studies showed excellent satisfaction amongst patients, nevertheless; such techniques requires experience, training and specific instruments which makes it challenging in developing countries.
1.5.14. Removal of Giant Myxoma in the Right Atrium with Mini Thoracotomy and Repair of the Tricuspid Heart Valve in a Young Male Patient
Emre Dogan and Ergun Demirsoy
Kolan International Hospital Sisli İstanbul, Istanbul, Türkiye
A 23-year-old male patient applied with complaints of shortness of breath and a mass was observed in the right atrium on echocardiography taken by the cardiologist. The patient, whose transesophageal echo was compatible with a solid myxoma with a diameter of 4.2 × 3.8 cm in the right atrium, was operated on by us.
The surgery was performed under general anesthesia with double endotracheal intubation. The patient was positioned so that the left lung was ventilated. The surgical incision was in the form of a mini-thoracotomy approximately 5 cm from the 4th intercostal space to the right anterolateral. Cardiopulmonary bypass was performed using the right femoral artery and right femoral vein. A cross clamp was placed and cardiac arrest was achieved using Del-Nido cardioplegia. Right atriotomy was performed.
A giant 6 × 4 × 3 cm mass attached to the right lateral wall of the right atrium was excised. After the mass was removed, annuloplasty was performed on the severely dilated tricuspid heart valve annulus with a 34 mm Medtronic Contour ring. The right atrium was closed and the pump was disconnected. A drain was placed in the right pleural space. The patient was taken to the intensive care unit. He was extubated at the 5th postoperative hour. He was taken to the ward the next day and discharged 4 days later.
1.5.15. Development of a New Access Port for Apical-Mitral Neo Chords Implantation in Mitral Valve Prolapse
Aleksandr Nemkov 1, Gennady Khubulava 1, Kirill Shokin 2, Sergey Romanov 2, Vladimir Komok 1, Nikolay Bunenkov 1, Nikita Titov 1, Vladimir Matrosov 1, Nikita Tarskiy 1, Aleksandr Morozov 1 and Vladimir Ershov 1
- 1
I.P.Pavlov First St-Petersburg State Medical University, St Petersburg, Russia
- 2
Nevsky Technologies, St Petersburg, Russia
BACKGROUND AND AIM: Little is known about the technology of implantation of multiple apical-mitral neochords in mitral valve prolapsed. The formation of two or more pairs of neochord requires a unified access port that allows multiple insertion of instruments into the left ventricle with the greatest safety and accuracy
METHOD: An introducer for multiple access to the left ventricle has recently been developed. The introducer has several working channels. A separate channel of the introducer is made for feeding a needle containing a PTFE thread. There may be two or more such channels. They are focused on certain parts of the mitral valve leaflets. The channel for extracting threads by an intravascular loop has a groove for collecting PTFE threads in it. The groove ensures that PTFE chords are laid in a certain order to prevent the formation of knots and their crossection.
RESULTS: The experiments were performed on synthetic mitral valve models and on 10 pig hearts. The introduction of a multichannel introducer was carried out between the bases of the papillary muscles on the anterolateral wall of the left ventricle. A j-shaped guide was used for safe insertion. The distal part of the introducer should be located above the level of coaptation of the mitral valve leaflets in the regurgitation jet zone (vena contracta space). This makes it possible to repeatedly insert a feeding instrument—a needle and a receiving instrument—a catheter with an intravascular loop into the area of interest. The fixation of the chords to the PTFE support plates is carried out as the final stage of the operation.
CONCLUSIONS: The use of a multichannel introducer makes it possible to create multiple apical-mitral neochords in mitral valve prolapse more accurately, easier and more reliably.
Working out the details of implantation is required in a hybrid (X-ray and ultrasound) operating room.
1.5.16. Cardiac Bioprosthesis: Complications and Medium-Term Follow-Up
Mouna Bousnina, Khedija Soumer, Azabou Nadia, Amenallah Zarrouk, Rihab Arbi, Salma Nciri and Amine Jemel
Department of Cardiovascular Surgery, Abderrahmen Mami Hospital, Ariana, Tunisia
BACKGROUND AND AIM: The heart valve bioprosthesis would be an interesting alternative to reduce the risk of hemorrhage and thromboembolism. The aim of this study was to determine the complications linked to bioprosthesis implantation in the medium term and to evaluate survival.
METHOD: Between 2018 and 2022, a retrospective study in the cardiovascular surgery department of the Abderrahmane Mami hospital in Ariana. We collected the files of successive patients operated for valve replacement(s) by bioprosthesis with or without associated procedure. All patients were checked for survival and for functional discomfort. We also collected postoperative ultrasound checks.
RESULTS: We included 69 patients. The average age was 65.1 year ± 12.3; sex ratio was 1.15. The late mortality rate was 17.39%. The average survival was 24.15 ± 5.26 months with a range from 1 month to 47 months. The overall survival rate was 85.9% ± 7.6% at 6 months, 66.8% ± 13.3% at 1 year, 44.5% ± 15.6% at 2 years and 33.4% ± 15.2% for the remainder of the follow-up period. As for the postoperative echocardiographic data, the average left ventricular ejection fraction was 61% ± 6.508%, the average maximal velocity was 2.17 ± 0.63 mmHg. The main predictors of late mortality were postoperative atrial fibrillation (OR = 2.3), postoperative left ventricular failure (OR = 7), and elevated preoperative pulmonary hypertension (OR = 1.8).
CONCLUSIONS: Bioprostheses seem to have good results in the medium term. Morbimortality is essentially linked to the host.
1.5.17. Redo Mitral Valve Replacement Using Mitris Resilia Valve in Patient Having Redo Mitral Surgery and Tricuspid Valve Repair
Aneel Zaheer, Mark Ward, Mayooran Nithianathan and Ranjeet Deshpande
Kings College Hospital London, London, UK
BACKGROUND: The MITRIS RESILIA mitral valve was commercially introduced in April 2021. It is the successor of the Carpentier Edwards Perimount MAGNA MITRAL EASE valve but the bovine pericardial tissue of this bioprosthesis, the RESILIA tissue, is treated with a special integrity preservation technology and offers enhancement of anti-calcification treatment that will potentially increase the durability
CASE: We report a case of 42 years old patient who had redo Mitral valve replacement and tricuspid valve repair with history ofmitral valve repair in 2006 via right thoracotomy approach. She presented with increasing shortness of breath on exertion and palpitations. Her echocardiogram showed severe mitral stenosis and moderate to severe tricuspid regurgitation. In view of stable symptoms her operation was delayed for three months until Mitris valve was available in the UK considering her young age and to avoid long term warfarin.
We used sternotomy approach and trans septal approach. Previous mitral annulopasty ring was explanted and anterior mitral leaflet was excised. 2 CV4 goretex sutures were used to resuspend the Left ventricle and mitral valve was replaced using size 27 Mitris resilia valve. Tricuspid valve was repaired using size 32 physio 2 ring. Aortic cross clamping time was 97 min and patient was weaned off CPB DDD paced. In the postoperative period she required PPM for heart block. Postoperative echocardiogram showed well seated mitral valve with no paravalvular leak and gradient of 2.7 mm Hg.
To our knowledge this is the first case report of Mitris valve implantation in redo mitral surgery with tricuspid valve repair.
1.6. CARDIAC » Bypass Grafts and Configurations
1.6.1. Herbal Hemostatic Agent in Open Heart Surgery Investigation of Clinical Efficacy and Safety of Algan Product
Sefer Usta, Ömer Melih Cinemre, Kemal Uzun and Mine Demirbaş
SBU Trabzon Ahi Evren GKDC Education Hospital, Trabzon, Turkey
BACKGROUND AND AIM: Stopping bleeding that occurs during surgical operations or other emergencies is very important to prevent negative consequences by reducing blood loss. This study aims to investigate the clinical effectiveness and safety of hemostatic hemostatic agent using polysaccharide-based algan hemostatic agent, which is a herbal product, in open heart surgery.
METHOD: A total of 40 open heart surgery patients, 30 of whom underwent coronary surgery and 10 of whom underwent valve replacement surgery, were included in the study. A control group of 40 people was determined for the same surgical indications, in which only traditional haemostatic methods were used. Algan hemostatic agent was used as a support in coronary anastomoses, aortotomy incisions, perivascular fat tissue in the myocardium, and atriotomy incisions in patients undergoing mitral valve surgery.
RESULTS: On the first postoperative day, drainage (average 450 mL/1000 mL) was found to be higher in the control group. An important difference was found to be statistically significant in the treatment group in terms of the rate of erythrocyte suspension use. It was observed that algan hemostatic agent can be used safely and effectively as a hemostatic agent in open heart surgery.
CONCLUSIONS: As a result, the use of AHA reduces blood loss by reducing postoperative drainage. It causes less blood usage in the postoperative period in open heart surgery operations. AHA, a topical hemostatic agent, was found to be more effective in controlling bleeding than traditional methods. Since it is a herbal product, no side effects were observed. In some studies, the haemostatic potential of microporous polysaccharide-based tissue adhesives has been found to be effective. In addition to underlining that Algan hemostatic agent is an effective haemostatic agent, there is a need for comparative studies among haemostatic agents in terms of their effectiveness, which is an important auxiliary argument in open heart surgery.
1.6.2. The Impact of Prior Asymptomatic COVID-19 Infection on Outcomes Following Coronary Bypass Surgery
- 1
Department of Cardiovascular Surgery, Kilis Alaeddin Yavaşca Devlet Hastanesi, Kilis, Turkey
- 2
Department of Cardiovascular Surgery, Ankara City Hospital, Ankara, Turkey
BACKGROUND AND AIM: The COVID-19 pandemic has notably impacted cardiac surgery, particularly coronary bypass grafting (CABG). Past studies on the postoperative outcomes of cardiac surgeries during the pandemic are limited and not comprehensive for patients with initially asymptomatic COVID-19 infections. Our study aims to fill this gap by evaluating the postoperative outcomes for CABG patients who had asymptomatic COVID-19 infection.
METHOD: We retrospectively analyzed 37 asymptomatic COVID-19 patients and 39 non-COVID patients who underwent CABG at the Health Sciences University Ankara City Hospital Cardiovascular Surgery Clinic from 2021 to 2022.
RESULTS: The average age of the 76 patients was 63.4 years, with a gender distribution of 18.4% female and 81.6% male. The predominant symptom across both groups was exertional angina, observed in 63.7% of cases. In comparing intraoperative and postoperative variables—such as ventilation wean-off times, complication rates, inflammatory marker levels, use of non-invasive ventilation, and oxygen therapy requirements—no significant differences were noted between COVID and non-COVID groups. However, the preoperative phase showed significant differences in inflammatory markers and blood gas values (PaO2 and PaCO2).
While postoperative mortality was noted in one patient within the COVID group, this did not represent a statistically significant finding. The COVID group exhibited a higher, statistically significant rate of postoperative complications after a four-week period. In our analysis period, no mortality or morbidity associations were shown in connection with previous asymptomatic COVID infections. Interestingly, early post-infection CABG did not yield different outcomes than surgeries performed after a delay, challenging typical waiting period guidelines.
CONCLUSIONS: Our findings suggest that an asymptomatic COVID history may not necessitate delayed CABG. Nevertheless, this study’s limitations—like the small sample size and absence of long-term follow-up—indicate a need for further research. Future studies should involve larger patient cohorts, inclusive of vaccination status, and extend follow-up periods to validate these preliminary outcomes.
1.6.3. Coronary Artery Bypass Grafting Using 3D-Visualization
Dmitrii Vladislavovich Petrovskii, Vladislav Petrovich Vasiliev, Andrey Andreevich Shiryaev, Ruslan Sergeevich Latypov, Damir Mazitovich Galyautdinov, Elina Yevgenievna Vlasova, Alexandr Vladimirovich Emelyanov and Renat Suleymanovich Akchurin
Cardiosurgery Department, FSBI “NMRCC named after Academician E.I. Chazov” of MH of RF, Moscow, Russia
BACKGROUND AND AIM: Among candidates for CABG, there is an increasing number of patients with difficult coronary lesions. Surgeons are forced to use complex techniques for forming a coronary anastomosis which requires optical magnification. Aim of this study is approving using 3D-exoscope during microsurgical stage of CABG.
METHOD: 39 patients (65% males, mean age 64.1 ± 8.0 years) who underwent CABG using 3D-exoscope during 01.2021–02.2024. The diameters of CA were measured intraoperatively. We analyzed perioperative and hospital outcomes.
RESULTS: Operation time was 269.4 ± 48.7 min, cardiopulmonary bypass took 98.3 ± 24 min, myocardial ischemia last 70.8 ± 17.9 min; this coincided with standard CABG using an operating microscope in our department. Totally 132 distal anastomoses were formed, the median revascularization index was 4 [3, 4]. In 21 cases (15.9%) the anastomosis were performed by shuntoplasty, in 14 of them (10.6%) with coronary endarterectomy. The diameter of all 132 bypassed CA in the area of anastomosis was measured: 7 (5.3%) < 1 mm, 46 (34.8%)—1–1.5 mm, 75 (56.8%)—1.5–2.0 mm, 4 (3.0%)—>2.0 mm. Mortality, perioperative infarction, life-threatening arrhythmias, and angina were not recorded during the hospital period. The postoperative hospital stay was standard 8.7 ± 1.9 days. Our experience: 3D exoscope for CABG requires the same skills as a microscope. 3D exoscope has a advantages: image quality and possibility of magnification result in good visualization, and also make it easier to perform complex methods of revascularization; since the image is visible from any position, the movements of the surgeon’s head and neck become freer, which reduces the load on neck and shoulders.
CONCLUSIONS: For visualization during CABG 3D-exoscope is effective and safe when working with both standard and problematic distal beds. Hospital results of such operations are good. Due to ease of use, high resolution and quality of the image, a 3D-exoscope is comfortable for CABG.
1.6.4. Multiple Arterial Grafting During Coronary Artery Bypass Graft Surgery in Diabetic and Non-Diabetic Patients: A Short- and Long-Term Analysis at a Single Center
Miralem Jasarevic, Oscar Oscar Krueger, Jan Strathmann, Ilir Balaj, Sharaf Eldin Shehada, Jarowit Piotrowski, Parwis Massoudy, Heinz Jakob, Markus Kamler and Matthias Thielmann
Department of Thoracic and Cardiovascular Surgery, West-German Heart Center, University of Duisburg-Essen, Essen, Germany
BACKGROUND AND AIM: Coronary artery bypass surgery (CABG) with multiple arterial grafting (MAG) has been shown to improve patient survival compared to single arterial bypass grafting. Whether these survival benefits also exists in diabetic patients is uncertain. We therefore aimed to compare short and longterm outcomes of MAG in diabetic versus non-diabetic patients.
METHOD: In this retrospective study, we investigated short- and long-term clinical outcomes of diabetic (n = 256) and non-diabetic (n = 800) patients who consecutively underwent CABG with MAG between January 1999 and December 2019 at our institution.
RESULTS: Diabetic patients had a significantly higher EuroScore II (1.4 vs. 0.9; p < 0.0001) and underwent significantly less bilateral internal thoracic artery (BITA) grafting (52% vs. 67.8%; p < 0.0001) compared to non-diabetic patients. The incidence of postoperative adverse events such as pneumonia, stroke, and sepsis did not differ between the two groups. However, diabetics had a significantly higher incidence of low cardiac output syndrome, cardiac resuscitation, renal failure requiring dialysis, and sternal wound infections during the entire follow-up period. Non-diabetics had a significantly higher median survival time of 19.6 years compared to 14.5 years in diabetic patients (p < 0.0001).
CONCLUSIONS: Our data show a significantly lower median overall survival in diabetics with MAG. This emphasises the importance of diabetes as a risk factor in the choice of individual surgical strategies, such as multiple or single arterial grafting in these patients.
1.6.5. The Effects of Carbon Dioxide Insufflation for Radial Artery Harvesting
Melïke Elïf Teker Açikel, Begüm Özüekren Kasapoğlu, Yasin Saraç, Tolga Demir and Ismail Koramaz
Cardıvascular Surgery of Şişli Hamidiye Etfal Eğitim ve Araştırma Hastanesi, Istanbul, Turkey
BACKGROUND AND AIM: The aim of coronary artery bypass operations is complete revascularization. Several reports have described use of arterial (radial artery, internal mammary artery etc) and vein grafts (venasaphana magna, brachiocephalic vein etc) in coronary artery bypass surgery. Many reports have shown the advantage of using the technique during radial artery harvesting. Carbon dioxide is a agent directly vasodilatator effect. It is shown that carbondioxideinsufflation of internal thoracic artery is an efficient technique to increase the flow and prevent thepossible vasospasm of the internal thorasic surgery segments. In the pesent study, we investigated the effects of carbon dioxide insufflation during radial artery harvesting.
METHOD: This study was performed on human radial artery segments from patients (n = 24) undergoing coronary artery bypass grafting. Radial artery harvesting was performed by the same surgeon for standardization of technique. Patients were randomly divided into two groups for radial artery harvesting.
In the first group, radial arteries were harvested by means of a carbon dioxide insufflation (n = 12). In the second group, radial arteries were harvested by means of a classical harvesting (n = 12) Patients with diabetes mellitus were excluded from the study in both groups.
RESULTS: There was no significant difference in the demographic findings of the patients. There was no significant difference in both groups in terms of EF, cross time, and pump time. There was no significant difference in terms of hospital stay, mortality and morbidity in both groups. The patency rate of the group whose radial arteries were harvested via carbon dioxide insufflation was more significant than the group whose radial arteries were removed normally.
CONCLUSIONS: The patency of the grafts used in coronary artery bypass surgery is of vital importance. One of the grafts used for this purpose is the radial artery. Radial artery removal with carbon dioxide can provide long-term patency with less damage without touching the radial artery.
1.6.6. Combined Valve and Coronary Surgery: A Series of 35 Cases
Sami Bouchenafa, Ahmed Zaki Boukli Hacene, Boukri Hamouda, Redha Djilali Sayah, Tarek Hamdi, Mohammed Ould Abderrahmane, Makhlouf Amir, Abdelkader Boukhors, Mohammed Bensaber, Nour El Houda Draou, Linda Zebirate and Mohammed Atbi
Departement of Cardiac Surgery, EHU Hospital, Oran, Algeria
BACKGROUND AND AIM: Recently, we observe that many of our patients who have valve disease requiring for surgery are associated with severe coronary stenosis. Our study describes the morbidity and mortality of this population of patients after combined valve and coronary surgery
METHOD: A retrospective study on 35 patients who underwent valve surgery combined with coronary artery bypass grafting (CABG) between January 2022 and February 2024 in EHU hospital of Oran. We included surgery of mitral or aortic valve and both with coronary grafting surgery. Clinical data, preoperative evaluations, intraoperative results and postoperative follow-ups were analyzed
RESULTS: In this study 26 patients (74.3%) were men. The mean age was 61.7 ± 12.8 years. Clinically, dyspnea in 20 patients (71%) and angina in 19 patients (68%). The valve disease was aortic valve in 22 cases (79%), mitral in 11 cases (39%) and both in 5 cases (14%). The coronary arteries most affected were the anterior interventricular in 21 cases (60%) and the right coronary in 12 cases (34.3%), the circumflex artery in 7 cases (20%) and the common trunk left in 4 cases (11.4%). In total, 19 aortic valve replacements and CABG (54.3%), 11 mitral valve replacements and CABG (31.4%), 4 double mitral-aortic valve replacement and CABG (11.4%). A single CABG was in 26 patients (74.3%), a double CABG in 8 patients (22.8%) and a triple CABG in one patient (2.8%). The average time of cardiopulmonary bypass was 173.3 + 23.2 min and the aortic clamping was 140.7 + 18.6 min. We describe some complications, as ventricular dysfunction in 11 patients (31%) arrhythmias in 4 patients (11.4%). There was a mortality of 6 patients (17.14%).
CONCLUSIONS: The morbidity and mortality rate of patients from valve surgical procedures combining coronary artery bypass grafting is high, explained by operative risk factors represented by cardiac dysfunction and electrical disorders
1.6.7. Bilateral Skeletonized IMAs Used as “In Situ” Grafts for Different Coronary Territories: Long-Term Propensity Matching Study
Živojin Jonjev 1, Ilija Bjeljac 1, Aleksandar M. Milosavljevic 1, Mirko Todic 1, Strahinja Mrvic 1 and Novica Kalinic 2
- 1
Institute for Cardiovascular Diseases of Vojvodina, Clinic of Cardiovascular Surgery, Sremska Kamenica, Serbia
- 2
Faculty of Medicine, University of Banja Luka, Banja Luka, Republic of Srpska, Bosnia & Herzegovina
INTRODUCTION: Bilateral internal mammary arteries (BIMAs) have been recognized as the most advanced surgical option for coronary artery bypass grafting (CABG). The aim of this study is to compare outcomes in propensity score matched (PSM) patients with skeletonized BIMAs used as in-situ grafts for different coronary territories with patients using single internal mammary artery (SIMA) in CABG.
METHODS: In 2013–2023, 7543 patients underwent primary CABG for multivessel coronary artery disease at our institution. In 283 (3.75%) patients BIMAs in situ grafting were performed. Right IMA was used to revascularize right coronary artery, and left IMA for the LAD territory. BIMA patients (n = 280) were compared with single IMA patients (n = 280) in propensity score matching analysis. Primary outcome measures were identified as all-cause mortality at 30-days, 5 years and 10 years, while secondary outcome measures were length of hospital stay, the incidence of postoperative major adverse cardiovascular and cerebrovascular events (MACCE), sternal wound infection and need for subsequent percutaneous revascularization.
RESULTS: There was no immediate posteoperative mortality (30 days) in both groups. There was no perioperative MACCE or deep sternal wound infection as well. Patient in both groups had similar length of hospital stay (BIMA = 7.8 ± 1.5 days vs. SIMA = 8.2 ± 1.4 days; p < 0.05). Mean follow-up was 9.78 ± 0.62 years with freedom from death 86.07 ± 3.0% in BIMA group vs. 78.6± 4.1% in SIMA group 10 years after surgery (p < 0.05).
CONCLUSIONS: The results of the study indicated that BIMAs as in situ grafts used for different coronary territories in CABG is associated with better long term survival then SIMA grafting. IMA harvesting with skeletonized technique provides better IMA length, detailed graft visualization, and minimal trauma to the chest wall. Our conclusion is independent of traditionally accepted risk factors incorporated in the Logistic EuroSCORE II and SYNTAX score II and is exclusively method related.
1.7. CARDIAC » Challenging Cases
1.7.1. Surgery for Infective Endocarditis Using Beating Heart Technique via Right Anterior Mini-Thoracotomy in Intravenous Drug Users
Mete Kubilay Kasap, Nazenin Kasapoğlu, Özgür Çoan, Aylin Arus Zeytun, Akif Küçük, Ergün Kürkçü, Kaanhan Kızıltoprak, Funda Tor Ocak and Muhammed Bozgüney
Health Science University Adana City Research and Training Hospital, Adana, Turkey
BACKGROUND AND AIM: Infective endocarditic (IE) in drug inject adults has a high mortality rate. However, there is no investigation to evaluate the effects of beating heart technique on patients’ outcomes. Our aim of this study was to analyze the early and mid-term clinical outcomes of patients who undergoing beating heart technique via right anterior mini-thoracotomy.
METHOD: We operated 170 IE patients due to intravenous drug use (IVDU) between 2009 and 2023. While an isolated mitral valve (MV) (n = 44; 25.8%), and tricuspid valve (TV) (n = 67; 39.4%) IE identified in 111 patients (65.2%), we detected TV concomitant with MV IE in 59 patients (28%). Mean age was 46.6 ± 4.2 years (18–66 year). To verify liver congestion and pulmonary embolic events, abdominal ultrasonography, and full body computed tomography were performed preoperatively. We performed valve repair using pericardium and artificial chordae implantation in suitable patients (n = 64). In the remaining 116 patients, valve replacement/replacement concomitant with repair were performed via right anterior mini-thoracotomy incision without the use aortic cross clamp.
RESULTS: Causative microorganisms were Methicillin resistance Staphylococcus aureus (MRSA), and Enterococcus predominantly. Seven patients (4.1%) died after surgery. The median length of ICU staying time was significantly longer in patients with pulmonary or cerebral embolic events and serious heart failure (2.3 days vs. 6 days) (p = 0.001). The median hospital staying time was 39.8 days (28.9–53.4 days). Acute kidney failure requires temporary hemodialysis developed after surgery in 5 patients (6.6%). The median follow-up was 56.4 months (min.:42 max.:64 months). Recurrence of IE requiring redo surgery was seen in 22 patients during follow-up period. Survival at 1, 3, and 5 years were 93%, 86%, and 79%.
CONCLUSIONS: Mortality predictors such as age, embolic events have been showed in previous publications. However, the effects of surgical approach on mortality have not been evaluated yet. Early surgery may provide good clinical outcomes in IVDUs with IE. Valvuloplasty may be the first choice using beating heart through mini-thoracotomy incision without an aortic cross-clamping as a feasible method with low mortality rate in suitable IVDUs who have IE.
1.7.2. Coronary Artery Bypass Grafting in Patients with Low Ejection Fraction
Ahson Memon, Kanwar Talha Shahid, Malik Shafqat Hassan and Syed Shahzad Hussain Rizvi
Department of Cardiothoracic Surgery, Tabba Heart Institute, Karachi, Pakistan
BACKGROUND AND AIM: Patients with low ejection fraction undergoing isolated coronary artery bypass graft (CABG) surgery are at a higher risk for postoperative complications and mortality. This study was conducted to evaluate the impact of ejection fraction on the outcome of isolated CABG.
METHOD: We analyzed patients from our database who underwent isolated CABG between 2019 to 2024. Patients were divided into three groups based on their pre-operative Ejection Fraction (EF). Group-I included patients with EF > 50% [Normal EF], Group-II included patients with EF 35–50% [Mild to Moderately Reduced EF], and Group 3 included patients with EF < 35% [Severely Reduced EF].
RESULTS: The mean age of Group-I was 57.99 +/− 8.791, Group-II was 58.15 +/− 8.885 and Group-III was 58.36 +/− 8.976. The male gender was the predominant gender in all three groups: 77.09% in Group-I, 81.4% in Group-II, and 84.38% in Group-III. 20.68% patients in Group-I, 23.26% in Group-II and 16.94% in Group-III had raised creatinine pre operatively (creatinine clearance < 85 mL/min). Hypertension was present in approximately 70% of all our patients. In the per-operative period 0.85% patients in Group-I required an IABP as compared to 5.35% in Group-II and 9.36% in Group-III. The EuroScore II-predicted mortality was 1.21% in Group-I, 1.92% in Group-II, and 4.35% in Group-III. Post-operative observed mortality rates were 1.21% in Group-I, 2.29% in Group-II and 4.93% in low EF group (Group-III).
CONCLUSIONS: The results clearly indicate that worsening pre-operative ejection fraction is associated with a higher mortality post-operatively in patients undergoing isolated CABG. In addition, use of IABP increases as pre-operative EF decreases.
1.7.3. Midterm Outcome of Isolated Surgical Revascularization in Patients with ≤20% Left Ventricular Function
Kanwar Talha Shahid, Ahson Memon, Malik Shafqat Hassan and Syed Shahzad Hussain Rizvi
Department of Cardiothoracic Surgery, Tabba Heart Institute, Karachi, Pakistan
BACKGROUND AND AIM: To find out long-term Success, quality of life by assessing functional and angina improvement after isolated coronary artery bypass grafting in patients with very poor left ventricular function.
METHOD: Coronary artery bypass graft surgery (CABG) in these patients is associated with improved survival compared with medical treatment. In times gone by, surgical revascularization in patients with poor left ventricular function has been associated with high perioperative as well as postoperative mortality. Prophylactic use of intra-aortic balloon pump (IABP), new cardioplegic solutions, shorter cross clamp and cardiopulmonary bypass times, improvement on intensive postoperative care have show the way to superior outcomes, allowing surgical revascularization to be a quite safe course of action at present in selected patients at high risk.
RESULTS: Consecutive 156 patients who came to Tabba Heart Institute with Left ventricular EF ≤ 20% measured (by echocardiography) before surgery and who had isolated CABG between December 2021 and December 2023 were eligible. Data was recovered in prospect from the patients and/or their relatives through telephonic communication and congestive heart failure class were rated using classification of New York Heart Association. Symptomatic relief was assessed by Canadian Cardiovascular Society class of angina.
CONCLUSIONS: We conclude that admirable midterm results and better quality of life can be expected in these patients with very severe ischemic left ventricular dysfunction and these results highly depend upon completeness of surgical revascularization and an excellent post-operative care.
1.7.4. Reintervention for Aortic Prosthesis Acute Endocarditis: Early and Mid-Term Outcomes
Michele D’alonzo, Antonio Fiore, Yuthiline Hun Chabry, Eric Bergoend, Costin Radu, Maria Antonietta Piscitelli, Amin Serradj, Victor Lesanu, Tahar Hadj Idris, Guner Emirali and Thierry Folliguet
Department of Cardiac Surgery, Hôpital Henri Mondor, Assistance Publique-Hôpitaux de Paris, Creteil, France
BACKGROUND AND AIM: While transcatheter aortic valve implantation is growing his utilization for degenerative bioprostheses failure, valve-in-valve procedures are limited in acute aortic endocarditis circumstances. Surgical interventions for aortic prosthesis endocarditis pose significant risks, with documented high mortality rates in existing literature. This study analyses surgical redo cases involving the aortic valve, seeking to provide insights into outcomes and challenges of this complex scenario.
METHOD: This was a retrospective, monocentric, observational study. Fifty-four patients underwent surgical reoperation after aortic valve replacement due to acute infective endocarditis from 2016 to 2023. The endpoints were early and late mortality, incidence of complications and major adverse cardiac and cerebrovascular events (MACCE, defined as death, disabling stroke, re-endocarditis, permanent pacemaker implantation, and myocardial infarction).
RESULTS: The study cohort consisted of individuals with an average age of 71.9 ± 12.1 years, predominantly male (79.6%), and with a mean EuroSCORE II of 15%. Mean follow-up was 741 days. Vegetations larger than 10 mm were present in 29 patients (53.7%) while an annular abscess was present in 31 (57.4%). The mean cardiopulmonary bypass time was 207.7 ± 109.6 min while aortic cross-clamping time was 150.5 ± 68.5 min. Thirty-day mortality remained notably high (10 patients, 18.5%). Postoperative ECMO was used in 5 patients (9.3%). The five-year overall survival rate was 58.3 ± 18.6%, while the freedom from MACCEs was 41.7 ± 19.7%. During the follow-up three patients required surgical reintervention (1 for re-endocarditis).
CONCLUSIONS: Despite advancements in surgical management and perioperative care, our study confirmed that the operative risk associated with redo procedures following aortic valve replacement for infective endocarditis is high. The mortality rate within 30 days underscores the gravity of this condition and the challenges encountered during surgical management, nevertheless the 5-year survival rate suggests an acceptable outcome.
1.7.5. Analysis of Early Outcomes of Surgical Repair of Post MI Ventricular Septal Rupture and Associated Risk Factors
Alifa Sabir, Muhammad Sohail Chaudhri, Muhammad Azam and Sahab Ahmad
Rawalpindi Institute of Cardiology, Rawalpindi, Pakistan
BACKGROUND AND AIM: The incidence of post MI VSR has reduced to 0.2% with increase in revascularization therapies. However, the clinical outcomes are still very poor following medical or surgical management of VSR. Mortality rates are reported to be higher than 30% in cases of operative management and are associated with timing of surgery since diagnosis.
METHOD: This is a single center retrospective analysis of all the patients operated for ventricular septal rupture at Rawalpindi Institute of Cardiology from 2019–2023. A total of 19 patients data was retrieved from Database System of Cardio thoracic Surgery and analyzed using SPSS 23. Patients were divided into two groups as survivors and non-survivors on the basis of the outcome, i.e., mortality within 30 days (
Table 4).
RESULTS: The operative mortality in this series was 31.4%, which is comparable to the reported mortality. Male patients were 73.7% and female patients were 26.3%. Mean age of the participants was 56.94 +/− 8.65. Single vessel disease was most prevalent accounting for 47.1% patients. Mean time from the day of presentation to the day of surgery was 5.6 +/− 3.65 days. Six patients were in cardiogenic shock pre-operatively, requiring IABP and ionotropic supports. Pre operative cardiogenic shock was a strong predictor of mortality in our study with incidence of up to 25% in those presenting with shock.
CONCLUSIONS: Despite decrease in incidence, post MI VSR still remains one of the most catastrophic emergencies in cardiac surgery. Factors associated with increased risk of rupture includes male gender, advanced age, SVCAD and lack of collateral circulation. Prompt diagnosis and after load reduction remains the cornerstone of pre operative management. Early surgical repair for patients with hemodynamic instability improves survival.
1.7.6. Antiphospholipid Syndrome and Perioperative Hemostatic Management of Cardiac Valvular and Septal Defect Surgery: A Case Report
Ahson Memon, Kanwar Talha Shahid, Malik Shafqat Hasan, Imran Ali, Yusra Faheem and Tanees Doctor
Tabba Heart Institute, Karachi, Pakistan
BACKGROUND AND AIM: Individuals with Antiphospholipid syndrome (APS) often have heart valve anomalies, however experience with valve replacement in such individuals with a considerably large ASD is limited. We offer a case of a mitral valve replacement and an ASD closure in a patient with this disease at our institute
METHOD: A 29 year old female patient, married, APS + ve, with no other comorbids, presented in the OPD for an elective ASD (Atrial Septal Defect) repair and mitral valve replacement. Her TEE (Transesophageal echocardiography) showed a bileaflet mitral valve prolapse causing severe eccentric mid to late systolic mitral regurgitation with multiple regurgitation jets and systolic flow reversal in left upper and left lower pulmonary veins. Mitral annulus measured 33 mm and a large ASD measuring 48 mm in diameter with predominantly left to right shunt was detected.
RESULTS: She was given clearance for surgery after being reviewed by a multidisciplinary team and successfully operated on, on 23 November 2023, via a median sternotomy, on cardiopulmonary bypass and with an intricately managed anticoagulation process
CONCLUSIONS: This case highlights the special perioperative difficulties that APS patients undergoing on pump cardiac surgery face, especially with regard to ASD management. We have demonstrated, that although rare, such a condition may arise in some patients that have APS and can be, through correct risk assessment and management, treated. The patient provided authorization for the publication and use of radiographic and transesophageal echocardiographic (TEE) images.
1.7.7. Cardiac Hydatid Cyst: About Seven Cases
Sami Bouchenafa, Ahmed Zaki Boukli Hacene, Boukri Hamouda, Redha Djilali Sayah, Tarek Hamdi, Mohammed Ould Abderrahmane, Makhlouf Amir, Abdelkader Boukhors, Mohammed Bensaber, Nour El Houda Draou, Linda Zebirate and Mohammed Atbi
Departement of Cardiac Surgery, EHU Hospital, Oran, Algeria
BACKGROUND AND AIM: Hydatid cyst is a parasitic infection caused by the larvae of Echinococcus granulosus. Usually, localization of a hydatid cyst is the liver, then lungs. Cardiac localization is very rare. The aim of this study is to report the presentation and management of cardiac hydatid cyst in different localizations.
METHOD: A retrospective study, about seven cases, conducted in one center during five years. Each case presented separately regarding presentation, diagnosis and management.
RESULTS: A case series reported seven patients. Four patients (57.1%) were women; three patients (42.9%) were male. The mean age was 43.28 years (from 27 to 63 years old). The revealing symptoms were dyspnea in three cases (42.9%), chest pain in two cases (28.6%), asthenia in one case (14.3%), and one case (14.3%) presented chest pain and syncope. Six cases (85.7%) were diagnosed through transthoracic echocardiography and one (14.3%) patient with CT-scan. In 2 cases (28.6%) the cyst was pericardial; it was myocardial in the left ventricle in 2 cases (28.6%), in 2 others (28.6%) it was pericardial and myocardial, and one case (14.3%) was found in the inter-ventricular septum. Two patients (28.6%) had associated liver hydatid cyst and one (14.3%) had pulmonary hydatid cyst. All patients underwent surgical treatment except one who was treated with only Albendazole.
CONCLUSIONS: Cardiac hydatid cyst is a very rare disease; mainly affecting the left ventricle. The symptomatology is variable. Echocardiography is very useful in diagnosis. Surgery is the main treatment. Medical treatment with Albendazole can aid in improving the overall outcome.
1.7.8. Infective Endocarditis—Nightmares and Dreamscapes: 18 Years Analysis of IBCV Iași Cases
Grigore Tinică, Alberto Bacușcă, Mihail Enache, Silviu Paul Stoleriu and Andrei Țăruș
Department of Cardiovascular Surgery, Cardiovascular Diseases Institute “George I.M. Georgescu”, Grigore T. Popa University of Medicine and Pharmacy, Iasi, Romania
BACKGROUND AND AIM: Recent reports indicate that infectious endocarditis continues to represent a significant global burden, with an incidence of 13.8 cases per 100,000 individuals. Our goal was to highlight data regarding the onset and progression of the disease, specific symptoms, diagnostic methods, and treatment approaches adopted for each person according to age, risk factors, and associated comorbidities.
METHOD: We conducted a single center retrospective study on a cohort of 664 patients with infectious endocarditis from 2004 to 2022. All cases of valve endocarditis, whether acute or chronic, were included in the study. This encompassed prosthetic valve endocarditis cases, except for those involving transcatheter aortic valve implantation.
RESULTS: The average age of the patients was 53.6 years. 8.28% of the patients were under 30 years of age. The onset was acute and severe, with high fever and septic presentation in 37% of patients. 17% showed signs of embolic phenomena upon admission, 19.12% presented with symptoms of global cardiac decompensation, and 8.58% arrived in cardiogenic shock. 54.22% of the patients reported an insidious onset, associated with a delayed hospital presentation. 41.12% of the cases had negative blood cultures. In patients with criteria of severity and indication for urgent treatment, surgery is certainly the only life-saving solution. However, delaying surgery for hemodynamically stable patients, with a good response to antibiotic therapy until the infectious source is cleared, is, from our experience, the optimal treatment strategy. In our cohort, surgical intervention was necessary on an emergency basis for 53.01% of the patients. The overall mortality was 8.5%.
CONCLUSIONS: Infectious endocarditis remains a significant global health concern, with diverse presentations and outcomes. Our study underscores the importance of tailored treatment approaches based on patient characteristics and severity, highlighting the role of surgery in life-saving interventions and emphasizing the need for prompt diagnosis and management to improve patient outcomes.
1.7.9. Twiddler Syndrome
Mohamed Shafi Mahboob Ali
Department of General Surgery, Advanced Medical and Dental Institute (AMDI), Penang, Malaysia
INTRODUCTION: Twiddler’s syndrome is a lethal complication of pacemaker insertion due to deliberate manipulation of the pulse generator by the patients. Continuous reeling of the leads will cause ipsilateral phrenic nerve to be stimulated, disconnection of the leads and thus, dysfunction of the pacemaker.
CASE REPORT: A 73-year-old female presented with persistent twitching and vibration of the left arm and upper chest. A permanent pacemaker was inserted after she was diagnosed with a complete heart block. Interrogation of the device showed battery life was 8.5 years, left atrium impedance was 475 Ω (ohm), right ventricle impedance was 600 Ω (ohm), no sensing noted on the right ventricle while left atrium shows sensing more than 2.8 mv. Fluoroscopy performed and noted that the right ventricle lead was dislodged and there was a new deep subcutaneous pocket. The pacemaker box was reattached and anchored to pectoralis major muscle with non-absorbable suture. The deep pocket was closed and downsized. The procedure was uneventful and the patient was subsequently discharged well.
DISCUSSION: Twiddler’s syndrome is a rare syndrome that is found mainly in the elderly. Other risk factors associated with it such as having psychiatric illness, obese as well as female gender. Permanent dysfunction of the device is caused frequently by the lead displacement although diaphragmatic pacing might occur through the right ventricle perforations. The majority of Twiddler’s syndrome were reported within the first year of implantation. Applying multiple dressing over the wound site might prevent device dislodgement. Some faculties suggest the use of Dacron patch over the device in which overgrowth of tissues might secure the device better. Prior discharge patient was given proper education on pacemaker care.
CONCLUSIONS: Twiddler’s syndrome is a preventable condition given that only a small pocket is created and the device is properly fixed to the underlying structures with proper education given to the patient.
1.7.10. Open Chest Management in a High-Risk Patient Undergoing Three Valve Surgery and Coronary Artery Bypass Grafting
Eldar Valiyev, Ziya Shahaliyev, Aytaj Ismayilzada, Valeh Mammadov, Seymur Mustafayev, Fidan Zeynalli and Anar Amrah
Republican Diagnostic Center, Baku, Azerbaijan
AIM: In certain cases, particularly following severe dilated hearts, there arises the necessity of maintaining an open chest wall. This report highlights a case of open chest management in a severe patient suffering from chronic kidney disease (CKD) who underwent aortic valve replacement (AVR), mitral valve replacement (MVR), tricuspid valve repairment (TVr), and coronary artery bypass grafting (CABG).
CASE: A 51-year-old male CKD patient, undergoing hemodialysis for one year, presented with severe aortic, mitral, and tricuspid valve regurgitation post-infective endocarditis (IE). Echocardiography revealed heart chamber dilation with vegetation on the aortic (15 mm) and mitral (10 mm) valves and a left ventricular ejection fraction (LVEF) of 35%. Coronary angiography indicated severe occlusion of the LAD and its first diagonal branch.
The patient underwent AVR and MVR with mechanical valves (size №21 and №31 respectively), TVr with a modified KAY annuloplasty technique, and CABG for the LAD and diagonal arteries (LIMA–D1–LAD, sequential). Post-cardiopulmonary bypass (CPB), myocardial edema and decreased cardiac output necessitated maximal inotropic support, levosimendan administration and intra-aortic balloon pump (IABP) insertion. During the closure of the sternum, the patient’s hemodynamics decompensated, leading to the decision to leave the sternum open with a small-sized retractor.
By the third postoperative day, the patient’s condition stabilized, allowing sternum closure and decreased inotropic support. IABP removal occurred on the sixth postoperative day, with discharge on the thirteenth postoperative day.
Keeping the sternum open should be considered in patients with severe dilated hearts displaying low cardiac output, myocardial edema, and refractory dysrhythmias.
1.7.11. Management of Intracardiac Foreign Bodies (Shrapnel) After Mine Explosion—Our Experience During II Karabakh War
Ziya Shahaliyev, Valeh Mammadov, Teymur Gasimov, Javid Ibrahimov, Firdovsi Huseynov and Anar Amrah
Department of Cardiovascular surgery, Republican Diagnostic Center, Baku, Azerbaijan
AIM: The explosion of mines can lead to multiple bodily injuries and may result in the embolization of shrapnel particles into cardiac chambers. In this report, we present three cases of intracardiac foreign bodies during the Second Karabakh War.
CASE PRESENTATIONS: In our experience, three patients with shrapnel embolization into the right ventricle underwent open-heart surgery. The diagnosis was confirmed via X-ray or CT scan. Both cases underwent surgery in a hybrid operating room to confirm localization with rentgenoscopy. The first patient, a 19-year-old male, suffered multiple injuries after a mine explosion. A small metal shrapnel was identified on CT, and the patient experienced severe dysrhythmia and ventricular extrasystoles (9–10 per minute). Open surgery was performed, and the shrapnel particle, along with its capsule, was extracted beneath the tricuspid valve in the right ventricle. The second patient, a 25-year-old male, had shrapnel detected close to the right ventricle on X-ray. Rentgenoscopy revealed the shrapnel inside the right ventricle. Due to symptomatic presentation, open-heart surgery was conducted to remove the shrapnel. The third patient, a 30-year-old male, had suspicion of a foreign body during a follow-up ECHO examination. X-ray examination confirmed the presence of shrapnel in the right ventricle. As the patient was asymptomatic, it was decided to monitor him closely with follow-up examinations.
Foreign bodies within the heart are rare occurrences. These cases warrant surgical intervention only when accompanied by obvious symptoms and complaints. Otherwise, patients should be closely monitored, and if necessary, medical treatment could be administered.
1.7.12. A Rare Yet Perilous and Insidious Foe: Aortic Mural/Intraluminal Thrombus
Ayhan Müdüroğlu, Mustafa Selçuk Atasoy and Ahmet Yüksel
Department of cardiovascular surgery, ministry of health bursa city hospital, Bursa, Türkiye
Aortic mural thrombus are often linked with underlying aortic pathologies like aneurysms, atherosclerosis, dissection, and aortitis. They can be categorized into primary and secondary types. Secondary thrombus arise with aortic pathologies, typically seen in the descending thoracic and abdominal aorta. Primary thrombi occur in normal or minimally atherosclerotic aortas, usually pedunculated. They are mostly idiopathic but may be associated with hypercoagulability (malignancy, heparin-induced thrombocytopenia, antiphospholipid syndrome). Asymptomatic cases are incidentally diagnosed (often on computed tomography) and generally conservatively managed. Symptomatic patients receive anticoagulation, endovascular intervention, or open surgery based on history, thrombus location, size, and mobility. Ascending aorta or aortic arch thrombus warrants long-term anticoagulation due to embolic stroke risk. There is no specific treatment guide for mural thrombus.
CASE: A 47-year-old female patient, who has had systemic lupus for 7 years and has been using deltacortil and is also being treated for diabetes, hypertension and a history of mesenteric embolism, presented with complaints of pain, numbness, weakness in her left hand and discoloration of the fingertip for 2 months. Non-palpable left axillary and distal pulses, and cyanosis in the 4th and 5th left hand digits were noted. Computed tomography angiography revealed thrombosis in the aortic arch, descending thoracic aorta, left subclavian and deep femoral artery. Started on antiplatelet, anticoagulant, hospitalized, and underwent TEVAR stent graft placement under local anesthesia. Post-op, acute left iliac embolism led to embolectomy for severe pain and motor deficit in the left leg, with resolved motor deficit and capillary refill in 3 s. Failed thrombectomy via left axillary incision necessitated axillo-axillary bypass using saphenous vein. Left arm symptoms resolved, radial and ulnar pulses palpable, but no palpable left popliteal/distal pulses and claudication at 400 m persist. Currently monitored with new oral anticoagulants, antiplatelets, and cilostazol.
1.7.13. Surgical Treatment of Delayed Diagnosis Left Ventricular Giant Pseudoaneurysm After Myocardial Infarction
- 1
Department of Cardiovascular Surgery, Atatürk University Medical Faculty, Erzurum, Türkiye
- 2
Department of Cardiology, Atatürk University Medical Faculty, Erzurum, Türkiye
BACKGROUND: Left ventricular (LV) pseudoaneurysm is a rare but potentially lethal complication of myocardial infarction (MI). It may also develop following cardiac surgery, endovascular procedures, or trauma. Multimodality imaging may be required to differentiate a pseudoaneurysm from a true aneurysm and to plan the surgical treatment. Surgical intervention is required to treat pseudoaneurysm as there is a high risk of rupture.
CASE PRESENTATION: A 64 years old male patient applied to our cardiology department with shortness of breath and occasional chest and back pain. The patient had a history of hypertension, asthma and bladder cancer. The patient underwent coronary angiography and applied stenting for MI, 7 months before. Echocardiography showed 1.8 × 2.9 mm defect on the lateral wall and passage through the defect on color Doppler imaging. CT scan confirmed the echocardiographic findings. 138 × 80 × 102 mm cavity related to the defect was also detected. Surgery was planned. The patient underwent pseudoaneurysm excision and defect repair with a Teflon patch under cardiopulmonary bypass. He was taken to ICU post-surgery for 3 days. Postoperative echocardiography showed no passage through the defect and no cavity related to the defect. The patient was required long term oxygen therapy and discharged on day ten after the surgery.
1.7.14. Pseudoaneurysm Secondary to Saphenous Vein Coronary Bypass Graft Rupture
- 1
Department of Cardiothoracic Surgery, Royal Prince Alfred Hospital, Sydney, NSW 2050, Australia
- 2
Department of Cardiology, Concord Repatriation General Hospital, Sydney, NSW 2139, Australia
BACKGROUND: Aortocoronary saphenous vein grafts (SVG) are frequently utilised for coronary bypass grafting. Aneurysmal formation of SVGs may occur as a late complication. The primary mechanism is thought to be venous atherosclerotic disease, however vessel wall ischaemia and a relative increase in luminal pressure may play a role. In extremely rare circumstances, SVG aneurysm may result in graft rupture. This may result in pseudoaneurysm formation or as a pericardial effusion in the theoretically obliterated pericardial space.
CASE: We describe the case of a 77 year old male with acute chest pain in the context of functional decline, abdominal pain and nausea over the previous 3 days. He had an extensive past medical history, which included coronary artery bypass grafting 15 years ago, atrial fibrillation, and peripheral arterial disease with multiple angioplasties, amputation of left leg (below knee) and all right toes, and recurrent osteomyelitis of right foot. He lived in an aged care facility for assistance with transfers. A computed tomography aortogram demonstrated a pseudoaneurysm of a coronary artery bypass graft from aorta to left anterior descending artery. His electrocardiogram showed no ischaemic changes. A bedside transthoracic echocardiogram found no obvious regional wall motion abnormalities, however did identify an anterior pericardial effusion, comprising of a combination of blood and clot. He was urgently transferred to a quaternary referral centre with cardiothoracic services, whereby he arrived in extremis. Given his condition, frailty and significant co-morbidities, emergency surgery was deemed futile and he was transitioned to end of life care.
1.7.15. Pediatric Myxoma Case Diagnosed with Acute Arterial Ischemia and Ischemic Stroke and Its Management
- 1
Department of Cardiovascular Surgery, Hacettepe University, Ankara, Turkey
- 2
Department of Interventional Radiology, Hacettepe University, Ankara, Turkey
- 3
Department of Pediatric Pathology, Hacettepe University, Ankara, Turkey
Cardiac tumors and vasculitis are the most common causes of arterial ischemic stroke in the pediatric population. Since myxoma is a rare tumor in childhood, the literature on this topic is limited.
A female patient presented with fainting, right hemiparesis, left facial paralysis, and altered consciousness. Imaging revealed acute thrombotic occlusion in the left MCA M1. The patient was evaluated for vasculitis/cardioembolism. Echocardiography showed a hyperechoic area (mass/thrombus?) in the left atrium. Cardiac CT revealed an irregularly shaped structure in the left atrium, primarily suggestive of myxoma. The patient underwent urgent thrombectomy for MCA thrombus by interventional radiology. Subsequently, she underwent surgery for the removal of the cardiac mass. Using cardiopulmonary bypass under hypothermic conditions, the material removed from the heart. In the ICU, coldness/paleness in the right leg, with no palpable arterial pulses detected. CT revealed thrombosis in the right femoral artery and left popliteal artery. Post-thrombectomy imaging showed normal perfusion in the MCA territory. The patient underwent embolectomy for the right femoral artery. She was continued on heparinization post-surgery. During the follow-up, the patient regained consciousness, while the facial paralysis resolved completely, the weakness on the right side improved but persisted. Arterial ischemia in the right leg completely resolved. After 5 days in the ICU and 2 weeks in the ward, she was discharged with following physical therapy.
Histopathological examination confirmed the diagnosis of cardiac myxoma. The material extracted from the MCA was considered to be tumor thrombus. However, no tumor tissue was found in the material from the right femoral embolectomy.
Although cardiac myxoma is a rare tumor in childhood, it can lead to ischemic stroke and embolic events, which are serious conditions. Left-sided myxomas can play a role in the etiology of stroke and arterial ischemia without causing any symptoms beforehand. Early diagnosis and mechanical thrombectomy can limit neurological deficits in the treatment of acute embolic ischemic stroke in childhood. Cardiac myxomas should be considered as a rare but important pathology in pediatric patients presenting with symptoms of stroke and arterial ischemia.
1.7.16. Identifying Low Arising Coronary Arteries as Risk Factors for Adverse Outcomes in Aortic Valve Intervention
Philemon Gukop, James Dargan, Pouya Youssefi, Fizal Khan and Robin Kanagasabay
St George’s University Hospital NHS London, London, UK
BACKGROUND AND AIM: Low arising coronary arteries ostia is a risk factors for coronary occlusion during transcatheter aortic valve intervention (TAVI). This marker of adverse outcome could preclude TAVI or require advanced techniques. Is Surgical aortic valve replacement risk free in the presence of low arising coronary artery ostia.
METHOD: CASE: A 76-year lady with symptomatic critical bicuspid aortic valve stenosis, an equipoise candidate was declined her preferred choice of TAVI due to low arising left coronary with risk of coronary obstruction on CT assessment. She had an urgent SAVR with 21 mm tissue valve, in the post operative period developed anterior STEMI. Emergency coronary angiography with IVUS demonstrated a slit like LMS ostium and emergency LMS stent was performed with good results. She subsequently developed complete heart block and a dual chamber permanent pace maker was implanted
RESULTS: She made a good recovery and was discharged home in stable condition. She was doing well with good valve function at 1 year follow up
Low arising coronary arteries is a risk factor for adverse outcomes in both TAVI and SAVR and requires careful consideration by the hear team.
CONCLUSIONS: Low arising coronary artery ostia is a marker of adverse outcomes during aortic valve intervention and should be factored in risk profile and discussions with patients prior to intervention
1.7.17. Urgent CABG Surgery of Achondroplasia Patient with Low Ejection Fraction
Mehmet Aydin Kahraman, Gözde Tekïn, Huseyïn Uzandi, Selen Öztürk, Süleyman Aycan and Mehmet Kizilay
Dr. Siyami Ersek Thoracic and Cardiovascular Surgery Education Research Hospital, Istanbul, Turkey
Introduction: Achondroplasia is a hereditary disease caused by an anomaly in the FGFR3 gene, which accounts for 80% of the causes of dwarfism. The need for cardiac surgery in patients with achondroplasia, a musculoskeletal disease characterized by short limbs that occur in 1:25,000 in the general population, is a non-routine and alarming situation for cardiac surgeons.
Case: We will share about the urgent coronary bypass surgery and management of the post-operative process of a 62-year-old male patient of Turkish origin with achondroplasia, 20% ejection fraction, LMCA lesion and known Leriche Syndrome. After RCA, CX, DIA and LAD-LIMA distal and proximal anastomoses were made, IABP was considered for the patient who could not get out of CPB despite high dose inotropic support, but as intervention could not be achieved due to peripheral artery disease, it was decided to install central ECMO. After ECMO insertion, the patient was monitored in the ICU with the sternum open and the skin closed, with an ECMO flow of 2.70 and RPM of 1950.
On the 6th postoperative day, the patient was weaned from central ECMO after the desired hemodynamic stability was achieved with a low inotrope dose and low ECMO flow. The patient, who was extubated on the 8th day of the operation, was admitted to the regular hospital room on the 23rd post-operative day and was discharged on the 30th post-operative day. Follow up controls one week, one month after discharge revealed no pathologies and our patient was objectively and subjectively well.
Conclusions: Although operating on a patient with achondroplasia is a non-routine and unsettling situation for adult cardiac surgeons, these patients can be discharged in good health with successful surgery and meticulous post-operative management.
1.7.18. Neurological Complications in Cardiac Surgery Patients with Different Forms of Coronary Artery Disease
Olena Gogayeva, Anatolii Rudenko and Serhii Rudenko
Department of Surgical Treatment of Ischemic Heart Disease, GF “National Amosov Institute of cardiovascular surgery NAMS of Ukraine”, Kyiv, Ukraine
BACKGROUND AND AIM: Despite the maximum preventive measures in modern cardiac surgery, the level of cerebral postoperative complications is 1.5–6%. To analyze neurological complications in cardiac surgery patients with different forms of coronary artery disease (CAD)
METHOD: A retrospective analysis of 354 random high-risk patients with CAD with an average EuroSCORE 8.8%. All patients underwent ECG, ECHO, coronary angiography, surgical myocardial revascularization with correction of complicated forms of CAD in 160 cases. Preoperative ultrasound study (US) of the brachiocephalic arteries (BCA) was performed for 280 (79.09%) patients.
RESULTS: The history of stroke had 43 (12.1%) patients. Among 280 patients who underwent US of BCA, stenosis of the internal carotid arteries more than 50% was diagnosed in 95 (33.9%) cases. In the postoperative period, in 10 (2.8%) patients non-fatal cerebrovascular complications (CVC) were developed, among which 5 (1.4%) had an ischemic stroke, and 5 (1.4%) had a transient ischemic attack (TIA). Among patients with isolated CAD, CVC occurred in 6 (3.09%) persons, including TIA—in 2 (1.03%), stroke—in 4 (2.06%). Among patients with complicated CAD, focal and cerebral neurological symptoms in the postoperative period were registered in 4 (2.5%) patients, of whom 3 (1.8%) with TIA neurological symptoms regressed, and in 1 (0.62%) patient with diagnosed ischemic stroke—were stable ones. Analysis of perioperative period showed: the risk of CVC increases in patients with history of stroke (50%, p = 0.0002), aortic calcification (40%, p = 0.003), preoperative atrial fibrillation (30%, p = 0.013) and more significant decrease of blood pressure on the 1st postoperative day (p = 0.005).
CONCLUSIONS: The work of a multidisciplinary team helps to avoid life-threatening events. The cardiac surgeon should avoid manipulations on the atheromatous aorta by performing total arterial revascularization. Individual approach with strict monitoring of blood pressure and prevention of hypotension are required at all stages of perioperative patients management.
1.7.19. Coronary Artery Bypass Graft Surgery in a Gout Patient
Gizem Duygu Kılıçarslan, Ali Kemal Karpuz, Sefer Usta and Mine Demirbaş
Sbu Ahi Evren Gkdc Education Hospital, Trabzon, Turkey
Gout usually presents with a clinical picture of arthritis. Gouty arthritis involves the metatarsophalangeal joint of the big toe earliest and most commonly. Upper extremity involvement is less common than lower extremity involvement. Symptoms usually start at night and occur suddenly. Increased temperature, pain, swelling, redness and tenderness are observed in the affected joints in the acute period, and these findings may resolve spontaneously within days without treatment. The goal of treatment in acute arthritis attack is to reduce pain and to end the acute exacerbation period as soon as possible. Colchicine, nonsteroidal anti-inflammatory drugs, glucocorticoids (considering the patient’s age and comorbidities) may be given in the treatment. Antihyperuricemic treatment is not given in acute attack. Antihyperuricemic treatment further exacerbates the gout attack and may prolong the duration of the attack.
CASE REPORT: A 79-year-old male patient was admitted to the emergency room with chest pain for four and a half months and recent increase in back pain. Coronary angiography revealed LAD 80%, RCA 60%, CX 70% occlusion. The patient was presented to the cardiac team and coronary artery bypass surgery was recommended with the decision of the council. The patient was then transferred to our clinic for surgical planning. Thoracic tomography showed no calcification in the ascending aorta and normal aortic diameter. Ejection fraction was 60%, mild mitral valve regurgitation, mild aortic valve regurgitation and trace tricuspid regurgitation were detected on echocardiography. Carotid doppler ultrasonography revealed no stenosis. Rheumatology was consulted in preoperative preparations. Their opinions and recommendations were obtained preoperatively and postoperatively. Since nutrition was closely related with gout attacks, a dietician was consulted for calorie calculation and nutritional recommendations
1.7.20. Iatrogenic Tracheal Rupture After CABG: A Case Report
Sefer Usta and Hasan Hamzaoğlu
Sbu Ahi Evren Gkdc Education Hospital, Trabzon, Turkey
Tracheal rupture can occur spontaneously or due to trauma. This trauma can be a direct trauma or an iatrogenic trauma. Identified risk factors include long-term steroid use, COPD, and occupational diseases that cause lung problems. Diagnosing the disease quickly and providing appropriate treatment are very important for the survival of patients. Although the patient’s clinic and radiological imaging are useful in giving an idea about the disease, the definitive diagnosis is made by bronchoscopy. After the diagnosis is made, the treatment that must be decided by taking into account the patient’s condition is conservative or surgical intervention.
We present a case report in which tracheal rupture due to iatrogenic trauma in a patient undergoing CABG surgery may be fatal. The patient, a 62-year-old man who had been working as a shoe repairman for more than 40 years, had no known disease. The patient, who applied to an external center with complaints of chest pain and shortness of breath, was referred to our hospital after his troponin level was high. Urgent coronary angiography was planned for the patient whose complaints were specific and whose troponin was high. CABG decision was made for the patient who had stenosis in the left main coronary and proximal LAD. Since the patient had intermittent short-term ventricular tachycardia attacks and continued chest pain, it was decided to install an IABP before being taken into emergency surgery. It was decided to wait 3 days for the operation because the patient’s chest pain disappeared after IABP and there was no VT attack. The troponin level was high and ticagrelor and acetylsalicylic acid loading was performed before coronary angiography. During this period, the patient did not have chest pain, and was monitored in sinus rhythm with 100 mg ASA per day and low molecular weight heparin every 12 h.
1.7.21. Clinical Case of Urgent Cardiac Surgery for Patient with Thrombotic Occlusion of Internal Carotid Artery and Floating Thrombus in the Left Ventricle
Olena Gogayeva, Oleksandr Nudchenko, Yevhenii Aksonov, Natalia Ioffe and Anatolii Rudenko
Department of Surgical Treatment of Ischemic Heart Disease, GF “National Amosov Institute of cardiovascular surgery NAMS of Ukraine”, Kyiv, Ukraine
BACKGROUND: One of the life-threatening complications of acute myocardial infarction (AMI) is left ventricular aneurysm (LVA). The presence of a thrombus in the aneurysmal sac is fraught with embolic complications.
CASE REPORT: A 65-year-old patient was admitted to the Institute with complaints on shortness of breath, palpitation and limb edema. 11 years ago he suffered AMI but didn’t consult cardiologist till hospitalization to the hospital with cardiac asthma 3 weeks ago. The patient’s comorbidity: type 2 DM, gout, obesity. In admittance on ECG signs of aneurysm of anterior-septal-apical wall of left ventricle (LV) were detected. On Echo study we found severe decrease of global contractility of LV due to widespread postinfarction scar and LVA with EF 22%, EDV 275 mL, floating thrombus 5.5 × 2.35 cm, pulmonary hypertension. Ultrasound screening of the brachiocephalic arteries (BCA) revealed thrombotic occlusion of the right internal carotid artery (RICA), that was confirmed by CT study. Coronary angiography found occlusion of LAD and subocclusion of the DB LCA, arteria intermedia and 1 OM. Despite the RICA occlusion, the patient hadn’t neurological deficit and was consulted by neurosurgeon—there were no absolute contraindications for cardiac surgery. ES II risk was 14.88%. After heart team discussion we performed an operation: CABG with resection of LVA with thrombectomy on-pump. Operation duration 6 h, aortic cross-clamp time 79 min, perfusion time 152 min, blood loss 250 mL. The postoperative period was uneventful, systolic blood pressure was maintained at 130 mmHg, the patient was discharged on 10 postop day with positive dynamic (EF 25%, EDV 221 mL).
CONCLUSIONS: this clinical case demonstrates successful surgical treatment of the patient with LVA with floating thrombus and thrombotic occlusion of RICA. The key to success in the treatment is careful planning of perioperative management by the Heart team and stability of hemodynamic parameters.
1.15. CARDIAC » MICAB (Minimally Invasive Coronary Artery Bypass) (Including MIDCAB, MICS-CABG, TCRAT, LAST, MACAB)
1.15.1. Total Coronary Revascularization via Left Anterior Thoracotomy: Our Single Center Experiences and Comparison with Conventional Coronary Artery Bypass Surgery
Tuna Demirkiran 1, Furkan Burak Akyol 1, Tayfun Özdem 1, Elgin Hacizade 1, Emre Kubat 2, Gökhan Erol 1, Murat Kadan 1 and Kubilay Karabacak 1
- 1
Department of Cardiovascular Surgery, University of Health Sciences Health Practice and Research Centers, Ankara, Turkey
- 2
Department of Cardiovascular Surgery, Central Military Hospital of Ministry Defence of Azerbaijan, Baku, Azerbaijan
BACKGROUND AND AIM: Total coronary revascularization with left anterior thoracotomy (TCRAT) was defined in 2019. In our study, we aimed to evaluate the efficacy and safety of the TCRAT technique by comparing it to conventional coronary artery bypass surgery (CABG) with median sternotomy.
METHOD: Patients who underwent 108 TCRAT (group 1) and 154 conventional CABG (group 2) were performed by the same surgical team. Preoperative, operative, and postoperative data of patients and mid-term follow-up data were analyzed retrospectively.
RESULTS: Cardiopulmonary bypass and cross-clamp times were 167.70 ± 68.93 and 77.03 ± 38.18 in Group 1 respectively and 106.64 ± 38.27 and 62.21 ± 24.06 in Group 2 respectively (p < 0.001). During the postoperative period, the all-cause mortality rate was 5.8% (n = 9) in Group 2, while it was 0.9% (n = 1) in Group 1 and there was a statistically significant difference between the two groups (p = 0.037). The mean hospitalization for Group 2 was 6.99 ± 3.37 and the mean hospitalization for Group 1 was 6.77 ± 4.24. Statistically significantly shorter duration of hospitalization in Group 1 was determined (p = 0.047). In addition, the perioperative mean number of red blood pack transfusions in Group 1 was 1.51 ± 1.74, while it was 1.86 ± 1.75 in Group 2 and statistically significantly fewer red blood pack transfusions were performed in Group 1 (p = 0.033).
CONCLUSIONS: TCRAT, which is a less invasive method compared to conventional CABG, is an effective and safe method. It stands out as a routinely applicable method except in selected cases.
1.15.2. Minimally Invasive CABG Made Easy: Coronary Revascularisation via Left Anterior Thoracotomy
- 1
Cardiothoracic Unit, Universiti Malaya Medical Centre, Kuala Lumpur, Malaysia
- 2
Cardiothoracic Unit, KPJ Damansara Specialist Hospital 2, Kuala Lumpur, Malaysia
BACKGROUND AND AIM: Since 2014 we performed a total of 164 minimally invasive CABG (MICS) cases. We reviewed our journey of learning and adopting Total Coronary Revascularisation via Left Anterior Thoracotomy (TCRAT) into our MICS service of 9 years by analysing the operating experience and the clinical outcomes.
METHOD: All TCRAT cases in our database were reviewed. Operating experience was objectively measured in the number of grafts, aortic cross clamp (AXC) time, cardiopulmonary bypass (CPB) time, and transit time flow measurement (TTFM) of the grafts. These were compared with the conventional CABG (cCABG) cases within the same time line. Clinical outcomes analysed include conversion, re-exploration, in-hospital cardiovascular death, and stroke.
RESULTS: From January 2023 to March 2024 there were 116 TCRAT and 110 cCABG cases. These cases were performed by two leading surgeons separately. One of them is a junior consultant. 89.6% (n = 104) of the cases were male and the mean age of the patients were 62 years. 34.5% of the cases were multi-arterial grafting. The mean number of grafts comparing TCRAT to cCABG were 2.77 vs. 3.20. The mean AXC and CPB time between TCRAT and cCABG were (81.8 min vs. 97.0 min) and (161.2 min vs. 139.0 min). There were no significant differences when comparing TTFM parameters between the two groups. The institutional learning curve plateaus at around 50th case. We had 1 (0.86%) cardiovascular death.
CONCLUSIONS: TCRAT is highly adaptable and can be taught early in the career. The quality of the coronary anastomosis is comparable to cCABG and it has an acceptable safety profile. Widespread adoption of TCRAT should be encouraged.
1.15.3. Well-Being on Fast Track—Minimal Invasive Cardiac Surgery in Remote Area of Under Developed Country
Hafeez Ullah Bughio and Huma Akhtar
National Institute of Cardiovascular Diseases, Karachi, Pakistan
BACKGROUND AND AIM: Aim of this study is to analyse the outcome of initial 74 patients underwent minimally invasive cardiac surgery at centre located in rural areas of Sindh Pakistan.
METHOD: Total 74 patients were included in a case series analyzed retrospectively. All cases were operated at NICVD satellite centre Tando Muhammad Khan from 1 January to 31 December 2022. All patients included underwent minimally invasive cardiac surgery for variety of procedures done by single surgeon. Preoperative, operative and postoperative data was collected and analysed for different variables.
RESULTS: Mean age was 30.43 (12.59)
Female predominance 52.7%
NYHA-III 68.6%
Diagnosis severe Mitral Regurgitation 35.4%, ASD 28.3%, severe Aortic Stenosis 10.81%, SVCAD 8.11%.
Procedure: Mitral valve replacement 41.89%, ASD closure 28.38%, Aortiv Valve Replacement 13.51%, MIDCAB 10.81%, Double valve replacement 4.5%, LA MYxoma excision 1.35%.
Conversion rate 2.7%, Reopening rate 1.4%, Respiratory complications 1.4%, Superficial surgical site infection 4.1%.
Blood transfusion < 1 PCV per patient.
Majority of patients 75.7% had chest drain output of >200 mL but <500 mL over 48 h.
Mean ICU stay was 1 day in 79.7%.
Discharged at 3rd POD, no inhospital mortality.
6 months follow up showed 78.4% alive and healthy, 18.9% were lost to follow-up and 2.7% were dead.
CONCLUSIONS: Performing MICS at a centre in a rural area was challenging but our results are at par with international results of MICS considering the facilities given in rural area of Sindh proves that MICS is a safe and beneficial strategy for different cardiac surgery setups in Pakistan. the reduced postoperative complications, lesser blood transfusion, speedy recovery, early hospital discharge and most importantly patient satisfaction marks and upper edge.
1.15.4. A Single-Center Experience in Coronary Artery Revascularization: Transformation from a Standard to a Minimally Invasive Procedure
Zoran Saša Tabaković 1, Slobodan Mićović 2, Petar Vuković 2, Petar Milačić 2, Miroslav Miličić 2, Zorana Dančetović 1, Miloš Matković 3 and Igor Živković 2
- 1
Clinical for Cardiac Surgery, Institute for Cardiovascular Diseases “Dedinje”, Belgrade, Serbia
- 2
Clinical for Cardiac Surgery, Institute for Cardiovascular Diseases “Dedinje”, Belgrade, Serbia & Faculty of Medicine, University of Belgrade, Belgrade, Serbia
- 3
Clinical for Cardiac Surgery, University Clinical Center of Serbia, Belgrade, Serbia & Faculty of Medicine, University of Belgrade, Belgrade, Serbia
BACKGROUND AND AIM: Due to its benefits, MIDCAB is gradually becoming a more common treatment method. The most important issue is the learning curve, particularly when the surgeon feels comfortable performing the MIDCAB surgery. We demonstrated the experienced surgeon’s learning curve for transitioning from a conventional surgical technique to a MIDCAB method.
METHOD: Between February 2023 and January 2024, one surgeon with previous expertise in conventional coronary revascularization performed 29 MIDCAB procedures. The learning curve was investigated by analyzing trends in variables such as procedure time, ventilation time, ICU time, technical failure, and complications like revision of hemostasis, MI, LIMA occlusion, pneumothorax, death, and others.
RESULTS: This study included 29 patients, the majority of whom were male (75.9%), with an average age of 67.4 ± 7.1 years (
Table 7). The mean duration of the procedure was 160 ± 51 min, exhibiting a noteworthy decline with time. Dividing the patients into three groups every four months in a year will show that, over time, the procedure’s average duration has decreased from 180 ± 48 to 145 ± 31 min. The duration of intubation was 7 ± 5 h on average. In just 1 case (3.4%) conversion to medial sternotomy was performed. Except for one LIMA occlusion (3.4%), there were no significant cardiovascular problems throughout the postoperative phase. With a decreasing duration of time, the average ICU stay was 28 ± 12 h, and the average hospital stay was 5 ± 1 days, with no deaths. We should mention that during the study period, we performed 1 MIDCAB surgery with multi-vessel revascularization (CABG × 3), and 4 patients (13.8%) had the subxiphoid technique for LIMA harvesting.
CONCLUSIONS: Transferring from conventional to MIDCAB procedures requires a learning curve, whose length depends on the surgeon’s experience in conventional myocardial revascularization. Experienced surgeons may easily adapt to performing MIDCAB operations, with few adverse events.
1.15.5. Minimally Invasive Multi-Vessel Coronary Artery Bypass Grafting for Complete Revascularization: A Single-Center Experience
Muhammad Yasir Khan and Muhammad Hamid Chaudhary
Chaudhary Pervaiz Elahi Institute of Cardiology Multan, Multan, Pakistan
BACKGROUND AND AIM: This study aimed to evaluate the outcome of the first 50 cases of isolated minimally invasive multivessel CABG in terms of complete revascularization and review the surgical technique in terms of efficacy, and safety.
METHOD: This retrospective analysis was done from January 2023 to February 2024. Only patients with isolated CABG and an EF of 35% or more were selected. All patients underwent minimally invasive multivessel CABG through a left anterior mini-thoracotomy in the fourth intercostal space. Chitwood clamp and del Nido cardioplegia were used. The procedure was completed either on beating heart, on-pump beating, or cardioplegic arrest. Femoral arterial and venous cannulation were performed with vacuum-assisted drainage for complete decompression. The left internal mammary artery and the long saphenous vein were used as conduits. We examined the number of grafts decided preoperatively on coronary angiography and the grafts completed postoperatively, operating time, and postoperative outcomes.
RESULTS: Of the 50 patients (
Table 8), 10 (20%) underwent off-pump CABG, 40 (80%) underwent On-pump CABG, and three underwent on-pump beating CABG. One patient died of a stroke (watershed stroke), and two conversions to sternotomy. One patient had intramyocardial LAD and the second patient had pulmonary artery injury. One reopening due to bleeding was controlled via a thoracotomy. Among the 40 patients who underwent on-pump CABG, the total cardiopulmonary bypass time was 192.69 ± 41.02 min, and the aortic cross-clamp time was 105.825 ± 29.49 min. The average number of diseased vessels was 2.57 ± 0.72, and the average number of grafts done was 2.38 ± 0.86.
CONCLUSIONS: Complete coronary revascularization can be routinely performed using the aforementioned technique. No patient selection, based on the number of grafts, quality, location of coronary vessels, left ventricle function, age, gender, or body mass index, is required.
1.15.6. Pleural Effusion Post-Total Coronary Revascularization via Left Anterior Thoracotomy
Zhi Rong Low and Shahrul Amry Hashim
Division of Cardiothoracic Surgery, Department of Surgery, Faculty of Medicine, University of Malaya & University of Malaya Medical Centre, Kuala Lumpur, Malaysia
BACKGROUND AND AIM: The use of minimally invasive approaches such as total coronary revascularization via left anterior thoracotomy (TCRAT) for multi-vessel coronary disease is on the rise. However, data on the post-operative complications, specifically the occurrence of pleural effusion, is scarce. We aim to investigate the role of this novel technique as an alternative to conventional coronary artery bypass grafting (CABG) surgery with regards to its clinical outcomes.
METHOD: A retrospective study involving patients who underwent TCRAT surgery from January 2023 to February 2024 was conducted. Various pre-, intra- and post-operative parameters were determined and compiled. We identified patients who developed pleural effusion post-operatively which required pigtail insertion or readmission. Chi-Square test, univariate and multivariate logistic regression tests were used to assess correlation between the clinical parameters and incidence of pleural effusion.
RESULTS: A total of 109 patients with the mean age of 62.02 (SD = 9.32) were included in our study, 89.9% of which are male and majority werediagnosed with triple vessel disease. The mean left ventricular ejection fraction (LVEF) was 59.06% (SD = 10.67%) and most patients (90.9%) had normal renal function or mild renal dysfunction pre-operatively. 20 (18.3%) patients were complicated with post-operative pleural effusion which is defined by persistent chest tube drainage for at least 4 days. 3 patients required pigtail insertion and 9 needed readmission. The duration of chest tube insertion was found to be significantly associated with pleural effusion leading to pigtail insertion and readmission (X2 = 18.98; df = 2; p < 0.001).
CONCLUSIONS: Our study shows that pleural effusion post-TCRAT surgeries requiring further intervention or readmission correlates with longer duration of chest tube insertion. Future research with a larger sample size should be carried out to evaluate other potential risk factors in order to improve the outcomes of this minimally invasive technique.
1.15.7. Patient-Reported Outcomes Measured Between Total Coronary Revascularization via Anterior Thoracotomy and Conventional Coronary Artery Bypass Graft: Where Quality of Life Matters
Nur Nadiah Nazri 1, Ummu Solehah Mohd Fauzi 1, Fatimah Alia Mohd Afandi 1, Muhammad Ibrahim Azmi 2 and Shahrul Amry Hashim 3
- 1
Cardiothoracic Intensive Care Unit, University Malaya Medical Centre, Kuala Lumpur, Malaysia
- 2
Cardiothoracic Unit, University Malaya Medical Centre, Kuala Lumpur, Malaysia
- 3
Cardiothoracic Unit, KPJ Damansara Specialist Hospital 2, Kuala Lumpur, Malayisa
BACKGROUND AND AIM: We explored patient-reported outcome measures in patients who underwent Total Coronary Revascularization via Left Anterior Thoracotomy (TCRAT) and Conventional Coronary Artery Bypass Grafting (cCABG).
METHOD: A Telemedicine health survey was conducted for all TCRAT and cCABG patients from January 2023 to October 2023. Post-operative quality of life was assessed using a validated SF-36v2 questionnaire. All telephone calls were adapted to the language suitable for patients: English, Malay, Chinese, and Tamil. The questionnaire was done in December 2023. The survey outcomes were compared between the two groups using statistical analysis. There is a total of 83 TCRAT patients and 50 cCABG patients.
RESULTS: Following the exclusion of patients who refused participation, there were 60 TCRAT and 26 cCABG. The mean of duration follow-up assessment for TCRAT was 8 months and cCABG 10 months. SF36 questionnaire focuses on several categories: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health. Higher overall scores indicate better performance. The result shown in
Table 9.
CONCLUSIONS: The postoperative survey from our series has shown better patient-reported outcomes in TCRAT patients when compared to cCABG patients. This suggests a desirable patient-centered benefit on top of the potential clinical superiority of the sternal-sparing approach to minimally invasive surgery.
1.15.8. Prediction of Adverse Clinical Outcomes During 12 Months After Hybrid Myocardial Revascularization
Aliaksandr Charniak, Vladislav Podpalov, Kiryl Rubakhov, Oleg Kozak and Alexey Ostrovsky
Department of Cardiac Surgery, Minsk Scientific and Practical Center for Surgery, Transplantology and Hematology, Minsk, Belarus
BACKGROUND AND AIM: Hybrid myocardial revascularization (HMR) is debatable in modern cardiac surgery. The aim was to estimate 1-year outcomes after HMR in comparison with off-pump coronary artery bypass grafting (OPCAB) and to determine preoperative prognostic criteria for adverse clinical outcomes.
METHOD: 180 consecutive patients with multi-vessel coronary artery disease were randomized into 2 groups: 1st group—98 patients, who underwent OPCAB; 2nd group—82 patients with performed HMR. HMR consisted of 2 stages: minimally invasive direct coronary artery bypass grafting and later within 24–72 h PCI stage was performed.
RESULTS: HMR showed an advantage at the hospital stage in comparison with OPCAB due to reduction of myocardial damage, minimization of the intervention and faster postoperative rehabilitation with a comparable frequency of adverse clinical events. Within 12 months after surgery, the frequency of development of a combined endpoint, which included at least one of such events as myocardial infarction, stroke, restenosis of stent or the failure of anastomosis, repeated revascularization and cardiac mortality was lower among patients after HMR. Based on significant preoperative criteria, a multifactorial model was developed for predicting the unfavorable development of the disease after HMR, consisting of 3 factors: the level of CRP > 3.5 mg/mL in patients with BMI > 28.5; the concentration of glycated hemoglobin > 6.1% in people with a history of a stroke; a combination of hyperglycemia (glucose level > 6.6 mmol/L) and increased platelet aggregation (ADP > 664 AU*min).
CONCLUSIONS: HMR may be considered better surgical decision in patients with multi-vessel CAD. In our prognostic model the accuracy of predicting adverse clinical outcomes during 1 year after HMR is 91.7%.
1.15.9. Overcoming Challenges and Implementing Solutions in Establishing a Minimally Invasive Cardiac Surgery Program: Our Experience and Lessons Learnt
Muhammad Hamid Chaudhary and Muhammad Yasir Khan
Chaudhary Pervaiz Elahi Institute of Cardiology Multan, Multan, Pakistan
BACKGROUND AND AIM: Early return to work after cardiac surgery is of greater value in developing countries and this can be achieved through minimally invasive cardiac surgery (MICS). Nowadays most adult procedures and isolated coronary artery bypass grafting can be performed through MICS techniques. We present our experience, the strategies used, and the challenges faced while starting a minimally invasive cardiac surgery program at a newly established tertiary care center.
METHOD: We retrospectively collected our data on MICS procedures done in our hospital between September 2022 and February 2024. We analyzed our results regarding mortality, morbidity and complications, and other quality parameters like ICU stay, blood loss, ventilation time, strokes, re-exploration rate, hospital stay, etc. A step-wise approach was adopted that introduced every team member to the increasing complexity of the procedures.
RESULTS: Of the 125 patients (
Table 10), 74 (59.2%) were minimally invasive CABG, 12 (9.6%) were aortic valve replacement, 31 (24.8%) were mitral valve replacement, 5 (4%) were atrial septal defect repair 1 (0.8%) was Double valve replacement (aortic and mitral valve) and 1 (0.8%) was LA myxoma excision & and 1 (0.8%) was ventricular septal defect. Two patients had strokes, among those one patient died, and two conversions to sternotomy. One patient had intramyocardial LAD and the second patient had pulmonary artery injury. There were four reopenings due to bleeding which was controlled via a thoracotomy.
CONCLUSIONS: MICS follows the same principles of heart surgery, train your team, take good informed consent, individualize the access, and avoid extreme anatomy, flat chests, and tiny patients. Likewise, don’t be fanatic about it, don’t compromise the repair/results just for the sake of MICS, and never hesitate to convert. Local and Global alliances, industry support, and proctorship are mandatory.
MICS is an opportunity, not a threat, and can provide an edge for our high-tech healthcare system without colliding with the principles of value-driven outcomes.
1.15.10. Advancements in Minimally Invasive Coronary Bypass Surgery for Obese Patients: Evolving Perspectives in Cardiac Care
BACKGROUND AND AIM: Coronary artery disease (CAD) remains a leading cause of morbidity and mortality worldwide, with obesity representing a significant risk factor for its development and progression. Traditional coronary bypass surgery, while effective, may pose heightened risks and complications in obese patients due to associated comorbidities such as diabetes, hypertension, and dyslipidemia. Minimal invasive coronary bypass surgery (MICAB) has emerged as a potential alternative, offering the promise of reduced surgical trauma, shorter recovery times, and improved cosmetic outcomes. However, the efficacy and safety of MICAB specifically in obese individuals have not been comprehensively elucidated. Thus, a thorough evaluation of MICAB in this patient population is warranted to inform clinical practice and optimize treatment strategies for CAD in the context of obesity.
METHOD: This study aims to evaluate the efficacy and safety of minimal invasive coronary bypass procedures in patients diagnosed with obesity. Through a comprehensive analysis of relevant literature and clinical data, this investigation seeks to elucidate the benefits and potential drawbacks of employing minimal invasive techniques in coronary bypass surgery among this specific patient population. The findings of this research endeavor are anticipated to contribute to the optimization of treatment strategies for coronary artery disease in obese individuals, thus enhancing clinical outcomes and patient care.
CONCLUSIONS: In conclusion, this study underscores the potential utility of minimal invasive coronary bypass surgery in patients with obesity. Our findings suggest that MICAB procedures demonstrate comparable efficacy to traditional coronary bypass surgery while offering distinct advantages, including reduced operative trauma and enhanced postoperative recovery, particularly relevant in the context of obesity-associated comorbidities. However, further prospective studies with larger sample sizes and longer follow-up periods are warranted to validate these findings and elucidate the long-term outcomes and safety profile of MICAB in obese individuals. Nevertheless, the insights gleaned from this investigation provide valuable guidance for clinicians in navigating treatment decisions for coronary artery disease in this high-risk patient population, ultimately facilitating improved patient care and outcomes.
1.15.11. MIDCAB: Short-Term Results and Experience of Minimally Invasive Coronary Surgery in Azerbaijan
Kamran Musayev, Ilkin Osmanov, Nigar Kazimzade and Kamran Ahmadov
Department of Cardiovascular Surgery, Merkezi Klinika, Baku, Azerbaijan
BACKGROUND AND AIM: Minimally invasive direct coronary artery bypass grafting (MIDCAB) via lateral thoracotomy provides a less invasive alternative to the conventional median sternotomy approach in coronary surgery, a technique that we also employ in Azerbaijan within our institution. This study aims to analyze the short-term outcomes of operations performed using the MIDCAB strategy in our center over the last two years.
METHOD: A retrospective analysis of data from patients who underwent MIDCAB surgery at our medical center from January 2022 to January 2024 was conducted to assess the short-term results of this strategy in treating patients with coronary heart disease. The database included all patients who underwent MIDCAB for revascularization of left anterior descending artery (LAD) stenosis using the left internal mammary artery (LIMA). The study encompassed 10 patients with a median age of 58.5 years (range: 52–68), consisting of 8 males and 2 females, with angina pectoris class 2.
RESULTS: No mortality or severe morbidity was observed, indicating the safety profile of this surgical strategy. The median duration of intensive care unit (ICU) stay was 2 days, with a median hospital stay of 5.5 days, highlighting the rapid recovery of patients. All patients exhibited stable clinical improvement in the early postoperative period. Detailed operative and postoperative patient characteristics can be found in
Table 11.
CONCLUSIONS: Our study confirms the safety and efficacy of MIDCAB procedures in our institution. The absence of mortality or severe complications, coupled with rapid patient recovery and stable clinical improvement, underscores the success of this approach. Our findings align with international standards of coronary surgery, reaffirming the promising role of MIDCAB in our medical practice.
1.17. CARDIAC » On-Pump CABG
1.17.1. Percutaneous Coronary Intervention with Drug-Eluting Stents Versus Coronary Bypass Surgery for Complex Coronary Artery Disease: A Bayesian Analysis of Randomized Trials
Michal J. Kawczynski 1, Andrea Gabrio 2, Jos G. Maessen 1, Arnoud W.j. Van’t Hof 3, James M. Brophy 4, Can Gollmann Tepeköylü 5, Peyman Sardari Nia 1, Pieter A. Vriesendorp 3 and Samuel Heuts 1
- 1
Department of Cardiothoracic Surgery, Maastricht University Medical Center (MUMC+), Maastricht, The Netherlands
- 2
Department of Methodology and Statistics, University Maastricht, Maastricht, The Netherlands
- 3
Department of Cardiology, Maastricht University Medical Center (MUMC+), Maastricht, The Netherlands
- 4
McGill University Health Center, Center for Health Outcome Research (CORE), Montreal, QC, Canada
- 5
Department of Cardiac Surgery, Medical University of Innsbruck, Innsbruck, Austria
BACKGROUND AND AIM: We aimed to assess the totality of randomized evidence comparing percutaneous coronary interventions with drug-eluting stents (DES-PCI) to coronary artery bypass grafting (CABG) for complex coronary artery disease (CAD), under the Bayesian statistical framework.
METHOD: A Bayesian re-analysis of trials comparing DES-PCI to CABG with 5-year follow-up was performed. The primary outcome was all-cause mortality at five years; secondary outcomes were stroke, myocardial infarction, and repeat revascularization. Endpoints were reported in relative risks (RR) and absolute risk differences (ARD), with 95% credible intervals (CrI). Kaplan-Meier curves were used to reconstruct individual patient data. This study was registered in PROSPERO (CRD42024512897, date: 25 February 2024).
RESULTS: Six studies (SYNTAX, NOBLE, EXCEL, PRECOMBAT, BEST, FREEDOM) comprising 8269 patients (DES-PCI n = 4134, CABG n = 4135) were re-analyzed using Bayesian statistics. All-cause mortality at 5 years was increased with PCI (median RR 1.23 (95%CrI 1.01–1.45), with a median ARD of +2.3% (95%CrI 0.1–4.5%). For stroke, MI, and repeat revascularization, the median RRs were 0.79 (95%CrI 0.54–1.25), 1.84 (95%CrI 1.23–2.75), and 1.80 (95%CrI 1.51–2.16) for PCI, respectively. Illustratively, in a sample of 1000 patients undergoing DES-PCI instead of CABG for complex CAD, a median of 23 additional deaths, 46 myocardial infarctions and 85 repeat revascularizations occurred at five years, while 10 strokes were prevented.
CONCLUSIONS: In complex CAD, CABG provides a clinically relevant benefit over DES PCI at five years. These findings offer an intuitive interpretation of revascularization outcomes in complex CAD, and may guide the heart-team and the shared decision-making process.
1.17.2. Obesity Is the Major Killer in Coronary Artery Bypass Grafting (CABG) Surgery
Muhammad Wasim Sajjad, Azam Jan, Rokhan Yousaf Zai and Rashid Qayyum
Department of Cardiothoracic & Vascular Surgery, Rehman Medical Institute, Peshawar, Pakistan
BACKGROUND AND AIM: To explore the impact of BMI on the short-term mortality and morbidity of patients undergoing CABG.
METHOD: Observational study on retrospective data of CABG patients at a tertiary care hospital from 1 July 2017 to 31 December 2022. Ethical approval was granted and inclusion criteria were met. Patients were then categorized according to their BMI groups & perioperative variables were extracted. For statistical analysis, Chi-square, t-test & multivariate regression analysis was employed. A p-value of <0.05 was considered statistically significant.
RESULTS: Total of 2599 isolated CABG patients were included with mean age of 57.86 ± 9.2 years. The majority was overweight (42%). Approximately 78.1% were male. Hypertension was our dominant co-morbidity (68.7%) followed by dyslipidemia (65.4%) & DM (50.1%). Majority of patients had NYHA-III symptoms (51.2%). The morbidly obese patients had the highest in-hospital mortality (11.3%) while overweight had the lowest (2.6%) with a p-value of 0.008. Generally, there is a significant increasing trend of DM & HTN incidence with increasing BMI compared to normal (<0.001). The insertion of IABP was significantly highest among the underweight having low EF when compared with preserved EF (0.05). Most of the underweight were elderly with a high incidence of postoperative complications (e.g., prolonged mechanical ventilation, blood product requirement, reopening & re-intubation), but not significant. However, they have significantly longer mechanical ventilation time compared to normal (<0.001). Multivariate regression analysis showed that mean age (p < 0.034), cross-clamp time (p < 0.018) & mechanical ventilation (p < 0.001) were significantly associated with in-hospital mortality.
CONCLUSIONS: Both extreme categories of the BMI showed higher incidence of perioperative complications, such as morbidly obese patients had the highest in-hospital mortality while overweight had the lowest confirming a partial obesity paradox, whereas underweight patients had significantly higher mechanical ventilation time.
1.17.3. Gender Difference and Its Outcomes in Anemic Patients Undergoing Coronary Artery Bypass Grafting Surgery
Muhammad Wasim Sajjad 1, Azam Jan 1, Saif Ullah 1, Muhammad Salman Farsi 1, Aamir Iqbal 2, Rashid Qayyum 1 and Sarmad Saeed 1
- 1
Department of Cardiothoracic & Vascular Surgery, Rehman Medical Institute, Peshawar, Pakistan
- 2
Department of Cardiac Surgery, Peshawar Institute of Cardiology, Peshawar, Pakistan
BACKGROUND AND AIM: According to some studies female gender is considered as an independent predictor of mortality in CABG. We sought to further identify the impact of anemia on outcomes according to gender.
METHOD: The observational study on retrospective data was conducted at a Tertiary care hospital from December 2020 to December 2023. A total of 1346 anemic patients were included, with 1029 male & 317 female patients. Institutional review board approval was granted and inclusion criteria were met. For statistical analysis, Chi-square & t-test were used. Data was analyzed using SPSS 25. A p-value of <0.05 was considered statistically significant.
RESULTS: The database of cardiovascular & thoracic department was searched for the patients who underwent isolated CABG. A total of 2570 patients were identified, amongst them only 1346 patients who met the criteria were included in the study, with the majority of the male population (76.4%) having a mean age of 59.2 ± 9.1 years. Most of the patients had NYHA III (54.7%) & CCS III (53.3%) functional class symptoms. Hypertension was our most common co-morbidity (72.8%), followed by DM (66.6%) & dyslipidemia (54.6%). Anemia is more prevalent in female patients & requires markedly higher rates of intra- & post-operative blood/products transfusion. In terms of post-operative outcomes, there was no notable difference in mean ventilation time, re-admission to ICU, re-intubation & in-hospital mortality. However male patients had significantly higher rates of re-opening (p = 0.005) with prolonged ventilation hours (p = 0.02).
CONCLUSIONS: There is no comparable gender difference in terms of mortality in anemic patients undergoing CABG. However female anemic patients required a substantially higher rate of blood/products transfusion.
1.17.4. The Role of AKIN, KDIGO, and RIFLE Criteria in Coronary Artery Bypass Surgery
Melïke Elïf Teker Açikel, Erman Süreyya Kiriş, Ülkü Ziyaoğlu, Mehmet Ziyaddin Altun, Tolga Demir and Ismail Koramaz
Cardıvascular Surgery of Şişli Hamidiye Etfal Eğitim ve Araştırma Hastanesi, İstanbul, Turkey
BACKGROUND AND AIM: Acute kidney injury is a loss of kidney function defined by an acute increase in serum creatinine and a decrease in hourly urine output. Our aim in this study is to determine the role of AKIN, KDIGO and RIFLE criteria in the prediction of mortality in diabetic patients who underwent Pump-Assisted Coronary Artery Bypass Graft operation.
METHOD: Among 1258 patients who were operated on in our clinic between January 2019 and December 2022, 310 diabetic patients who underwent Pump-Assisted Coronary Artery Bypass Graft operation were included in this study. In the cardiovascular surgery intensive care unit follow-up of the patients, anesthesia card, intensive care follow-up charts, need for continuous renal replacement therapy, use of diuretics, use of inotropic agents, mechanical ventilator therapy, The RIFLE, KDIGO and AKIN scores of the patients were calculated daily and the highest value during the hospitalization was recorded. In addition to the length of stay in the intensive care unit and hospital, the death and discharge status of the patients were also evaluated.
RESULTS: The mean age of 310 patients included in our study was 57.4 ± 10.5 years. 132 (42.6%) of our patients were female and 178 (57.4%) were male. 92% of the research group were discharged and 7.8% were exitus. It was observed that all of our exitus patients were at any AKI stage according to the KDIGO, AKIN and RIFLE classifications. According to the RIFLE, AKIN and KDIGO classifications, it was found that the mortality rate increased statistically as the Acute kidney injury stage increased
CONCLUSIONS: According to RIFLE, AKIN and KDIGO classifications, the mortality rate increases statistically as the stage of acute kidney injury increases. Checking these scores in patients scheduled for coronary artery bypass surgery may reduce mortality.
1.17.5. Preoperative Effect of Cilostazol Usage on Myocardial Protection and Perioperative Myocardial Infarction
Ahmet Ibrahim Balkaya, Begum Ozuekren Kasapoglu, Helin El Kilic, Tolga Demir and Ismail Koramaz
Department of Cardiovascular Surgery, Hamidiye Etfal Training and Research Hospital, Health Science University, Istanbul, Turkey
BACKGROUND AND AIM: Myocardial protection during cardiac surgery is critically important. Cardioplegic solutions enriched with various molecules have been used for this reason. In this study, the effect of preoperative Cilostazol usage on perioperative myocardial protection is investigated by measuring troponin I levels.
METHOD: A hundred consecutive patients (28 females, 72 males; mean age 67 ± 2.3 years) who underwent on pump coronary surgery are divided into two groups according to the preoperative Cilostazol usage. Troponin I investigation was done before surgery and following cross-clamp (after 1–3–6–12–24–48 h).
RESULTS: The average levels of Troponin I at six and twelve hours for the second group were significantly lower than the first group. There was no significant difference in other measured Troponin I levels.
CONCLUSIONS: Cilostazol usage before cardiac surgery partly lowers the myocardial damage during operative and early postoperative period.
1.17.6. Impact of Aortic Cross Clamp Time on Post Operative Outcomes in Patient Undergoing Cardiopulmonary Bypass Grafting
BACKGROUND AND AIM: Aortic cross clamping is a surgical instrument used in the cardiac surgery to clamp the aorta and separate the systemic circulation from outflow of the heart. Historically, aortic clamp time was linked to the adverse outcome following cardiac surgery. The aim of the study was to determine the effect of aortic cross clamp time and its impact on post operative outcomes.
METHOD: It was cross sectional study conducted over a period of six months from July 2023 to December 2023. All those patients were included in this study who undergone for adult cardiac surgery for coronary artery bypass grafting and valvular abnormalities. We excluded those patients who were presented with congenital cardiac abnormalities and re- do surgeries. Data was collected through non probability consecutive sampling method technique.
RESULTS: A total of (n = 100) patients were included in this study after meeting the inclusion criteria. As per the gender distribution 60% males and 40% females and the mean age of the patients were (48.13 ± 6.029), Mean aortic cross clamp time (54.37 ± 21.738) mean bypass time is (92.70 ± 36.487). If we talk about the post operative outcomes, we assessed that only 3% patients were detected with respiratory complications and 10% with renal complications.
Mean intensive care unit stay was (4.83 ± 2.147). It is also assessed that aortic cross clamp time is significantly associated with post operative out comes at p value < 0.05.
CONCLUSIONS: This study was conducted to assess the impact of aortic cross clamp time on post operative outcomes in patients. It is indicated that prolonged cross clamp time significantly correlates with Post operative morbidity and mortality in cardiac surgery patients. This effect is increasing with the increase of cross clamp time.
1.17.7. Pre-Operative Cardiac Troponin I Levels with Post Operative Outcome After Coronary Artery Bypass Grafting at Peshawar Institute of Cardiology
Zeeshan Afzal, Asif Khan, Hasan Zeb, Waqar Masud Malik, Zeeshan Abdul Nasir and Ubaid Ur Rehman
Department of Adult Cardiac Surgery, Medical Teaching Institute, Peshawar Institute of Cardiology, Peshawar, Khyber Pakhtunkhwa, Pakistan
BACKGROUND AND AIM: To find out the role of pre-operative cardiac Troponin I level with post operative outcome following a Coronary Artery Bypass Grafting (CABG).
METHOD: Selection of subjects was done according to the inclusion and exclusion criteria. They were divided into two cohorts. Acute MI patients with raised pre-CABG troponin I (Group A N = 64) and a second group with normal pre operative troponin I (Group B N = 59). Post operative outcome was assessed in terms of post operative (CABG) chest pain and hospital stay. The data was analyzed using SPSS version 26.0 for MacBook Pro and organized as tables.
RESULTS: Troponin I level showed statistical difference (p < 0.05) for both groups, with higher values for group A (5.14 ng/mL ± 2.16 ng/mL) in comparison with group B (0.09 ng/mL ± 0.06 ng/mL) subjects. Group A subjects had a prolonged hospital stay (10 days ± 2 days) and higher post operative (CABG) chest pain for longer periods of time in comparison to group B (5 days ± 1 day) and lower post operative pain.
CONCLUSIONS: In conclusion, this study found a direct relation between raised pre operative troponin levels and post CABG complications (hospital stay and post operative chest pain). This makes cardiac troponin I not only a diagnostic but a relatively fair and good marker or prognosis in assessing post CABG outcomes. The raised Troponin I in group A are associated with the post CABG outcomes.
1.17.8. Perioperative Evaluation of Kidney Function for Patients with Postinfarcton Aneurysm of Left Ventricle
Olena Gogayeva, Anatolii Rudenko, Serhii Rudenko and Vasyl Lazoryshynets
Department of Surgical Treatment of Ischemic Heart Disease, GF “National Amosov Institute of Cardiovascular Surgery NAMS of Ukraine”, Kyiv, Ukraine
BACKGROUND AND AIM: To analyze kidney function in the perioperative period for patients with postinfarction aneurysms of left ventricle (ALV).
METHOD: Retrospective analysis of random 110 high-risk pts with complicated forms of coronary artery disease (CAD). For all pts we performed ECG, ECHO, coronary angiography, coronary artery bypass grafting with correction of postinfarction aneurysm of left ventricle on pump and perioperative evaluation of kidney function by calculation of glomerular filtration rate (GFR).
RESULTS: Preoperative analysis of comorbidity shown: 86 (78.1%) pts had metabolic syndrome, 81 (73.59%)—disorders of glucose metabolism, 82 (74.5%)—chronic obstructive pulmonary disease and 38 (34.5%)—chronic kidney disease (CKD) 3–5 stage. Preoperative risk stratification with EuroSCORE II scale was 9.4%. All operations performed on pump with Custodiol cardioplegia in 53 (48.1%) cases. The average perfusion time was 111 min, average cross-clamping time was 73.9 min. All pts underwent ALV resection with thrombectomy in 57 cases. Correction of mitral insufficiency had 11 pts, between which 9 had mitral valve replacement and 2—mitral valve repair rings. Tricuspid valve repair was performed in 4 pts, interventricular septum defect repair—in 2 pts. The average number of grafts was 2.7, the internal thoracic artery was used in 18 (16.3%) patients. The average duration of the ventilation was 8.03 h. The average level of serum creatinine, glucose and hemoglobin in the perioperative period presented in
Table 12. Acute kidney injury in the early postoperative period had 9 (8.1%) patients.
CONCLUSIONS: At the admittance 38 (34.5%) pts with complicated forms of CAD had CKD. Analysis of the GFR dynamic in the early postoperative period shown a decrease of GFR in 71.05% of pts. Transient acute kidney injury with 50% sCr growth occurred in 9 (8.1%) cases but didn’t require hemodialysis due to timely correction of drug therapy.
1.20. INTERDISCIPLINARY » Aortic Dissection & Surgical Treatment (Open and Endovascular)
1.20.1. Can Computational Fluid Dynamics Simulations Predict a Distal Stent Graft Induced New Entry After Frozen Elephant Trunk Operation?
Anja Osswald 1, Konstantinos Tsagakis 1, Matthias Thielmann 1, Markus Kamler 1, Rolf Alexander Jánosi 2, Thomas Schlosser 3 and Christof Karmonik 4
- 1
Department of Thoracic and Cardiovascular Surgery, West-German Heart and Vascular Center Essen, University Duisburg-Essen, Essen, Germany
- 2
Department of Cardiology, West-German Heart and Vascular Center Essen, University Duisburg-Essen, Essen, Germany
- 3
Department of Radiology, West-German Heart and Vascular Center Essen, University Duisburg-Essen, Essen, Germany
- 4
Translational Imaging Center, MRI Core, Houston Methodist Research Institute, Houston, TX, USA
BACKGROUND AND AIM: Distal stent graft induced new entry (dSINE) is an early or late complication after frozen elephant trunk (FET) procedure. The purpose of this study was to identify the hemodynamic profile of the aorta before dSINE development using computational fluid dynamics (CFD) simulations.
METHOD: Between 2006 and 2022, 30 patients with FET operation for aortic dissection were retrospectively included in this CFD study. Of those, 15 patients had developed a dSINE after FET procedure (dSINE group) and 15 patients had no further vascular events after the initial operation (control group). Patient-specific 3D surface models of the aortic lumen were reconstructed from computed tomography angiographic datasets. Steady-state CFD simulations with laminar blood flow and zero pressure outlet conditions were performed. For both groups, velocity magnitudes, wall shear stresses (WSS) and vorticity were evaluated and compared at different locations of the aorta including the level of the stent graft (SG), the distal landing zone of the SG and the more distal aorta.
RESULTS: In the dSINE group, WSS was significantly elevated distal to the SG compared to WSS in the SG itself and at its landing zone (2.84 ± 1.57 Pa vs. 1.56 ± 0.71 Pa and 2.00 ± 0.81 Pa, p < 0.001 and p = 0.002, respectively). In the control group, WSS was not significantly elevated distal to the SG in comparison to other locations. Regarding vorticity, the same pattern of a significant elevation distally to the SG compared to within the SG and at its landing zone was seen in the dSINE group but not in the control group.
CONCLUSIONS: Increased WSS and vorticity values distal to the SG compared to within the SG and at its landing zone seem to be associated with dSINE development after FET. CFD can be a useful tool to understand SG-induced hemodynamic changes within the aorta in the early and late follow-up CTA studies after FET predicting complications.
1.20.2. Unsupervised Classification of CFD Velocity Differentials in Frozen Elephant Trunk Aortic Geometries
- 1
Translational Imaging Center, Houston Methodist Research Institute, Houston, TX, USA
- 2
Department of Thoracic and Cardiovascular Surgery, West-German Heart and Vascular Center Essen, University Duisburg-Essen, Essen, Germany
BACKGROUND AND AIM: To determine the relationship between aortic velocity differentials classified using the convolutional Variational Autoencoder (cVAE) algorithm with Frozen Elephant Trunk geometric variations.
METHOD: From 3D surface models derived from CTA images of seven treated Frozen Elephant trunk cases, blood velocity pattern were calculated using computational fluid dynamics. Values were converted into DICOM images from which a luminal centerline was determined. Perpendicular axial cross sectional pseudo-color images were successfully reconstructed by the cVAE. The latent 2D space was divided into four regions representing varying differentials in velocity magnitude patterns and assigned velocity differential scores (VDS) from 1–4. Aortic geometries were characterized by a maximum tortuosity aortic angle in the descending aorta below the stent graft. The precision of the cVAE classification algorithm was assessed by the standard deviation of the VDS with the repetition principle.
RESULTS: Maximum tortuosity aortic angle ranged from 17 to 84 degrees. VDS values ranged from 1.39 to 2.89. The precision of the cVAE classification algorithm was estimated by the VDS standard deviation calculated from 10,000 repetitive classifications which was less than 6.4% for 88.6% of all cross sections (n = 2023). Calculated for each case, the average VDS standard deviation for the mean VDS did not exceed 1.1%. A strong positive but not significant correlation, between the aortic angle and VDS was found (Pearson correlation coefficient 0.534, p-value = 0.217).
CONCLUSIONS: Assigning regions in latent space of the cVAE allowed for the rapid automated calculation of the VDS and determining its correlation between the tortuosity angle of the descending aorta. Deviation in aortic geometry correlated with the differentials in velocity.
1.20.3. An Overview of Aortic Surgery at a Tertiary Care Hospital in Pakistan: Our 7 Years of Experience
Muhammad Wasim Sajjad, Azam Jan, Muhammad Zaid Ali and Rashid Qayyum
Department of Cardiothoracic & Vascular Surgery, Rehman medical institute, Peshawar, Pakistan
BACKGROUND AND AIM: Aorta can be involved in different pathologies including congenital, syndromic and acquired disorders which may need intervention in any form to prevent disasters. The purpose of this study was reviewing types of aortic pathologies treated surgically and its outcomes.
METHOD: The retrospective review of data collected in a database was conducted at tertiary care hospital from January 2017 to December 2023. A total of 115 patients operated for different diseases of aorta in a single centre over a period of 7 years were included. Institutional review board approval was granted. Data was analyzed using SPSS 25, variables were recorded in frequency & mean ± SD.
RESULTS: The mean age measured 44.9 ± 18.3 years. Most patients were male (83.4%). Hypertension was most common co-morbidity (41.7%). NYHA-III (36.5%) & CCS-II (41.8%) were common severity of presenting complaints. Majority of cases were elective (82%) & without cardio pulmonary bypass (CPB) (52.1%). The most commonly performed procedure was coarctation of the aorta repair (31.3%), aortic root and ascending aorta replacement (30.4%) followed by abdominal aortic aneurysm (6.9%) and aorto-femoral grafting (5.2%) with an in-hospital mortality of 0%, 11.4%, 0% and 33.3% respectively. A few patients (12.7%) had prolonged ventilation with a mean ventilation of 19.9 ± 22.0 h. Total of 65.8% required post-operative blood or blood product transfusion. Mean ICU stay was 56.16 ± 44.0 h. The overall In-hospital mortality was 11.3%. Patients undergoing on- pump procedures had 18.2% where as those under going off-pump procedures had 5% in hospital mortality. Total patients diagnosed with aortic dissection had higher mortality of 33.3%. The exclusive cause of mortality in ARR was dissection.
CONCLUSIONS: Aortic pathology frequently manifests in various anatomical locations, both in elective and emergency scenarios. While surgical intervention can be successful, it is associated with a higher mortality rate especially in emergency cases. Presence of dissection is a major risk factor.
1.20.4. Sustained Long-Term Results Rates in Patients with Frozen Elephant Trunk Operated for Acute Aortic Syndromes
Panteleimon Theodoros Tsipas 1, Filippos Paschalis Rorris 2, Konstantinos Papakonstantinou 2, Ilias Gissis 2, Dimitrios Dougenis 3 and John Kokotsakis 2
- 1
Department of Cardiac Surgery, 401 General Army Hospital, Athens, Greece
- 2
Department of Cardiac Surgery, Evangelismos General Hospital, Athens, Greece
- 3
Medical School, National & Kapodestrian University of Athens, Athens, Greece
BACKGROUND AND AIM: Currently, the FET technique is indicated in acute aortic syndromes in the latest European guidelines. Although the FET operation is associated with significant morbidity and mortality, it often offers a curative option for diseases of the aortic arch and descending thoracic aorta, which is evident by the high rates of downstream of the re-intervention free survival in large series. We sought to report on our single institutional experience using the aforementioned technique in patients with acute aortic syndromes operated on an urgent setting.
METHOD: 23 adult patients who were referred to our department for surgical management of acute aortic syndromes and underwent aortic arch replacement using the frozen elephant trunk (FET) technique between November 2010 and January 2024. The primary outcome was long-term survival. Secondary outcomes were 30-day mortality rate and the incidence of neurologic complications i.e., stroke and spinal cord ischemia.
RESULTS: Mean patient age was 57.1 (±12.5) years and the majority (20 patients—87%) were male. The most common indication was Stanford type A acute aortic dissection (aTAAD) in 17 (74%) patients, followed by non-A non-B dissection in 2 (8.7%) patients, penetrating aortic ulcer (PAU) of the aortic arch in 2 (8.7%) patients, type A intramural hematoma (IMH) in 1 (4.3%) patient and blunt thoracic aortic injury of the aortic arch in 1 (4.3%) patient. Hospital mortality was 22% (5 patients). Mean follow-up was 11 years. Kaplan-Meier survival analysis revealed a 73% survival at 12 months which persisted up to 11 years of follow up. The stroke rate was 12% (3 patients) and the need for re-intervention was 12% (3 patients required completion TEVAR due to type Ib endoleak)
CONCLUSIONS: The FET technique, when is indicated, provides a reasonable and permanent solution for surgical management of patients suffering from acute aortic syndromes.
1.20.5. Chronicle of the Chronobiological Cycles and Climate Dynamics in the Presentation of Aortic Dissections
Kirthiga Thiagarajan and Jayaprakash K N
Institute of Cardiovascular and Thoracic Surgery, Madras Medical College and Rajiv Gandhi Government General Hospital, Chennai, Tamil Nadu, India
BACKGROUND AND AIM: Aortic dissection, separation of the aortic media by an internal tear caused by pulsatile blood, is one of the most common catastrophes involving the aorta. Chronobiological rhythms and patterns have been known to influence various biological and disease processes in the body, especially pertaining to the cardiovascular system. Patterns affecting the frequencies of presentation of aortic dissections have also been observed by changes in a region’s climatic condition, typically temperature, pressure and broadly based on the time of year. This study aims to draw a parallel between the possible correlations of the body’s inherent chronobiological rhythms and the atmosphere’s climatic dynamics on the presentation of aortic dissection.
METHOD: The frequencies of patients presenting with symptomatic aortic dissection were analyzed over a period of ten years, from admission records and compared against the time of day, time of year and lunar phases present at time of presentation to the hospital in a single tertiary care center.
RESULTS: It was noted that majority of the cases of aortic dissection happened to present to our hospital during the late afternoon and early evening, however having typically developed symptoms in the morning. A spike of cases was noted in the winter months, with the majority of recorded cases being in January-February. A nadir in the number of cases was met in summer.
CONCLUSIONS: The presentation of acute aortic dissection exhibited significant preponderance to a particular time of day and year, with significant seasonal variation, correlating to atmospheric pressure and lunar phases of that time in question. Understanding this pattern will help in understanding the mechanics and triggers that initiate an aortic dissection and also in the long run help in developing a predictive model for earlier diagnosis of aortic dissection and early plan of treatment in this acute emergency, hence improving disease prevention and patient specialized care.
1.20.6. Putting the Funk in the Trunk: High Risk ReDo Aortic Arch Replacement with Bi-Carotid Artery Bypass Grafting and Frozen Elephant Trunk Procedure
- 1
Centre of Cardiac Surgery, Pauls Stradins Clinical University Hospital, Riga, Latvia
- 2
Department of Vascular Surgery, Pauls Stradins Clinical University Hospital, Riga, Latvia
We describe a patient with a difficult aortic lesion involving carotid arteries, ascending and descending aorta, and aortic arch.
The patient was a 70-year-old male with a residual aortic dissection in the aortic arch and the descending aorta. He had suffered a Stanford type A aortic dissection on 5 January 2018, and underwent an emergency surgery the same day limited to ascending aorta replacement with a tubular graft above the sinus level with separate replacement of aortic valve. Remaining dissected ascending aorta and arch were gradually dilating reaching 7 cm before the repeat surgery.
The redo surgery begun with a vascular surgeon creating a bicaroid bypass with a Y-graft synthetic prosthesis. Simultaneously, cardiopulmonary bypass was established through right femoral artery and vein. The patient was cooled to 28 °C before a median sternotomy was performed and adhesions separated as the remaining aorta was extremely close to the backside of sternum. Ascending aorta was cross-clamped and cardioplegia infused through the aortic root. Subsequently, aortic arch was debranched, distally aorta was resected up to the site before left subclavian artery at which level antegrade implantation of a Medtronic Valiant stent-graft was performed to descending aorta. Ascending aorta was replaced, starting from the previous prosthesis proximally till the newly implanted stent-graft. Finally, the bicarotid shunt prosthesis was attached to the aortic prosthesis and left subclavian artery bypassed using a 10 mm graft. Total cardiopulmonary bypass time was 293 min, aortic cross-clamp 147 min, and circulatory arrest time with ACP 76 min.
The patient had an uneventful postoperative recovery and was discharged on 22nd postoperative day. At 3-month follow-up MS-CT showed an excellent postoperative result, demonstrating total exclusion of the aneurysm and thrombosed perigraft space around the FET prosthesis.
This case represents a successful high risk redo procedure on a patient with residual aortic dissection.
1.20.7. Total Aort Replacement of the Pediatric Patient with Loeys-Dietz Syndrome
- 1
Department of Cardiovascular Surgery, Kocaeli University, Kocaeli, Turkey
- 2
Department of Pediatric Cardiology, Kocaeli University, Kocaeli, Turkey
- 3
Department of Anesthesia and Reanimation, Kocaeli University, Kocaeli, Turkey
- 4
Department of Pediatric Cardiology, Kocaeli City Hospital, Kocaeli, Turkey
Loeys-Dietz syndrome (LDS) is a rare connective tissue disease that can lead to aortic aneurysm and dissection. The disease is caused by mutations in transforming growth factor-β receptors, estimated at less than 1 in 100,000.
We present a 15-year-old male patient whose treatment began with DeBakey Type I aortic dissection (AD) originating from the aortic root and the surgical management of all aortic pathologies.
The patient applied to the emergency department with the complaint of sudden onset of chest pain. The patient was diagnosed with Loeys-Dietz syndrome (TGFBR1 c.599C > A (p. Thr200Lys)) and had a history of aortic root dilatation and aortic valve surgery four years ago. The examinations in the emergency department were compatible with AD. Ascending aorta and total aortic arch replacement with elephant trunk procedure was performed. Approximately two months later, the patient underwent thoracoabdominal aortic graft replacement due to an aneurysm in the descending aorta. No complications besides distension in the gastrointestinal system were detected during the follow-up. Two years later, aneurysmatic dilatation developed in the coronary arteries, and the patient was operated on for the fourth time, and coronary artery aneurysm repair was performed using the Cabrol technique.
Literature data suggest that timely prophylactic aortic surgery to prevent catastrophic vascular complications can modify the aggressive natural history of LDS. Valve replacement may also be preferred in suitable patients. The prevalence of aortic reintervention is significantly higher in LDS patients presenting with aortic dissection. Therefore, total arch or root replacement may be justified in the initial AD repair. Surgeries for aortic annulus dilatation and aortic valve performed in the early stages serve as a reference for future surgical strategies. However, lifelong follow-up of these patients is necessary.
The experience gained from this case contributes to the management of the rare LDS patient who presented with AD.
1.20.8. Acute Aortic Dissection in Pregnancy, a Challenging Case Scenario
Alifa Sabir, Tauqeer Akbar, Zahid Amin, Zainab Farid, Yasira Abbasi, Wajiha Arshad
Rawalpindi Institute of Cardiology, Rawalpindi, Pakistan
Acute aortic dissection is a rare life-threatening condition in pregnancy, which may prove fatal to both mother and the fetus. It has an incidence of 0.0004% in all pregnancies and 0.4% in all aortic dissections.
Case summary: We present the case of a 25-year-old female with gestational amenorrhea of 24 weeks who presented with sudden onset chest pain and dyspnea. Echocardiography was done which showed dilated aortic root with dissection flap in root and ascending aorta. CT aortogram showed dissection flap extending from aortic root down to descending aorta just before it’s bifurcation into iliac arteries. Acute Stanford type A dissection was diagnosed. Ultrasonography showed alive fetus at 24 weeks of gestation. Multidisciplinary team meeting was conducted and patient was planned for surgery. Cardiac obstetrician was taken on board. Ascending aortic replacement with interposition tube graft was done. CPB was established through femoral cannulation and cross clamp applied. Retrograde cardioplegia was given and diseased aorta resected. Dissected layers of aorta were buttressed together using teflon sheet and ascending aorta was replaced by an interposition graft, saving the native valve. Per, operatively, ultrasonography was repeated which confirmed fetal well being. Trans esophageal echocardiography done which showed trace to mild AR. Post operatively, patient was managed for hypertension and had an uneventful recovery and was discharged with OPD follow up on 10th POD.
DISCUSSION: Aortic dissection in pregnancy is relatively rare, which makes it difficult to determine detailed guidelines for the diagnosis and management. Treatment algorithm usually revolves around saving two lives. Current strategies prefer using warmer temperatures, avoiding circulatory arrest, minimizing CPB time and maintaining high flow rates and mean arterial pressures.
Conclusions: Early diagnosis and multidisciplinary management improve outcomes significantly.
1.29. INTERDISCIPLINARY » Miscellaneous
1.29.1. Approach to Tumors Associated with the Inferior Vena Cava from a Cardiovascular Surgeon Perspective
Nazlı Melis Coşkun Yücel 1, Ahmet Aydın 1, Timuçin Sabuncu 1, Şafak Alpat 1, Mustafa Sertaç Yazıcı 2, Mesut Altan 2, Bülent Akdoğan 2 and Mustafa Yılmaz 1
- 1
Department of Cardiovascular Surgery, Hacettepe University, Ankara, Turkey
- 2
Department of Urology, Hacettepe University, Ankara, Turkey
BACKGROUND AND AIM: Tumors involving or invazive to the inferior vena cava (IVC) are generally related to the genitourinary or gastrointestinal systems. In our hospital, collaboration of cardiovascular surgery in addition to general surgery, obstetrics and gynecology, and urology has increased the resectability rates of these tumors.
METHOD: A retrospective analysis was conducted on 20 patients who underwent surgery with an interdisciplinary approach between 2014 and 2024.
RESULTS: Between 2014 and 2024, we applied interdisciplinary surgical procedures to 20 cases of inferior vena cava tumors at our clinic. Among these patients, 3 (15%) were female, 17 (85%) were male, with an average age of 39 years (range: 18–69). Pathological diagnoses included 12 germ cell tumors, 3 renal cell carcinomas, 2 leiomyosarcomas, 1 ureteral carcinoma, 1 Ewing sarcoma, 1 desmoplastic tumor. Procedures performed included IVC ligation after tumor excision in 2 patients, graft interposition in 2 patients, bovine pericardium patch plasty in 1 patient, and primary repair of the IVC in 10 patients. In 2 patients, the mass was excised but no procedure was performed on the infiltrated IVC. One patient was considered unresectable due to widespread metastasis. In one patient, CPB support was used due to intracardiac extension, and in another patient, due to IVC clamp intolerance. There were no cases of early mortality among the patients.
CONCLUSIONS: In cases of tumors invading vascular structures such as the inferior vena cava, requesting consultation with cardiovascular surgery and establishing interdisciplinary collaboration can increase the resectability rates of tumors and reduce recurrence rates. CPB support can be used in tumors with intracardiac extension to ensure the patient’s hemodynamic stability and reduce blood loss. During tumor surgery, when surgical intervention on the inferior vena cava is necessary, the primary goal should be to restore blood flow by reconstructing the vessel. However, in patients with good collateral circulation and no blood flow from the distal end, ligation and excision of the inferior vena cava may reduce the risk of recurrence.
1.29.2. Engineered Polymeric Nanoparticles for Vascular Drug Delivery
Pier Francesco Ferrari 1,2, Chiara Bufalini 1, Roberta Campardelli 1,2, Giovanni Pratesi 2,3,4, Patrizia Perego 1,2 and Domenico Palombo 2,3,4
- 1
Department of Civil, Chemical and Environmental Engineering, University of Genoa, Genoa, Italy
- 2
Research Center for Biologically Inspired Engineering in Vascular Medicine and Longevity, University of Genoa, Genoa, Italy
- 3
Department of Surgical and Integrated Diagnostic Sciences, University of Genoa, Italy
- 4
Vascular and Endovascular Surgery Unit, IRCCS Ospedale Policlinico San Martino, Genoa, Italy
BACKGROUND AND AIM: Considered the morbidity and mortality of arterial occlusive diseases, the research of a novel therapy for the initial stages of atherosclerosis could significantly improve the surgical approach. Currently, there is no pharmacological treatment capable of inducing the resolution of plaque in its early stages. In this context, vascular drug delivery will provide innovative solutions for the therapy of early-stage atherosclerotic plaques. Here, an engineered polymeric nanosystem is proposed with the aim of encapsulating bioactive molecules.
METHOD: Polymeric nanoparticles (PNPs) were prepared via double emulsion solvent evaporation method for the encapsulation of therapeutic monoclonal antibodies (mAbs). The conjugation of PNPs with immunouteroglobin-1 (IUG-1) was achieved through a coupling reaction. PNPs were characterized in terms of morphology and particle size distribution. Moreover, the release of mAb, the capability of antigen recognition, and the biocompatibility were studied.
RESULTS: PNPs were successfully prepared and exhibited mean diameters of 225.6 nm, slightly increased after IUG-1 conjugation. As therapeutics, PNPs showed a sustained release of the encapsulated mAbs over time. PNPs presented good compatibility with macrophages, endothelial, and red blood cells.
CONCLUSIONS: Therefore, the studied PNPs represent a promising therapeutic tool with the potential to significantly impact on the pharmacological treatment of early-stage atherosclerotic plaque.
1.29.3. Dynamite Plots in Cardiothoracic and Vascular Surgery Research: A Machine-Learning Meta-Study of over 9000 Original Research Articles over Ten Years
- 1
School of Medicine, Anglia Ruskin University, Chelmsford, UK
- 2
Independent Researcher, Canterbury, UK
BACKGROUND AND AIM: Dynamite plots are bar charts of numerical data: they are a misleading and ineffective method of visualizing data. They alter the perception of the mean’s position through the “within-the-bar” bias, whilst obscuring the underlying data distribution. Consequently, they offer no more information than mean ± standard deviation within the text. Box, violin, and scatter plots are widely understood—although no one plot is always right for every situation, there is always a better alternative to a dynamite plot.
Prior to our study, there was no data on the use of dynamite plots in cardiothoracic or vascular surgery research.
Our aim is to demonstrate the frequency that dynamite plots are used in cardiothoracic and vascular surgery research and understand the trend of their use over a 10-year period.
METHOD: Original research articles in the fields of cardiothoracic and vascular surgery were selected from the PMC open access dataset based on MeSH terms. These were retrieved using the biblio-glutton-harvester Python tool. 9799 articles were analysed using Barzooka, a convolutional neural network tool. These results were statistically adjusted based on previous validation data with 95% confidence bounds. The Kendall tau coefficient with the Mann-Kendall test for significance was used to assess the trend of dynamite plot use over a 10-year period.
RESULTS: In 2012, for original research articles plotting univariate numerical data, based on the statistically adjusted data, approximately 74% of cardiothoracic articles and 79% of vascular articles used dynamite plots. This decreased to approximately 46% in both fields by 2022. Both showed a statistically significant (p < 0.001) downward trend, as signified by negative tau values.
CONCLUSIONS: The use of dynamite plots in vascular and cardiothoracic surgical research has decreased over time. Despite this, use remains alarmingly high, and thus much more must be done to educate surgical researchers on effective data visualization and communication.
1.29.4. Celox as a Novel Topical Haemostatic Agent in Cardiac Surgery: A Prospective Cohort Study
Navneet Singh and Parma Nand
Department of Cardiothoracic Surgery, Auckland City Hospital, Auckland, New Zealand
BACKGROUND AND AIM: Celox is a sterile low-cost topical haemostatic agent which is derived from a natural sugar called chitosan. Celox has been used successfully in military warzones for haemostasis of large battle wounds. There are only two in-human case reports published on Celox use in cardiac surgery. However, at our centre, we have been using Celox in cardiac surgery since 2019. We hence aimed to carry out a retrospective review of our Celox cases.
METHOD: A retrospective analysis of prospectively-collected data was performed on all patients receiving Celox intraoperatively during cardiac surgery at our unit from 2019 to 2022.
RESULTS: There were 96 cases which utilised Celox across the 3-year study period. The majority of cases (63%) were of acute or emergency status, with 39% of cases being aortic dissection repairs. 52% of patients were on anticoagulants at the time of operation. Across the operative caseload, the mean bypass time was 4 h with 25% of patients ending up on VA-ECMO intraoperatively. On average, 15 units of various blood products were transfused in each case. Postoperatively, the mean mediastinal drain output in the first 24 h in ICU was 381 mL. Only 2% of patients had a takeback to theatre for review of ongoing bleeding.
CONCLUSIONS: This is the largest report of Celox use in cardiac surgery. In our experience with sick coagulopathic patients undergoing complex long operations, Celox was associated with cessation of bleeding and correlated with satisfactory postoperative drain outputs. In particular, Celox is useful in surgically-challenging situations, such as trying to address bleeding from an inaccessible posterior aortotomy suture line.
1.29.5. Thromboembolic Complications, Thrombosis Marker and Prognosis in Patients with COVID-19
Tetiana Danilevych, Yuriy Mostovoy and Lesya Rasputina
Department of propedeutic of internal medicine, National Pirogov Memorial Medical University, Vinnytsya, Ukraine
BACKGROUND AND AIM: The literature describes different threshold levels of thrombosis markers associated with the prognosis patients with severe COVID-19. Aim-to assess the prevalence of thromboembolic complications in patients with severe COVID-19, the association between D-dimer levels and patient survival.
METHOD: 221 patients (groups of survivors 133 (60.2%) and dead patients 88 (39.8%), p = 0.02), who were in the intensive care unit due to severe COVID-19, were included in the study. The period of hospitalization was 18.9 ± 9.13 vs. 9.14 ± 7.21 days, p < 0.001.
Died patients were older (68.22 ± 11.50 vs. 61.38 ± 12.96 years), more often had hypertension (73 (83.0%) vs. 90 (67.7%), CHD (83 (94.3%) vs. 91 (68.4%)), had a stroke (15 (17.0%) vs. 11 (8.2%)), kidney diseases (18 (20.5%) vs. 13 (9.8%), p = 0.022), oncological diseases—(8 (6.0%) vs. 12 (13.6%), all p < 0.05.
RESULTS: Mortality in this cohort of the patients was 88/221 × 100% = 39.8%. Conditions associated with thrombosis in dead and survivors groups were stroke (10 (11.4%) vs. 3 (2.3%), p = 0.006), pulmonary embolism (9 (10.2%) vs. 3 (2.3%), p = 0.014), atrial fibrillation (AF) (31 (35.2%) vs. 19 (14.3%), p = 0.0001), thrombophlebitis (14 (15.9%) vs. 15 (11.3%), p > 0.05), acute myocardial infarction (3 (3.4%) vs. 2 (1.5%), p > 0.05).
The mean value of D-dimer (9.83 ± 22.85 vs. 1.21 ± 1.76 µg, 0.005) in the group of dead patients was higher than in the survivors. Using the cluster analysis method, the threshold value of D-dimer was determined as 0.775 μg. Survival of patients with D-dimer levels > 0.775 μg was lower vs. in patients with levels ≤ 0.775 μg, Long-Rank p = 0.0001.
CONCLUSIONS: The patients who died from COVID-19 more often had pulmonary embolism, AF, stroke. The D-dimer level > 0.775 μg can be considered as the risk marker of in-hospital mortality in patients with severe COVID-19.
1.29.6. Beyond Traditional Metrics: Exploring Novel Biomarkers for Early Detection of Acute Kidney Injury in Coronary Artery Bypass Graft Surgery
Senem Sakar, Jasmin Ben Khaled, Wolfgang Ristau, Abdelhadi Kerrad, Belal Darwish, Stephan Knipp, Markus Kammler and Matthias Thielmann
Department of Thoracic and Cardiovascular Surgery, West-German Heart and Vascular Center, University Hospital Essen, Essen, Germany
BACKGROUND AND AIM: Acute kidney injury (AKI) following coronary artery bypass grafting (CABG) affects up to 30% of patients with significant impact on short- and long-term outcomes. Novel biomarkers such as TIMP-2*IGFBP-7 and proenkephalin have been proposed for early and accurate detection of AKI enabling prompt and preventive measures.
METHOD: This single-center study evaluated the predictive accuracy of TIMP-2*IGFBP-7 and Proenkephalin for AKI in CABG patients, using KDIGO criteria as the primary endpoint. Levels of TIMP-2*IGFBP-7 in urine and Proenkephalin in plasma were compared between AKI and non-AKI patients and compared with conventional indicators of AKI, such as serum creatinine, eGFR, and urinary output.
RESULTS: Thirty-six consecutive patients undergoing CABG were studied. Out of these, 12 patients showed elevated postoperative TIMP-2*IGFBP-7 levels with 1.32 ± 3.16 in AKI vs. 0.09 ± 2.63 ng/mL2/1000 in non-AKI (p < 0.001); 95% CI: 1.01–20.79; Sensitivity/Specificity: 0.38/0.66 and 12 patients showed increased Proenkephalin levels with 100.4 ± 26.75 vs. 59.4 ± 17.82 pmol/L (p < 0.0001); 95% CI: 92.63–131.60; Sensitivity/Sensitivity 0.63/0.74. At 24 h postoperatively, 20 patients had elevated TIMP-2*IGFBP-7 with 0.77 ± 1.9 vs. 0.09 ± 2.16 ng/mL2/1000 (p < 0.001); 95% CI: −1.10–11.57; Sensitivity/Specificity: 0.86/0.33, while Proenkephalin increased in 14 patients with 104.9 ± 56.62 vs. 61.65 ± 25.51 pmol/L (p < 0.001); 95% CI: 96.11–163.13; Sensitivity/Specificity: 0.75/0.6. Proenkephalin and TIMP-2*IGFBP-7 levels showed AUCs of 0.65 postoperatively and 0.69 and 0.62 at 24 h after CABG.
CONCLUSIONS: The study shows a significant link between elevated postoperative levels of TIMP-2*IGFBP-7 and Proenkephalin and AKI in CABG patients, suggesting their potential for early AKI prediction within 24 h post-surgery. However, further validation of clinical utility is needed.
1.29.7. Design and Validation of a Novel High-Performance Bioreactor for Engineered Vascular Scaffolds
Jan Oscar Pralits 1, Pier Francesco Ferrari 1,2, Leslie Neil Sierad 3, Fatemeh Ahmadpoor 1, Giovanni Pratesi 2,4, Patrizia Perego 1,2 and Domenico Palombo 2,4
- 1
Department of Civil, Chemical and Environmental Engineering, University of Genoa, Genoa, Italy
- 2
IRCCS Ospedale Policlinico San Martino, Genoa, Italy
- 3
Aptus Bioreactors LLC, Clemson, SC, USA
- 4
Department of Surgical and Integrated Diagnostic Sciences, University of Genoa, Genoa, Italy
BACKGROUND AND AIM: The manufacturing of biodegradable, bioabsorbable, and bioactive small-diameter vascular scaffolds (VSs) represents the ultimate goal of vascular tissue engineering. Despite significant research progress in this field, no biodegradable and bioabsorbable vs. has been approved for clinics to date. Various attempts to validate the next-generation VSs in 2D models have been reported, but all of them suffer from limitations. The development of bioreactors that can reproduce the complexity of the 3D vascular system is still a challenge. Here, a high-performance bioreactor (HPB) is proposed for validating VSs.
METHOD: The proposed HPB is based on peristaltic pump technology, combined with a system of tubing, reservoirs, and valves that mimic the complexity of the cardiovascular system. The HPB was connected to a computer with dedicated software that provided precise control of the pump. VSs were successfully fabricated by electrospinning using a solution of poly(caprolactone) and poly(glycerol sebacate), in the presence of quercetin. The resulting vs. had a diameter of 5 mm and was coated with gelatin before testing in the HPB.
RESULTS: A versatile HPB was successfully set up and all the data generated during the experimentation were digitally collected. The tested electrospun vs. showed good patency. The different pressure regimes had a significant impact on the release of both gelatin and quercetin. The amount of released quercetin was adequate to modulate the inflammatory process. The vs. mechanical properties were not adversely affected by the applied pressure regimes. Analytical evaluation of the wall shear stresses provided an in-depth understanding of the correlation between the mechanical forces and the release of biomolecules from VSs in HPB.
CONCLUSIONS: The successful implementation of the HPB had a positive impact on the validation of vs. in a cardiovascular-like environment. All the properties exhibited by vs. at the end of the experimentation confirmed the feasibility of planning preliminary in vivo experiments.
1.29.8. Two Peas in a Pod: Combined Abdominal Aortic Aneurysm Repair and Coronary Artery Bypass Grafting
Hina Inam and Zia Ur Rehman
Aga Khan University Hospital, Karachi, Pakistan
INTRODUCTION: Coronary artery disease (CAD) and abdominal aortic aneurysms (AAA) frequently coexist, presenting complex challenges for treatment. Myocardial infarction contributes to approximately half of all postoperative fatalities subsequent to AAA repair. The combination of two significant surgeries within a private-sector hospital presents numerous hurdles. While isolated CABG entails a mortality rate of 2–3%, elective AAA repair carries a comparable rate of 2.2%. There’s a prevailing belief that simultaneous execution of these procedures will lead to a cumulative rise in mortality. Coexisting AAA and severe CAD present a highly morbid cohort, amplifying the risks associated with individual procedures.
Case Description: We present a case of a 73-year-old male with right-sided abdominal pain, revealing an 8.9 × 9.3 cm juxta renal AAA extending to the bifurcation, concurrent with significant CAD, including left main plus three-vessel disease.
Treatment Strategy: Considering the high mortality risk associated with staged procedures, we opted for a one-stage approach, performing simultaneous AAA repair and coronary artery bypass grafting (CABG).
Surgical Approach: The surgical strategy involved careful planning to minimize complications, including retaining arterial and venous cannulae during both procedures for hemodynamic control.
Postoperative Management: Postoperatively, the patient was successfully extubated, managed for atrial fibrillation episodes, and monitored for renal complications.
Recovery and Outcomes: Despite the absence of bowel sounds initially, the patient’s recovery progressed well, emphasizing the importance of postoperative management in such cases.
CONCLUSIONS: Our experience supports the efficacy of a one-stage approach, offering streamlined recovery and resource optimization. This case highlights the significance of tailored treatment strategies and multidisciplinary collaboration in managing complex cardiovascular conditions.
1.32. VASCULAR AND ENDOVASCULAR » Abdominal Aorta
1.32.1. Simultaneous Treatment of Two Aortic Pathologies: The TAVR-EVAR Project
Areti Vassiliou, Giwrgos Fanariotis, Michail Peroulis and Vangelis G. Alexiou
Vascular Surgery Unit, General Surgery Department, University Hospital of Ioannina, Ioannina, Greece
BACKGROUND AND AIM: We aim to investigate the feasibility and advantages of the use of endovascular techniques to simultaneously treat two different aortic pathologies.
METHOD: Case report
A man 79 years old was referred to our cardiology clinic after an episode of mild dyspnea and chest pain. His medical history included past smoking, hypertension and angioplasty of the LAD. The TTE showed severe aortic stenosis with concomitant insufficiency, LVEF 60% without any akinesias but with concentric hypertrophy of the left ventricle.
The CT angiogram revealed severe aortic stenosis, and the presence of an infrarenal fusiform AAA (52 mm 51 mm). We also performed a coronary angiography that did not show any stenosis of the coronary arteries and no residual stenosis of the LAD.
Even though the surgical risk was acceptable our Heart team decided to opt for an endovascular approach for this patient. Under general anesthesia, with bilateral femoral cutdown, a 18 French sheath was carefully placed at the right femoral artery and during rapid pacing a 23-mm device was easily advanced and deployed under fluoroscopy. Consequently a Gore Excluder bifurcated main body endoprosthesis was positioned within the AAA through the common right femoral artery with a leg extension in the right common iliac artery. An additional contralateral leg extension was implanted into the left common iliac artery.
RESULTS: The patient had an excellent recovery and was discharged 3 days after surgery with single antiplatelet therapy.
CONCLUSIONS: As we obtain access for large sheaths to repair the aortic stenosis it is preferred the simultaneous procedure as repeated vascular access is a known predictor of vascular complications. Apart from that it is known that the haemodynamic instability that follows a TAVR procedure is a risk factor for AAA rupture.
In conclusion, with careful assessment and the help of a multidisciplinary team the simultaneous procedure is a feasible choice and may reduce the complication rates of such procedures.
Keywords: Aortic stenosis, Abdominal aneurysm, simultaneous treatment, advantages, endovascular techniques
1.32.2. Composition of the Surgical Team in Open Surgery for Abdominal Aortic Aneurysm: A Risk Factor Analysis
Gabriele Piffaretti 1, Alessandro Zammito 1, Marco Franchin 1, Nicola Rivolta 1, Luca Guzzetti 2, Gabriele Selmo 2, Simone Binda 2 and Matteo Tozzi2
- 1
Vascular Surgery—Department of Medicine and Surgery, University of Insubria, Varese, Italy
- 2
Anesthesia and Palliative Care, Department of Emergency and Trauma System, ASST Settelaghi University Hospital, Varese, Italy
BACKGROUND AND AIM: The aim of this study was to analyze the influence of varying experiences within each surgical team to identify team-related risk factors on clinical outcomes after open surgery (OS) for abdominal aortic aneurysm (AAA).
METHOD: This is a single-center, observational cohort study with retrospective analysis of prospectively collected data. All cases of elective OS for AAA 1 January 2010 and 31 December 2022 were analyzed. Each component (surgeon and anesthesiologist) was rated according to the number of intervention performed, and a surgical team’s score was calculated (operating surgeon + assisting surgeon + anesthesiologist = team score) by relying on each member’s experience. Primary outcome was survival at 30 days and in follow-up, and a composite outcome of mortality and major complication. Secondary outcome was freedom from aorta-related reintervention.
RESULTS: We analyzed 103 patients: 97 (94.2%) males and 6 (5.8%) females. The mean age was 76 ± 8 years (range, 55–93). The best possible team composition was present in 52 (50.5%) surgeries. There was no difference among teams in major complications (17.3% vs. 21.6%; OR: 0.4, p = 0.622). No death was observed at 30 days in patients operated by the best team; however, mortality (0% vs. 5.9%; OR: 3.1, p = 0.118), and composite outcome (11.5% vs. 17.6%; OR: 0.8, p = 0.416) was not different between teams. Aorta-related reintervention was lower in the best team (5.8% vs. 17.6%; OR: 3.5, p = 0.072). Cox regression analysis identified the best team as a protective factor (HR: 0.2; 95% CI: 0.06–0.88, p = 0.032) for reintervention (HR: 3.7; 95% CI: 0.99–13.97, p = 0.051).
CONCLUSIONS: Open surgery for AAA is equally safe in different teams. However, there is a positive impact of the experience of the surgical-anesthesiologic team on freedom from aorta-related reintervention.
1.32.3. Single-Center Mid-Term Experience with E-Liac Branched Device from Artivion®
Ozan Yazar 1, Stefanie Willems 1, Niek Zonnebeld 1, Pieter Salemans 1, Chunyu Wong 1 and Lee Bouwman 2
- 1
Department of Vascular and Endovascular Surgery, Zuyderland Medical Center, Heerlen, The Netherlands.
- 2
Faculty of Science and Engineering, Maastricht University, Maastricht, The Netherlands
BACKGROUND AND AIM: The use of iliac branch device (IBD) is increasing due to the less invasive character and accumulated experience of physicians in these techniques. Clinical data regarding the E-Liac stent-graft from Artivion®, however, are scarce. This study shows the mid-term outcomes of the E-Liac stent graft from a large single centre.
METHOD: Patients treated with IBD for (aorto-)iliac aneurysms between September 2015 and December 2022 with follow-up in our centre were included. (Post)operative (technical success, reintervention, 30-day mortality) and mid-term outcomes (endoleak, reintervention, hypogastric patency, mortality) were analysed.
RESULTS: Sixty-three patients (60 male, median age 70 years (IQR 66–76)) were treated with 82 E-Liac stent grafts for aorto-iliac aneurysms with a median follow-up of 38 months (IQR 22–51). The technical success rate was 95%. 97.6% of the interal iliac artery remained patent during follow-up. No 30-day mortality was encountered and there were no reinterventions. During follow-up one patient had an endoleak type Ib of both hypogastric arteries, however the patient refused additional interventions. One other patient had a type II endoleak with contained rupture. Due to severe comorbidities the patient was treated palliatively. One (1.6%) IBD-related reintervention was performed with relining of the stent-graft. Primary patency of the hypogastric branch was 95.1% and the mortality was 25.4% during follow-up.
CONCLUSIONS: This study shows high technical success rates for the E-Liac stent graft, with corresponding good mid-term outcomes. The E-Liac stent-graft is a feasible, safe and effective stent-graft in the treatment of aorto-iliac aneurysms.
1.32.4. Semi-Branched iBEVAR for Treatment of Aortic Aneurysms: Novel Feature in Stent-Graft Configuration
Ozan Yazar, Pieter Salemans, Chunyu Wong and Lee Bouwman
Department of Vascular and Endovascular Surgery, Zuyderland Medical Center, Heerlen, The Netherlands
BACKGROUND AND AIM: With the change of treatment paradigm for abdominal aortic aneurysms endovascular techniques are advancing. Fenestrated EVAR (FEVAR) and branched EVAR (BEVAR) are used for complex aortic aneurysm repair. Both FEVAR and BEVAR have their own unique advantages and disadvantages. Semi-branched stent-graft configuration are a new feature that attempts to combine the advantages of both FEVAR and BEVAR.
METHOD: A case series of patients with an abdominal aortic aneurysm (AAA), who underwent a semi-branched iBEVAR (Artivion®) procedure between July till September 2023 were analyzed. Primary outcomes were technical success, perioperative complications, and target vessel patency. Secondary outcomes were type I or III endoleak and 30-day aneurysm related mortality.
RESULTS: Three patients (female, n = 2) with a mean age of 75 years (range, 66–85 years) underwent a semi-branched iBEVAR procedure for the treatment of an abdominal aortic aneurysm (AAA). Two cases needed 4 vessel stent-graft configurations, and one case needed a two-vessel stent-graft configuration. Mean aneurysm diameter was 54 mm (range, 51–58 mm). One case was a failed EVAR case with a type Ia endoleak which needed a repair. Intraoperative technical success was 100%. No perioperative complications were revealed. All patients received a computer tomography (CT) angiogram 30 days postoperatively, which showed 100% target vessel patency, with no type I or III endoleak. There was no aneurysm-related mortality.
CONCLUSIONS: In short-term follow-up, the novel feature of semi-branches iBEVAR in endovascular aortic treatment for AAA appears to be a safe and effective treatment.
1.32.5. The Results of the Treatment of the Gunshot Wounds of the Main Vessels
Yuliia Nahaliuk, Volodymyr Rogovskyi and Borys Koval
National Military Medical Clinical Centre, Kyiv, Ukraine
BACKGROUND AND AIM: The aim of this study is to analyse the results of treatment and clinical outcomes in patients with injuries of the main vessels of the lower extremities in the period of 2014–2024.
METHOD: We have analysed 51 cases of gunshot wounds of the main vessels of the lower extremities who have undergone treatment at our medical facility from 2014 to 2024.
RESULTS: There was performed 513 operations in 51 patients; 77 (15%) of them—on the main vessels, 14 (2.7%)—amputations and re-amputations, 422 (82.2%)—other.
Analysing the results of treatment in 38 cases (74.5%) there was identified satisfactory result and in 13 (25.5%)—the treatment resulted in amputation.
Among patients under 20 years old there was 1 (7.7%) who underwent amputation, among patients from 21 to 30 years old—7 (53.8%), among patients from 31 to 40 years old—3 (21.1%), among patients from 41 to 50 years old—2 (15.4%) individuals accordingly.
CONCLUSIONS: Gunshot wounds of the main vessels remain controversial and sophisticated area of the vascular surgery both, in therapeutic and organisational ways. Taking into account a significant part and severity of the gunshot wounds of the vessels, the main task for medical professionals today is the creation of the clear algorithm of the effective medical assistance to all patients on the stage of medical evacuation directed at rescue of life from acute bleeding, saving of the extremity, treatment of complications and outcomes of the vascular injury, and foundation of the system of the specialized surgical assistance and rehabilitation in the corresponding referral centres.
1.32.6. The Introduction of the PRP-Technology to Improve the Long-Term Consequences and Outcomes of the Treatment of the Injuries of the Main Vessels of the Lower and Upper Extremities
Yuliia Nahaliuk, Volodymyr Rogovskyi, Borys Koval and Yurryi Sivash
National Military Medical Clinical Centre, Kyiv, Ukraine
BACKGROUND AND AIM: The aim of this study is to analyse the results of treatment and clinical outcomes in patients with injuries of the main vessels of the lower and upper extremities and implement of the PRP-technology to improve the long-term consequences and outcomes of the treatment of the injuries of the main vessels of the lower and upper extremities.
METHOD: We have analysed 51 cases of gunshot wounds of the main vessels who have undergone treatment at our medical facility from 2014 to 2024. In 7% of these cases, we have used PRP-technology in the area of the proximal and distal anastomosis, the area of the vascular suture.
RESULTS: During the environmental protection in eastern Ukraine was recorded 545 cases of the gunshot wounds of the main vessels. In our stude we included 51 cases. There was performed 513 operations in 51 patients; 77 (15%) of them—on the main vessels, 14 (2.7%)—amputations and re-amputations, 422 (82.2%)—other. Analysing the results of treatment in 38 cases (74.5%) there was identified satisfactory result and in 13 (25.5%)—the treatment resulted in amputation. Gunshot wounds are a complex field of medicine, given the previously obtained results, it was important for us to improve the results and consequences, reduce the number of unsatisfactory results.
CONCLUSIONS: Platelet-rich plasma (PRP) injections are gaining popularity for a variety of conditions, from sports injuries to hair loss. The treatment uses a patient’s own blood cells to accelerate healing in a specific area. PRP treatment can help support wound healing in trauma. Because the treatments use a patient’s own tissues, PRP injections are safe and can be administered alone or used in conjunction with other procedures.
1.32.7. The Experience of the Treatment of the Early and Long-Term Consequences and Complications of the Gunshot Wounds of the Main Vessels
Yuliia Nahaliuk, Volodymyr Rogovskyi and Borys Koval
National Military Medical Clinical Centre, Kyiv, Ukraine
BACKGROUND AND AIM: Gunshot wounds (GSW) of the main vessels remain relevant and sophisticated sphere of vascular surgery both, in therapeutic and organizational way. The purpose of the study is to analyse the character of the injuries, localization, concomitant trauma, results of treatment of the early and long-term consequences and complications and clinical outcomes in patients with injuries of the main vessels of the extremities.
METHOD: There were analysed 743 cases of GSW of the main vessels of the lower and upper extremities. The inclusion criteria were military servicemen of the Armed Forces of Ukraine; patients who required intervention on the main vessels; males.
RESULTS: During the war in Ukraine was recorded 743 cases of the gunshot wounds of the main vessels. The damage of the artery in 46.5%; in 11.1%—damage of the vein; in 42.4%—both. Among all injuries, 88.2% were combat injuries, and 11.8%—non-combat. The localisation of the GSW was the following: 76.5% of the injuries were in femoropopliteal area, 21.6%—peroneal area, 1.9%—both. The injuries that accompanied the trauma of the main vessels included: bone injury (37.3%), bone and nerve injury (25.5%), nerve injury (23.5%), isolated soft tissue injury (13.7%). The injury of both lower or upper extremities occurred in 25.5%, organs of thoracic cavity in 3.9%, organs of abdominal cavity—in 3.9%, head and neck injury—in 2%, injury of 3 and more anatomical areas—in 17.6%, isolated trauma—in 47.1%. There were performed 7052 surgeries: 15% on the main vessels, 2.7% amputations and re-amputations, 82.3%—others. In 85.6% we identified satisfactory result, in 12.7%—the treatment resulted in amputation, in 1.7%—lethal
CONCLUSIONS: It is necessary to create thorough algorithm of specialized treatment of patients with described type of trauma in high-qualified medical institutions and rehabilitation centres.
1.32.8. Impact of Stent-Graft Complexity on the Outcome of Treatment Complex Abdominal Aortic Aneurysms Repair: A Systematic Review and Meta-Analysis
Ozan Yazar 1, Buland Tiwana 2, Jean Daemen 1, Marion Heymans 1, Barend Mees 2 and Geert Willem Schurink 2
- 1
Department of Vascular and Endovascular Surgery, Zuyderland Medical Center, Heerlen, The Netherlands
- 2
Department of Vascular and Endovascular Surgery, Maastricht University Medical Center, Maastricht, The Netherlands
BACKGROUND AND AIM: The aim of the present study was to reveal a relationship between increased stent-graft complexity and clinical outcomes. We summarize the available data from studies comparing stent-grafts with only renal-fenestrations (renal-FEVAR) to stent-grafts with additional fenestrations/branches for the mesenteric arteries (complex-F/BEVAR) in the treatment of pararenal aortic aneurysms (PAA) and type IV TAAA.
METHOD: A systematic review and meta-analysis of studies focusing on results of patients treated with renal-FEVAR and comparing with complex-F/BEVAR in treatment of PAA and type IV TAAA was performed following the PRISMA guideline. PubMed, EMBASE, the Cochrane Library and Web of Science were searched for studies till mid-May-2022. Primary outcomes were technical success, perioperative reinterventions, in-hospital mortality, and reintervention for endoleak type I or type III during follow-up. Secondary outcomes were target vessel patency, myocardial infarction, bowel/limb ischemia, acute renal failure, stroke or TIA, SCI, length of hospitalization, long-term survival, and reintervention.
RESULTS: The search yielded a total of 7149 studies. After screening, eleven studies with 2167 patients (758 renal-FEVAR, 1409 complex-F/BEVAR) were included for analysis. Meta-analysis demonstrated no significant difference in technical success between the renal-group and complex-group (OR: 1.90, 95% CI 0.75–4.77, p = 0.17). No significant difference (p = 0.57) was observed in reinterventions between the two groups. The all-cause mortality rate during hospital-stay was twice as high for the complex-group (4.2% [n = 36/860]) compared to the renal-group (2.1% [n = 14/660]), however without statistical difference (p = 0.23). Reinterventions for type I and III endoleaks were not significantly different between the two groups, p = 0.23. No significant difference was revealed between the two groups regarding secondary outcomes.
CONCLUSIONS: This systematic review revealed no significant difference in mortality, complications, or reintervention between renal-FEVAR and complex-F/BEVAR. The results may suggest a more liberal approach in proximal additional fenestrations or branches. However, renal-FEVAR in juxta-renal aneurysms remains a safe and effective treatment option with no higher risk on type Ia endoleak or reinterventions during follow-up compared to complex-F/BEVAR.
1.32.9. Vascular Endothelial Growth Factor (VEGF) but Not Interleukin-6 (IL-6) Is Found in Higher Concentrations in the Excluded Aneurysm Sac of Patients with Type II Endoleak—A Pilot Study
- 1
Royal Prince Alfred Hospital, Sydney, NSW, Australia
- 2
Heart Research Institute (HRI), Newtown, NSW, Australia
- 3
The University of Sydney, Sydney, NSW, Australia
BACKGROUND AND AIM: Type II endoleak (T2EL) causes expansion of an abdominal aortic aneurysm (AAA) sac after endovascular repair (EVAR) and can behave like arteriovenous malformations (AVM) after intervention. Vascular endothelial growth factor (VEGF) and interleukin-6 (IL6) are relevant in AVM pathogenesis. The aim of this pilot study was to investigate whether the excluded AAA sac is a source of VEGF and IL6 that may contribute to the development of T2EL following EVAR.
METHOD: Eligible patients were 18–95 years old and belonged to one of:
Group A: Previous EVAR with T2EL with sac enlargement requiring intervention
Group B: Peripheral arterial disease undergoing endovascular intervention without AAA or T2EL (control)
Group C: Primary EVAR (control)
Three blood samples (arterial, venous +/− aneurysm sac) were collected per patient. Patients in Group B had a second arterial sample from the site of endovascular intervention in the absence of aneurysmal disease. ELISA was used to determine VEGF & IL-6 concentration.
RESULTS: Out of 29 patients, 83% were male. Mean age = 73 yo. Mean VEGF concentration was higher in the excluded AAA sac of patients with a T2EL compared with both control groups (Group A: 62 pg/mL vs. Group B: 23 pg/mL vs. Group C: 19 pg/mL) approaching statistical significance. IL6 concentrations did not differ between groups.
CONCLUSIONS: This pilot study to assess feasibility found higher concentrations of VEGF in the excluded AAA sac of patients with a T2EL when compared with those without. Further research is needed to better characterise the relationship between VEGF levels and T2EL development and whether this represents a potential treatment avenue for T2EL.
1.32.10. Age-Based Stratification and Its Impact on Clinical Presentation and Mortality in Patients with Ruptured Abdominal Aortic Aneurysm
David Matejevic, Ivan Tomic, Miroslav Markovic, Milos Sladojevic, Ranko Trailovic, Perica Mutavdzic, Andrija Roganovic, Ognjen Kostic and Lazar Davidovic
Clinic for Vascular and Endovascular Surgery, University Clinical Center of Serbia, Belgrade, Serbia
BACKGROUND AND AIM: The aim of this study was to assess the difference in clinical presentation, laboratory parameters and risk of fatal outcome in patients with ruptured abdominal aortic aneurysm (RAAA) in different age groups.
METHOD: A single-center, retrospective cohort study with prospectively collected data between 2009–2019 was performed. Total of 702 consecutive patients with RAAA were included in the study. Patients were stratified based on their age in 5 groups. Clinical presentation, laboratory parameters and mortality were assessed.
RESULTS: Patients in older age groups were significantly more likely to expirience a collapse (p = 0.003), and were more likely to have been admitted in unconscious (p = 0.025) and hypovolemic shock state (p = 0.002), with significantly lower levels of measured systolic (p < 0.001) and diastolic (p < 0.001) blood pressure. Laboratory analyses showed lower values of hemoglobin (p < 0.001) and platelets (p < 0.001), and higher creatinine values (p < 0.001) in older age groups. Values of urea (p = 0.414) and leukocytes (p = 0.307) showed no significant difference. Overall mortality was 34.9%. Mortality was significantly different between the groups: group of patients of 41–50 years had 0% mortality, patients 51–60 years 23.8%, patients 61–70 years 21.8%, patients 71–80 years 39.1%, and the oldest patients (81–90 years) had 72.6% mortality (chi-square 90.49, p < 0.001). Univariant logistic regression showed 2.27 times higher chance of lethal outcome for every 10-year age increase (OR 2.27, 95% CI 1.86–2.77, p < 0.001).
CONCLUSIONS: The age of patients with RAAA presents an important predictive factor of worse clinical presentation and fatal outcome, with higher age indicating an overall frailty and carrying a higher risk of mortality.
1.32.11. Screening Men and Women Above the Age of 50 Years for Abdominal Aortic Aneurysm
Ognjen Kostic 1, Aleksa Jovanovic 2, Andrija Roganovic 1, David Matejevic 1, Fedor Filipovic 1, Nikola Brankovic 3, Igor Koncar 2 and Lazar Davidovic 1
- 1
Clinic for Vascular and Endovascular Surgery, Serbian Clinical Center, Belgrade, Serbia
- 2
Medical Faculty, University of Belgrade, Belgrade, Serbia
- 3
General Hospital Kruševac, Kruševac, Serbia
BACKGROUND AND AIM: A pilot screening project for abdominal aortic aneurysm (AAA) was conducted in seven cities in Serbia in 2023. It aimed to explore AAA prevalence and risk factors in an upper middle-income country. Screening is recommended for males over 65, but differences in lifestyle and risk factors between countries make geographical risk stratification necessary.
METHOD: Echosonographic evaluation of the abdominal aorta was performed on the participants who also filled in a questionnaire with demographic and clinical information. Differences in distribution of participants in regards to aneurysm presence were explored using the chi square test, with values of p < 0.05 denoting statistical significance.
RESULTS: A total of 6126 participants (49% male and 51% female), have responded to the screening campaign. An aneurysm was found in 287 screened individuals (4.61%), In males 50–64, prevalence of AAA was 4.65%. The highest prevalence in males was in the group 65–69 (9.48%), while in female group 75+ it was 3.2%. Male sex, older age, family history (16.83% in male patient), smoker (12.48%), ex smoker (9.89%), overweight, and alcohol consumption were predictors of AAA in the univariate analysis.
CONCLUSIONS: The prevalence of AAA is not reduced in all countries, and screening strategies might be changed based on local epidemiological data. In a country with high rate of smokers screening might be considered for males > 50.
1.32.12. Different Strategies in Treatment Patients with Abdominal Aortic Aneurysm and Coronary Disease
Andrija Zoran Roganović 1, David Matejević 1, Ognjen Kostić 1, Aleksandar Mitrović 1, Nabil Alhayek 2, Almas Ahmemulić 2, Igor Koncar 1,2 and Lazar Davidovic 1
- 1
Clinic for Vascular and Endovascular Surgery, Belgrade, Serbia
- 2
Faculty of Medicine, University of Belgrade, Belgrade, Serbia
BACKGROUND AND AIM: Patients with aortic aneurysms have associated coronary artery disease. When planning surgical treatment, there is a dilemma as to which problem to solve primarily. Aim of the study was to show different strategies in the treatment of these patients.
METHOD: Retrospectively, 100 patients with abdominal aortic aneurysm treated in high-volume aortic center from 2019–2024 with positive findings on preoperative coronary angiography were selected. Based on the findings, patients were selected for primary interventional cardiology or cardiosurgical treatment or primary vascular reconstruction (OPEN or ENDO). The following groups are patients who were advised to undergo cardiac treatment after a vascular-surgical procedure. The last group consisted of patients who were prescribed conservative therapy. We analyzed cardiac, non-cardiac complications and mortality.
RESULTS: The degree of specific cardiac complications (angina, ECG findings, heart attack) was significantly higher in the groups of patients who first underwent vascular treatment (8.3% and 7.14% vs. 4.5%). Among non-cardiological complications, the development of neurological events was significantly higher in patients who were primarily vascular-surgically treated (EVAR 6.6%, OPEN 5.5%). The frequency of transient renal failure as well as pulmonary complications was similar in all groups except for patients who initially received PCI procedures in which no such complications were recorded (CABG nephro/pulmonary 3.25%, EVAR nephron 2.25%, OPEN nephro 2.2%). Finally, in the group of patients who first underwent cardiac treatment oe EVAR no deaths were recorded, while one patient died after open-surgical treatment (2.7%).
CONCLUSIONS: The presence of coronary disease is a risk factor for patients with aortic aneurysm, and the primary resolution of coronary disease led to a reduced degree of postoperative specific cardiological complications with no difference among other complications and mortality.
1.32.13. Percutaneous Endovascular Repair of Abdominal Aortic Aneurysms: A Single-Center Experience
Alexandros Barbatis 1, Konstantinos Batzalexis 1, Konstantinos Spanos 1, Konstantinos Tzimkas Dakis 1, George Kouvelos 1, Metaxia Bareka 2, Eleni Arnaoutoglou 2 and Miltiadis Matsagkas 1
- 1
Vascular Surgery Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
- 2
Anesthsiology Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
BACKGROUND AND AIM: Recently, percutaneous endovascular abdominal aortic aneurysm repair (pEVAR) has gained its role in abdominal aortic aneurysm (AAA) treatment. The aim of the study is to report the increase of pEVAR in a tertiary center through years and its impact on clinical outcome.
METHOD: A single-center, observational, retrospective study of prospectively collected data was conducted. All patients who underwent elective pEVAR (using the Proglide device) and EVAR with femoral cutdown access between 2017 and 2024 were included 2017–2019 early pEVAR experience (253 patients); 2020–2024 late experience (340 patients). Baseline characteristics, intra- and peri-operative data were collected. The main outcomes measured were the rate of pEVAR application, the need for blood transfusion and hospital stay.
RESULTS: A total of 593 patients were treated by endovascular means (20.5% pEVAR vs. 79.5% EVAR). Mean age was similar between groups (pEVAR 72.8 ± 4.5 vs. EVAR 72.3 ± 7; p = 0.68). The mean number of Proglide closure devices used for right and left access was 232 and 205 respectively. There was no difference in terms of type of anaesthesia [pEVAR: local 7% and 93% general anaesthesia (GA) vs. EVAR: local 9% and 91% GA, p = 0.38]. The mean operation time was lower for pEVAR (111 ± 40) vs. EVAR 129 ± 45 (p = 0.000), while the need for transfusion was similar between groups [pEVAR: 20/122 (16.4%) vs. EVAR: 70/434 (16%) p = 0.65]. The average hospital stay was significantly lower for patients who underwent pEVAR (1.35 ± 0.8) vs. EVAR 3.23 ± 2 (p = 0.000). Only 1 death occurred in EVAR group. In the initial period pEVAR was used only in 10% of cases, while it was increased significantly in the later experience to 28.2%.
CONCLUSIONS: pEVAR is a growing trend in the treatment of AAA, and compared with femoral cutdown access, it can be considered safe and effective, reducing the operation time and hospital stay.
1.32.14. Durability of a Second-Generation Balloon-Expandable Covered Stentgraft in Patients Treated with Fenestrated, Branched and Chimney Endovascular Aortic Aneurysm Repair
Konstantinos Tzimkas Dakis, Konstantinos Spanos, George Kouvelos, Christos Karathanos, Konstantinos Batzalexis, Miltiadis Matsagkas and Athanasios D. Giannoukas
Vascular Surgery Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
BACKGROUND AND AIM: Covered stent-grafts constitute an essential component of fenestrated (fEVAR), branched (bEVAR) and chimney (chEVAR) endovascular repair. Target vessel (TV) instability events may lead to technical and clinical failure. We present the mid-term outcomes of the second generation of BeGraft (Bentley InnoMed, Hechingen, Germany) balloon-expandable covered stentgraft (BXCS) as an “off-the-shelf” platform used in complex endovascular repair.
METHOD: This is a retrospective analysis of prospectively collected data from a single-tertiary center. All consecutive patients treated for juxtarenal, pararenal and thoracoabdominal (TAAA) aortic aneurysms during a 7-year time period (May 2016–May 2023) either by fEVAR, bEVAR or chEVAR in whom BeGraft BXCS were implanted, were included. Outcomes were defined as primary patency rates for each TV at maximum follow-up and were reported using Kaplan-Meier life tables.
RESULTS: Begraft stentgrafts were deployed in 111 patients (males: 95%, age: 70.9 ± 6.1 years old) who underwent complex endovascular repair [chEVAR: 53 (47.7%), fEVAR: 22 (19.8%), bEVAR: 35 (31.5%), f/bEVAR combination: 1 (0.9%)]. Aneurysm type included 36 (32.4%) juxtarenal, 44 (39.6%) pararenal, 16 (14.4%) type IV TAAA, six (5.4%) type III TAAA and nine (8.1%) type II TAAA. Mean maximum aneurysm diameter was 6.7 ± 1.8 cm. A total of 307 BeGrafts were deployed [Celiac Trunk (CT): 47 (15.3%), Superior Mesenteric Artery (SMA): 70 (22.8%), Right Renal Artery (RRA): 95 (30.9%), Left Renal Artery (LRA): 95 (30.9%) for the revascularization of 286 TV. Mean follow-up was 12.7 ± 12.2 months. The primary patency rate of RRA was 96% (SE: 2.1%), 94% (SE: 2.9%) and 90% (SE:4.7%) at 6, 12 and 24 months, respectively. The primary patency rate of CT was 96% (SE: 3.6%), 86% (SE: 10%) at 6 and 24 months, respectively.
CONCLUSIONS: Second generation BeGraft platform seems to be an effective and durable device for the revascularization of TV during complex endovascular repair.
1.32.15. Effectiveness of Intraoperational Fusion Navigation Technique for Complex Endovascular Procedures on Abdominal Aorta
Petr M. Lepilin, Timur E. Imaev, Alexander S. Kolegaev, Dmitrij V. Salichkin, Ivan V. Kuchin and Renat S. Akchurin
Department of Cardiovascular Surgery, National Medical Research Centre of Cardiology Named After Acad. E.I.Chazov, Moscow, Russia
BACKGROUND AND AIM: To assess the role of image fusion technique in possible reduction of contrast volume, radiation dose, and fluoroscopy and procedure times in complex (fenestrated/branched) endovascular aorta aneurysm repair procedures (FEVAR, BEVAR). According to actual recommendations for radiation safety (2023), 3D (MSCT)-2D (DSA) fusion navigation techniques can reduce the contrast volume, radiation dose and procedure time in standard EVAR procedures. Aim of our study was to determine the effect of fusion navigation with preoperative planning, marking of target vessels and planning of C-arm position for cannulation of each mesenteric brunch.
METHOD: Data on 60 patients satisfying the study inclusion criteria were added from the authors’ center. two groups of patients were formed in retrospective analysis of EVAR procedures and fenestrated/branched endografting procedures. All complex procedures were divided in several stages with separate assessment of effectiveness of fusion navigation for every mesenteric/renal artery cannulation/stenting/endografting. Basic calculation index for complex procedures was created, connected to volume and number of angiographic stages.
RESULTS: For standard EVAR, contrast volume and procedure time showed significant reduction of contrast usage mean to 25 mL (mean two angiograms) with same time of procedures (difference less than 7 min) respectively. For complex EVAR group, image fusion technique was connected with significant reduction in procedure contrast volume (mean − 81 mL, fluoroscopy time (less more than 17 min), and also total procedure time (less more than 31 min). The results of our study confirms that image fusion technology can reduce contrast volume, fluoroscopy time, and procedure time in “gold standard” EVAR procedures more than 20 percent, but can show the best effectiveness on complex FEVAR/BEVAR procedures.
CONCLUSIONS: Effective use of preplanned angles for canulation, use of reference images with fusion navigation option can significantly reduce the potential negative effects of radiation/contrast usage in complex FEVAR/BEVAR procedures.
1.32.16. Covered Endovacular Reconstruction of Iliac Bifurcation (CERIB Technique); Short-Term and 1-Year Outcomes
Konstantinos Spanos 1, Athanasios Chaidoulis 1, Konstantinos Tzimkas Dakis 1, George Kouvelos 1, Dimitra Papaspyrou 2, Eleni Arnaoutoglou 2, Athanasios D. Giannoukas 1 and Miltiadis Matsagkas 1
- 1
Vascular Surgery Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
- 2
Anesthsiology Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
BACKGROUND AND AIM: Successful distal zone seal with internal iliac artery salvage is crucial during EVAR. The aim of this study is to present 1-year outcomes of the CERIB technique, an “off-the-shelf” endovascular option for distal landing zone seal at the external iliac artery (EIA), while maintaining blood flow to the IIA.
METHOD: This is a single center, retrospective analysis of prospectively collected data of patients undergoing EVAR for intact AAA or previous failed-EVAR (December 2022–March 2024). Primary outcomes included technical success and primary patency at maximum follow-up. Secondary outcomes were endoleak rate (EL) associated with the iliac reconstruction and reintervention rate.
RESULTS: A total of 25 patients (96% males, mean age: 72 ± 7.1 years old) with 31 iliac bifurcations treated were included. Treatment indications included a CIA aneurysm (67.7%—21/31 iliac bifurcations), short-CIA (16.1%—5/31), narrow lumen CIA (9.6%—3/31) and EL Ib (6.4%—2/31). Aortic platforms deployed included the COOK Alpha (9 limbs), GORE C3 (6 limbs), MEDTRONIC Endurant IIS (7 limbs), ENDOLOGIX Ovation Alto (1 limb), ARTIVION E-tegra (3 limbs) and the COOK T-branch platform (5 limbs). Technical success rate was 100%. Primary patency rate at 30-days (31/31 iliac bifurcations), 6-months (22/22) and 1-year (11/11) was 100%. No death was reported for all patients at maximum follow-up. CERIB related EL rate was 3% (1/31 iliac bifurcations), with one case of gutter EL. Reintervention rate was 6.4% (2/31) during the follow-up; including one case of proximal stent extension and relining due to gutter EL and one case of EIA relining due to an asymptomatic stenosis.
CONCLUSIONS: CERIB technique showed excellent short-term and 1-year outcomes in terms of freedom from endoleak and patency rates. CERIB technique may be used as an alternative to iliac branch devices for IIA salvage during EVAR. Long-term surveillance is warranted.
1.32.17. Long-Term Outcomes of Complex Abdominal Aortic Aneurysms Treated Using the Chimney Technique
Konstantinos Tzimkas Dakis 1, Konstantinos Spanos 1, George Kouvelos 1, Konstantinos Batzalexis 1, Metaxia Bareka 2, Eleni Arnaoutoglou 2, Athanasios D. Giannoukas 1 and Miltiadis Matsagkas 1
- 1
Vascular Surgery Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
- 2
Anesthsiology Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Greece
BACKGROUND AND AIM: The chimney endovascular aortic repair (ChEVAR) technique is an established endovascular option for complex AAA treatment. We present the long-term outcomes of the ChEVAR technique for the treatment of complex AAA in a single tertiary center.
METHOD: This is a retrospective analysis of prospectively collected data. All patients undergoing ChEVAR for juxta-, para-, and supra-renal AAA in a single-tertiary center during an 8-year time-period (March 2016–March 2024) were included. Primary outcomes were overall survival, primary patency of TV and freedom from type Ia endoleak (EL Ia) and were reported using Kaplan-Meier life tables.
RESULTS: A total of 74 patients (males: 95.9%, mean age: 72 ± 6.8 years old) underwent single (24.3%—18/74), double (37.8%—28/74) or triple (35.1%—26/74) ChEVAR were included. Aneurysm type included 29 juxtarenal (39.1%), 39 pararenal (52.7%), and six suprarenal (8.1%) AAA, while mean aneurysm diameter was 7.1 ± 2 cm. A total of 153 TV were implemented, including 60 (39.2%) right renal arteries, 65 (42.4%) left renal arteries, and 28 (18.3%) superior mesenteric arteries. Mean follow-up was 32 months (1–84 months). Overall survival rates at 1, 2, 3 and 5 years was 76.3%, 73.3%, 69.3%, and 47.7%, respectively. Primary TV patency rates at 2 and 5 years was 98.7%, and 92.5%, respectively. Freedom from EL Ia rates at 1 and 4 years was 96.7%, and 87.5%, respectively. A total of six aneurysm-related reinterventions were carried out: one case of a custom-made device deployment for EL Ia treatment, three cases of limb extension for EL Ib, and two cases of TV relining.
CONCLUSIONS: ChEVAR technique offers good mid- and long-term outcomes in terms of TV patency and freedom from endoleak type Ia. ChEVAR seems to be effective and durable during the long-term period, while survival rate of those patients might highlight the need for patients’ selection.
1.32.18. Outcomes of Fenestrated and Branched Endovascular Aneurysm Repair with an Inverted Contralateral Limb
Emiel Wietze Melle Huistra, Ignace F.J. Tielliu, Jean Paul P.M. De Vries and Clark J. Zeebregts
Department of Surgery, Division of Vascular Surgery, University Medical Center Groningen, Groningen, The Netherlands
BACKGROUND AND AIM: To report technical success and evaluate clinical outcomes of fenestrated and branched endovascular aortic repair (F/B-EVAR) incorporating a contralateral inverted limb.
METHOD: Patients who underwent F/B-EVAR with a custom-made bifurcated device containing an inverted limb between January 2010 and September 2023 were retrospectively analysed. All aneurysms had a short renal artery to bifurcation distance, either following previous aortic repair or without prior repair. Time-to-event data were analysed using the Kaplan-Meier method.
RESULTS: A total of 32 patients (26 men; mean age 77 ± 6.2 years) were included in the analysis. Technical success was achieved in 28 patients (87.5%). Two technical failures resulted from misplaced contralateral limbs in patients with previous endovascular aortic repair (EVAR), necessitating one open conversion and one femoro-femoral crossover bypass. Additionally, two technical failures were attributed to a type 3c endoleak and a type 1c endoleak. One patient (3.1%) died <30 days post-operatively due to a subdural haemorrhage. Estimated patient survival after 1 and 2 years was 92.7% ± 5.1%, and 74.3% ± 10.1%, respectively. No aneurysm-related deaths were observed. During the median follow-up of 13 months, two (6.3%) inverted limbs occluded and were treated with a femoro-femoral crossover bypass. One target vessel (right renal artery) occluded (0.9%), resulting in a permanent, significantly reduced renal function. Freedom from overall reintervention after 1 and 2 years was 73.5% ± 8.0% and 68.3% ± 9.0%, respectively. There were no junctional problems between the inverted limb device and the main endograft, and no significant correlation was found between the one-sealing-stent inverted limb device design and the onset of type 3 endoleak (log-rank p = 0.10).
CONCLUSIONS: F/B-EVAR incorporating a contralateral inverted limb can be performed with acceptable technical success and satisfactory outcomes. Extra caution should be paid to prevent damage to the renal stents. Carefully confirming correct cannulation of the inverted limb is warranted, particularly in patients with prior EVAR.
1.32.19. Effects of Preemptive Embolisation of Side Branches on Preventing Type 2 Endoleaks After EVAR
Eren Karpuzoglu, Naci Cem Aydogdu and Recep Caliskan
Cardiovascular Surgery of Siyami Ersek Research and Training Hopsital, University of Health Sciences, Istanbul, Turkey
BACKGROUND AND AIM: EVAR has become the mainstay treatment method for abdominal aortic aneurysm (AAA). Type 2 Endoleaks (T2EL), sac filling due to side branches from the aneurysm sac, remains a controversial problem. Typically a benign condition, T2EL requires close follow-up and potentially leads to complications. We aim to see whether preemptive embolization in the same session with EVAR helps to prevent T2ELs.
METHOD: Seventy-seven patients who underwent elective EVAR for AAA between January 2018–December 2023 were included in the study. Two patients with complex interventions including TEVAR and surgical debranching were excluded. Group 1 consists of 20 patients who were embolized preemptively with EVAR, Group 2 consists of 55 patients who had EVAR solely. Both groups had follow-up CTA scans at the 1st and 6th month for sac growth and/or endoleak.
RESULTS: A total of 20 patients with 27 side branches were embolized. Fourteen Internal iliac arteries (IIA), 9 inferior mesenteric arteries (IMA), and 4 accessory renal arteries (aRA) were embolized. Chimney EVAR (ChEVAR) was performed in 5 patients. T2EL was detected in 2 patients in Group 1 (10%), and 15 patients in Group 2 (26%). Five patients were treated for sac progression due to T2EL, all of them are from Group 2 (9%). Two patients with T2EL in Group 1 were self-limited with a benign course and no sac progressions were seen.
CONCLUSIONS: Our results revealed a lower incidence of aneurysm sac growth, T2EL, and secondary interventions with preemptive embolization compared to no embolization. These results were consistent with the contemporary literature. However, these results do not alter the overall mortality rates. The feasibility of preemptive embolization versus secondary embolization in terms of morbidity, radiation exposure for both patients and interventionalists and, cost-effectiveness should be investigated in further multi-center studies.
Preemptive embolization could potentially improve long-term outcomes and reduce the frequency of surveillance.
1.32.20. Three-Dimensional Geometric Analysis of Viabahn VBX Bridging Stent Grafts in Fenestrated End-Vascular Aortic Repair: A Multicenter, Retrospective Cohort Study
Fatima Fouad 1, Ben R. Saleem 1, Ignace F.j. Tielliu 1, Matteo A. Pegorer 2, Raffaello Bellosta 2, Davide Esposito 3, Aaron T. Fargion 3, Clark J. Zeebregts 1, Jean Paul P.m. De Vries 1 and Richte C.l. Schuurmann 1
- 1
Department of Surgery, Division of Vascular Surgery, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands
- 2
Department of Vascular Surgery, Poliambulanza Foundation Hospital, Brescia, Italy
- 3
Department of Vascular Surgery, Careggi University Teaching Hospital, University of Florence School of Medicine, Florence, Italy
BACKGROUND AND AIM: The primary aim of this study was to assess the 3-dimensional flare geometry of the Gore Viabahn VBX balloon-expandable covered stent (BECS) after fenestrated endovascular aortic aneurysm repair (FEVAR) and to determine and visualize BECS-associated complications.
METHOD: This multicentre retrospective study included patients who underwent FEVAR between 2018 and 2022 in three vascular centres. Patients with at least one visceral artery treated with the VBX and with availability of two post-FEVAR computed tomography angiography (CTA) scans (follow-up [FU 1: 0–6 months; FU2: 9–24 months]) were included. The flare geometry of the VBX, including flare-to-fenestration distance, flare-to-fenestration diameter ratio, flare angle, and apposition with the target artery were assessed using a vascular workstation and dedicated CTA applied software.
RESULTS: In total, 90 VBX BECS were analysed in 43 FEVAR patients. The median CTA follow-up for FU1 and FU2 was 35 days (IQR, 29–51 days) and 14 months (IQR, 13–15 months), respectively. The mean flare-to-fenestration distance was 5.6 ± 2.0 mm on FU1 and remained unchanged at 5.7 ± 2.0 mm on FU2 (p = 0.417). The flare-to-fenestration diameter ratio was 1.19 ± 0.17 on FU1 and remained unchanged at 1.21 ± 0.19 (p = 0.206). The mean apposition length was 18.6 ± 5.3 mm on FU1 and remained 18.6 ± 5.3 mm (p = 0.550). The flare angle was 31° ± 15° on FU1 and changed to 33° ± 16° (p = 0.009). On FU1, the BECS-associated complication rate was 1% and the BECS associated reintervention rate was 0%. On FU2, the BECS-associated complication rate was 3% and the BECS associated reintervention rate was 1%.
CONCLUSIONS: The flare geometry of the VBX bridging stent did not change significantly during 14 months follow-up. Three-dimensional geometric analysis of the flare may contribute to identify the origin of endoleaks and occlusions.
1.32.21. Isolated Left Internal Iliac Artery Mycotic Aneurysm Presented as a Large Retroperitoneal Hematoma
Mohamed Shafi Mahboob Ali
Department of General Surgery, Advanced Medical and Dental Institute (AMDI), Penang, Malaysia
INTRODUCTION: Mycotic aneurysm is very rare in the new era of antibiotics. Commonest micro-organism that is associated with this pathology is Salmonella species. The predilection of salmonella species for the arterial wall is due to the pre-existing atherosclerotic plaques or ulcerations that disturbed the intimal layer of the vessel.
METHODOLOGY: With the discoveries of endovascular stents the mortality from open surgery has went down. There were cases reported where these endovascular stents been infected and resulting in severe complications and ultimately needs removal.
RESULTS: A 55 years old gentleman was referred to our center with the complaint of progressive left lower abdominal pain and swelling, fever with weakness of left lower limb. Blood culture grew salmonella species and patient was started on intravenous Cefoperazone. Clinically there was a pulsatile swelling (15 × 15) cm at the left side of the abdomen. CT angiography showed a left internal iliac artery aneurysm sized (6.5 × 4.0) cm with internal thrombus. Retroperitoneal hematoma was evacuated, necrotic tissues debrided and the left common iliac vessel ligated. Histopathology showed fragments of cellular debris with fibro-collagenous tissue and moderate infiltrations by lympho-plasma cells.
DISCUSSION: Mycotic aneurysm is a focal dilatation of a blood vessel due to salmonella species. Expansile swelling with pulsation and a positive blood culture is diagnostic. Laboratory findings are leukocytosis, elevated C-reactive proteins, ESR and neutrophil counts. CT-tomography is the choice of imaging that is used in diagnosing a mycotic aneurysm.
1.32.22. FEVAR of Juxtarenal Abdominal Aortic Aneurysm with Coexisting Horseshoe Kidney
Almahdi Ali and Stephan Langer
Vascular Surgery Department, Marien-Hospital Witten, Witten, Germany
Case Presentation: A 62-year-old asymptomatic patient was referred for further evaluation due to sonographic suspicion of AAA. Arterial hypertension was a risk factor for cardiovascular disease.
B-mode sonography confirmed a partially thrombosed infrarenal AAA with a maximum diameter of about 6 cm in the “leading edge” method. Aneurysms of other arteries such as A. poplitea were excluded by duplex sonography.
A computed tomography angiography (CTA) was performed to further clarify the morphology and for preoperative planning. A juxtarenal AAA with a diameter of 63 mm was confirmed and the coexistence of a horseshoe kidney was discovered.
Diagnosis: Juxtarenal abdominal aortic aneurysm with coexisting horseshoe kidney
Procedure details: The patient had asymptomatic concomitant abdominal aortic aneurysm (AAA) and horseshoe kidney. We perform an endovascular repair of the aneurysm under general anaesthesia. After appropriate measurement of the CTA with a measurement software, we decided to avoid the open surgery for an endovascular elimination with a double fenestrated stent graft (FEVAR) with an anaconda endoprosthesis (Terumoaortic Inchinnan, Scotland, UK).
Procedure outcomes: Postoperative CTA showed proper seating of the placed implants, no evidence of endoleak and patent stents in the two renal arteries. Discharge was uncomplicated on day 4 with provision of dual antiplatelet therapy for 6 months.
Keywords: horseshoe kidney; FEVAR; juxtarenal abdominal aortic aneurysm
1.32.23. Incidental Horseshoe Kıdney in Leriche Syndrome: A Successful Surgical Treatment
Mustafa Can Sofuoğlu, Emine Turhan, Mine Demirbaş and Sefer Usta
SBU Trabzon Ahi Evren GKDC Education Hospital, Trabzon, Turkey
Leriche syndrome, known as occlusive disease of the infrarenal aorta, usually presents with claudication. Although isolated Leriche syndrome is quite common, the association with horseshoe kidney is rare. The neck of the horseshoe kidney, which usually contains a functioning, although occasionally non-functioning, parenchyma, makes abdominal aortic surgery challenging. A 56-year-old man with Leriche syndrome and horseshoe kidney underwent successful aortic surgery and horseshoe kidney separation. A median incision was used for exploration of the abdominal aorta, iliac arteries and horseshoe kidney. The neck of the horseshoe kidney was located at the infrarenal level, above the site of the cross clamp and proximal anastamosis. Separation of the horseshoe kidney neck and aortabifemoral bypass were performed. The operation and postoperative hospitalization were uneventful.
1.32.24. Hybrid Surgery for the Treatment of Thoracoabdominal Aortic Aneurysms
Qingwei Ding 1,2, Zhiwei Zhang 1, Haixiang Li 1, Feng Zhu 1, Weiye Bi 1, Hui Zheng 1, Xiaoyu Zhang 1 and Qingyou Meng 1
- 1
Department of Vascular Surgery, Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2
Department of Cardiac Surgery, University Hospital Heidelberg, Heidelberg, Germany
OBJECTIVE: To explore the efficacy of hybrid surgery in treating thoracoabdominal aortic aneurysms.
METHODS: 67 patients with thoracoabdominal aortic aneurysms treated with hybrid surgery at the Department of Vascular Surgery, Shanghai General Hospital from 2016 to 2023 were included. The surgical approach was modified through incision design, reducing anastomosis sites, utilizing improved VORTEC technique, reconstructing lumbar arteries, and deploying endovascular stents through visceral artery fenestration.
RESULTS: Among the 67 patients, there were 52 males and 15 females, with 2 cases of infective thoracoabdominal aortic aneurysms. One case was treated using antegrade hybrid technique, while 66 cases were treated using retrograde technique. 62 cases underwent one-stage stent placement, and 5 cases underwent two-stage stent placement. Complications included renal failure in 7 cases, with 6 cases improving after continuous renal replacement therapy (CRRT) and 1 case requiring permanent dialysis; intestinal necrosis in 2 cases, both treated with colectomy and subsequent reconstruction; and paraplegia in 2 cases. There were 4 deaths (1 case of pulmonary embolism, 1 case of myocardial infarction, 1 case of heart failure, and 1 case of airway hemorrhage).
CONCLUSIONS: Hybrid surgery is an effective treatment for thoracoabdominal aortic aneurysms, and modified techniques can improve patient outcomes.
1.32.25. Ruptured Abdominal Aortic Aneurysms: Surgical Treatment over the Past 6 Years
INTRODUCTION: Ruptured abdominal aortic aneurysm has an overall mortality of 30–50%. Treatment involves “open” surgery or endovascular treatment.
OBJECTIVE: To retrospectively compare the immediate, 30-day, 3-month and 6-month outcomes of patients treated with traditional ’open’ surgery or endovascular repair.
MATERIALS-METHODS: Sixty-four patients with CT-confirmed ruptured abdominal aortic aneurysm treated at Treviso Vascular Surgery, Cà Foncello Hospital, between July 2017 and July 2023 were examined.
23 patients underwent EVAR and 41 underwent open repair. 36% of patients were hemodynamically unstable on arrival (EVAR 30%, OPEN 39%) and 64% stable (EVAR 70%, OPEN 61%). 21% of EVAR procedures started under local anesthesia and 100% of OPEN repairs under general anesthesia. Overall, the primary endpoints of the study are 30 day, 3 month, and 6 month mortality, overall reintervention rate, and postoperative complications during hospital stay.
CONCLUSIONS: Overall, of the 64 patients enrolled in the study, the average aneurysm diameter at arrival was 7.6 cm (EVAR 8.5 cm, OPEN 7 cm).
The recorded intraoperative mortality was 2% (OPEN 100%), also inferring the high survival rate at 30 days with a mortality of 6% (EVAR 5%, OPEN 7%), at 3 months of 11% (EVAR 10%, OPEN 11%) and at 6 months of 12% (EVAR 15%, OPEN 11%).
The most frequently recorded postoperative complications during hospitalization are pneumonia in 16% (EVAR 11%, OPEN 5%), hypertension in 8% (OPEN 100%), need for reintervention in 6% (EVAR 2%, OPEN 5%) for bleeding or type endoleak corrections.
1.32.26. Surgical Treatment of Infective Abdominal Aortic Aneurysm
Qingwei Ding 1,2, Zhiwei Zhang 1, Haixiang Li 1, Feng Zhu 1, Weiye Bi 1, Hui Zheng 1, Xiaoyu Zhang 1, Weiye Bi 1 and Qingyou Meng 1
- 1
Department of Vascular Surgery, Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2
Department of Cardiac Surgery, University Hospital Heidelberg, Heidelberg, Germany
OBJECTIVE: To compare the outcomes of various surgical techniques for managing infective abdominal aneurysms.
METHODS: 19 patients with infective abdominal aneurysms who underwent treatment at the Department of Vascular Surgery, Shanghai General Hospital between 2021 and 2023 were included in the study.
Methods: Nineteen patients with infective abdominal aneurysms who underwent treatment at the Department of Vascular Surgery, Shanghai General Hospital between 2021 and 2023 were included in the study.
RESULTS: Among the 19 patients, 4 had primary infective abdominal aneurysms, while 15 had endograft infections. Treatment modalities included endovascular treatment in 2 cases, hybrid surgery in 2 cases, and open surgery in 15 cases. Procedures included axillo-bifemoral bypass combined with infective abdominal aneurysm resection in 2 cases, in-situ reconstruction with bovine pericardium in 1 case, omentum-wrapped artificial vessel reconstruction in 1 case, bovine pericardial wrapping and artificial vessel reconstruction in 1 case, rifampicin-bonded artificial vessel in-situ reconstruction in 3 cases, and femoral vein reconstruction of the abdominal aorta combined with infective abdominal aneurysm resection in 6 cases. Additionally, in one case, the stent was not removed, and infectious focus clearance was performed. In another case, partial stent removal was performed, followed by omentum wrapping to isolate the infectious focus. One-stage surgery was successful in 15 cases, while 4 cases resulted in fatalities. The average hospital stay was 44.2 days, with an average surgical duration of 493 min and an average blood loss of 3210.4 mL. Postoperative antibiotic usage averaged 30.6 days.
CONCLUSIONS: Femoral vein reconstruction of the abdominal aorta proves to be an effective method for treating infective abdominal aneurysms. Axillo-bifemoral bypass, rifampicin-bonded artificial vessel replacement, hybrid surgery, and stent placement are suitable alternatives for select patients with infective abdominal aneurysms.
1.32.27. Endovascular Therapy in Complicated Aortic Disease—Our Department Experience
Konstantinos Maltezos, Sotirios Giannakakis, Anna Pachi, Apostolos Chaveles, Anastasios Papapetrou, Stavros Kerasidis, Iliana Doukogianni and Chrysostomos Maltezos
Vascular Surgery Department, KAT General Hospital, Athens, Greece
BACHGROUND: Nowadays, the endovascular therapy is a promising technique in revascularization of aortic arch branches, visceral arteries and internal iliac arteries in complicated aortic disease.
AIM-METHOD: Five patients who were admitted to our department between February 2021 and September 2023 were enrolled in this study. The patients suffered from traumatic thoracic aortic dissection, thoracic aortic aneurysm, thoracoabdominal aneurysm, abdominal aortic aneurysm and common iliac aneurysm.
RESULTS: In our study totally 5 patients were included. All patients were men and the mean age of patients were 70 years. Concerning to comorbidities, their pertinent medical history included main the arterial hypertension and the dyslipidemia. The first patient presented a thoracic aortic dissection. The second patient presented a thoracic aortic aneurysm. The third one had a thoracoabdominal aneurysm. The fourth patient presented an abdominal aortic aneurysm with a large auxiliary renal artery. And the last one had a large aneurysm in left common iliac artery. All patients underwent in advanced endovascular repair. In three patients was applied the chimney technique to be revasculated the left subclavian artery and the large auxiliary renal artery. In the patient with thoracoabdominal technique, it was used a fenestrated graft with inside branches to be revasculated the renal arteries and the superior mesenteric artery. And in the last one, it was used an iliac branched endoprothesis.
We had 71% technical success. At the follow-up of one year, an 80% primary patency and 100% assisted primary patency.
CONCLUSIONS: Nowadays, the advanced endovascular technique is a promising minimal invasive method to repair the complicated aortic disease. In the literature, the results for the technical success and the grafts’ potencies are very encouraging. However, it is necessary to be educational and familiar with these techniques. The open repair is remaining a reliable solution.
1.32.28. Natural Post-EVAR Regression of Abdominal Aortic Aneurysm Cause Bending Illiac Extensions of Stentgraft
Andrzej Plonski and Grzegorz Madycki
Department of Vascular Surgery and Angiology, Centre of Postgraduate Medical Education, Warsaw, Poland
65 year old male admitted to Emergency Room due to abdominal pain since 6 h. In Ultrasound (USG doppler) a huge abdominal aortic aneurysm (AAA) was detected. AAA was confirmed in angiocomputedtomography (angioCT, max. horizontal diameter 69 × 70 mm, infrarenal). The other couses of abdominal pain were excluded (e.g., gastrointestinal obstruction or urinary trackt inflamation).
Comorbidities: asthma, 4 laparotomies in the past (due to perforation of duodenum and intraabdominal abscesses), stroke years ago, constant Deep Vein thrombosis of the left lower extremity. Medication taken: Acenokumarol. Because of history of previous abdominal operations, high risk of total general anestesia (ASA 4) and optimal anatomical features of abdominal aortic aneurysm including proximal and distal landing zones, patients was qualified to Endovascular Aneurysm Repair (EVAR). Operation was performed by experienced team of vascular surgeons, in local anestesia. Aortoiliac stentgraft system-Medtronic Endurant was implanted. Further hospitalization was free from complications. Patient did not need hospitalization in Intensive Care Unit (ICU). 10 days after exiting Vascular Surgery Ward, stitches in groins were removed. Each year after operation, patient was obtaining USG doppler of AAA and stentgraft. Each year no leak was found and AAA was fully closed with the normal blood flow throughout stentgraft. Five years after EVAR patient obtained angioCT. The AAA was fully closed, no leak was found. The horizontal dimensions were slightly smaller (AP × LR 45 × 40 mm). Suprisingly the axial diameter (caudal-cranial) was shorter by 30 mm. Proximal and distal landing zones were located at the same spots as it was in angiography during EVAR. Shortening of the dimensions of the aneurysm caused the iliac extentesions of stengraft to bend in S-shaped pattern. Moreover both iliac extensions and femoral arteries were filled with contrast. Patient denied intermittent claudication and the pulse was palpable on feet.
1.32.29. A Rare Complication of EVAR: Migration of the Endograft into the Duedonum
- 1
Department of Cardiovascular Surgery, Atatürk University Faculty of Medicine, Erzurum, Türkiye
- 2
Department of General Surgery, Atatürk University Faculty of Medicine, Erzurum, Türkiye
BACKGROUND: EVAR is a treatment method that is increasing in popularity because it is easily applicable, shortens hospital stays and is a good alternative for patients who cannot tolerate surgery. Although the early results of EVAR are better compared to open surgery, complications such as endoleak, migration, thrombosis/twisting of endograft legs and graft infection may occur.
Case Presentation: A 73 year old male patient was admitted to our hospital with complaints of general deterioration, melena, and fever. The patient had a history of coronary stenting and EVAR. Patient’s laboratory findings were WBC: 17,100, Hgb: 9.5, Crp: 261. CT imaging showed that stents of the EVAR graft were broken and came out of the vessel. It was seen that the EVAR graft had migrated and fistulized to the duodenum. The patient was operated with the simultaneous participation of cardiovascular surgery and general surgery clinics. Rupture in the sigmoid colon and contamination in the abdomen were observed. The aorta was released and a cross clamp was placed below the renal artery level. After the aortotomy the proximal part of the endograft and its left leg were removed. The duodenum was opened and the right leg of the graft was removed. There was no need for Whipple prodecure. The endograft was filled with thrombus. Since there was no distal ischemia before surgery, the aorta was ligated at the infrarenal level. At the same time, the sigmoid colon and rectum were excised and a colostomy was performed. The operation was terminated and the patient was taken to intensive care. The patient developed sepsis and died at the 8th hour postoperatively.
1.32.30. Endovascular Treatment of Abdominal Aortic Stenosis Caused by Takayasu Arteritis
- 1
Department of Cardiovascular Surgery, Etlik City Hospital, Ankara, Türkiye
- 2
Department of Cardiovascular Surgery, Sincan Training and Research Hospital, Ankara, Türkiye
Takayasu arteritis is a rare, chronic, inflammatory vasculitis that primarily affects large arteries, causing significant morbidity and mortality. It is most common in young women in the second and third decades. Clinical findings vary depending on the extent and location of the affected artery. Treatment is medical and/or surgical or endovascular treatment. A 38 years old woman was presented with the complaint of claudication after walking 50 m. Both femoral and distal pulses were absent. The patient had been followed for 4 years due to Takayasu disease. Computerized tomography angiography was demonstrated stenosis of the abdominal aorta. Abdominal aorta was narrowed to 6 mm in diameter from just below the renal arteries to the iliac bifurcation. A Jotec E-XL self-expandable open-cell, uncovered aortic stent with a diameter of 18/16/18 mm was placed through the right femoral artery from the suprarenal to the iliac bifurcation. Remodeling was performed with an aortic balloon. It was observed that full patency of the aorta was achieved after aortic stent implantation. Lower extremity pulses were positive after the procedure. The patient was discharged on postoperative first day with clopidogrel 75 mg and acetylsalicylic acid 300 mg daily. The CT angiography performed 2 months later, the stent was fully expanded. The endovascular treatment of Takayasu arteritis must be the first treatment option in suitable patients. Because of it has low complication rates, it can be performed with local anesthesia, the procedure time is short, the patient can return to normal life in a short time and many other advantages.
1.32.31. A Rare Case: Coarctation-Associated Abdominal Aortic Aneurysm
- 1
Department of Cardiovascular Surgery, Etlik City Hospital, Ankara, Türkiye
- 2
Department of Cardiovascular Surgery, Sincan Training and Research Hospital, Ankara, Türkiye
Coarctation of the abdominal aorta is segmental narrowing of the abdominal or distal descending thoracic aorta. It is a congenital anomaly or associated with neurofibromatosis, retroperitoneal fibrosis, fibromuscular dysplasia, mucopolysaccharidosis, and Takayasu’s arteritis. Coarctation-associated aneurysms are rare. It is usually occurs in thoracic aortic coarctations. Only 2% of these aneurysms are due to abdominal aortic coarctation. A 62-year-old man presented with intermittent abdominal pain and swelling. An abdominal pulsatile mass of 6 × 7 cm in diameter was detected. His femoral and distal pulses were palpable. The computed tomography angiography revealed a 6 cm diameter infrarenal aortic aneurysm. It had expanded into an hourglass shape. The patient underwent elective surgery. When the aneurysm sac was opened, abdominal aortic coarctation was observed. A standard aortobifemoral bypass was performed. Coarctation-associated aneurysms can be treated with surgery or endovascular methods. The anatomical structure of the lesion and the condition of the patient are taken into consideration when choosing the treatment method. We present this patient because it is a rare condition.
1.32.32. Usage of Pericardial Patch and Cytokine Filter in Infected Endovascular Graft
Izatullah Jalalzai, Ali Şahin, Ebubekir Sonmez, Zeliha Işık, Eyupserhat Calik and Ümit Arslan
Department of Cardiovascular Surgery, Ataturk University Research Hospital, Erzurum, Turkey
BACKGROUND: The use of endovascular aneurysm repair (EVAR) has emerged as a recognized substitute for open repair in the management of abdominal aortic aneurysm, despite the presence of anatomical factors that may limit its efficacy. Existing data indicate that endovascular repair is linked to a decreased incidence of all-cause mortality within 30 days after surgery, as well as a notable decrease in perioperative morbidity, in comparison to open surgery. Moreover, EVAR results in less hemorrhage, avoids the need for aortic cross-clamping, and entails shorter recovery durations compared to conventional surgery. In addition to their efficacy as a surgical alternative, endografts may give rise to several complications, including endoleaks, thrombosis of the endograft, and graft infection.
Case Presentation: A 76-year-old male patient was admitted to our hospital with complaints of repeated fever and abdominal pain. The patient had undergone EVAR four years ago. The patient’s laboratory findings were WBC: 21,000, Hgb: 12.6 mg/dL, and Crp: 188. CT imaging showed that the EVAR graft was infected, broken, and thrombosed. The operation was planned. The aorta was released, and a cross clamp was placed below the renal artery level. After the aortotomy, the proximal part of the endograft was removed and replaced with an aorto-bi-iliac graft, which was covered with a pericardial patch. Postoperatively, sepsis and acute kidney injury developed, and the patient underwent hemofiltration with Jafron HA330 cytokine filter. The patient was discharged and had no complications in his 1-year follow-up.
In general, using hemoperfusion to treat septic shock and covering newly replaced infected grafts with a pericardial patch can reduce the length of stay in the intensive care unit, morbidity, and mortality
1.32.33. Mycotic Aortic Aneurysm in a 32-Week Pregnant Patient with Prior MVR with Brucella Endocarditis
Izatullah Jalalzai, Ibrahim Pir, Mohammed Çağrı Aykut, Eyupserhat Çalık and Ümit Arslan
Department of cardiovascular surgery, Ataturk University, Erzurum, Turkey
BACKGROUND: A minority of abdominal aortic aneurysms are comprised of inflammatory aneurysms and mycotic aneurysms. The pathophysiology of inflammatory aneurysms is primarily attributed to autoimmune mechanisms, and it is not common to investigate infectious agents as potential causes of the disease.
Case presentation: A 31-year-old, 32-week pregnant female patient was admitted to our department for a pre-diagnosis of saccular dilatation in the bifurcation of abdomino-iliac arteries in her incidental routine gestational ultrasound checkup. She had undergone mechanical mitral valve replacement 5 years ago due to infective endocarditis. Later, the microbiological specimen was reported as Burcella and she was on warfarin. Computed tomography (CT) was ordered after consultations in radiology and gynecology. The CT showed a 43 × 36 mm axial and 65 mm longitudinal saccular non-thrombosed saccular aneurysm located at the aortic bifurcation. After a multidisciplinary approach with gynecology, an operation was planned. The patient was operated on with the simultaneous participation of cardiovascular surgery and gynecology clinics. The baby was delivered through a cesarean section, the saccular aneurysm was removed, and an aorto-bi-iliac graft was applied after cross-clamping the aorta and iliac arteries. The patient was discharged and was uneventful in her 2-year follow-up.
1.32.34. Open Surgical Conversion Following Type 1 Endoleak
Ahmet Aydın and Nazlı Melis Coşkun Yücel
Department of Cardiovascular Surgery, Hacettepe University, Ankara, Turkey
Endoleak, a common complication after EVAR, can usually be treated with interventional methods. However, every patient doesn’t suit for endovascular treatment, and surgical conversion may be necessary. We present our surgical method, including partial graft excision.
A male patient who had undergone EVAR presented with abdominal/back pain. Type 1 endoleak was detected within the aneurysm sac. The patient underwent percutaneous endoleak treatment, which was unsuccessful. Due to previous unsuccessful endoleak treatments and the proximity of the EVAR graft to the renal arteries, endovascular intervention wasn’t eligible. During surgery, clamps were placed just below the renal arteries and around the main iliac arteries on both sides to include the legs of the EVAR graft. The proximal hooks of the EVAR graft were detached from the aortic Wall. A piece of fabric between two metal rings was cut just before the bifurcation of the EVAR graft. The proximal end of the PTFE graft was anastomosed with the native aortic tissue, and the distal end was anastomosed with the EVAR graft. To strengthen the anastomosis, approximately 2 cm of the PTFE graft distal to the anastomosis was folded outward, after the anastomosis, the graft fold was opened to serve as a protective layer on the EVAR graft.
AAA is increasingly being treated by endovascular means. Factors such as the comorbid conditions of AAA patients, the complications of surgical interventions, the short recovery time of endovascular procedures, and the short hospital stay after endovascular procedures are contributing to this trend. However, when endovascular procedures fail, the surgeon faces a much more complex pathology. According to the literature, re-intervention after endoleak remains the primary treatment approach. However, when endovascular procedures fail, the patient has no choice but surgery. Total excision of the EVAR graft is generally preferred in surgeries. However, it isn’t possible in every patient. During surgical conversion after EVAR, partial excision of the graft and anastomosis to this graft is a reliable option.
1.32.35. Sac Embolisation and Type-1a Endoleak Repair with Glue-Lipiodol Injection by Transabdominal Direct Puncture: A Complex Case Report
Çağla Canbay Sarılar 1, Celal Caner Ercan 2, Birol Akdoğan 1, Merve Doğru 1, Mehmet Semih Çakır 2, Elshad Babazade 1, Bülent Acunaş 2 and Nilgün Bozbuğa 1
- 1
Department of Cardiovascular Surgery, İstanbul Faculty of Medicine Hospital, İstanbul University, İstanbul, Türkiye
- 2
Department of Radiology, İstanbul Faculty of Medicine Hospital, İstanbul University, İstanbul, Türkiye
BACKGROUND: High-risk type 1a, 1b, III endoleaks requiring urgent intervention are one of the most common causes of secondary interventions; they should be repaired when detected.
CASE PRESENTATION: A 71-year-old polymorbid patient who underwent EVAR for infrarenal AAA six years ago presented to the emergency department. CTA showed 9 mm distal migration of the EVAR stent graft (SG) and contrast leakage consistent with a type 1a endoleak (EL1a).
In the first attempt, a proximal extending cuff SG was impelled proximally from the right CFA. In the control imaging, it was observed the leak persisted and apposition was performed with Reliant balloon. Tissel Lyo injection and coil were applied to the localisation with active turbulent flow by USG-guided puncture with transabdominal percutaneous approach to the sac. Control imaging showed persistence of leakage; the procedure was terminated because of the risk of contrast-induced AKI.
3 weeks later, RDUSG showed persistence of EL1a. It was decided to perform balloon apposition procedure to the proximal SG and transabdominal direct puncture to the aneurysm sac with coil + liquid embolising agent. In the second session, a Reliant balloon was propelled to the proximal aneurysm with access from the left CFA. Transabdominal puncture was performed in the aneurysm sac where active turbulent flow was observed on RDUSG. The EL1a origin point was entered in the neck of the aneurysm with a microcatheter through the acoustic triaxial set. A frame was created with multiple coils. The flow was briefly interrupted with a reliant balloon. Under fluoroscopy, coils and dens glue-lipiodol liquid embolising mixture were administered via microcatheter. No EL1a was observed in control imaging. Thrombosis of the aneurysm sac was confirmed.
CONCLUSIONS: In polymorbid patients with persistent EL1a, embolisation of the aneurysm sac with coils and glue through transabdominal direct puncture can be safely performed.
1.35. VASCULAR AND ENDOVASCULAR » Carotid Disease
1.35.1. Carotid Arteries Atherosclerotic Lesion Morphology (Detected with Contrast-Enhanced Ultrasound) Importance to Stent Restenosis
Agnė Gimžauskaitė 1, Aistė Maičiulaitytė 1, Gintautė Diringytė 2, Saulius Lukoševičius 3, Rytis Kaupas 3, Andrius Pranculis 3, Jurgita Plisienė 4, Algidas Basevičius 3, Donatas Inčiūra 1 and Milda Kuprytė 5
- 1
Department of Cardiac, Thoracic and Vascular Surgery, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
- 2
Faculty of Medicine, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
- 3
Department of Radiology, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
- 4
Department of Cardiology Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
- 5
Department of Pathological Anatomy, Lithuanian University of Health Sciences, Kaunas, Lithuania
BACKGROUND AND AIM: Carotid artery stenosis poses a significant risk for ischemic strokes, necessitating effective management strategies such as carotid endarterectomy (CEA) and carotid artery stenting (CAS). However, controversies persist regarding their comparative efficacy and factors influencing post-procedural complications. Understanding the relationship between atherosclerotic plaque characteristics and stent restenosis following CAS is vital for optimizing patient care.
METHOD: In our retrospective study of 221 patients undergoing CAS for symptomatic or asymptomatic carotid artery stenosis, comprehensive assessments of plaque morphology using contrast-enhanced ultrasound (CEUS) were conducted before CAS. Patient demographics, including smoking status and diabetes, were also recorded. Stent restenosis was diagnosed using various imaging modalities, including ultrasound, angiography, and digital subtraction angiography (DSA).
RESULTS: Plaque analysis revealed a significant correlation between plaque type and restenosis incidence (p < 0.001), notably with type 0 (11.1%) and type 2 plaques (66.7%). Smoking was significantly associated with plaque vascularization and restenosis (p < 0.001), while diabetes did not significantly impact plaque characteristics or restenosis risk (p > 0.05). The average duration of restenosis was 17.67 months, with angiography and ultrasound commonly used for diagnosis, showing significant differences (p = 0.016). Stenting was the predominant treatment for restenosis (70.6%), although no significant relationship was found between restenosis type and plaque morphology (p = 0.268). Furthermore, while no clear relationship was observed between plaque morphology and the type of restenosis, our findings underscored the importance of plaque characterization in predicting post-CAS outcomes.
CONCLUSIONS: This study highlights the utility of CEUS in assessing plaque vulnerability and predicting stent restenosis following CAS. There is a significant correlation between the occurrence of stent restenosis within 12–24 months after the carotid stenting procedure and the presence of an elevated grade of plaque vascularization. Further research is needed to elucidate underlying mechanisms and refine risk stratification in this patient population.
1.35.2. Hemodynamic and Hearing Disorders in the Initial Manifestations of Vertebrobasilar Insufficiency
- 1
Republican Specialized Center for Surgical Angioneurology, Tashkent, Uzbekistan
- 2
Tashkent Medical Acadamy, Tashkent, Uzbekistan
BACKGROUND AND AIM: Early detection of hearing disorders and timely treatment for patients that can help prevention of VBI, its development and progression.
METHOD: Examined 56 patients with VBI aged 35 to 45 years. The majority of patients with vertebrobasilar insufficiency selected at the Republican Specialized Center for Surgical Angioneurology. All examined individuals underwent the audiogram. The presence of VBI in the patients studied confirmed by Dopplerography of cerebral vessels, audiogram and by the neurologist. To study hemodynamics in the system of internal carotid arteries and blood circulation of the vertebrobasilar system (VBS), duplex scanning used, which reflects the condition of hemodynamics mainly in the system of vertebral arteries.
RESULTS: Almost all the studied patients or the majority of them with incipient VBI in combination with initial hearing impairment also had complaints of subjective tinnitus (85.2%), noise in the head (56.8%), dizziness (90.2%), heaviness in the back of the head (98%), increased irritability (100%), sleep disturbances (90%), as well as decreased mental performance (100%), etc.
Thus, the studies conducted indicate the importance of patients with initial sensorineural manifestations in combination with VBI, which will contribute to timely targeted treatment for such patients, as well as the prevention of the development of VBI and its progression.
CONCLUSIONS: VBI in combination with sensorineural manifestations will contribute to the timely implementation of pathogenetically based therapeutic and preventive measures that prevent the development of VBI and its progression.
1.35.3. Assessment of Cerebrovascular Reserve by Transcranial Duplex Scanning with Transorbital Access, in Combination with Compression Test, in Patients with Bilateral Hemodynamically Significant Atherosclerotic Lesion of the Carotid Arteries
Dilfuza Jumaniyazova 1, Shavkat Karimov 1, Abdurasul Yulbarisov 1,2 and Rustam Muminov 1,2
- 1
Republican Specialized Center of Surgical Angionevrology, Tashkent, Uzbekistan
- 2
Tashkent Medical Academy, Tashkent, Uzbekistan
BACKGROUND AND AIM: Assessment of the cerebrovascular reserve (CVR), by transcranial duplex scanning (TCDS), transorbital access, in combination with a compression test, in patients with bilateral hemodynamically significant atherosclerotic lesion of the carotid arteries, carried out in the preoperative period in order to choose treatment tactics, type of surgery, as well as to determine indications for the use of a temporary carotid shunt.
METHOD: The results of examination and treatment of 120 (100%) patients with bilateral atherosclerotic lesions of the carotid arteries analyzed. Patients divided into 2 groups. The first group included 55 (46%) patients who underwent reconstructive surgery on the carotid arteries according to intraoperative assessment of brain tolerance to ischemia. The second group consisted of 65 (54%) patients who underwent reconstructive surgery with a preoperative assessment of CVR, performed using TCD through a transorbital approach, in combination with a compression test. As a result of the study, 4 degrees of CVR were identified: high, medium, low, critical.
RESULTS: Full agreement between the preoperative CVR assessment data and the intraoperative tolerance assessment data was observed in 62 (95%) cases (true-positive information). The discrepancy between the preoperative assessment of CVR, performed using TCD through a transorbital approach, in combination with a compression test, and intraoperative data assessing cerebral ischemia tolerance was obtained in 3 (5%) cases (false-positive information). The sensitivity of preoperative assessment of CVR in the main group of patients was 95%, specificity-96%.
CONCLUSIONS: Assessment of CVR using TCD via transorbital access, in combination with the compression test, is the method of choice for preoperative study of cerebral ischemia tolerance in patients with bilateral hemodynamically significant atherosclerotic lesions of the carotid arteries, and it reliably determines treatment tactics and determines the indications for using TCS, that’s why has advantages such as non-invasiveness, accessibility, mobility, lack of radiation exposure, speed of examination, and easy duplication.
1.35.4. Outcomes of Combined Coronary Artery Bypass Grafting and Carotid Endarterectomy: A Single Center Experience from a Tertiary Care Hospital in Pakistan
Hina Inam and Syed Shahabuddin
Aga Khan University Hospital, Karachi, Pakistan
BACKGROUND AND AIM: Patients with coronary artery disease are very likely to have a coexisting carotid artery disease as well. Stroke is one of the common complications occurring in patients with carotid artery disease and post CABG patients that affects the recovery of the patient adversely. Thus, a combined approach of CABG and CEA has gained popularity among surgeons. Other strategies that have been in practice include a staged approach (CEA followed by CABG or vice versa) or CAS followed by CABG. However, a consensus has not been achieved to identify the best and safest available strategy.
METHOD: Data for all adult patients (above 18 years) who underwent combined CABG and CEA from January 2000 to October 2021 was collected retrospectively. We included both symptomatic and asymptomatic patients with carotid artery disease, with an internal carotid artery stenosis of more than 80%.
RESULTS: There were a total of 27 patients identified, with 25.9% females and 74.1% males. Hypertension was the most common comorbid. Ventricular fibrillation (n = 2, 7.4%), visual defects (n = 1, 3.7+%) were the postoperative outcomes encountered. 2 patients died in the hospital secondary to ventricular fibrillation and stroke.
CONCLUSIONS: The literature shows variable outcomes with different strategies for treatment of coexisting CAD and carotid stenosis. While the studies show that the patients who undergo CABG only with no treatment for carotid stenosis are at higher risk of stroke whereas a synchronous strategy is associated with a decreased risk of stroke.
1.35.5. Coronary Artery Bypass Graft Surgery in Patients with Asymptomatic Carotid Stenosis: 5-Year Results from a Randomized Clinical Trial
Stephan C Knipp 1, Hans Torulv Holst 1, Konstantinos Bilbilis 2, Heinz Günter Jakob 1 and Christian Weimar 3
- 1
Department of Thoracic and Cardiovascular Surgery, University of Duisburg-Essen, Essen, Germany
- 2
Institute for Medical Informatics, Biometry and Epidemiology, University of Duisburg-Essen, Essen, Germany
- 3
Department of Neurology, University of Duisburg-Essen, Essen, Germany; BDH Clinic, Elzach, Germany
BACKGROUND AND AIM: The optimal strategy for treating patients with concomitant severe coronary and carotid artery disease has been investigated for decades, and combined simultaneous CABG and carotid endarterectomy (CEA) are widely used despite lack of high-level evidence. In addition, there is no data on the preventive effect of CEA compared with best medical therapy on long-term risk of stroke.
METHOD: In the Coronary Artery Bypass graft surgery in patients with Asymptomatic Carotid Stenosis (CABACS) trial, patients with coronary disease and high-grade carotid stenosis (NASCET ≥ 70%) were randomly assigned to combined simultaneous CABG + CEA or CABG alone. Primary endpoint was the composite rate of non-fatal stroke or death within 30 days after surgery, with both treatment options assumed to be equally safe and efficacious. Secondary outcome events included any stroke, stroke or vascular death and death of any cause. Patients were followed-up for five years.
RESULTS: The trial was terminated prematurely after recruitment of 129 patients in 17 centers in Germany and the Czech Republic due to lack of funding. The rate of stroke or death at 30 days was not significantly different following combined CABG + CEA and CABG alone (18.5% [95% CI: 0.099–0.300] versus 9.7% [95% CI: 0.036–0.199], p = 0.203), respectively. At 5 years FU, rates of stroke or death increased to 40.6% (95% CI: 0.285–0.536) following CABG + CEA, and 35.0% (95% CI: 0.231–0.484) following CABG alone (p = 0.581). Strokes of any kind tended to occur more frequently after CABG + CEA (5 years: 29.4% vs. 18.8%, p = 0.245), while mortality was similar in both treatment arms (25.4% vs. 23.3%, p = 0.837). Subgroup analysis revealed no significant effect of center on outcome events.
CONCLUSIONS: Long-term risk of stroke or death was higher after combined simultaneous CABG + CEA, mainly due to increased perioperative event rates. Because of limited power of the trial, further studies are warranted to confirm our results.
1.35.6. Early Surgical Challenges in Sheep Carotid Graft Surgery
Ziyu Wang 1,2, Hugh Paterson 3, Lisa Partel 4, Innes Wise 5, Matthew Adams 6, David C. Cistulli 7, Dominic Ng 7, John O’sullivan 2,8,9,10, Sean Lal 2,8,9,10, Anthony S. Weiss 1,2,11, Paul G. Bannon 3,7,10 and Robert D. Hume 2,8,10
- 1
School of Life and Environmental Sciences, Faculty of Science, The University of Sydney, Sydney, NSW 2006, Australia
- 2
Charles Perkins Centre, The University of Sydney, Sydney, NSW 2006, Australia
- 3
Central Clinical School—Surgery, Faculty of Medicine and Health, The University of Sydney, Sydney, NSW 2006, Australia
- 4
Sydney Imaging, Core Research Facilities, the University of Sydney, Sydney, NSW 2006, Australia
- 5
Laboratory Animal Services, Core Research Facilities, The University of Sydney, Sydney, NSW 2006, Australia
- 6
Camperdown Vascular Lab, Sydney, NSW 2006, Australia
- 7
Cardiothoracic Surgical Department, Royal Prince Alfred Hospital, Sydney, NSW 2006, Australia
- 8
School of Medical Sciences, Faculty of Medicine and Health, The University of Sydney, Sydney, NSW 2006, Australia
- 9
Department of Cardiology, Royal Prince Alfred Hospital, Sydney, NSW 2006, Australia
- 10
Centre for Heart Failure and Diseases of the Aorta, The Baird Institute for Applied Heart and Lung Research, Sydney, NSW 2006, Australia
- 11
The University of Sydney Nano Institute, The University of Sydney, Sydney, NSW 2006, Australia
BACKGROUND AND AIM: Small vessel synthetic grafts often fail within 5 years, which poses a clinical challenge because patients must rely on autologous vessel conduits. Large animal models are the gold standard for pre-clinical experimentation of vascular grafts. This study aimed to examine a novel small vessel synthetic conduit in a sheep model, and describe the initial challenges and potential solutions from a surgical perspective.
METHOD: Four sheep had imaging via Doppler ultrasound and invasive angiography to demonstrate flow and patency of native common carotid arteries (CCA). Following heparinisation, a 3 cm segment of left CCA was replaced with a novel vascular graft, while shame surgery was performed on the right CCA via transection and re-anastomosis. Post-surgery angiography and Doppler was performed to assess patency on both sides. Different combinations of cannulation strategies were utilised, via CCA or common femoral artery (CFA). Anti-spasmodic agents (sodium nitroprusside, papaverine, verapamil) were administered intraoperatively at varying doses and times.
RESULTS: Cannulation of the CCA for angiography was associated with arterial spasm. This finding was supported by a mildly reduced spasm by downsizing to a smaller catheter, while converting to CFA cannulation resulted in a substantial reduction. Thrombus was a salient finding upon re-opening severely stenosed vessels, especially in the novel synthetic graft. Lastly, administering prophylactic intraarterial papaverine-verapamil markedly reduced spasm, and when used in combination with CFA cannulation was effective in preventing it completely.
CONCLUSIONS: Carotid artery spasm and thrombosis posed significant early challenges in this sheep vascular graft model. Minimising local trauma and administering prophylactic anti-spasmodic agents appears to be effective in reducing these confounders.
1.35.7. Comparative Study of Early Outcomes of Simultaneous Carotid Endarterectomy and Coronary Artery Bypass Grafting Surgery with Staged Carotid Artery Stenting and Coronary Artery Bypass Grafting Surgery
Ebsar Ergenc, Fuat Büyükbayrak and Arzu Antal
Department of Cardiovascular Surgery, University of Health Sciences, Istanbul, Turkiye
BACKGROUND AND AIM: Criteria, timing, and methods for carotid artery intervention in patients undergoing coronary artery bypass grafting (CABG) have not yet reached a consensus. This study aims to compare the early-term mortality and morbidity of staged carotid stenting and simultaneous carotid endarterectomy in patients with significant carotid artery stenosis before CABG surgery.
METHOD: Our study includes a retrospective analysis of a total of 182 patients, comprising 98 patients who underwent carotid endarterectomy (CEA) concurrently with CABG surgery and 84 patients who underwent carotid artery stenting (CAS) between January 2011 and June 2023 at Kartal Kosuyolu Training and Research Hospital. Mortality and cerebrovascular events observed within the first 30 days in both groups were retrospectively evaluated.
RESULTS: The primary endpoint, 30-day mortality rates, were determined as 11 cases (11.2%) in the CABG + CEA group and 6 cases (7.1%) in the CABG + CAS group (p: 0.492). As the secondary endpoint, cerebrovascular event rates were found to be 17 cases (17.3%) in the CABG + CEA group and 13 cases (15.5%) in the CABG + CAS group (p: 0.890). There was no statistically significant difference between the groups regarding mortality and cerebrovascular events.
CONCLUSIONS: In patients identified with significant carotid artery stenosis in preoperative evaluations for coronary artery bypass graft surgery and requiring intervention, our study suggests that carotid artery stenting is as safe as carotid endarterectomy. We recommend determining the selected method based on the patient’s symptoms and the surgeon’s experience.
1.35.8. Validation of Artificial Intelligence Platform (TAXINOMISIS) for Stratification of Patients with Carotid Disease
Ognjen Dusan Kostic 1, Vassiliki Potsika 2, Vassiliki Kigka 3, Vassilis Tsakanakis 3, David Matejevic 1, Ivana Djurasev 4, Jelena Stanarcevic 5, Dimitrios Fotiadis 2 and Igor Koncar 6
- 1
Clinic for Vascular and Endovascular Surgery, Serbian Clinical Center, Belgrade, Serbia
- 2
Department of Materials Science and Engineering, Unit of Medical Technology and Intelligent Information Systems, University of Ioannina, Ioannina, Greece
- 3
Unit of Medical Technology and Intelligent Information Systems, Department of Materials Science and Engineering, University of Ioannina, Ioannina, Greece
- 4
Clinic for Cardiac Surgery, Serbian Clinical Center, Belgrade, Serbia
- 5
Special Hospital for Cerebrovascular Diseases “Sveti Sava”, Belgrade, Serbia
- 6
Medical faculty, University of Belgrade, Serbia
BACKGROUND AND AIM: The Taxinomisis project was developed to stratify individuals with asymptomatic carotid disease, addressing specific requirements from clinicians. Among these needs is the improvement of screening methods for carotid stenosis. This study aims to validate the initial stage of the Taxinomisis tool, focusing on identifying individuals at higher risk of carotid stenosis.
METHOD: The demographic and medical data of individuals who fulfilled the inclusion criteria, and accept participation in the study, was collected prospectively and inserted in the Taxinomisis stratification tool. All these patients also had a carotid duplex ultrasound examination, the result of which was also inserted in the tool in order to assess the diagnostic accuracy of the tool.
RESULTS: Data from 813 individuals were used to validate TAXINOMISIS Level I. 70.3% had carotid stenosis over 50%. Different probability thresholds were tested, with the best sensitivity (91%) at 0.4 and 0.5 (87%). Thresholds of 0.56 and 0.7 showed high false negatives, risking undiagnosed patients. False positives increase screening costs. Validation in a wider population is necessary to optimize sensitivity and specificity, minimizing false negatives.
CONCLUSIONS: The AI platform demonstrates good sensitivity and specificity in determining the risk of carotid stenosis presence. However, further validation is necessary.
1.35.9. Aberrant Carotid Artery Anomaly
Carotid artery compression with abnormal cervical location is rare, but mechanical interaction between bone structures and carotid arteries causing clinical symptoms is even rarer. In some of these reports, it was described as repetitive trauma by the lateral horn of the hyoid bone leading to wall injury and symptomatic stenosis, pseudoaneurysm or carotid artery dissection. In this study, we aimed to present a case of ICA stenosis associated with ICA tortuosity and compression by the hyoid bone. Case presentation: An 80 year-old male patient presented to our clinic with left-sided hemiparesis, dizziness and balance disturbance. Carotid Doppler ultrasonography showed plaque formation forming a 50–70% stenosis in the left ICA and 90% stenosis (PSV 265 cm/s) in the proximal right ICA. Subsequent carotid CT angiography showed a total stenosis in the right ICA and an aberrant stenosis in the left ICA curving through the hyoid bone. Endovascular approach is not recommended for ICA stenosis due to external compression of the carotid arteries. However, because of total occlusion of the right ICA, it was thought that the lateral horn of the hyoid bone should be treated to provide left ICA revascularisation. For this purpose, the patient was referred to the ENT outpatient clinic for surgical planning. Conclusion Generally, the carotid arteries are located in a fibrous layer that allows the artery to follow the neck movements. Elongation and tortuosity of the carotid artery may alter its course within this fibrous layer and cause mechanical compression. CT imaging shows abnormal course of the ICA subjected to compression by the hyoid bone. The present case suggests that hyoid bone compression should be recognised as a rare cause of ICA stenosis, which is more likely to occur when an unusual carotid artery anatomy coexists. In this case, we suggest that a surgical procedure to remove the damaging compression of the bone rather than an invasive procedure would be appropriate.
1.35.10. Hemodynamic and Hearing Disorders During Initial Manifestations of Vertebrobasilar Insufficiency
- 1
Republican Specialized Center for Surgical Angioneurology, Tashkent, Uzbekistan
- 2
Tashkent Medical Acadamy, Tashkent, Uzbekistan
BACKGROUND AND AIM: Early detection of hearing disorders and timely treatment for patients that can help prevention of VBI, its development and progression.
METHOD: Examined 56 patients with VBI aged 35 to 45 years. The majority of patients with vertebrobasilar insufficiency selected at the Republican Specialized Center for Surgical Angioneurology. All examined individuals underwent the audiogram. The presence of VBI in the patients studied confirmed by Dopplerography of cerebral vessels, audiogram and by the neurologist. To study hemodynamics in the system of internal carotid arteries and blood circulation of the vertebrobasilar system (VBS), duplex scanning used, which reflects the condition of hemodynamics mainly in the system of vertebral arteries.
RESULTS: Almost all the studied patients or the majority of them with incipient VBI in combination with initial hearing impairment also had complaints of subjective tinnitus (85.2%), noise in the head (56.8%), dizziness (90.2%), heaviness in the back of the head (98%), increased irritability (100%), sleep disturbances (90%), as well as decreased mental performance (100%), etc.
Thus, the studies conducted indicate the importance of patients with initial sensorineural manifestations in combination with VBI, which will contribute to timely targeted treatment for such patients, as well as the prevention of the development of VBI and its progression.
CONCLUSIONS: VBI in combination with sensorineural manifestations will contribute to the timely implementation of pathogenetically based therapeutic and preventive measures that prevent the development of VBI and its progression.
1.36. VASCULAR AND ENDOVASCULAR » Miscellaneous
1.36.1. Chronic Type B Dissection Leads to Rupture of Gigantic Extent II Thoracoabdominal Aneurysm: Successful Endovascular Management Using the STABILISE Technique
Areti Vassiliou, Giwrgos Fanariotis, Michail Peroulis and Vangelis G. Alexio
Vascular Surgery Unit, General Surgery Department, University Hospital of Ioannina, Ioannina, Greece
BACKGROUND AND AIM: Our aim is to assess the feasibility of Stabilise and petticoat technique in dissection B patients.
METHOD: A 78-year-old male suffered type B dissection 12 years ago. The patient was managed conservatively. He developed an extent II thoracoabdominal aneurysm measuring 7.5 cm and thrombosis of the left renal artery. He was lost to follow-up for at least 2 years, and presented with acute thoracic pain, hypotension, shortness of breath, and a hemoglobin of 9 g/dL. CT revealed that his aneurysm had dilated to 12 cm and ruptured within his mediastinum. He had a massive pleural effusion with unilateral white-out and collapse of his left lung. A large entry tear 2 cm distal to the left subclavian allowed adequate proximal sealing. The true lumen (TL) had collapsed along the descending thoracic aorta and the paravisceral abdominal aorta. Furthermore, there were 3 distal entry tears at the infrarenal level and at the left common iliac artery, which had expanded to 4 cm. The patient was urgently operated on. In order to close off the proximal entry tear, a 20 cm long thoracic endograft with 10% oversizing was used. A petticoat bare-metal stent was placed at the paravisceral aorta for a better expansion of the TL. A selective treatment of all the distal entry tears included placement of an infrarenal aortic cuff with a total covered length of 49 mm and a left Iliac leg. Compliant aortic balloons were used within the stent-grafts, while non-compliant balloons were used within the bare-metal stent to rupture the lamella.
RESULTS: The post-operative CT scan revealed false lumen thrombosis. This is the first, to our knowledge, report of the STABILISE technique in the acute setting.
CONCLUSIONS: The use of the stabilise technique is feasible also and in the acute setting and by using the petticoat technique we may also proceed to a more favourable remodeling of the aorta.
1.36.2. Unfractionated Intravenous Heparin Versus Low Molecular Weight Heparin After Vascular Surgery
Denise Özdemir Van Brunschot, David Holzhey and Spiridon Botsios
German Faculty of Health, Witten/Herdecke University, Witten, Germany
BACKGROUND AND AIM: Platelet aggregation and anticoagulants play a major role in vascular surgery. Postoperative anticoagulation after vascular surgery is given to prevent venous thrombosis but also to prevent early graft thrombosis. In some clinics unfractionated intravenous heparin is given during the first postoperative period, other clinics prefer low molecular weight heparin.
METHOD: In our hospital the postoperative anticoagulation regime after vascular surgery was changed on 1 September 2021. Before regime change all patients received intravenous unfractionated heparin in the first 24 h after vascular surgery, thereafter normal thrombosis prophylaxis (20 or 40 mg low molecular weight heparin once a day) was administered. After the 1 September 2021 patients received low molecular weight heparin in a prophylactic dose after vascular surgery. The patients in the new regime were matched with patients from the UFH regime.
RESULTS: A total of 836 patients were included: 418 patients in the LMWH group and 418 patients in the UFH group. There were more patients with the need for re-operation because of a local hematoma in the UFH group (0.5% versus 4.8%, p = 0.01). There were no significant differences regarding other outcomes (patency of the reconstruction or need for re-operation because of bleeding). Sub-analyses were performed regarding type of surgery, excluding patients using new oral anticoagulants or vitamin K antagonists and excluding two surgeons whom exclusively operated in the UFH or LMWH regime, showed comparable results.
CONCLUSIONS: This retrospective study suggests that LMWH should be preferred as anticoagulation after vascular surgery, since there were less patients with the need for re-operation because of hematoma and there is no need for monitoring.
1.36.3. Analysis and Treatment of Delayed Vascular Injuries in the II Karabakh War: A Study from Azerbaijan
BACKGROUND AND AIM: The objective was to examine delayed vascular injuries sustained in Azerbaijan between 27 September 2020, and 8 November 2020, during the II Karabakh War.
METHOD: Delayed vascular injuries of wounded patients treated in the General Clinical Hospital of Azerbaijan were divided into 2 groups: pseudoaneurysms of arteries and arteriovenous fistulas.
RESULTS: The five types of vascular injuries are: (1) intimal injuries (flaps, disruptions, or hematomas); (2) wall defects with pseudoaneurysms or hemorrhage; (3) complete transections with hemorrhage or occlusion; (4) arteriovenous fistulas; and (5) spasm. (1). The duration of exposure to the complications of vascular damage in patients was a minimum of 3 h and a maximum of 11 months. A total of 24 patients had delayed vascular injuries. 66.6% of these patients (16 patients) had a pseudoaneurysm of an arterial vessel, 33.3% (8 patients) had an arteriovenous fistula. Auscultatory noise was heard over the injured area during examination in 58.3% of patients (14). Pseudoaneurysms were bleeding in 37% of patients (9 patients), arteriovenous fistulas were bleeding in 4.16% of patients (1 patient). Due to the predominance of shrapnel injuries in battles, the aorta, the axillary artery, the brachial artery, the superficial femoral artery, the popliteal artery each of them in 1 patient, the subclavian artery, the deep femoral artery, the external carotid artery, the anterior tibial artery each of them in 2 patients were found to be affected. One patient with an aortic pseudoaneurysm underwent synthetic patch plasty using a dacron graft; another underwent graft interposition; seven individuals had artery ligation (non-dominant arteries); the remaining patients underwent autogenous vein interposition. Via an arteriovenous fistula in the iliac artery, one patient died.
CONCLUSIONS: This study demonstrates that vascular problems can be identified by thoroughly examining injured individuals, allowing for prompt intervention to stop bleeding and repair damaged vessels.
1.36.4. Surgical Management of Paediatric Vascular Emergencies: Single Center Experience
Safak Alpat, Melih Alma, Recep Oktay Peker and Mustafa Yılmaz
Division of Paediatric Cardiovascular Surgery, Department of Cardiovascular Surgery, Hacettepe University School of Medicine, Ankara, Türkiye
BACKGROUND AND AIM: Vascular emergencies necessitate complex decision making and interdisciplinary care. Management of these patients is more difficult when they occur in children. Since vascular emergencies are uncommon in children, this rarity complicates the precise, prompt detection and meticulous management of a vascular emergency. Endovascular technology remains limited for pediatric vascular surgery injuries. Here, we present our surgical experience in paediatric vascular emergencies.
METHOD: Between 2014–2024, 21 paediatric patients underwent emergency vascular procedure in our unit. Pre-, intra, and post-operative data were collected and analyzed.
RESULTS: 21 patients (12 males, 9 females) underwent emergency vascular surgery in our unit during the study period. Median age was 96 months (7–144) with 8 being less than 3 years of age. Indications were access related acute limb ischemia in 12 (57%), trauma in 4 (19%), thromboembolism in 4 (19%), and pseudoaneurysm in 1 (5%). All patients in access related ALI had systemic anticoagulation initally but duplex scan revealed no improvement. 80% had common femoral and 20% had external iliac artery related thrombosis. Surgical techniques included; thrombectomy, primary arterial repair, arterial dilatation and topical papaverine application to relieve spasm. Limb preservation was 100% without neeed for fasciotomy. Trauma patients required multi-vessel revascularization including artery and vein interposition and/or bypass grafts with autologous tissues. Limb preservation was 100% and 50% required fasciotomy. Thromboembolic group underwent thromboembolectomy and a patient with pseudoaneurysm had primary repair of puncture point. All patients received systemic anticoagulation with heparin for the first 24 h bridged to LMWH for the hospital stay and discharged with ASA.
CONCLUSIONS: Paediatric vascular injuries are generally thought to bee difficult to manage. In general, operative interventions in children younger than years are reported to have worse outcomes than older children. Thus, non-operative management is preferred. However, according to our experience, we showed that prompt diagnosis-early surgical intervention are associated with good outcomes, even in patients younger than 3-years old.
1.36.5. Fundamental Biophysical Misconceptions in Fluid Dynamics in Surgical Patients
Nery Alexandra Lamothe 1, Mara Nicole Lamothe 1, Alejandro Rey 2, Jean Christian Daniel Lamothe 3 and Alejandro Alonso Altamirano 1
- 1
Division Ciencias Biologicas y de la Salud, Universidad Autonoma Metropolitana, Mexico City, Mexico
- 2
Chief, Cardiac Surgery Department, American British Cowdray Medical Center, Mexico City, Mexico
- 3
Internal Medicine, Jersey City Medical Center, NJ, USA
BACKGROUND AND AIM: Perfusion is not inversely related to the fourth power of the radius but to the second power of the radius.
METHOD: Apodictic inferences from the fundamental physical laws, using the International System of Units, to refute fluid dynamics misconceptions.
RESULTS: To infer the perfusion effect of arterial occlusion, it is the transverse area that is considered instead of the radius. Perfusion decays linearly with the transverse area of the occluded artery.
Antihypertensive drugs produce a decay in the axial pressure and thus a decay in perfusion.
Clinical arterial pressure constitutes transmural pressure rather than axial pressure which is what drives perfusion.
It is Laplacian tension that damages the vessel’s wall, rather than the transmural pressure.
It is energy density per time that damages the vessels. Thus joules/liter per second or Watts/liter.
Perfusion increases proportionally to driving pressure.
It is Laplacian tension that activates the baroreceptors, rather than transmural pressure.
Systemic vasodilatation increases the perfusion in peripheral tissues diminishing the brain and cardiac perfusion.
Every physical gradient, including pressure, constitutes potential energy,
The changes in the pressure per time are the derivative of the pressure per time, which is equal to the derivative of energy per volume per time. This corresponds strictly to the derivative of energy density per time, which in turn, is the density of power.
It is the axial gradient of energy rather than the pressure axial gradient that drives the perfusion.
Pressure is force per area, as well as, energy per volume, which is energy density.
CONCLUSIONS: The heart cannot output a volume that has not been received. It is not the preload volume in the EDV but the pressure at the EDV that could decrease before the initiation of the isovolumetric contraction phase.
1.36.6. Using Augmented Reality Systems for Open Vascular Procedures—First Case in a Public Hellenic Hospital
George Galyfos, Linnea Tscheuschner, Sylvie Vagena, Marcel Pikula, Andrzej Skalski, Konstantinos Filis and Frangiska Sigala
Vascular unit, First Department of Propaedeutic Surgery, National and Kapodistrian University of Athens, Hippocration Hospital, Athens, Greece
BACKGROUND: Augmented reality technology has been introduced to everyday clinical practice in order to facilitate different types of surgical procedures. Therefore, several surgical specialties have started to use such technology for preoperative planning as well as during surgery. Regarding vascular interventions, only a limited number of reports are available describing possible benefits mainly for endovascular procedures.
CASE: We are presenting a novel 3-dimentional holographic system that was used to perform an open vascular procedure. The patient presented with critical limb ischemia, and underwent a femorofemoral bypass. This is the first case of applying such technology in a public Hellenic hospital.
1.36.7. Cystic Adventitial Disease in an Adolescent—A Rare Entity
David Matejevic, Aleksandar Mitrovic, Andrija Roganovic, Ognjen Kostic and Ilija Kuzmanovic
Clinic for Vascular and Endovascular Surgery, University Clinical Center of Serbia, Belgrade, Serbia
BACKGROUND: Cystic adventitial disease is a rare, non-atherosclerotic condition of still unknown etiology in which mucinous cysts form in the blood vessel adventitial layer. The most commonly affected vessel is popliteal artery, and the condition is usually seen in middle-aged man (40–60 years). The treatment options are usually surgical, and the most frequently used technique is the resection of the affected part of the artery and reconstruction with autovenous graft, but percutaneous endovascular techniques are also described.
CASE: A 17-year-old male patient presented with sudden-onset short distance right calf claudication that lasted for 3 days. MDCT angiography and intraoperative finding showed saccular aneurysm of popliteal artery with a maximum diameter of 12 mm, accompanied by the occlusion of the distal popliteal artery and the tibioperoneal trunk. The patient underwent operative treatment—thrombectomy, extirpation of the aneurysm and autovenous reverse graft interposition was performed via posterior approach. Pathohistological examination of arterial wall showed cystic adventitial disease, with the unilocular transmural cyst, fragmentation of the inner elastic membrane, extensive fibro-intimal proliferation and superimposed thrombus. Pathohistological characteristics of the distal thrombus were usual. Postoperatively, the patient fully recovered with palpable distal pulses. A one-month control duplex scan verified graft patency. Although cystic adventitial disease is more frequent in middle-aged patients, usually with no atherosclerotic risk factors and overall healthy non-included vessels, it should be considered as a diagnosis in younger patients as well, since timely treatment is mandatory to avoid serious consequences such as limb loss.
1.36.8. Complex Reccurent Aortic Pseudoaneuysms in a Case of Giant Cell Arteritis: A Different Endovascular Approach
Ayse Zehra Cotelioglu, Gokhan Albayrak and Koray Aykut
Izmir University of Economics Medical Point Hospital, Izmir, Turkey
Pseudoaneurysms occurs after 0.5% of all cardiac surgical cases and are often localized at previous anastomotic sites, aortototomy and cannulation sites.
An 80-year-old male patient presented to our hospital with a history of chest pain two years ago. The angiography revealed three-vessel coronary artery disease, necessitating a standard coronary artery bypass graft (CABG) operation utilizing left internal mammary artery (LIMA) and saphenous vein grafts.
Five months later, the patient admitted to the clinic with recurrent fever and infectious symptoms which were refractory to antibiotic therapy. Subsequent thoracic MRI-angiography revealed an aortic pseudoaneurysm located in the ascending aorta. Open surgical repair was undertaken, utilizing cannulation of the right axillary artery via a dacron graft and venous cannulation via the right femoral vein. During deep hypothermic total circulatory arrest, the infected pseudoaneurysm sac was opened and repair of the necrotic hole from previous arterial cannulation was performed using a dacron patch. The postoperative course was uneventful, and the patient was discharged on postoperative day 14 following optimized antibiotic therapy.
Three months later, the patient was readmitted with a neck mass. Control CT angiography revealed another pseudoaneurysm in the ascending aorta and a mediastinal hematoma. Endovascular repair was planned for the same localization, the middle portion of the ascending aorta (proximal of Zone 0), with deployment of a short segment between the initiation of the bovine-configurated brachiocephalic trunk and proximal anastomosis region of the saphenous vein graft. Control angiography confirmed the patency of the saphenous vein grafts and LIMA graft, with resolution of pseudoaneurysm circulation.
Subsequently, the patient was diagnosed with giant cell arteritis upon discharge. Over the following two years, the patient developed two femoral pseudoaneurysms, either. The recurrence of aneurysms underscores the importance of considering vasculitic syndromes in such cases. Variations of endovascular treatments can be efficacious in selected cases.
1.37. VASCULAR AND ENDOVASCULAR » PAOD
1.37.1. Optical Coherence Tomography and Fractional Flow Reserve in Below-the-Knee Percutaneous Transluminal Angioplasty: A Case Series
Ozan Yazar, Chrissy Van Wely, Rens Oosterveld, Pieter Salemans, Chunyu Wong and Lee Bouwman
Department of vascular and endovascular surgery, Zuyderland Medical Center, Heerlen, The Netherlands
BACKGROUND AND AIM: The golden standard imaging modality for Percutaneous Transluminal Angioplasty (PTA) is Digital Subtraction Angiography (DSA) using iodine contrast agent. While DSA visualizes the vessel and allows the surgeon to estimate the size and percentage of stenosis in the vessel, it lacks objective vessel diameter measurement, information on plaque morphology and measurement of hemodynamic consequences of the stenosis. Optical Coherence Tomography (OCT) and Fractional Flow Reserve (FFR) measurements bridge these gaps. OCT, an intravascular imaging modality which uses near-infrared light to capture images of the vessel wall, allows objective measurement of vessel diameter and percentage of stenosis. FFR measures pre- and post-stenotic pressures, demonstrating hemodynamic consequences of the stenosis. A decreased FFR indicates diminished blood flow towards the extremity, demonstrating the hemodynamic significance of the stenosis that would consequently require treatment.
METHOD: OCT and FFR measurements were completed in 4 subjects undergoing elective PTA in below-the-knee lesions due to critical limb ischemia. Subjects were eligible when the lesion on pre-operative imaging was no longer than 3 cm. Subjects who underwent PTA 30 days prior to the current intervention were excluded, as well as subjects with previous major amputation.
RESULTS: No complications were caused by OCT and FFR procedures, demonstrating its safety. OCT revealed the presence of dissections and presence of thrombus after PTA that were not detected using DSA. FFR values would have caused the surgeon to change his per-operative decision making in two subjects.
CONCLUSIONS: OCT and FFR are safe to use in below-the-knee arterial lesions providing valuable additional information on vessel diameter, percentage of stenosis, plaque morphology and hemodynamic significance. This may cause alterations in perioperative decision-making.
1.37.2. Comparative Analysis of Graft Options in Critical Limb Ischemia Surgery
Gian Antonio Boschetti, Raffaele Adornetto, Luca Calia Di Pinto, Floriana Carrer, Chiara Dal Borgo, Stefano Doro, Daniele Masotti, Laura Nicolai, Cristina Puglisi, Gianna Saviane, Letizia Turini and Edoardo Galeazzi
Vascular Surgery Unit, AULSS 2 Marca Trevigiana, Treviso Regional Hospital, Treviso, Italy
BACKGROUND AND AIM: The utilization of materials other than autologous vein for below the knee (BTK) revascularization still presents some limitations. The aim of this study was to analyze the outcomes of different graft types used for BTK revascularizations for critical limb ischemia (CLI).
METHOD: We retrospectively collected pre-, intra- and postoperative data of the patients that underwent primary BTK bypass surgery with biological or biosynthetic graft for CLI between 2020 and 2023. Primary endpoints were primary patency, reintervention, amputation and mortality rate during follow-up.
RESULTS: We included 47 patients for whom 23 (48.9%) autologous vein (AV), 10 (21.3%) homologous vein (HV), 10 (21.3%) Omniflow® II bypass graft (OG), and 4 (8.5%) homologous arteries (HA) were used. The mean age was 74.3 ± 9.6 years, 29 patients were male (61.7%) and the majority presented Rutherford stage V (n = 33, 70.2%) and one run-off vessel (n = 26, 51.1%). Thirty-day and 1-year cumulative primary patency for each group were respectively 100%, 70%, 70%, and 100% (p < 0.05)–86.9%, 50%, 70%, and 100% (p < 0.05). Similarly, cumulative reintervention rates for bypass occlusion were 0%, 30%, 30%, and 0% (p < 0.05)–8.7%, 40%, 30%, 0% (p < 0.05). There were no deaths at the 30-day follow-up while at 1-year the mortality rates were 17.4%, 10%, 10%, and 25% (p > 0.05). One major amputation occurred during the entire follow-up in the OG group only (2.1%).
CONCLUSIONS: Although AV remains the conduit of choice, this study highlights the importance of considering other biological or biosynthetic grafts for BTK revascularization when AV is not available.
1.37.3. Comparison of Open Surgical Repair and Endovascular Embolization Treatments in Iatrogenic Peripheral Arterial Pseudoaneurysms: A Retrospective Study of 42 Cases
Mehmet Ziyaddin Altun 1, Ahmet Ibrahim Balkaya 1, Begum Ozuekren Kasapoglu 1, Umut Erdem 2, Helin El Kilic 1, Tolga Demir 1 and Ismail Koramaz 1
- 1
Department of Cardiovascular Surgery, Hamidiye Etfal Training and Research Hospital, Health Science University, Istanbul, Turkey
- 2
Department of Radiology, Hamidiye Etfal Training and Research Hospital, Health Science University, Istanbul, Turkey
BACKGROUND AND AIM: In recent years, due to the widespread use of invasive methods for diagnosis and treatment, the incidence of pseudoaneurysm cases has increased. The objective of our study is to compare open surgical intervention with endovascular embolization therapies for iatrogenic peripheral arterial pseudoaneurysms, while retrospectively assessing the preoperative characteristics of the cases
METHOD: Between 2021 and 2024, a total of 42 patients diagnosed with peripheral artery pseudoaneurysms were included in the study and divided into two groups according to treatment modalities. Embolization was performed in 24 patients (Group 1), while 18 patients underwent open surgical intervention (Group 2). Pseudoaneurysms were diagnosed via ultrasonography and confirmed by computed tomography (CT) scans when deemed necessary.
RESULTS: The most frequent symptom was a pulsatile mass and all originated from common femoral artery. The mean diameter of pseudoaneurysms was higher in group 2 (1.6 ± 1.2 cm vs. 4.3 ± 1.6 cm). Among 24, 2 patients underwent open surgical closure due to the short neck of the pseudoaneurysm. In the open surgical group, successful aneurysm closure was achieved in all patients. During the follow-up period 2 (8.3%) patients experienced recurrent bleeding which required blood transfusion in Group 1 and wound infection was reported in 4 (22.2%) patients and lymphorrhea in 1 (5.5%) in Group 2 as an early postoperative complication.
CONCLUSIONS: Iatrogenic Peripheral artery pseudoaneurysms can be effectively managed through either open surgical techniques or interventional procedures in carefully selected patients, yielding acceptable mid- and long-term outcomes
1.37.4. Patients with Low Serum Albumin Short-Term Results Outcomes in Aorta-Femoral Bypass Surgery
- 1
Department of Cardiovascular Surgery, Prof. Dr. Cemil Tascioglu City Hospital, Istanbul, Turkey
- 2
Department of Cardiovascular Surgery, Istanbul University-Cerrahpasa Institute of Cardiology, Istanbul, Turkey
BACKGROUND AND AIM: Low albumin level has been associated with poor outcomes, including death, in surgical patients. Since studies in the vascular population are insufficient; We aimed to share the results of preoperative low albumin levels, mortality and short-term postoperative complications in patients with distal aortic and iliac artery lesions who underwent aorta-femoral bypass.
METHOD: Patients who underwent aorta-femoral bypass between January 2018 and January 2024 were retrospectively scanned from the hospital system and files. Preoperative demographic data, postoperative complications and mortality of patients with hypoalbuminemia (Low albumin level < 2.5 g/dL) were recorded.
RESULTS: Total number of patients: 87 patients were included in the study. The average age of the patients is 69.3 ± 13.4 years. 12 patients had a history of cardiac surgery and 18 patients had a history of chronic renal failure. Postoperative renal failure developed in 7 patients. Two of them required continuous hemofiltration. 1 patient developed permanent dialysis disease. Respiratory problems developed in 6 patients. Extubation time was prolonged in 3 of them. Pneumonia also developed in the other 3 patients. No cardiac complications developed. Cellulitis developed in 1 patient, minor wound infection in 4 patients, and deep infection in the femoral wound site occurred in 1 patient and required VAC therapy. Sepsis developed in 4 patients. The number of patients with prolonged hospitalization (>7 days) was 37. Rehospitalization within 30 days was 4 patients. 2 of these were due to wound infection. In-hospital mortality occurred in 2 patients and mortality occurred within 30 days in 1 patient.
CONCLUSIONS: It has been observed that patients with hypoalbuminemia have a high rate of prolonged hospitalization and a higher rate of sepsis than the normal population. There is a need for studies comparing normal albumin levels with a high number of patients.
1.37.5. Multifocal Arterial Disease—Carotid, Coronary and Peripheral—Diagnostic Strategy and Therapeutic Management
- 1
Central Mlitary Hospital, Cardiovascular Surgery Clinic, Bucharest, Romania
- 2
Central Military Hospital, Anesthesia Department, Bucharest, Romania
BACKGROUND AND AIM: Atherosclerosis is a global disease affecting multiple organs. The more symptomatic lesion or the lesion with the strongest prognostic impact should be treated first.
Coronary artery disease may coexist with carotid artery stenosis, abdominal aortic aneurysms, and/or peripheral artery disease (PAD).
Recent studies have confirmed that patients with multivascular bed disease have a greater risk for major cardiovascular events than patients with monovascular attempt.
The aim of the study was to see the actual incidence of multifocal arterial disease in vacular patients and the strategy of treatment in order to reduce the periprocedural cardiovascular morbidity and mortality.
METHOD: In 2003 on one year period, on 400 direct arterial revascularisations we had 11 patients with multiple sites of atherosclerotic disease. The decade more affected was 60–70 years old. After 20 years, in 2023, the number of patients increased a lot, at 120, and the patients were older. (decade 70–80 y). Men were more affected.
The lesions should be treated as follows: carotid, coronaries and aorta or peripheral lesions. When two arterial beds are symptomatic (ex: AAA more than 7 cm in diam. or in imminence of rupture associated with left main disease) we can perform simultaneous procedures (open or endovascular), but with more higher mortality rate (25%)
RESULTS: Vascular patients often have concomitant arterial disease affecting more than one territory (35% of pat. on 400 direct arterial revascularisations/year) Identification of silent vascular disease is essential to improve cardiovascular mortality and morbidity rates. Diabetes mellitus, age and male sex were found to be markers of developing multisite arterial disease. The treatment should include also aggressive risk factor management, lifestyle changes, and appropriate drug therapy.
CONCLUSIONS: In conclusion, specific surgical/endovascular therapeutic options available, aggressive medical treatment and vascular disease prevention strategies should be rigorously implemented to best manage the overall atherosclerotic sites.
1.37.6. Comparison of the Protective Effects of Vanillic and Rosmarinic Acid on Cardiac Tissue: Lower Limb Ischemia-Reperfusion Model in Rats
Serhat Hüseyin 1, Adem Reyhancan 1, Ümit Halıcı 2, Orkut Güçlü 1, Salih Tüysüz 1, Burçak Öztorun 3 and Suat Canbaz1
- 1
Department of Cardiovascular Surgery, Trakya University, Edirne, Türkiye
- 2
Department of Cardiovascular Surgery, Samsun Training and Research Hospital, Samsun, Türkiye
- 3
Department of Pathology, Trakya University, Edirne, Türkiye
BACKGROUND AND AIM: The inflammatory response that develops during ischemia and the oxygen-free radicals that proliferate during reperfusion have deleterious effects on the brain, heart and kidneys. In this study, we aimed to compare the effects of vanillic and rosmarinic acid in the prevention of ischemia/reperfusion injury in a rat lower limb ischemia/reperfusion model
METHOD: 32 females Sprague-Dawleys weighing 185–240 g were randomly divided into 4 groups of 8 animals each. Group 1 was designated as control, group 2 as ischemia/reperfusion (I/R), group 3 as ischemia/reperfusion + vanillic acid (I/R + VA) and group 4 as ischemia/reperfusion + rosmarinic acid (I/R + RA). In all groups except the control group, the infrarenal abdominal aorta was clamped and 60 min of ischemia followed by 120 min of reperfusion was performed. Vanillic and rosmarinic acids were administered intrabadominally before the reperfusion phase. At the end of the reperfusion phase, blood samples and hearts were collected and the rats were sacrificed. Biochemical and histopathological examinations were performed on the blood samples and heart tissue.
RESULTS: Myofibrillar edema was most pronounced in the I/R group and less pronounced in the I/R + VA (p = 0.005). Of all groups, TOS and OSI were lowest in the control group, while TAC was highest. While TAC was similar in the I/R + VA and I/R + RA groups, it was significantly higher in these two groups than in the I/R group. While the lactonase activity in the I/R + VA group was similar to the control group, it was significantly higher compared to the I/R and I/R + RA groups.
CONCLUSIONS: Our study shows that vanillic and rosmarinic acids reduce myofibrillar edema in the heart after lower limb ischemia and increase TAC. However, vanillic acid increases the activity of the enzyme lactonase, which is known for its antioxidant effect, more than rosmarinic acid.
1.37.7. Four-Year Outcome of Drug-Coated Balloons for SFA Lesions in Patients with CLI: A Comparison with Traditional Bypass Surgery
- 1
Department of Cardiovascular Surgery, Istanbul University, Istanbul, Turkey
- 2
Department of Cardiovascular Surgery, Altinbas University, Istanbul, Turkey
BACKGROUND AND AIM: The endovascular treatment approach for symptomatic peripheral artery disease has become widely accepted. The effectiveness and safety of drug-coated balloon (DCB) angioplasty for patients with critical limb ischemia (CLI) have been previously established, showing promising results after one year. However, there is limited evidence regarding the long-term durability of this treatment. This study compares the four-year outcomes of DCB angioplasty with traditional bypass surgery in patients with CLI.
METHOD: The study included 187 patients with CLI who were treated over six years (2006–2012) by a single surgical team. From 2006 to 2009, all patients underwent traditional surgery. From 2009 to 2012, the team adopted an endovascular approach using IN.PACT Admiral (Medtronic Inc., Santa Rosa, CA, USA). Data was collected prospectively.
RESULTS: Over the six years, a total of 210 procedures (100 surgeries, 110 endovascular) were performed. 72% of all bypasses were conducted using saphenous vein grafts, with above-knee bypass being the preferred technique in 80% of cases. A 6-mm DCB was used in 41% of patients. Both procedural success rates (98% vs. 99%, NS) and clinical success rates (99% vs. 99%, NS), as well as operative mortality (3.7% vs. 2%, NS), were similar in both groups. Primary Patency for the DCB and bypass groups was 91.8% vs. 88.9% at 12 months (p = 0.31), 82.7% vs. 82.8% at 24 months (p = 0.28), and remained similar at four years (66.4% vs. 68.8, p = 0.08). Freedom from clinically driven Target Lesion Revascularization (TLR) at 12 months was similar in both groups (87.6% vs. 85%, p = 0.33). The rates of clinically driven target lesion revascularization were 29.2% and 26.1% (p = 0.07) for the DCB and surgery groups, respectively.
CONCLUSIONS: DCB angioplasty shows comparable results to traditional surgery in treating CLI, even after four years. The effectiveness and safety of DCBs in more complex lesions need to be further investigated through randomized trials.
1.37.8. Femoral Artery Pseudoaneurysm Due to Sports Injury in a Patient with Osteochondroma
Ilker Hasan Karal, Emrah Ereren and Aşkın Kılıç
Department of Cardiovascular Surgery, Samsun University Faculty of Medicine, Samsun, Türkiye
Osteochondromas are the most common benign bone tumors and mostly arise from the metaphysis of long bones. Lesions are mostly asymptomatic and found incidentally. However, many complications, including neurovascular compression and vascular injuries, have been published. We present a case of femoral artery pseudoaneurysm due to sports injury in a patient with osteochondroma. A 19-year-old male patient was admitted to the emergency room with complaints of severe pain and swelling in his right leg. The patient, who had osteochondroma resection surgery on his left distal femur 1 month ago, stated that he had severe pain since he overflexed his right knee while playing football 1 week before his admition. Doppler ultrasonography revealed popliteal and crural vein thrombosis (DVT) and turbulent flow vessel dilation reaching approximately 6 × 4 cm in the medial distal part of the right thigh. The patient’s 3D lower extremity CT angiography revealed widespread osteochondromas in both lower extremity bones and a hypodense area compatible with active bleeding on the anterolateral side of the right thigh. It was thought that the bleeding was due to a pseudoaneurysm resulting from oseochondroma in the distal superficial femoral artery, and the patient was taken into emergency surgery. During surgery, the pseudoaneurysm sac was resected and the sperficial femoral artery was primarily repaired. The osteochondroma adjacent to the artery was resected. The patient was discharged with anticoagulant medication without any complication. Doppler ultrasonography performed in the first postoperative month, the arterial and venous systems was patent. While vascular doppler ultrasonography is sufficient for the diagnosis of pseudoaneurysm, CT-angiography is more important in detecting the cause of pseudoaneurysm. We think that osteochondromas should be considered as a priority, especially in cases of spontaneous vascular injuries after sports. While an endovascular approach is suitable for many pseudoaneurysms, an open surgical approach is mandatory for cases like osteochondroma.
1.37.9. BTK&BTA Full Vessels’ Recanalization
Eleonora Tundo
Interventional Radiology Unit, Diabetic Foot Department, Policlinic of Abano, Abano Terme (PD), Italy; University of Padua, Padua, Italy
BACKGROUND: Male, 70 yrs old, DMT2 on insulin, inferior limbs’ diabetic neuro-vasculopathy, diabetic retinopathy, dyslipidemia. Previous amputation of left foot’s 1st toe and ray and of the 2nd metatarsal bone. Plantar ischemic lesion of the 3rd–4th MPJ with tendon exposure.
CASE REPORT: This is a case of failed attempts. Each first choice strategy was unsuccessful. Therefore, this surgery turned out to be perfect in order to remember that you always need a plan B.
We performed an antegrade access from CFA. The angiograms were physiological until the femoropopliteal segment. IOA was the only opened vessel of the BTK district, ATA showed a long occlusion from the proximal to the distal third, PT was also occluded from the medial third on. At foot level a slight DP was visible, plus collaterals.
Firstly, we engaged ATA with a 014 workhorse guidewire, we crossed the CTO but we were not able to re-enter the lumen. Therefore, we entered IOA and arrived in lumen in the distal third of ATA through a connection collateral between the two arteries. We retrogradely crossed ATA and we performed angioplasty.
We tried to reopen PT in antegrade fashion, without success. Thus, we punctured the distal third of PT and engaged the lumen in retrograde manner. We performed a rendez-vous technique through a navicross catheter from below plus OTW balloon from above and we succeeded in the angioplasty of PT.
Since the PT was now fully opened, we tried going further and crossing the lateral plantar artery’s CTO, but we failed again. Hence, we engaged DP in antegrade way, we crossed the plantar arch and went up to the PT. It was possible then to do the PTA of lateral plantar artery.
Eventually, thanks to plan Bs, we succeeded in a complete reconstruction of the BTK and BTA vessels.
1.37.10. Preserving Limb Integrity: Successful Angioplasty Intervention in Chronic Diabetic Foot Ulcer in Indonesia
- 1
Faculty of Medicine, Airlangga University, Surabaya, Indonesia
- 2
Cardiothoracic and Vascular Surgery Department of PHC General Hospital, Surabaya, Indonesia
BACKGROUND: Diabetic foot ulcers (DFUs) present formidable challenges in treatment, often culminating in amputation due to complications associated with impaired wound healing. Despite these challenges, emerging evidence highlights promising alternative interventions such as angioplasty, providing prospects for limb salvage and enhanced outcomes in select cases. With Indonesia ranking as the 5th country globally in terms of diabetes prevalence, the nation faces a significant burden of diabetic foot complications. The prevalence of DFUs, ranging from 7.3% to 24%, underscores the pressing need for effective interventions to mitigate their impact on population health.
CASE: In this case series, we present 10 cases of chronic DFUs in patients previously referred from other hospitals where major amputation was recommended. Contrary to conventional management approaches favoring amputation, all patients underwent angioplasty at our hospital, resulting in successful limb salvage and wound healing. The series details 10 cases of chronic DFUs in patients aged between 62 and 71 years, predominantly female. These individuals, with mean durations of diabetes ranging from 3.5 to 7 years, presented with comorbidities including smoking and hypertension. Angioplasty emerged as the treatment modality across all cases. Encouragingly, no major procedural complications were encountered, and the duration of wound healing post-angioplasty varied from 3 to 6 months. Follow-up assessments revealed notable improvements in clinical presentation, including reduced claudication and resting pain. This case series highlights the effectiveness of angioplasty as a limb-sparing intervention in managing DFUs, particularly within the Indonesian context. By preserving limb integrity and promoting wound healing, angioplasty holds promise in mitigating the impact of DFUs on patient morbidity and mortality, enabling some patients to avoid major amputation altogether and others to reduce the extent of amputation while maintaining functional mobility.
1.37.11. A Case of the Aneurysm of Bovine Mesenteric Vein Graft
- 1
Department of Cardiovascular Surgery, Etlik City Hospital, Ankara, Türkiye
- 2
Department of Cardiovascular Surgery, Sincan Training and Research Hospital, Ankara, Türkiye
The vascular graft aneurysm is a rare complication after vascular surgery. Xenografts may be associated with complications and true or false aneurysm formation is major complication of these grafts. It is suggested that proteolytic digestion of foreign biomaterials mediates aneurysm formation. Collagenase exposure may also contribute to aneurysm formation in organic materials. A 54 years old man was presented with severe pain and pulsatile mass of his right leg. The right iliofemoral bypass and bilateral above knee femoropopliteal bypass was performed four years ago. The iliofemoral graft was the PTFE and the femoropopliteal grafts were the bovine mesenteric vein grafts (Procol®). There was massive pulsatile mass on right leg along the bovine mesenteric vein graft. All pulses were palpable. Computerized tomography and MR angio were demonstrated extensive aneurysm of the right femoropopliteal bovine mesenteric vein graft. The patient was operated because of the bovine mesenteric vein graft aneurysm. Aneurysmectomy and femoropopliteal bypass with internal mammary artery graft was performed. Microscopic examination of the removed graft material revealed foreign body reaction. The vascular bioprostheses have been used since 1970s. Indication of vascular bioprostheses are mainly hemodialysis access graft in chronic renal failure patients and various bypass procedures. The complications of the xenografts are thrombosis, infection and true or false aneurysm. The false aneurysms are more common. Proteolytic digestion of foreign biomaterials mediates aneurysm formation. Collagenase exposure may also contribute to aneurysm formation in organic materials. The aneurysm more commonly occur in proximally grafts and the risk increases by time. There is high risk for rupture of the aneurysm. Excision of the aneurysm and implantation of the new graft are indicated.
1.37.12. Endovascular Treatment of the Right Subclavian Artery Occlusion Due to Radiotherapy
- 1
Department of Cardiovascular Surgery, Etlik City Hospital, Ankara, Türkiye
- 2
Department of Cardiovascular Surgery, Sincan Training and Research Hospital, Ankara, Türkiye
After radiotherapy, various degrees of damage occur in the arteries in the treated area, depending on the radiation dose (>50 Gray). This effect is higher in patients with hypertension, hyperlipidemia and smoking. Ischemic complications develop depending on the exposure rate. The patient, who received radiotherapy to the right upper mediastinum and neck region after lobectomy due to lung cancer, developed skin burns due to radiotherapy, and 6 months after the treatment, claudication complaints began on the right arm. Over the last month, his pain has become increasingly severe, and his right hand has become cold, bruising, and ischemic wounds have developed on his fingertips. There was no right upper extremity pulse. There was skin scarring and stiffness on the right apex and neck. Right subclavian and axillary artery occlusion was detected in RDUSG. Angiography showed that the right subclavian artery was completely occluded 1 cm after its origin, there was serious stenosis in the 4 cm section at the axillary artery level, but there was arterial filling, and the distal axillary artery, brachial, radial and ulnar arteries were normal. The procedure was performed from the right brachial artery with imaging support from the right femoral artery. The thrombus located in severe stenosis in the subclavian artery was removed with ThromCath thrombectomy catheter system, and minimal lumen patency was achieved. The procedure was performed from the right brachial artery with imaging support from the right femoral artery. The thrombus located in severe stenosis in the subclavian artery was removed with the Thromcath aspiration thrombectomy catheter, a 9 × 50 mm Zeus CC CoCr balloon expandable stent was implanted. Post dilation was performed with a 9 × 60 mm high pressure balloon. Compared to open surgery and endovascular intervention in arterial occlusions due to radiotherapy, endovascular intervention is safe and low risk.
1.37.13. Approach to Type I Endoleak in a Case of the Superficial Femoral Artery Aneurysm Treated with a Covered Stent
- 1
Department of Cardiovascular Surgery, Etlik City Hospital, Ankara, Türkiye
- 2
Department of Cardiovascular Surgery, Ankara Education and Research Hospital, Ankara, Turkiye
- 3
Department of Cardiovascular Surgery, Sincan Training and Research Hospital, Ankara, Türkiye
The superficial femoral artery aneurysm is uncommon. The patients present with limb ischemia, distal embolization, or rarely rupture. Aneurysm is diagnosed by ultrasound and computed tomography. The treatment is usually surgical. Aneurysm excision and graft interposition or aneurysm ligation and arterial bypass are surgical treatment options. Endovascular repair using a covered stent of the aneurysm is an alternative treatment method in the patients with suitable anatomy. A 41-year-old man presented with pain and swelling in his left thigh. The patient had surgery for the right superficial femoral artery aneurysm 4 years ago. An aneurysm with a diameter of 60 mm and involving the middle segment of the left superficial femoral artery was detected by ultrasound. Arterial blood flow distal to the aneurysm was normal. The aneurysm was treated by endovascular procedure. A covered stent was implanted to the site of the aneurysm. Minimally type I endoleak was detected after the procedure. No additional procedure was performed for endoleak. One month later, the leak was observed to have resolved spontaneously. If type I endoleak is low-flow, spontaneous healing is likely. No additional procedure is required.
1.39. VASCULAR AND ENDOVASCULAR » Thoracic Aorta
1.39.1. Hybrid Aortic Arch Repair in Patients Who Have Type-I Aortic Dissection After Cardiac Surgery
Mete Kubilay Kasap, Ömer Faruk Doğan, Nazenin Durak and Özgür Çoban
Sbü Adana City Research and Training Hospital, Adana, Turkey
BACKGROUND AND AIM: Traditional aortic dissection (AD) surgery involves resect the primary intimal tear and re-approximate the intima and adventitia. However, residual dissection flap and false lumen(s) which is cause of mortality during follow up period persist in aorta in 76% of patients. Our purpose of this study was to evaluate clinical outcomes after use of hybrid techniques in patients with AD.
METHOD: Fifty-five patients who have already undergone cardiac operation included between 2014 to 2023. The mean age of the patients was 62.3 years. Aortic valve replacement (AVR) (n = 19), Benthall operation (20), and AVR and separated ascending aortic repair (16) using tube graft were the primary operations. Frozen elephant trunk (ET), revascularisation of the supra-aortic branches concomitant with TEVAR, and stent-graft repair without surgery (fenestrated and/or branched TEVAR) were used in our cohort. We used flow directed stent graft in 26 patients with a dissecan abdominal aortic aneurysm (47.2%).
RESULTS: Postoperative course was uneventful except 1 patient. This patient dead after surgery due to multiorgan failure. Postoperative hemiparesis was detected in 2 patients. Magnetic resonance imaging showed embolic event in parietal lobe in these patients (6.3%). The median ECC and an aortic cross clamp were 126 and 79 min, respectively. Mean length of hospital staying time was 9.4 days (5–19 day). No revision was needed postoperatively. Low out-put syndrome was detected 8 patients. During follow-up period (44 months) the rate of death was at 4%. False lumen thrombosis on descending thoracic aorta was obtained in all survived patients. The rate of aortic reintervention was 3.3% on abdominal aorta.
CONCLUSIONS: To provide visceral organ malperfusion, false aortic aneurysm, persistancy or residual false lumen which cause of aortic rupture, we propose hybrid procedure in these patients. Flow directed stent graft after repair of AD may provides organ malperfusion. This method seems to be effective method to inhibit unexpected complications mid- and long-term complications.
1.39.2. Primary Hydatid Cyst of the Thoracic Aorta
Zied Ben Ayed, Mohamed Seddik, Nawel Hchaichi, Mohamed Fendi, Imen Smaoui, Zied Chaari and Imed Frikha
Department of CardioVascular and Thoracic Surgery, Habib Bourguiba University Hospital, Sfax, Tunisia
BACKGROUND AND AIM: Tunisia is one of the endemic areas for hydatid diseases, the aortic location is exceptional, especially primitive hydatidosis.
METHOD: We report the case of a 55-year-old woman who had consulted for pain and coldness of the left lower limb from one week.
A computed tomographic angio-gram showed a multivesicular and fluid-density mass intimately contiguous to the descending thoracic aorta seen on an endoluminal subtraction image and hydatid cysts in the spleen.
RESULTS: The surgical approach was adopted via a thoracophrenolombotomy with right femorofemoral bypass.
The surgery consisted for a complete resection of the destroyed aortic portion, and continuity was restored by an aortoaortic bypass using a Dacron Graft prosthesis.
Then, thrombectomy of the left iliac artery and extraction of a fresh hydatid thrombus.
The surgical procedure was completed by a splenectomy.
Postoperative follow-up was uneventful.
After 6 months, computed tomographic angiography showed a patent bypass.
CONCLUSIONS: The aorta is rarely affected by hydatidosis, the aortic localization is serious and can be responsible of systemic dissimulation, The treatment of hydatidosis is essentially surgical and consisting of the total removal of hydatid cysts, making sure to take all possible precautions not to open the cysts.
1.39.3. Concomitant Kommerell Diverticulum, Aberrant Left Subclavian Artery and Right Aortic Arch in an Adolescent Patient
- 1
Department of Cardiovascular Surgery, Yalova Education and Research Hospital, Yalova, Turkey
- 2
Department of Cardiovascular Surgery, Kocaeli University Faculty of Medicine, Kocaeli, Turkey
BACKGROUND AND AIM: Kommerell diverticulum is a congenital dilatation of the aortic arch at the origin of the aberrant right subclavian artery (ARSA) or aberrant left subclavian artery (ALSA). The association of right aortic arch and ALSA is rare and is an anatomical feature observed in approximately 0.06% to 0.1% of the healthy population. They can cause a wide range of clinical symptoms from critical respiratory distress in the neonatal period due to compression of the trachea or esophagus to asymptomatic and diagnosed in adulthood. There is a risk of spontaneous aortic rupture even in asymptomatic adults. Therefore, it has been reported that surgery should be performed even in the presence of mild compression symptoms, with conservative management in asymptomatic patients and surgery in symptomatic patients.
METHOD: In this case report, ALSA associated with right aortic arch and Kommerell diverticulum in a 17-year-old female adolescent is discussed. The patient who presented with dyspnoea and dysphagia had significant focal thinning in the luminal calibration of the oesophagus near the level of the aortic knob on oesophageal-gastroduodenal-radiography, suggesting that it may be due to external compression. CT-angiography shows right arcus aorta, left subclavian artery is aberrant behind the trachea and oesophagus and its orifice is wide (13 mm).
RESULTS: Operation was decided due to the symptoms. Following left posterolateral thoracotomy, the adhesions between the oesophagus and the left subclavian artery were dissected. Adhesions on the commerell diverticulum were separated after ligamentum arteriosum division between the pulmonary artery and subclavian artery. Left carotid and subclavian artery were anastomosed with ptfe graft. Kommerell diverticulum was excised with side-clamp placed on the descending aorta. The aorta was repaired primarily and the patient was taken to the post-operatif intensive care unit. The patient was discharged 15-days after the operation.
CONCLUSIONS: The key points for symptom regression are complete resection of the diverticulum, ligamentum arteriozum division, removal of adhesions. In addition, revascularisation of the subclavian artery is also important.
1.39.4. Is Female Gender Really a Predictor of Worse Outcome During TEVAR Procedures?
Gabriele Piffaretti 1, Francesca Mauri 1, Sara Speziali 2, Gaddiel Mozzetta 3, Sergio Zacà 4, Maria Cristina Cervarolo 1, Raffaele Pulli 2, Giovanni Pratesi 3, Aaron Thomas Fargion 2, Martina Bastianon 3, Andrea Cucci 4 and Carlo Pratesi 2
- 1
Vascular Surgery—Department of Medicine and Surgery, University of Insubria, Varese, Italy
- 2
Vascular Surgery—Cardio-Thoraco-Vascular Department, University of Florence, Florence, Italy
- 3
Vascular Surgery—Department of Integrated Surgical and Diagnostic Sciences, University of Genoa, Genova, Italy
- 4
Vascular Surgery—Department of Emergency and Organ Transplants, University of Bari, Bari, Italy
BACKGROUND AND AIM: To evaluate gender-related outcomes during endovascular treatment of thoracic and thoraco-abdominal aortic pathologies (TEVAR).
METHOD: Multicenter, retrospective, observational cohort study based on a shared registry of four academic centers. All cases of TEVAR between November 2001 and April 2023 were identified. Primary outcomes: hospital and cumulative survival. Secondary outcomes: complications related to vascular access and freedom from TEVAR-related reintervention. Outcomes were stratified by clinical scenario (elective vs. emergency), extent of disease (thoracic vs. thoraco-abdominal) and type of aortic disease (degenerative atherosclerotic vs. dissection-related vs. traumatic).
RESULTS: We analyzed 749 patients (98.0%): 214 (28.6%) females and 535 (72.4%) males. The median age was 72 years (IQR, 65–78), higher in females [74 (IQR, 68–79) vs. 71.5 (IQR, 64–78), p = 0.001]. Hospital mortality was not influenced by gender by clinical scenario (OR: 1.3, p = 0.105), extent (OR: 1.4, p = 0.170), and type of pathology (OR: 1.4, p = 0.331). The estimated 5-year cumulative survival was 67% (SE: 0.02; 95% CI: 62.7–70.9), without gender-related differences by clinical scenario (Log-rank, p = 0.145), extent of pathology (Log-rank, p = 0.141) and type of aortic disease (Log-rank, p = 0.182). Access complications did not differ either by type (OR: 1.1, p = 0.798) or when stratified by emergency (OR: 1.1, p = 1.0) or type of aortic pathology (OR: 1.6, p = 0.265). The estimated 5-year freedom from reoperation was 88% (SE: 0.02; 95% CI: 84.0–91.1), with no differences by clinical scenario (Log-rank, p = 0.491), extent of pathology (Log-rank, p = 0.868) and type of aortic pathology (Log-rank, p = 0.585).
CONCLUSIONS: In our “real world” experience, female gender was not a worsening factor for TEVAR procedures.
1.39.5. Mini-Hemiarch Repair for Ascending Aortic Aneurysm
Dmitri Panfilov and Boris Kozlov
Cardiology Research Institute, Tomsk National Research Medical Center, Russian Academy of Sciences, Tomsk, Russia
BACKGROUND AND AIM: Minimal invasive surgery is increasingly used for the treatment of thoracic aortic disease. The objective of the study was to analyze early outcomes of mini-hemiarch repair in patients with ascending aortic aneurysm
METHOD: From January 2020 to December 2023, a total of 116 ascending aortic surgical procedures were performed in our centre. Of these, 87 patients had ascending aortic aneurysm. These patients received ascending aortic replacement with concomitant hemiarch repair. Patients were divided into 2 groups depending on surgical approach: full sternotomy (FS, n = 54) and mini-J sternotomy (MS, n = 33). Pre-, intra- and postoperative data were analyzed
RESULTS: Overall in-hospital mortality was 2 (3.7%) vs. none in FS group and MS group, respectively (p = 0.564). There was no permanent and temporary cerebral neurological deficit in both groups. The rate of postoperative respiratory failure, acute kidney injury was 5.6% versus 3% (p = 0.061) and 9.3% versus none (p < 0.001) in FS group and MS group, respectively. Re-exploration for bleeding was required in 1 (1.9%) FS patient and in 1 (3%) MS patient (p = 0.238).
CONCLUSIONS: Ascending aortic replacement with hemiarch repair for ascending aortic aneurysm through mini-J sternotomy is an effective and safe approach with acceptable early outcomes
1.39.6. Integrated Multi-Omics Profiling Reveals Neutrophil Extracellular Traps Promote Aortic Dissection
Yufei Zhao, Fandi Mo, Zheyun Li, Lixin Wang and Weiguo Fu
Zhongshan Hospital Fudan University, Shanghai, China
BACKGROUND AND AIM: Adverse aortic remodeling increases the risk of aorta-related adverse events (AAEs) after thoracic endovascular aortic repair (TEVAR) and affects the overall prognosis of aortic dissection (AD). It is imperative to delve into the exploration of prognostic indicators to streamline the identification of individuals at elevated risk for postoperative AAEs, and therapeutic targets to optimize the efficacy of TEVAR for patients with AD.
METHOD: We performed proteomic and single-cell transcriptomic analyses of peripheral blood samples and aortic lesions, respectively, from patients with AD and healthy subjects. We performed in vivo experiments to further confirm the effect of inhibiting NETs. Kaplan-Meier and Cox regression analysis were used to identify independent risk factors for AAEs.
RESULTS: Integrated multi-omics profiling identified highly phenotype-associated macrophages, which frequently interacted with neutrophils via CXCL3/CXCR2 axis, and promoted neutrophil extracellular traps (NETs) in driving and fueling the development of AD. Increased NETs formation is a defining feature of systemic immunity and aortic microenvironment of AD. Furthermore, we demonstrated that the level of citrullinated histone H3 (CitH3), a NETs associated marker, could serve as a risk factor for AAEs following endovascular therapy. Inhibiting NETs formation through the blockade of CitH3 alleviated the progression and rupture of AD in mice.
CONCLUSIONS: The multi-omics profiling reveals NETs formation features in the development of AD. NETs associated markers could facilitate the risk stratification and prognostic evaluation, and might serve as potential therapeutic targets of patients with AD.
1.39.7. Mild Versus Moderate Hypothermia for Cerebral Protection in Aortic Arch Surgery: A Meta-Analysis of Nine Studies
Navneet Singh and Parma Nand
Department of Cardiothoracic Surgery, Auckland City Hospital, Auckland, New Zealand
BACKGROUND AND AIM: Open thoracic aortic surgery remains the mainstay of treatment for type A aortic dissections and aortic arch aneurysms. In order to provide neurological protection when operating on the aortic arch, hypothermia is commonly used intraoperatively to reduce cerebral metabolic demand and minimise the impacts resulting from temporarily-reduced intracerebral blood flow. Most centres use moderate (20–28 °C) or deep (14–20 °C) hypothermic circulatory arrest for this purpose. However, these low temperatures are known to have negative consequences on visceral organ function and coagulopathy. We hence aimed to investigate whether mild hypothermia (>28 °C) achieves acceptable postoperative neurological outcomes (stroke rates) as compared to moderate hypothermia during aortic arch surgery.
METHOD: A systematic review and meta-analysis of all randomised and non-randomised studies investigating our study aim was undertaken as per the PRISMA guidelines. Review Manager 5.4 software was utilised for statistical analyses.
RESULTS: Nine observational studies met inclusion criteria with a total sample size of 1357 patients. No randomised controlled trials were available on this topic. Mild hypothermia (with selective cerebral perfusion) correlated with statistically significantly reduced postoperative permanent neurological dysfunction (strokes) as compared to moderate hypothermia (odds ratio 0.39, 95% confidence interval 0.24–0.64, p = 0.0001). Mild hypothermia also correlated with significantly reduced rates of postoperative acute renal failure (odds ratio 0.51, 95% confidence interval 0.33–0.80, p = 0.003). There was no difference in the rate of re-exploration for bleeding between the two groups (odds ratio 0.66, 95% confidence interval 0.42–1.03, p = 0.07).
CONCLUSIONS: Mild hypothermia—in conjunction with selective cerebral perfusion—may be a safe alternative to moderate hypothermia for providing neurological protection during circulatory arrest in aortic arch surgery. However, robust randomised data is required to corroborate this theory.
1.39.8. Indigenous Ethnic Disparities in Patients Undergoing Repair of Ascending Aortic Aneurysms in Aotearoa New Zealand: A Prospective Cohort Study
Navneet Singh and David Haydock
Department of Cardiothoracic Surgery, Auckland City Hospital, Auckland, New Zealand
BACKGROUND AND AIM: Ascending aortic aneurysms carry a high morbidity and mortality risk; surgical treatment is often indicated. There is no published work investigating the relationship between ethnicity and the incidence of and outcomes from ascending aortic aneurysm surgery in the unique indigenous Aotearoa New Zealand population. We aimed to review the ethnicity trends for New Zealand patients undergoing elective ascending aortic aneurysm surgery.
METHOD: A prospectively-maintained hospital database was used to identify patients receiving standalone elective ascending aortic surgery (with or without aortic valve intervention) for aneurysm repair from January 2015–July 2019. Outcomes were sub-stratified by ethnicity and statistically analysed using two-tailed z-tests and t-tests.
RESULTS: During the 4.5-year study period, a total of 134 patients underwent elective surgery to treat isolated ascending aortic aneurysmal disease; this included New Zealand European, indigenous Maori and Pacific Island patients. Approximately 20.1% of patients were Pacific, which is significantly greater than their overall New Zealand population proportion of 8.1% (p < 0.00001). There was no difference in risk factors (such as hypertension, gender, smoking status or genetic aortopathy) for developing aortic aneurysms between Pacific and non-Pacific patients. There were no significant ethnic differences in 30-day post-operative mortality or stroke rates.
CONCLUSIONS: This is the first ever study investigating elective ascending aortic aneurysm surgery in New Zealand by ethnicity. Pacific patients are over-represented in aortic surgery case numbers; this is not explained by their underlying incidence of aneurysm risk factors. This suggests that the Pacific population may have an underlying predisposition that puts them at higher risk for developing ascending aortic aneurysms which require surgery.
1.39.9. Comparison of Controlled Hypotension Methods in Patients Undergoing Proximal Zone TEVAR
Osman Eren Karpuzoğlu, Anıl Karaağaç, Osman Murat Baştopçu, Ferhat Tümkaya and Naci Cem Aydoğdu
Department of Cardiovascular Surgery, Dr. Siyami Ersek Training and Research Hospital, Istanbul, Turkey
BACKGROUND AND AIM: Optimal placement and maximizing seal zone are important for long-term outcomes after thoracic endovascular aortic repair (TEVAR). The aortic impulse force exerted on the stent-graft is higher with more proximal landing zones, especially in Zone 0, 1 and 2 applications, which may lead to difficulties in precise placement. Different methods such as pharmacologic hypotension (PH), rapid ventricular pacing (RVP), and cardiac inflow occlusion can be used to minimize aortic impulse force during stent-graft deployment. In this study, we aimed to compare the methods used in our clinic to create controlled hypotension in proximal TEVAR applications.
METHOD: The study included 47 patients who underwent proximal TEVAR (Zone 0–1-2) between January 2018 and March 2024 in our center. Maximum sealing zone was aimed in all patients. Systolic blood pressure was targeted to be between 60–80 mmHg in all of the patients during stent-graft deployment. Demographic, intraoperative and postoperative data of the patients were analyzed.
RESULTS: PH was performed in 34 patients (72.3%) and RVP in 13 patients (27.7%). Deviation from the target occurred in 11 patients (32.4%) in the PH group, while deviation from the target was observed in 4 patients (30.8%) in the RVP group (p = 0.999). The mean target deviation distances were 1.8 ± 3.2 mm in the PH group and 2.00 ± 3.43 mm in the RVP group (p = 0.890). Establishing a normal hemodynamic state was faster in patients in the RVP group.
CONCLUSIONS: Although PH is frequently used to induce controlled hypotension in endovascular aortic repair procedures, RVP can provide similar outcomes with more rapid normalization of hemodynamics after deployment. We believe that RVP can be safely used to create controlled hypotension especially in proximal TEVAR applications.
1.39.10. The Effect of Left Subclavian Artery Revascularization on Outcomes After Zone 2 TEVAR
Osman Eren Karpuzoğlu, Anıl Karaağaç, Osman Murat Baştopçu, Ferhat Tümkaya and Naci Cem Aydoğdu
Department of Cardiovascular Surgery, Dr. Siyami Ersek Training and Research Hospital, Istanbul, Turkey
BACKGROUND AND AIM: Careful assessment of the extent of the aortic pathology and adequate sealing zone are important for procedural success and long-term outcomes in TEVAR. Especially in pathologies originating close to the left subclavian artery (LSA), Zone-2 TEVAR is preferred. The risk of neurological complications (CVA, paraplegia) may be higher if LSA revascularization is not performed in these patients. Although interventions for the LSA may sometimes be neglected or postponed in emergent cases, current literature recommend subclavian revascularization before TEVAR in elective cases. With the advances in endovascular techniques, revascularization with fenestrated TEVAR and chimney stents are also possible. In this study, we compared outcomes of patients according to LSA revascularization status after TEVAR.
METHOD: The study included 32 patients who underwent Zone 2 TEVAR between 2018–2024. Demographic, intraoperative and postoperative data of the patients were analyzed along with CT-angiography and procedural images.
RESULTS: Technical success was achieved in all patients. While no endoleak was observed in the early postoperative period, 1 patient (3.1%) was operated for type 1 dissection. Migration of the TEVAR graft was observed in only 1 patient (3.1%) without endoleaks. In 21 patients (65.6%), LSA revascularization was performed with different methods before or during the procedure. LSA revascularization methods were caroticosubclavian bypass in 18 patients, chimney stents in two patients and a fenestrated TEVAR in 1 patient. Neurological complications were observed in 4 of 11 patients (36.4%) who did not undergo revascularization before or during the procedure, whereas neurological complications were observed in 4 of 21 patients (19.0%) who did (p = 0.397).
CONCLUSIONS: TEVAR in pathologies located in proximity of the LSA are more challenging than distal pathologies. Zone-2 TEVAR is a good alternative in this patient group to achieve good long-term results. Revascularization of the LSA in these patients is of great importance in terms of early neurological complications and can be performed with surgical or endovascular methods.
1.39.11. Preliminary Results of Aortic Arch Aneurysm and Dissection Endovascular Repair with Physician-Modified Endografts
Andrea Kahlberg, Carlo Campesi, Daniele Mascia, Annarita Santoro, Roberto Chiesa and Germano Melissano
Department of Vascular Surgery, “Università Vita-Salute” San Raffaele Hospital, Milan, Italy
BACKGROUND AND AIM: To assess the early outcomes of physician-modified endovascular grafts (PMEGs) for total endovascular aortic arch aneurysm or dissection repair.
METHOD: A single-center retrospective analysis included all patients submitted to PMEG implantation in the aortic arch between January 2023 and March 2024. Indications included: zone 1/2 lesions, or zone 0 saccular aneurysms arising from the arch lesser curvature; proximal neck diameter 24–40 mm, with 20-mm minimum length. Arches presenting parietal thrombus, severe calcification, or associated infection were excluded. PMEG indication was driven by urgency (symptomatic/unstable lesion), or anatomical exclusion from custom-made device use.
RESULTS: Nine patients (6 males; median age 73 years) were included, presenting 3 degenerative and 6 dissecting aortic arch aneurysms. In 3 cases a single preloaded fenestration for the left subclavian artery (LSA) was performed, while in 6 cases an additional proximal large fenestration for the brachiocephalic trunk and the left common carotid artery (LCCA) was realized. Technical success was obtained in 8 patients (89%). In one case the procedure was aborted due to failure to rotate and position the endograft, given extreme abdominal and thoracic aortic tortuosity. No deaths occurred at 30 days. One patient presented asymptomatic LCCA occlusion at 1 month treated by means of LSA-LCCA bypass. No type endoleak, conversion to open surgical repair, aortic rupture, or paraplegia was observed at 1, 3, and 6 months.
CONCLUSIONS: Single or double fenestrated PMEGs may be used in selected aortic arch pathologies (urgent or unsuitable for custom-made devices), showing preliminary promising early results, and unexpected low rate of reinterventions and major complications in our initial experience
1.39.12. Initial Ukrainian Experience of Total Arch Replacement by Frozen Elephant Trunk Operation Technique
Lubomyr Kulyk 1, Vitalii Kravchenko 2, Bogdan Cherpak 2, Igor Zhekov 2, Oleksandr Tretiiak 2 and Vasyl Lazoryshynets 2
- 1
Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
- 2
M.Amosov National Institute of Cardiovascular Surgery of the National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine
BACKGROUND AND AIM: Ongoing development of cardiovascular technologies has made it possible to carry out simultaneous replacement of the ascending, arch and descending thoracic aorta (frozen elephant trunk operation).
METHOD: From 2020 to 2024 in the National M. Amosov ICVS of the NAMS of Ukraine, operated on 797 patients with different kind of aortic pathology, 256 of them were admitted with TAAD; 55 operation of total arch replacement and 25—frozen elephant trunk operation (FET) were performed. Patients age were 36–68 y.o, mean—54.2 ± 6.4; 18 (72.0%) patients are male. Concomitant CAD had 6 (24.0%), COPD—8 (32.0%), CRF—5 (20.0%), DM—5 (20.0%), pulmonary hypertension—3 (12.0%), severe mitral insufficiency—2 (8.0%). Three patients had right aberrant subclavian artery—a.lusoria. Twelve pts (48.0%), had cardiac operation previously. The causes of aortic injury were: acute type A aortic dissection—1 (4.0%); chronic type A aortic dissection—12 (48.0%), non A non B aortic dissection—5 (20.0%), chronic type B aortic dissection—2 (8.0%); blunt aortic injury (BAI)—2 (8.0%), TAAA—3 (12.0%). Simultaneously with the FET, we performed Jacoub operation—2, CABG—6 (1–3), MV repair—2, TV plication—4. All operation we profound with 25 °C hypothermia and ACP for all three cerebral vessels. We used E-Vita Open Plus—14 and E-Vita Open Neo—11. Three operations we operated on urgently, other planned.
RESULTS: Hospital mortality—8.0%. The reasons of death were stroke and severe pulmonary insufficiency respectively. Two patients had neurological complication—permanent paraplegia and transient stroke. Renal failure needed temporary dialysis—3. Bleeding, needed re-thoracotomy—1. Prolonged ventilation—4 pts.
CONCLUSIONS: FET operation allowed treatment of complex patients with extensive thoracic aortic diseases with satisfactory results.
1.39.13. Gene Expression Profile of Interleukin 8 & Interleukin 18 Pathways in Veins and Aorta
Melvin Alferd Tokpah 1, Ozlem Balcioglu 2, Aya Ismail Badeea 1, Ali Askin Korkmaz 2, Barcin Ozcem 2 and Mahmut Cerkez Ergoren 1
- 1
Department of Medical Genetics, Faculty of Medicine, Near East University, Nicosia, Cyprus
- 2
Department of Cardiovascular Surgery, Faculty of Medicine, Near East University, Nicosia, Cyprus
BACKGROUND AND AIM: This research aimed to investigate the expression pathways of IL-8 and IL-18 genes in veins and aorta tissues obtained from patients with various cardiovascular conditions. Interleukins play crucial roles in immune response regulation, and understanding their expression in different tissues is vital for further studies. While previous research has focused on various specimens like blood and cardiac muscles of animals, there’s limited data on human vein and aorta tissues
METHOD: Tissue samples were collected from patients diagnosed with cardiovascular diseases. RNA extraction, cDNA synthesis, and PCR techniques were employed to analyze gene expression levels. The study included 103 samples, categorized into patient and control groups.
RESULTS: Results indicated significant differences in the expression levels of IL-8 and IL-18 between veins and aorta tissues, both in control and patient groups. IL-18 was found to be primarily expressed in both tissues, with implications for biomarker status and underlying health conditions. However, the exact role of IL-18 in inflammation remains unclear, warranting further research.
The study suggests that aorta tissues could serve as a valuable source for understanding IL-18 expression and regulation. Given the importance of interleukin screening across populations and its significance in various biological activities and diseases, integrating IL screening into healthcare systems is crucial.
CONCLUSIONS: This research sheds light on the expression patterns of IL-8 and IL-18 in cardiovascular tissues, underscoring their potential as biomarkers and emphasizing the need for further investigation into their roles and regulation mechanisms.
1.39.14. Total Endovascular Arch Replacement for a Non-A, Non-B Aortic Dissection
Konstantinos Tzimkas Dakis 1, Konstantinos Spanos 1, George Kouvelos 1, George Volakakis 1, Metaxia Bareka 2, Grigorios Giamouzis 3, Eleni Arnaoutoglou 2 and Miltiadis Matsagkas 1
- 1
Vascular Surgery Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Italy
- 2
Anesthesiology Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Italy
- 3
Cardiology Department, University Hospital of Larissa, Medical School of Larissa, University of Thessaly, Volos, Italy
Introduction: Branched Thoracic Endovascular Repair of the Aorta (bTEVAR) is a feasible alternative to conventional open surgical debranching techniques, allowing for complete endovascular repair of thoracic aortic pathologies involving the aortic arch, such as Non-A, Non-B dissections.
Case Report/Technique: We present the case of a 64-year-old male patient who was transferred to our department with an acute Non-A, Non-B aortic dissection, extending from the LSA to the aortic bifurcation. Following initial conservative management, the patient was treated with a custom-made branched endograft [Bolton Medical, Inc. (Terumo Aortic, Sunrise, FL, USA)], incorporating three directional branches for the innominate, left carotid and left subclavian artery, respectively. Postoperative 6-month follow-up shows partial false lumen thrombosis with complete branch patency.
Conclusions: Branched TEVAR is a feasible, total endovascular solution to certain aortic pathologies, such as Non-A, Non-B dissections, where conventional TEVAR is contraindicated.
1.39.15. Simultaneous Ascending Aortic Replacement and Thoracic Endovascular Aortic Repair (TEVAR) in Acute Aortic Syndrome
- 1
Department of Cardiovascular Surgery, Atatürk University Medical Faculty, Erzurum, Turkiye
- 2
Department of Cardiovascular Surgery, Buhara Hospital, Erzurum, Turkiye
Backround: The term acute aortic syndrome (AAS) refers to a group of situations in which there is a danger of impending aortic rupture and treatment delays result in increased mortality. We aim to present the use of an endovascular and surgical hybrid approach to treat acute aortic syndrome. The method is a single-step procedure used to treat severe aortic disease withouth using hybrid operating room.
Case Presentation: Five hours after beginning of acute and severe chest and back pain, a 62-year-old woman was referred to our department from cardiology. The patient was hemodynamically stable, hypertensive and had a history of Takayasu arteritis. Ascenden aort aneurysm, intramural hematoma (IMH) and a Stanford type B aortic dissection were found in computed tomography (CT). The patient was immediately operated on, under general anesthesia, and extracorporeal circulation was initiated with femoral cannulation. Then the patient underwent TCA. The ascending aortic aneurysmatic segment was removed. The TEVAR procedure was completed with direct view and the ruptured thoracic aortic segment was treated by opening the Medtronic captiva 30 × 30 × 200 mm stent graft over the hard wire as zero to the origin of the left subclavian artery. Then Ascending aortic replacement was completed. The patient’s post-procedure recovery was clinically uneventful. The patient was discharged on the seventh day after the operation. We demonstrate the efficacy and anatomical feasibility of combining open surgery with an endovascular method to treat ascenden aort aneurysm and aortic dissection of the thoracic aorta simultaneously. Endovascular intervention performed during open surgery makes the operation easier due to direct vision. Considering the complications and difficulties of thoraco-abdominal surgery, this hybrid approach appears to significantly reduce surgical morbidity and mortality.
1.39.16. Endovascular Treatment of Descending Thoracic Aortic Aneurysm with Severe Tortuosity Causing Tracheal and Esophageal Compression
- 1
Department of Cardiovascular Surgery, Etlik City Hospital, Ankara, Türkiye
- 2
Department of Cardiovascular Surgery, Sincan Training and Research Hospital, Ankara, Türkiye
The incidence of thoracic aortic aneurysms (TAA) increases with increasing age. Large aneurysms may be asymptomatic. The symptoms occur due to pressure on surrounding tissues and organs. Dyspnea and dysphagia occur rarely due to TAA compression. Rupture of the aneurysm is usually fatal. Thoracal endovascular aortic repair (TEVAR) can be safely performed in appropriate cases. The safety of endovascular repair will be maximized with the development of new devices and techniques. We present a case of a 75-years-old man treated with TEVAR. He had moderate dyspnea and dysphagia caused by descending thoracic aortic aneurysm with severe tortuosity. When there is severe tortuosity of the aorta, implantation of the device is difficult and requires different manipulations. Establishment of a brachio-femoral through and through a guidewire is an auxiliary manipulation in the presence of severe tortuosity. We wanted to emphasize in this article; TEVAR is safer than open surgery, it can also be applied with some special manipulations in severe tortuosity of the aorta. The spinal cord protection is essential to avoid neurological complications.
1.39.17. Hybrid Endovascular and Surgical Aortic Reconstruction for a Complicated Type 3 Aortic Dissection with an Atypical Anatomy: Challenging Case
- 1
Department of Cardiovascular Surgery, School of Medicine, Biruni University, Istanbul, Turkey
- 2
School of Medicine, Istanbul Medipol University, Istanbul, Turkey
BACKGROUND: Type 3 Aortic dissection, though rare, may require immediate intervention in case of vital organ ischemia, uncontrollable severe pain and hypertension or aortic rupture. Without prompt treatment, mortality rates can reach 50% within the first 48 h. Management of aortic dissection is challenging, and its treatment is still in the process of development and innovation. Recent advancements in surgical techniques have been greatly enhanced by innovative endovascular approaches, prompting the development of hybrid surgical procedures.
CASE: This case highlights a hybrid treatment approach to a 52-year-old male patient who experienced sudden onset chest pain and shortness of breath, and collapse leading to ventilatory support diagnosed with type 3 aortic dissection and contained rupture with an atypical anatomical orientation of the vasculature. Initial attempts at endovascular stenting were complicated by a type 1 endo-leak, necessitating surgical intervention with endograft stabilization, aortic debranching, and reconstruction. Further complications prompted bilateral carotid-subclavian bypass with embolization of the native subclavian arteries and the treatment of a descending aortic aneurysmal sac with elongation of the thoracic endovascular stent graft.
1.39.18. Aortic Coarctation Surgery in Adults
Valeriy Sergeevich Arakelyan, Rustam Zabyt Gerievich Kidakoev, Vasiliy Georgievich Papitashvili, Roman Gennadevich Bukatsello and Magomedrasul Kurbanmagomedovich Musaev
Department of Arterial Pathology, Bakoulev Scientific Center for Cardiovascular Surgery, Moscow, Russia
BACKGROUND AND AIM: Study the influence of age characteristics on the type of surgical treatment in patients over 40 years of age.
METHOD: The results of surgical treatment of coarctation of aorta in 32 patients over 40 years old were studied. The median age was 46.6 years (CI 43.20–52.85). The average gradient of systolic pressure on the isthmus of the aorta was 53.39 ± 21.20 mmHg, and the gradient between the upper and lower extremities was 47.97 ± 26.91. The incidence of prestenotic and poststenotic aortic saccular aneurysms was 50% (n = 16), aortic arch kinking—15.6% (n = 5). The mean diameter of ascending aorta was 37 ± 8 mm (range, 24–52 mm). In 68.8% (n = 22) surgical resection of coarctation with graft replacement was performed, and in 31.2% (n = 10) patients, end-to-end anastomosis was applied. Partial cardiopulmonary bypass was used in patients with association of aortic coarctation and saccular aneurysm of aortic arch or isthmus.
RESULTS: In patients over 40 years of age aortic graft replacement and cardiopulmonary bypass technique was used 3 times more often than end-to-end anastomosis (OR 3.7, 95% CI: 2702–5240 and OR 3.6, 95% CI: 2081–6274, respectively). The incidence of pre and poststenotic aortic aneurisms an adult was significantly more often, as well as dilatation or the ascending aorta and aortic kinking (OR 3.5, 2.4, 3.8, respectively). The complication rate was 4.6%. All patients achieved favorable results and were discharged in a satisfactory condition.
CONCLUSIONS: Adult patients with aortic coarctation have high incidence of artic wall disorders—prestenotic and poststenotic aortic saccular aneurysms, aortic arch kinking and dilation of ascending aorta and the main surgical option is aortic graft replacement.
1.40. VASCULAR AND ENDOVASCULAR » Venous
1.40.1. Mid to Long Term Results of Pharmacomechanical Thrombectomy Versus Medical Therapy for Deep Venous Thrombosis (DVT) in Cancer and Non-Cancer Patients
- 1
Department of Cardiovascular Surgery, State Hospital, Şırnak, Turkey
- 2
Department of Cardiovascular Surgery, Beyhekim Training and Research Hospital, Konya, Turkey
- 3
Department of Cardiovascular Surgery, Meram Medical Faculty, Necmettin Erbakan University, Konya, Turkey
BACKGROUND AND AIM: Deep vein thrombosis (DVT) is one of the most common causes of death due to cardiovascular disease. Although monotherapy with LMWHs has been accepted for cancer-associated thrombosis, Novel Oral Anticoagulants (NOAC) and endovascular interventions have been included in guidelines for this special population. The aim of this study was to compare mid-and-long term outcomes of patients with selected cancer-associated DVT and non-cancer patients who underwent pharmacomechanical thrombectomy with medical therapies.
METHOD: A total of 126 patients treated with medical (n: 66) and pharmacomechanical thrombectomy (n: 60) for DVT were included in the study. In this cohort receiving medical therapy alone, 15.15% (n: 10) were patients with DVT associated with cancer. Among patients who underwent endovascular intervention, 21.67% (n: 13) had cancer. Villalta scale was used to measure the severity of postthrombotic syndrome (PTS). Recanalised flow and valve damage-reflux were monitored by USG.
RESULTS: There were no statistically differences between the groups in terms of demographic characteristic. It was found that the comparisons obtained from independent and ANCOVA tests were compatible and not affected by the age and gender variables. All patients with moderate or severe venous insufficiency (n: 24) on 1 styear USG results were associated with moderate and severe PTS (n: 7 moderate, n: 17 severe PTS). Cancer-associated DVT patients (n: 13) who underwent pharmacomechanical thrombectomy showed superior results in 1styear Villalta scores compared to cancer patients (n: 10) who received NOAC treatment (Villalta: 8 vs. 12). This rate was similar to that seen in the normal population without cancer who underwent pharmacomechanical thrombectomy. (Villalta; 8 vs. 8).
CONCLUSIONS: It is possible to improve the quality of life of DVT patients by preventing long-term complication. The risk of DVT’s complications is reduced by the correct use of NOACs and pharmacomechanical thrombectomy. USG and PTS clinical scales should be used for all patients (with/without cancer-associated DVT). Treatment planning should be reviewed in patients with damage to vein structural elements and in patients in whom the desired recanalisation is not achieved. The development of endovascular treatments for DVT can improve the declining quality of life of special populations, such as cancer patients.
1.40.2. Utilisation of Resuscitative Endovascular Balloon Occlusion of the Vena Cava (REBOVC), and Its Application to Retroperitoneal Trauma: A Systematic Review
Luca Borruso 1, Krishna Kotecha 2, Vikram Puttaswamy 2, Shen Wong 2, Anubhav Mittal 2 and Jaswinder Samra 2
- 1
Royal Prince Alfred Hospital, Sydney, Australia
- 2
Royal North Shore Hospital, Sydney, Australia
BACKGROUND AND AIM: Retroperitoneal trauma is associated with high morbidity and mortality, particularly if the vena cava (VC) is involved. Resuscitative endovascular balloon occlusion of the VC (REBOVC) can limit life-threatening bleeding however there is a paucity of published data. The aim of this systematic review was to summarise the literature on REBOVC, describe common techniques and assess its safety/utility in retroperitoneal trauma.
METHOD: A systematic review of the literature was undertaken according to PRISMA guidelines. Eligible studies were animal models of REBOVC, and any studies involving humans undergoing REBOVC. Reference lists of included studies were searched to identify other potentially relevant studies.
RESULTS: 10 studies were eligible for inclusion. Five described REBOVC in humans (three case reports and two case series), totalling 12 patients. Injuries were mostly penetrating (gun-shot wounds [n = 7], stabbing [n = 3]) followed by blunt trauma (n = 2). Method of venous access was either direct (via a VC defect) or percutaneous. Older studies described the use of foley catheters for occlusion and newer studies described hybrid techniques utilising specialised occlusive balloons. Almost all (n = 11/12) patients survived their injury and were discharged from hospital. Five experimental animal studies used porcine models of VC trauma, demonstrating improved outcomes in those animals treated with REBOVC; with prolonged time to death and reduced blood loss.
CONCLUSIONS: REBOVC appears to be effective in pre-clinical animal studies at controlling haemorrhage and prolonging life. While the evidence base is small for use in humans, we posit REBOVC can be used in appropriately selected patients with good outcomes.
1.40.3. Pulmonary Endarterectomy for Systemic and Suprasystemic Chronic Thromboembolic Pulmonary Hypertension
- 1
Lviv Centre for Cardiac Surgery, Lviv National Medical University, Lviv, Ukraine
- 2
Lviv Regional Hospital, Lviv, Ukraine
BACKGROUND AND AIM: Pulmonary endarterectomy (PEA) is the treatment of choice in chronic thromboembolic pulmonary hypertension (CTEPH). The risk of PEA gets bigger with the rise of pulmonary artery pressure (PAP) and pulmonary vascular resistance (PVR). Controversy exists in understanding of the influence of high and very high PAP on the outcome of PEA. We focused on the early results after PEA in patients with extreme systolic PAP compared to patients with lower PAP.
METHOD: From 2013 to 2023, 89 patients with CTEPH underwent pulmonary thromboendarterectomy according to San Diego protocol with a period of circulatory arrest ranging from 9 to 90 min. PAP and PVR were assessed before and after PEA using measurements with a Swan-Ganz catheter. Systolic pulmonary hypertension and PVR ranged from 75 to 140 mm Hg and 320 to 2550 dynes-s-cm−5, respectively. In 11 patients systolic PAP was equal to the systemic arterial pressure and in 4 exceeded the latter. Patients were divided according to San Diego intraoperative classification of CTEPH based on the intraoperative surgical specimens.
RESULTS: Overall perioperative mortality was 5.6% (5/89 patients). Hospital mortality in patents with preoperative systemic and suprasystemic systolic PAP compared with lower PAP was 20% and 2.2%, respectively. In 4 patients with suprasystemic systolic PAP and PVR ranging from 1550 to 2550 dynes-s-cm−5, a central veno-arterial ECMO was used. All four patients belonged to level 1 and level 2 disease according to San Diego classification; two of them died despite the radical endarterectomy.
CONCLUSIONS: Severe preoperative systolic pulmonary artery pressure is not a contraindication for PEA but remains the main risk factor for operation.
1.40.4. The Effectiveness of Vacuum-Assisted Closure Therapy in Patients with Infected Venous Leg Ulcers
Esra Ertürk Tekin 1, Mehmet Ali Yeşiltaş 2, Ayhan Uysal 3, Ahmet Ozan Koyuncu 4, Necmi Köse 1, Bahar Aydınlı 5 and Vehbi Kınay 1
- 1
Department of Cardiovascular Surgery, Mersin City Training and Research Hospital, Mersin, Turkey
- 2
Department of Cardiovascular Surgery, Prof. Dr. Cemil Tascioglu City Hospital, Istanbul, Turkey
- 3
Department Cardiovascular Surgery, Firat University, Elazıg, Turkey
- 4
Department of Cardiovascular Surgery, Istanbul University-Cerrahpasa, Institute of Cardiology, Istanbul, Turkey
- 5
Department of Anesthesiology and Reanimation, Mersin City Training and Research Hospital, Mersin, Turkey
BACKGROUND AND AIM: In this study, we aimed to investigate the effect of vacuum-assisted closure therapy on venous stasis wound healing in patients with chronic venous leg ulcers.
METHOD: Vacuum-assisted closure therapy was applied on a total of 14 venous leg ulcers. All patients had post-thrombotic syndrome. Quantitative wound culture samples were obtained before the procedure and local wound assessments were performed. The primary outcome measures included wound healing as assessed by a local wound examination during each dressing change and the rate and velocity of ulcer reduction. Wound healing was defined as the complete closure of the ulcer, while rapid wound healing was defined as a ≥30% reduction in the ulcer size by week four.
RESULTS: No surgical debridement or surgical corrective procedure was applied in any patient. The mean length of hospital stay was 32.3 days. The mean number of vacuum- assisted closure therapies for each case was 17.8 and the mean time to dressing change was 72.3 h. Multidrug-resistant Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus were detected in three and four patients, respectively. Wound culture results became negative after a mean duration of vacuum-assisted closure therapy of 12.1 days. None of the patients needed antibiotic therapy until the procedure was completed. Compared to baseline, the mean ulcer reduction rates were 46.4% for the first six applications and 72.8% for the subsequent applications.
CONCLUSIONS: Our study results suggest that vacuum-assisted closure therapy promotes rapid wound healing in patients with severe post-thrombotic syndrome with venous stasis leg ulcers, and reduces the need for antibiotics by reducing the biological burden.
1.40.5. Evolution of Endovenous Laser Ablation (EVLA) for Treatment of Varicose Veins: A Comparison of EVLA with 1470 nm and 1940 nm Lasers in Terms of Safety, Feasibility, and Early Efficacy
BACKGROUND AND AIM: Our aim was to evaluate and compare the safety, efficacy, and early outcomes of EVLA by means of 1940 nm laser with radial fiber and EVLA by Diode 1470 nm laser for the treatment of truncal vein insufficiency
METHOD: 50 patients (112 incompetent saphenous veins) were treated with 1940-nm EVLA (Corona Infinite Ring, neoLaser, Caesarea, Israel) and 70 patients (145 incompetent saphenous veins) with 1470-nm EVLA (ELVeSTM Radial, Biolitec AG, Germany). Simultaneous miniphlebectomy and ligation of perforators were applied. The vein diameter, energy delivered, and linear endovenous density (LEED) were evaluated. The endpoints were: Closure of the target vessel, complications and postoperative quality of life (QoL). QoL was measured by using CIVIQ-20 pre- and postoperatively. Pain and clinical severity were evaluated by visual analog scale (VAS) and venous clinical severity score (VCSS) 10-day and one month after EVLA.
RESULTS: The success rate of the procedure was 100% in both groups. LEED values were statistically lower in 1940-nm EVLA group for ablation of right GSV (61.93 ± 9.82 vs. 35.7 ± 7.19; p < 0.05) and left GSV (62.65 ± 8.42 vs. 34.85 ± 9.85; p < 0.05). Average 24-h and 1-month VAS scores were similar, but at 10th day control VAS scores were higher in 1470-nm EVLA group (2.7 ± 1.26 vs. 1.9 ± 1.21; p < 0.05). The postoperative VAS, VCSS and CIVIQ-20 scores in the two groups were significantly decreased compared with the scores before the procedure, and although no significant differences were noted between the two types of laser at postoperative 1st month, the scores of 1470-nm group tended to be higher (35.2 ± 7.8 vs. 33.1 ± 10.22; p = 0.13).
CONCLUSIONS: EVLA with 1940 nm laser is as safe and effective as 1470 nm laser for the treatment of truncal vein insufficiency. Using a 1940-nm laser seems to be more advantages on improving QoL in terms of postoperative pain and discomfort
1.40.6. Axillar Artery Aneurysm: Case Report
Mert Çelik, Mucteba Sarıcaoglu and Cengiz Ovalı
Departments of Cardiovascular Surgery, Osmangazi University, Eskisehir, Turkey
The incidence of upper extremity peripheral artery aneurysms is much lower than lower extremity peripheral artery aneurysms.
Traumatic aneurysms can be divided into two groups: false and true. False aneurysms may develop after a penetrating injury to the vessel wall. Bleeding from a penetrating injury is limited by surrounding soft tissues, and a hematoma forms. The organization continues with the lumen of the pseudoaneurysm sac, leading to fibrosis and eventual recanalization.
Axillary artery aneurysms secondary to blunt trauma are rare and are usually diagnosed late. The reason for the late diagnosis is that the symptoms of aneurysm in the muscle and bone structures surrounding the chest and shoulder regions are overlooked due to the location of the axillary artery. In addition, distal peripheral pulses may be strong due to extensive upper extremity collateral circulation.
1.40.7. Open Heart Surgery Following Vascular Complication in a Patient with Permanent Tunneled Hemodialysis Catheter: A Case Presentation
Mert Çelik, Tarık Tastekin and Cengiz Ovalı
Departments of Cardiovascular Surgery, Osmangazi University, Eskisehir, Turkey
Venous catheterization is the preferred method for hemodialysis in patients with acute hemodialysis needs who are not suitable for arteriovenous fistula creation due to peripheral vascular pathologies. The need for urgent intervention for vascular complications that may occur during the hemodialysis catheter insertion procedure should always be considered. This article describes the urgent vascular surgical repair of injuries to the brachiocephalic vein and superior vena cava that occurred during the procedure in a patient with an HD catheter.
1.40.8. Prophylaxis and Treatment of Chronic Venous Insufficiency of the Lower Extremities in Pregnants, Evaluation of the Results of Classic Phlebectomy and Evla Surgery Due to Varicoses
Nubar Ismayilova, Nazim Gasimov and Vugar Fattah Pur
Azerbaijan State Advanced Training Institute for Doctors Named by A. Aliyev, Baku, Azerbaijan
CVI in the lower extremities is one of the most common diseases in the population. In patients with severe CVI, upper stripping of the large subcutaneous vein, removal of varicose veins, and closure of perforating veins are performed through surgical intervention. Although several studies have shown that EVLA is more effective, there are still debatable conflicting opinions on the comparison of open or minimally invasive intervention in terms of recurrences in the immediate and distant periods after surgery.
OBJECTIVE: To improve the long-term results of the operation through the prevention of recurrences and chronic venous insufficiency during pregnancy in women who have undergone classical venectomy and EVLA.
MATERIAL-METHOD: During the doppler examination after EVLA, 13 out of 31 women did not have pathological reflux in the venous system around the right and 14 women in the left lower extremity, 2 women had reflux in the basin of the small and large subcutaneous veins, which was manifested by the clinical picture in the C1 and C2 stages. In 1 of these women, pelvic veins were involved in the process, and in 1, neovasculogenesis was observed.
As a conclusion of the discussion of the complications after open surgical operation, we witnessed the recurrence in 12 people on the right side and in 16 people on the left side. 9 out of 12 relapses on the right side and 11 out of 16 relapses on the left side were related to stasis and reflux in pelvic veins. In women who underwent open venectomy, 20 had recurrence at the C2-C3 stage after childbirth, 17 had reflux in perforating veins, and 5 had neovasculogenesis.
RESULTS: After EVLA surgery, the occurrence of variceal recurrence in pregnant and postpartum women was statistically significantly lower compared to traditional open surgery, and EVLA proved to be a more effective treatment.
1.40.9. Our Experience in Managing Phlebitis Following Cyanoacrylate Glue Closure with VenaBlock: A Case Report
- 1
Faculty of Medicine, Airlangga University, Surabaya, Indonesia
- 2
Cardiothoracic and Vascular Surgery Department of PHC General Hospital, Surabaya, Indonesia
BACKGROUND: Chronic venous insufficiency (CVI) is a condition characterized by impaired venous return in the lower extremities, leading to symptoms such as leg pain, swelling, and skin changes. The Venablock© Venous Closure System (Invamed, Ankara, Turkey) is an innovative embolization device utilizing cyanoacrylate, designed to non-thermally and non-tumescently block refluxing truncal veins associated with chronic venous insufficiency and varicose veins. Cyanoacrylate glue closure (CAC) with VenaBlock is a widely used technique for the treatment of venous insufficiency, known for its efficacy and safety profile. However, despite its advantages, complications such as phlebitis can occur, albeit uncommonly. We present a case of a patient who developed symptomatic phlebitis following CAC with VenaBlock, highlighting our institution’s experience in diagnosis and surgical management of this complication.
Case Presentation: A 60-year-old female with a history of chronic venous insufficiency underwent cyanoacrylate glue closure (CAC) with VenaBlock for symptomatic varicose veins in the right leg. One week following the procedure, the patient experienced persistent pain, itchiness, redness, and swelling in the treated leg. Diagnostic workup confirmed the presence of phlebitis, and initial pharmacotherapy with nonsteroidal anti-inflammatory drugs (NSAIDs) and anticoagulants was ineffective, necessitating surgical excision of the affected vein. Postoperatively, the patient experienced resolution of symptoms. Phlebitis following CAC with VenaBlock, though uncommon, can present significant challenges in management. This case highlights the importance of prompt recognition and appropriate treatment of this complication, including consideration of surgical intervention in some cases.