Abstract
Some pharmaceutical excipients are able to modify intestinal permeability, thus influencing drug absorption and bioavailability. The effect of four polyols (mannitol, maltitol, sorbitol and xylitol) on the permeability of seven active pharmaceutical ingredients (API), representing different BCS classes (furosemide, amiloride, atenolol, ranitidine, nadolol, L-thyroxine and acyclovir), was investigated using the Caco-2 cell permeability model. Analytical methods for the sensitive polyol and API quantification were developed using Ultra High Performance Liquid Chromatography coupled to triple-quadrupole Mass Spectrometry (UHPLC-QqQ). Apparent permeability coefficients (Papp) were calculated from the measured concentrations in the apical and basolateral compartments. The cell monolayer remained intact throughout the experiment in all trials, neither significant Lucifer Yellow (LY) passage, nor modification of the electrical resistance was detected, demonstrating that no active principle or excipient (or combinations thereof) modulated the paracellular transport. The Papp values for apical to basolateral and basolateral to apical directions of drug + excipient combinations were compared with the Papp values for the drug substance alone. Our results show that mannitol, maltitol, sorbitol and xylitol did not modify the permeability of furosemide, amiloride, atenolol, ranitidine, nadolol, acyclovir and L-thyroxine APIs. Moreover, the presence of polyols did not alter the efflux of the active principle (basolateral to apical).
Keywords:
polyols; xylitol; sorbitol; maltitol; mannitol; BCS; Caco-2; permeation; intestinal; excipient; active; furosemide; amiloride; thyroxine; atenolol; ranitidine; nadolol; acyclovir; UHPLC; triple quad; Papp; apparent permeability coefficient 1. Introduction
The use of pharmaceutical excipients is mandatory for producing effective pharmaceutical preparations with active pharmaceutical ingredients (API). Excipients are appropriately evaluated for their safety and inclusion in drug formulation, selected for their chemical inertness and expected galenical function. In the past, they were considered as inactive substances used, e.g., as diluents, binders, lubricants, sweeteners or coatings, However, scientific data from recent years show that some excipients are capable of influencing drug absorption and bioavailability through the modification of its solubility or changes in intestinal permeability and the modulation of the gastrointestinal motility [1,2]. Among these excipients, polyols are frequently used in tablets and capsules. They are selected for its good tableting properties and serve as soluble filler-binder in many tablets [3,4,5]. Orodispersible and effervescent formulations rely on specific galenic properties of polyols. Due to its sweetness and its selected texture, polyols are the preferred choice in OTC formulations. Polyols such as mannitol [5,6] exhibit many strong advantages such as a low hygroscopicity, a strong inertness with both the API and the patient’s body and the ability to produce extremely robust tablets. Nevertheless, according to a certain paper, Sorbitol, another widely used sugar alcohol in the formulations of various drugs, may alter oral absorption and bioavailability of certain drugs, especially when sustained release formulation was used in place of immediate release formulation and for certain API [7].
The Biopharmaceutics Classification System (BCS), based on aqueous solubility and intestinal permeability, is an approach used to predict drug absorption during pharmaceutical development to justify a waiver for in vivo bioequivalence [8]. Thereby, it is essential to know the role of an excipient in the formulation and consider the drug bioavailability, particularly for class III drugs exhibiting high solubility and low permeability.
The data from the literature have demonstrated that some excipients (many sugar alcohols, polyethylene glycol (PEG), sodium acid pyrophosphate) could influence the absorption of poorly permeable drugs via their osmotic pressure in the small intestine [2,8,9,10,11]. Another potential matter for extending BCS biowaivers to low-permeability drugs is the potential of some excipients to modulate the intestinal drug permeability. In vivo and in vitro human data indicate that microcrystalline cellulose, hydroxypropyl methylcellulose, sodium lauryl sulfate, corn starch, sodium starch glycolate, colloidal silicon dioxide, dibasic calcium phosphate, crospovidone, lactose, povidone, stearic acid, pregelatinized starch, croscarmellose sodium and magnesium stearate do not modify the absorption of BCS class III drugs (high solubility/low permeability) cimetidine and acyclovir in humans [12]. Nevertheless, some excipients such as polysorbate 80 and docusate modulate the Caco-2 permeability of low permeable drugs, such as furosemide, cimetidine and hydrochlorothiazide, by inhibiting their active efflux and increasing the apical to basolateral direction permeability [13]. Caco-2 cells are derived from the human colon adenocarcinoma cell line and have been identified as a good in vitro experimental model for the study of drug absorption mechanism [14]. According to the literature, in vitro cell experiments can more accurately reflect the effect of excipient on drug absorption than integral animal experiments [15]. According to different authors, CaCo-2 cells are cultured on a porous permeable polycarbonate membrane, and they can grow, fuse, differentiate, and form a continuous monolayer. Moreover, their morphology and function are similar to human small intestinal epithelial cells, and marker enzyme expression, uptake, transport, and permeability characteristics are all similar to the small intestinal epithelial cells and can be a robust model for the absorption process of the small intestinal epithelial cells [16,17]. The main efflux transport proteins, P-glycoprotein (P-GP), Multidrug resistance-associated proteins (MRP), and Breast cancer resistance protein (BCRP) are highly expressed on Caco-2 [18].
Due to contradictory results regarding the excipients’ effect on intestinal drug absorption, it is important to study the possible effect of polyols on drug bioavailability. This work investigates the absorption of four polyols—mannitol, maltitol, sorbitol and xylitol—and their influence on drug permeability. Seven active substances were tested based on their low permeability and varying physicochemical properties: furosemide (BCS class 4: low solubility/low permeability) and drugs of the critical BCS class 3: amiloride, atenolol, ranitidine, nadolol, L-thyroxine and acyclovir. Permeability assays were performed with Caco-2 cells (human intestinal epithelial cells derived from a colorectal adenocarcinoma).
2. Materials and Methods
All tested polyol samples were of pharmaceutical excipient quality. PEARLITOL® 200 SD mannitol, SweetPearl® P90 maltitol, NEOSORB® P 200 SD sorbitol and XYLISORB® 90 xylitol were supplied by Roquette Frères, Lestrem, France. Active substances were obtained from Sigma Aldrich, St. Quentin Fallavier, France. The study was performed in three steps: cytotoxicity evaluation of the tested compounds, development of analytical methods and permeability studies on Caco-2 cells.
2.1. Cytotoxicity Determination
The first step was to determine possible cytotoxic effects and the optimal nontoxic test concentrations for seven active substances and four excipients (and combinations thereof) on Caco-2 cells to avoid cellular membrane damage and leakages in cell monolayer. Each of the excipients, drug substances and combinations were co-incubated with the cells for one hour at 37 °C in the presence of 5% CO2. Caco-2 cells were seeded in 384w plate format two days prior to the experiment at eight different concentrations: 500–1000–2000–3000–4000–6000–8000 and 10,000 cell/well using HBSS incubation buffer. The cytotoxicity was evaluated by ATP luminescence technology using CellTiter-Glo Luminescent Cell Viability Assay Kit (Promega, Charbonnières-les-Bains, France). The detection period was 30 min at room temperature. For control, a test in the absence of cells was also performed to trace an eventual interference with the luminescence detection method.
2.2. Analytical Methods
Analytical methods were developed for a highly sensitive quantification of the polyols and the active substances by using Ultra High Performance Liquid Chromatography coupled to triple-quadrupole Mass Spectrometry (UHPLC-QqQ). The quantification of each active substance and polyol was performed by a 1290 Infinity Binary LC system (Agilent Technologies, Waldbronn, Germany) coupled with a Q-TRAP® 5500 mass spectrometer with an ESI Turbo V ion source (SCIEX, Foster City, CA, USA). Liquid chromatography parameters were defined to separate active substances, excipients and components of Caco-2 assay buffer A and B (salts and hepes/mes). Two column chemistries were used: Poroshell 120, EC-C18 (Agilent, Les Ulis, France), BEH Hilic (Waters, Saint-Quentin-en-Yvelines, France). The polyols and the active substances were quantified using chromatographic column with the Hilic and C18 chemistry, respectively. All used parameters for the chromatographic separations in the subsequent phases are given in Table 1 and Table 2.

Table 1.
Elution gradient used for C18 column for active substances quantification.

Table 2.
Elution gradient used for BEH Hilic column for polyols quantification.
For each substance, the linearity range, correlation coefficient r2 and accuracy were determined. The limit of detection (LoD) was defined as the lowest concentration for a measured peak intensity three-fold superior to the baseline (three-fold the signal noise ratio).
2.3. Permeability Assay on Caco-2 Cells
All excipients, active substances and their combinations were tested at doses without detected cytotoxicity, solubilized in dimethyl sulphoxide (DMSO).
Permeability assays were performed with Caco-2 cells as previously described [19], using commercially ready-to-use plates (ReadyCell™, Barcelona, Spain) and by testing in either apical to basolateral (A–B direction) or basolateral to apical (B–A direction).
The test samples were dissolved in buffer A for apical compartment (HBSS + 5 mM MES pH 6.5) and in buffer B for basal compartment (HBSS + 10 mM Hepes pH 7.4) with a final concentration of DMSO of 1% (v/v).
The incubation times for the permeability trials were the following: A–B: 60 min 37 °C (5% CO2); B–A: 40 min 37 °C (5% CO2). Colchicine (PgP-transporter control) and ranitidine (very low permeability), labetalol (medium permeability) and propranolol (high permeability) were tested as four standard controls at a concentration of 10 μM. A standard curve for Lucifer Yellow (LY) using eight different concentrations (0/10/20/50/100/250/500/1,000 μM) was established. A total of 100 µM LY was added as internal standard in each experimental well. Moreover, transepithelial/endothelial electrical resistance (TEER) was measured to confirm the integrity and permeability of the monolayer, before and after the transfer [20].
Apparent permeability coefficients (Papp) were calculated as previously described [21] using analytically measured concentrations in the A and B compartments for combinations of actives and polyols and compared to active alone for apical to basolateral and basolateral to apical directions. The recovery of each compound was calculated between A and B compartments. The apparent permeability coefficient (Papp) of the test compound and its recovery are calculated as follows:
where Papp is the apparent permeability coefficient (cm s−1), dQ/dt the amount of drug permeated per unit of time, A the effective surface area of the cell membrane exposed to the medium and C0 the initial drug concentration in the donor compartment.
Papp = dQ/dt × 1/AC0
3. Results
Concerning cytotoxicity assays, no interference was detected for all the tested substances in the presence of 1 µM ATP (without cells). No cytotoxicity was found with any of the four polyols and seven active substances, alone or in combination, at doses up to 10 µM.
LC-MS methods were optimized for the detection of four excipients and seven active substances in medium A and B for the permeability assay (Table 3).

Table 3.
Range of linearity and limit of detection of detectable compounds in assay buffer A or B.
The obtained data show that the analytical methods are suitable for detection and quantification of all tested compounds in medium A and B for the permeability assay, with good linearity (r2 > 0.98), accuracy (from 80% to 120%) and selectivity (data not shown). During all tests, no significant LY passage was detected with no modification of the electrical resistance TEER, demonstrating that the cell monolayer remained intact throughout the experiments. Neither the active principles nor the excipients or their combinations modulated the paracellular transport.
Based on Caco-2 permeability assays (Table 4, Table 5 and Table 6), maltitol and sorbitol showed a very low passage from apical to basolateral compartments of the Caco-2 model whereas mannitol and xylitol had a medium permeability across the Caco-2 model. From basolateral to apical region, maltitol did not cross the barrier whereas mannitol, sorbitol and xylitol had a very low passage (Table 4).

Table 4.
Mean Papp (+/− standard deviation) of four polyols alone, basolateral to apical and apical to basolateral Caco-2 permeability assay.

Table 5.
Mean Papp (+/− standard deviation) of seven active substances in apical to basolateral Caco-2 permeability assay, either alone or in the presence of an excipient (ND: not determined).

Table 6.
Mean Papp (+/− standard deviation) of seven active substances basolateral to apical Caco-2 permeability assay, either alone or in the presence of an excipient (ND: not determined).
The active substances furosemide, amiloride, atenolol, ranitidine, nadolol, acyclovir and L-thyroxine did not cross from the apical to the basolateral region or from the basolateral to apical region when combined with any polyol. No modification of the permeability of the tested active substances in either direction was observed under the test conditions (Table 5 and Table 6).
4. Discussion
The results show that polyols have a very low to medium intestinal permeability in the Caco-2 model. This observation is in accordance with several results obtained on the human intestine, which indicated the slow and incomplete absorption of polyols. These compounds are slowly and incompletely absorbed in the small intestine via passive diffusion without additional energy input. The process and amount of absorption varies depending on the individual polyol [22].
According to Lenhart and Chey [22], polyols are absorbed via passive diffusion without any energy requirement. The molecular size of polyols influences its absorption rate. When comparing different monosaccharide polyols, such as sorbitol and erythritol, the larger size of sorbitol may be approaching the upper limit for diffusion across the small intestinal epithelium, resulting hence in poorer absorption. The lower molecular size of erythritol may explain its more complete absorption in comparison to other polyols. In our study, we find the same phenomenon: the results for Papp values obtained for passages from apical to basolateral compartments of the Caco-2 model decrease with the increasing molecule size as follows: xylitol > mannitol > sorbitol > maltitol. Moreover, the Papp value obtained for mannitol corresponds with those found in the literature: 1.9 × 10−6 cms−1 [23]; 2.6 × 10−6 cms−1 [13], 2.63 × 10−6 cms−1 [24] and it is approximately ten times higher than the value recovered with 11C-mannitol [25]. According to Lenhart and Chey [22], monosaccharides may be absorbed via the transcellular route, whereas larger disaccharide molecules may be absorbed in a lesser extent paracellularly. Intestinal glucose absorption is predominantly facilitated by sodium-dependent glucose transporter 1 (SGLT1), whereas glucose efflux from enterocytes into the blood is mediated by glucose transporter 2 (GLUT2) [26]. In another way, the absorption mechanism could differ, comparing the polysaccharides structures. Cyclic oligosaccharide such as cyclodextrins, often used as excipients for the solubility and permeability enhancement of poorly soluble active pharmaceutical ingredients, are absorbed on Caco-2 cells via cellular internalization and endocytosis, with some differences between the internalization probably due to hydrophilicity or lipophilicity of the different cyclodextrins derivatives [27]. According to Artursson and Borchardt (1997) [28], mannitol is hydrophilic, not metabolized by Caco-2 cells and absorbed through a paracellular pathway, through the tight junctions. Moreover, this molecule is not distributed in the membrane cells. The monosaccharide polyols with lower molecular size (Figure 1) could be absorbed via the transcellular route (xylitol, molecular weight: 152 g/mol; sorbitol and mannitol, molecular weight: 182 g/mol), while the disaccharide-polyol (maltitol, molecular weight: 344 g/mol), with the largest molecular size, could be absorbed via paracellular mechanism. These findings correlate with the reported molar volumes [29] with 90.70 mL/mol for erythritol, 110.68 mL/mol for xylitol and 130.62 mL/mol for both sorbitol and mannitol and may, therefore, explain the differences of the observed Papp’s.
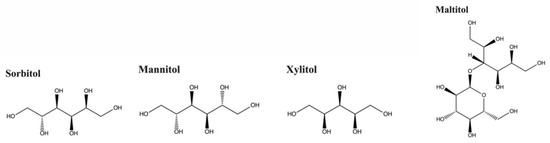
Figure 1.
Chemical structures of polyols.
Concerning the effects on the active substances, the results show that intestinal permeability of the seven selected drug substances is not modulated by the presence of polyols under the used experimental conditions and concentrations (Table 4 and Table 5).
Previously, the permeability of four BCS class III compounds (including acyclovir, atenolol and nadolol) was studied with two different models: Caco-2 cell monolayers and in situ rat intestinal perfusion in the presence of five excipients (lactose, povidone, hydroxypropyl methylcellulose, sodium lauryl sulfate and PEG 400). No increase in the permeability of any of the active substances was observed in the presence of any of the tested excipients in either of the models [30].
Nevertheless, some excipients could have some influence on intestinal permeability of active substances: Rege et al. [13] showed that polysorbate 80, sodium dodecyl sulfate and docusate have an impact on the Caco-2 permeability of low permeable drugs, such as furosemide, cimetidine and hydrochlorothiazide. These excipients increased the apical to basolateral direction permeability of these active substances. For example, polysorbate 80 could inhibit active efflux transporter P-gp. It significantly increases 7.49-fold furosemide Papp from apical to basolateral direction, which is very highest than the results obtained for all tested polyols (from 0.875- to 1-fold). Moreover, regarding basolateral to apical Papp and Papp ratio basolateral/apical values, polyols have no impact on efflux mechanism compared to polysorbate 80 on Ranitidine.
Another example is that the pharmaceutical excipient polyethylene glycol 400 has interaction with efflux transport proteins and leads to changes in the absorption characteristics of some active substances [15].
Compared to the results obtained for docusate, sodium dodecylsulfate or polysorbate, our study shows that mannitol, maltitol, sorbitol and xylitol did not modify the permeability of furosemide, amiloride, atenolol, ranitidine, nadolol, acyclovir and L-thyroxine. These tested drug models represent the relevant three different BCS classes and a majority of currently used drug substances, considering their solubility and permeability.
Moreover, according to different authors [9,13,31,32], the Caco-2 cell model seems to be oversensitive for describing the modulation of the drug permeability by excipients, compared to in vivo models. In our in vitro studies, polyols did not influence the Caco-2 transport of the tested drugs, owning different permeabilities. In addition, Caco-2 cells do not express mucins; hence, the mucus layer is absent in this cell model: mucus could limit the impact on active permeation enhancement of excipients with surfactant characteristics (Polysorbate®, Kolliphor®, Labrafil® and Labrasol®) [33].
It is, therefore, reasonable to assume that polyols will not have an impact on the intestinal absorption of these active ingredients in vivo. Further work is needed to evaluate in vivo the absorption of these drugs in the presence of polyols.
Author Contributions
Conceptualization, D.T. and M.R.; methodology, D.T., M.M., S.C., J.L. and M.R.; software, M.M., S.C., J.L. and M.R.; validation, D.T., M.M., S.C., J.L. and M.R.; formal analysis D.T., M.M., S.C., J.L. and M.R.; investigation, D.T., M.M., S.C., J.L. and M.R.; resources, D.T.; data curation, D.T., M.M., S.C., J.L. and M.R.; writing—original draft preparation, D.T. and O.H.; writing—review and editing, D.T. and O.H.; visualization, D.T. and O.H.; supervision D.T.; project administration, D.T.; funding acquisition, D.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Adkin, D.A.; Davis, S.S.; Sparrow, R.A.; Huckle, P.D.; Philips, A.J.; Wilding, I.R. The effects of pharmaceutical excipients on small intestinal transit. Br. J. Clin. Pharmacol. 1995, 39, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Ashiru, D.A.; Patel, R.; Basit, A.W. Polyethylene glycol 400 enhances the bioavailability of a BCS Class III drug (ranitidine) in male subjects but not females. Pharm. Res. 2008, 25, 2327–2333. [Google Scholar] [CrossRef] [PubMed]
- Basedow, A.; Gernot, M.; Schmidt, P.C. Sorbitol Instant an Excipient with Unique Tableting Properties. Drug Dev. Ind. Pharm. 2008, 12, 11–13. [Google Scholar] [CrossRef]
- Bolhuis, K.G.; Rexwinkel G., E.; Zuurman, K. Polyols as filler-binders for disintegrating tablets prepared by direct compaction. Drug Dev. Ind. Pharm. 2009, 35, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Tarlier, N.; Soulairol, I.; Sanchez-Ballester, N.; Gilles Baylac, G.; Aubert, A.; Lefevre, P.; Bataille, B.; Sharkawia, T. Deformation behavior of crystallized mannitol during compression using a rotary tablet press simulator. Int. J. Pharm. 2018, 547, 142–149. [Google Scholar] [CrossRef]
- Ohrem, H.L.; Schornick, E.; Kalivoda, A.R. Why is mannitol becoming more and more popular as a pharmaceutical excipient in solid dosage forms? Pharm. Dev. Technol. 2014, 19, 257–262. [Google Scholar] [CrossRef]
- Dash, R.P.; Srinivas, N.R.; Babu, R.J. Use of sorbitol as pharmaceutical excipient in the present day formulations-issues and challenges for drug absorption and bioavailability. Drug Dev. Ind. Pharm. 2019, 45, 1421–1429. [Google Scholar] [CrossRef] [PubMed]
- Amidon, G.L.; Lennernäs, H.; Shah, V.P.; Crison, J.R. A theoretical basis for a biopharmaceutics drug classification: The correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995, 12, 13–20. [Google Scholar]
- Aungst, B.J. Intestinal permeation enhancers. J. Pharm. Sci. 2000, 89, 429–442. [Google Scholar] [CrossRef]
- Adkin, A.D.; Davis, S.S.; Sparrow, R.A.; Huckle, P.D.; Phillips, A.J.; Wilding, I.R. The Effect of Mannitol on the Oral Bioavailability of Cimetidine. J. Pharm. Sci. 1995, 39, 381–387. [Google Scholar] [CrossRef]
- Chen, M.L.; Sadrieh, N.; Yu, L. Impact of Osmotically Active Excipients on Bioavailability and Bioequivalence of BCS Class III Drugs. AAPS J. 2013, 15, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Vaithianathan, S.; Haidar, S.H.; Zhang, X.; Jiang, W.; Avon, C.; Dowling, T.C.; Shao, C.; Kane, M.; Hoag, S.W.; Flasar, M.H.; et al. Effect of Common Excipients on the Oral Drug Absorption of Biopharmaceutics Classification System Class 3 Drugs Cimetidine and Acyclovir. J. Pharm. Sci. 2016, 105, 996–1005. [Google Scholar] [CrossRef] [PubMed]
- Rege, B.D.; Yu, L.X.; Hussain, A.S.; Polli, J.E. Effect of Common Excipients on Caco-2 Transport of Low-Permeability Drugs. J. Pharm. Sci. 2001, 90, 1770–1786. [Google Scholar] [CrossRef] [PubMed]
- Van Breemen, R.B.; Li, Y. Caco-2 cell permeability assays to measure drug absorption. Expert Opin. Drug Metab. Toxicol. 2005, 1, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.; Hang, M.; Yuan, M.; Yang, D.; Zhao, M.; Zhang, S.; Wang, P.; Zhang, R.; Gao, X. The pharmaceutical excipient PEG400 affect the absorption of baicalein in Caco-2 monolayer model by interacting with UDP-glucuronosyltransferases and efflux transport proteins. Pharmacol. Res. Perspect. 2022, 10, 928–942. [Google Scholar] [CrossRef]
- Xin, Z.; Li-Fang, W.; Jia-Qi, C.; Bo-Lin, Z.; Xiu-Hong, C.; Jun, L.I.; Peng-Fei, T.; Jin-Ling, W. Absorption mechanism of dragon’s blood phenolic extracts in Caco-2 cells. Zhongguo Zhong Yao Za Zhi. 2020, 45, 4889–4895. [Google Scholar]
- Zhen, Z.; Zhe, L.S.; Shuo, Z.; Jia, L.X.; Hui, L.; Qin, S.; Qing, Y.L. Transport of curcumin derivatives in Caco-2 cell monolayers. Eur. J. Pharm. Biopharm. 2017, 117, 123–131. [Google Scholar]
- Li, H.; Jin, H.E.; Kim, W.; Han, Y.H.; Kim, D.D.; Chung, S.J.; Shim, C.K. Involvement of P-glycoprotein, multidrug resistance protein 2 and breast cancer resistance protein in the transport of belotecan and topotecan in Caco-2 and MDCKII cells. Pharm Res. 2008, 25, 2601–2612. [Google Scholar] [CrossRef]
- Liu, Y.; Liang, X.; Zou, Y.; Peng, Y.; McClements, D.J.; Hu, K. Resveratrol-loaded biopolymer core-shell nanoparticles: Bioavailability and anti-inflammatory effects. Food Funct. 2020, 11, 4014–4025. [Google Scholar] [CrossRef]
- Calatayud, M.; Devesa, V.; Montoro, R.; Vélez, D. In vitro study of intestinal transport of arsenite, monomethylarsonous acid, and dimethylarsinous acid by Caco-2 cell line. Toxicol. Lett. 2011, 204, 127–133. [Google Scholar] [CrossRef]
- Ma, B.; Wang, J.; Sun, J.; Li, M.; Xu, H.; Sun, G.; Sun, X. Permeability of rhynchophylline across human intestinal cell in vitro. Int. J. Clin. Exp. Pathol. 2014, 7, 1957–1966. [Google Scholar] [PubMed]
- Lenhart, A.; Chey, W.D. A Systematic Review of the Effects of Polyols on Gastrointestinal Health and Irritable Bowel Syndrome. Adv. Nutr. 2017, 8, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Saha, P.; Kou, J.H. Effect of solubilizing excipients on permeation of poorly water-soluble compounds across Caco-2 cell monolayers. Eur. J. Pharm. Biopharm. 2000, 50, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Dale, O.; Nilsen, T.; Olaussen, G.; Tvedt, K.E.; Skorpen, F.; Smidsrød, O.; Vårum, K.M. Transepithelial transport of morphine and mannitol in Caco-2 cells: The influence of chitosans of different molecular weights and degrees of acetylation. J. Pharm. Pharmacol. 2006, 58, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Lazorova, L.; Gråsjö, J.; Artursson, P.; Bergström, M.; Wu, F.; Petterman-Bergström, E.; Ogren, M.; Långström, B. Quantification and imaging of mannitol transport through Caco-2 cell monolayers using a positron-emitting tracer. Pharm. Res. 1998, 15, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Müller, U.; Stübl, F.; Schwarzinger, B.; Sandner, G.; Iken, M.; Himmelsbach, M.; Schwarzinger, C.; Ollinger, N.; Stadlbauer, V.; Höglinger, O.; et al. In Vitro and In Vivo Inhibition of Intestinal Glucose Transport by Guava (Psidium Guajava) Extracts. Mol. Nutr. Food Res. 2018, 62, 1–11. [Google Scholar] [CrossRef]
- Rusznyák, A.; Palicskó, M.; Malanga, M.; Fenyvesi, E.; Szente, L.; Váradi, J.; Bácskay, I.; Vecsernyés, M.; Réti-Nagy, K.S.; Vasvári, G.; et al. Cellular Effects of Cyclodextrins: Studies on HeLa Cells. Molecules 2022, 27, 1589. [Google Scholar] [CrossRef]
- Artursson, P.; Borchardt, R.T. Intestinal drug absorption and metabolism in cell cultures: Caco-2 and beyond. Pharm. Res. 1997, 14, 1655–1658. [Google Scholar] [CrossRef]
- Cheméo—Chemical & Physical Properties by Cheméo Home page. Available online: http://www.chemeo.com (accessed on 1 February 2023).
- Parr, A.; Hidalgo, I.J.; Bode, C.; Brown, W.; Yazdanian, M.; Gonzalez, M.A.; Sagawa, K.; Miller, K.; Jiang, W.; Stippler, E.S. The Effect of Excipients on the Permeability of BCS Class III Compounds and Implications for Biowaivers. Pharm Res. 2016, 33, 167–176. [Google Scholar] [CrossRef]
- Artursson, P.; Lindmark, T.; Davis, S.S.; Illum, L. Effect of chitosan on the permeability of monolayers of intestinal epithelial-cells (Caco-2). Pharm. Res. 1994, 11, 1358–1361. [Google Scholar] [CrossRef]
- Anderberg, E.K.; Artursson, P. Cell Cultures to Access Drug Absorption Enhancement; De Boer, A.G., Ed.; Drug absorption enhancement; Hardwood Academic Publishers: Chur, Switzerland, 1994; pp. 113–114. [Google Scholar]
- Jakobsen, S.; Ge, L.G.; Pedersen, M.; Griffin, B.T.; Holm, R.; Nielsen, C. P-glycoprotein-mediated transport in a mucus-supplemented Caco-2 cell model in the presence of different surfactants. Int. J. Pharm. 2022, 624, 121885–121895. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).