Kiwifruit (Actinidia spp.) Dietary Consumption for Constipation: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
1.1. Kiwifruit Species and Their Nutritional Characteristics
1.2. Constipation and Its Causes
1.3. A First-Line Clinical Approach to Constipation
1.4. Research Objectives
2. Methods
2.1. Eligibility Criteria
- P (population): patients suffering from chronic constipation (any cause of benign origin). Studies involving healthy participants were included all the same, provided that they reported relevant outcomes;
- I (intervention): kiwifruit consumption, preferably peeled (as customary in common dietary habits). Studies with kiwifruit-derived dietary supplements were excluded from the main search but still mentioned in the ‘Introduction’ Section for better comprehensiveness;
- C (comparison): any type, including no control;
- O (outcomes): bowel movements per day or week and stool consistency (preferably assessed with the Bristol score);
- S (study design): clinical studies, either controlled trials or pre–post studies. In vitro and in vivo laboratory experiments were excluded.
2.2. Information Sources
2.3. Search Strategy
2.4. Selection Process
2.5. Data Collection Process
2.6. Data Items and Effect Measures
2.7. Study Risk of Bias Assessment
2.8. Synthesis Methods
- P (population): patients suffering from chronic constipation or healthy participants (only per-protocol and no-intention-to-treat study populations were considered);
- I (intervention): kiwifruit dietary consumption;
- C (comparison): kiwifruit-free diet/placebo pills/control drinks or sources of fibre intake other than kiwifruits (these two study categories were kept separated in a dedicated subgroup analysis);
- O (outcomes): defecation frequency or bowel movements per time period (day or week). It was decided not to meta-analyse data about stool consistency because of heterogeneous outcome measures;
- S (study design): randomised controlled trials.
2.9. Reporting Bias Assessment
2.10. Certainty Assessment
3. Results
3.1. Qualitative Results
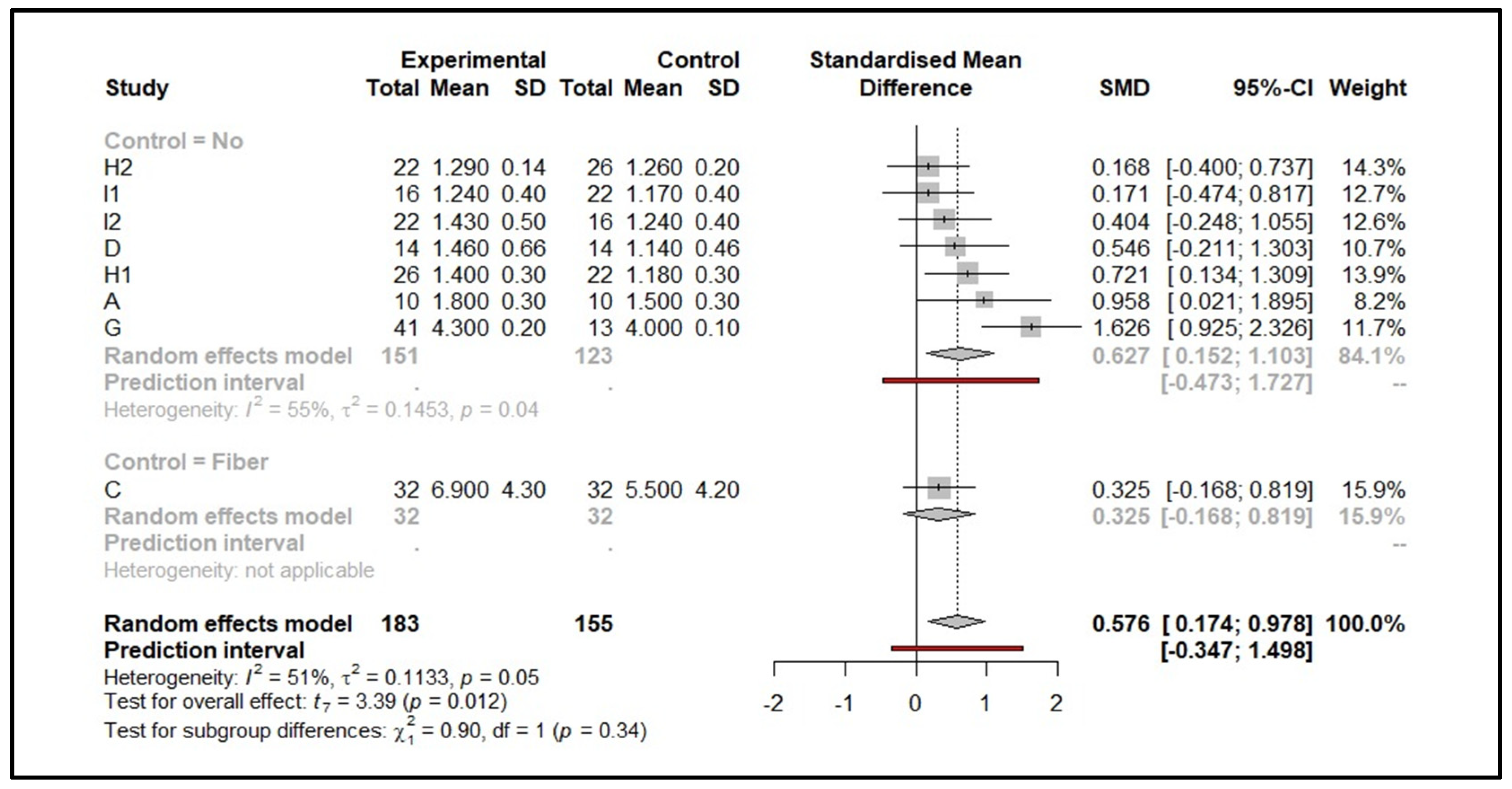
3.2. Quantitative Results
4. Discussion
4.1. A critical Overview of Qualitative–Quantitative Evidence
4.2. Mechanism of Action
4.3. Safety and Tolerability of Intervention
4.4. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Crowhurst, R.N.; Gleave, A.P.; MacRae, E.A.; Ampomah-Dwamena, C.; Atkinson, R.G.; Beuning, L.L.; Bulley, S.M.; Chagne, D.; Marsh, K.B.; Matich, A.J.; et al. Analysis of Expressed Sequence Tags from Actinidia: Applications of a Cross Species EST Database for Gene Discovery in the Areas of Flavor, Health, Color and Ripening. BMC Genom. 2008, 9, 351. [Google Scholar] [CrossRef] [Green Version]
- Dias, M.; Caleja, C.; Pereira, C.; Calhelha, R.C.; Kostic, M.; Sokovic, M.; Tavares, D.; Baraldi, I.J.; Barros, L.; Ferreira, I.C.F.R. Chemical Composition and Bioactive Properties of Byproducts from Two Different Kiwi Varieties. Food Res. Int. 2020, 127, 108753. [Google Scholar] [CrossRef]
- Nishiyama, I.; Yamashita, Y.; Yamanaka, M.; Shimohashi, A.; Fukuda, T.; Oota, T. Varietal Difference in Vitamin C Content in the Fruit of Kiwifruit and Other Actinidia Species. J. Agric. Food Chem. 2004, 52, 5472–5475. [Google Scholar] [CrossRef]
- Food Data Central. Available online: https://fdc.nal.usda.gov/ (accessed on 25 August 2021).
- He, X.; Fang, J.; Chen, X.; Zhao, Z.; Li, Y.; Meng, Y.; Huang, L. Actinidia Chinensis Planch: A Review of Chemistry and Pharmacology. Front. Pharmacol. 2019, 10, 1236. [Google Scholar] [CrossRef] [PubMed]
- Celik, A.; Ercisli, S.; Turgut, N. Some Physical, Pomological and Nutritional Properties of Kiwifruit Cv. Hayward. Int. J. Food Sci. Nutr. 2007, 58, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Lembo, A.; Camilleri, M. Chronic Constipation. N. Engl. J. Med. 2003, 349, 1360–1368. [Google Scholar] [CrossRef]
- Higgins, P.D.R.; Johanson, J.F. Epidemiology of Constipation in North America: A Systematic Review. Am. J. Gastroenterol. 2004, 99, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Annells, M.; Koch, T. Constipation and the Preached Trio: Diet, Fluid Intake, Exercise. Int. J. Nurs. Stud. 2003, 40, 843–852. [Google Scholar] [CrossRef]
- Bayer, S.B.; Gearry, R.B.; Drummond, L.N. Putative Mechanisms of Kiwifruit on Maintenance of Normal Gastrointestinal Function. Crit. Rev. Food Sci. Nutr. 2018, 58, 2432–2452. [Google Scholar] [CrossRef] [Green Version]
- Alame, A.M.; Bahna, H. Evaluation of Constipation. Clin. Colon Rectal Surg. 2012, 25, 5–11. [Google Scholar] [CrossRef] [Green Version]
- Rigby, D.; Powell, M. Causes of Constipation and Treatment Options. Prim. Health Care Res. Dev. 2005, 15, 41–50. [Google Scholar] [CrossRef]
- Bae, S.H. Diets for Constipation. Pediatr. Gastroenterol. Hepatol. Nutr. 2014, 17, 203–208. [Google Scholar] [CrossRef] [Green Version]
- Drummond, L.; Gearry, R.B. Kiwifruit Modulation of Gastrointestinal Motility. Adv. Food Nutr. Res. 2013, 68, 219–232. [Google Scholar] [CrossRef]
- Weir, I.; Shu, Q.; Wei, N.; Wei, C.; Zhu, Y. Efficacy of Actinidin-Containing Kiwifruit Extract Zyactinase on Constipation: A Randomised Double-Blinded Placebo-Controlled Clinical Trial. Asia Pac. J. Clin. Nutr. 2018, 27, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Ansell, J.; Butts, C.A.; Paturi, G.; Eady, S.L.; Wallace, A.J.; Hedderley, D.; Gearry, R.B. Kiwifruit-Derived Supplements Increase Stool Frequency in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study. Nutr. Res. 2015, 35, 401–408. [Google Scholar] [CrossRef] [Green Version]
- Udani, J.K.; Bloom, D.W. Effects of Kivia Powder on Gut Health in Patients with Occasional Constipation: A Randomized, Double-Blind, Placebo-Controlled Study. Nutr. J. 2013, 12, 78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kindleysides, S.; Kuhn-Sherlock, B.; Yip, W.; Poppitt, S.D. Encapsulated Green Kiwifruit Extract: A Randomised Controlled Trial Investigating Alleviation of Constipation in Otherwise Healthy Adults. Asia Pac. J. Clin. Nutr. 2015, 24, 421–429. [Google Scholar] [CrossRef]
- Zhuang, Z.; Chen, M.; Niu, J.; Qu, N.; Ji, B.; Duan, X.; Liu, Z.; Liu, X.; Wang, Y.; Zhao, B. The Manufacturing Process of Kiwifruit Fruit Powder with High Dietary Fiber and Its Laxative Effect. Molecules 2019, 24, 3813. [Google Scholar] [CrossRef] [Green Version]
- Abbasalizadeh, S.; Ebrahimi, B.; Azizi, A.; Dargahi, R.; Tayebali, M.; Ghadim, S.T.; Foroumandi, E.; Aliasghari, F.; Javadi, M.; Izadi, A.; et al. Review of Constipation Treatment Methods with Emphasis on Laxative Foods. Curr. Nutr. Food Sci. 2020, 16, 675–688. [Google Scholar] [CrossRef]
- Montoya, C.A.; Henare, S.J.; O’Donoghue, E.M.; Rosendale, D.; Edwards, P.; Moughan, P.J. Kiwifruit (Actinidia Deliciosa), Compared with Cellulose and Psyllium, Influences the Histology and Mucus Layer of the Gastrointestinal Tract in the Growing Pig. Food Funct. 2021, 12, 8007–8016. [Google Scholar] [CrossRef]
- EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA); Turck, D.; Castenmiller, J.; De Henauw, S.; Hirsch-Ernst, K.I.; Kearney, J.; Knutsen, H.K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; et al. Green Kiwifruit (lat. Var. Hayward) and Maintenance of Normal Defecation: Evaluation of a Health Claim pursuant to Article 13(5) of Regulation (EC) No 1924/2006. EFSA J. 2021, 19, e06641. [Google Scholar] [CrossRef] [PubMed]
- Xing, J.H.; Soffer, E.E. Adverse Effects of Laxatives. Dis. Colon Rectum 2001, 44, 1201–1209. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the Quality of Reports of Randomized Clinical Trials: Is Blinding Necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Kjaergard, L.L.; Villumsen, J.; Gluud, C. Reported Methodologic Quality and Discrepancies between Large and Small Randomized Trials in Meta-Analyses. Ann. Intern. Med. 2001, 135, 982–989. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Wiley Cochrane Series; Wiley-Blackwell: Hoboken, NJ, USA, 2019; ISBN 9781119536628. [Google Scholar]
- IntHout, J.; Ioannidis, J.P.A.; Borm, G.F. The Hartung-Knapp-Sidik-Jonkman Method for Random Effects Meta-Analysis Is Straightforward and Considerably Outperforms the Standard DerSimonian-Laird Method. BMC Med. Res. Methodol. 2014, 14, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldet, G.; Howick, J. Understanding GRADE: An Introduction. J. Evid. Based Med. 2013, 6, 50–54. [Google Scholar] [CrossRef]
- Caballero, N.; Benslaiman, B.; Ansell, J.; Serra, J. The Effect of Green Kiwifruit on Gas Transit and Tolerance in Healthy Humans. Neurogastroenterol. Motil. 2020, 32, e13874. [Google Scholar] [CrossRef] [PubMed]
- Eady, S.L.; Wallace, A.J.; Hedderley, D.I.; Bentley-Hewitt, K.L.; Butts, C.A. The Effects on Immune Function and Digestive Health of Consuming the Skin and Flesh of Zespri SunGold Kiwifruit (Var. “Zesy002”) in Healthy and IBS-Constipated Individuals. Nutrients 2020, 12, 1453. [Google Scholar] [CrossRef]
- Eady, S.L.; Wallace, A.J.; Butts, C.A.; Hedderley, D.; Drummond, L.; Ansell, J.; Gearry, R.B. The Effect of “Zesy002” Kiwifruit (Var.) on Gut Health Function: A Randomised Cross-over Clinical Trial. J. Nutr. Sci. 2019, 8, e18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilkinson-Smith, V.; Dellschaft, N.; Ansell, J.; Hoad, C.; Marciani, L.; Gowland, P.; Spiller, R. Mechanisms Underlying Effects of Kiwifruit on Intestinal Function Shown by MRI in Healthy Volunteers. Aliment. Pharmacol. Ther. 2019, 49, 759–768. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.-O.-O.; Leung, G.; Tong, T.; Wong, N.-Y. Increasing Dietary Fiber Intake in Terms of Kiwifruit Improves Constipation in Chinese Patients. World J. Gastroenterol. 2007, 13, 4771–4775. [Google Scholar] [CrossRef]
- Chey, S.W.; Chey, W.D.; Jackson, K.; Eswaran, S. Exploratory Comparative Effectiveness Trial of Green Kiwifruit, Psyllium, or Prunes in US Patients With Chronic Constipation. Am. J. Gastroenterol. 2021, 116, 1304–1312. [Google Scholar] [CrossRef]
- Chang, C.-C.; Lin, Y.-T.; Lu, Y.-T.; Liu, Y.-S.; Liu, J.-F. Kiwifruit Improves Bowel Function in Patients with Irritable Bowel Syndrome with Constipation. Asia Pac. J. Clin. Nutr. 2010, 19, 451–457. [Google Scholar]
- Rush, E.C.; Patel, M.; Plank, L.D.; Ferguson, L.R. Kiwifruit Promotes Laxation in the Elderly. Asia Pac. J. Clin. Nutr. 2002, 11, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Senn, S.S. Cross-Over Trials in Clinical Research; John Wiley & Sons: Hoboken, NJ, USA, 2002; ISBN 9780471496533. [Google Scholar]
- McCrea, G.L.; Miaskowski, C.; Stotts, N.A.; Macera, L.; Varma, M.G. A Review of the Literature on Gender and Age Differences in the Prevalence and Characteristics of Constipation in North America. J. Pain Symptom Manag. 2009, 37, 737–745. [Google Scholar] [CrossRef]
- Cremon, C.; Ansell, J.; Pagano, I.; Kuhn-Sherlock, B.; Drummond, L.; Barbaro, M.R.; Capelli, E.; Bellacosa, L.; Stanghellini, V.; Barbara, G. Su1659–A Randomized, Controlled, Single-Blind, Cross-over Study Assessing the Effect of Green Kiwifruit on Digestive Functions and Microbiota in Constipated Patients. Gastroenterology 2018, 154, S565–S566. [Google Scholar] [CrossRef]
- Wilkinson-Smith, V.; Dellschaft, N.; Hoad, C.; Marciani, L.; Gowland, P.; Spiller, R. Increase in small bowel water content and fluidity of ascending colon contents induced by kiwifruit is associated with more frequent looser stools in healthy volunteers: A mechanistic MRI study (Oral Presentations). Neurogastroenterol. Motil. 2018, 30, e13422. [Google Scholar] [CrossRef] [Green Version]
- McRorie, J.W.; McKeown, N.M. Understanding the Physics of Functional Fibers in the Gastrointestinal Tract: An Evidence-Based Approach to Resolving Enduring Misconceptions about Insoluble and Soluble Fiber. J. Acad. Nutr. Diet. 2017, 117, 251–264. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.K.; Low, K.Y.; Siah, K.; Drummond, L.M.; Gwee, K.-A. Kiwifruit (Actinidia Deliciosa) Changes Intestinal Microbial Profile. Microb. Ecol. Health Dis. 2012, 23. [Google Scholar] [CrossRef]
- Chalabi, M.; Khademi, F.; Yarani, R.; Mostafaie, A. Proteolytic Activities of Kiwifruit Actinidin (Actinidia Deliciosa Cv. Hayward) on Different Fibrous and Globular Proteins: A Comparative Study of Actinidin with Papain. Appl. Biochem. Biotechnol. 2014, 172, 4025–4037. [Google Scholar] [CrossRef]
- Henare, S.J.; Rutherfurd, S.M. Digestion of Kiwifruit Fiber. Adv. Food Nutr. Res. 2013, 68, 187–203. [Google Scholar] [CrossRef]
- Allison, M.J.; Cook, H.M.; Milne, D.B.; Gallagher, S.; Clayman, R.V. Oxalate Degradation by Gastrointestinal Bacteria from Humans. J. Nutr. 1986, 116, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.S.A.; Lewis, S.A.; Hourihane, J.O. Kiwi Fruit Allergy: A Review. Pediatr. Allergy Immunol. 2003, 14, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Henley, S.; Misner, S. Dietary Fiber. Available online: http://mail.konjacfoods.com/fiber/fiberar.pdf (accessed on 26 October 2021).
- Kishimoto, Y.; Kanahori, S.; Sakano, K.; Ebihara, S. The Maximum Single Dose of Resistant Maltodextrin That Does Not Cause Diarrhea in Humans. J. Nutr. Sci. Vitaminol. 2013, 59, 352–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Components of Kiwifruit | Yellow Kiwifruit | Green Kiwifruit | ||||
|---|---|---|---|---|---|---|
| Average Amount (Per 100 g of Product) | % DRI *-Males | % DRI *-Females | Average Amount (Per 100 g of Product) | % DRI *-Males | % DRI *-Females | |
| Water | 82.4 g | 2% | 3% | 83.9 g | 2% | 3% |
| Proteins | 1.02 g | 2% | 2% | 1.06 g | 2% | 2% |
| Lipids | 0.28 g | <1% | <1% | 0.44 g | <1% | 1% |
| Carbohydrates | 15.8 g | 12% | 12% | 12.0–14.0 g | 10% | 10% |
| Fiber | 1.4 g | 4% | 6% | 3.0 g | 8% | 12% |
| Calcium | 17.0 mg | 2% | 2% | 35.0 mg | 4% | 4% |
| Magnesium | 12.0 mg | 3% | 4% | 15.7 mg | 4% | 5% |
| Potassium | 315.0 mg | 10% | 13% | 198.0 mg | 6% | 8% |
| Beta-carotene | 1.0 µg | <1% | <1% | 52.0 µg | 6% | 7% |
| Vitamin C | 161.3 mg | 179% | 216% | 74.7 mg | 83% | 100% |
| Vitamin K | 6.1 µg | 5% | 7% | 40.3 µg | 34% | 45% |
| Study ID | Population | Study Participants’ Diseases § | Lifestyle Habits Prescribed during the Study Period | Drugs Allowed | Drugs Excluded | Differences between Groups at Baseline | Intervention | Comparison | Outcomes (Mean ± SD Unless Otherwise Indicated) | Study Design | Jadad Score | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 11 healthy subjects (8F/3M), age range: 18–23 | None (absence of gastrointestinal symptoms) | Low-flatulogenic diet excluding legumes, vegetables, garlic, onion, cucumber, nuts, cereals, whole-meal bread, and fizzy drinks | − | − | No (cross-over design) | 2 peeled GKs every day for 2 weeks | No intervention | BMs/day (int. vs. con.) (mean ± SE): 1.8 ± 0.1 vs. 1.5 ± 0.1 (*) SC (int. vs. con.) (mean ± SE): 3.3 ± 0.2 vs. 2.8 ± 0.1 (*) | Cross-over RCT (2-week washout period) | 4 | [30] |
| B | 19 healthy subjects + 19 patients with IBS-C (27F/11M), age range: 22–65 | None or IBS-C diagnosed according to the Rome III criteria (patients with severe or unstable health conditions were excluded) | Fibre supplements-free diet and no laxatives for at least 2 weeks before starting the study and during the entire trial period | Antidepressants, opioids, anti-inflammatory drugs, anti-diabetic agents | Others, including laxatives | No (cross-over design) | 3 peeled YKs every day for 4 weeks | 3 unpeeled YKs every day for 4 weeks | -Healthy subjects (peeled YKs): CBMs/week (int.): from 9.7 ± 5.6 to 9.7 ± 5.6 SC (int.): from 3.3 ± 0.7 to 4.0 ± 1.0 (*) -Patients with IBS-C (peeled YKs): CBMs/week (int.): from 6.7 ± 4.8 to 8.7 ± 6.9 SC (int.): from 3.5 ± 1.0 to 3.9 ± 1.0 | Cross-over RCT (4-week washout period) | 2 | [31] |
| C | 32 patients with constipation (32F/0M), age range: 21–65 | Mild constipation (patients with severe or unstable health conditions were excluded) | No (cross-over design) | 3 peeled YKs every day for 4 weeks | Dietary fibre (Metamucil®): 5 g/day for 4 weeks | CBMs/week (int.): from 4.2 ± 3.1 to 6.9 ± 4.3 (*) CBMs/week (int. vs. con.): 6.9 ± 4.3 vs. 5.5 ± 4.2 SC (int.): from 3.24 ± 1.13 to 4.15 ± 1.26 (*) SC (int. vs. con.): 4.15 ± 1.26 vs. 3.52 ± 1.27 (*) | Cross-over RCT (4-week washout period) | 4 | [32] | |||
| D | 14 healthy subjects (6F/8M), age range: 21–33 | None (patients with gastrointestinal disorders, recent surgery, or contraindications to MRI scans were excluded) | Abstinence from caffeine, alcohol, and strenuous exercise for at least 48 h prior to outcome assessment | − | Medications affecting intestinal motility | No (cross-over design) | 4 peeled GKs every day for 3 days | A control drink once a day for 3 days | DF/day (int. vs. con.): 1.46 ± 0.66 vs. 1.14 ± 0.46 (*) SC (int. vs. con.): significantly softer stools in the GK arm (*)-results only graphically displayed. | Cross-over RCT (15-day washout period) | 3 | [33] |
| E | 20 healthy subjects + 33 patients with constipation (42F/11M), age: 49.9 ± 12.0 | None or chronic constipation lasting for at least 6 (patients with unstable or severe health conditions were excluded, along with pregnant or breastfeeding women, and subjects unable to understand Chinese) | Average dietary pattern (China) and no changes in physical activity levels during the study period | Laxatives (their use among patients was recorded) | − | Yes (case–control study) | 2 peeled GKs every day for 4 weeks administered to patients with constipation | The same intervention in healthy subjects | -Healthy subjects: CBMs/week (int.): from 6.5 ± 1.6 to 7.1 ± 2.2 (*) SC (int.): from 4.0 ± 0.9 to 4.2 ± 0.8 -Patients with constipation: CBMs/week (int.): from 2.2 ± 2.6 to 4.4 ± 4.6 (*) SC (int.): from 3.1 ± 1.9 to 3.3 ± 1.2 | Case control study | − | [34] |
| F | 79 patients with chronic constipation (69F/10M), age range: 18–76 | IBS-C diagnosed according to the Rome IV criteria with chronic constipation lasting for at least 3 months (patients with unstable or severe health conditions were excluded, along with pregnant women and subjects taking probiotics or antibiotics for any reason) | Avoid any changes in dietary habits and other sources of kiwifruit, prunes, or psyllium | − | Probiotics, antibiotics, opioids, laxative drugs, and supplements | No, except for the abdominal pain score (higher in the kiwifruit group) | 2 peeled GKs every day for 4 weeks (n = 30) | Con. 1: 100 g prunes every day (n = 26) Con. 2: 12 g psyllium every day (n = 23) for 4 weeks | -CBMs/week: no significant difference between groups (mean). Int.: from 1.2 to 2.2 (*) Con. 1: from 1.0 to 3.7 (*) Con. 2: from 1.1 to 2.8 (*) -SC: no significant difference between groups (mean). Int.: from 3.2 to 3.6 (*) Con. 1: from 3.1 to 3.6 (*) Con. 2: from 2.9 to 3.1 | RCT | 3 | [35] |
| G | 16 healthy subjects + 54 patients with IBS-C (65F/5M), mean age: 20–30 | None or IBS-C diagnosed according to the Rome III criteria (patients using laxatives or who underwent recent surgery were excluded) | Average dietary pattern (Taiwan) and no changes in physical activity levels during the study period | − | Laxatives, dietary supplements, and fortified foods | Yes (defecation frequency was lower among patients with IBS if compared with healthy controls) | 2 peeled GKs every day for 4 weeks | 2 placebo capsules every day for 4 weeks | DF was significantly higher in the IBS-C int. group compared to the IBS-C con. group after 1 week of treatment (*). However, DF was still significantly lower in the IBS-C int. group compared to healthy controls after 2 weeks of treatment. No significant difference between groups was observed in faecal volume changes. | Placebo-controlled trial | 1 | [36] |
| H | 48 healthy subjects (30F/18M), age: 33 ± 1 | None | Average dietary pattern (New Zealand) and no changes in physical activity levels during the study period | − | − | No (cross-over design) | 1 GK for every 30 kg of body weight on a daily basis for 3 weeks | A kiwifruit-free diet for 3 weeks | Intervention significantly decreased SC (*) without significant variations in CBMs (mean ± SE). Pre-cross-over period (int. vs. con.): DF: 1.40 ± 0.04 vs. 1.18 ± 0.04 SC: 2.34 ± 0.03 vs. 2.90 ± 0.03 Post-cross-over period (int. vs. con.): DF: 1.26 ± 0.04 vs. 1.29 ± 0.03 SC: 2.84 ± 0.03 vs. 2.59 ± 0.03 | Cross-over RCT (no washout period) | 2 | [37] |
| I | 38 healthy subjects (25F/13M), age > 60 years old | None (patients with severe health conditions or unable to provide reliable feedback due to marked cognitive decline were excluded) | Laxatives (their use among patients was recorded) | − | No (cross-over design) | Intervention significantly increased DF and decreased SC (*) (mean ± SE). Pre-cross-over period (int. vs. con.): DF: 1.24 ± 0.11 vs. 1.17 ± 0.07 SC: 2.59 ± 0.10 vs. 2.69 ± 0.09 Post-cross-over period (int. vs. con.): DF: 1.24 ± 0.11 vs. 1.43 ± 0.11 SC: 2.83 ± 0.08 vs. 2.28 ± 0.11 | Cross-over RCT (no washout period) |
| Study ID | Population (n) | N of Fruits | Duration | Significant Change from Baseline within Intervention Groups | Significant Post-Test Difference between Groups (Int. vs. Con.) | Reference | ||
|---|---|---|---|---|---|---|---|---|
| DF/CBMs | SC | DF/CBMs | SC | |||||
| A | 11 | 2/day | 2 weeks | Yes (*) | Yes (*) | [30] | ||
| B | 19 | 3/day | 4 weeks | No | Yes (*) | [31] | ||
| D | 14 | 4/day | 3 days | Yes (*) | Yes (*) | [33] | ||
| E | 20 | 2/day | 4 weeks | Yes (*) | No | [34] | ||
| H | 48 | 2–3/day | 3 weeks | No | Yes (*) | [37] | ||
| I | 38 | Yes (*) | Yes (*) | |||||
| Study ID | Population (n) | N of Fruits | Duration | Significant Change from Baseline within Intervention Groups | Significant Post-Test Difference between Groups (Int. vs. Con.) | Reference | ||
|---|---|---|---|---|---|---|---|---|
| DF/CBMs | SC | DF/CBMs | SC | |||||
| B | 19 | 3/day | 4 weeks | No | No | [31] | ||
| C | 32 | 3/day | 4 weeks | Yes (*) | Yes (*) | No | Yes (*) | [32] |
| E | 33 | 2/day | 4 weeks | Yes (*) | No | [34] | ||
| F | 79 | 2/day | 4 weeks | Yes (*) | Yes (*) | No | No | [35] |
| G | 54 | 2/day | 4 weeks | Yes (*) | No | [36] | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonelli, M.; Donelli, D. Kiwifruit (Actinidia spp.) Dietary Consumption for Constipation: A Systematic Review and Meta-Analysis. Future Pharmacol. 2021, 1, 27-40. https://doi.org/10.3390/futurepharmacol1010003
Antonelli M, Donelli D. Kiwifruit (Actinidia spp.) Dietary Consumption for Constipation: A Systematic Review and Meta-Analysis. Future Pharmacology. 2021; 1(1):27-40. https://doi.org/10.3390/futurepharmacol1010003
Chicago/Turabian StyleAntonelli, Michele, and Davide Donelli. 2021. "Kiwifruit (Actinidia spp.) Dietary Consumption for Constipation: A Systematic Review and Meta-Analysis" Future Pharmacology 1, no. 1: 27-40. https://doi.org/10.3390/futurepharmacol1010003
APA StyleAntonelli, M., & Donelli, D. (2021). Kiwifruit (Actinidia spp.) Dietary Consumption for Constipation: A Systematic Review and Meta-Analysis. Future Pharmacology, 1(1), 27-40. https://doi.org/10.3390/futurepharmacol1010003







