Control of Aerosolised Type A Influenza Virus H1N1 and a Coronavirus with Vapours Containing Catmint Essential Oil
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses and Cell Lines
2.2. Preparation of Catmint Oil Formulations
2.3. Antiviral Activity
2.3.1. In Solution
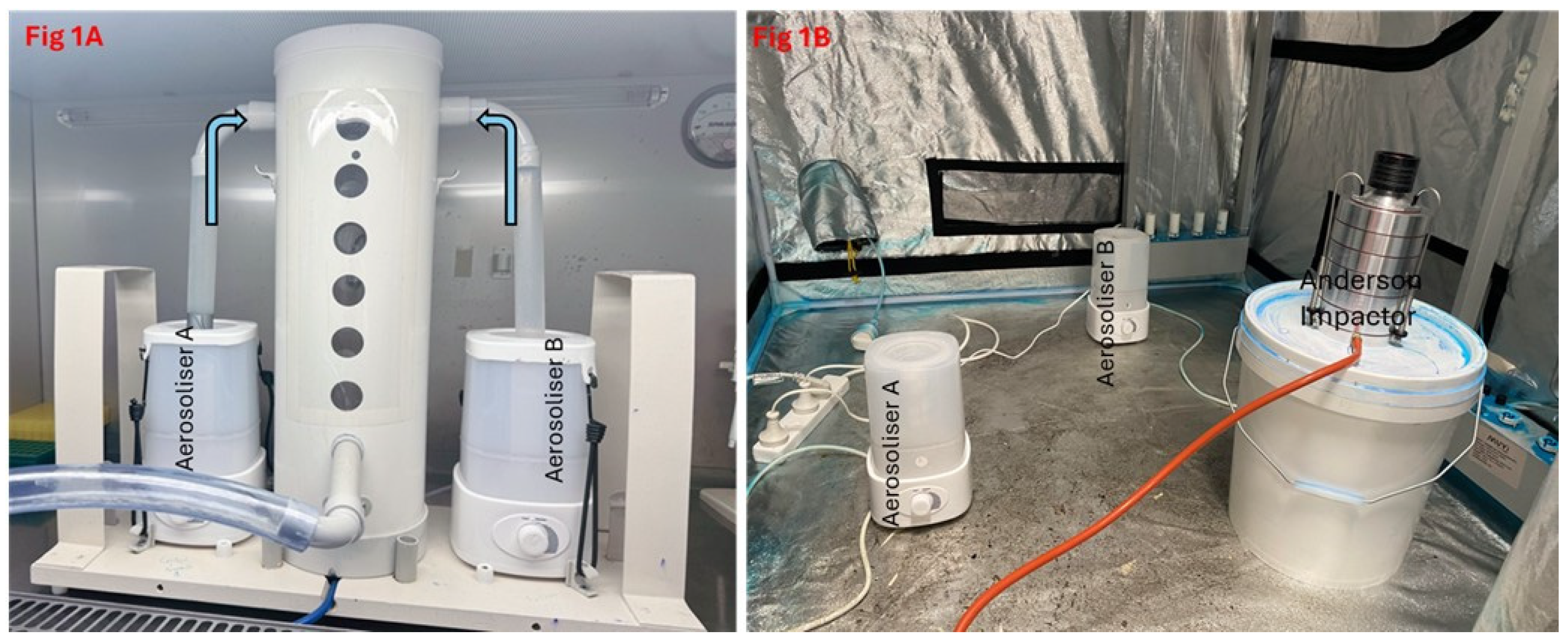
2.3.2. In Aerosolised Form
2.4. Determination of TCID50
2.5. Plaque Assay
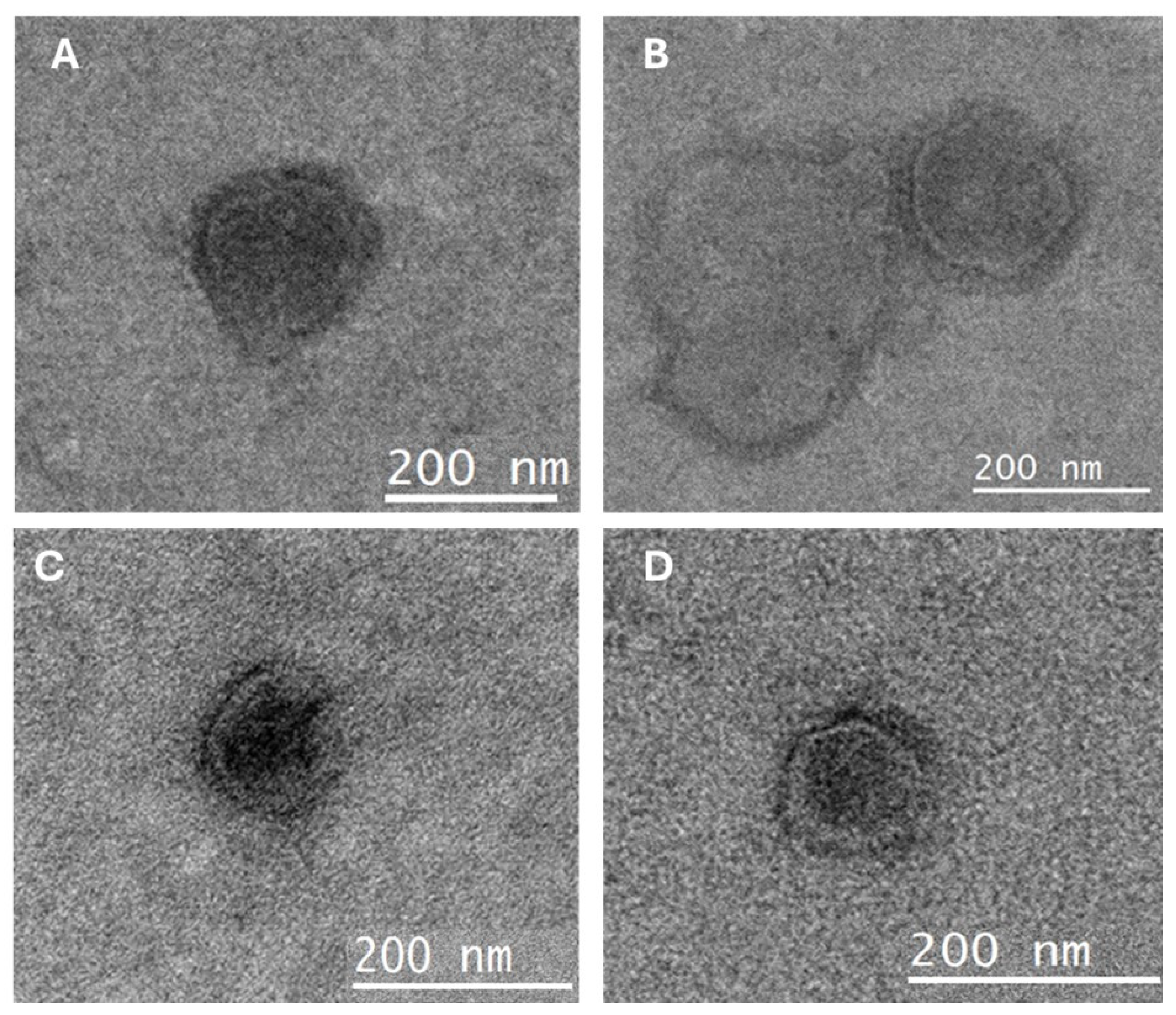
2.6. Transmission Electron Microscopy
2.7. Statistical Analysis
3. Results
3.1. Effect of Formulation (1) in Solution
3.2. In Aerosol Form
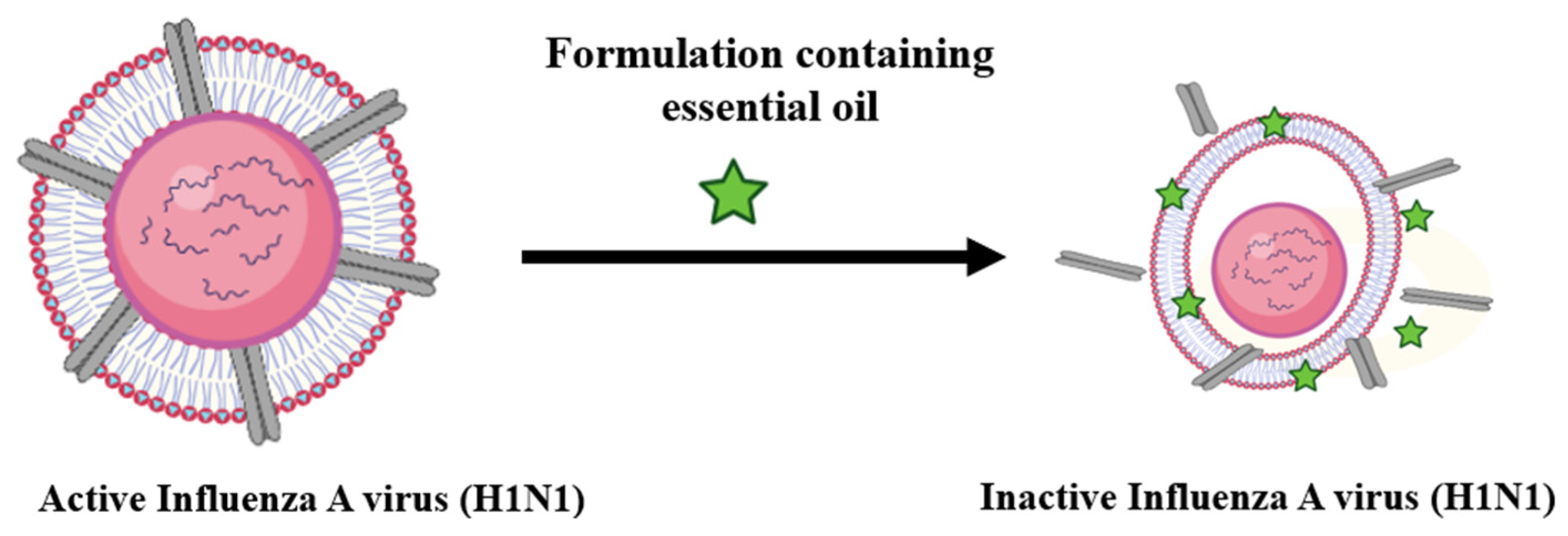
3.3. Transmission Electron Microscopy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HCO | Hydrogenated catmint oil |
| NHCO | Non-hydrogenated catmint oil |
| TEM | Transmission electron microscopy |
| TCID50 | Tissue culture infection dose |
| MHV-1 | Murine hepatitis virus |
| TGA | Therapeutic Goods Administration |
References
- Cowling, B.J.; Ip, D.K.; Fang, V.J.; Suntarattiwong, P.; Olsen, S.J.; Levy, J.; Uyeki, T.M.; Leung, G.M.; Malik Peiris, J.; Chotpitayasunondh, T. Aerosol transmission is an important mode of influenza A virus spread. Nat. Commun. 2013, 4, 1935. [Google Scholar] [PubMed]
- Koster, F. The experimental aerosol transmission of influenza virus. Future Virol. 2013, 8, 969–981. [Google Scholar]
- Corzo, C.A.; Culhane, M.; Dee, S.; Morrison, R.B.; Torremorell, M. Airborne detection and quantification of swine influenza a virus in air samples collected inside, outside and downwind from swine barns. PLoS ONE 2013, 8, e71444. [Google Scholar] [CrossRef]
- Zhang, H.; Li, X.; Ma, R.; Li, X.; Zhou, Y.; Dong, H.; Li, X.; Li, Q.; Zhang, M.; Liu, Z.; et al. Airborne spread and infection of a novel swine-origin influenza A (H1N1) virus. Virol. J. 2013, 10, 204. [Google Scholar] [CrossRef] [PubMed]
- Tellier, R. Review of aerosol transmission of influenza A virus. Emerg. Infect. Dis. 2006, 12, 1657. [Google Scholar]
- Neira, V.; Rabinowitz, P.; Rendahl, A.; Paccha, B.; Gibbs, S.G.; Torremorell, M. Characterization of Viral Load, Viability and Persistence of Influenza A Virus in Air and on Surfaces of Swine Production Facilities. PLoS ONE 2016, 11, e0146616. [Google Scholar] [CrossRef]
- Andraud, M.; Herve, S.; Gorin, S.; Barbier, N.; Queguiner, S.; Paboeuf, F.; Simon, G.; Rose, N. Evaluation of early single dose vaccination on swine influenza A virus transmission in piglets: From experimental data to mechanistic modelling. Vaccine 2023, 41, 3119–3127. [Google Scholar] [CrossRef]
- Konishi, T. Mutations in SARS-CoV-2 are on the increase against the acquired immunity. PLoS ONE 2022, 17, e0271305. [Google Scholar] [CrossRef]
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Primers 2018, 4, 3. [Google Scholar] [CrossRef]
- Nuwarda, R.F.; Alharbi, A.A.; Kayser, V. An Overview of Influenza Viruses and Vaccines. Vaccines 2021, 9, 1032. [Google Scholar] [CrossRef]
- Najar, B.; Nardi, V.; Stincarelli, M.A.; Patrissi, S.; Pistelli, L.; Giannecchini, S. Screening of the essential oil effects on human H1N1 influenza virus infection: An in vitro study in MDCK cells. Nat. Prod. Res. 2022, 36, 3149–3152. [Google Scholar] [CrossRef]
- Vimalanathan, S.; Hudson, J. Anti-influenza virus activity of essential oils and vapors. Am. J. Essent. Oils Nat. Prod. 2014, 2, 47–53. [Google Scholar]
- Oh, Y.J.; Kim, Y.S.; Kim, J.W.; Kim, D.W. Antibacterial and Antiviral Properties of Pinus densiflora Essential Oil. Foods 2023, 12, 4279. [Google Scholar] [CrossRef] [PubMed]
- Rao, H.; Ahmad, S.; Aati, H.Y.; Basit, A.; Ahmad, I.; Ghalloo, B.A.; Shehzad, M.N.; Nazar, R.; Zeeshan, M.; Nasim, M.J.; et al. Phytochemical screening, biological evaluation, and molecular docking studies of aerial parts of Trigonella hamosa (branched Fenugreek). Arab. J. Chem. 2023, 16, 104795. [Google Scholar]
- Singh, H.; Singh, D.; Lekhak, M.M. Ethnobotany, botany, phytochemistry and ethnopharmacology of the genus Thalictrum L. (Ranunculaceae): A review. J. Ethnopharmacol. 2023, 305, 115950. [Google Scholar] [CrossRef]
- Tang, Y.Q.N.; Deng, J.; Li, L.; Yan, J.; Lin, L.M.; Li, Y.M.; Lin, Y.; Xia, B.H. Essential oil from Prunella vulgaris L. as a valuable source of bioactive constituents: In vitro anti-bacterial, anti-viral, immunoregulatory, anti inflammatory, and chemical profiles. South Afr. J. Bot. 2022, 151, 614–627. [Google Scholar]
- Najar, B.; Mecacci, G.; Nardi, V.; Cervelli, C.; Nardoni, S.; Mancianti, F.; Ebani, V.V.; Giannecchini, S.; Pistelli, L. Volatiles and Antifungal-Antibacterial-Antiviral Activity of South African Salvia spp. Essential Oils Cultivated in Uniform Conditions. Molecules 2021, 26, 2826. [Google Scholar] [CrossRef]
- Oriola, A.O.; Oyedeji, A.O. Essential Oils and Their Compounds as Potential Anti-Influenza Agents. Molecules 2022, 27, 7797. [Google Scholar] [CrossRef]
- Wu, S.; Patel, K.B.; Booth, L.J.; Metcalf, J.P.; Lin, H.K.; Wu, W. Protective essential oil attenuates influenza virus infection: An in vitro study in MDCK cells. BMC Complement. Altern. Med. 2010, 10, 69. [Google Scholar] [CrossRef]
- Mao, X.; Gu, S.; Sang, H.; Ye, Y.; Li, J.; Teng, Y.; Zhang, F.; Ma, Q.; Jiang, P.; Yang, Z.; et al. Essential Oil-Rich Chinese Formula Luofushan-Baicao Oil Inhibits the Infection of Influenza A Virus through the Regulation of NF-kappaB P65 and IRF3 Activation. Evid. Based Complement. Altern. Med. 2021, 2021, 5547424. [Google Scholar] [CrossRef]
- Astani, A.; Reichling, J.; Schnitzler, P. Comparative study on the antiviral activity of selected monoterpenes derived from essential oils. Phytotherapy Research. Phytother Res. 2010, 24, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Schnitzler, P. Essential oils for the treatment of herpes simplex virus infections. Chemotherapy 2019, 64, 1–7. [Google Scholar] [CrossRef]
- Rouf, R.; Uddin, S.J.; Sarker, D.K.; Islam, M.T.; Ali, E.S.; Shilpi, J.A.; Nahar, L.; Tiralongo, E.; Sarker, S.D. Antiviral potential of garlic (Allium sativum) and its organosulfur compounds: A systematic update of pre-clinical and clinical data. Trends Food Sci. Technol. 2020, 104, 219–234. [Google Scholar] [CrossRef]
- Mirskaya, E.; Agranovski, I.E. Control of airborne microorganisms by essential oils released by VaxiPod. Atmosphere 2021, 12, 1418. [Google Scholar] [CrossRef]
- Jackwood, M.; Rosenbloom, R.; Petteruti, M.; Hilt, D.; McCall, A.; Williams, S. Avian coronavirus infectious bronchitis virus susceptibility to botanical oleoresins and essential oils in vitro and in vivo. Virus Res. 2010, 149, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.; Khan, M.A.; Ullah, N.; Nadhman, A. Therapeutic potential of medicinal plants against COVID-19: The role of antiviral medicinal metabolites. Biocatal. Agric. Biotechnol. 2021, 31, 101890. [Google Scholar] [CrossRef]
- Petrova, D.; Gasic, U.; Yocheva, L.; Hinkov, A.; Yordanova, Z.; Chaneva, G.; Mantovska, D.; Paunov, M.; Ivanova, L.; Rogova, M.; et al. Catmint (Nepeta nuda L.) Phylogenetics and Metabolic Responses in Variable Growth Conditions. Front. Plant Sci. 2022, 13, 866777. [Google Scholar] [CrossRef] [PubMed]
- Hinkov, A.; Angelova, P.; Marchev, A.; Hodzhev, Y.; Tsvetkov, Y.; Dragolova, D.; Todorov, D.; Shishkova, K.; Kapchina-Toteva, V.; Blundell, R.; et al. Nepeta nuda ssp. nuda L. water extract: Inhibition of replication of some strains of human alpha herpes virus (genus simplex virus) in vitro, mode of action and NMR-based metabolomics. J. Herb. Med. 2020, 21, 100334. [Google Scholar] [CrossRef]
- Greig, A.; Bouillant, A. Binding effects of concanavalin A on a coronavirus. Can. J. Comp. Med. 1977, 41, 122. [Google Scholar]
- Schlegel, A.; Schaller, J.; Jentsch, P.; Kempf, C. Semliki Forest virus core protein fragmentation: Its possible role in nucleocapsid disassembly. Biosci. Rep. 1993, 13, 333–347. [Google Scholar] [CrossRef]
- Amini, A.; Masoumi-Moghaddam, S.; Morris, D.L. Utility of Bromelain and N-Acetylcysteine in Treatment of Peritoneal Dissemination of Gastrointestinal Mucin-Producing Malignancies; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Akhter, J.; Quéromès, G.; Pillai, K.; Kepenekian, V.; Badar, S.; Mekkawy, A.H.; Frobert, E.; Valle, S.J.; Morris, D.L. The Combination of Bromelain and Acetylcysteine (BromAc) Synergistically Inactivates SARS-CoV-2. Viruses 2021, 13, 425. [Google Scholar] [CrossRef]
- Mayo, D.R.; Beckwith, W.H., 3rd. Inactivation of West Nile virus during serologic testing and transport. J. Clin. Microbiol. 2002, 40, 3044–3046. [Google Scholar] [CrossRef] [PubMed]
- Webster, R.G.; Darlington, R.W. Disruption of myxoviruses with Tween 20 and isolation of biologically active hemagglutinin and neuraminidase subunits. J. Virol. 1969, 4, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Suschkea, U.; Sporera, F.; Schneelea, J.; Geissb, H.K.; Reichlinga, J. Antibacterial and Cytotoxic Activity of Nepeta cataria L., N. cataria var. citriodora (Beck.) Balb. and Melissa officinalis L. Essential Oils. Nat. Prod. Commun. 2007, 2, 1277–1286. [Google Scholar]
- Borlace, G.N.; Singh, R.; Seubsasana, S.; Chantaranothai, P.; Thongkham, E.; Aiemsaard, J. Antimicrobial effects of catnip (Nepeta cataria L.) essential oil against canine skin infection pathogens. Vet. World 2024, 17, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Sagar, S.; Rathinavel, A.K.; Lutz, W.E.; Struble, L.R.; Khurana, S.; Schnaubelt, A.T.; Mishra, N.K.; Guda, C.; Palermo, N.Y.; Broadhurst, M.J.; et al. Bromelain inhibits SARS-CoV-2 infection via targeting ACE-2, TMPRSS2, and spike protein. Clin. Transl. Med. 2021, 11, e281. [Google Scholar] [CrossRef]
- Yasir, M.; Vijay, K.A.; Willcox, M. Antiviral effect of multipurpose contact lens disinfecting solutions against coronavirus. Contact Lens Anterior Eye 2022, 45, 101513. [Google Scholar] [CrossRef]
- Urmi, U.L.; Attard, S.; Vijay, A.K.; Willcox, M.D.; Kumar, N.; Islam, S.; Kuppusamy, R. Antiviral Activity of Anthranilamide Peptidomimetics against Herpes Simplex Virus 1 and a Coronavirus. Antibiotics 2023, 12, 1436. [Google Scholar]
- Lelešius, R.; Karpovaitė, A.; Mickienė, R.; Drevinskas, T.; Tiso, N.; Ragažinskienė, O.; Kubilienė, L.; Maruška, A.; Šalomskas, A. In vitro antiviral activity of fifteen plant extracts against avian infectious bronchitis virus. BMC Vet. Res. 2019, 15, 178. [Google Scholar]
- Jiang, X.; Zhao, C.; Chen, Y.; Gao, X.; Zhang, Q.; Chen, Z.; Li, C.; Zhao, X.; Liu, Z.; Huang, W.; et al. Probable Evidence of Aerosol Transmission of SARS-COV-2 in a COVID-19 Outbreak of a High-Rise Building. Environ. Health Insights 2023, 17, 11786302231188269. [Google Scholar] [CrossRef]
- Jayaweera, M.; Perera, H.; Gunawardana, B.; Manatunge, J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020, 188, 109819. [Google Scholar] [CrossRef] [PubMed]
- Sezer, B. The imminent danger related to measles virus infection from the perspective of paediatric dentistry. Eur. Arch. Paediatr. Dent. 2024, 25, 605–606. [Google Scholar] [PubMed]
- Shan, H.; Yan, L.Y.; Prasanna, N.; Hung, C.K.; Yi, L.J.K.; Ngai, H.F.; Colman, M. Effectiveness of Preprocedural Mouthwashes: A Triple-Blind Randomised Controlled Clinical Trial. Int. Dent. J. 2024, 75, 868–876. [Google Scholar] [CrossRef]
- Munjaković, H.; Mikuletič, T.; Zayed, N.; Kolenc, M.; Manevski, D.; Triglav, T.; Steyer, A.; Teughels, W.; Seme, K.; Fidler, A.; et al. Electrolyzed Saline Prevents Virus Transmission in Dental Procedures: An In Vitro Study. J. Dent. Res. 2025, 104, 211–220. [Google Scholar] [CrossRef]
- Madia, V.N.; Toscanelli, W.; De Vita, D.; De Angelis, M.; Messore, A.; Ialongo, D.; Scipione, L.; Tudino, V.; D’Auria, F.D.; Di Santo, R. Ultrastructural damages to H1N1 influenza virus caused by vapor essential oils. Molecules 2022, 27, 3718. [Google Scholar] [CrossRef]
- Kalaiselvan, P.; Yasir, M.; Kuppusamy, R.; Willcox, M.; Vijay, A.K. Ability of Essential Oil Vapours to Reduce Numbers of Culturable Aerosolised Coronavirus, Bacteria and Fungi. Antibiotics 2022, 11, 393. [Google Scholar] [CrossRef] [PubMed]
- Asif, M.; Saleem, M.; Saadullah, M.; Yaseen, H.S.; Al Zarzour, R. COVID-19 and therapy with essential oils having antiviral, anti-inflammatory, and immunomodulatory properties. Inflammopharmacology 2020, 28, 1153–1161. [Google Scholar]
- Graves, C.; Ghaltakhchyan, N.; Ngo, T.Q.; Liu, C.; Babikow, E.; Shoji, A.; Bocklage, C.; Sang, Y.; Phillips, S.T.; Bowman, N.; et al. A Cetylpyridinium Chloride Oral Rinse Reduces Salivary Viral Load in Randomized Controlled Trials. JDR Clin. Trans. Res. 2024. [Google Scholar] [CrossRef]
- Said-Al Ahl, H.; Naguib, N.Y.; Hussein, M.S. Evaluation growth and essential oil content of catmint and lemon catnip plants as new cultivated medicinal plants in Egypt. Ann. Agric. Sci. 2018, 63, 201–205. [Google Scholar] [CrossRef]
- Zomorodian, K.; Saharkhiz, M.J.; Shariati, S.; Pakshir, K.; Rahimi, M.J.; Khashei, R. Chemical Composition and Antimicrobial Activities of Essential Oils from Nepeta cataria L. against Common Causes of Food-Borne Infections. ISRN Pharm. 2012, 2012, 591953. [Google Scholar] [CrossRef]
- Kansakar, U.; Trimarco, V.; Manzi, M.V.; Cervi, E.; Mone, P.; Santulli, G. Exploring the Therapeutic Potential of Bromelain: Applications, Benefits, and Mechanisms. Nutrients 2024, 16, 2060. [Google Scholar] [CrossRef]
- Wang, W.; Suguitan Jr, A.L.; Zengel, J.; Chen, Z.; Jin, H. Generation of recombinant pandemic H1N1 influenza virus with the HA cleavable by bromelain and identification of the residues influencing HA bromelain cleavage. Vaccine 2012, 30, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Hua, T.; Zhang, X.; Tang, B.; Chang, C.; Liu, G.; Feng, L.; Yu, Y.; Zhang, D.; Hou, J. Tween-20 transiently changes the surface morphology of PK-15 cells and improves PCV2 infection. BMC Vet. Res. 2018, 14, 138. [Google Scholar] [CrossRef]
- Pyankov, O.V.; Usachev, E.V.; Pyankova, O.; Agranovski, I.E. Inactivation of Airborne Influenza Virus by Tea Tree and Eucalyptus Oils. Aerosol Sci. Technol. 2012, 46, 1295–1302. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Blachere, F.M.; Thewlis, R.E.; Vishnu, A.; Davis, K.A.; Cao, G.; Palmer, J.E.; Clark, K.E.; Fisher, M.A.; Khakoo, R. Measurements of airborne influenza virus in aerosol particles from human coughs. PLoS ONE 2010, 5, e15100. [Google Scholar]
- Alford, R.H.; Kasel, J.A.; Gerone, P.J.; Knight, V. Human influenza resulting from aerosol inhalation. Proc. Soc. Exp. Biol. Med. 1966, 122, 800–804. [Google Scholar] [CrossRef]
- Tang, J.W.; Wilson, P.; Shetty, N.; Noakes, C.J. Aerosol-Transmitted Infections-a New Consideration for Public Health and Infection Control Teams. Curr. Treat. Options Infect. Dis. 2015, 7, 176–201. [Google Scholar] [CrossRef]
- Malmgren, R.; Välimaa, H.; Oksanen, L.; Sanmark, E.; Nikuri, P.; Heikkilä, P.; Hakala, J.; Ahola, A.; Yli-Urpo, S.; Palomäki, V.; et al. High-volume evacuation mitigates viral aerosol spread in dental procedures. Sci. Rep. 2023, 13, 18984. [Google Scholar] [CrossRef]
- Firquet, S.; Beaujard, S.; Lobert, P.-E.; Sané, F.; Caloone, D.; Izard, D.; Hober, D. Survival of enveloped and non-enveloped viruses on inanimate surfaces. Microbes Environ. 2015, 30, 140–144. [Google Scholar]

| Disinfectants | Number of Aerosolised Viruses Log10 (PFU/mL) | Water Control/ Number of Aerosolised Viruses Log10 (PFU/mL) | Reduction of Viruses (Log10) | p Values |
|---|---|---|---|---|
| HCO + Bromelain + NAC + Tween 20 (1) | 2.33 ± 0.14 | 5.33 ± 0.14 | 3.00 ± 0.14 | 0.002 |
| NHCO + Bromelain + NAC + Tween 20 (2) | 2.00 ± 0.28 | 4.34 ± 0.13 | 2.34 ± 0.24 | 0.025 |
| HCO + NAC + Tween 20 (3) | 2.60 ± 1.14 | 4.17 ± 0.14 | 1.57 ± 0.14 | 0.008 |
| Bromelain + NAC + Tween 20 (4) | 3.33 ± 0.14 | 4.33 ± 0.14 | 1.00 ± 0.14 | 0.046 |
| NAC + Tween 20 (5) | 4.33 ± 0.28 | 4.33 ± 0.13 | 0.00 ± 0.00 | 0.966 |
| Disinfectants | Number of Aerosolised Viruses Log10 (PFU/mL) | Water Control/ Number of Aerosolised Viruses Log10 (PFU/mL) | Reduction of Viruses (Log10) | p Values |
|---|---|---|---|---|
| HCO + Bromelain + NAC + Tween 20 (1) | 0.00 ± 0.00 | 3.10 ± 0.04 | 3.10 ± 0.04 | <0.001 |
| HCO + NAC + Tween 20 (3) | 1.80 ± 0.42 | 1.30 ± 0.04 | 0.057 | |
| Bromelain + NAC + Tween 20 (4) | 2.03 ± 0.05 | 1.07 ± 0.02 | 0.013 | |
| NAC + Tween 20 (5) | 2.94 ± 0.05 | 0.16 ± 0.03 | 0.910 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yasir, M.; Willcox, M.D.P.; Ings, J.; Bruinessen, P.v. Control of Aerosolised Type A Influenza Virus H1N1 and a Coronavirus with Vapours Containing Catmint Essential Oil. Hygiene 2025, 5, 15. https://doi.org/10.3390/hygiene5020015
Yasir M, Willcox MDP, Ings J, Bruinessen Pv. Control of Aerosolised Type A Influenza Virus H1N1 and a Coronavirus with Vapours Containing Catmint Essential Oil. Hygiene. 2025; 5(2):15. https://doi.org/10.3390/hygiene5020015
Chicago/Turabian StyleYasir, Muhammad, Mark D. P. Willcox, John Ings, and Peter van Bruinessen. 2025. "Control of Aerosolised Type A Influenza Virus H1N1 and a Coronavirus with Vapours Containing Catmint Essential Oil" Hygiene 5, no. 2: 15. https://doi.org/10.3390/hygiene5020015
APA StyleYasir, M., Willcox, M. D. P., Ings, J., & Bruinessen, P. v. (2025). Control of Aerosolised Type A Influenza Virus H1N1 and a Coronavirus with Vapours Containing Catmint Essential Oil. Hygiene, 5(2), 15. https://doi.org/10.3390/hygiene5020015








