Oral Hygiene and Cardiovascular Health
Abstract
1. Introduction
2. Epidemiology of Oral Hygiene and Cardiovascular Disease
3. Biological Connections Between Gum Disease, Systemic Inflammation, and Cardiovascular Health
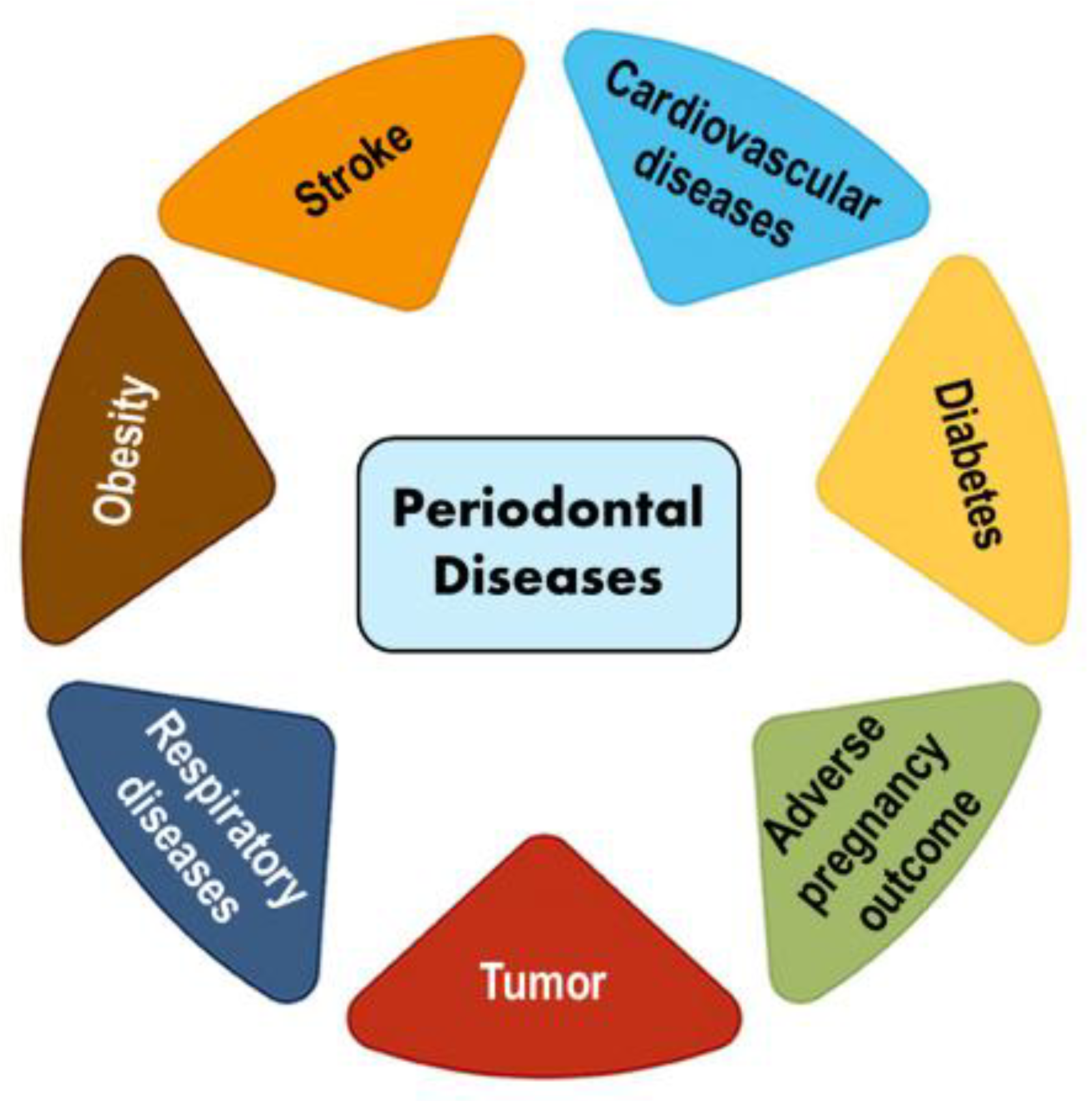
4. Association of Oral Hygiene with CVD
5. Risk Factors Linking Periodontal Disease and Cardiovascular Health
6. Public Health Strategies
7. Prevention Strategies and Clinical Implications
8. Limitations and Future Research
9. Discussion
10. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Verma, D.; Garg, P.K.; Dubey, A.K. Insights into the human oral microbiome. Arch. Microbiol. 2018, 200, 525–540. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Minty, M.; Vinel, A.; Canceill, T.; Loubières, P.; Burcelin, R.; Kaddech, M.; Blasco-Baque, V.; Laurencin-Dalicieux, S. Oral Microbiota: A Major Player in the Diagnosis of Systemic Diseases. Diagnostics 2021, 11, 1376. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, P.D.; Tsigalou, C.; Valsamaki, P.N.; Konstantinidis, T.G.; Voidarou, C.; Bezirtzoglou, E. The Emerging Role of the Gut Microbiome in Cardiovascular Disease: Current Knowledge and Perspectives. Biomedicines 2022, 10, 948. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pisano, M.; Giordano, F.; Sangiovanni, G.; Capuano, N.; Acerra, A.; D’Ambrosio, F. The Interaction between the Oral Microbiome and Systemic Diseases: A Narrative Review. Microbiol. Res. 2023, 14, 1862–1878. [Google Scholar] [CrossRef]
- Nascimento, M.M. The Oral Microbiome, in Oral Bacteria—An Overview; Science Direct; Academic Press: Cambridge, MA, USA, 2019; Available online: https://www.sciencedirect.com/topics/medicine-and-dentistry/oral-bacteria#:~:text=The%20Oral%20Environment,by%20other%20bacteria%20%5B23%5D (accessed on 18 October 2024).
- Sharma, S.; Mohler, J.; Mahajan, S.D.; Schwartz, S.A.; Bruggemann, L.; Aalinkeel, R. Microbial Biofilm: A Review on Formation, Infection, Antibiotic Resistance, Control Measures, and Innovative Treatment. Microorganisms 2023, 11, 1614. [Google Scholar] [CrossRef]
- Rajasekaran, J.J.; Krishnamurthy, H.K.; Bosco, J.; Jayaraman, V.; Krishna, K.; Wang, T.; Bei, K. Oral Microbiome: A Review of Its Impact on Oral and Systemic Health. Microorganisms 2024, 12, 1797. [Google Scholar] [CrossRef]
- Li, Y.; Zhu, M.; Liu, Y.; Luo, B.; Cui, J.; Huang, L.; Chen, K.; Liu, Y. The oral microbiota and cardiometabolic health: A comprehensive review and emerging insights. Front. Immunol. 2022, 13, 1010368. [Google Scholar] [CrossRef]
- Siddiqui, R.; Badran, Z.; Boghossian, A.; Alharbi, A.M.; Alfahemi, H.; Khan, N.A. The Increasing Importance of the Oral Microbiome in Periodontal Health and Disease. Future Sci. OA 2023, 9, FSO856. Available online: https://www.tandfonline.com/doi/epdf/10.2144/fsoa-2023-0062?needAccess=true (accessed on 18 October 2024). [CrossRef]
- Slocum, C.; Kramer, C.; Genco, C.A. Immune dysregulation mediated by the oral microbiome: A potential link to chronic inflammation and atherosclerosis. J. Intern. Med. 2016, 280, 114–128. [Google Scholar] [CrossRef]
- Song, B.; Bie, Y.; Feng, H.; Xie, B.; Liu, M.; Zhao, F. Inflammatory Factors Driving Atherosclerotic Plaque Progression New Insights. J. Transl. Int. Med. 2022, 10, 36–47. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Blum, A.; Kryuger, K.; Eizenberg, M.M.; Tatour, S.; Vigder, F.; Laster, Z.; Front, E. Periodontal care may improve endothelial function. Eur. J. Int. Med. 2007, 18, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Gasner, N.S.; Schure, R.S. Periodontal Disease; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554590/ (accessed on 18 October 2024).
- Kozak, M.; Pawlik, A. The Role of the Oral Microbiome in the Development of Diseases. Int. J. Mol. Sci. 2023, 24, 5231. [Google Scholar] [CrossRef] [PubMed]
- Care Quest. The Relationship Between Oral Health and Heart Disease; Care Quest: Boston, MA, USA, 2023; Available online: https://www.carequest.org/about/blog-post/relationship-between-oral-health-and-heart-disease (accessed on 18 December 2024).
- Tonetti, M.S.; Van Dyke, T.E. Periodontitis and atherosclerotic cardiovascular disease: Consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Periodontol. 2013, 84 (Suppl. S4), S24–S29. [Google Scholar] [CrossRef] [PubMed]
- Desvarieux, M.; Demmer, R.T.; Jacobs, D.R.; Rundek, T.; Boden-Albala, B.; Sacco, R.L.; Papapanou, P.N. Periodontal bacteria and hypertension: The oral infections and vascular disease epidemiology study. J. Hypertens. 2010, 28, 1413–1421. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; del Castillo, A.M.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef] [PubMed]
- Mathews, M.J.; Mathews, E.H.; Mathews, G.E. Oral health and coronary heart disease. BMC Oral Health 2016, 16, 122. [Google Scholar] [CrossRef] [PubMed]
- Rydén, L.; Buhlin, K.; Ekstrand, E.; de Faire, U.; Gustafsson, A.; Holmer, J. Periodontitis Increases the Risk of a First Myocardial Infarction: A Report From the PAROKRANK Study. Circulation 2016, 133, 576–583. [Google Scholar] [CrossRef]
- Zardawi, F.; Gul, S.; Abdulkareem, A.; Sha, A.; Yates, J. Association Between Periodontal Disease and Atherosclerotic Cardiovascular Diseases: Revisited. Front. Cardiovasc. Med. 2021, 15, 625579. [Google Scholar] [CrossRef] [PubMed]
- NIH. Oral Hygiene; National Institute of Dental and Craniofacial Research: Bethesda, Maryland, 2024. Available online: https://www.nidcr.nih.gov/health-info/oral-hygiene#:~:text=Clean%20Between%20Your%20Teeth,particles%2C%20from%20between%20your%20teeth. (accessed on 20 October 2024).
- Kalburgi, V.; Sravya, L.; Warad, S.; Vijayalaxmi, K.; Sejal, P.; Hazeil, D. Role of systemic markers in periodontal diseases: A possible inflammatory burden and risk factor for cardiovascular diseases? Ann. Med. Health Sci. Res. 2014, 4, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Medina-Leyte, D.J.; Zepeda-García, O.; Domínguez-Pérez, M.; González-Garrido, A.; Villarreal-Molina, T.; Jacobo-Albavera, L. Endothelial dysfunction, inflammation and coronary artery disease: Potential biomarkers and promising therapeutical approaches. Int. J. Mol. Sci. 2021, 22, 3850. [Google Scholar] [CrossRef]
- Sen, S.; Giamberardino, L.D.; Moss, K.; Morelli, T.; Rosamond, W.D.; Gottesman, R.F.; Beck, J.; Offenbacher, S. Periodontal Disease, Regular Dental Care Use, and Incident Ischemic Stroke. Stroke 2018, 49, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Science News. Hidden Tooth Infections May Predispose People to Heart Disease; Science News: Washington, DC, USA, 2016; Available online: https://www.sciencedaily.com/releases/2016/08/160802104159.htm (accessed on 19 October 2024).
- Patel, A.B.; Sanghvi, K.; Shelly, S.; Patel, V. Association of low socioeconomic status and limited dental health-care access on poor oral health outcomes among United States adults. SRM J. Res. Dent. Sci. 2019, 10, 183–186. [Google Scholar]
- Northridge, M.E.; Kumar, A.; Kaur, R. Disparities in Access to Oral Health Care. Annu. Rev. Public Health 2020, 41, 513–535. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Watt, R.G.; Tsakos, G.; de Oliveira, C.; Hamer, M. Tooth loss and cardiovascular disease mortality risk--results from the Scottish Health Survey. PLoS ONE 2012, 7, e30797. [Google Scholar] [CrossRef] [PubMed Central]
- Febbraio, M.; Roy, C.B.; Levin, L. Is There a Causal Link Between Periodontitis and Cardiovascular Disease? A Concise Review of Recent Findings. Int. Dent. J. 2022, 72, 37–51. [Google Scholar] [CrossRef] [PubMed Central]
- CDC. About Periodontal (Gum) Disease; Center for Disease Control: Atlanta, GA, USA, 2024. Available online: https://www.cdc.gov/oral-health/about/gum-periodontal-disease.html (accessed on 20 October 2024).
- NYC Periodontics. 2024, Understanding Gingivitis; NYC Periodontics & Implant Dentistry: New York, NY, USA, 2024; Available online: https://implant-periodontist-nyc.com/gum-disease-vs-gingivitis-understanding-the-stages/ (accessed on 20 October 2024).
- Potempa, J.; Gomis-Ruth, F.X.; Karim, A.Y. Handbook of Proteolytic Enzymes, 3rd ed.; Elsevier Ltd.: Amsterdam, The Netherlands, 2013; ISBN 978-0-12-382219-2. [Google Scholar] [CrossRef]
- Bravo-Lopez, M.; Villa-Islas, V.; Arriaga, C.R.; Villaseñor-Altamirano, A.B.; Guzmán-Solís, A.; Sandoval-Velasco, M.; Wesp, J.K.; Alcantara, K.; López-Corral, A.; Gómez-Valdés, J.; et al. Paleogenomic insights into the red complex bacteria Tannerella forsythia in Pre-Hispanic and Colonial individuals from Mexico. Phil. Trans. R. Soc. B 2020, 375, 20190580. [Google Scholar] [CrossRef]
- Kurtzman, G.M.; Horowitz, R.A.; Johnson, R.; Prestiano, R.A.; Klein, B.I. The systemic oral health connection: Biofilms. Medicine 2022, 18, e30517. [Google Scholar] [CrossRef]
- Leishman, S.J.; Do, H.L.; Ford, P.J. Cardiovascular disease and the role of oral bacteria. J. Oral Microbiol. 2010, 21, 2. [Google Scholar] [CrossRef]
- Mohammad, S.; Thiemermann, C. Role of Metabolic Endotoxemiain Systemic Inflammation and Potential Interventions. Front. Immunol. 2021, 11, 594150. [Google Scholar] [CrossRef]
- Wang, P.L.; Ohura, K. Porphyromonas gingivalis lipopolysaccharide signaling in gingival fibroblasts-CD14 and Toll-like receptors. Crit. Rev. Oral Biol. Med. 2002, 13, 132–142. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, C.; Zhang, X.; Chen, H.; Dong, J.; Lu, W.; Song, Z.; Zhou, W. Porphyromonas gingivalis lipopolysaccharide induces cognitive dysfunction, mediated by neuronal inflammation via activation of the TLR4 signaling pathway in C57BL/6 mice. J. Neuroinflamm. 2018, 15, 37. [Google Scholar] [CrossRef] [PubMed]
- Martínez-García, M.; Hernández-Lemus, E. Periodontal Inflammation and Systemic Diseases: An Overview. Front. Physiol. 2021, 27, 709438. [Google Scholar] [CrossRef] [PubMed Central]
- Neurath, N.; Kesting, M. Cytokines in gingivitis and periodontitis: From pathogenesis to therapeutic targets. Front. Immunol. 2024, 15, 1435054. [Google Scholar] [CrossRef] [PubMed]
- Badimon, L.; Padró, T.; Vilahur, G. Atherosclerosis, platelets and thrombosis in acute ischaemic heart disease. Eur. Heart J. Acute Cardiovasc. Care 2012, 1, 60–74. [Google Scholar] [CrossRef] [PubMed]
- Kong, P.; Cui, Z.; Huang, X.; Zhang, D.; Guo, R.; Han, M. Inflammation and atherosclerosis: Signaling pathways and therapeutic intervention. Signal Transduct. Target. Ther. 2022, 7, 131. [Google Scholar] [CrossRef]
- Sun, H.J.; Wu, Z.Y.; Nie, X.W.; Bian, J.S. Role of Endothelial Dysfunction in Cardiovascular Diseases: The Link Between Inflammation and Hydrogen Sulfide. Front. Pharmacol. 2020, 10, 1568. [Google Scholar] [CrossRef] [PubMed]
- Mussbacher, M.; Schossleitner, K.; Kral-Pointner, J.B.; Salzmann, M.; Schrammel, A.; Schmid, J.A. More than Just a Monolayer: The Multifaceted Role of Endothelial Cells in the Pathophysiology of Atherosclerosis. Curr. Atheroscler. Rep. 2022, 24, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.W. Endothelial adhesion molecules and their role in inflammation. Can. J. Physiol. Pharmacol. 1993, 71, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Xie, M.; Lu, X.; Mei, F.; Song, W.; Liu, Y.; Chen, L. The Roles of Periodontal Bacteria in Atherosclerosis. Int. J. Mol. Sci. 2023, 24, 12861. [Google Scholar] [CrossRef]
- Bansal, T.; Pandey, A.; Asthana, A.K. C-Reactive Protein (CRP) and its Association with Periodontal Disease: A Brief Review. J. Clin. Diagn. Res. 2014, 8, ZE21–ZE24. [Google Scholar] [CrossRef] [PubMed]
- Bian, F.; Yang, X.; Zhou, F.; Wu, P.; Xing, S.; Xu, G.; Li, W.; Chi, J.; Ouyang, C.; Zhang, Y.; et al. C-reactive protein promotes atherosclerosis by increasing LDL transcytosis across endothelial cells. Br. J. Pharmacol. 2014, 171, 2671–2684. [Google Scholar] [CrossRef] [PubMed]
- Czerniuk, M.R.; Surma, S.; Romańczyk, M.; Nowak, J.M.; Wojtowicz, A.; Filipiak, K.J. Unexpected Relationships: Periodontal Diseases: Atherosclerosis-Plaque Destabilization? From the Teeth to a Coronary Event. Biology 2022, 11, 272. [Google Scholar] [CrossRef] [PubMed]
- Del Giudice, C.; Vaia, E.; Liccardo, D.; Marzano, F.; Valletta, A.; Spagnuolo, G.; Rengo, G. Infective endocarditis: A focus on oral microbiota. Microorganisms 2021, 9, 1218. [Google Scholar] [CrossRef]
- Lockhart, P.B.; Brennan, M.T.; Thornhill, M.; Michalowicz, B.S.; Noll, J.; Bahrani-Mougeot, F.K.; Sasser, H.C. Poor oral hygiene as a risk factor for infective endocarditis–related bacteremia. J. Am. Dent. Assoc. 2009, 140, 1238–1244. [Google Scholar]
- Bumm, C.V.; Folwaczny, M. Infective endocarditis and oral health—A Narrative Review. Cardiovas Diagn. Ther. 2021, 11, 1403. [Google Scholar]
- Lockhart, P.B.; Chu, V.; Zhao, J.; Gohs, F.; Thornhill, M.H.; Pihlstrom, B.; O’Gara, P.T. Oral hygiene and infective endocarditis: A case control study. Oral Pathol. Oral Radiol. 2023, 136, 333–342. [Google Scholar]
- Pink, C.; Holtfreter, B.; Völzke, H.; Nauck, M.; Dörr, M.; Kocher, T. Periodontitis and systemic inflammation as independent and interacting risk factors for mortality: Evidence from a prospective cohort study. BMC Med. 2023, 21, 430. [Google Scholar] [CrossRef]
- CDC. Smoking, Gum Disease, and Tooth Loss; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2024. Available online: https://www.cdc.gov/tobacco/campaign/tips/diseases/periodontal-gum-disease.html (accessed on 24 October 2024).
- CDC. About Heart Disease; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2024. Available online: https://www.cdc.gov/heart-disease/about/index.html (accessed on 20 October 2024).
- NLM. U.S. Coronary Heart Disease; National Library of Medicine: Bethesda, MD, USA, 2024. Available online: https://medlineplus.gov/ency/article/007115.htm (accessed on 24 November 2024).
- AAP. Gum Disease and Other Diseases; American Academy of Periodontology: Chicago, IL, USA, 2024; Available online: https://www.perio.org/for-patients/gum-disease-information/gum-disease-and-other-diseases/#:~:text=People%20with%20diabetes%20are%20more,the%20risk%20for%20diabetic%20complications (accessed on 24 November 2024).
- Ye, J.; Li, L.; Wang, M.; Ma, Q.; Tian, Y.; Zhang, Q.; Liu, J.; Li, B.; Zhang, B.; Liu, H.; et al. Diabetes Mellitus Promotes the Development of Atherosclerosis: The Role of NLRP3. Front. Immunol. 2022, 13, 900254. [Google Scholar] [CrossRef]
- Ceriello, A.; Prattichizzo, F. Variability of Risk Factors and Diabetes Complications. Cardiovasc. Diabetol. 2021, 20, 101. [Google Scholar] [CrossRef]
- Liccardo, D.; Cannavo, A.; Spagnuolo, G.; Ferrara, N.; Cittadini, A.; Rengo, C.; Rengo, G. Periodontal Disease: A Risk Factor for Diabetes and Cardiovascular Disease. Int. J. Mol. Sci. 2019, 20, 1414. [Google Scholar] [CrossRef]
- Aizenbud, I.; Wilensky, A.; Almoznino, G. Periodontal Disease and Its Association with Metabolic Syndrome-A Comprehensive Review. Int. J. Mol. Sci. 2023, 24, 13011. [Google Scholar] [CrossRef] [PubMed]
- DQA. Measuring Oral Healthcare Quality for Older Adults; Dental Quality Alliance: Chicago, IL, USA, 2021; Available online: https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/dqa/educational-resources/measuring_oral_healthcare_quality_in_older_adults_report.pdf (accessed on 24 November 2024).
- Nazir, M.A. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int. J. Health Sci. 2017, 11, 72–80. [Google Scholar]
- Sanghvi, M.; Ramírez, J.; Chadalavada, S.; Augn, N.; Munroe, P.B.; Donos, N.; Peterson, S.E. The Association Between Periodontal Disease and Cardiovascular Disease: Insights From Imaging, Observational, and Genetic Data. JACC Adv. 2024, 3, 101241. [Google Scholar] [CrossRef]
- Borrell, L.N.; Crawford, N.D. Socioeconomic position indicators and periodontitis: Examining the evidence. Periodontology 2012, 58, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Mannoh, I.; Hussien, M.; Commodore-Mensah, Y.; Michos, E.D. Impact of social determinants of health on cardiovascular disease prevention. Curr. Opin. Cardiol. 2021, 36, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Cao, Y.; Miao, C.; Liu, W.; Dong, L.; Lv, Z.; Iheozor-Ejiofor, Z.; Li, C. Periodontal therapy for primary or secondary prevention of cardiovascular disease in people with periodontitis. Cochrane Database Syst. Rev. 2022, 10, CD009197. [Google Scholar] [CrossRef]
- NIH. 2021 National Healthcare Quality and Disparities Report [Internet]; Disparities in Healthcare; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK578532/ (accessed on 25 November 2024).
- ADA. Nutrition and Oral Health; American Dental Association: Chicago, IL, USA, 2023; Available online: https://www.ada.org/resources/ada-library/oral-health-topics/nutrition-and-oral-health (accessed on 25 November 2024).
- WHO. Sugars and Dental Caries; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries#:~:text=Limiting%20free%20sugars%20intake%20to,absenteeism%20at%20school%20or%20work (accessed on 25 November 2024).
- Moynihan, P. Sugars and Dental Caries: Evidence for Setting a Recommended Threshold for Intake. Adv. Nutr. 2016, 7, 149–156. [Google Scholar] [CrossRef] [PubMed]
- UIC. The Best Foods for A Healthy Smile and Whole Body; University of Illinois: Chicago, IL, USA, 2018; Available online: https://dentistry.uic.edu/news-stories/the-best-foods-for-a-healthy-smile-and-whole-body/#:~:text=Nuts%20are%20full%20of%20health,vitamin%20B6%2C%20potassium%20and%20zinc (accessed on 26 November 2024).
- Uwitonze, A.M.; Ojeh, N.; Murererehe, J.; Atfi, A.; Razzaque, M.S. Zinc Adequacy Is Essential for the Maintenance of Optimal Oral Health. Nutrients 2020, 12, 949. [Google Scholar] [CrossRef] [PubMed]
- Badrasawi, M.M.H.; Hijjeh, N.H.; Amer, R.S.; Allan, R.M.; Altamimi, M. Nutrition Awareness and Oral Health among Dental Patients in Palestine: A Cross-Sectional Study. Int. J. Dent. 2020, 2020, 3472753. [Google Scholar] [CrossRef] [PubMed]
- Favero, V.; Bacci, C.; Volpato, A.; Bandiera, M.; Favero, L.; Zanette, G. Pregnancy, and Dentistry: A Literature Review on Risk Management during Dental Surgical Procedures. Dent. J. 2021, 9, 46. [Google Scholar] [CrossRef]
- Uriza, C.L.; Arregoces, F.E.; Porras, J.V.; Camargo, M.B.; Morales, A.R. Ultra-Sensitive C-Reactive Protein (US-CRP) in Patients With Periodontal Disease and Risk of Acute Myocardial Infarction. Cardiol. Res. 2011, 2, 27–35. [Google Scholar] [CrossRef] [PubMed][Green Version]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaman, M.S.; Alam, S.M.G.; Razzaque, M.S. Oral Hygiene and Cardiovascular Health. Hygiene 2025, 5, 14. https://doi.org/10.3390/hygiene5020014
Zaman MS, Alam SMG, Razzaque MS. Oral Hygiene and Cardiovascular Health. Hygiene. 2025; 5(2):14. https://doi.org/10.3390/hygiene5020014
Chicago/Turabian StyleZaman, Md S., S. M. Golam Alam, and Mohammed S. Razzaque. 2025. "Oral Hygiene and Cardiovascular Health" Hygiene 5, no. 2: 14. https://doi.org/10.3390/hygiene5020014
APA StyleZaman, M. S., Alam, S. M. G., & Razzaque, M. S. (2025). Oral Hygiene and Cardiovascular Health. Hygiene, 5(2), 14. https://doi.org/10.3390/hygiene5020014




