Abstract
Handwashing with soap is a fundamental practice for preventing communicable diseases, particularly in resource-constrained settings like Nepal, where various factors influence maternal handwashing behaviours. A systematic search encompassing PubMed/Medline, Embase, PsycINFO, CINAHL and grey literature source was conducted. Extracted eligible articles underwent descriptive analysis and their quality assessment was carried out following STROBE guidelines. From the initial screening of 187 database articles and 18 from grey literature, a total of 120 full text articles and records were retrieved to evaluated for inclusion in the review, identifying nine articles meeting the inclusion criteria for the review. Maternal handwashing with soap frequencies varied during critical moments ranging from 6% to 100%, and a 47% availability of soap and water at the household level was reported. Factors influencing handwashing included education, wealth, ecology, and participation in health promotion campaigns. Barriers included knowledge gaps, contrary beliefs, unavailability of soap and water, financial constraints, maternal demotivation, and low participation in decision-making. Limitations include study design heterogeneity (cross-sectional, Randomized Controlled Trials-RCT, Cohort), sample size variability, and geographical bias, potentially limiting generalizability of this study, limited reporting on soap and water availability for mothers at the household level is noted, and temporal variability introduces study inconsistency. Availability of soap, water, and effective health education is crucial for promoting sustained handwashing practices. Community-based interventions involving mothers in decision making and policy initiatives are essential for overcoming barriers and promote behavioural change to improve public health outcomes. This paper aims to determine the rates of handwashing with soap among mothers in Nepalese households and explore the factors associated with the uptake of handwashing.
1. Introduction
Handwashing with soap is a practical, cheap, feasible, and straightforward way to prevent and control communicable diseases, especially in low-resource settings like Nepal [1,2,3]. It is a significant component of the prevention and control of skin infections, acute respiratory infections, and diarrhoea among children under five years [1,4,5,6]. This has been apparent at the global level with the campaigns related to COVID-19 transmission about prevention through handwashing with soap [7,8,9]. The COVID-19 pandemic has shown that hand washing with soap helps lower the risk of infection [10,11]. Reducing exposure to pathogens is a global health priority [12]; demonstrates, via the Sustainable Development Goals 6 (SDGs 2016–2030), that priority has been given to achieving universal access to all aspects of water, sanitation and hygiene (WASH) by 2030 [13,14].
Handwashing at the household level is determined by a several factors, such as knowledge of the importance of handwashing, risk communication, availability of water and soap, family ownership of soap, water and a fixed place for handwashing, installation of tippy taps (a hands-free way to wash hands—especially appropriate for water scarce rural areas—which is operated by a foot lever and may increase the rate of handwashing with soap), perceived cost, and an individuals’ busy schedule and tiredness [15,16,17,18,19,20]. Household handwashing in Nepal is also influenced by context-specific handwashing policies, strategies and guidelines, as well as geographical and environmental factors [21,22,23]. Handwashing within households as a standard practice is still not widespread throughout the country. Despite these facilitators and challenges, handwashing remains a key method of reducing communicable diseases rates [4,24].
In Nepal, mothers are primarily caregivers for their children. They teach children at home about handwashing with soap, and managing handwashing facilities with family members support [25,26]. Handwashing with soap promotion campaigns have a positive impact on children’s health [27]. Handwashing with soap practice provides children with safe and clean home environments [28]. Family members, such as the husband, father-in-law, and mother-in-law, can handwash with soap by buying soap, managing water and providing fixed places for handwashing. In this discourse, mothers are important persons, as they can be role models in the household.
The five key critical moments recommended to wash hands are: before eating or preparing food; before breastfeeding and feeding children; after defaecating or using the toilet; after cleaning a child faeces or handling nappies; and after touching a source of contamination [1]. In Nepal, the overall handwashing knowledge of mothers was 60% in 2014 [29]. The rate of handwashing with soap by mothers before handling food was 67% after a three-month awareness program in Kavre district, while the baseline survey rate of handwashing with soap was only 5% in 2015 [30]. A study conducted in Rolpa district showed the self-reported prevalence of handwashing was 8% at baseline, 96% after a handwashing intervention, and 77% at follow-up, 30 months after the intervention [31]. However, the rates of handwashing with soap before preparing food, before feeding children or breastfeeding, and after cleaning children’s bottoms was between 6% and 22% in Nepal [29]. The application of existing knowledge regarding handwashing, especially before child feeding and breastfeeding and after the disposal of child faeces, is a challenge and barrier to good hygiene practices. With such varying rates of handwashing with soap during critical moments, it is essential to examine this issue in Nepal. This paper aims to determine the rates of handwashing with soap among mothers in Nepalese households and explore the factors associated with the uptake of handwashing.
2. Methods
2.1. Search Strategy and Criteria Selection
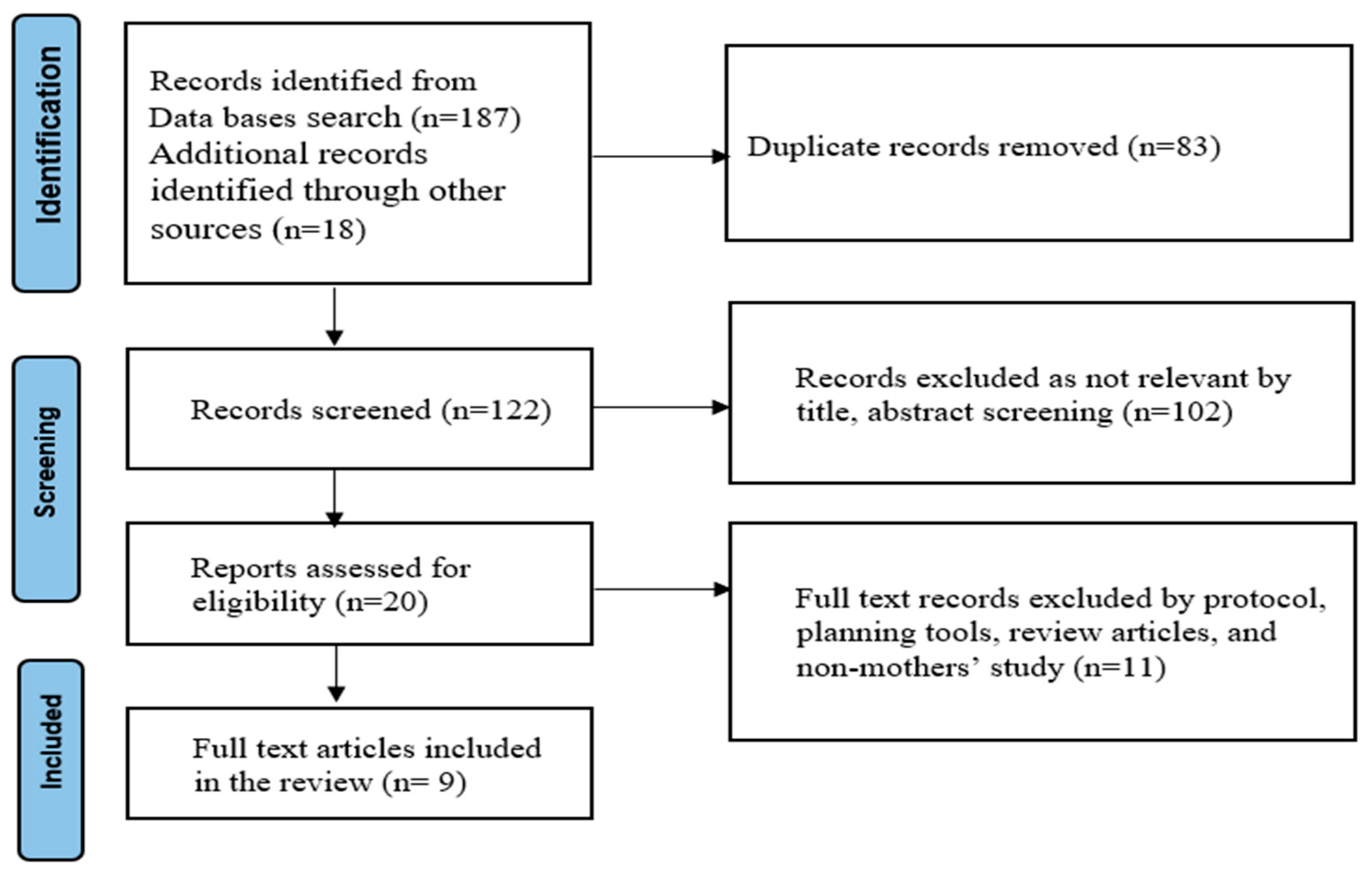
This systematic review adopted the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist (http://www.prisma-statement.org/PRISMAStatement/, accessed on 30 October 2023) [32]. The protocol was registered in PROSPERO (CRD42021158009). Published literature was searched in the following databases: PubMed/Medline, Embase, PsycINFO, and Cumulative Index to Nursing & Allied Health Literature (CINAHL). A manual search for articles was also conducted in Google Scholar. The grey literature (e.g., government reports, project reports, working papers, technical reports, and unpublished theses) was searched using keywords that were the same as those used to search the peer-reviewed literature. Relevant papers were also hand-searched. Articles were included if (i) the study was conducted in Nepal, (ii) information was collected from mothers, and (iii) the study was published in English. No limits were placed on the dates of data collection or publication. Articles were excluded if they were, non-mother samples, protocol papers, systematic reviews, abstracts only, or editorials. The search was completed in October 2023. The details of the screening of articles are in the PRISMA flow chart (Figure 1).
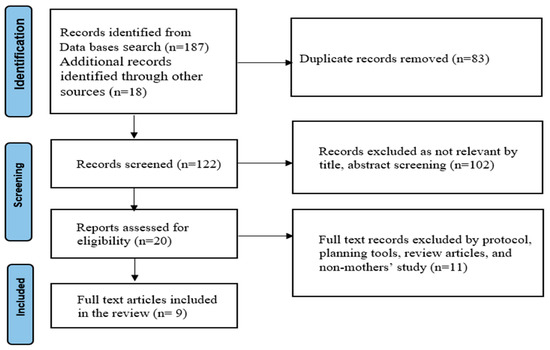
Figure 1.
PRISMA flow diagram.
2.2. Data Extraction, Analysis and Quality Assessment
All eligible articles and records were extracted and recorded in an Excel spreadsheet. Extracted information included author, year of publication, study design, participants, age group, study place, study periods, and outcome measures.
Descriptive analysis was performed for this review paper. Two reviewers (SRD and TB) finalised the list of articles and records that would be included. Meta-analysis was impossible due to the low number of studies identified and the heterogeneity of the outcome measures. A quality assessment was done using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [33]. All required fields of the guidelines were completed by the first reviewer (SRD), and cross-verification was performed by the second reviewer (TB). Once the extraction of eligible studies was completed, a narrative synthesis was made to provide evidence about handwashing with soap by mothers. The characteristics recorded for all eligible articles comprised of first author’s name, publication year, study design, study population, sample size, study periods, and key findings.
3. Results
3.1. Study Flow and Characteristics of Included Studies
Initially, 187 articles were identified from the database search, and 18 records through the grey literature search. Of the total 205 records, 83 were excluded because of duplication. The remaining 122 were screened, and further records (n = 102) were excluded due to exclusion criteria of irrelevant titles or abstracts. A total of 20 records were assessed for eligibility. Then, 11 full text articles and records were excluded by protocol, planning tools, review articles, and non-mothers studies. Finally, nine full-text articles met all inclusion criteria (Figure 1). Of the nine studies found, three studies described randomized controlled trials (RCT), conducted in Kavre, Kathmandu, and Chitwan, Makwanpur, and Nuwakot districts. Five studies were cross sectional, conducted in a rural and urban settings. One study described a cohort study, conducted in Sarlahi district.
3.2. Rates of Household Handwashing with Soap by Mothers in Nepal
Maternal rates of handwashing with soap varied during different critical moments in the eligible studies. The rate of handwashing is normally called percentage of household mothers who washed their hands where denominator is the total number of households mothers included in the study. In 2023, Dhital et al. conducted a cross sectional study using Nepal Demographic and Health Survey (NDHS) 2016 found the availability of soap and water was 47% [34]. Two municipalities Shankarapur and Tandi in Chitwan were 28% and 34%, respectively [35]. A cross-sectional study conducted by Kafle and Pradhan in Makwanpur district among 178 mothers in 2018 reported that approximately 43% of mothers washed their hands with soap at critical moment [36]. Gautam et al. conducted a RCT between October 2012 and December 2013 using structured observations of handwashing with soap among 239 mothers with children aged 6–59 months in Kavre showed that handwashing with soap before eating and feeding a child was 67% after a food hygiene campaign, which was significantly higher than the 5% who undertook handwashing with soap before eating or feeding a child at baseline [30]. Langford and Panter–Brick conducted a RCT in the slum area of Kathmandu in 2013. They reported that the handwashing with soap rates were 100% after using the toilet and after cleaning children’s bottoms, 71% before cooking food, 62% before child feeding, and 60% before eating in the handwashing intervention arms of the study; while the results for the control arms were 91% after using the toilet, 84% after cleaning children’s bottoms, 19% before child feeding, 2.3% before cooking and zero percent before eating [37]. An observational prospective cohort study carried out in 2008 in Sarlahi district showed that mothers’ handwashing with soap prior to handling infants was only 15% [27]. Likewise, another retrospective cross-sectional study conducted in the Makwanpur district among 5411 mothers aged 15–49 years who had live births in the previous year in 2002 showed that approximately 50% of the birth attendants washed their hands prior to attending the deliveries [38]. These results indicated that handwashing with soap rates had a wide variation depending on the areas, circumstances, education, and critical time point being assessed, with the majority of results showing far less than optimal rates of handwashing with soap across the country. The key summary result of this review on household rates of handwashing with soap by mothers is presented in Table 1, while Table 2 outlines the factors associated with the uptake of handwashing.

Table 1.
Rates of handwashing by household mothers.

Table 2.
Factors associated with the uptake of handwashing.
3.3. Factors Associated with Maternal Handwashing in Nepal
The key factors associated with handwashing with soap and water are education, wealth and ecology [34]. A cross-sectional study carried out among randomly selected mothers from 178 households in Makwanpur district in 2018 found maternal knowledge and the household wealth index affect handwashing with soap practices [36]. In 2017, Kandel et al. conducted a cross sectional study using the 2014 Multiple Indicator Cluster Survey (MICS) dataset among 1421 households’ mothers and reported that the faecal contamination of water was associated with the availability of adequate handwashing facilities with soap and water [39]. As mentioned above, an RCT carried out in a rural village in Kavre district in 2015 found mothers’ participation in Health Mothers’ Group meetings, and motivation through family support and rewards are enabling factors for handwashing with soap, while poor participation, demotivation, and punishment decrease handwashing with soap [30]. This study further found that an integrated health promotion campaign increased the rate of handwashing with soap. Miller et al. conducted a RCT in Chitwan, Nawalparasi, and Nuwakot districts reported that women who attained higher-level of education had more frequent use of soap during handwashing compared with women with no education in 2017 and the participatory community development program was an effective way of increasing hygiene practices [40].
A study carried out in Kathmandu in 2013 showed that family and community beliefs, such as believing handwashing with soap is unnecessary, being unsure about good health after using soap, and the financial burden of buying soap, are barriers to effective handwashing with soap [37]. This study found that community strongly believed that keeping children clean all the time causes illness, and some infectious diseases are caused by cold weather, fever, and evil spirits, not due to poor handwashing practices. A strong misconception that handwashing with soap may not be necessary to prevent diseases can have adverse health effects on the people, especially the vulnerable populations such as children, pregnant mothers and the elderly. A further barrier to handwashing with soap is that household members need to spend money on food, which takes priority over soap. A cohort study carried out in 2008 in the plain region in Sarlahi district of Nepal indicated that the possible factors associated with maternal handwashing were a lack of education, absence of a toilet at home, and having low-birthweight babies [27]. A study conducted by Osrin and colleagues in the Makwanpur district among 4511 mothers in 2002 found a lack of knowledge about the importance of handwashing and hygiene, especially during breastfeeding and birth attendance, which is a possible factor affecting effective handwashing in Nepal [38].
4. Discussion
This paper aims to determine the rates of handwashing with soap among mothers in Nepalese households and explore the factors associated with the uptake of handwashing. Nepalese mothers typically take the primary caring role for children and family members, including household cleaning. These roles are traditionally established and socially constructed in Nepal. Although handwashing is a shared responsibility, mothers often experience feel more pressure to ensure safe hygiene for their children [41]. These caregiving roles are not recognized as work with the home in Nepal [42].
The first and foremost issue for a general family education on handwashing is improving maternal handwashing knowledge. The NDHS 2016 results showed that handwashing facilities with soap and water at the household level was 47%, whereas the MICS 2014 found that mothers’ handwashing with soap knowledge varied depending on the specific critical moment being observed. For example, after cleaning children’s bottoms or changing nappies, handwashing rates of 6% were found compared to before meal, when 92% washed their hands with soap [29,43]. The NDHS 2022 results showed that the availability of basic handwashing facilities with soap and water at household level was 72%, reflecting a 25% increase from the baseline data of NDHS 2016 [44] This surge could be attributed to the global COVID-19 pandemic, fostering a habitual practice of handwashing.
This review determined that maternal knowledge about the importance of handwashing with soap before eating or child feeding was higher after food hygiene intervention; [30] compared to after cleaning a child who has defaecated; [37] and this is one of Nepal’s significant public health challenges [29]. Similarly, less than half of the mothers washed their hands with soap who attended childbirth [38]. The low rates of handwashing by mothers may be attributed to a lack of health knowledge about the threat and severity of not washing hands, unavailability of soap and water, financial crisis, and the cultural belief that communicable diseases (for example diarrhoea) exist because of colds, fever, or evil spirits, rather than lack of handwashing [37]. In Nepal, mothers who are poor and those in rural and hard-to-reach areas remain most vulnerable to communicable diseases, due to inadequate access to health education and handwashing services [29]. The gap between handwashing knowledge and access to handwashing facilities with soap and water is a further challenge in Nepal [36].
This review highlighted those key factors and barriers to handwashing with soap include a lack of knowledge, contrary beliefs, unavailability of soap and water, financial constraints, maternal demotivation, and low mother’s participation in household decision-making. Maternal knowledge is associated with handwashing practices [45]. Availability of soap, clean water, fixed places for handwashing, adequate time, and family and community support positively influence handwashing by mothers [19,46]. Health education by trained health care providers in overcoming barriers, reinforcing the importance of handwashing at critical moments. Mothers as key role models, shape household handwashing situations. This statement is supported by a previous study carried out in Korea in 2013, which argued that providing health education improved handwashing [47]. The results of this review indicate that factors affecting handwashing were similar to a 2015 Nepal-specific study of four various plains districts (Mahottari, Siraha, Saptari and Sarlahi), which showed that participating mothers were more likely to wash their hands with soap when their hands looked dirty, to have their hands soft and smelling good, and to keep their dignity [48]. Challenges include providing high-quality education to increase health literacy and fostering habits of utilizing available resources. Other determinants include family roles, household structure, geography, and climate [31].
Effectively improving handwashing practices hinges on the challenging task of changing community mindsets, though this is complex and hindered by economic growth challenges and societal inequalities. This review highlights the need for health promotion campaigns, the production of context-specific handwashing materials, and timely, high-quality health education sessions on handwashing. The policy, guidelines and strategies documents are needed. Simple, affordable, and practical local interventions should consider cultural, social, economic, and geographical factors [49]. Community-based health promotion actions are recommended, involving advocacy, services delivery, and policy approaches [50,51]. This review suggests future research priorities, including multivariate and multi-level analyses on handwashing and sanitation facilities in Nepal. It advocates for participant observation studies and emphasizes the importance of health education, human resources and high-quality handwashing facilities.
The limitations of this review are acknowledged. Firstly, there is heterogeneity in study designs (cross-sectional, RCT and Cohort), posing challenges for the direct comparisons. Secondly, not all household-level handwashing rates and facilities were covered. Thirdly, none of the included studies reported the availability of soap and water at the household level for mothers in Nepal. Fourthly, information about corrective measures for effectively improving handwashing knowledge and behavioural change through community efforts was lacking. Finally, this review shows a variability of sample size and geographical bias with a focus on Nepal-specific studies, potentially limiting the generalizability of findings beyond the Nepalese context.
5. Conclusions
Addressing variations in handwashing practice among household mothers requires a comprehensive approach, considering education, economic status, geography and cultural influences. Challenges like knowledge gaps and limited soap and water underscore the need for fostering consistent handwashing habits. The lack of a specific handwashing policy and strategy in Nepal poses a challenge, emphasizing the potential benefits of adopting available handwashing guidelines, thereby benefitting from their implementation. This review highlights the crucial role of ensuring an adequate supply of soap and water, along with designated handwashing places and effective health education, to improve handwashing practices. Achieving this requires tailored community development and health promotion programs in Nepal.
Author Contributions
S.R.D. conceptualized, coded data, extracted findings of articles, prepared the manuscript and reviewed it. T.B. provided input for reviewed this manuscript. D.L. and C.C. contributed through academic and scientific feedback and suggestions with necessary modification. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval was waived for this study as it constitutes a literature review.
Data Availability Statement
Data extracted from the original articles supporting the results can be provided upon request from the corresponding author.
Acknowledgments
We would like to thank Ryan O’Neill from the University of Newcastle, Australia for providing a language editorial review.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
MICS: Multiple Indicator Cluster Survey; PRISMA: Preferred Reporting Items for Systematic reviews and Meta-Analysis; RCT: Randomized Controlled Trails; STROBE: Strengthening the Reporting of Observational Studies in Epidemiology; SDGs: Sustainable Development Goals; WASH: Water, Sanitation and Hygiene.
References
- Curtis, V.; Cairncross, S. Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infect. Dis. 2003, 3, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Curtis, V.A.; Danquah, L.O.; Aunger, R.V. Planned, motivated and habitual hygiene behaviour: An eleven-country review. Health Educ. Res. 2009, 24, 655–673. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Loughnan, L.; Luyendijk, R.; Hernandez, O.; Weinger, M.; Arnold, F.; Ram, P.K. Handwashing in 51 countries: Analysis of proxy measures of handwashing behavior in multiple indicator cluster surveys and demographic and health surveys, 2010–2013. Am. J. Trop. Med. Hyg. 2017, 97, 447. [Google Scholar] [CrossRef] [PubMed]
- Aiello, A.E.; Coulborn, R.M.; Perez, V.; Larson, E.L. Effect of hand hygiene on infectious disease risk in the community setting: A meta-analysis. Am. J. Public Health 2008, 98, 1372–1381. [Google Scholar] [CrossRef] [PubMed]
- Luby, S.P.; Agboatwalla, M.; Feikin, D.R.; Painter, J.; Billhimer, W.; Altaf, A.; Hoekstra, R.M. Effect of handwashing on child health: A randomised controlled trial. Lancet 2005, 366, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Ross, I.; Bick, S.; Ayieko, P.; Dreibelbis, R.; Wolf, J.; Freeman, M.C.; Allen, E.; Brauer, M.; Cumming, O. Effectiveness of handwashing with soap for preventing acute respiratory infections in low-income and middle-income countries: A systematic review and meta-analysis. Lancet 2023, 401, 1681–1690. [Google Scholar] [CrossRef]
- Brauer, M.; Zhao, J.T.; Bennitt, F.B.; Stanaway, J.D. Global access to handwashing: Implications for COVID-19 control in low-income countries. Environ. Health Perspect. 2020, 128, 057005. [Google Scholar] [CrossRef]
- Hannah, D.M.; Lynch, I.; Mao, F.; Miller, J.D.; Young, S.L.; Krause, S. Water and sanitation for all in a pandemic. Nat. Sustain. 2020, 3, 773–775. [Google Scholar] [CrossRef]
- Amegah, A.K. Improving handwashing habits and household air quality in Africa after COVID-19. Lancet Glob. Health 2020, 8, e1110–e1111. [Google Scholar] [CrossRef]
- Beale, S.; Johnson, A.M.; Zambon, M.; Flu Watch Group; Hayward, A.C.; Fragaszy, E.B. Hand hygiene practices and the risk of human coronavirus infections in a UK community cohort. Wellcome Open Res. 2021, 5, 98. [Google Scholar] [CrossRef]
- Horga, N.G.; Cirnatu, D.; Kundnani, N.R.; Ciurariu, E.; Parvu, S.; Ignea, A.L.; Borza, C.; Sharma, A.; Morariu, S. Evaluation of non-pharmacological measures implemented in the management of the COVID-19 pandemic in Romania. Healthcare 2022, 10, 1756. [Google Scholar] [CrossRef] [PubMed]
- Biran, A.; Rabie, T.; Schmidt, W.; Juvekar, S.; Hirve, S.; Curtis, V. Comparing the performance of indicators of hand-washing practices in rural Indian households. Trop. Med. Int. Health 2008, 13, 278–285. [Google Scholar] [CrossRef] [PubMed]
- National Planning Commission. Sustainable Development Goals, Status and Roadmap 2016–2030; Government of Nepal, National Planning Commission: Kathmandu, Nepal, 2015.
- Hutton, G.; Chase, C. The knowledge base for achieving the sustainable development goal targets on water supply, sanitation and hygiene. Int. J. Environ. Res. Public Health 2016, 13, 536. [Google Scholar] [CrossRef] [PubMed]
- Aunger, R.; Schmidt, W.P.; Ranpura, A.; Coombes, Y.; Maina, P.M.; Matiko, C.N.; Curtis, V. Three kinds of psychological determinants for hand-washing behaviour in Kenya. Soc. Sci. Med. 2010, 70, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, W.P.; Aunger, R.; Coombes, Y.; Maina, P.M.; Matiko, C.N.; Biran, A.; Curtis, V. Determinants of handwashing practices in Kenya: The role of media exposure, poverty and infrastructure. Trop. Med. Int. Health 2009, 14, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Seward, N.; Prost, A.; Copas, A.; Corbin, M.; Li, L.; Colbourn, T.; Osrin, D.; Neuman, M.; Azad, K.; Kuddus, A.; et al. Using observational data to estimate the effect of hand washing and clean delivery kit use by birth attendants on maternal deaths after home deliveries in rural Bangladesh, India and Nepal. PLoS ONE 2015, 10, e0136152. [Google Scholar] [CrossRef]
- Langford, R.; Lunn, P.; Brick, C.P. Hand-washing, subclinical infections, and growth: A longitudinal evaluation of an intervention in Nepali slums. Am. J. Hum. Biol. 2011, 23, 621–629. [Google Scholar] [CrossRef]
- Rabbi, S.E.; Dey, N.C. Exploring the gap between hand washing knowledge and practices in Bangladesh: A cross-sectional comparative study. BMC Public Health 2013, 13, 1–7. [Google Scholar] [CrossRef]
- Zhang, C.; Mosa, A.J.; Hayward, A.S.; Matthews, S.A. Promoting clean hands among children in Uganda: A school-based intervention using ‘tippy-taps’. Public Health 2013, 127, 586. [Google Scholar] [CrossRef]
- Gammon, J.; Hunt, J. The neglected element of hand hygiene-significance of hand drying, efficiency of different methods and clinical implication: A review. J. Infect. Prev. 2019, 20, 66–74. [Google Scholar] [CrossRef]
- Budhathoki, C.B. Water supply, sanitation and hygiene situation in Nepal: A review. J. Health Promot. 2019, 7, 65–76. [Google Scholar] [CrossRef]
- White, S.; Thorseth, A.H.; Dreibelbis, R.; Curtis, V. The determinants of handwashing behaviour in domestic settings: An integrative systematic review. Int. J. Hyg. Environ. Health 2020, 227, 113512. [Google Scholar] [CrossRef] [PubMed]
- Luby, S.P.; Agboatwalla, M.; Painter, J.; Altaf, A.; Billhimer, W.L.; Hoekstra, R.M. Effect of intensive handwashing promotion on childhood diarrhea in high-risk communities in Pakistan: A randomized controlled trial. JAMA 2004, 291, 2547–2554. [Google Scholar] [CrossRef] [PubMed]
- Freiburger, M.A. Mothers as Children’s “First and Best Teachers”: An Institutional Ethnography. Ph.D. Dissertation, University of Kansas, Lawrence, KS, USA, 2010. [Google Scholar]
- Lam, W.; Fowler, C.; Dawson, A. The approaches Hong Kong Chinese mothers adopt to teach their preschool children to prevent influenza: A multiple case study at household level. BMC Nurs. 2016, 15, 51. [Google Scholar] [CrossRef] [PubMed]
- Rhee, V.; Mullany, L.C.; Khatry, S.K.; Katz, J.; LeClerq, S.C.; Darmstadt, G.L.; Tielsch, J.M. Maternal and birth attendant hand washing and neonatal mortality in southern Nepal. Arch. Pediatr. Adolesc. Med. 2008, 162, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Mitlin, D. Equity and gender. In Pathfinder Report; Sanitation and Hygiene Applied Research for Equity (SHARE); Water Aid/Macro Betti: India, 2011; Available online: https://www.susana.org/en/community/partners/list/details/1561# (accessed on 30 October 2023).
- Central Bureau of Statistics. Nepal Multiple Indicator Cluster Survey (MICS) 2014, Final Report; National Planning Commission, Central Bureau Statistics (CBS), UNICEF: Kathmandu, Nepal, 2014.
- Gautam, O.P.; Schmidt, W.P.; Cairncross, S.; Cavill, S.; Curtis, V. Trial of a novel intervention to improve multiple food hygiene behaviors in Nepal. Am. J. Trop. Med. Hyg. 2017, 96, 1415. [Google Scholar] [CrossRef]
- McMichael, C.; Robinson, P. Drivers of sustained hygiene behaviour change: A case study from mid-western Nepal. Soc. Sci. Med. 2016, 163, 28–36. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- Dhital, S.R.; Chojenta, C.; Evans, T.J.; Acharya, T.D.; Loxton, D. Prevalence and Correlates of Water, Sanitation, and Hygiene (WASH) and Spatial Distribution of Unimproved WASH in Nepal. Int. J. Environ. Res. Public Health 2022, 19, 3507. [Google Scholar] [CrossRef]
- Sekh, N.; Shekh, R.; Kaphle, K.; Ansari, I.A. Handwashing Habits before Pandemic COVID-19 in the Chitwan District of Nepal and Implication for COVID-19 Control. Open J. Soc. Sci. 2022, 10, 471–478. [Google Scholar] [CrossRef]
- Kafle, S.; Pradhan, B. Situation of water, sanitation and hygiene and diarrhoeal disease after open defecation free declaration and associated factors of Makwanpur District, Nepal. J. Nepal Health Res. Counc. 2018, 16, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Langford, R.; Panter-Brick, C. A health equity critique of social marketing: Where interventions have impact but insufficient reach. Soc. Sci. Med. 2013, 83, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Osrin, D.; Tumbahangphe, K.M.; Shrestha, D.; Mesko, N.; Shrestha, B.P.; Manandhar, M.K.; Standing, H.; Manandhar, D.S.; Anthony, M.D. Cross sectional, community-based study of care of newborn infants in Nepal. BMJ 2002, 325, 1063. [Google Scholar] [CrossRef] [PubMed]
- Kandel, P.; Kunwar, R.; Lamichhane, P.; Karki, S. Extent of fecal contamination of household drinking water in Nepal: Further analysis of Nepal Multiple Indicator Cluster Survey 2014. Am. J. Trop. Med. Hyg. 2017, 96, 446. [Google Scholar] [CrossRef][Green Version]
- Miller, L.C.; Joshi, N.; Lohani, M.; Rogers, B.; Mahato, S.; Ghosh, S.; Webb, P. Women’s education level amplifies the effects of a livelihoods-based intervention on household wealth, child diet, and child growth in rural Nepal. Int. J. Equity Health 2017, 16, 183. [Google Scholar] [CrossRef] [PubMed]
- Aihara, Y.; Shrestha, S.; Sharma, J. Household water insecurity, depression and quality of life among postnatal women living in urban Nepal. J. Water Health 2016, 14, 317–324. [Google Scholar] [CrossRef]
- McCarthy Ribbens, J.; Edwards, R. Key Concepts in Family Studies; Sage: London, UK, 2011. [Google Scholar]
- Ministry of Health and Population. Nepal Demographic and Health Survey; MOHP, New Era and Inner City Fund International: Kathmandu, Nepal, 2016.
- Ministry of Health and Population. Nepal Demographic and Health Survey; MOHP, New Era and Inner City Fund International: Kathmandu, Nepal, 2022.
- Suen, L.K.; Rana, T. Knowledge level and hand hygiene practice of Nepalese immigrants and their host country population: A comparative study. Int. J. Environ. Res. Public Health 2020, 17, 4019. [Google Scholar] [CrossRef]
- Rajbhandari, A.K.; Sagtani, R.A.; Baral, K.P. Hand hygiene compliance among rural healthcare workers of Nepal. J. Patan Acad. Health Sci. 2018, 5, 90–95. [Google Scholar] [CrossRef]
- Song, I.H.; Kim, S.A.; Park, W.S. Family factors associated with children’s handwashing hygiene behavior. J. Child Health Care 2013, 17, 164–173. [Google Scholar] [CrossRef]
- Nguyen, N.K.; Gurung, H. Barriers and Facilitators to Hygienic Use and Maintenance of Latrines and Handwashing with Soap in Sarlahi, Mahottari, Siraha and Saptari Districts of the Terai, Nepal; Formative Research WASH Nepal, Netherland: SNV Smart Development Work; 2015; pp. 1–50. Available online: https://sanitationlearninghub.org/resource/barriers-and-facilitators-to-hygienic-use-and-maintenance-of-latrines-and-handwashing-with-soap-in-sarlahi-mahottari-siraha-and-saptari-districts-of-the-terai-nepal/ (accessed on 30 October 2023).
- Ghimire, M.; Pradhan, Y.V.; Maskey, M.K. Community-based interventions for diarrhoeal diseases and acute respiratory infections in Nepal. Bull. World Health Organ. 2010, 88, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Green, L.W. Health Program Planning: An Educational and Ecological Approach, 4th ed.; McGraw Hill: New York, NY, USA, 2005. [Google Scholar]
- Koirala Dhital, M.; Dhital, S.R.; Kc, B.B.; Owens, V.; Khadka, H.R.; Gyawali, P. Successful health promotion, its challenges and the way forward in Nepal. Glob. Health Promot. 2023, 30, 68–71. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).