Successful Disinfection of a New Healthcare Facility Contaminated with Pseudomonas aeruginosa
Abstract
:1. Introduction
2. Materials and Methods
2.1. Diagnostic and Identification of Areas at Bacterial Risk
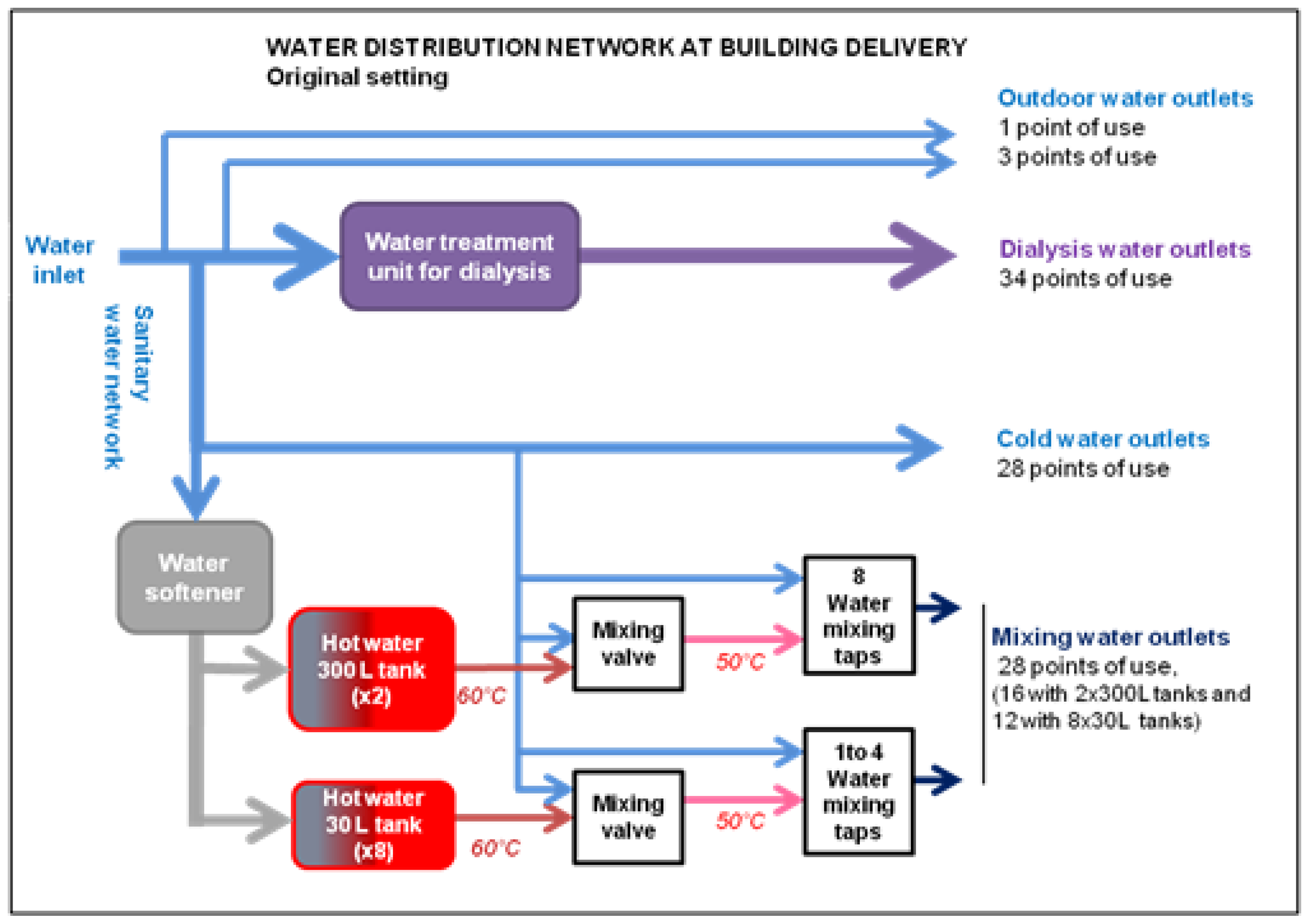
2.1.1. Inspection and Evaluation of the Water Distribution System
2.1.2. Bacterial Charge Quantification by ATPmetry
2.1.3. Water Sampling
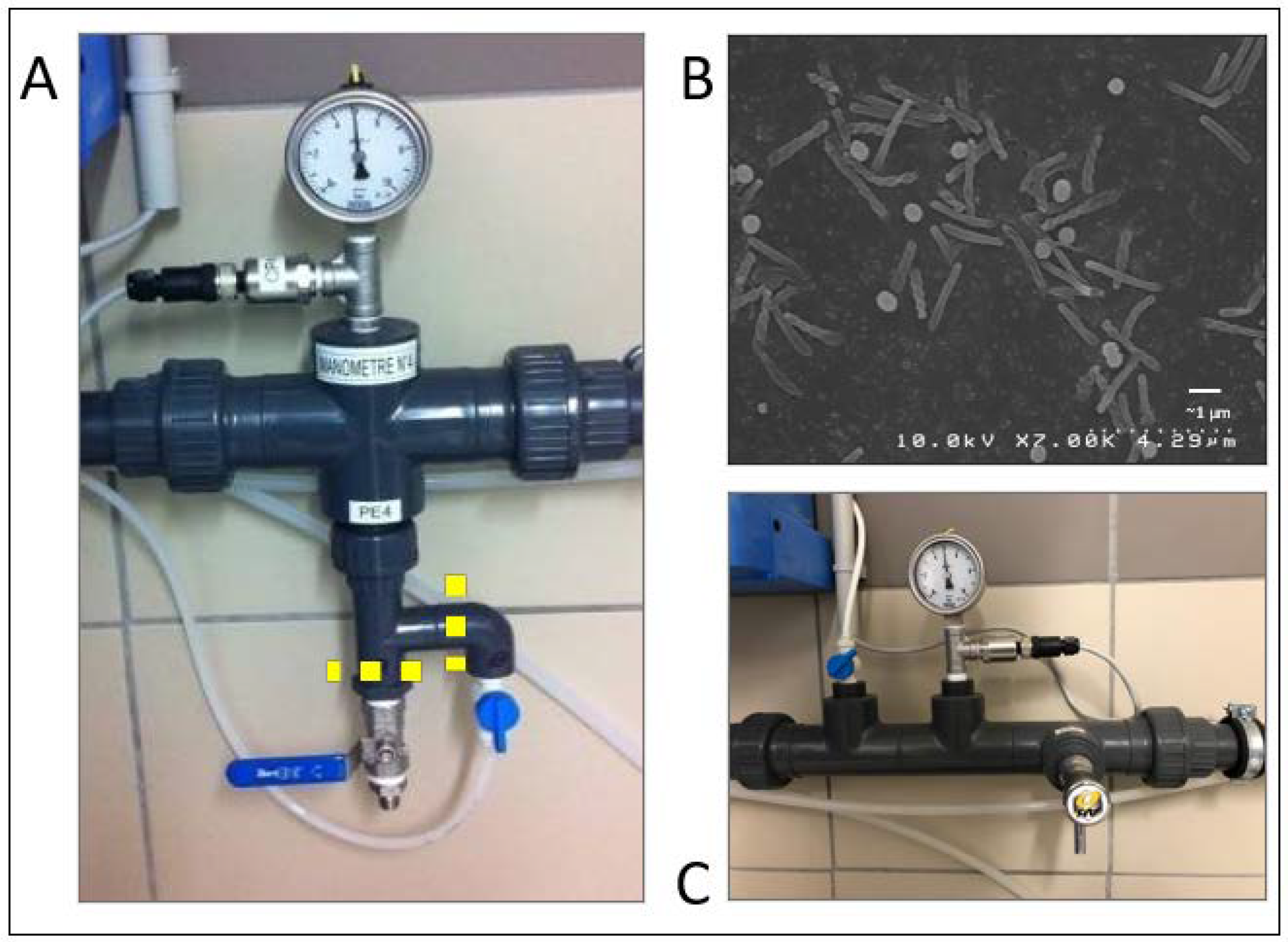
2.1.4. Demonstration of P. aeruginosa Contamination in Specific Segments of the Water Distribution System
2.2. Corrective Measures
2.3. Disinfection
2.3.1. Analysis of Previous Disinfection Procedures
2.3.2. Proposed Disinfection Procedure
2.4. Maintenance Measures
3. Results
3.1. Diagnostic and Identification of Areas at Bacterial Risk
3.1.1. Inspection and Evaluation of the Water Distribution System
3.1.2. ATPmetry Results
3.1.3. Water Sampling
3.1.4. Demonstration of P. aeruginosa Contamination in Specific Segments of the Water Distribution System
- Filters of the main pipes
- Automated hand washing taps.
- Water treatment unit for dialysis.
3.2. Corrective Measures in the Water Distribution Network
3.3. Disinfection
3.4. Maintenance and Controls
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Venier, A.-G.; Leroyer, C.; Slekovec, C.; Talon, D.; Bertrand, X.; Parer, S.; Alfandari, S.; Guerin, J.-M.; Megarbane, B.; Lawrence, C.; et al. Risk Factors for Pseudomonas aeruginosa Acquisition in Intensive Care Units: A Prospective Multicentre Study. J. Hosp. Infect. 2014, 88, 103–108. [Google Scholar] [CrossRef]
- Watnick, P.; Kolter, R. Biofilm, City of Microbes. J. Bacteriol. 2000, 182, 2675–2679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wingender, J.; Flemming, H.-C. Biofilms in Drinking Water and Their Role as Reservoir for Pathogens. Int. J. Hyg. Environ. Health 2011, 214, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Lenz, J.; Linke, S.; Gemein, S.; Exner, M.; Gebel, J. Verification of the Efficiency of Chemical Disinfection and Sanitation Measures in In-Building Distribution Systems. Int. J. Hyg. Environ. Health 2010, 213, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Schwering, M.; Song, J.; Louie, M.; Turner, R.J.; Ceri, H. Multi-Species Biofilms Defined from Drinking Water Microorganisms Provide Increased Protection against Chlorine Disinfection. Biofouling 2013, 29, 917–928. [Google Scholar] [CrossRef]
- Loveday, H.P.; Wilson, J.A.; Kerr, K.; Pitchers, R.; Walker, J.T.; Browne, J. Association between Healthcare Water Systems and Pseudomonas aeruginosa Infections: A Rapid Systematic Review. J. Hosp. Infect. 2014, 86, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Trautmann, M.; Bauer, C.; Schumann, C.; Hahn, P.; Höher, M.; Haller, M.; Lepper, P.M. Common RAPD Pattern of Pseudomonas aeruginosa from Patients and Tap Water in a Medical Intensive Care Unit. Int. J. Hyg. Environ. Health 2006, 209, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Kerr, K.G.; Snelling, A.M. Pseudomonas aeruginosa: A Formidable and Ever-Present Adversary. J. Hosp. Infect. 2017, 73, 338–344. [Google Scholar] [CrossRef]
- Regulation and Quality Improvement Authority-RQIA. Inspection Reports|Regulation and Quality Improvement Authority Standards Reports. Available online: https://www.rqia.org.uk/reviews/review-reports/2012-2015/rqia-pseudomonas-review/rqia-independent-review-of-pseudomonas-final-repor/ (accessed on 17 December 2021).
- Walker, J.T.; Jhutty, A.; Parks, S.; Willis, C.; Copley, V.; Turton, J.F.; Hoffman, P.N.; Bennett, A.M. Investigation of Healthcare-Acquired Infections Associated with Pseudomonas aeruginosa Biofilms in Taps in Neonatal Units in Northern Ireland. J. Hosp. Infect. 2014, 86, 16–23. [Google Scholar] [CrossRef]
- Bédard, E.; Prévost, M.; Déziel, E. Pseudomonas aeruginosa in Premise Plumbing of Large Buildings. MicrobiologyOpen 2016, 5, 937–956. [Google Scholar] [CrossRef]
- Lefebvre, A.; Quantin, C.; Vanhems, P.; Lucet, J.-C.; Bertrand, X.; Astruc, K.; Chavanet, P.; Aho-Glélé, L.S. Impact of New Water Systems on Healthcare-Associated Colonization or Infection with Pseudomonas aeruginosa. 2016. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4886352/ (accessed on 15 December 2021).
- Lucena, R.; Boccato, C.; Vienken, J.; Evans, D. Water and Dialysis Fluids: A Quality Management Guide; Patbst Science Publishers: Lengerich, Germany, 2015. [Google Scholar]
- Völker, S.; Schreiber, C.; Kistemann, T. Drinking Water Quality in Household Supply Infrastructure—A Survey of the Current Situation in Germany. Int. J. Hyg. Environ. Health 2010, 213, 204–209. [Google Scholar] [CrossRef]
- Ortolano, G.A.; McAlister, M.B.; Angelbeck, J.A.; Schaffer, J.; Russell, R.L.; Maynard, E.; Wenz, B. Hospital Water Point-of-Use Filtration: A Complementary Strategy to Reduce the Risk of Nosocomial Infection. Am. J. Infect. Control 2005, 33, S1–S19. [Google Scholar] [CrossRef]
- Trautmann, M.; Halder, S.; Hoegel, J.; Royer, H.; Haller, M. Point-of-Use Water Filtration Reduces Endemic Pseudomonas aeruginosa Infections on a Surgical Intensive Care Unit. Am. J. Infect. Control 2008, 36, 421–429. [Google Scholar] [CrossRef]
- Totaro, M.; Valentini, P.; Casini, B.; Miccoli, M.; Costa, A.L.; Baggiani, A. Experimental Comparison of Point-of-Use Filters for Drinking Water Ultrafiltration. J. Hosp. Infect. 2017, 96, 172–176. [Google Scholar] [CrossRef]
- Baranovsky, S.; Jumas-Bilak, E.; Lotthé, A.; Marchandin, H.; Parer, S.; Hicheri, Y.; Romano-Bertrand, S. Tracking the Spread Routes of Opportunistic Premise Plumbing Pathogens in a Haematology Unit with Water Points-of-Use Protected by Antimicrobial Filters. J. Hosp. Infect. 2018, 98, 53–59. [Google Scholar] [CrossRef]
- Garvey, M.I.; Bradley, C.W.; Wilkinson, M.A.C.; Bradley, C.; Holden, E. Engineering Waterborne Pseudomonas aeruginosa out of a Critical Care Unit. Int. J. Hyg. Environ. Health 2017, 220, 1014–1019. [Google Scholar] [CrossRef]
- Qiu, L.; Zhou, Z.; Liu, Q.; Ni, Y.; Zhao, F.; Cheng, H. Investigating the Failure of Repeated Standard Cleaning and Disinfection of a Pseudomonas aeruginosa–Infected Pancreatic and Biliary Endoscope. Am. J. Infect. Control 2015, 43, e43–e46. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.I.; Blumrosen, G.; Vecchio, D.; Golberg, A.; McCormack, M.C.; Yarmush, M.L.; Hamblin, M.R.; Austen, W.G. Eradication of Multidrug-Resistant Pseudomonas Biofilm with Pulsed Electric Fields: Eradication of Multidrug-Resistant Pseudomonas. Biotechnol. Bioeng. 2016, 113, 643–650. [Google Scholar] [CrossRef] [Green Version]
- Ministère Des Solidarités et de La Santé. Qualité de l’eau Dans Les Établissements de Santé. Available online: https://solidarites-sante.gouv.fr/sante-et-environnement/eaux/article/qualite-de-l-eau-dans-les-etablissements-de-sante (accessed on 21 October 2019).
- Safe Water in Healthcare Premises (HTM 04-01). Available online: https://www.gov.uk/government/publications/hot-and-cold-water-supply-storage-and-distribution-systems-for-healthcare-premises (accessed on 5 October 2020).
- Walker, J.; Moore, G. Pseudomonas aeruginosa in Hospital Water Systems: Biofilms, Guidelines, and Practicalities. J. Hosp. Infect. 2015, 89, 324–327. [Google Scholar] [CrossRef]
- Suchomel, M.; Diab-Elschahawi, M.; Kundi, M.; Assadian, O. Influence of Pre- and Post-Usage Flushing Frequencies on Bacterial Water Quality of Non-Touch Water Fittings. BMC Infect. Dis. 2013, 13, 402. [Google Scholar] [CrossRef] [Green Version]
- van der Kooij, D.; Vrouwenvelder, J.S.; Veenendaal, H.R. Elucidation and Control of Biofilm Formation Processes in Water Treatment and Distribution Using the Unified Biofilm Approach. Water Sci. Technol. J. Int. Assoc. Water Pollut. Res. 2003, 47, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Accueil|COFRAC-Comité Français D’accréditation. Available online: https://www.cofrac.fr/ (accessed on 18 February 2020).
- ISO 19458:2006(En), Water Quality—Sampling for Microbiological Analysis. Available online: https://www.iso.org/obp/ui/#iso:std:iso:19458:ed-1:v1:en (accessed on 17 February 2020).
- FD T90-520-Octobre 2005. Available online: https://www.boutique.afnor.org/norme/fd-t90-520/qualite-de-l-eau-guide-technique-de-prelevement-pour-le-suivi-sanitaire-des-eaux-an-application-du-code-de-la-sante-publique/article/678996/fa140129?gclid=CjwKCAjwiOv7BRBREiwAXHbv3HDU-AYhe2SFXGYOo5RBZnzPYV2MJBbjoVzOPZCHqnrwb43XN3ZoQBoCUUoQAvD_BwE (accessed on 5 October 2020).
- ISO 6222:1999(En), Water Quality—Enumeration of Culturable Micro-Organisms—Colony Count by Inoculation in a Nutrient Agar Culture Medium. Available online: https://www.iso.org/obp/ui/#iso:std:iso:6222:ed-2:v1:en:sec:foreword (accessed on 18 February 2020).
- ISO 16266:2006(En), Water Quality—Detection and Enumeration of Pseudomonas aeruginosa—Method by Membrane Filtration. Available online: https://www.iso.org/obp/ui/#iso:std:iso:16266:ed-1:v1:en (accessed on 18 February 2020).
- Product-Types–ECHA. Available online: https://echa.europa.eu/regulations/biocidal-products-regulation/product-types (accessed on 18 February 2020).
- NF EN 1040-Avril 2006. Available online: https://www.boutique.afnor.org/norme/nf-en-1040/antiseptiques-et-desinfectants-chimiques-essai-quantitatif-de-suspension-pour-l-evaluation-de-l-activite-bactericide-de-base-des/article/727990/fa139438 (accessed on 18 February 2020).
- NF EN 1276-Août 2019. Available online: https://www.boutique.afnor.org/norme/nf-en-1276/antiseptiques-et-desinfectants-chimiques-essai-quantitatif-de-suspension-pour-l-evaluation-de-l-activite-bactericide-des-antisep/article/915853/fa189955?lang=13&gclid=Cj0KCQiAs67yBRC7ARIsAF49CdVfFyKUPwmq8N8jhk-jhItTo4v2ob-7DgNSijRZaWdhthLJDIANNKwaAgP9EALw_wcB (accessed on 18 February 2020).
- Réseaux d’eau Destinée à la Consommation Humaine à l’intérieur des Bâtiments: Guide Technique de Maintenance. Désinfection Chimique d’un Réseau EFS et/ou ECS, Centre Scientifique et Technique du Bâtiment. 2005, p. 83. Available online: https://boutique.cstb.fr/reseaux-d-eau-et-assainissement/268-reseaux-deau-destinee-a-la-consommation-humaine-a-linterieur-des-batiments-partie-2-9782868913258.html (accessed on 5 October 2020).
- Falkinham, J.; Pruden, A.; Edwards, M. Opportunistic Premise Plumbing Pathogens: Increasingly Important Pathogens in Drinking Water. Pathogens 2015, 4, 373–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cossali, G.; Routledge, E.J.; Ratcliffe, M.S.; Blakes, H.; Fielder, J.E.; Karayiannis, T.G. Inactivation of E. Coli, Legionella, and Pseudomonas in Tap Water Using Electrochemical Disinfection. J. Environ. Eng. 2016, 142, 04016063. [Google Scholar] [CrossRef]
- Bédard, E.; Laferrière, C.; Déziel, E.; Prévost, M. Impact of Stagnation and Sampling Volume on Water Microbial Quality Monitoring in Large Buildings. PLoS ONE 2018, 13, e0199429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, G.; Stevenson, D.; Thompson, K.-A.; Parks, S.; Ngabo, D.; Bennett, A.M.; Walker, J.T. Biofilm Formation in an Experimental Water Distribution System: The Contamination of Non-Touch Sensor Taps and the Implication for Healthcare. Biofouling 2015, 31, 677–687. [Google Scholar] [CrossRef]
- Centre Scientifique et Technique du Bâtiment; Agence Régionale de la Santé Pays de Loire. Document d’aide à La Conception Des Installations d’eau Sanitaire à l’intérieur Des Bâtiments. Available online: https://www.normandie.ars.sante.fr/system/files/2018-01/conception_reseauxECS.pdf (accessed on 21 October 2019).
- van der Mee-Marquet, N.; Bloc, D.; Briand, L.; Besnier, J.-M.; Quentin, R. Non-Touch Fittings in Hospitals: A Procedure to Eradicate Pseudomonas aeruginosa Contamination. J. Hosp. Infect. 2005, 60, 235–239. [Google Scholar] [CrossRef]



| Feature Type | Features Enhancing Contamination | Correction |
|---|---|---|
| Missing equipment | On the main water supply, there was no possibility of carrying out controlled chemical decontamination. | Installation of connectors to install a volume-controlled mixing pump for chemical disinfection. |
| Network | Outdoor taps were connected to a pipe dedicated to the treatment of water for dialysis. | Separation of the two networks |
| Network | Dead legs | Shorten or remove the dead legs |
| Network | Presence of thermostatic valves mixing hot and cold water, distant from points of use (range: 3–10 m) | Removal of hot and cold water mixing valves located over 3 m from point of use. Mechanical adjustment of maximum allowable temperature (50 °C) on user taps |
| Unfavourable equipment | Large water softener | Removal of the water softener |
| Unfavourable equipment | Thermostatic faucets | Change for simple mixing faucets |
| Unfavourable equipment | Automatic faucets without automatic periodic rinsing | Change for manual faucets |
| Unfavourable equipment | Faucet aerators | Replacement by flow straightener and specific disinfection |
| Unfavourable equipment | Solenoid valves of specialized faucets | Replacement and specific disinfection |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ficheux, A.; Réthoret, J.; Laget, J.; Baux, C.; Gayrard, N.; Duranton, F.; Vetromile, F.; Szwarc, I.; Cazevieille, C.; Servel, M.-F.; et al. Successful Disinfection of a New Healthcare Facility Contaminated with Pseudomonas aeruginosa. Hygiene 2022, 2, 1-13. https://doi.org/10.3390/hygiene2010001
Ficheux A, Réthoret J, Laget J, Baux C, Gayrard N, Duranton F, Vetromile F, Szwarc I, Cazevieille C, Servel M-F, et al. Successful Disinfection of a New Healthcare Facility Contaminated with Pseudomonas aeruginosa. Hygiene. 2022; 2(1):1-13. https://doi.org/10.3390/hygiene2010001
Chicago/Turabian StyleFicheux, Alain, Jérémy Réthoret, Jonas Laget, Cristel Baux, Nathalie Gayrard, Flore Duranton, Fernando Vetromile, Ilan Szwarc, Chantal Cazevieille, Marie-Françoise Servel, and et al. 2022. "Successful Disinfection of a New Healthcare Facility Contaminated with Pseudomonas aeruginosa" Hygiene 2, no. 1: 1-13. https://doi.org/10.3390/hygiene2010001
APA StyleFicheux, A., Réthoret, J., Laget, J., Baux, C., Gayrard, N., Duranton, F., Vetromile, F., Szwarc, I., Cazevieille, C., Servel, M.-F., & Argilés, À. (2022). Successful Disinfection of a New Healthcare Facility Contaminated with Pseudomonas aeruginosa. Hygiene, 2(1), 1-13. https://doi.org/10.3390/hygiene2010001






