Identifying Older Adults at Risk of Accelerated Decline in Gait Speed and Grip Strength: Insights from the National Health and Aging Trends Study (NHATS) †
Abstract
1. Introduction
2. Methods
2.1. Study Participants
2.2. Gait Speed and Grip Strength
2.3. Covariates
2.4. Statistical Analysis
3. Results
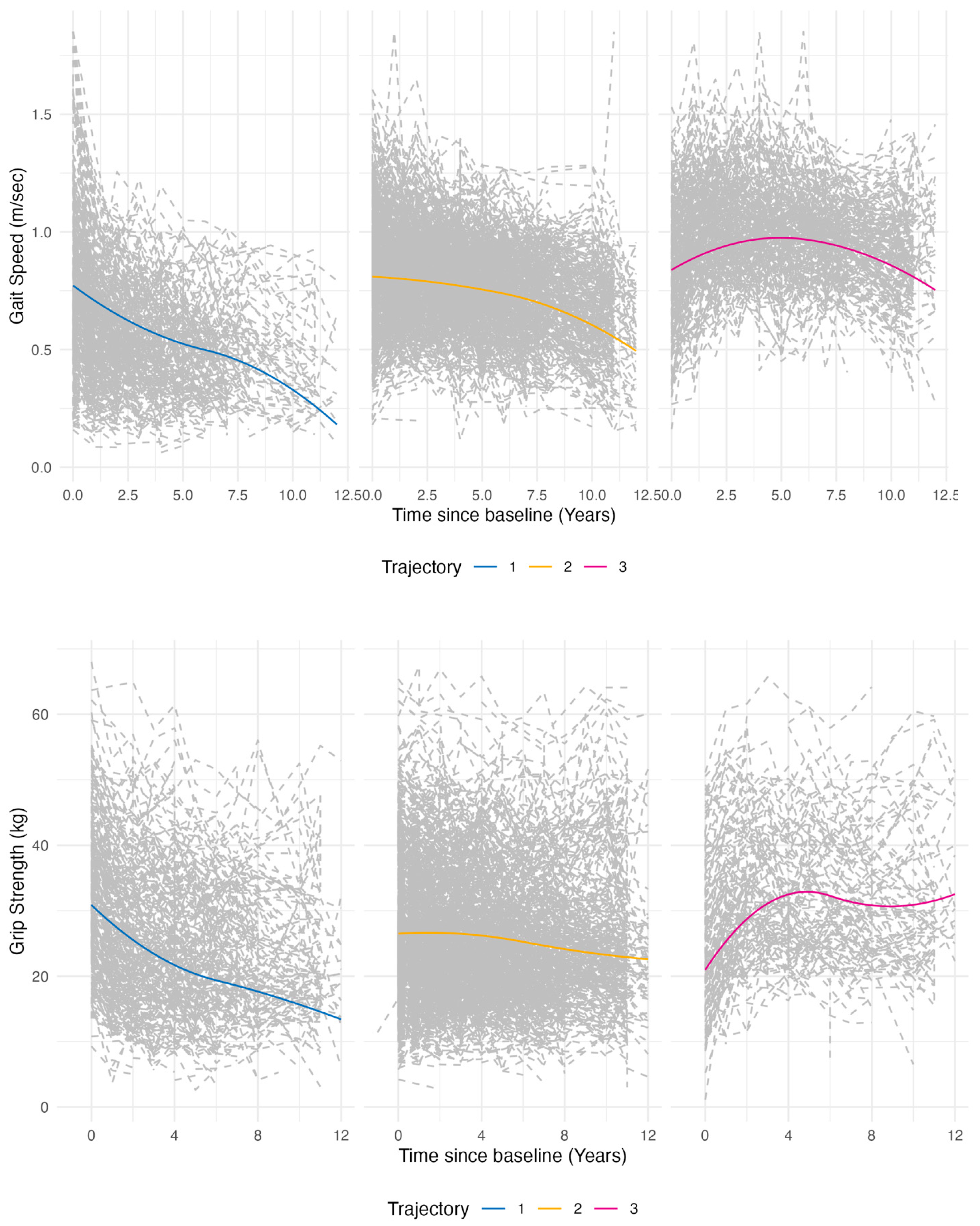
3.1. Latent Class Growth Analysis
3.2. Baseline Characteristics by Trajectory Classification
3.3. Multinomial Logistic Regression Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gill, T.M.; Gahbauer, E.A.; Han, L.; Allore, H.G. Trajectories of disability in the last year of life. N. Engl. J. Med. 2010, 362, 1173–1180. [Google Scholar] [CrossRef] [PubMed]
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. JAMA 2014, 311, 2387–2396. [Google Scholar] [CrossRef] [PubMed]
- Church, D.D.; Hoffman, J.R.; Mangine, G.T.; Jajtner, A.R.; Townsend, J.R.; Beyer, K.S.; Wang, R.; La Monica, M.B.; Fukuda, D.H.; Jeffrey, R. Comparison of high-intensity vs. high-volume resistance training on the BDNF response to exercise. J. Appl. Physiol. 2016, 121, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Ashley, E.A. Towards precision medicine. Nat. Rev. Genet. 2016, 17, 507–522. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.Y.; Bruyère, O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q.L.; Beamer, B.A.; Chaves, P.H.; Guralnik, J.M.; Fried, L.P. Heterogeneity in rate of decline in grip, hip, and knee strength and the risk of all-cause mortality: The Women’s Health and Aging Study II. J. Am. Geriatr. Soc. 2010, 58, 2076–2084. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, W.C.; Scherbov, S.; Weber, D.; Bordone, V. Combined Measures of Upper and Lower Body Strength and Subgroup Differences in Subsequent Survival Among the Older Population of England. J. Aging Health 2016, 28, 1178–1193. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R.; et al. Prognostic value of grip strength: Findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Bandeen-Roche, K.; Chaves, P.H.; Johnson, B.A. Preclinical mobility disability predicts incident mobility disability in older women. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M43–M52. [Google Scholar] [CrossRef] [PubMed]
- Carey, E.C.; Covinsky, K.E.; Lui, L.Y.; Eng, C.; Sands, L.P.; Walter, L.C. Prediction of Mortality in Community-Living Frail Elderly People with Long-Term Care Needs. J. Am. Geriatr. Soc. 2008, 56, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Newman, A.B.; Simonsick, E.M.; Naydeck, B.L.; Boudreau, R.M.; Kritchevsky, S.B.; Nevitt, M.C.; Pahor, M.; Satterfield, S.; Brach, J.S.; Studenski, S.A.; et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA 2006, 295, 2018–2026. [Google Scholar] [CrossRef] [PubMed]
- Porto, J.M.; Nakaishi, A.P.M.; Cangussu-Oliveira, L.M.; Freire Júnior, R.C.; Spilla, S.B.; Abreu, D.C.C. Relationship between grip strength and global muscle strength in community-dwelling older people. Arch. Gerontol. Geriatr. 2019, 82, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker for Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Hébert, R. Functional decline in old age. CMAJ 1997, 157, 1037–1045. [Google Scholar] [PubMed]
- Buurman, B.M.; Hoogerduijn, J.G.; de Haan, R.J.; Abu-Hanna, A.; Lagaay, A.M.; Verhaar, H.J.; Schuurmans, M.J.; Levi, M.; de Rooij, S.E. Geriatric conditions in acutely hospitalized older patients: Prevalence and one-year survival and functional decline. PLoS ONE 2011, 6, e26951. [Google Scholar] [CrossRef] [PubMed]
- Geyskens, L.; Jeuris, A.; Deschodt, M.; Grootven, B.V.; Gielen, E.; Flamaing, J. Patient-related risk factors for in-hospital functional decline in older adults: A systematic review and meta-analysis. Age Ageing 2022, 51, afac007. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wang, M. Socioeconomic status and ADL disability of the older adults: Cumulative health effects, social outcomes and impact mechanisms. PLoS ONE 2022, 17, e0262808. [Google Scholar] [CrossRef] [PubMed]
- Mcmaughan, D.J.; Oloruntoba, O.; Smith, M.L. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front. Public Health 2020, 8, 231. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.J.; Latham, N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst. Rev. 2009, CD002759. [Google Scholar] [CrossRef] [PubMed]
| Variable—Mean (SD) | Total (N = 4961) | Worsening (N = 1409) | Stable (N = 2709) | Improving (N = 843) | p-Value |
|---|---|---|---|---|---|
| Baseline Gait Speed | 0.85 (0.01) | 0.79 (0.02) | 0.86 (0.01) | 0.91 (0.01) | <0.001 |
| Yearly Change in Gait Speed | −0.03 (0.002) | −0.09 (0.004) | −0.02 (0.002) | 0.03 (0.004) | <0.001 |
| Demographics—N (%) | |||||
| Age 65–74 years | 2140 (43.1) | 355 (25.2) | 1194 (44.1) | 591 (70.1) | <0.001 |
| 75–84 years | 1999 (40.3) | 618 (43.9) | 1157 (42.7) | 224 (26.6) | |
| ≥85 years | 822 (16.6) | 436 (30.9) | 358 (13.2) | 28 (3.3) | |
| Gender: Female | 2822 (55.4) | 891 (61.4) | 1527 (56.0) | 404 (47.7) | <0.001 |
| Race White | 3553 (82.8) | 923 (77.8) | 1962 (82.9) | 668 (87.7) | <0.001 |
| Black | 980 (7.3) | 351 (10.5) | 516 (7.0) | 113 (4.7) | |
| Hispanic | 269 (6.1) | 81 (7.1) | 152 (6.4) | 36 (4.3) | |
| Other | 159 (3.8) | 54 (4.5) | 79 (3.6) | 26 (3.3) | |
| Marital Status Married/Living with Partner | 2627 (53.0) | 572 (40.6) | 1466 (54.1) | 589 (69.9) | <0.001 |
| Non-partnered | 2334 (47.0) | 837 (59.4) | 1243 (45.9) | 254 (30.1) | |
| Socioeconomic Status | |||||
| Education High School or Less | 2505 (50.5) | 855 (60.7) | 1348 (49.8) | 302 (35.8) | <0.001 |
| Some College or More | 2456 (49.5) | 554 (39.3) | 1361 (50.2) | 541 (64.2) | |
| Income Low (≤USD 49,999) | 2032 (41.0) | 641 (45.5) | 1139 (42.0) | 252 (29.9) | <0.001 |
| Middle (USD 50,000–99,999) | 622 (12.5) | 104 (7.4) | 364 (13.4) | 154 (18.3) | |
| High (≥USD 100,000) | 296 (6.0) | 38 (2.7) | 149 (5.5) | 109 (12.9) | |
| Missing | 2011 (40.5) | 626 (44.4) | 1057 (39.0) | 328 (38.9) | |
| Insurance Public Insurance | 2116 (42.7) | 658 (46.7) | 1135 (41.9) | 323 (38.3) | <0.001 |
| Private Insurance | 2845 (57.3) | 751 (53.3) | 1574 (58.1) | 520 (61.7) | |
| Health Conditions | |||||
| Arthritis | 2636 (53.1) | 856 (60.8) | 1406 (51.9) | 374 (44.4) | <0.001 |
| Cancer | 1272 (25.6) | 366 (26.0) | 706 (26.1) | 200 (23.7) | 0.21 |
| Cardiovascular Disease | 1208 (24.3) | 435 (30.9) | 635 (23.4) | 138 (16.4) | <0.001 |
| Current Smoker | 413 (8.3) | 104 (7.4) | 244 (9.0) | 65 (7.7) | 0.02 |
| Dementia | 127 (2.6) | 75 (5.3) | 44 (1.6) | 8 (0.9) | <0.001 |
| Elevated Waist Circumference | 3070 (61.9) | 952 (67.6) | 1710 (63.1) | 408 (48.4) | <0.001 |
| High Blood Pressure | 3275 (66.0) | 982 (69.7) | 1822 (67.3) | 471 (55.9) | <0.001 |
| Low Physical Activity | 1381 (27.8) | 511 (36.3) | 718 (26.5) | 152 (18.0) | <0.001 |
| Lung Disease | 703 (14.2) | 226 (16.0) | 382 (14.1) | 95 (11.3) | 0.04 |
| Osteoporosis | 972 (19.6) | 320 (22.7) | 511 (18.9) | 141 (16.7) | <0.001 |
| Type II Diabetes | 1174 (23.7) | 399 (28.3) | 639 (23.6) | 136 (16.1) | <0.001 |
| Unintentional Weight Loss | 638 (12.9) | 260 (18.4) | 307 (11.3) | 71 (8.4) | <0.001 |
| Multiple Chronic Conditions (≥2) | 3554 (71.6) | 1110 (78.8) | 1947 (71.9) | 497 (58.9) | <0.001 |
| Variable | Worsening Gait Speed OR (95% CI) (Ref: Stable) | Worsening Grip Strength OR (95% CI) (Ref: Stable) |
|---|---|---|
| Demographics | ||
| Age | ||
| 65–74 years | Reference | Reference |
| 75–84 years | 1.74 (1.33, 2.27) | 1.33 (1.03, 1.73) |
| ≥85 years | 4.80 (3.47, 6.64) | 2.28 (1.61, 3.21) |
| Race | ||
| White | Reference | Reference |
| Black | 1.43 (1.11, 1.85) | 0.98 (0.79, 1.22) |
| Hispanic/Other | 1.10 (0.84, 1.45) | 1.18 (0.83, 1.58) |
| Gender | ||
| Male | Reference | Reference |
| Female | 1.08 (0.91, 1.29) | 1.55 (1.15, 2.08) |
| Socioeconomic Status | ||
| Education | ||
| High School or Less | Reference | Reference |
| Some College | 0.67 (0.53, 0.85) | 1.03 (0.78, 1.36) |
| Marital Status | ||
| Married/Living with Partner | Reference | Reference |
| Non-partnered | 1.10 (0.84, 1.41) | 0.94 (0.72, 1.22) |
| Income | ||
| Low (≤USD 49,999) | Reference | Reference |
| Middle (USD 50,000–99,999) | 0.68 (0.53, 0.88) | 0.60 (0.43, 0.84) |
| High (≥USD 100,000) | 0.61 (0.41, 0.91) | 0.47 (0.30, 0.73) |
| Insurance | ||
| Public Insurance | Reference | Reference |
| Private Insurance | 0.69 (0.51, 0.92) | 0.84 (0.61, 1.15) |
| Health Conditions | ||
| Multiple Chronic Conditions (≥2) | 1.29 (1.07, 1.56) | 1.43 (1.21, 1.68) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lynch, D.H.; Spangler, H.; Griffin, J.S.; Kahkoska, A.; Boccaccio, D.; Xie, W.; Lin, F.-C.; Batsis, J.A.; Fielding, R.A. Identifying Older Adults at Risk of Accelerated Decline in Gait Speed and Grip Strength: Insights from the National Health and Aging Trends Study (NHATS). J. Ageing Longev. 2025, 5, 19. https://doi.org/10.3390/jal5020019
Lynch DH, Spangler H, Griffin JS, Kahkoska A, Boccaccio D, Xie W, Lin F-C, Batsis JA, Fielding RA. Identifying Older Adults at Risk of Accelerated Decline in Gait Speed and Grip Strength: Insights from the National Health and Aging Trends Study (NHATS). Journal of Ageing and Longevity. 2025; 5(2):19. https://doi.org/10.3390/jal5020019
Chicago/Turabian StyleLynch, David H., Hillary Spangler, Jacob S. Griffin, Anna Kahkoska, Dominic Boccaccio, Wenyi Xie, Feng-Chang Lin, John A. Batsis, and Roger A. Fielding. 2025. "Identifying Older Adults at Risk of Accelerated Decline in Gait Speed and Grip Strength: Insights from the National Health and Aging Trends Study (NHATS)" Journal of Ageing and Longevity 5, no. 2: 19. https://doi.org/10.3390/jal5020019
APA StyleLynch, D. H., Spangler, H., Griffin, J. S., Kahkoska, A., Boccaccio, D., Xie, W., Lin, F.-C., Batsis, J. A., & Fielding, R. A. (2025). Identifying Older Adults at Risk of Accelerated Decline in Gait Speed and Grip Strength: Insights from the National Health and Aging Trends Study (NHATS). Journal of Ageing and Longevity, 5(2), 19. https://doi.org/10.3390/jal5020019







