Abstract
Introduction: Up to 50% of community-dwelling older adults report living with some chronic pain that interferes with their daily functioning and leads to disabilities. Hence, it is crucial to provide these individuals with strategies to effectively manage pain. An interdisciplinary approach is warranted considering the numerous factors contributing to pain among older adults. Although several studies have been conducted on various interdisciplinary pain self-management programs, little effort has been made to synthesize knowledge about such programs for older adults. Objective: The objective of this review was to synthesize the characteristics and effects of interdisciplinary chronic pain self-management interventions targeting community-dwelling older adults. Methods: A scoping review was conducted following the steps recommended by Arksey and O’Malley (2005) and Levac et al. (2010). Keyword searches were performed in MEDLINE, CINAHL, EMBASE, and the Cochrane Library. Results: Sixty-six articles were included. Most interventions were based on a cognitive-behavioral group approach and used a combination of modalities, including education and training on the use of self-management strategies. The professionals most frequently involved in group interventions were psychologists, physiotherapists, and occupational therapists. Several benefits of these programs have been reported concerning pain intensity, independence in daily functioning, mental health, and quality of life. Conclusions: Interdisciplinary chronic pain self-management programs appear promising in guiding clinical and rehabilitation interventions for older adults living with chronic pain.
1. Introduction
Chronic pain is a public health priority [1], as this problem is highly prevalent and has significant consequences at both the individual and societal levels. Chronic pain is defined as persistent or recurrent pain lasting longer than three months [2]. In Canada, one in five adults suffer from chronic pain [3,4]. Several studies show that the prevalence of chronic pain increases with age [3,4,5]. An epidemiological longitudinal study indicates that 27% of Canadians aged 65 and over report chronic pain [6].
Chronic pain is a complex phenomenon that has an impact on several aspects of a person’s life, such as the ability to engage in physical activities [7,8], social activities [7,9], and activities related to productivity such as household management and work [7,10]. Chronic pain can also interfere with sleep [7,11] and mood [11]. Studies show that pain intensity is associated with a deterioration of quality of life [11] and the inability to maintain an independent lifestyle [9,11]. People affected by chronic pain frequently report a lack of control over pain symptoms and difficulty in predicting their onset [9,12,13]. A robust epidemiologic study conducted among 8245 American community-dwelling older adults revealed that more than half of the study participants presented chronic pain that interfered with their daily functioning [8].
A comprehensive chronic pain management program relying on an interdisciplinary approach appears to be the most appropriate one [14,15]. In fact, there is evidence that an interdisciplinary approach can lead to a decrease in disability and pain intensity, as well as an attenuation of several psychological signs and symptoms related to chronic pain, such as depression, anxiety, stress, and fear [16]. Comprehensive chronic pain management programs relying on an interdisciplinary approach are particularly recommended for older adults [17,18], as they often present comorbidities and their health needs are often more complex to address than those of younger individuals [19].
Furthermore, there is evidence that self-management interventions are essential to optimizing health outcomes for older adults with chronic pain [17]. A self-management paradigm involves an active role for patients in the management of their health condition, and a collaborative relationship between patients and the health care team [20,21]. Some studies demonstrate that self-management programs can be effective in reducing health care utilization [22,23]. These interventions typically address physical, psychological, and social dimensions and generally combine educational and skills development approaches to build self-efficacy for managing pain [17,24]. Consistent with the Chronic Care Model [25], self-management support provided by health professionals from several disciplines is associated with improved patient health outcomes and self-management behaviors [26].
A few systematic reviews have examined the impact of interdisciplinary pain self-management programs and support their efficacy [27,28]. However, little effort has been devoted to synthesizing knowledge about interdisciplinary chronic pain self-management interventions targeting community-dwelling older adults. There is a need to synthesize evidence regarding the effects of these interventions and to document their components (e.g., topics addressed, type of exercises) and format (e.g., number of sessions, frequency, duration) to better inform practice and research. Thus, this paper aims to synthesize the characteristics and effects of interdisciplinary chronic pain self-management interventions targeting community-dwelling older adults.
Context of the Study
This review was part of a research project aimed primarily at informing the clinical practices of an interdisciplinary team providing health care services to community-dwelling older adults suffering from chronic pain. The members of this interdisciplinary team—geriatricians, occupational therapists, physiotherapists, nurses, and a psychologist—were interested in collaborating on this scoping review since they were keen to offer a chronic pain self-management program to their patients that was supported by the most recent scientific evidence available in this domain.
2. Methods
A scoping review was undertaken according to Arksey and O’Malley’s [29] methodological framework and the recommendations by Levac et al. [30]. The following steps were performed: (1) identification of the research question; (2) identification of relevant studies; (3) study selection; (4) data extraction; (5) data synthesis; and (6) consultation. The PRISMA Extension for Scoping Reviews (PRISMA-ScR) [31] was used for reporting the methods and results of this study.
2.1. Step 1: Identifying the Research Questions
The following questions guided the research process of this scoping review:
- -
- What is known about the effects of interdisciplinary chronic pain self-management interventions targeting community-dwelling older adults?
- -
- What are the characteristics of these interventions? More precisely, what are the conceptual foundations of these interventions? What is their content? Who is involved in these interventions? In what format are they delivered?
2.2. Step 2: Identifying Relevant Studies
A search in bibliographic databases was conducted in May 2020 by the second author (MEL) with support from an academic librarian specialized in rehabilitation and health research and the author responsible for the research project (JF). The scoping review’s objective was to inform the research team of the characteristics of programs that had shown the most promising outcomes. The following databases were searched: MEDLINE, CINAHL, EMBASE, and Cochrane Library. The relevant articles were searched using the following keywords and MESH terms: chronic pain, fibromyalgia, persistent pain, long term pain, arthr*, osteoarthr*, rheumat*, self-management, self-care, self-efficacy, pain management, pain rehabilitation, pain program, patient care team, interprofessional relations, interdiscipl*, multidiscipl*, transdiscipl*, integrative team, collaborative team, team, and teams. See Table 1 for an example of a search strategy in one database. References from each database search were imported into Endnote X9. A manual search of the reference lists of included studies and relevant review articles (e.g., systematic reviews, scoping reviews) found with the search strategy was also conducted to find other potentially relevant studies. Finally, a manual search was conducted in the following key journals: BMC Geriatrics, British Journal of Pain, Clinical Journal of Pain, Disability and Rehabilitation, Journal of Rehabilitation Medicine, and Journal of Pain Research. These journals were chosen because of their relevance to the topic of this review.

Table 1.
Search strategy conducted in MEDLINE.
Inclusion criteria for the selection of articles were the following: (1) the study examined the impact of a chronic pain self-management intervention; (2) the studied intervention was delivered by at least two health professionals from different disciplines; and (3) the study targeted or included community-dwelling adults aged 65 or over living with chronic pain (defined as pain that persisted for three months or more). Since a limited number of studies specifically targeted people aged 65 or over, we have subsequently chosen to broaden the last inclusion criterion. Based on the available literature, we included studies with a sample of participants aged 55 or more (on average).
Authors were contacted by email if an article did not provide sufficient information regarding the age of participants or if any other important information was missing to determine if the article should be included or not in the scoping review. Articles were excluded if (1) they concerned a study conducted on a population suffering from a very specific type of pain, such as headaches, cancer pain, or spinal cord injury/orofacial/pelvic pain, or (2) the primary goal of the intervention under study was to facilitate return to work. Articles reporting the results of quantitative, qualitative, and mixed-method studies and published in English or French in a peer-reviewed journal were considered in this scoping review.
2.3. Step 3: Study Selection
The selection process was conducted independently by two reviewers. Reviewers first screened the articles identified through the keyword strategy based on their titles and abstracts using inclusion and exclusion criteria. Subsequently, the full text of all potentially relevant articles was reviewed to determine if they should be considered in the scoping review. The rationale for the exclusion of studies in this phase was documented in the “research notes” section of Endnote X9. The results of the selection process of the two reviewers were compared. A consensus-based discussion allowed the few disagreements between the two reviewers to be resolved. A third reviewer was involved in the final decision to resolve any remaining disagreements. Figure 1 illustrates the PRISMA flow diagram summarizing the search process.
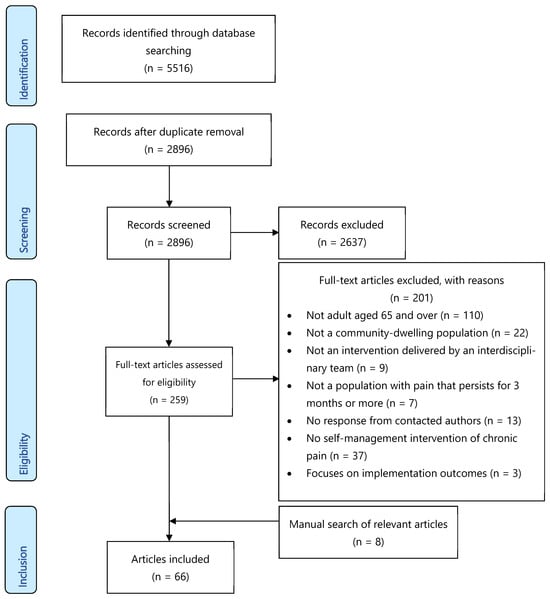
Figure 1.
Flow chart depicting the selection process of the scoping review.
2.4. Step 4: Charting the Data
For each included article, data were extracted in an Excel table. Data extracted included but were not limited to (1) the characteristics of the study (e.g., authors, year of publication, country where the study was conducted, study design, sample size), (2) the description of the intervention(s) (e.g., type, format, regimen, conceptual or theoretical roots), and (3) intervention outcomes (e.g., variables of interest; assessment tools; measurement times; short-term, mid-term, and long-term outcomes). The second author and a research assistant independently extracted information from the first ten studies to validate data extraction. In case of disagreement, the last author was involved in the discussions until a consensus was reached. The second author then completed the data charting grid for the remaining articles.
2.5. Step 5: Collating, Summarizing, and Reporting the Results
Extracted data were organized in summary tables. Descriptive analyses (means, standard deviations, and proportions) were used to describe the samples of primary studies. Data about the characteristics of the interventions were organized in accordance with the British Pain Society’s guidelines [32] for pain management programs for adults, namely (1) modes of delivery (interventions delivered in a group format, an individual format, or a combined format), (2) intervention components (education, exercises, skills training, etc.), and (3) intervention dosage (session duration and frequency).
Data about the short-term, mid-term, and long-term outcomes of the interventions were organized in accordance with the following dimensions: (1) pain severity; (2) pain self-efficacy (i.e., confidence regarding one’s ability to carry out daily activities despite the presence of pain); (3) mental health (which encompasses depression, anxiety symptoms, and general emotional well-being); (4) physical performance (which encompasses mobility, dexterity, and capacity to carry out daily physical activities); (5) daily functioning (i.e., the ability to engage and perform everyday activities independently); and (6) quality of life. The organization of the data was carried out independently by two of the authors. Subsequently, data were subjected to quantitative analysis and narrative summaries.
2.6. Step 6: Consultation of Clinicians
In addition to the researchers and research staff, several health professionals providing care to older adults with chronic pain were consulted from the very beginning of the review process. The research team met with these stakeholders to obtain their insights on the research questions, the eligibility criteria, and the search strategy and to share and discuss preliminary findings.
3. Results
Electronic searches in databases yielded a total of 2896 references after the removal of duplicates. At the end of the selection process, 58 articles were retained for inclusion in the scoping review. Additionally, eight articles were found through manual search in journals, reference lists of included studies, and relevant reviews. Finally, a total of 66 articles were included in this review [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98]. The PRISMA flow diagram in Figure 1 depicts the number of articles selected and excluded at each stage of the process as well as the reasons for exclusion.
3.1. Study Characteristics
The 66 articles selected for this scoping review included 61 quantitative studies [33,34,35,36,37,38,40,41,42,43,44,45,46,47,48,49,50,51,52,53,55,56,57,58,59,60,61,62,63,64,65,66,68,69,70,71,72,73,75,76,77,78,79,80,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98], 1 qualitative study [74], and 4 mixed-method studies [39,54,67,81]. Most quantitative studies relied on pretest–posttest designs (n = 42). The remaining articles reported results from randomized controlled trials (n = 14), quasi-experimental studies (n = 4), and a randomized, concurrent, multiple-baseline single-case design (n = 1). The mixed-method studies relied on a single-group pretest–posttest study design complemented with qualitative data collection. The sample size of quantitative studies ranged from 5 to 1510 participants. Studies were conducted in 17 different countries, predominantly in the United States (n = 17), Australia (n = 10), Canada (n = 8), and the Netherlands (n = 9). The most frequent implementation settings were hospital-based outpatient clinics (n = 28) and community-based outpatient clinics (n = 27). Other settings included outpatient clinics nested in research centers (n = 4) and elderly community centers (n = 1). Six articles did not mention the research setting.
Of the 66 articles, 38 involved participants with a diversity of chronic pain diagnoses. Other studies targeted participants with a specific diagnosis such as chronic widespread pain (n = 12) (e.g., fibromyalgia), chronic musculoskeletal pain (n = 10) (e.g., chronic back pain, chronic neck pain, chronic regional pain syndrome), and rheumatic diseases (n = 6) (e.g., osteoarthritis, chronic inflammatory arthritis).
These 66 articles covered a total of 57 programs. More precisely, results from five programs were reported in more than one publication [37,42,46,47,48,59,60,68,69,88,92,93,94,95,96]. A single study compared the effects of two programs [85]. Most of the programs were delivered through a combined approach (group and individual format) (n = 27) or a group approach (n = 25). Five programs relied solely on an individual approach.
Table 2 presents the main characteristics of the selected articles (authors, year of publication, country where the study was conducted, study design, sample size, and a short description of the intervention(s)) and summarizes intervention outcomes. A detailed description of the interventions is available in Appendix A.

Table 2.
Characteristics of included studies, interventions, and outcomes.
3.2. Underlying Models or Theories for Intervention
Most programs were based on the cognitive-behavioral (n = 18) [33,36,39,40,44,46,47,48,49,51,54,56,59,63,66,68,71,75,87,88,92] or biopsychosocial (n = 12) models [35,36,37,39,41,42,72,73,75,78,79,83,84,85,93,94,95,96,97]. Some interventions were based on the patient-centered care model (n = 3) [38,58,80] or the multimodal approach (n = 2) [82,86]. Less frequently, programs were based on the chronic disease self-management model (n = 1) [38], the social cognitive theory (n = 1) [57], a community-based model of care (n = 1) [81], the osteoarthritis research society guidelines [81], or a spiritual-based approach (n = 1) [64]. Sixteen programs did not describe the model or theory underlying the treatment [34,43,45,50,52,53,61,62,65,67,70,76,77,90,91,98].
3.3. Description of Programs Using a Combined Approach (Group and Individual) (n = 27)
3.3.1. Duration and Frequency
On average, the programs with a combined approach lasted 6 weeks, with a mean total duration of 84 h, an average of 16 sessions, and a mean frequency of 4 sessions per week.
3.3.2. Description of Programs
The professionals most frequently involved in group interventions were psychologists (n = 20) and physiotherapists (n = 20), followed by general physicians or specialist physicians (n = 11), occupational therapists (n = 11), nurses (n = 10), and social workers (n = 5). Data on the professionals involved were missing for three programs. In addition to sessions led by health professionals, one program [81] included a 2 h peer-led support group session from the Arthritis Society.
Of the 27 programs using a combined approach, 23 included group education. Of these programs, the most frequently discussed topics pertained to different aspects of pain (e.g., neurophysiology of pain, neuroplasticity, chronic pain cycle, usual course of symptoms, gate control theory) (n = 13), conservative treatments (e.g., information about medication use, risks and benefits of medical treatments, strategies for managing medication) (n = 8), and nutrition (e.g., how nutrition affects pain management, instructions on healthy diet) (n = 8). Less common topics were the effects of stress on pain (e.g., education on the relationship between stress management and pain, psychosocial influences on pain, the “stress response system”) (n = 6), physical activity (e.g., relation between physical activity and pain, education about the benefits of exercise on pain and functional ability) (n = 4), and healthy lifestyle (n = 1) (e.g., advice related to general health). Finally, one program provided information on specific anatomy features (e.g., anatomy of the spinal cord) or ergonomic principles. Data on the topics covered during educational sessions were missing for two programs.
More than half (n = 15) of the programs using a combined approach included in-group physical exercise sessions. Of these programs, five offered group hydrotherapy [34,43,50,51,65], whereas four programs involved a movement-based therapy component founded on techniques such as yoga [39,79], tai chi [39], qigong [39,79], or the Feldenkrais method [65].
All programs included in-group training in self-management skills. Most programs (n = 17) taught strategies to help people manage stress. Nine programs included relaxation training [39,40,50,59,65,75,76,79,90]. In some studies, breathing (e.g., controlled deep breathing, diaphragmatic breathing) [43,46,47,48,52,83,85,89,93] or progressive muscle relaxation [33,43,52,96] was taught and practiced. Thirteen programs taught activity pacing as a self-management strategy. Studies described activity pacing as performing daily activities in a time-contingent rather than pain-contingent manner to improve function in a sustainable way [41,78]. Mostly, advice regarding pacing revolved around the structuring and planning of daily activities [45,61,84,93]. Key messages were the importance of balance between physical activity and rest [96] and moderation in activities [40,59,61,93]. Eight programs taught strategies to better manage sleep, including information on sleep hygiene (e.g., establishing a consistent sleep schedule, reducing, or eliminating daytime napping, relaxation) [33,40,43,50,52,61,75,81]. Nine programs included a communication and interaction skills component [33,43,45,52,60,61,74,75,95]. Most of the time, relationship difficulties were addressed, and a problem-solving approach was undertaken. Assertive communication skills training was performed in four programs [43,45,52,93]. Only two programs demonstrated and practiced ergonomic principles [45,61]. Of the 27 programs, only 4 presented problem-solving strategies to participants [43,52,61,75]. Some (n = 5) helped participants develop mindfulness skills [43,52,65,74,79]. Finally, three programs included exercises based on acceptance and commitment therapy (ACT) [43,52,74]. In thirteen programs using skills training, participants were instructed to set relevant and realistic individual goals at the onset of the treatment, and their progress was monitored [33,34,39,43,45,52,61,65,66,75,84,86,94]. Eight programs included strategies to encourage participants to practice and maintain the learned skills in their daily lives, such as giving them homework to do in between sessions [43,93] and encouraging them to practice skills or exercises [33,34]. Data on the content of group skills training were missing for two programs.
Eleven programs included group psychotherapy [33,42,43,50,61,66,75,76,84,90,91]. Some authors described cognitive restructuring as a strategy to help participants identify and challenge unhelpful pain-related thoughts [66,71,93]. Some programs offered cognitive restructuring within the context of cognitive-behavioral therapy [43,50,52,66,93].
Six programs involved family or friends in the intervention [33,39,59,61,75,86]. For two programs, most of the intervention was delivered to both patients and their partners. More precisely, in the study of Abbasi et al. 2012 [33], patients and their spouses assisted in all sessions together, and information on the most effective strategies for requesting and providing spousal assistance was given. Each participant and their spouse were asked to set weekly health-related goals. In the study of Ramke et al. 2016 [75], spouses participated in a family education day and received four weekly couple-based telephone consultations with a psychologist targeting different education themes (e.g., pain mechanisms, communication, and assertiveness strategies). Craner et al. 2016 [39] included a 2-day family educational program, and Kurklinsky et al. 2016 [61] offered weekly sessions for family or friends to learn about the intervention and ask questions. Kowal et al. 2015 [59] included a single interactive session for patients and family members to address interpersonal aspects of chronic pain. Finally, Vincent et al. 2013 [86] encouraged family members to attend all educational sessions of the program.
The majority of programs included an individual pharmacological intervention (n = 19). Based on participants’ reports of limited or lack of symptom relief, eight of these programs explicitly aimed to reduce or discontinue the use of medication susceptible to induce dependence (e.g., benzodiazepines, non-opioid analgesic medications, muscle relaxants) [39,40,42,43,50,61,76,91], and three programs supported and monitored withdrawal of opioid medication [35,40,91]. Finally, one program encouraged the discontinuation of medical cannabis use [77].
Regarding the health professionals’ involvement, sixteen programs described the implication of a general or a specialist physician in the interdisciplinary team (e.g., orthopedic surgeon, psychiatrist, rehabilitation physician). Their principal role was generally medical management [33,39,43,45,51,65,81,86,90,91], but some of them provided injections (e.g., spinal or local injection, anesthetic procedures) [43,90]. Pharmacists were involved in individual interventions in two of the combined approach programs. In the study by Smeeding et al. 2011 [79], the pharmacist advised participants about supplements and was involved in the delivery of a tobacco cessation program. Almost half of the programs involved an occupational therapist in the delivery of individual interventions (n = 12) [34,36,42,45,50,59,61,65,77,84,90,91]. For example, this health professional taught ergonomic principles and activity pacing [36,90] and helped participants rediscover personal interests and abilities [84]. In one program, the occupational therapist used desensitization techniques, graded motor imagery, and mirror therapy for chronic regional pain syndrome participants [65]. The role of the occupational therapist was not described in detail for eight programs. Most programs included individual interventions delivered by a physiotherapist (n = 18) [33,34,35,36,42,45,50,51,52,59,65,74,76,77,79,81,90,91]. For example, physiotherapists prescribed an individualized therapeutic exercise program [33,34,52,81], taught self-massage [35] and musculoskeletal release techniques [52], and provided acceptance and commitment therapy [51]. The role of the physiotherapist was not described in detail for 13 programs. Only three programs included an individual intervention delivered by a nurse. The role of the nurse was not described in detail for two of these programs. In the study of Hâllstam et al. (2016), nurses gave instructions to patients about the use of transcutaneous electric nerve stimulation and were responsible for medical follow-ups. In the study of Kurklinsky et al. 2016 [61], nurses supervised by a physician had the lead role in pharmacological management and oversaw the coordination of individualized patient care. A psychologist was involved in delivering an individual intervention in 15 programs [36,39,42,43,45,50,51,52,59,65,74,76,79,90,91]. Moreover, in some of the programs, the psychologist met participants at the program midpoint to discuss progress and review individual goals [44,52]. Psychology interventions were optional in two programs and were delivered according to participants’ needs [39,90]. Five of the programs involved an individual intervention with a social worker [36,42,45,59,74]. However, the role of this professional was not clearly defined.
3.4. Description of Programs with a Group Component Only (n = 25)
3.4.1. Duration and Frequency
On average, the programs involving only a group approach lasted 6 weeks. The mean total duration was 25 h. On average, programs included eight sessions, and sessions were held twice a week. The mean session duration was 3 h.
3.4.2. Description of Programs
The most common health professionals involved in group interventions were physiotherapists (n = 21) and general or specialist physicians (n = 16). Other professionals involved were occupational therapists (n = 13), psychologists (n = 12), nurses (n = 10), social workers (n = 3), pharmacists (n = 3), and kinesiologists (n = 1).
Of the 25 programs using a group approach, 22 involved an educational component. The most frequently addressed topics were pain (e.g., neurophysiology of pain, neuroplasticity, chronic pain cycle, usual course of symptoms, gate control theory) (n = 15) [41,44,46,49,53,55,64,71,72,73,78,83,85,89,98], conservative treatments (e.g., information about medication use and surgery, risks and benefits of medical treatments, strategies for managing medication) (n = 11) [41,53,55,58,67,73,78,83,85,93,98], and physical activity (e.g., relation between physical activity and pain, education about the benefits of exercise on pain and functional ability) (n = 11) [41,46,53,55,58,67,73,78,83,85,98]. Less frequently covered topics were the effect of stress on pain (e.g., education on the relationship between stress management and pain, psychosocial influences on pain, the “stress response system”) (n = 4) [41,46,72,78] and nutrition (e.g., how nutrition affects pain management, instructions on healthy diet) (n= 4) [46,53,56,58]. Finally, some programs provided information on healthy lifestyles (n = 4) [55,67,73,85], specific anatomy features (e.g., anatomy of the spinal cord) (n = 5) [56,71,72,85,89], and ergonomic principles (n = 3) [44,72,98]. Data on the educational topics were missing for two programs.
Fifteen of the programs included physical exercise sessions [46,49,54,55,56,62,64,67,71,72,83,85,89,93,98]. All these programs included exercises on the floor (e.g., strengthening, stretching, or aerobic exercises), and one program also offered group hydrotherapy [56]. Of the 25 programs, only 2 included movement-based therapy, such as tai chi [55] or dance [57].
All programs involved training in self-management skills. Most programs (n = 17) taught strategies to better manage stress. Relaxation training was included in four programs [44,49,62,71]. In some studies, breathing (e.g., controlled deep breathing, diaphragmatic breathing) [46,47,48,83,85,89] or progressive muscle relaxation [46,47,48] was taught and practiced. Almost half of the programs including self-management skills training (n = 10) taught activity pacing as a self-management strategy. Advice for structuring and planning daily activities was given in most programs [41,44,70,78]. Key messages were the importance of balance between physical activity and rest [98] and moderation in activities [40,98]. Four programs taught strategies to better manage sleep, such as providing information on sleep hygiene (e.g., establishing a regular sleep schedule, reducing, or eliminating daytime napping, relaxation) [40,44,49,70]. Six programs included a communication and interaction skills component [44,46,49,58,68,69,71], and seven included demonstration and practice of ergonomic principles (e.g., normal postures, ergonomics use of the spine in daily occupations, daily mechanics) [53,63,70,72,83,89,98]. Of the 25 programs, only two included problem-solving strategies [67,68]. Six programs helped participants develop mindfulness skills [41,49,58,71,73,78]. For half of the programs, participants were instructed to set relevant and realistic individual goals at the onset of the treatment, and their progress was monitored. Thirteen programs included strategies to encourage participants to practice and maintain the acquired skills in their daily lives, such as giving them homework to do between sessions [46,68,71,85], encouraging them to practice skills or exercises [83], or signing a “pain contract” to write participants’ reasons for joining the program and their own pain management plan [83]. Another strategy was to dedicate a session of the program to summing up the educational content covered or supporting the maintenance of treatment gains [47,58,68].
Five programs included group psychotherapy [56,58,70,71,73]. One program [67] included a short interactive presentation from a patient who was an ambassador of The Arthritis Program. His role was to share his journey and experiences with chronic pain to help support others in the program.
Two programs involved family members or friends in the intervention. In the program studied by Nam et al. 2014 [67], family members or friends were invited to learn about chronic pain and ask their questions. Hapidou et al. 2016 [54] studied a program that provided a family intervention, but no details on this intervention were available. Only one in-group program included follow-up interventions; the study by Dysvik et al. 2013 [46] involved a 6-month post-intervention session consisting of therapeutic education and physical exercises and a 12-month telephone booster session consultation.
3.5. Description of Programs with an Individual Component Only (n = 5)
3.5.1. Duration and Frequency
On average, the programs using an individual approach only lasted 18 weeks, and sessions were offered on a weekly basis. The mean duration of sessions was one hour.
3.5.2. Description of Programs
Participants in all programs (n = 5) had individualized appointments with a physiotherapist. The follow-up with the physiotherapist included strength and mobility exercises in four studies [38,80,87,97] and instructions on physical activity in two studies [80,82]. In the study by Nishie et al. 2018 [97], the focus of the self-management treatment was the performance of exercises at home. Three programs involved appointments with an occupational therapist [38,80,87]. In one of these, the occupational therapist trained participants in activity pacing. The role of this professional was not clearly defined in the two other studies. Two programs included individual appointments with a dietician who gave nutritional advice related to weight loss [38] or information about the benefit of an optimal bodyweight [80]. In the study by Claes et al. 2015 [38], ongoing support and monitoring of weight loss were provided for participants who had pain related to hip or knee osteoarthritis. Psychologists were involved in three of the programs using an individual approach only. Psychologists offered individual psychological support [82,87] or referred participants to other specialists if needed [97]. In the study led by Tetsunaga et al. 2015 [82], the psychologist provided advice on pain coping strategies to patients and their families. Physicians were involved in three programs. They provided recommendations regarding the treatment plan [87,97] or were responsible for pharmacotherapy [38]. Two programs included the provision of orthotics and information related to their use [38,80].
Only one individual program included follow-up interventions. Participants in the study of Stoffer-Marx et al. (2018) received a structured telephone follow-up consultation one month after the initial session to discuss relevant matters for them and ask questions if needed.
3.6. Outcomes of Interdisciplinary Chronic Pain Self-Management Programs
In this section, results from RCTs (n = 14) and quasi-experimental (n = 4) studies regarding program outcomes are presented first. These are followed by results from pre–post studies. Since these studies were numerous (n = 46), their findings are presented according to the following subsections: (1) pain severity; (2) pain self-efficacy; (3) mental health; (4) physical performance; (5) daily functioning; and (6) quality of life. Table 1 also provides a summary of the findings of each study. Finally, this section ends with a presentation of qualitative findings.
3.6.1. Outcomes Reported from RCTs and Quasi-Experimental Studies
Of the 14 RCTs, 13 had sufficient evidence to confirm positive treatment effects in favor of the intervention group in comparison with the control group [33,53,63,68,69,75,80,83,85,93,94,95,96]. Only one article reported no significant effect of the studied intervention [98].
Hansson et al. 2010 [53] showed that 6 months after the intervention, participants in the experimental group had significantly higher self-perceived health (including mobility, self-care, usual activities, pain severity, and anxiety/depression) and balance than those in the control group. Martin and colleagues published four articles related to an RCT that included a sample of 153 participants and compared a program combining coordinated psychological, medical, educational, and physiotherapeutic components (PSYMEPHY) to standard pharmacologic care [93,94,95,96]. At the 6-month follow-up, the results were in favor of the experimental group for quality of life, physical functioning, and pain. One year after the intervention, improvements were maintained, and a significant reduction in anxiety and depression levels was found. Abbasi et al. (2012) compared a spouse-assisted pain management program with patients receiving standard medical care. One year post-intervention, participants in the experimental group had a significant reduction in kinesiophobia, pain severity, and disability compared to control group participants. Interestingly, results also showed an increase in the disability score for the control group one year post-intervention.
The weekly interdisciplinary program (WIP) studied by Martins et al. 2014 [63] showed a significant reduction in pain severity and an improvement in health-related quality of life, functioning, mental health, and sleep directly post-intervention in individuals with fibromyalgia compared to a control group that did not receive any intervention. Nicholas et al. 2013 [69]; 2017 [68] compared the efficacy of a pain self-management (PSM) group with an exercise–attention control (EAC) group. Immediately after the intervention, participants in the experimental group showed an improvement in pain distress, disability, mood, unhelpful pain beliefs, and Functional Reach scores compared to the control group [69]. At the 1-month follow-up, 44% of the PSM group achieved a clinically significant improvement in pain disability in comparison with 22% in the control group [69]. A weakening of effects was observed at the 1-year follow-up, but not to a significant degree, except for the Functional Reach scores [68]. The study by Paolucci et al. 2017 [72], which included a sample of 53 participants, found that a Back School self-management program and a Feldenkrais group intervention were comparable in efficacy in reducing pain and disability.
The study by Stoffer-Marx et al. 2018 [80], which compared the effects of an interdisciplinary intervention using an individual approach with routine care plus a placebo in patients with hand osteoarthritis, noted an increased grip strength and hand function in participants of the experimental group after 8 weeks, while a decrease in grip strength was observed in the control group participants. Tse et al. 2013 [83] showed that in a sample of 31 community-dwelling older persons with chronic pain, a program including motivational interviewing and physical exercise was associated with a significant reduction in pain, better physical mobility, psychological well-being, and self-efficacy in the experimental group compared to a control group. Vanhaudenhuyse et al. 2017 [85] compared the effects of two programs—psychoeducation combined with physiotherapy and self-hypnosis combined with self-care learning—with a no-intervention group. The results showed a significant positive effect of psychoeducation combined with physiotherapy on pain control and a significant positive effect of self-hypnosis combined with self-care on disability and pain. Both interventions were associated with higher utilization of active coping strategies.
All studies with a quasi-experimental design (n = 4) [37,46,47,48] reported positive effects of interdisciplinary self-management programs on several health-related variables. In a study with a sample of 78 participants with chronic pain, Dysvik et al. 2010 [48]; 2013 [46] found that a cognitive-behavioral pain management program had positive significant short-term effects on health-related quality of life, pain intensity and interference in daily life, readiness-to-change, and physical functioning measures. Dysvik et al. 2012 [47] also reported that significant positive results for pain intensity, quality of life, and readiness-to-change measures were maintained one year after the program and suggested that this could be explained by the 6- and 12-month follow-up sessions. The results from the study by Chao et al. 2019 [37] showed that a pain management program led to statistically significant improvements in pain interference, pain intensity, global mental health, and pain self-efficacy at 3 and 6 months, while no significant change was observed in the control group, except for improved physical functioning at 3 months.
3.6.2. Outcomes Reported from Pre–Post Studies
Pain Severity
Out of the 46 pre–post studies, 32 (69.6%) measured pain severity immediately after completion of the program. Of these, 20 studies reported a significant reduction in pain severity immediately post-intervention, 2 studies reported a positive tendency towards the reduction in pain severity, and 10 studies reported no significant effect on pain severity. Among the studies that reported significant reductions in pain severity in the short term (n = 6), 5 studies (83.3%) found that statistically significant effects were maintained in the mid–long term, while one study noted a significant decrease in the previously noted improvements. Of the studies that did not report significant effects on pain severity in the short term, one found significant reductions in pain severity in the mid–long term. Finally, all studies that only measured pain severity in the mid–long term (n = 4) reported significant reductions in pain severity. The most common tools used to measure pain severity were a visual analogue scale (61.1%) and a numerical rating scale (13.9%).
Pain Self-Efficacy
Out of the 46 pre–post studies, 8 (17.4%) measured pain self-efficacy immediately after completion of the program. Of these, seven studies (87.5%) reported significant improvements in pain self-efficacy immediately post-intervention, and one study reported no significant effects. Among the seven studies that did report significant improvements in pain self-efficacy immediately after the intervention, three also measured this outcome in the mid–long term. The latter studies all reported that significant improvements in pain self-efficacy were maintained in the mid–long term. Finally, all studies that only measured pain self-efficacy in the mid–long term (n = 2) reported significant positive effects. The most common tool used to measure this outcome was the Pain Self-Efficacy Questionnaire (n = 6; 60.0%).
Mental Health
Out of the 46 pre–post studies, 29 (63.0%) measured programs’ effects on mental health immediately after completion of the program. Of these, 23 studies (79.3%) reported significant improvements in mental health, 1 study reported a positive tendency towards the improvement of mental health, and 5 studies reported no significant effects. Of the 29 pre–post studies, 11 measured mental health in the mid–long term. Among the studies that reported significant improvements in mental health in the short term (n = 10), six studies (60.0%) found that statistically significant effects were maintained in the mid–long term, two studies noted a significant decrease in previously noted improvements, and two reported that the significant improvements previously noted were not maintained. Finally, two out of the three studies that only measured mental health in the mid–long term reported significant positive effects. The most common tools used to assess mental health were the Hospital Anxiety and Depression Scale (n = 10; 31.3%), the Depression Anxiety Stress Scales (n = 5; 15.6%), the Beck Depression Inventory-II (n = 5; 15.6%), and the Center for Epidemiological Studies Depression Scale (n = 4; 12.5%).
Physical Performance
Out of the 46 pre–post studies, 16 (34.8%) measured physical performance immediately after completion of the program. Of these, 13 studies (81.3%) reported significant improvements in physical performance immediately after the intervention, 1 study reported a positive tendency towards the improvement of physical performance, and 2 studies reported no significant effects. Of the 16 studies, 7 measured physical performance in the mid–long term. All the studies that reported a significant improvement of physical performance in the short term (n = 5) and measured physical performance at mid-long term showed that positive outcomes were maintained on this variable. Finally, all studies that only measured physical performance in the mid–long term (n = 3) reported significant positive effects. The most common tools used to measure physical performance were the physical component score of the 36-Item Short Form Survey (n = 7; 36.8%), the Six-Minute Walk Test (n = 6; 31.2%), the Stair Climb Test (n = 3; 15.8%), the Time Up and Go Test (n = 2; 10.5%), and the One Leg Stand Test (n = 2; 10.5%).
Daily Functioning
Out of the 46 pre–post studies, 34 (73.9%) measured daily functioning immediately after completion of the program. Of these, 27 (79.4%) reported significant improvements in daily functioning immediately post-intervention and 7 studies (20.6%) reported no significant positive effects. Among the 27 studies that did report significant improvements immediately post-intervention, 12 measured this outcome in the mid–long term. Of these, nine studies (75.0%) found that statistically significant effects were maintained in the mid–long term, one noted a significant decrease in previously noted improvements, and one study reported that the significant improvements previously noted were not maintained. Finally, all studies that only measured daily functioning in the mid–long term (n = 4) reported significant positive effects. The most common tools used to measure daily functioning were the Pain Disability Index (n = 10; 26.3%), the 36-Item Short Form Survey (n = 4; 10.5%), the Pain Disability Assessment Scale (n = 3; 7.9%), the Multidimensional Pain Inventory (n = 3; 7.9%), and the Brief Pain Inventory (n = 3; 7.9%).
Quality of Life
Out of the 46 pre–post studies, 8 (17.4%) measured quality of life immediately after completion of the program. Of these, four studies (50%) reported significant improvements in quality of life immediately post-intervention, one study noted a positive tendency towards the improvement of quality of life, and three studies (37.5%) reported no significant effects. All the studies that reported significant improvements in quality of life in the short term (n = 4) also assessed this outcome in the mid–long term. Of these, two studies (50.0%) found that this significant improvement in quality of life was maintained in the mid–long term, while two studies (50.0%) reported that this significant improvement was not maintained. Finally, the single study that only measured quality of life in the mid–long term reported significant positive effects. The most common tool used to measure this variable was the EuroQol-5D (n = 5; 55.6%).
3.7. Qualitative Findings
Five studies qualitatively investigated participants’ experience or self-reported outcomes in a self-management program [39,54,67,74,81]. They include one qualitative study [74] and four mixed-method studies [39,54,67,81]. First, Hapidou et al. 2016 [54] explored the experience of 50 older adults who participated in a Canadian self-management program based on a cognitive-behavioral approach. Participants reported that they had learned new coping strategies that facilitate living with their pain. They perceived that the program contributed to improving their mental health and understood they had to accept their condition and find ways to live with the pain rather than trying to cure it. Participants were planning to continue applying newly acquired skills after the program and were optimistic about their progress. In the study by Nam et al. 2014 [67], participants reported that their anxiety levels decreased after the completion of the program. They mentioned that expressing their difficulties in a group setting contributed to their well-being. In the study by Penney et al. 2019 [74], interviews and focus groups were conducted to better understand the experience of veterans who participated in an interdisciplinary chronic pain coaching program. Veterans described multiple areas of improvement, such as adopting new lifestyle habits (e.g., physical exercises, medication management, healthy nutrition). They reported feeling more in control of their pain (e.g., better at adjusting tasks and not pushing beyond their limits). However, a small portion of participants reported no improvement after the program; they were hopeless about the possibility that their condition may improve; they felt like they were “stuck” in the same place as before their participation. The results of the study by Craner et al. 2016 [39] were derived from open-ended questions after completion of the program and revealed that patients endorsed self-management strategies, particularly relaxation skills (85%); moderation and/or modification of activities (47%); and exercise, stretching, and/or physical therapy (39%) as the most important aspects of treatment. Finally, the study of Teo et al. (2017) conducted with patients living with fibromyalgia and professionals leading the program attested to the added value of an interdisciplinary approach to the treatment of chronic pain.
4. Discussion
The purpose of this scoping review was to synthesize the characteristics and effects of interdisciplinary chronic pain self-management interventions targeting community-dwelling older adults. Over 65% of the articles focused on heterogeneous populations, i.e., populations with pain caused by a variety of health conditions.
Surprisingly, only three articles included in this review specifically targeted adults aged 65 years or over. Fine 2009 [99] suggested that the social (e.g., greater risk of social isolation) and physiological (e.g., longer transit time of pharmaceutical agents) changes that occur with aging require clinicians working in chronic pain management to provide interventions specifically tailored for older adults [99]. Moreover, a qualitative study exploring the experience of older adults seeking treatment for chronic pain demonstrated that this experience was positive when older adults felt understood and heard and received patient-centered care [100]. This further supports the need to develop and evaluate chronic pain self-management programs that are designed specifically for older adults. This is of particular importance considering that the prevalence of chronic pain in people aged above 60 is twice that of younger people and that pain in the elderly often remains untreated and misdiagnosed [101].
The results of this scoping review show that chronic pain self-management programs are very heterogeneous. However, most of them are based on the cognitive-behavioral or the biopsychosocial model, which is consistent with scientific evidence recommending holistic approaches for the management of chronic pain for older adults [102,103]. In 2020, Miaskowski et al. developed an adaptation of the biopsychosocial model of chronic pain for older adults. This model should be of added value for the development of research study designs for this population, as it considers the interactions between many characteristics associated with older adults, ranging from agism to multimorbidity or social isolation [102].
The programs examined in this scoping review were varied in terms of delivery modes and components, but most of them included a group approach. In fact, it is reported that a group format allows opportunities for social support and creates a sense of belonging that can contribute to the general health and well-being of older adults [104,105]. The high prevalence of group interventions is also consistent with the adult learning theory. This theory suggests that educators should include group discussion as a teaching technique because it creates an opportunity for building on previous experiences and sharing them with others, resulting in faster and more effective learning [106]. Almost all programs included a combination of an educational component and training in self-management skills. This is consistent with the recommendations of the British Pain Society [32], which considered that information alone can improve understanding and knowledge but should be combined with practice in the use of self-management skills to better support behavior changes. Interestingly, many programs included strategies to encourage participants to practice and maintain learned skills. Because people tend to forget learned skills if they do not use them regularly, it is important to provide an opportunity to practice newly acquired skills as soon as possible [106]. Most programs with a combined approach included an individual pharmacological intervention. This is consistent with the literature, which suggests that a model that successfully integrates evidence-based biomedical and psychosocial advances should be considered for optimal health management [107].
4.1. Future Studies
The large variability of pain self-management programs and the limited number of studies about their efficacy for older adults living with chronic pain underline the need for more research in this field. Furthermore, since it is important that older adults identify with these programs, feel heard, and are able to contribute to the decision-making processes that concern them, we believe that a participatory approach should be used when developing and studying pain self-management programs. Research teams should also establish partnerships with clinicians with expertise in pain management, community or institutional organizations offering chronic pain self-management services, and relatives of older adults living with chronic pain. These partnerships are key ingredients for the development of relevant and feasible programs for older adults. Another important avenue for future research is to synthesize knowledge regarding the factors contributing to the successful implementation of chronic pain self-management programs among older adults.
4.2. Strengths and Limitations
One strength of this scoping review is the large number of included articles (n = 66), allowing for a comprehensive review of the available scientific literature. Also, many authors were contacted (n = 24) in the selection process when important information was missing in their article to determine their eligibility. Finally, during the process, key stakeholders from an interdisciplinary team of health professionals with clinical expertise with older adults suffering from chronic pain were consulted to ensure the relevance of the review for clinical practice. They guided the research team on the eligibility criteria and shared their opinions during the data extraction process. They also guided the decisions on how to present the results.
Given practical issues related to time and funding, we acknowledge that some methodological aspects can limit the breadth and comprehensiveness of this review. First, we limited our search to articles published after 2010. This timeframe allowed the restriction of the number of results from the search strategy. Also, we did not review the grey literature, although it can be included in scoping reviews and can also provide valuable information [29]. It is worth noting that many articles included in the present scoping review did indeed focus on interdisciplinary interventions, but often lacked specific details regarding the nature of collaboration among the disciplines involved. As a result, it became challenging to offer more extensive details regarding the nature of interdisciplinary relationships and collaborations. Future studies should aim to better describe the nature of interdisciplinarity, as it is also essential to understand how the dynamics of an interdisciplinary team can impact on the outcomes of self-management pain programs.
5. Conclusions
This scoping review integrates the available scientific literature about the characteristics and effects of interdisciplinary chronic pain self-management interventions targeting community-dwelling older adults. It reveals that chronic pain self-management programs are very heterogeneous and involve a wide variety of health professionals. Most programs are based on holistic approaches as recommended by the guidelines for chronic pain management. They used group approaches more frequently than individual approaches. Most of them combine an educational component, training in self-management skills, and a pharmacological component. Overall, the included articles reported positive effects of interdisciplinary chronic pain self-management on pain severity, pain self-efficacy, mental health, physical performance, daily functioning, and quality of life. Considering the aging population and the high prevalence of chronic pain and its impacts on older adults’ daily functioning, the development of chronic pain self-management programs tailored to this population—and their evaluation—should be a research priority in the coming years.
Author Contributions
Conceptualization, J.F. and M.-È.L.; methodology, J.F., M.-È.L., C.S., J.R., J.M., J.H., P.R., D.L., F.D., C.G., K.S., L.A. and M.V.; formal analysis, M.-È.L., J.F. and S.T.; writing—original draft preparation, S.T., M.-È.L., J.M. and J.F.; supervision of the study, J.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Programme d’appui à des projets de recherche stratégiques et structurants of the Centre de recherche de l’Institut universitaire de gériatrie de Montréal-CIUSSS du Centre-Sud-de-l’Île-de-Montréal. Samuel Turcotte is a fellow from the Canadian Strategy for Patient-Oriented Research of the Canadian Institutes of Health Research (SPOR-CIHR) (POR Award—Transition to Leadership Stream, 2023–2026). Marie-Ève Lapointe was supported by a PREMIER Undergraduate Research Scholarship from the Université de Montréal’s Faculty of Medicine.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data available on request.
Acknowledgments
The authors wish to thank Alain Tran for his contribution to the data extraction and validation phase of the scoping review and Yasmina Sleb for sharing ideas at the beginning of the project. Université de Montréal is situated on land where, long before the arrival of the French, people of many Indigenous nations came together and interacted. We wish to acknowledge these nations, their descendants, and the spirit of fraternity that presided over the signing in 1701 of the Great Peace of Montreal, a treaty that fostered peaceful relationships between France, its Indigenous allies, and the Haudenosaunee federation (pronunciation: O-di-no-sho-ni). The spirit of fraternity that inspired this treaty serves as a model for our own university community.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Table A1 details the characteristics of the programs examined in the selected studies. It presents the format of the programs, the health professionals involved, the topics addressed in the educational component of the programs, the self-management skills training of interest, and the physical exercises included or prescribed in the programs, when applicable.

Table A1.
Characteristics of the programs.
Table A1.
Characteristics of the programs.
| Authors, Year of Publication | Group Approach | Individual Approach | Individual Interventions | Group Interventions | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Health Professionals | Health Professionals | Educational Topics | Self-Management Skills Training | Physical Exercises | ||||||||||||||||||||||||||||
| Physician/Medicine Specialists | Occupational Therapists | Physiotherapists | Nurses | Psychologists | Other(s) | Physician/Medicine Specialists | Occupational Therapists | Physiotherapists | Nurses | Psychologists | Other(s) | Pain | Conventional Treatments | Effects of Physical Activity | Effect of Stress on Pain | Lifestyle Change/Nutrition | Other(s) | Relaxation Strategies | Cognitive Restructuring | Activity Pacing | Sleep Management | Problem-Solving Strategies | Communication and Interaction Skills | Mindfulness Skills | Identifying/Planning/Pursuing Goals | Other(s) | Floor Exercises 1 | Hydrotherapy | Movement-Based Therapy | |||
| Abbasi et al. 2012 [33] | • | • | • | • | • | • | • | • | • | Spinal cord anatomy | • | • | • | • | • | • | Strategies to request and give spousal assistance | • | ||||||||||||||
| Ajeganova et al. 2016 [34] | • | • | • | • | • | • | NS | NS | NS | NS | NS | • | • | • | • | • | ||||||||||||||||
| Anamkath et al. 2018 [35] | • | • | • | • | NS | NS | NS | NS | NS | NS | NS | NS | ||||||||||||||||||||
| Artner et al. 2012 [90] | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||
| Boosntra et al. 2015 [36] | • | • | • | • | • | • | S | • | • | • | • | S | Ergonomics | • | ||||||||||||||||||
| Claes et al. 2015 [38] | • | • | • | • | S, D | |||||||||||||||||||||||||||
| Craner et al. 2016 [39] | • | • | • | • | • | • | • | • | • | |||||||||||||||||||||||
| Darchuk et al. 2010 [40] | • | • | NS | NS | NS | NS | NS | • | • | • | • | • | • | OT for job, leisure, and home activities | ||||||||||||||||||
| Davies et al. 2011 [41] | • | • | • | • | • | • | • | • | • | Benefits of multimodal approach | • | • | • | Threat exposure | ||||||||||||||||||
| Davin et al. 2014 [42]: Wilt et al. 2016 [88] | • | • | • | • | • | S, C | • | S, C | • | |||||||||||||||||||||||
| Day et al. 2018 [43] | • | • | • | • | • | • | • | • | D | • | • | • | • | • | • | • | • | • | • | • | • | • | ACT, OT, use of aids if necessary | • | • | |||||||
| de la vega et al. 2019 [44] | • | • | • | • | • | Adaptative equipment, ergonomics | • | • | • | • | • | |||||||||||||||||||||
| De Rooij et al. 2013 [45] | • | • | • | • | • | • | S | • | • | • | • | S | • | • | • | • | • | • | Ergonomics | • | ||||||||||||
| Dysvik et al. 2010 [48]; 2012 [47]; 2013 [46] | • | • | • | • | • | D, peer leader | • | • | • | • | • | • | • | Strategies to improve self-esteem | • | |||||||||||||||||
| Fedoroff et al. 2014 [49] | • | NS | NS | NS | NS | NS | • | • | • | • | • | • | • | Strategies to manage emotions | • | |||||||||||||||||
| Gagnon et al. 2018 [50] | • | • | • | • | • | • | • | • | • | • | • | • | • | Laugh therapy, vocational counseling | • | • | ||||||||||||||||
| Hâllstam et al. 2016 [51] | • | • | • | • | • | • | • | • | • | • | NS | NS | NS | NS | NS | Body awareness therapy and other SMS (not specified) | • | • | ||||||||||||||
| Han et al. 2011 [52] | • | • | • | • | • | • | • | • | • | D, exercise physiologist | • | • | • | • | • | • | • | • | • | • | • | ACT, OT | ||||||||||
| Hansson et al. 2010 [53] | • | • | • | • | • | D | • | • | • | • | Orthopedic aids, ergonomics | |||||||||||||||||||||
| Hapidou et al. 2016 [54] | • | • | • | • | • | S, P, psychometrist | • | • | Vocational counseling, functional activity class | • | ||||||||||||||||||||||
| Hoogeboom et al. 2012 [55] | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||||||||||
| Huffman et al. 2017 [91] | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||||
| Inoue et al. 2014 [56] | • | • | • | • | D, trainer | • | Functional anatomy | • | • | • | Automatic thinking, pain awareness | • | • | |||||||||||||||||||
| Jongen et al. 2017 [57] | • | • | • | • | Dance therapist | • | Pain awareness | • | ||||||||||||||||||||||||
| Joypaul et al. 2019 [58] | • | • | • | • | • | P, D, exercise physiologist | • | • | • | • | • | • | • | |||||||||||||||||||
| Kowal et al. 2010 [60]; 2011 [92]; 2015 [59] | • | • | • | • | • | S | • | • | • | • | S | • | • | • | • | • | ||||||||||||||||
| Kurklinsky et al. 2016 [61] | • | • | • | • | • | • | • | • | • | • | • | fall prevention, body mechanics | • | • | • | • | • | • | • | Posture, distraction from pain | • | |||||||||||
| Marcus et al. 2014 [62] | • | • | • | • | • | NS | NS | NS | NS | NS | • | • | ||||||||||||||||||||
| Martin et al. 2012 [94]; 2014a [93]; 2014b [95]; 2014c [96] | • | • | NS | NS | NS | NS | NS | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||
| Martins et al. 2014 [63] | • | • | • | • | • | S | • | • | • | Ergonomics, how to perform ADLs | • | |||||||||||||||||||||
| McCabe et al. 2018 [64] | • | • | • | • | • | • | • | Discussion on spiritual and existential factors | • | |||||||||||||||||||||||
| McCormick et al. 2015 [65] | • | • | • | • | • | • | • | • | • | • | NS | NS | NS | NS | NS | • | • | • | Mirror therapy, desensitization techniques | • | • | • | ||||||||||
| Motoya et al. 2017 [66] | • | • | NS | NS | NS | NS | NS | • | • | • | • | • | • | • | • | Exposure | • | |||||||||||||||
| Nam et al. 2014 [67] | • | • | • | • | S, P, K | • | • | • | • | • | One peer-led session | • | ||||||||||||||||||||
| Nicholas et al. 2013 [69]; 2017 [68] | • | • | • | • | • | • | • | • | • | • | Discussion on fear-avoidance concept, exposure | • | ||||||||||||||||||||
| Nishie et al. 2018 [97] | • | • | • | • | • | |||||||||||||||||||||||||||
| Oh et al. 2010 [70] | • | • | • | • | • | • | • | • | • | • | • | Posture, body mechanics, work | ||||||||||||||||||||
| Oliver et al. 2017 [71] | • | • | • | • | • | • | Anatomy | • | • | • | • | • | • | |||||||||||||||||||
| Paolucci et al. 2017 [72] | • | • | • | • | • | Spinal anatomy, ergonomics for the spine | • | • | Ergonomics | • | ||||||||||||||||||||||
| Pate et al. 2019 [73] | • | • | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||||||
| Penney et al. 2019 [74] | • | • | • | • | • | S, clerks, chaplain | • | • | • | S, clerks, chaplain | • | • | • | ACT | • | |||||||||||||||||
| Ramke et al. 2016 [75] | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||||
| Ruscheweyh et al. 2015 [76] | • | • | • | • | • | • | • | |||||||||||||||||||||||||
| Shah et al. 2017 [77] | • | • | • | • | NS | NS | NS | NS | NS | • | Classes on mood management | |||||||||||||||||||||
| Slater et al. 2012 [78] | • | • | • | • | • | • | • | • | • | Benefits of multimodal approach | • | • | • | Threat exposure | ||||||||||||||||||
| Smeeding et al. 2011 [79] | • | • | • | • | • | P | • | • | D | • | • | • | ||||||||||||||||||||
| Stoffer-Marx et al. 2018 [80] | • | • | • | • | D | |||||||||||||||||||||||||||
| Stukstette et al. 2013 [98] | • | • | • | • | • | • | Ergonomics, joint protection principles | • | • | • | ||||||||||||||||||||||
| Teo et al. 2017 [81] | • | • | • | • | • | • | • | • | • | • | • | A single peer-led support group | ||||||||||||||||||||
| Tetsunaga et al. 2015 [82] | • | • | • | • | ||||||||||||||||||||||||||||
| Tse et al. 2013 [83] | • | • | • | • | • | • | • | • | Posture, motivational interviewing | • | ||||||||||||||||||||||
| Van Den Houte et al. 2017 [84] | • | • | • | • | • | • | • | • | • | • | • | • | Psychomotor therapy | • | ||||||||||||||||||
| Vanhaudenhuyse et al. 2017 [85] 2 | • | • | • | • | • | • | • | • | • | Spinal functional anatomy | • | Muscle awareness, proprioception | • | |||||||||||||||||||
| Vanhaudenhuyse et al. 2017 [85] 2 | • | • | • | Self-hypnosis and self-care learning | ||||||||||||||||||||||||||||
| Vincent et al. 2013 [86] | • | • | • | Exercise coach | • | • | • | • | • | • | • | • | ||||||||||||||||||||
| Waterschoot et al. 2015 [87] | • | • | • | • | • | |||||||||||||||||||||||||||
| Yang et al. 2010 [89] | • | • | • | • | Spinal anatomy and physiology | • | Posture | • | ||||||||||||||||||||||||
Legend: D: dietician/nutritionist; K: kinesiologist; P: pharmacist; S: social worker; C: counselor; ACT: acceptance and commitment therapy; ADLs: activities of daily living; OT: occupational therapy; NS: not specified. 1 Includes strengthening, aerobic, and/or stretching exercises. 2 A study of two separate interventions.
References
- Goldberg, D.S.; McGee, S.J. Pain as a global public health priority. BMC Public Health 2011, 11, 770. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Reitsma, M.L.; Tranmer, J.E.; Buchanan, D.M.; Vandenkerkhof, E.G. The prevalence of chronic pain and pain-related interference in the Canadian population from 1994 to 2008. Chronic Dis. Can. 2011, 31, 157–164. [Google Scholar] [CrossRef]
- Schopflocher, D.; Taenzer, P.; Jovey, R. The prevalence of chronic pain in Canada. Pain Res. Manag. 2011, 16, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Dahlhamer, J.; Lucas, J.; Zelaya, C.; Nahin, R.; Mackey, S.; DeBar, L.; Kerns, R.; Von Korff, M.; Porter, L.; Helmick, C. Prevalence of chronic pain and high impact chronic pain among adults. Morb. Mortal. Wkly. Rep. 2018, 67, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Chronic Pain in Canadian Seniors. Available online: https://www150.statcan.gc.ca/n1/pub/82-003-x/2008001/article/10514-eng.pdf (accessed on 12 December 2019).
- Duenas, M.; Ojeda, B.; Salazar, A.; Mico, J.A.; Failde, I. A review of chronic pain impact on patients, their social environment and the health care system. J. Pain Res. 2016, 9, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.V.; Guralnik, J.M.; Dansie, E.J.; Turk, D.C. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 national health and aging trends study. Pain 2013, 154, 2649–2657. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Kennedy, N.; Harmon, D. Constructing the experience of chronic pain through discourse. Scand. J. Occup. Ther. 2013, 20, 93–100. [Google Scholar] [CrossRef]
- Persson, E.; Lexell, J.; Rivano-Fischer, M.; Eklund, M. Everyday occupational problems perceived by participants in a pain rehabilitation programme. Scand. J. Occup. Ther. 2013, 20, 306–314. [Google Scholar] [CrossRef]
- Rochette, A.; Prefontaine, K. A literature review on chronic pain: The daily overcoming of a complex problem. Br. J. Occup. Ther. 2013, 76, 280–286. [Google Scholar]
- Ong, B.N.; Hooper, H.; Dunn, K.; Croft, P. Establishing self and meaning in low back pain narratives. Sociol. Rev. 2004, 52, 532–549. [Google Scholar] [CrossRef]
- Patel, S.; Greasley, K.; Watson, P.J. Barriers to rehabilitation and return to work for unemployed chronic pain patients: A qualitative study. Eur. J. Pain 2007, 11, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. CDC Guideline for Prescribing Opioids for Chronic Pain—United States. Morb. Mortal. Wkly. Rep. 2016, 65, 1–49. [Google Scholar]
- Gatchel, R.J.; McGeary, D.D.; McGeary, C.A.; Lippe, B. Interdisciplinary chronic pain management: Past, present, and future. Am. Psychol. 2014, 69, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Canadian Pain Task Force. Chronic Pain in Canada: Laying a Foundation for Action: A Report by the Canadian Pain Task Force; Health Canada: Ottawa, ON, Canada, 2019.
- Reid, M.C.; Eccleston, C.; Pillemer, K. Management of chronic pain in older adults. Br. Med. J. 2015, 350, h532. [Google Scholar] [CrossRef] [PubMed]
- Tick, H.; Nielsen, A.; Pelletier, K.R.; Bonakdar, R.; Simmons, S.; Glick, R.; Ratner, E.; Lemmon, R.L.; Wayne, P.; Zador, V.; et al. Evidence-Based Nonpharmacologic Strategies for Comprehensive Pain Care: The Consortium Pain Task Force White Paper. Explore 2018, 14, 177–211. [Google Scholar] [CrossRef] [PubMed]
- Mion, L.; Odegard, P.S.; Resnick, B.; Segal-Galan, F.; Geriatrics Interdisciplinary Advisory Group; American Geriatrics Society. Interdisciplinary care for older adults with complex needs: American Geriatrics Society position statement. J. Am. Geriatr. Soc. 2006, 54, 849–852. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient self-management of chronic disease in primary care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef]
- Bodenheimer, T.; Wagner, E.H.; Grumbach, K. Improving primary care for patients with chronic illness. JAMA 2002, 288, 1775–1779. [Google Scholar] [CrossRef]
- Panagioti, M.; Richardson, G.; Small, N.; Murray, E.; Rogers, A.; Kennedy, A.; Newman, S.; Bower, P. Self-management support interventions to reduce health care utilisation without compromising outcomes: A systematic review and metaanalysis. BMC Health Serv. Res. 2014, 14, 356. [Google Scholar] [CrossRef]
- Ory, M.G.; Ahn, S.; Jiang, L.; Lorig, K.; Ritter, P.; Laurent, D.D.; Whitelaw, N.; Smith, M.L. National study of chronic disease self-management: Six-month outcome findings. J. Aging Health 2013, 25, 1258–1274. [Google Scholar] [CrossRef]
- Sullivan, M.D.; Vowles, K.E. Patient action: As means and end for chronic pain care. Pain 2017, 158, 1405–1407. [Google Scholar] [CrossRef]
- Wagner, E.H. Chronic disease management: What will it take to improve care for chronic illness? Eff. Clin. Pract. 1998, 1, 2–4. [Google Scholar]
- Battersby, M.; Von Korff, M.; Schaefer, J.; Davis, C.; Ludman, E.; Green, S.M.; Parkerton, M.; Wagner, E.H. Twelve evidence-based principles for implementing self-management support in primary care. Jt. Comm. J. Qual. Patient Saf. 2010, 36, 561–570. [Google Scholar] [CrossRef]
- Kamper, S.J.; Apeldoorn, A.T.; Chiarotto, A.; Smeets, R.J.E.M.; Ostelo, R.W.J.G.; Guzman, J.; van Tulder, M.W. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. Br. Med. J. 2015, 350, h444. [Google Scholar] [CrossRef]
- Scascighini, L.; Toma, V.; Dober-Spielmann, S.; Sprott, H. Multidisciplinary treatment for chronic pain: A systematic review of interventions and outcomes. Rheumatology 2008, 47, 670–678. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping Studies: Advancing the Methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters MD, J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- British Pain Society. Guidelines for Pain Management Programmes for Adults: An Evidence-Based Review Prepared on Behalf of the British Pain Society. Available online: https://www.britishpainsociety.org (accessed on 5 June 2022).
- Abbasi, M.; Dehghani, M.; Keefe, F.J.; Jafari, H.; Behtash, H.; Shams, J. Spouse-assisted training in pain coping skills and the outcome of multidisciplinary pain management for chronic low back pain treatment: A 1-year randomized controlled trial. Eur. J. Pain 2012, 16, 1033–1043. [Google Scholar] [CrossRef]
- Ajeganova, S.; Wornert, M.; Hafstrom, I. A four-week team-rehabilitation programme in a warm climate decreases disability and improves health and body function for up to one year: A prospective study in Swedish patients with inflammatory joint diseases. J. Rehabil. Med. 2016, 48, 711–718. [Google Scholar] [CrossRef]
- Anamkath, N.S.; Palyo, S.A.; Jacobs, S.C.; Lartigue, A.; Schopmeyer, K.; Strigo, I.A. An Interdisciplinary Pain Rehabilitation Program for Veterans with Chronic Pain: Description and Initial Evaluation of Outcomes. Pain Res. Manag. 2018, 2018, 3941682. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Reneman, M.F.; Waaksma, B.R.; Schiphorst Preuper, H.R.; Stewart, R.E. Predictors of multidisciplinary treatment outcome in patients with chronic musculoskeletal pain. Disabil. Rehabil. 2015, 37, 1242–1250. [Google Scholar] [CrossRef] [PubMed]
- Chao, M.T.; Hurstak, E.; Leonoudakis-Watts, K.; Sidders, F.; Pace, J.; Hammer, H.; Wismer, B. Patient-reported outcomes of an integrative pain management program implemented in a primary care safety net clinic: A quasi-experimental study. J. Gen. Intern. Med. 2019, 34, 1105–1107. [Google Scholar] [CrossRef]
- Claes, B.E.A.; Leung, H.W.C.; Matters, K.; Williams, M.J.; Hunter, D.J. Interim analysis: An interdisciplinary team approach in facilitating weight reduction and improving function for people with knee or hip osteoarthritis. The Osteoarthritis Chronic Care Program at Royal North Shore Hospital. Nutr. Diet. 2015, 72, 232–239. [Google Scholar] [CrossRef]
- Craner, J.R.; Skipper, R.R.; Gilliam, W.P.; Morrison, E.J.; Sperry, J.A. Patients’ perceptions of a chronic pain rehabilitation program: Changing the conversation. Curr. Med. Res. Opin. 2016, 32, 879–883. [Google Scholar] [CrossRef] [PubMed]
- Darchuk, K.M.; Townsend, C.O.; Rome, J.D.; Bruce, B.K.; Hooten, W.M. Longitudinal treatment outcomes for geriatric patients with chronic non-cancer pain at an interdisciplinary pain rehabilitation program. Pain Med. 2010, 11, 1352–1364. [Google Scholar] [CrossRef]
- Davies, S.; Quintner, J.; Parsons, R.; Parkitny, L.; Knight, P.; Forrester, E.; Roberts, M.; Graham, C.; Visser, E.; Antill, T.; et al. Preclinic group education sessions reduce waiting times and costs at public pain medicine units. Pain Med. 2011, 12, 59–71. [Google Scholar] [CrossRef]
- Davin, S.; Wilt, J.; Covington, E.; Scheman, J. Variability in the relationship between sleep and pain in patients undergoing interdisciplinary rehabilitation for chronic pain. Pain Med. 2014, 15, 1043–1051. [Google Scholar] [CrossRef][Green Version]
- Day, M.A.; Brinums, M.; Craig, N.; Geffen, L.; Geffen, S.; Lovai, M.; Geffen, G. Predictors of Responsivity to Interdisciplinary Pain Management. Pain Med. 2018, 19, 1848–1861. [Google Scholar] [CrossRef]
- de la Vega, R.; Racine, M.; Castarlenas, E.; Sole, E.; Roy, R.; Jensen, M.P.; Miro, J.; Cane, D. The Role of Sleep Quality and Fatigue on the Benefits of an Interdisciplinary Treatment for Adults With Chronic Pain. Pain Pract. 2019, 19, 354–362. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, A.; van der Leeden, M.; Roorda, L.D.; Steultjens, M.P.; Dekker, J. Predictors of outcome of multidisciplinary treatment in chronic widespread pain: An observational study. BMC Musculoskelet. Disord. 2013, 14, 133. [Google Scholar] [CrossRef]
- Dysvik, E.; Kvaløy, J.T.; Furnes, B. Evaluating physical functioning as part of a Cognitive Behavioural Therapy approach in treatment of people suffering from chronic pain. J. Clin. Nurs. 2013, 22, 806–816. [Google Scholar] [CrossRef]
- Dysvik, E.; Kvaloy, J.T.; Natvig, G.K. The effectiveness of an improved multidisciplinary pain management programme: A 6- and 12-month follow-up study. J. Adv. Nurs. 2012, 68, 1061–1072. [Google Scholar] [CrossRef] [PubMed]
- Dysvik, E.; Kvaløy, J.T.; Stokkeland, R.; Natvig, G.K. The effectiveness of a multidisciplinary pain management programme managing chronic pain on pain perceptions, health-related quality of life and stages of change—A non-randomized controlled study. Int. J. Nurs. Stud. 2010, 47, 826–835. [Google Scholar] [CrossRef]
- Fedoroff, I.C.; Blackwell, E.; Speed, B. Evaluation of group and individual change in a multidisciplinary pain management program. Clin. J. Pain 2014, 30, 399–408. [Google Scholar] [CrossRef]
- Gagnon, C.M.; Scholten, P.; Atchison, J. Multidimensional Patient Impression of Change Following Interdisciplinary Pain Management. Pain Pract. 2018, 18, 997–1010. [Google Scholar] [CrossRef] [PubMed]
- Hallstam, A.; Lofgren, M.; Svensen, C.; Stalnacke, B.M. Patients with chronic pain: One-year follow-up of a multimodal rehabilitation programme at a pain clinic. Scand. J. Pain 2016, 10, 36–42. [Google Scholar] [CrossRef]
- Han, X.; Geffen, S.; Browning, M.; Kenardy, J.; Geffen, G. Outcome evaluation of a multidisciplinary pain management programme comparing group with individual change measures. Clin. Psychol. 2011, 15, 133–138. [Google Scholar] [CrossRef]
- Hansson, E.E.; Jönsson-Lundgren, M.; Ronnheden, A.M.; Sörensson, E.; Bjärnung, Å.; Dahlberg, L.E. Effect of an education programme for patients with osteoarthritis in primary care—A randomized controlled trial. BMC Musculoskelet. Disord. 2010, 11, 244. [Google Scholar] [CrossRef]
- Hapidou, E.G.; Horst, E. Learning to Manage Chronic Pain: The Patients’ Perspective. Pain Ther. 2016, 5, 93–105. [Google Scholar] [CrossRef][Green Version]
- Hoogeboom, T.J.; Kwakkenbos, L.; Rietveld, L.; Den Broeder, A.A.; De Bie, R.A.; Van Den Ende, C.H.M. Feasibility and potential effectiveness of a non-pharmacological multidisciplinary care programme for persons with generalised osteoarthritis: A randomised, multiple-baseline single-case study. BMJ Open 2012, 2, e001161. [Google Scholar] [CrossRef]
- Inoue, M.; Inoue, S.; Ikemoto, T.; Arai, Y.-C.P.; Nakata, M.; Miyazaki, A.; Nishihara, M.; Kawai, T.; Hatakeyama, N.; Yamaguchi, S.; et al. The efficacy of a multidisciplinary group program for patients with refractory chronic pain. Pain Res. Manag. 2014, 19, 302–308. [Google Scholar] [CrossRef][Green Version]
- Jongen, P.J.; Ruimschotel, R.P.; Museler-Kreijns, Y.M.; Dragstra, T.M.C.; Duyverman, L.; Valkenburg-Vissers, J.; Hartog, A. mproved health-related quality of life, participation, and autonomy in patients with treatment-resistant chronic pain after an intensive social cognitive intervention with the participation of support partners. J. Pain Res. 2017, 10, 2725. [Google Scholar] [CrossRef]
- Joypaul, S.; Kelly, F.S.; King, M.A. Turning Pain into Gain: Evaluation of a Multidisciplinary Chronic Pain Management Program in Primary Care. Pain Med. 2019, 20, 925–933. [Google Scholar] [CrossRef]
- Kowal, J.; McWilliams, L.; Péloquin, K.; Wilson, K.; Henderson, P.; Fergusson, D. Attachment insecurity predicts responses to an interdisciplinary chronic pain rehabilitation program. J. Behav. Med. 2015, 38, 518–526. [Google Scholar] [CrossRef]
- Kowal, J.; Wilson, K.G.; Corace, K.; Henderson, P.R.; D’Eon, J.L. Patient and clinician global ratings of change following interdisciplinary treatment for chronic pain. J. Pain Manag. 2010, 3, 159–170. [Google Scholar]
- Kurklinsky, S.; Perez, R.B.; Lacayo, E.R.; Sletten, C.D. The Efficacy of Interdisciplinary Rehabilitation for Improving Function in People with Chronic Pain. Pain Res. Treat. 2016, 2016, 7217684. [Google Scholar] [CrossRef]
- Marcus, D.A.; Bernstein, C.D.; Haq, A.; Breuer, P. Including a Range of Outcome Targets Offers a Broader View of Fibromyalgia Treatment Outcome: Results from a Retrospective Review of Multidisciplinary Treatment. Musculoskelet. Care 2014, 12, 74–81. [Google Scholar] [CrossRef]
- Martins, M.R.; Gritti, C.C.; dos Santos Junior, R.; de Araujo, M.C.; Dias, L.C.; Foss, M.H.; de Andrade, L.B.; Rocha, C.E. Randomized controlled trial of a therapeutic intervention group in patients with fibromyalgia syndrome. Rev. Bras. Reumatol. 2014, 54, 179–184. [Google Scholar] [CrossRef]
- McCabe, R.; Murray, R.; Austin, P.; Siddall, P. Spiritual and existential factors predict pain relief in a pain management program with a meaning-based component. J. Pain Manag. 2018, 11, 163–170. [Google Scholar]
- McCormick, Z.L.; Gagnon, C.M.; Caldwell, M.; Patel, J.; Kornfeld, S.; Atchison, J.; Stanos, S.; Harden, R.N.; Calisoff, R. Short-Term Functional, Emotional, and Pain Outcomes of Patients with Complex Regional Pain Syndrome Treated in a Comprehensive Interdisciplinary Pain Management Program. Pain Med. 2015, 16, 2357–2367. [Google Scholar] [CrossRef] [PubMed]
- Motoya, R.; Otani, K.; Nikaido, T.; Ono, Y.; Matsumoto, T.; Yamagishi, R.; Yabuki, S.; Konno, S.I.; Niwa, S.I.; Yabe, H. Short-term effect of back school based on cognitive behavioral therapy involving multidisciplinary collaboration. Fukushima J. Med. Sci. 2017, 63, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.; Tin, D.; Bain, L.; Thorne, J.C.; Ginsburg, L. Clinical utility of the Hospital Anxiety and Depression Scale (HADS) for an outpatient fibromyalgia education program. Clin. Rheumatol. 2014, 33, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, M.K.; Asghari, A.; Blyth, F.M.; Wood, B.M.; Murray, R.; McCabe, R.; Brnabic, A.; Beeston, L.; Corbett, M.; Sherrington, C.; et al. Long-term outcomes from training in self-management of chronic pain in an elderly population: A randomized controlled trial. Pain 2017, 158, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, M.K.; Asghari, A.; Blyth, F.M.; Wood, B.M.; Murray, R.; McCabe, R.; Overton, S. Self-management intervention for chronic pain in older adults: A randomised controlled trial. Pain 2013, 154, 824–835. [Google Scholar] [CrossRef] [PubMed]
- Oh, T.H.; Stueve, M.H.; Hoskin, T.L.; Luedtke, C.A.; Vincent, A.; Moder, K.G.; Thompson, J.M. Brief interdisciplinary treatment program for fibromyalgia: Six to twelve months outcome. Am. J. Phys. Med. Rehabil. 2010, 89, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Oliver, S.; Fisher, K.; Childs, S. What psychological and physical changes predict patients’ attainment of personally meaningful goals six months following a CBT based pain management intervention? Disabil. Rehabil. 2017, 39, 2308–2314. [Google Scholar] [CrossRef]
- Paolucci, T.; Zangrando, F.; Iosa, M.; De Angelis, S.; Marzoli, C.; Piccinini, G.; Saraceni, V.M. Improved interoceptive awareness in chronic low back pain: A comparison of Back school versus Feldenkrais method. Disabil. Rehabil. 2017, 39, 994–1001. [Google Scholar] [CrossRef]
- Pate, J.W.; Veage, S.; Lee, S.; Hancock, M.J.; Hush, J.M.; Pacey, V. Which Patients With Chronic Pain Are More Likely to Improve Pain Biology Knowledge Following Education? Pain Pract. 2019, 19, 363–369. [Google Scholar] [CrossRef]
- Penney, L.S.; Haro, E. Qualitative evaluation of an interdisciplinary chronic pain intervention: Outcomes and barriers and facilitators to ongoing pain management. J. Pain Res. 2019, 12, 865–878. [Google Scholar] [CrossRef]
- Ramke, S.; Sharpe, L.; Newton-John, T. Adjunctive cognitive behavioural treatment for chronic pain couples improves marital satisfaction but not pain management outcomes. Eur. J. Pain 2016, 20, 1667–1677. [Google Scholar] [CrossRef] [PubMed]
- Ruscheweyh, R.; Dany, K.; Marziniak, M.; Gralow, I. Basal Pain Sensitivity does not Predict the Outcome of Multidisciplinary Chronic Pain Treatment. Pain Med. 2015, 16, 1635–1642. [Google Scholar] [CrossRef]
- Shah, A.; Craner, J.; Cunningham, J.L. Medical cannabis use among patients with chronic pain in an interdisciplinary pain rehabilitation program: Characterization and treatment outcomes. J. Subst. Abus. Treat. 2017, 77, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Slater, H.; Briggs, A.M.; Bunzli, S.; Davies, S.J.; Smith, A.J.; Quintner, J.L. Engaging consumers living in remote areas of Western Australia in the self-management of back pain: A prospective cohort study. BMC Musculoskelet. Disord. 2012, 13, 69. [Google Scholar] [CrossRef] [PubMed]
- Smeeding, S.J.; Bradshaw, D.H.; Kumpfer, K.L.; Trevithick, S.; Stoddard, G.J. Outcome evaluation of the Veterans Affairs Salt Lake City Integrative Health Clinic for Chronic Nonmalignant Pain. Clin. J. Pain 2011, 27, 146–155. [Google Scholar] [CrossRef]
- Stoffer-Marx, M.A.; Klinger, M.; Luschin, S.; Meriaux-Kratochvila, S.; Zettel-Tomenendal, M.; Nell-Duxneuner, V.; Zwerina, J.; Kjeken, I.; Hackl, M.; Ohlinger, S.; et al. Functional consultation and exercises improve grip strength in osteoarthritis of the hand—A randomised controlled trial. Arthritis Res. Ther. 2018, 20, 253. [Google Scholar] [CrossRef]
- Teo, M.; Mohan, B.; Oelke, N.D. Developing and Implementing a Community-Based Model of Care for Fibromyalgia: A Feasibility Study. Pain Res. Manag. 2017, 2017, 4521389. [Google Scholar] [CrossRef] [PubMed]
- Tetsunaga, T.; Tetsunaga, T.; Nishie, H.; Ozaki, T. Establishment of a liaison clinic for patients with intractable chronic pain. J. Orthop. Sci. 2015, 20, 907–913. [Google Scholar] [CrossRef]
- Tse, M.M.Y.; Wan, V.T.C.; Vong, S.K.S. Health-related profile and quality of life among nursing home residents: Does pain matter? Pain Manag. Nurs. 2013, 14, e173–e184. [Google Scholar] [CrossRef]
- Van Den Houte, M.; Luyckx, K.; Van Oudenhove, L.; Bogaerts, K.; Van Diest, I.; De Bie, J.; Van den Bergh, O. Differentiating progress in a clinical group of fibromyalgia patients during and following a multicomponent treatment program. J. Psychosom. Res. 2017, 98, 47–54. [Google Scholar] [CrossRef]
- Vanhaudenhuyse, A.; Gillet, A.; Malaise, N.; Salamun, I.; Grosdent, S.; Maquet, D.; Nyssen, A.S.; Faymonville, M.E. Psychological interventions influence patients’ attitudes and beliefs about their chronic pain. J. Tradit. Complement. Med. 2017, 8, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.; Whipple, M.O.; Oh, T.H.; Guderian, J.A.; Barton, D.L.; Luedtke, C.A. Early experience with a brief, multimodal, multidisciplinary treatment program for fibromyalgia. Pain Manag. Nurs. 2013, 14, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Waterschoot, F.P.C.; Dijkstra, P.U.; Geertzen, J.H.B.; Reneman, M.F. Course of disability reduction during a pain rehabilitation program: A prospective clinical study. Int. J. Rehabil. Res. 2015, 38, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Wilt, J.A.; Davin, S.; Scheman, J. A multilevel path model analysis of the relations between sleep, pain, and pain catastrophizing in chronic pain rehabilitation patients. Scand. J. Pain. 2016, 10, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Yang, E.J.; Park, W.B.; Shin, H.I.; Lim, J.Y. The effect of back school integrated with core strengthening in patients with chronic low-back pain. Am. J. Phys. Med. Rehabil. 2010, 89, 744–754. [Google Scholar] [CrossRef]
- Artner, J.; Kurz, S.; Cakir, B.; Reichel, H.; Lattig, F. Intensive interdisciplinary outpatient pain management program for chronic back pain: A pilot study. J. Pain Res. 2012, 5, 209–216. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huffman, K.L.; Rush, T.E.; Fan, Y.; Sweis, G.W.; Vij, B.; Covington, E.C.; Scheman, J.; Mathews, M. Sustained improvements in pain, mood, function and opioid use post interdisciplinary pain rehabilitation in patients weaned from high and low dose chronic opioid therapy. Pain 2017, 158, 1380–1394. [Google Scholar] [CrossRef] [PubMed]
- Kowal, J.; Wilson, K.G.; Geck, C.M.; Henderson, P.R.; D’Eon, J.L.; Kowal, J.; Wilson, K.G.; Geck, C.M.; Henderson, P.R.; D’Eon, J.L. Changes in perceived pain severity following interdisciplinary treatment for chronic pain. Pain Res. Manag. 2011, 16, 451–456. [Google Scholar] [CrossRef]
- Martin, J.; Torre, F.; Aguirre, U.; Gonzalez, N.; Padierna, A.; Matellanes, B.; Quintana, J.M. Evaluation of the interdisciplinary PSYMEPHY treatment on patients with fibromyalgia: A randomized control trial. Pain Med. 2014, 15, 682–691. [Google Scholar] [CrossRef]
- Martin, J.; Torre, F.; Padierna, A.; Aguirre, U.; Gonzalez, N.; Garcia, S.; Matellanes, B.; Quintana, J.M. Six-and 12-month follow-up of an interdisciplinary fibromyalgia treatment programme: Results of a randomised trial. Clin. Exp. Rheumatol. 2012, 30, 103–111. [Google Scholar] [PubMed]
- Martin, J.; Torre, F.; Padierna, A.; Aguirre, U.; González, N.; Matellanes, B.; Quintana, J.M. Interdisciplinary Treatment of Patients with Fibromyalgia: Improvement of Their Health-Related Quality of Life. Pain Pract. 2014, 14, 721–731. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Torre, F.; Padierna, A.; Aguirre, U.; González, N.; Matellanes, B.; Quintana, J.M. Impact of interdisciplinary treatment on physical and psychosocial parameters in patients with fibromyalgia: Results of a randomised trial. Int. J. Clin. Pract. 2014, 68, 618–627. [Google Scholar] [CrossRef] [PubMed]
- Nishie, H.; Tetsunaga, T.; Kanzaki, H.; Oda, K.; Inoue, S.; Ryuo, Y.; Ota, H.; Miyawaki, T.; Arakawa, K.; Tetsunaga, T.; et al. A Multidisciplinary Approach to the Management of Chronic Pain through a Self-managed Behavioral Exercise Program: A Pilot Study in Japan. Acta Medica Okayama 2018, 72, 343–350. [Google Scholar] [CrossRef]
- Stukstette, M.J.; Dekker, J.; Den Broeder, A.A.; Noort Van Der Laan, W.; Bijlsma, J.W.; Van Den Ende, C.H. No evidence for the effectiveness of a multidisciplinary group based treatment program in patients with osteoarthritis of hands on the short term; results of a randomized controlled trial. Osteoarthr. Cartil. 2013, 21, 901–910. [Google Scholar] [CrossRef] [PubMed]
- Fine, P.G. Chronic pain management in older adults: Special considerations. J. Pain Symptom Manag. 2009, 38, S4–S14. [Google Scholar] [CrossRef] [PubMed]
- Teh, C.F.; Karp, J.F.; Kleinman, A.; Reynolds III, C.F.; Weiner, D.K.; Cleary, P.D. Older people’s experiences of patient-centered treatment for chronic pain: A qualitative study. Pain Med. 2009, 10, 521–530. [Google Scholar] [CrossRef]
- Noroozian, M.; Raeesi, S.; Hashemi, R.; Khedmat, L.; Vahabi, Z. Pain: The neglect issue in old people’s life. Open Access Maced. J. Med. Sci. 2018, 6, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Miaskowski, C.; Blyth, F.; Nicosia, F.; Haan, M.; Keefe, F.; Smith, A.; Ritchie, C. A biopsychosocial model of chronic pain for older adults. Pain Med. 2020, 21, 1793–1805. [Google Scholar] [CrossRef]
- Lagueux, E.; Dépelteau, A.; Masse, J. Occupational therapy’s unique contribution to chronic pain management: A scoping review. Pain Res. Manag. 2018, 2018, 5378451. [Google Scholar] [CrossRef]
- Walumbe, J.; Belton, J.; Denneny, D. Pain management programmes via video conferencing: A rapid review. Scand. J. Pain 2021, 21, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Villagomez, P.; Zurlini, C.; Wimmer, M.; Roberts, L.; Trieu, B.; McGrath, B.; Wiesel, R.; Ologhobo, T.; Goldsmith, S.; Robbins, L. Shift to virtual self-management programs during COVID-19: Ensuring access and efficacy for older adults. Front. Public Health 2021, 9, 663875. [Google Scholar] [CrossRef] [PubMed]
- Merriam, S.B. Adult learning theory: Evolution and future directions. In Contemporary Theories of Learning; Routledge: London, UK, 2018; pp. 83–96. [Google Scholar]
- Farre, A.; Rapley, T. The New Old (and Old New) Medical Model: Four Decades Navigating the Biomedical and Psychosocial Understandings of Health and Illness. Healthcare 2017, 5, 88. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).