A Mobile App for Chronic Disease Self-Management for Individuals with Low Health Literacy: A Multisite Randomized Controlled Clinical Trial
Abstract
1. Introduction
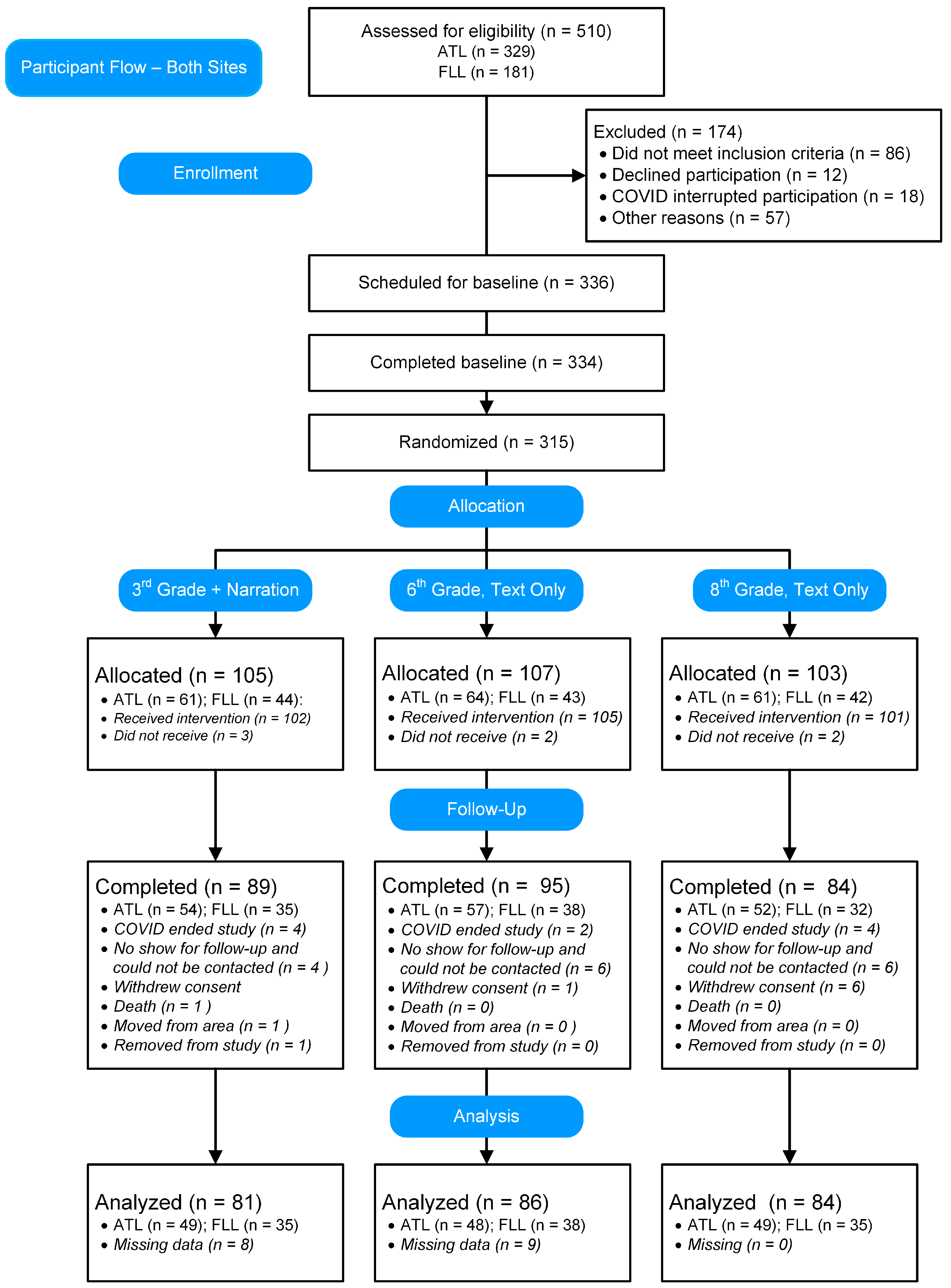
2. Materials and Methods
2.1. Development
2.2. Participants
2.3. Screening
2.4. Inclusion and Exclusion Criteria
2.5. Measures
2.6. Outcomes
2.7. Procedures
2.8. Human Subjects Approval
2.9. Statistical Analyses
2.9.1. Sample Size
2.9.2. Evaluation of Minimal Clinically Important Difference (MCID)
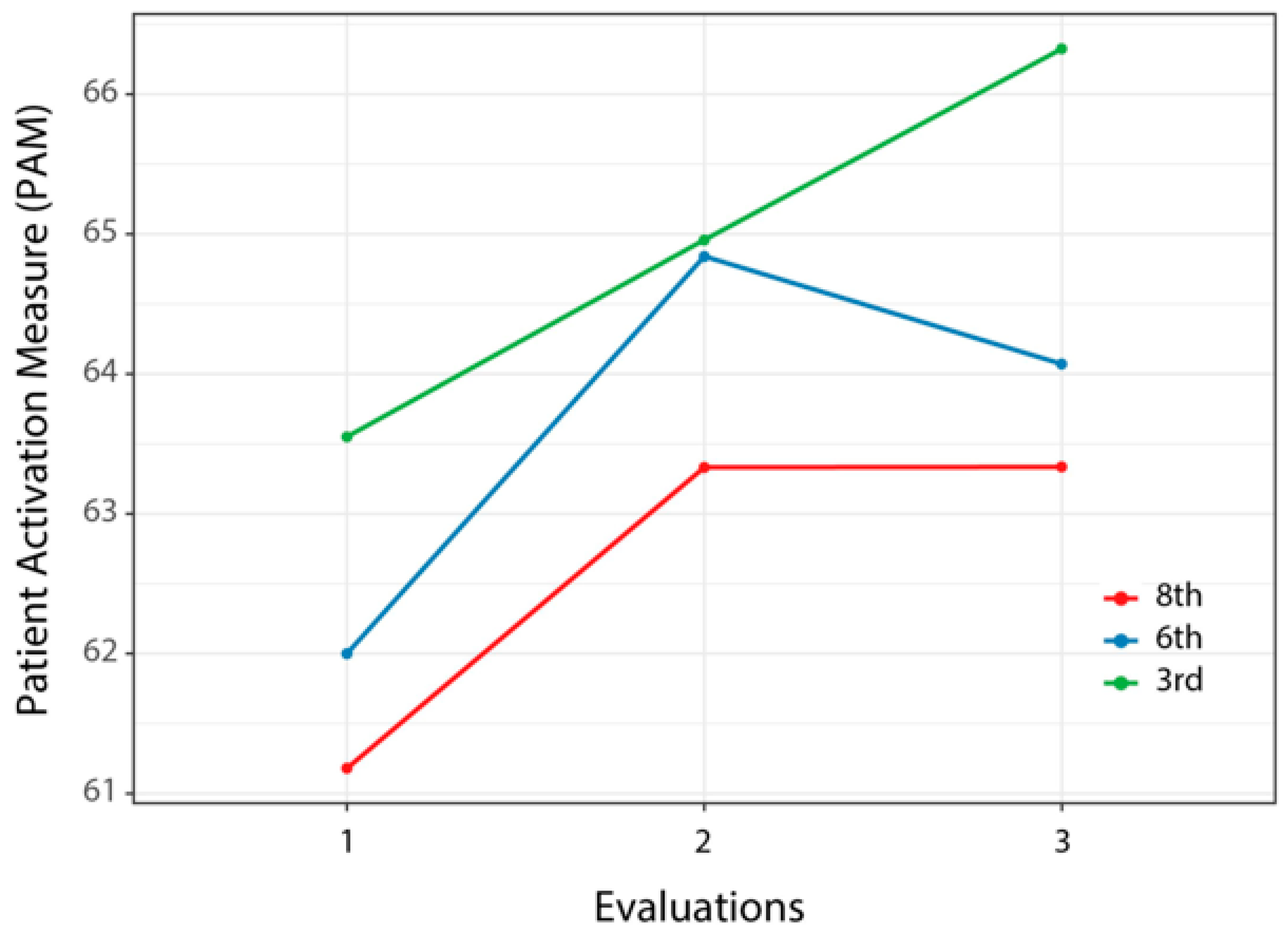
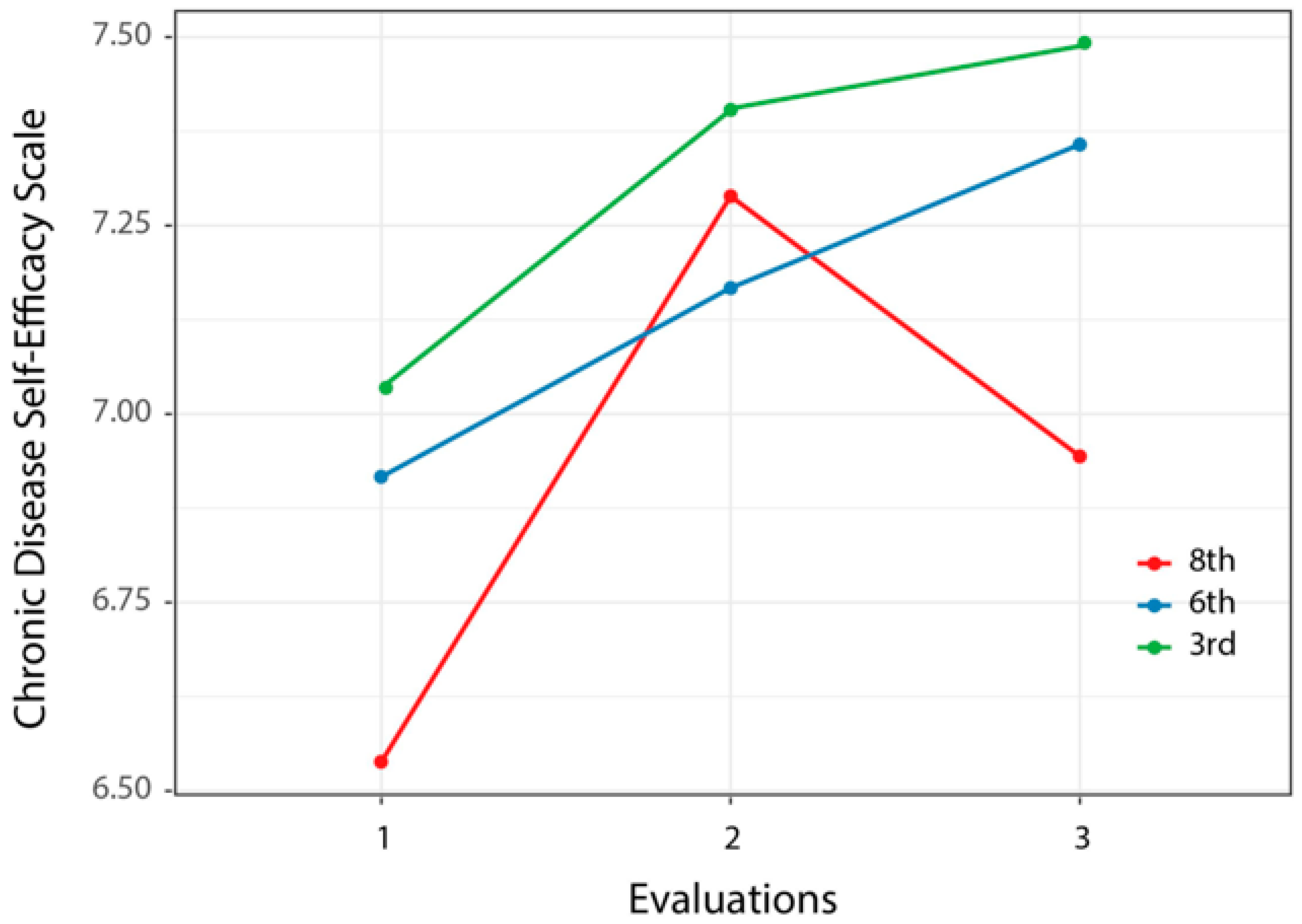
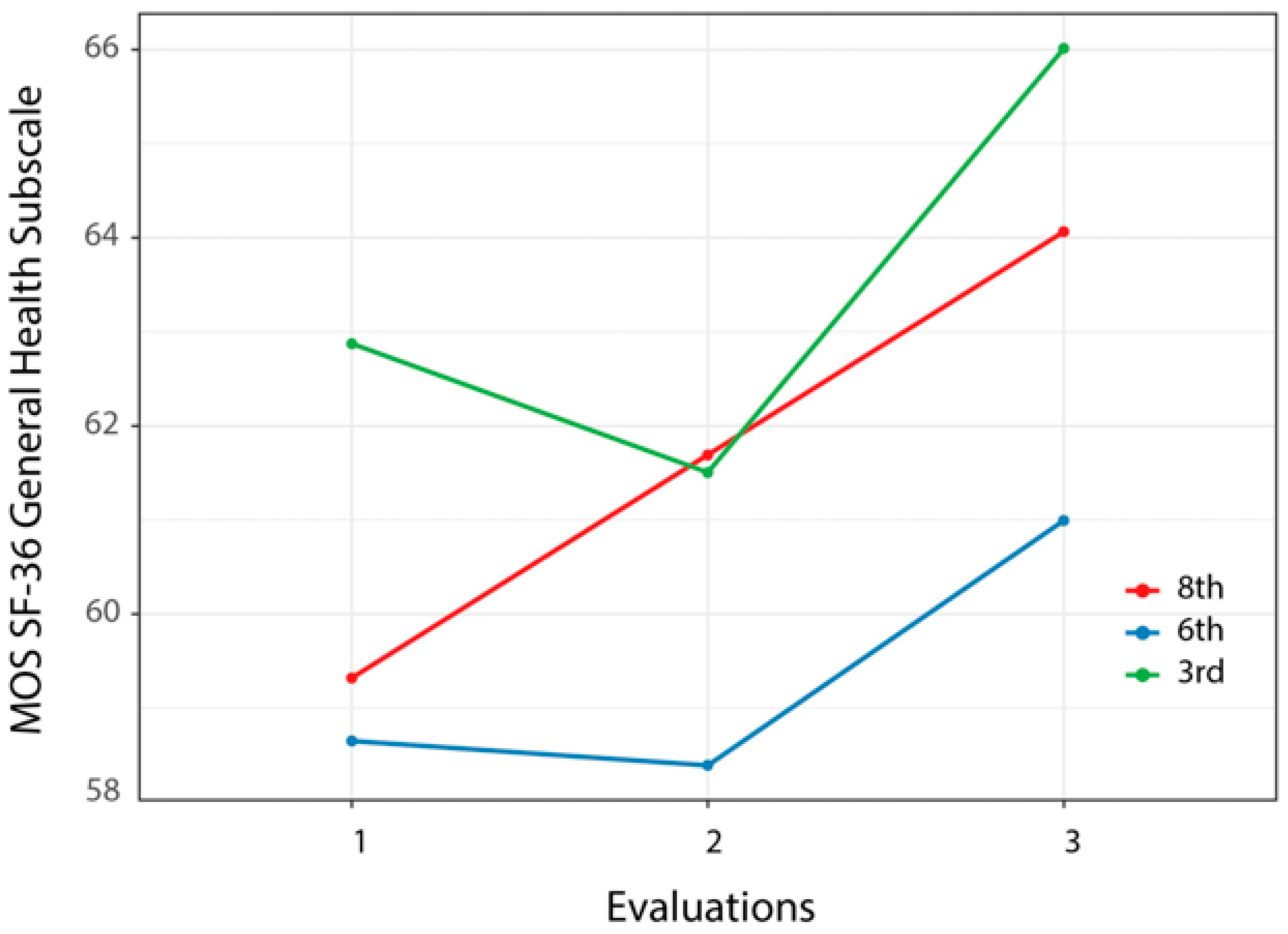
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- US Department of Health and Human Services. Healthy People 2030: Health Literacy; Department of Health and Human Services: Washington, DC, USA, 2023. Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/health-literacy (accessed on 13 September 2023).
- Kutner, M.; Greenberg, E.; Jin, Y.; Paulsen, C. The Health Literacy of America’s Adults: Results from the 2003 National Asessment of Adult Literacy (NCES 2006-483); US Department of Education, National Center for Educational Statistics: Washington, DC, USA, 2006. [Google Scholar]
- OECD. OECD Skills Outlook 2013: First Results from the Survey of Adults Skills; OECD Publishing: Paris, France, 2013.
- National Center for Educational Statistics. US Adults with Low Literacy and Numeracy Skills: 2012/2014 to 2017; National Center for Educational Statistics: Washington, DC, USA, 2022.
- Baccolini, V.; Rosso, A.; Di Paolo, C.; Isonne, C.; Salerno, C.; Migliara, G.; Prencipe, G.P.; Massimi, A.; Marzuillo, C.; De Vito, C.; et al. What is the prevalence of low health literacy in European Union member states? A systematic review and meta-analysis. J. Gen. Intern. Med. 2021, 36, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Canadian Council on Learning. Health Literacy in Canada: A Healthy Understanding; Canadian Council on Learning: Ottawa, ON, Canada, 2008. [Google Scholar]
- Adekoya-Cole, T.O.; Akinmokun, O.I.; Enweluzo, G.O.; Badmus, O.O.; Alabi, E.O. Poor health literacy in Nigeria: Causes, consequences and measures to improve it. Niger. Q. J. Hosp. Med. 2015, 25, 112–117. [Google Scholar]
- Paasche-Orlow, M.K.; Wolf, M.S. Promoting health literacy research to reduce health disparities. J. Health Commun. 2010, 15 (Suppl. S2), 34–41. [Google Scholar] [CrossRef] [PubMed]
- Stormacq, C.; Van den Broucke, S.; Wosinski, J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot. Int. 2019, 34, e1–e17. [Google Scholar] [CrossRef] [PubMed]
- Mantwill, S.; Monestel-Umana, S.; Schulz, P.J. The relationship between health literacy and health disparities: A systematic review. PLoS ONE 2015, 10, e0145455. [Google Scholar] [CrossRef]
- Pignone, M.; Dewalt, D.A.; Sheridan, S.; Berkman, N.; Lohr, K.N. Interventions to improve health outcomes for patients with low literacy. A systematic review. J. Gen. Intern. Med. 2005, 20, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Bo, A.; Friis, K.; Osborne, R.H.; Maindal, H.T. National indicators of health literacy: Ability to understand health information and to engage actively with healthcare providers—A population-based survey among Danish adults. BMC Public Health 2014, 14, 1095. [Google Scholar] [CrossRef] [PubMed]
- Osborn, C.Y.; Cavanaugh, K.; Wallston, K.A.; Kripalani, S.; Elasy, T.A.; Rothman, R.L.; White, R.O. Health literacy explains racial disparities in diabetes medication adherence. J. Health Commun. 2011, 16 (Suppl. S3), 268–278. [Google Scholar] [CrossRef]
- Osborn, C.Y.; Cavanaugh, K.; Wallston, K.A.; White, R.O.; Rothman, R.L. Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control. Diabetes Care 2009, 32, 1614–1619. [Google Scholar] [CrossRef]
- Osborn, C.Y.; Paasche-Orlow, M.K.; Bailey, S.C.; Wolf, M.S. The mechanisms linking health literacy to behavior and health status. Am. J. Health Behav. 2011, 35, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Osborn, C.Y.; Paasche-Orlow, M.K.; Davis, T.C.; Wolf, M.S. Health literacy: An overlooked factor in understanding HIV health disparities. Am. J. Prev. Med. 2007, 33, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Waldrop-Valverde, D.; Osborn, C.Y.; Rodriguez, A.; Rothman, R.L.; Kumar, M.; Jones, D.L. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010, 14, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, G.; Protheroe, J.; Winkley, J.; Richardson, M.; Seed, P.T.; Rudd, R. A mismatch between population health literacy and the complexity of health information: An observational study. Br. J. Gen. Pract. 2015, 65, e379–e386. [Google Scholar] [CrossRef] [PubMed]
- Kessels, R.P.C. Patients’ memory for medical information. J. R. Soc. Med. 2003, 96, 219–222. [Google Scholar] [PubMed]
- Kravitz, R.L.; Hays, R.D.; Sherbourne, C.D.; DiMatteo, M.R.; Rogers, W.H.; Ordway, L.; Greenfield, S. Recall of recommendations and adherence to advice among patients with chronic medical conditions. Arch. Intern. Med. 1993, 153, 1869–1878. [Google Scholar] [CrossRef]
- Vinker, S.; Eliyahu, V.; Yaphe, J. The effect of drug information leaflets on patient behavior. Isr. Med. Assoc. J. 2007, 9, 383–386. [Google Scholar] [PubMed]
- Herber, O.R.; Gies, V.; Schwappach, D.; Thurmann, P.; Wilm, S. Patient information leaflets: Informing or frightening? A focus group study exploring patients’ emotional reactions and subsequent behavior towards package leaflets of commonly prescribed medications in family practices. BMC Fam. Pract. 2014, 15, 163. [Google Scholar] [CrossRef] [PubMed]
- Kreuter, M.; Farrell, D.; Olevitch, L.; Brennan, L. Tailoring Health Messages; Lawrence Erlbaum: Mahwah, NJ, USA, 2000. [Google Scholar]
- Schapira, M.M.; Swartz, S.; Ganschow, P.S.; Jacobs, E.A.; Neuner, J.M.; Walker, C.M.; Fletcher, K.E. Tailoring educational and behavioral interventions to level of health literacy: A systematic review. MDM Policy Pract. 2017, 2. [Google Scholar] [CrossRef]
- Taggart, J.; Williams, A.; Dennis, S.; Newall, A.; Shortus, T.; Zwar, N.; Denney-Wilson, E.; Harris, M.F. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam. Pract. 2012, 13, 49. [Google Scholar] [CrossRef]
- Schillinger, D.; Duran, N.D.; McNamara, D.S.; Crossley, S.A.; Balyan, R.; Karter, A.J. Precision communication: Physicians’ linguistic adaptation to patients’ health literacy. Sci. Adv. 2021, 7, eabj2836. [Google Scholar] [CrossRef]
- Ghalibaf, A.K.; Nazari, E.; Gholian-Aval, M.; Tara, M. Comprehensive overview of computer-based health information tailoring: A systematic scoping review. BMJ Open 2019, 9, e021022. [Google Scholar] [CrossRef] [PubMed]
- Lustria, M.L.; Noar, S.M.; Cortese, J.; Van Stee, S.K.; Glueckauf, R.L.; Lee, J. A meta-analysis of web-delivered tailored health behavior change interventions. J. Health Commun. 2013, 18, 1039–1069. [Google Scholar] [CrossRef] [PubMed]
- Ownby, R.L.; Acevedo, A.; Waldrop-Valverde, D. Enhancing the impact of mobile health literacy interventions to reduce health disparities. Q. Rev. Distance Educ. 2019, 10, 15–34. [Google Scholar]
- Ginsburg, G.S.; Phillips, K.A. Precision medicine: From science to value. Health Aff. 2018, 37, 694–701. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. Healthy People 2020: Topics and Objectives; Department of Health and Human Services: Washington, DC, USA, 2011. Available online: http://healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf (accessed on 1 August 2011).
- Centers for Disease Control. CDC Clear Communication Index User Guide; Centers for Disease Control: Atlanta, GA, USA, 2019.
- Protheroe, J.; Rowlands, G. Matching clinical information with levels of patient health literacy. Nurs. Manag. 2013, 20, 20–21. [Google Scholar] [CrossRef] [PubMed]
- Eltorai, A.E.; Ghanian, S.; Adams, C.A., Jr.; Born, C.T.; Daniels, A.H. Readability of patient education materials on the American Association for Surgery of Trauma website. Arch. Trauma Res. 2014, 3, e18161. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, N.; Baird, G.L.; Garg, M. Examining the reading level of internet medical information for common internal medicine diagnoses. Am. J. Med. 2016, 129, 637–639. [Google Scholar] [CrossRef]
- Miles, R.C.; Baird, G.L.; Choi, P.; Falomo, E.; Dibble, E.H.; Garg, M. Readability of online patient educational materials related to breast lesions requiring surgery. Radiology 2019, 291, 112–118. [Google Scholar] [CrossRef]
- Rooney, M.K.; Santiago, G.; Perni, S.; Horowitz, D.P.; McCall, A.R.; Einstein, A.J.; Jagsi, R.; Golden, D.W. Readability of patient education materials from high-impact medical journals: A 20-year analysis. J. Patient Exp. 2021, 8. [Google Scholar] [CrossRef]
- Ownby, R.L. Readability of consumer-oriented geriatric depression information on the Internet. Clin. Gerontol. 2006, 29, 17–32. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Viera, A.; Crotty, K.; Holland, A.; Brasure, M.; Lohr, K.N.; Harden, E.; et al. Health Literacy Interventions and Outcomes: An Updated Systematic Review. Evidence Report/Technology Assesment No. 199; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2011. [Google Scholar]
- Lewis, D. Computer-based approaches to patient education: A review of the literature. J. Am. Med. Inform. Assoc. 1999, 6, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Lustria, M.L.; Cortese, J.; Noar, S.M.; Glueckauf, R.L. Computer-tailored health interventions delivered over the Web: Review and analysis of key components. Patient Educ. Couns. 2009, 74, 156–173. [Google Scholar] [CrossRef]
- Kuhn, E.; Weiss, B.J.; Taylor, K.L.; Hoffman, J.E.; Ramsey, K.M.; Manber, R.; Gehrman, P.; Crowley, J.J.; Ruzek, J.I.; Trockel, M. CBT-I Coach: A description and clinician perceptions of a mobile app for cognitive behavioral therapy for insomnia. J. Clin. Sleep Med. 2016, 12, 597–606. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, J.L. Brief interventions for depression in primary care: A systematic review. Can. Fam. Physician 2009, 55, 789–796. [Google Scholar]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.; Hibbard, J.H. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Intern. Med. 2012, 27, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, H.; Verma, I.; Gopaldasani, V. Patient activation and Type 2 diabetes mellitus self-management: A systematic review and meta-analysis. Aust. J. Prim. Health 2020, 26, 431–442. [Google Scholar] [CrossRef]
- Mosen, D.M.; Schmittdiel, J.; Hibbard, J.; Sobel, D.; Remmers, C.; Bellows, J. Is patient activation associated with outcomes of care for adults with chronic conditions? J. Ambul. Care Manag. 2007, 30, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Greene, J. What the evidence shows about patient activation: Better health outcomes and care experiences; fewer eata on costs. Health Aff. 2013, 32, 207–214. [Google Scholar] [CrossRef]
- Greene, J.; Hibbard, J.; Tusler, M. How Much Do Health Literacy and Patient Activation Contribute to Older Adults’ Ability to Manage Their Health; AARP: Washington, DC, USA, 2005; Available online: http://assets.aarp.org/rgcenter/health/2005_05_literacy.pdf (accessed on 11 June 2013).
- Greene, J.; Hibbard, J.H.; Sacks, R.; Overton, V.; Parrotta, C.D. When patient activation levels change, health outcomes and costs change, too. Health Aff. 2015, 34, 431–437. [Google Scholar] [CrossRef]
- Lindsay, A.; Hibbard, J.H.; Boothroyd, D.B.; Glaseroff, A.; Asch, S.M. Patient activation changes as a potential signal for changes in health care costs: Cohort study of US high-cost patients. J. Gen. Intern. Med. 2018, 33, 2106–2112. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. The primacy of self-regulation in health promotion. Appl. Psychol. 2005, 54, 245–254. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion from the perspective of social cognitive theory. In Understanding and Changing Health Behaviour; Psychology Press: London, UK, 2013; pp. 623–649. [Google Scholar]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient self-management of chronic disease in primary care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.R.; Ritter, P.; Stewart, A.L.; Sobel, D.S.; Brown, B.W., Jr.; Bandura, A.; Gonzalez, V.M.; Laurent, D.D.; Holman, H.R. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med. Care 2001, 39, 1217–1223. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.R.; Ritter, P.L.; Laurent, D.D.; Plant, K. Internet-based chronic disease self-management: A randomized trial. Med. Care 2006, 44, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Tian, Y.; Yin, M.; Lin, W.; Tuersun, Y.; Li, L.; Yang, J.; Wu, F.; Kan, Y.; Li, X.; et al. Relationship between self-efficacy and adherence to self-management and medication among patients with chronic diseases in China: A multicentre cross-sectional study. J. Psychosom. Res. 2023, 164, 111105. [Google Scholar] [CrossRef]
- Hoong, J.M.; Koh, H.A.; Wong, K.; Lee, H.H. Effects of a community-based chronic disease self-management programme on chronic disease patients in Singapore. Chronic Illn. 2023, 19, 434–443. [Google Scholar] [CrossRef]
- Farley, H. Promoting self-efficacy in patients with chronic disease beyond traditional education: A literature review. Nurs. Open 2020, 7, 30–41. [Google Scholar] [CrossRef]
- Lorig, K.R.; Sobel, D.S.; Ritter, P.L.; Laurent, D.; Hobbs, M. Effect of a self-management program on patients with chronic disease. Eff. Clin. Pract. 2001, 4, 256–262. [Google Scholar]
- Ory, M.G.; Ahn, S.; Jiang, L.; Smith, M.L.; Ritter, P.L.; Whitelaw, N.; Lorig, K. Successes of a national study of the Chronic Disease Self-Management Program: Meeting the triple aim of health care reform. Med. Care 2013, 51, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Lazaro, C.I.; García-González, J.M.; Adams, D.P.; Fernandez-Lazaro, D.; Mielgo-Ayuso, J.; Caballero-Garcia, A.; Moreno Racionero, F.; Córdova, A.; Miron-Canelo, J.A. Adherence to treatment and related factors among patients with chronic conditions in primary care: A cross-sectional study. BMC Fam. Pract. 2019, 20, 132. [Google Scholar] [CrossRef] [PubMed]
- DiMatteo, M.R. Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Med. Care 2004, 42, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Walsh, C.A.; Cahir, C.; Tecklenborg, S.; Byrne, C.; Culbertson, M.A.; Bennett, K.E. The association between medication non-adherence and adverse health outcomes in ageing populations: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2019, 85, 2464–2478. [Google Scholar] [CrossRef] [PubMed]
- Cutler, R.L.; Fernandez-Llimos, F.; Frommer, M.; Benrimoj, C.; Garcia-Cardenas, V. Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open 2018, 8, e016982. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.; Ritter, P.L.; Ory, M.G.; Whitelaw, N. Effectiveness of a generic chronic disease self-management program for people with type 2 diabetes: A translation study. Diabetes Educ. 2013, 39, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Jaglal, S.; Guilcher, S.; Hawker, G.; Lou, W.; Salbach, N.; Manno, M.; Zwarenstein, M. Impact of a chronic disease self-management program on health care utilization in rural communities: A retrospective cohort study using linked administrative data. BMC Health Serv. Res. 2014, 14, 198. [Google Scholar] [CrossRef]
- Ownby, R.L.; Acevedo, A.; Waldrop-Valverde, D.; Caballero, J.; Simonson, M.; Davenport, R.; Kondwani, K.; Jacobs, R.J. A mobile app for chronic disease self-management: Protocol for a randomized controlled trial. JMIR Res. Protoc. 2017, 6, e53. [Google Scholar] [CrossRef]
- Jacobs, R.J.; Ownby, R.L.; Acevedo, A.; Waldrop-Valverde, D. A qualitative study examining health literacy and chronic illness self-management in Hispanic and non-Hispanic older adults. J. Multidiscip. Healthc. 2017, 10, 167–177. [Google Scholar] [CrossRef]
- Mayer, R.E. Multimedia Learning, 2nd ed.; Cambridge University Press: New York City, NY, USA, 2009. [Google Scholar]
- Patel, N.; Waldrop, D.; Ownby, R.L. Creating a tailored info app to promote self-management skills in persons with chronic health conditions: Development strategies and user experience. Distance Learn. 2023, 20, 9–18. [Google Scholar]
- Fry, E. A readability formula that saves time. J. Read. 1968, 11, 513–578. [Google Scholar]
- Flesch, R. A new readability yardstick. J. Appl. Psychol. 1948, 32, 221–233. [Google Scholar] [CrossRef]
- Kincaid, J.P.; Fishburne, R.P.; Rogers, R.L.; Chissom, B.S. Derivation of New Readability Formulas (Automated Readability Index, Fog Count, and Flesch Reading Ease Formula) for Navy Enlisted Personnel; Chief of Naval Technical Training: Millington, TN, USA, 1975; Available online: http://www.dtic.mil/dtic/tr/fulltext/u2/a006655.pdf (accessed on 14 July 2013).
- National Institutes of Health Staff. What Are the Requirements for Reporting on Human Study Participant Age, Sex/Gender, and Race/Ethnicity? Available online: https://nexus.od.nih.gov/all/2021/04/29/what-are-the-requirements-for-reporting-on-human-study-participant-age-sex-gender-and-race-ethnicity/ (accessed on 28 March 2023).
- Murphy, P.W.; Davis, T.C.; Long, S.W.; Jackson, R.H.; Decker, B.C. Rapid Estimate of Adult Literacy in Medicine (REALM): A quick reading test for patients. J. Read. 1993, 37, 124–130. [Google Scholar]
- Han, H.J.; Acevedo, A.; Waldrop-Valverde, D.; Ownby, R.L. Evaluation of short forms of the Rapid Estimate of Adult Literacy in Medicine (REALM). In Proceedings of the International Conference on Communication in Healthcare/Health Literacy Annual Researach Conference, Baltimore, MD, USA, 8–11 October 2017. [Google Scholar]
- Fried, V.M.; Bernstein, A.B.; Bush, M.A. Multiple Chronic Conditions among Adults Aged 45 and Over: Trends over the Past 10 Years. NCHS Data Brief, No. 100; National Center for Health Statistics: Hyattsville, MD, USA, 2012. [Google Scholar]
- Solé-Auró, A.; Michaud, P.-C.; Hurd, M.; Crimmins, E. Disease incidence and mortality among older Americans and Europeans. Demography 2015, 52, 593–611. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Fried, T.R.; Boyd, C.M. Designing health care for the most common chronic condition--multimorbidity. JAMA 2012, 307, 2493–2494. [Google Scholar] [CrossRef]
- Groll, D.L.; To, T.; Bombardier, C.; Wright, J.G. The development of a comorbidity index with physical function as the outcome. J. Clin. Epidemiol. 2005, 58, 595–602. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services. Chronic Conditions among Medicare Beneficiaries, Chartbook, 2012th ed.; Centers for Medicare and Medicaid Services: Baltimore, MD, USA, 2012.
- Diederichs, C.; Berger, K.; Bartels, D.B. The measurement of multiple chronic diseases—A systematic review on existing multimorbidity indices. J. Gerontol. Ser. A 2010, 66, 301–311. [Google Scholar] [CrossRef]
- Woodcock, R.W.; McGrew, K.S.; Mather, N. Woodcock-Johnson III Normative Update; Riverside: Rolling Meadows, IL, USA, 2007. [Google Scholar]
- Ownby, R.L.; Acevedo, A.; Waldrop-Valverde, D.; Jacobs, R.J.; Homs, A.M.; Czaja, S.J.; Loewenstein, D. Development and initial validation of a computer-administered health literacy assessment in Spanish and English: FLIGHT/VIDAS. Patient Relat. Outcome Meas. 2013, 4, 21–35. [Google Scholar] [CrossRef]
- Pleasant, A. Advancing health literacy measurement: A pathway to better health and health system performance. J. Health Commun. 2014, 19, 1481–1496. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and testing of a short form of the Patient Activation Measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef]
- Skolasky, R.L.; Green, A.F.; Scharfstein, D.; Boult, C.; Reider, L.; Wegener, S.T. Psychometric properties of the patient activation measure among multimorbid older adults. Health Serv. Res. 2011, 46, 457–478. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.; Stewart, A.; Ritter, P.; Gonzalez, V.M.; Laurent, D.; Lynch, J. Outcome Measures for Health Education and Other Health Care Interventions; Sage: Thousand Oaks, CA, USA, 1996. [Google Scholar]
- Ritter, P.L.; Lorig, K. The English and Spanish Self-Efficacy to Manage Chronic Disease Scale measures were validated using multiple studies. J. Clin. Epidemiol. 2014, 67, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 478–483. [Google Scholar] [CrossRef]
- Peeters, G.; Waller, M.; Dobson, A.J. SF-36 normative values according to level of functioning in older women. Qual. Life Res. 2019, 28, 979–989. [Google Scholar] [CrossRef] [PubMed]
- Lyons, R.A.; Perry, I.M.; Littlepage, B.N.C. Evidence for the validity of the Short-form 36 Questionnaire (SF-36) in an elderly population. Age Ageing 1994, 23, 182–184. [Google Scholar] [CrossRef] [PubMed]
- McHorney, C.A.; Ware, J.E., Jr.; Lu, J.F.; Sherbourne, C.D. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med. Care 1994, 32, 40–66. [Google Scholar] [CrossRef]
- Gonzalez, J.S.; Schneider, H.E.; Wexler, D.J.; Psaros, C.; Delahanty, L.M.; Cagliero, E.; Safren, S.A. Validity of medication adherence self-reports in adults with type 2 diabetes. Diabetes Care 2013, 36, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Safren, S.A.; Skolnik, P.R.; Rogers, W.H.; Coady, W.; Hardy, H.; Wilson, I.B. Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav. 2008, 12, 86–94. [Google Scholar] [CrossRef]
- McNeish, D.; Wolf, M.G. Thinking twice about sum scores. Behav. Res. Methods 2020, 52, 2287–2305. [Google Scholar] [CrossRef]
- Ferrando, P.J.; Lorenzo-Seva, U. On the added value of multiple factor score estimates in essentially unidimensional models. Educ. Psychol. Meas. 2019, 79, 249–271. [Google Scholar] [CrossRef]
- Horton, J.C.; Jones, M.R. Warning on inaccurate Rosenbaum cards for testing near vision. Surv. Ophthalmol. 1997, 42, 169–174. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Bates, D.; Maechler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 48. [Google Scholar] [CrossRef]
- Luke, S.G. Evaluating significance in linear mixed-effects models in R. Behav. Res. Methods 2017, 49, 1494–1502. [Google Scholar] [CrossRef]
- Lenth, R. Emmeans: Estimated Marginal Means, Aka Least-Squares Means; R Package Version 1.8.7; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://cran.r-project.org/web/packages/emmeans/index.html (accessed on 17 November 2020).
- Hintze, J. PASS, 16; NCSS, LLC.: Kaysville, UT, USA, 2018. [Google Scholar]
- Ownby, R.L.; Waldrop-Valverde, D.; Caballero, J.; Jacobs, R.J. Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehav. HIV Med. 2012, 4, 113–121. [Google Scholar] [CrossRef][Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Ludecke, D. esc: Effect Size Computation for Meta Analysis; Version 0.5.1; Zenodo: Geneve, Switzerland, 2019. [Google Scholar] [CrossRef]
- Mouelhi, Y.; Jouve, E.; Castelli, C.; Gentile, S. How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual. Life Outcomes 2020, 18, 136. [Google Scholar] [CrossRef]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med. Care 2003, 41, 582–592. [Google Scholar] [CrossRef]
- Sloan, J.A.; Dueck, A. Issues for statisticians in conducting analyses and translating results for quality of life end points in clinical trials. J. Biopharm. Stat. 2004, 14, 73–96. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-Y.; Weng, W.-S.; Apriliyasari, R.W.; Van Truong, P.; Tsai, P.-S. Effects of patient activation intervention on chronic diseases: A meta-analysis. J. Nurs. Res. 2020, 28, e116. [Google Scholar] [CrossRef] [PubMed]
- Innab, A.; Kerari, A. Impact of behavioral interventions on patient activation in adults with hypertension: A systematic review and meta-analysis. Inquiry 2022, 59, 469580221090408. [Google Scholar] [CrossRef]
- Gholami, M.; Abdoli Talaei, A.; Tarrahi, M.J.; Mirzaei Taqi, F.; Galehdar, N.; Pirinezhad, P. The effect of self-management support program on patient activation and inner strength in patients with cardiovascular disease. Patient Educ. Couns. 2021, 104, 2979–2988. [Google Scholar] [CrossRef]
- Ownby, R.L.; Waldrop-Valverde, D.; Jacobs, R.J.; Acevedo, A.; Caballero, J. Cost effectiveness of a computer-delivered intervention to improve HIV medication adherence. BMC Med. Inform. Decis. Mak. 2013, 13, 29. [Google Scholar] [CrossRef]
- Gentili, A.; Failla, G.; Melnyk, A.; Puleo, V.; Tanna, G.L.D.; Ricciardi, W.; Cascini, F. The cost-effectiveness of digital health interventions: A systematic review of the literature. Front. Public Health 2022, 10, 787135. [Google Scholar] [CrossRef] [PubMed]
- Moreno, R.; Mayer, R.E. Cognitive principles of multimedia learning: The role of modality and contiguity. J. Educ. Psychol. 1999, 91, 358–368. [Google Scholar] [CrossRef]
- Klimova, B.; Zamborova, K. Use of mobile applications in developing reading comprehension in second language acquisition—A review study. Educ. Sci. 2020, 10, 391. [Google Scholar] [CrossRef]
- Sawesi, S.; Rashrash, M.; Phalakornkule, K.; Carpenter, J.S.; Jones, J.F. The impact of information technology on patient engagement and health behavior change: A systematic review of the literature. JMIR Med. Inform. 2016, 4, e1. [Google Scholar] [CrossRef] [PubMed]
- Rikard, R.V.; Thompson, M.S.; McKinney, J.; Beauchamp, A. Examining health literacy disparities in the United States: A third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health 2016, 16, 975. [Google Scholar] [CrossRef]
- Ryan, C.L.; Bauman, K. Educational Attainment in the United States: 2015; US Census Bureau: Suitland, MD, USA, 2016. [Google Scholar]
- Chen, C.; Ding, S.; Wang, J. Digital health for aging populations. Nat. Med. 2023, 29, 1623–1630. [Google Scholar] [CrossRef]
- Wilson, J.; Heinsch, M.; Betts, D.; Booth, D.; Kay-Lambkin, F. Barriers and facilitators to the use of e-health by older adults: A scoping review. BMC Public Health 2021, 21, 1556. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Institute for Healthcare Improvement. Ask Me 3 Brochure. Available online: https://www.ihi.org/resources/Pages/Tools/Ask-Me-3-Good-Questions-for-Your-Good-Health.aspx (accessed on 22 April 2024).
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
| Arthritis, rheumatoid or osteoarthritis *, 1 |
| Osteoporosis * |
| Asthma * |
| Chronic obstructive pulmonary disease (COPD) * |
| Angina * |
| Congestive heart failure (CHF) * |
| Heart attack * |
| Hypertension |
| Dyslipidemia |
| Multiple sclerosis; treated with oral or injectable medications * (in FCI 2 as part of neurological conditions) |
| Parkinson’s disease * (in FCI 2 as part of neurological conditions) |
| Migraine, if occurring at least 3 times per month and treated |
| Dementia (including mild cognitive impairment if diagnosed and treated) |
| Seizure disorder |
| Head injury; eligible if taking medications for pain or seizure prophylaxis |
| Cerebrovascular accident or transient ischemic attacks |
| Peripheral vascular disease * |
| Diabetes I or II * |
| Ulcer * (in FCI 2 as part of gastrointestinal [GI] conditions) |
| Hernia * (in FCI 2 as part of GI conditions) |
| Gastroesophageal reflux disease * (in FCI 2 as part of GI conditions) |
| Depression * |
| Anxiety or panic disorder * |
| Bipolar I or II |
| Psychotic disorder |
| Psychosis in the context of mood disorder |
| Cataracts |
| Glaucoma |
| Macular degeneration |
| Vision impairment (screening procedure described in text) * |
| Hearing impairment, check whether using amplification * |
| Back pain, including degenerative disc disease * |
| Obesity * |
| HIV/AIDS |
| Hepatitis, if taking medication |
| Chronic fatigue syndrome/myalgic encephalomyelitis |
| Substance abuse |
| Variable Count | Atlanta | Fort Lauderdale | Total | Χ2 | df | p | Effect Size (d) |
|---|---|---|---|---|---|---|---|
| Men | 65 | 79 | 144 | ||||
| Women | 118 | 47 | 165 | 22.15 | 1 | <0.001 | 0.56 |
| White | 7 | 34 | 41 | ||||
| Nonwhite | 176 | 92 | 268 | 37.78 | 1 | <0.001 | 0.71 |
| Variable Mean (SD) | t | df | p | ES | |||
| Age in Years | 58.10 (8.61) | 56.95 (8.09) | 57.63 (8.41) | 1.18 | 307 | 0.24 | 0.14 |
| Education Years | 12.02 (1.76) | 11.64 (1.97) | 11.86 (1.85) | 1.75 | 307 | 0.08 | 0.20 |
| Total Number of Health Conditions | 5.92 (2.66) | 7.26 (2.77) | 6.47 (2.78) | 4.28 | 307 | <0.001 | 0.50 |
| WJ Reading Grade 1 | 6.60 (4.10) | 7.74 (3.97) | 7.06 (4.08) | 2.44 | 307 | 0.02 | 0.28 |
| Flight/Vidas Health Literacy 1 | 9.59 (3.92) | 10.97 (4.09) | 10.17 (4.04) | 2.89 | 307 | 0.004 | 0.35 |
| PAM Score 1 | 61.37 (16.03) | 61.94 (15.96) | 61.61 (15.97) | 0.30 | 291 2 | 0.76 | 0.04 |
| CDSE Mean 1 | 6.96 (2.01) | 6.61 (1.93) | 6.82 (1.98) | 1.46 | 290 2 | 0.15 | 0.18 |
| HRQOL (SF General Health) 1 | 60.21 (19.38) | 60.16 (20.10) | 60.19 (19.66) | 0.02 | 288 2 | 0.98 | 0.003 |
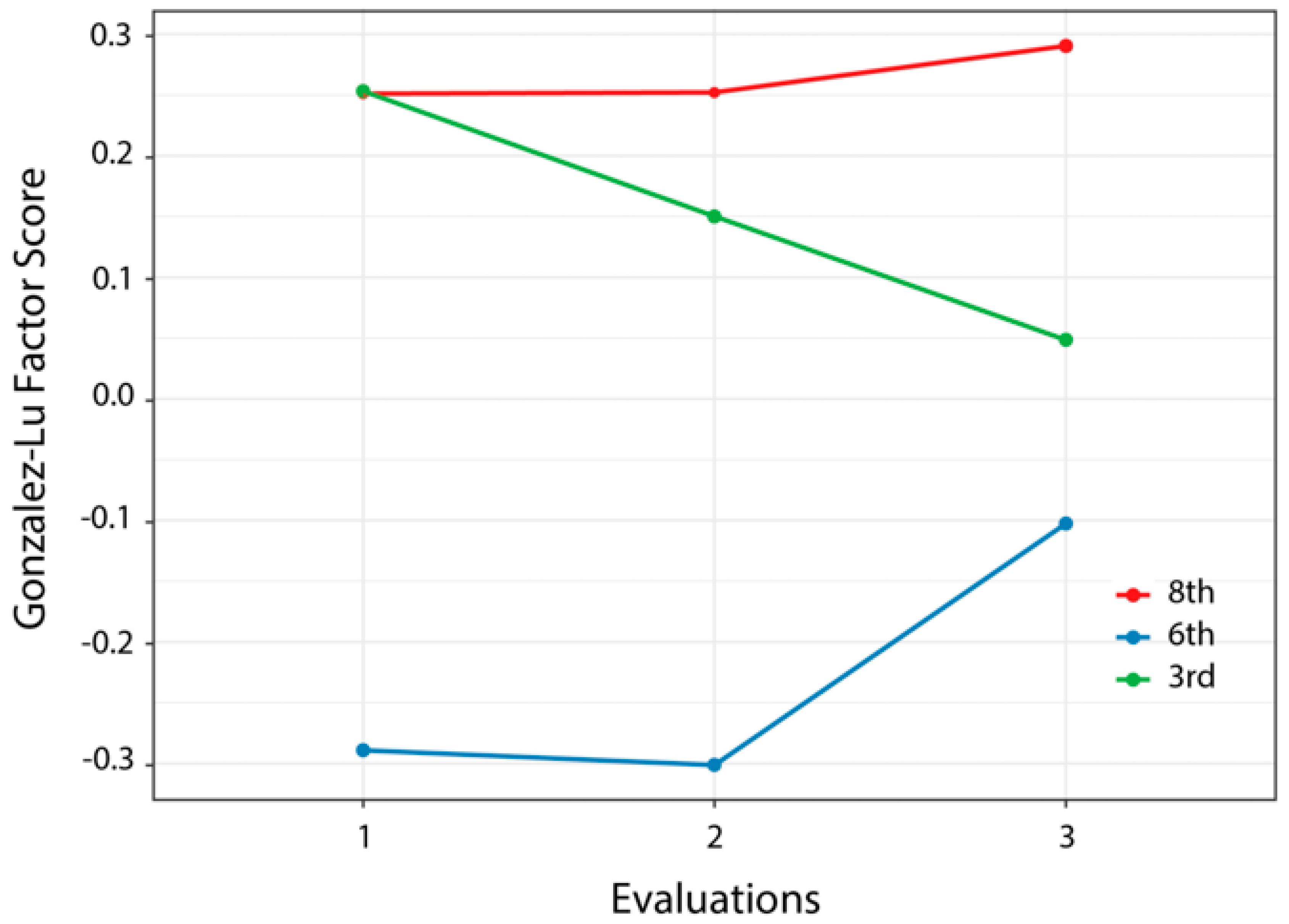
| Gonzalez Lu Factor Score 1 | −0.09 (1.07) | 0.14 (1.02) | 0.01 (1.06) | 1.89 | 291 2 | 0.06 | 0.22 |
| Sum of Squares | Mean Squares | Numerator df | Denominator df | F | p | |
|---|---|---|---|---|---|---|
| Age | 601.86 | 601.86 | 1 | 281.16 | 4.90 | 0.03 1 |
| Gender | 394.9 | 394.9 | 1 | 274.52 | 3.21 | 0.07 |
| Race | 82.26 | 82.26 | 1 | 276.27 | 0.67 | 0.41 |
| Education | 143.46 | 143.46 | 1 | 270.92 | 1.17 | 0.28 |
| Health Literacy | 309.17 | 309.17 | 1 | 276.78 | 2.51 | 0.11 |
| Health Conditions | 189.27 | 189.27 | 1 | 281.6 | 1.54 | 0.22 |
| Site | 17.73 | 17.73 | 1 | 271.62 | 0.14 | 0.70 |
| Time | 822.22 | 411.11 | 2 | 482.77 | 3.34 | 0.04 1 |
| Group | 159 | 79.5 | 2 | 276.84 | 0.65 | 0.52 |
| Time x Group | 92.61 | 23.15 | 4 | 482.3 | 0.19 | 0.94 |
| Sum of Squares | Mean Squares | Numerator df | Denominator df | F | p | |
|---|---|---|---|---|---|---|
| Age | 1.20 | 1.17 | 1 | 291 | 0.90 | 0.34 |
| Gender | 1.30 | 1.31 | 1 | 285 | 1.01 | 0.32 |
| Race | 0.10 | 0.13 | 1 | 297 | 0.10 | 0.75 |
| Education | 14.60 | 14.58 | 1 | 279 | 11.24 | <0.001 1 |
| Health Literacy | 14.10 | 14.10 | 1 | 285 | 10.88 | 0.0011 1 |
| Health Conditions | 19.30 | 19.28 | 1 | 286 | 14.87 | <0.001 1 |
| Site | 0.60 | 0.62 | 1 | 287 | 0.48 | 0.49 |
| Time | 32.20 | 16.08 | 2 | 470 | 12.40 | <0.001 1 |
| Group | 3.80 | 1.92 | 2 | 287 | 1.48 | 0.23 |
| Time x Group | 7.60 | 1.91 | 4 | 470 | 1.47 | 0.21 |
| Sum of Squares | Mean Squares | Numerator df | Denominator df | F | p | |
|---|---|---|---|---|---|---|
| Age | 46 | 46 | 1 | 287 | 0.47 | 0.50 |
| Gender | 250 | 250 | 1 | 276 | 2.52 | 0.11 |
| Race | 13 | 13 | 1 | 276 | 0.13 | 0.72 |
| Education | 1139 | 1139 | 1 | 274 | 11.51 | <0.001 1 |
| Health Literacy | 259 | 259 | 1 | 277 | 2.62 | 0.11 |
| Health Conditions | 1739 | 1739 | 1 | 280 | 17.57 | <0.001 1 |
| Site | 172 | 172 | 1 | 274 | 1.74 | 0.19 |
| Time | 1558 | 779 | 2 | 474 | 7.87 | <0.001 1 |
| Group | 272 | 136 | 2 | 277 | 1.37 | 0.26 |
| Time x Group | 355 | 89 | 4 | 474 | 0.9 | 0.47 |
| Sum of Squares | Mean Squares | Numerator df | Denominator df | F | p | |
|---|---|---|---|---|---|---|
| Age | 1.12 | 1.119 | 1 | 282 | 3.19 | 0.07 |
| Gender | 1.35 | 1.355 | 1 | 274 | 3.87 | 0.0503 |
| Race | 0.63 | 0.633 | 1 | 274 | 1.81 | 0.18 |
| Education | 0.01 | 0.008 | 1 | 270 | 0.02 | 0.88 |
| Health Literacy | 1.61 | 1.609 | 1 | 275 | 4.59 | 0.03 1 |
| Health Conditions | 0.94 | 0.94 | 1 | 280 | 2.68 | 0.10 |
| Site | 0.79 | 0.786 | 1 | 272 | 2.24 | 0.14 |
| Time | 0.28 | 0.138 | 2 | 476 | 0.39 | 0.67 |
| Group | 5.73 | 2.864 | 2 | 276 | 8.18 | <0.001 1 |
| Time x Group | 3.09 | 0.772 | 4 | 476 | 2.2 | 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ownby, R.L.; Simonson, M.; Caballero, J.; Thomas-Purcell, K.; Davenport, R.; Purcell, D.; Ayala, V.; Gonzalez, J.; Patel, N.; Kondwani, K. A Mobile App for Chronic Disease Self-Management for Individuals with Low Health Literacy: A Multisite Randomized Controlled Clinical Trial. J. Ageing Longev. 2024, 4, 51-71. https://doi.org/10.3390/jal4020005
Ownby RL, Simonson M, Caballero J, Thomas-Purcell K, Davenport R, Purcell D, Ayala V, Gonzalez J, Patel N, Kondwani K. A Mobile App for Chronic Disease Self-Management for Individuals with Low Health Literacy: A Multisite Randomized Controlled Clinical Trial. Journal of Ageing and Longevity. 2024; 4(2):51-71. https://doi.org/10.3390/jal4020005
Chicago/Turabian StyleOwnby, Raymond L., Michael Simonson, Joshua Caballero, Kamilah Thomas-Purcell, Rosemary Davenport, Donrie Purcell, Victoria Ayala, Juan Gonzalez, Neil Patel, and Kofi Kondwani. 2024. "A Mobile App for Chronic Disease Self-Management for Individuals with Low Health Literacy: A Multisite Randomized Controlled Clinical Trial" Journal of Ageing and Longevity 4, no. 2: 51-71. https://doi.org/10.3390/jal4020005
APA StyleOwnby, R. L., Simonson, M., Caballero, J., Thomas-Purcell, K., Davenport, R., Purcell, D., Ayala, V., Gonzalez, J., Patel, N., & Kondwani, K. (2024). A Mobile App for Chronic Disease Self-Management for Individuals with Low Health Literacy: A Multisite Randomized Controlled Clinical Trial. Journal of Ageing and Longevity, 4(2), 51-71. https://doi.org/10.3390/jal4020005







