Therapeutic Architecture and Temporality: Evidence-Based Design for Long-Stay Facilities for Individuals with Severe Intellectual Disabilities and Challenging Behaviour
Abstract
1. Introduction
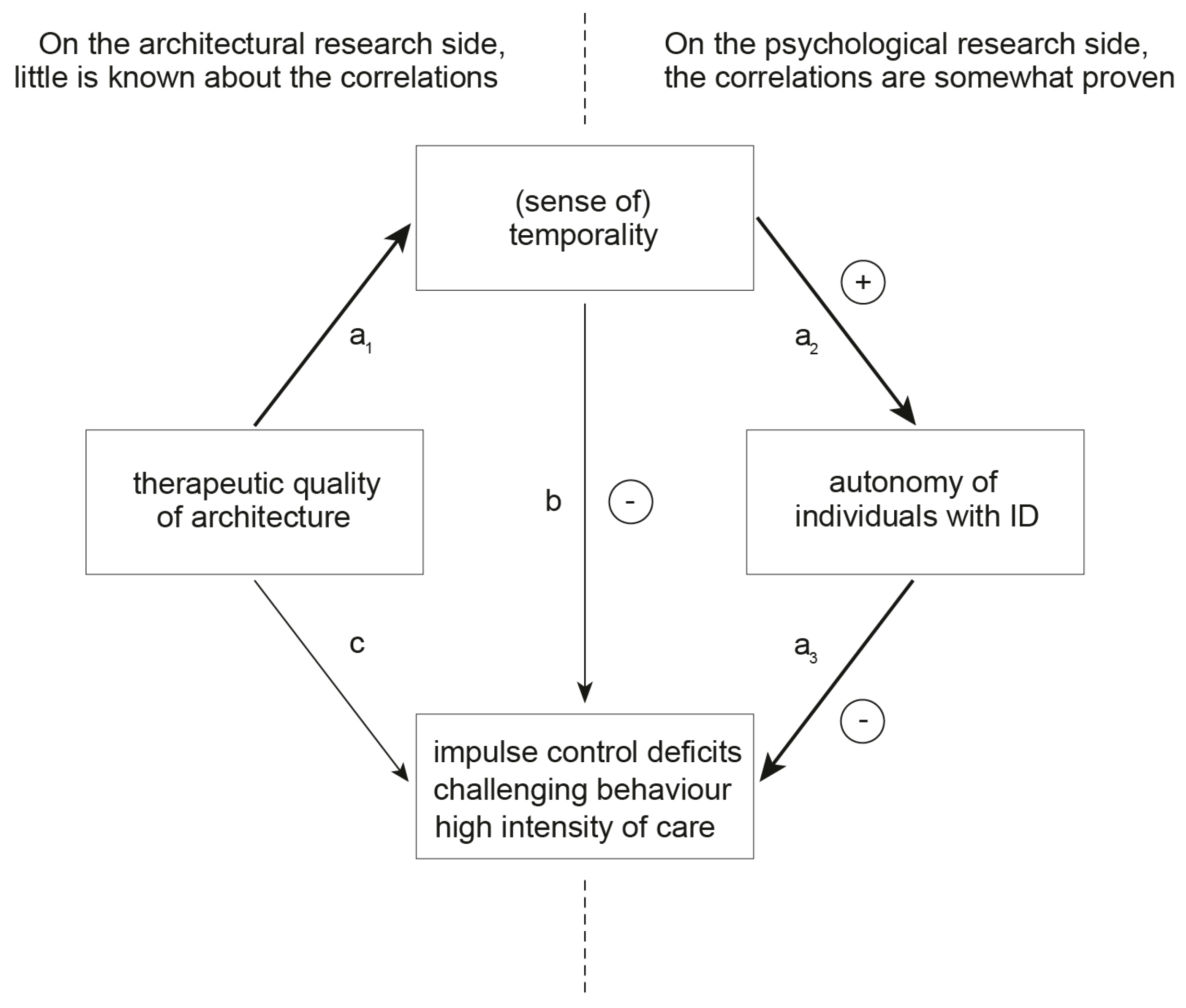
1.1. Therapeutic Architecture
1.2. Architectural Temporality
1.3. Time Perception and Temporality in Individuals with Intellectual Disabilities
1.4. Challenging Behaviour and Housing Individuals with Intellectual Disabilities
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Systematic Behavioural Observation
2.4. Structured Interviews
- Do you think that more autonomy in the eight observed and repetitive activities within a day could help the client show less CB?
- In which of the eight observed activities within a day could it be helpful for the development of autonomy …
- (a)
- … having less contact/proximity to the group. Please label the group contact as “stimulating”;
- (b)
- … having more contact/proximity to the group. Please mark the group contact as “stimulating”;
- (c)
- … having less contact/proximity to the caregiver. Please mark the caregiver contact as “calming”;
- (d)
- … having more contact/proximity to the caregiver. Please mark the caregiver contact as “reassuring”.
- What spatial or design interventions could you imagine to be helpful to achieve 2(a)–(d)?
2.5. UV-Index Method
2.6. Focus Groups
3. Results
3.1. Temporality through Spatial Sequencing and Repetition

3.2. Temporality through Privacy-Related Variation of Spatial Dimensions

3.3. Temporality through Spatial Orchestration of Daylight
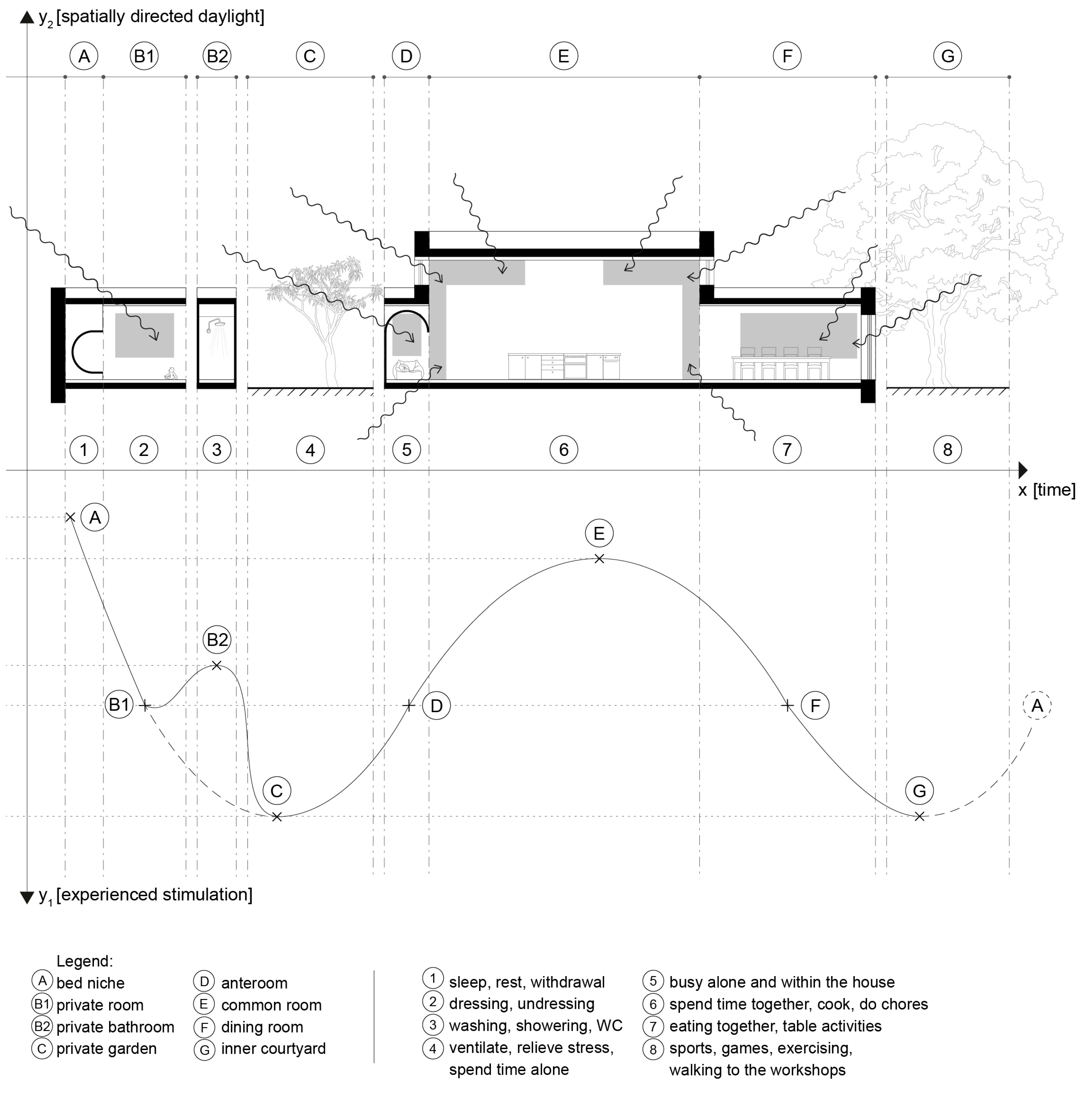
3.4. Temporality through Spatial Regulation of Emotional Proximity to the Caregiver

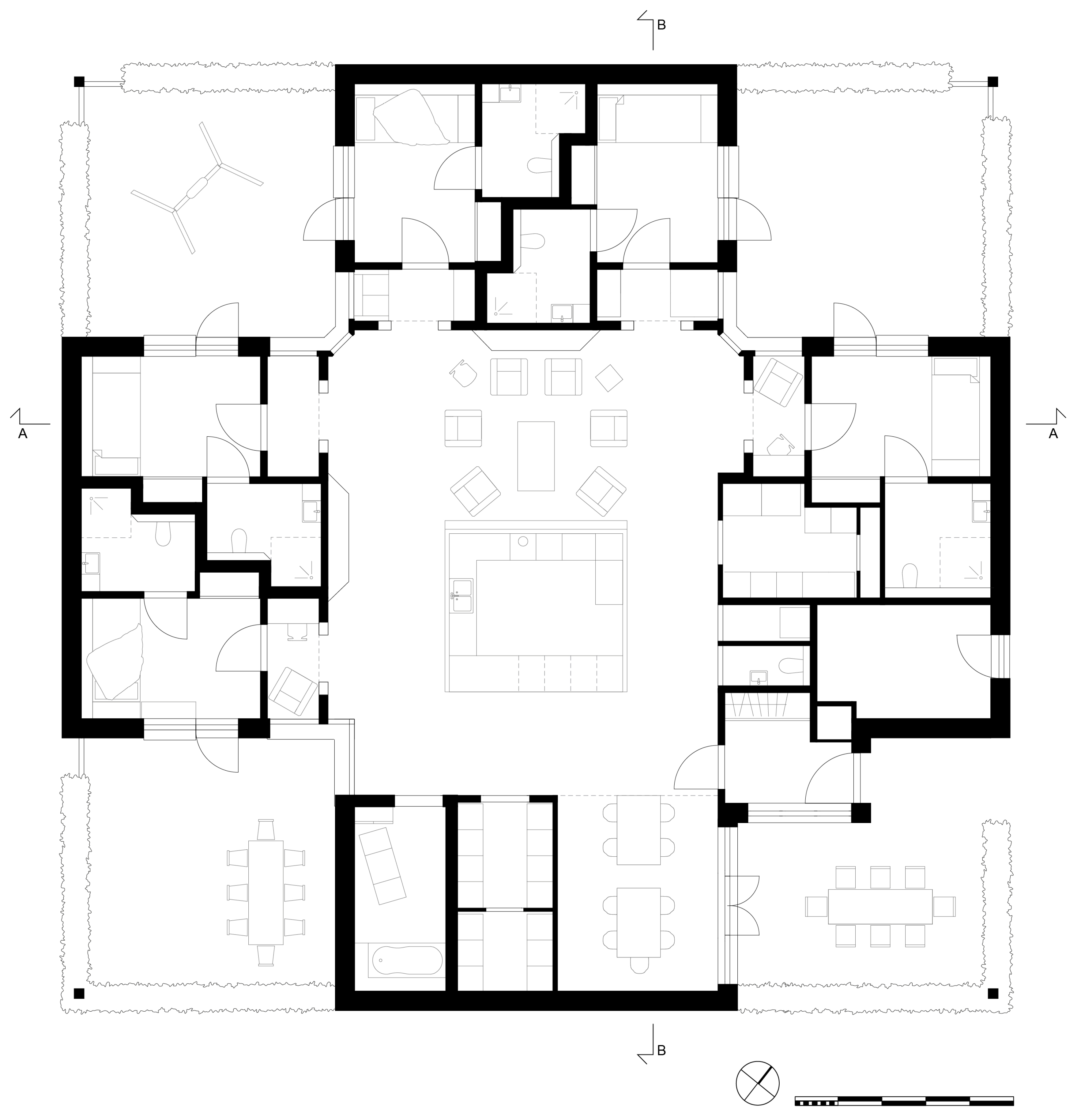
3.5. Application of the Four Design Criteria to Architecture: IPSE-Plus Typology


4. Discussion
4.1. Spatial Sequencing and Repetition for Individuals with ID and CB
4.2. Privacy-Related Variation of Spatial Dimensions
4.3. Spatial Orchestration of Daylight
4.4. Spatial Regulation of Emotional Proximity to Caregiver
4.5. The IPSE-Plus Typology
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Owen, A.L.; Wilson, R.R. Unlocking the riddle of time in learning disability. J. Intellect. Disabil. 2006, 10, 9–17. [Google Scholar] [CrossRef]
- Innes, A.; Mccabe, L.; Watchman, K. Caring for older people with an intellectual disability: A systematic review. Maturitas 2012, 72, 286–295. [Google Scholar] [CrossRef]
- Hogan, L.; Bigby, C. Supporting People with Complex and Challenging Behaviour. In Disability Practice; Bigby, C., Hough, A., Eds.; Palgrave Macmillan: Singapore, 2024; pp. 161–182. [Google Scholar]
- Thompson, J.; Bradley, V.; Buntinx, W.; Schalock, R.; Shogren, K.; Snell, M.; Wehmeyer, M.; Borthwick-Duffy, S.; Coulter, D.; Craig, E.; et al. Conceptualizing Supports and the Support Needs of People with Intellectual Disability. Intellect. Dev. Disabil. 2009, 47, 135–146. [Google Scholar] [CrossRef]
- Bowring, D.L.; Painter, J.; Hastings, R.P. Prevalence of Challenging Behaviour in Adults with Intellectual Disabilities, Correlates, and Association with Mental Health. Curr. Dev. Disord. Rep. 2019, 6, 173–181. [Google Scholar] [CrossRef]
- Roos, J.; Koppen, G.; Vollmer, T.C.; van Schijndel-Speet, M.; Dijkxhoorn, Y. Unlimited surrounding: A scoping review on the impact of the built environment on health, behavior, and quality of life of individuals with intellectual disabilities in long-term care. HERD Health Environ. Res. Des. J. 2022, 15, 295–314. [Google Scholar] [CrossRef]
- Shaw, K.; Cartwright, C.; Craig, J. The housing and support needs of people with an intellectual disability into older age. J. Intellect. Disabil. Res. JIDR 2011, 55, 895–903. [Google Scholar] [CrossRef]
- Bertelli, M.; Salvador-Carulla, L.; Lassi, S.; Zappella, M.; Ceccotto, R.; Palterer, D.; de Groef, J.; Benni, L.; Rossi Prodi, P. Quality of life and living arrangements for people with intellectual disability. Adv. Ment. Health Intellect. Disabil. 2013, 7, 220–231. [Google Scholar] [CrossRef]
- Ulrich, R. Effects of interior design on wellness: Theory and recent scientific research. J. Health Care Inter. Des. 1991, 3, 97–109. [Google Scholar]
- Huisman, E.R.C.M.; Morales, E.; van Hoof, J.; Kort, H.S.M. Healing environment: A review of the impact of physical environmental factors on users. Build. Environ. 2012, 58, 70–80. [Google Scholar] [CrossRef]
- Zhang, Y.; Tzortzopoulos, P.; Kagioglou, M. Healing built-environment effects on health outcomes: Environment-occupant-health framework. Build. Res. Inf. 2019, 47, 747–766. [Google Scholar] [CrossRef]
- Vollmer, T.C.; Koppen, G. Architectuur als tweede lichaam: De rol van architectuur bij de verzorging van kanker [Architecture as a second body: The role of architecture in cancer care]. Layout 2010, 11, 1–16. [Google Scholar]
- Koppen, G.; Vollmer, T.C. Architektur als Zweiter Körper: Eine Entwurfslehre für den Evidenzbasierten Gesundheitsbau [Architecture as a Second Body: A Design Theory for Evidence-Based Healthcare Construction]; Gebrüder Mann Verlag: Berlin, Germany, 2022. [Google Scholar]
- Koppen, G.; Vollmer, T.C. The Healing Seven. In Building to Heal: New Architectures for Hospitals; Vollmer, T.C., Lepik, A., Luksch, L., Eds.; Architangle: Berlin, Germany, 2023; pp. 120–133. [Google Scholar]
- Vollmer, T.C.; Lepik, A.; Luksch, L. (Eds.) Building to Heal: New Architecture for Hospitals; Architangle: Berlin, Germany, 2023. [Google Scholar]
- Ulrich, R.; Zimring, C.; Zhu, X.; DuBose, J.; Seo, H.; Choi, Y.-S.; Quan, X.; Joseph, A. A Review of the Research Literature on Evidence-Based Healthcare Design. HERD Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Malkin, J. A Visual Reference for Evidence-Based Design; The Centre for Health Design: Concord, CA, USA, 2008. [Google Scholar]
- Stichler, J.F.; Hamilton, D.K. Evidence-Based Design: What is It? HERD Health Environ. Res. Des. J. 2008, 1, 3–4. [Google Scholar] [CrossRef]
- Vollmer, T.C.; Koppen, G.; Kohler, K. Wie Stadtarchitektur die Gesundheit beeinflusst: Das PAKARA-Modell [How urban architecture influences health: The PAKARA model]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2020, 63, 972–978. [Google Scholar] [CrossRef]
- Koppen, G.; Vollmer, T.C.; Kohler, K. Designing urban health: The PAKARA Model. In Human Scale Remeasured: New Spatial Requirements, Societal Demands and Economic Values in Architecture; ANCB the Aedes Metropolitan Laboratory, Ed.; AEDES Publisher: Berlin, Germany, 2021; pp. 172–174. [Google Scholar]
- Hall, E.T. The Hidden Dimension; Anchor Books: New York, NY, USA, 1990. [Google Scholar]
- Nute, K. The Architecture of Expectation. Architecture 2023, 3, 671–680. [Google Scholar] [CrossRef]
- Teuscher, U.; McQuire, M.; Collins, J.; Coulson, S. Congruity Effects in Time and Space: Behavioral and ERP Measures. Cogn. Sci. 2008, 32, 563–578. [Google Scholar] [CrossRef]
- Roussel, M.; Grondin, S.; Killeen, P. Spatial Effects on Temporal Categorisation. Perception 2009, 38, 748–762. [Google Scholar] [CrossRef]
- Northoff, G.; Huang, Z. How do the brain’s time and space mediate consciousness and its different dimensions? Temporo-spatial theory of consciousness (TTC). Neurosci. Biobehav. Rev. 2017, 80, 630–645. [Google Scholar] [CrossRef]
- Nute, K.; Chen, Z. Temporal Cues in Built Environments. Int. J. Constr. Environ. 2018, 9, 1–18. [Google Scholar] [CrossRef]
- Chen, Z.J.; Nute, K. Looking forward to the future: Visual prospects and optimism. Int. J. Health Wellness Soc. 2021, 16, 163–174. [Google Scholar]
- Vollmer, T.C.; Wittmann, M.; Schweiger, C.; Hiddemann, W. Preoccupation with death as predictor of psychological distress in patients with haematologic malignancies. Eur. J. Cancer Care 2011, 20, 403–411. [Google Scholar] [CrossRef]
- Wittman, M.; Vollmer, T.C.; Schweiger, C.; Hiddemann, W. The relation between the experience of time and psychological distress in patients with hematological malignancies. Palliat. Support. Care 2006, 4, 357–363. [Google Scholar] [CrossRef]
- Wittmann, M.; Dietrich, S.; Schmidt, S.; Vollmer, T. Zeiterleben und Umgang mit Zeit bei Patienten der Onkologie und in der Palliativmedizin; Kohlhammer: Stuttgart, Germany, 2020; pp. 108–129. [Google Scholar]
- Vollmer, T.C.; Koppen, G. Die Erkrankung des Raumes: Raumwahrnehmung im Zustand Körperlicher Versehrtheit und deren Bedeutung für die Architektur; Herbert Utz Verlag: München, Germany, 2010. [Google Scholar]
- Koppen, G.H.; Vollmer, T. ‘If walls could talk’—The willingness of talking about death and dying and its association to space awareness in patients with cancer. Psycho-Oncology 2006, 15, S82. [Google Scholar]
- Vollmer, T.; Koppen, G.H. Architekturwahrnehmung und Stresserleben schwerst- und chronisch Kranker. In Architektur Wahrnehmen; Abel, A., Rudolf, B., Eds.; Transcript: Bielefeld, Germany, 2018; pp. 207–227. [Google Scholar]
- Vollmer, T.C. La Infirmita: The scientific human scale of a new hospital architecture and its necessity. In Building to Heal: New Architecture for Hospitals; Vollmer, T.C., Lepik, A., Luksch, L., Eds.; Architangle: Berlin, Germany, 2023; pp. 14–19. [Google Scholar]
- Ulrich, R.S. View through a window may influence recovery from surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef]
- Appleton, J. The Experience of Landscape; John Wiley: London, UK, 1975. [Google Scholar]
- Lorenz, K.Z. King Solomon’s Ring: New Light on Animal Ways; The Reprint Society: London, UK, 1953. [Google Scholar]
- Stamps, A.E. Some Findings on Prospect and Refuge: I. Percept. Mot. Ski. 2008, 106, 147–162. [Google Scholar] [CrossRef]
- Dosen, A.; Ostwald, M. Evidence for prospect-refuge theory: A meta-analysis of the findings of environmental preference research. City Territ. Arch. 2016, 2016, 3. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. International Classification of Diseases: 11th Revision (ICD-11); World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Luna, R.E. What Is Intellectual Disability? Available online: https://www.psychiatry.org/patients-families/intellectual-disability/what-is-intellectual-disability#section_5 (accessed on 25 April 2024).
- Bruss, F.T.; Rüschendorf, L. On the Perception of Time. Gerontology 2009, 56, 361–370. [Google Scholar] [CrossRef]
- Wittmann, M. Gefühlte Zeit: Kleine Psychologie des Zeitempfindens [Perceived Time: A Brief Psychology of the Perception of Time]; C.H. Beck: München, Germany, 2012. [Google Scholar]
- Vogel, D.H.V.; Jording, M.; Kupke, C.; Vogeley, K. The temporality of situated cognition. Front. Psychol. 2020, 11, 546212. [Google Scholar] [CrossRef]
- Di Nuovo, S.; Belluardo, G.; Belluardo, D.; Castiglia, D.; Fanzone, M.; Granata, S.; Notti, A. Time processing skills in typical and impaired development. Life Span Disabil. 2015, 18, 233–248. [Google Scholar]
- Wittmann, M. Wenn die Zeit Stehen Bleibt: Kleine Psychologie der Grenzerfahrungen [When Time Stands Still: A Brief Psychology of Borderline Experiences]; C.H. Beck: München, Germany, 2015. [Google Scholar]
- Bschor, T.; Ising, M.; Bauer, M.; Lewitzka, U.; Skerstupeit, M.; Müller-Oerlinghausen, B.; Baethge, C. Time experience and time judgment in major depression, mania and healthy subjects. A controlled study of 93 subjects. Acta Psychiatr. Scand. 2004, 109, 222–229. [Google Scholar] [CrossRef]
- Twenge, J.; Catanese, K.; Baumeister, R. Social Exclusion and the Deconstructed State: Time Perception, Meaninglessness, Lethargy, Lack of Emotion, and Self-Awareness. J. Personal. Soc. Psychol. 2003, 85, 409–423. [Google Scholar] [CrossRef]
- Rubia, K.; Halari, R.; Christakou, A.; Taylor, E. Impulsiveness as a timing disturbance: Neurocognitive abnormalities in attention-deficit hyperactivity disorder during temporal processes and normalization with methylphenidate. Philos. Trans. R. Soc. B Biol. Sci. 2009, 364, 1919–1931. [Google Scholar] [CrossRef]
- Casassus, M.; Poliakoff, E.; Gowen, E.; Poole, D.; Jones, L.A. Time perception and autistic spectrum condition: A systematic review. Autism Res. 2019, 12, 1440–1462. [Google Scholar] [CrossRef]
- Davies, D.K.; Stock, S.E.; Wehmeyer, M.L. Enhancing independent time-management skills of individuals with mental retardation using a palmtop personal computer. Ment. Retard. 2002, 40, 358–365. [Google Scholar] [CrossRef]
- Sharp, K.; Murray, G.; Mckenzie, K.; Quigley, A.; Patrick, S. A matter of time. Learn. Disabil. Pract. 2001, 3, 10–13. [Google Scholar] [CrossRef]
- WHO. ICD-10. Available online: https://icd.who.int/browse10/2019/en#/F70-F79 (accessed on 7 May 2024).
- Friedman, W.J. Children’s Representations of the Pattern of Daily Activities. Child Dev. 1990, 61, 1399–1412. [Google Scholar] [CrossRef]
- Brackbill, Y.; Fitzgerald, H.E. Stereotype Temporal Conditioning in Infants. Psychophysiology 1972, 9, 569–577. [Google Scholar] [CrossRef]
- VanMarle, K.; Wynn, K. Six-month-old infants use analog magnitudes to represent duration. Dev. Sci. 2006, 9, F41–F49. [Google Scholar] [CrossRef]
- Droit-Volet, S. Time perception in children: A neurodevelopmental approach. Neuropsychologia 2013, 51, 220–234. [Google Scholar] [CrossRef]
- Allman, M.; Pelphrey, K.; Meck, W. Developmental neuroscience of time and number: Implications for autism and other neurodevelopmental disabilities. Front. Integr. Neurosci. 2012, 6, 7. [Google Scholar] [CrossRef]
- Emerson, E. Challenging Behavior: Analysis and Intervention in People with Intellectual Disabilities, 1st ed.; Cambridge University Press: Cambridge, UK, 1995. [Google Scholar]
- Emerson, E.; Einfeld, S.L. Challenging Behaviour; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Emerson, E.; Robertson, J.; Gregory, N.; Hatton, C.; Kessissoglou, S.; Hallam, A.; Hillery, J. Treatment and management of challenging behaviours in residential settings. J. Appl. Res. Intellect. Disabil. 2000, 13, 197–215. [Google Scholar] [CrossRef]
- Felce, D.; Kerr, M.; Hastings, R.P. A general practice-based study of the relationship between indicators of mental illness and challenging behaviour among adults with intellectual disabilities. J. Intellect. Disabil. Res. 2009, 53, 243–254. [Google Scholar] [CrossRef]
- Lamoureux-Hébert, M.; Morin, D.; Crocker, A. Support Needs of Individuals With Mild and Moderate Intellectual Disabilities and Challenging Behaviors. J. Ment. Health Res. Intellect. Disabil. 2010, 3, 67–84. [Google Scholar] [CrossRef]
- Verhaar, L.; Dijkxhoorn, Y.M.; de Sonneville, L.; Swaab, H. A three-years follow-up of extra intensive support for individuals with intellectual disability and severe challenging behaviour in the Netherlands. J. Intellect. Disabil. 2024. [Google Scholar] [CrossRef]
- Tyrer, P.; Bajaj, P. Nidotherapy: Making the environment do the therapeutic work. Adv. Psychiatr. Treat. 2005, 11, 232–238. [Google Scholar] [CrossRef]
- Tyrer, P.; Kramo, K. Nidotherapy in practice. J. Ment. Health 2007, 16, 117–129. [Google Scholar] [CrossRef]
- Tyrer, P.; Tarabi, S.A.; Bassett, P.; Liedtka, N.; Hall, R.; Nagar, J.; Imrie, A.; Tyrer, H. Nidotherapy compared with enhanced care programme approach training for adults with aggressive challenging behaviour and intellectual disability (NIDABID): Cluster randomised controlled trial. J. Intellect. Disabil. Res. 2017, 61, 521–531. [Google Scholar] [CrossRef]
- Roos, J.; Möhn, A.; Ponsioen, A.; Didden, R. Redesigning Rooms of Clients with Intellectual Disabilities and Severe Behavioral Problems in a Long-term Care Facility: Three Case Studies. J. Dev. Phys. Disabil. 2024, 1–30. [Google Scholar] [CrossRef]
- Roos, B.A.; Mobach, M.; Heylighen, A. How does architecture contribute to reducing behaviours that challenge? A scoping review. Res. Dev. Disabil. 2022, 127, 104229. [Google Scholar] [CrossRef]
- Carnemolla, P. Individualized Apartment Accommodation for People with Intellectual Disability: Protocol for a Qualitative Study Examining the Well-Being and Support Outcomes Linking Housing and Health. JMIR Res. Protoc. 2020, 9, e18248. [Google Scholar] [CrossRef]
- Bigby, C.; Beadle-Brown, J. Improving quality of life outcomes in supported accommodation for people with intellectual disability: What makes a difference? J. Appl. Res. Intellect. Disabil. 2018, 31, e182–e200. [Google Scholar] [CrossRef]
- Simons, M.A.G.; Koordeman, R.; Willems, A.P.A.M.; Hermsen, M.; Rooijackers, L.M.; Otten, R. Factors facilitating or hindering meaningful staff-client interactions in people with intellectual disabilities and challenging behaviour: A systematic mixed studies review using thematic synthesis. J. Appl. Res. Intellect. Disabil. 2021, 34, 446–458. [Google Scholar] [CrossRef]
- Mueller-Schotte, S.; Huisman, E.R.C.M.; Huisman, C.; Kort, H. The influence of the indoor environment on people displaying challenging behaviour: A scoping review. Technol. Disabil. 2022, 34, 133–140. [Google Scholar] [CrossRef]
- Glaesser, R.S.; Perkins, E.A. Self-injurious behavior in older adults with intellectual disabilities. Soc. Work 2013, 58, 213–221. [Google Scholar] [CrossRef]
- Young, L. Community and cluster centre residential services for adults with intellectual disability: Long-term results from an Australian-matched sample. J. Intellect. Disabil. Res. 2006, 50, 419–431. [Google Scholar] [CrossRef]
- Roebuck, M. Housing for People with Intellectual Disabilities: A Scoping Review. J. Dev. Disabil. 2021, 26, 1–25. [Google Scholar] [CrossRef]
- Vollmer, T.C.; Koppen, G. Vom Bedürfnis zum Beweis [From need to evidence]. In Architekturpsychologie Perspektiven: Band 1 Forschung und Lehre [Perspectives on Architectural Psychology: Volume 1 Research and Teaching]; Vollmer, T.C., Ed.; Springer Fachmedien Wiesbaden: Wiesbaden, Germany, 2023; pp. 7–34. [Google Scholar]
- Zimring, C.; Bosch, S. Building the Evidence Base for Evidence-Based Design: Editors’ Introduction; SAGE Publications Sage CA: Los Angeles, CA, USA, 2008. [Google Scholar]
- Koppen, G.; Vollmer, T.C. Der Mensch als Maßstab: Architektur und Psychosoziale Gesundheit im Bezahlbaren Wohnungsbau. Bedürfnisse, Analysen, Konzepte [Humans as a Scale: Architecture and Psychosocial Health in Affordable Housing. Needs, Analyses, Concepts]; Pabst Science Publisher: Lengerich, Germany, 2023. [Google Scholar]
- Barrios, B.A. Direct observation. In Handbook of Child and Adolescent Assessment; Ollendick Thomas, H., Hersen, M., Eds.; Allyn & Bacon: Boston, MA, USA, 1993; pp. 140–164. [Google Scholar]
- Tryon, W.W. Behavioral observation. In Behavioral Assessment: A Practical Handbook, 4th ed.; Bellack, A.S., Hersen, M., Eds.; Allyn & Bacon: Boston, MA, USA, 1998; pp. 79–103. [Google Scholar]
- Koppen, G.; Vollmer, T.; Iovița, C.; Schießl, L. Evaluating different architectural typologies of long-stay facilities on their impact on the Emotional Development in individuals with severe and profound Intellectual Disabilities. Lifesp. Dev. Ment. Health 2024. submission in progress. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse [Qualitative content analysis]. In Texte Verstehen: Konzepte, Methoden, Werkzeuge [Understanding Texts: Concepts, Methods, Tools]; Boehm, A., Mengel, A., Muhr, T., Eds.; UVK UniversitätsverlagKonstanz: Konstanz, Germany, 1994; Volume 14, pp. 159–175. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen und Techniken (Neuausgabe) [Qualitative Content Analysis: Basics and Techniques (New Edition)]; Beltz: Frankfurt am Main, Germany, 2010. [Google Scholar]
- Niezabitowski, A. Study of residential environment and psychological needs. Des. Stud. 1987, 8, 109–116. [Google Scholar] [CrossRef]
- Vink, P.; Imada, A.S.; Zink, K.J. Defining stakeholder involvement in participatory design processes. Appl. Ergon. 2008, 39, 519–526. [Google Scholar] [CrossRef]
- Spinuzzi, C. The methodology of participatory design. Tech. Commun. 2005, 52, 163–174. [Google Scholar]
- Huisman, E.; Appel-Meulenbroek, R.; Kort, H. A structural approach for the redesign of a small-scale care facility as a guideline for decision-makers. Intell. Build. Int. 2020, 12, 32–43. [Google Scholar] [CrossRef]
- Schalock, R.L.; Luckasson, R. American Association on Mental Retardation’s Definition, Classification, and System of Supports and Its Relation to International Trends and Issues in the Field of Intellectual Disabilities. J. Policy Pract. Intellect. Disabil. 2004, 1, 136–146. [Google Scholar] [CrossRef]
- Lawton, M.P.; Nahemow, L. Ecology and the aging process. In The Psychology of Adult Development and Aging; Eisdorfer, C., Lawton, M.P., Eds.; American Psychological Association: Washington, DC, USA, 1973. [Google Scholar]
- Sörgel, H. Theorie der Baukunst: Architektur-Ästhetik [Theory of Architecture: Architectural Aesthetics]; Piloty & Loehle: Munich, Germany, 1921. [Google Scholar]
- Schmarsow, A. Das Wesen der Architektonischen Schöpfung: Antrittsvorlesung, Gehalten in der Aula der K. Universität Leipzig am 8. November 1893 [The Essence of Architectural Creation: Inaugural Lecture, held in the Auditorium of the K. University of Leipzig on 8 November 1893]; Hiersemann: Leipzig, Germany, 1894. [Google Scholar]
- Schmarsow, A. Uber den Werth der Dimensionen im Menschlichen Raumgebilde [On the Value of Dimensions in the Human Spatial Structure]. In Berichte über die Verhandlungen der Königlich Sächsischen Gesellschaft der Wissenschaften zu Leipzig, Philologisch-Historische Klasse [Reports on the proceedings of the Royal Saxon Society of Sciences in Leipzig, Philological-Historical Class]; Königlich Sächsische Gesellschaft der Wissenschaften. Philologisch-Historische Klasse: Leipzig, Germany, 1896. [Google Scholar]
- Ellis, N.; Yi, Y.J. Systematic Review on Environmental Design for Adaptive and Problem Behaviors of People with Intellectual and Developmental Disabilities. HERD Health Environ. Res. Des. J. 2023, 16, 213–239. [Google Scholar] [CrossRef] [PubMed]
- Casson, J.; Hamdani, Y.; Dobranowski, K.; Lake, J.; Mcmorris, C.; Lunsky, Y.; Balogh, R. Housing Design and Modifications for Individuals With Intellectual and Developmental Disabilities and Complex Behavioral Needs: Scoping Review. J. Policy Pract. Intellect. Disabil. 2021, 18, 217–228. [Google Scholar] [CrossRef]
- Zisberg, A.; Young, H.M.; Schepp, K.; Zysberg, L. A concept analysis of routine: Relevance to nursing. J. Adv. Nurs. 2007, 57, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Parris, A.; Watson, K. Environmental interventions. In Challenging Behaviour and People with Learning Disabilities: A Handbook; Hardy, S., Joyce, T., Eds.; Pavilion Publishing and Media Ltd.: Shoreham-by-Sea, UK, 2011; pp. 1–11. [Google Scholar]
- Khare, R.; Mullick, A. Incorporating the Behavioral Dimension in Designing Inclusive Learning Environment for Autism. Archnet-Ijar 2009, 3, 45–64. [Google Scholar]
- Mostafa, M. Architecture for autism: Autism ASPECTSS in school design. Int. J. Archit. Res. ArchNet-IJAR 2014, 8, 143–158. [Google Scholar] [CrossRef]
- de Long, A.J. The use of scale-models in spatial-behavioral research. Man-Environ. Syst. 1976, 6, 179–182. [Google Scholar]
- de Long, A.J.; Lubar, J.F. Scale and Neurological Function, Summary; University of Tennessee Press: Knoxville, TN, USA, 1978. [Google Scholar]
- Wittmann, M. Perceived time in space. In Building to Heal: New Architectures for Hospitals; Vollmer, T.C., Lepik, A., Luksch, L., Eds.; Architangle: Berlin, Germany, 2023; pp. 206–209. [Google Scholar]
- Roos, B.A.; Mobach, M.; Heylighen, A. How Architecture Can Support Self-Regulating Interpersonal Distance for Individuals Showing Challenging Behaviour: A Case Study at a Very-Intensive-Care Facility. In Proceedings of the Design4Health 2020, Amsterdam, The Netherlands, 1–3 July 2020. [Google Scholar]
- Felce, D.; Emerson, E. Living with support in a home in the community: Predictors of behavioral development and household and community activity. Ment. Retard. Dev. Disabil. Res. Rev. 2001, 7, 75–83. [Google Scholar] [CrossRef]
- Karol, E.; Smith, D. Impact of Design on Emotional, Psychological, or Social Well-Being for People with Cognitive Impairment. HERD Health Environ. Res. Des. J. 2019, 12, 220–232. [Google Scholar] [CrossRef]
- Heller, T.; Miller, A.B.; Factor, A. Environmental characteristics of nursing homes and community-based settings, and the well-being of adults with intellectual disability. J. Intellect. Disabil. Res. 1998, 42, 418–428. [Google Scholar] [CrossRef]
- Carnemolla, P. Apartment Living and Community Care: Experiences of People with Intellectual Disability, Their Families, and Support Staff. Urban Plan. 2022, 7, 398–408. [Google Scholar] [CrossRef]
- Davydenko, M.; Peetz, J. Time grows on trees: The effect of nature settings on time perception. J. Environ. Psychol. 2017, 54, 20–26. [Google Scholar] [CrossRef]
- Berry, M.S.; Repke, M.A.; Nickerson, N.P.; Conway, L.G., III; Odum, A.L.; Jordan, K.E. Making Time for Nature: Visual Exposure to Natural Environments Lengthens Subjective Time Perception and Reduces Impulsivity. PLoS ONE 2015, 10, e0141030. [Google Scholar] [CrossRef]
- Aschoff, J. Circadian Timing. Ann. N. Y. Acad. Sci. 1984, 423, 442–468. [Google Scholar] [CrossRef]
- McGill, P.; Bradshaw, J.; Smyth, G.; Hurman, M.; Roy, A. Capable environments. Tizard Learn. Disabil. Rev. 2020, 25, 109–116. [Google Scholar] [CrossRef]
- Gbyl, K.; Østergaard Madsen, H.; Dunker Svendsen, S.; Petersen, P.M.; Hageman, I.; Volf, C.; Martiny, K. Depressed patients hospitalized in southeast-facing rooms are discharged earlier than patients in northwest-facing rooms. Neuropsychobiology 2017, 74, 193–201. [Google Scholar] [CrossRef]
- Koppen, G.; Vollmer, T.C. NKOC—Het Ontwikkelingsgericht Gebouw: Ontwerpuitgangspunten Resulterend uit Ontwerpend Onderzoek voor de Nieuwbouw van het Nederlands Kinder Oncologisch Centrum [NKOC—The Development-Oriented Building: Design Principles Resulting from Design Research for the New Building of the Dutch Paediatric Oncology Centre]; SKION: Den Haag, The Netherlands, 2010. [Google Scholar]
- Vollmer, T.C.; Koppen, G. The parent-child patient unit (PCPU): Evidence-based patient room design and parental distress in pediatric cancer centers. Int. J. Environ. Res. Public Health 2021, 18, 9993. [Google Scholar] [CrossRef]
- Vollmer, T.C.; Koppen, G.; Vraetz, T.; Niemeyer, C. Entwicklungsräume [Developmental spaces]. JuKiP-Ihr Fachmag. Für Gesundh.-Und Kinderkrankenpflege 2017, 6, 239–244. [Google Scholar]
- Vollmer, T.C.; Deubzer, H.; Koppen, G.; Kéré Francis, D.; Niemeyer, C.; Vraetz, T.; Iovița, C.; Kohler, K.; Bauer, M.; Eggers, I. Ren(n), Wenn du Kannst. Architektur und Psychosoziale Gesundheit Schwerkranker Kinder und Jugendlicher Sowie Ihrer Eltern im Krankenhaus [Run if You Can. Architecture and Psychosocial Health of Seriously Ill Children and Adolescents and Their Co-Admitted Parents]. BBSR-Online-Publikation 2024, 76. [Google Scholar]
- Bentham, J. The Panopticon Writings; Verso: New York, NY, USA, 1995. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vollmer, T.C.; Koppen, G.; Iovița, C.; Schießl, L. Therapeutic Architecture and Temporality: Evidence-Based Design for Long-Stay Facilities for Individuals with Severe Intellectual Disabilities and Challenging Behaviour. Architecture 2024, 4, 541-570. https://doi.org/10.3390/architecture4030029
Vollmer TC, Koppen G, Iovița C, Schießl L. Therapeutic Architecture and Temporality: Evidence-Based Design for Long-Stay Facilities for Individuals with Severe Intellectual Disabilities and Challenging Behaviour. Architecture. 2024; 4(3):541-570. https://doi.org/10.3390/architecture4030029
Chicago/Turabian StyleVollmer, Tanja C., Gemma Koppen, Claudia Iovița, and Lara Schießl. 2024. "Therapeutic Architecture and Temporality: Evidence-Based Design for Long-Stay Facilities for Individuals with Severe Intellectual Disabilities and Challenging Behaviour" Architecture 4, no. 3: 541-570. https://doi.org/10.3390/architecture4030029
APA StyleVollmer, T. C., Koppen, G., Iovița, C., & Schießl, L. (2024). Therapeutic Architecture and Temporality: Evidence-Based Design for Long-Stay Facilities for Individuals with Severe Intellectual Disabilities and Challenging Behaviour. Architecture, 4(3), 541-570. https://doi.org/10.3390/architecture4030029








