First Evidence of the Possible Influence of Avoiding Daily Liquid Intake from Plastic and Glass Beverage Bottles on Blood Pressure in Healthy Volunteers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Experimental Design
2.3. Data Collection
2.4. Statistical Analysis
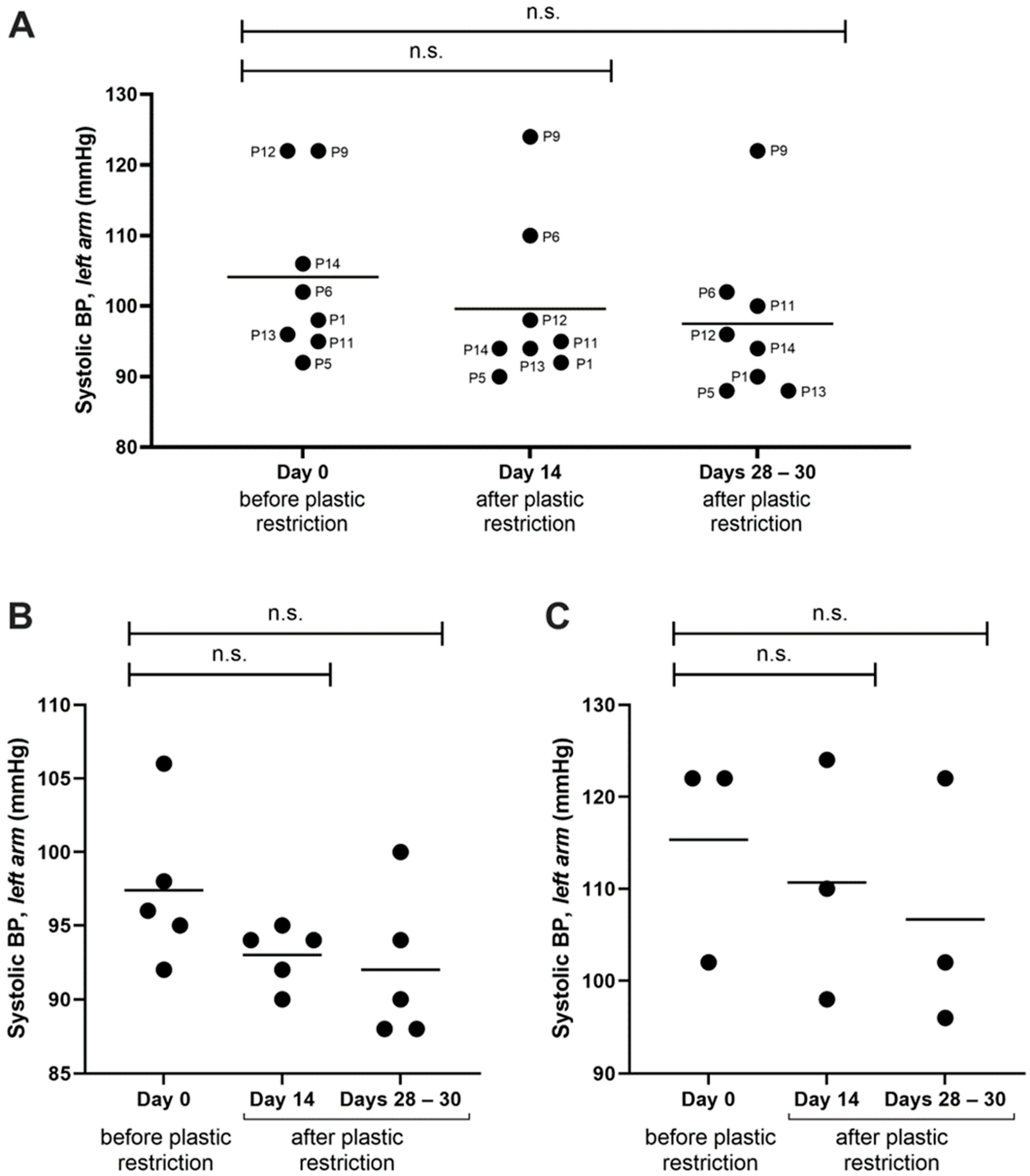
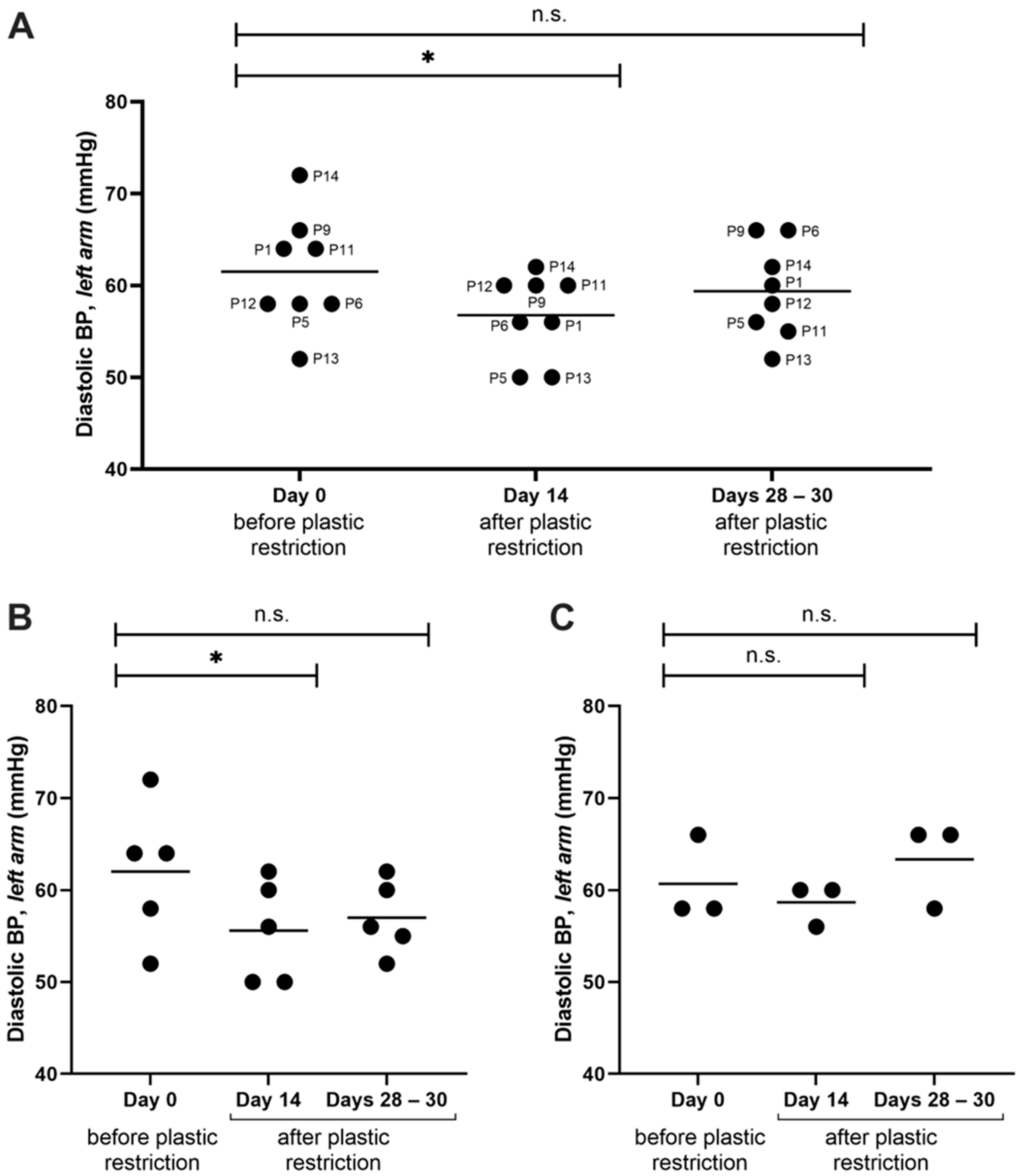
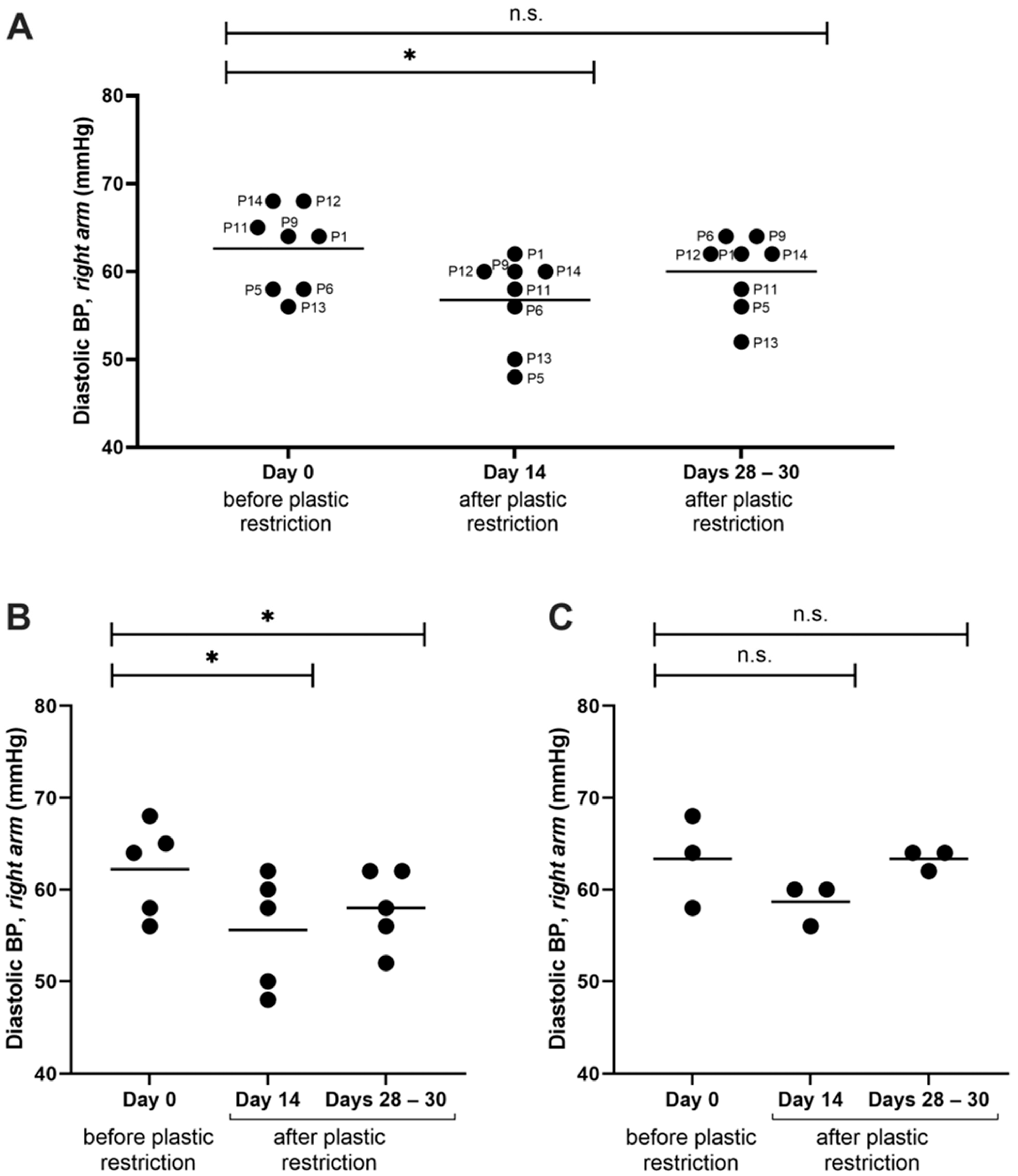
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Santos, L.H.M.L.M.; Insa, S.; Arxé, M.; Buttiglieri, G.; Rodríguez-Mozaz, S.; Barceló, D. Analysis of Microplastics in the Environment: Identification and Quantification of Trace Levels of Common Types of Plastic Polymers Using Pyrolysis-GC/MS. MethodsX 2023, 10, 102143. [Google Scholar] [CrossRef] [PubMed]
- Briassoulis, D. Agricultural Plastics as a Potential Threat to Food Security, Health, and Environment through Soil Pollution by Microplastics: Problem Definition. Sci. Total Environ. 2023, 892, 164533. [Google Scholar] [CrossRef] [PubMed]
- Zuri, G.; Karanasiou, A.; Lacorte, S. Microplastics: Human Exposure Assessment through Air, Water, and Food. Environ. Int. 2023, 179, 108150. [Google Scholar] [CrossRef] [PubMed]
- Gigault, J.; Halle, A.T.; Baudrimont, M.; Pascal, P.Y.; Gauffre, F.; Phi, T.L.; El Hadri, H.; Grassl, B.; Reynaud, S. Current Opinion: What Is a Nanoplastic? Environ. Pollut. Barking Essex 2018, 235, 1030–1034. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, N.B.; Hüffer, T.; Thompson, R.C.; Hassellöv, M.; Verschoor, A.; Daugaard, A.E.; Rist, S.; Karlsson, T.; Brennholt, N.; Cole, M.; et al. Are We Speaking the Same Language? Recommendations for a Definition and Categorization Framework for Plastic Debris. Environ. Sci. Technol. 2019, 53, 1039–1047. [Google Scholar] [CrossRef]
- Ramsperger, A.F.R.M.; Bergamaschi, E.; Panizzolo, M.; Fenoglio, I.; Barbero, F.; Peters, R.; Undas, A.; Purker, S.; Giese, B.; Lalyer, C.R.; et al. Nano- and Microplastics: A Comprehensive Review on Their Exposure Routes, Translocation, and Fate in Humans. NanoImpact 2023, 29, 100441. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Luo, C.; Wang, Y.; Zhao, Y.; Qiu, Y. Nanoplastics Dominate the Cotransport of Small-Scale Plastics in Seawater-Saturated Porous Media. Water Res. 2022, 221, 118773. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.B.; Böhmert, L.; Hsiao, I.L.; Braeuning, A.; Sieg, H. Complex Intestinal and Hepatic in Vitro Barrier Models Reveal Information on Uptake and Impact of Micro, Submicro and Nanoplastics. Environ. Int. 2023, 179, 108172. [Google Scholar] [CrossRef]
- Leslie, H.A.; van Velzen, M.J.M.; Brandsma, S.H.; Vethaak, A.D.; Garcia-Vallejo, J.J.; Lamoree, M.H. Discovery and Quantification of Plastic Particle Pollution in Human Blood. Environ. Int. 2022, 163, 107199. [Google Scholar] [CrossRef]
- Horvatits, T.; Tamminga, M.; Liu, B.; Sebode, M.; Carambia, A.; Fischer, L.; Püschel, K.; Huber, S.; Fischer, E.K. Microplastics Detected in Cirrhotic Liver Tissue. eBioMedicine 2022, 82, 104147. [Google Scholar] [CrossRef]
- Barshtein, G.; Arbell, D.; Yedgar, S. Hemolytic Effect of Polymeric Nanoparticles: Role of Albumin. IEEE Trans. NanoBioscience 2011, 10, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Fleury, J.B.; Baulin, V.A. Microplastics Destabilize Lipid Membranes by Mechanical Stretching. Proc. Natl. Acad. Sci. USA 2021, 118, e2104610118. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, P.M.; Saranya, V.; Vijayakumar, S.; Mythili Meera, M.; Ruprekha, S.; Kunal, R.; Pranay, A.; Thomas, J.; Mukherjee, A.; Chandrasekaran, N. Assessment on Interactive Prospectives of Nanoplastics with Plasma Proteins and the Toxicological Impacts of Virgin, Coronated and Environmentally Released-Nanoplastics. Sci. Rep. 2019, 9, 8860. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Choi, S.; Kim, D.; Park, H.J.; Bian, Y.; Choi, S.H.; Chung, H.Y.; Bae, O.N. Amine-Modified Nanoplastics Promote the Procoagulant Activation of Isolated Human Red Blood Cells and Thrombus Formation in Rats. Part. Fibre Toxicol. 2022, 19, 60. [Google Scholar] [CrossRef] [PubMed]
- McGuinnes, C.; Duffin, R.; Brown, S.L.; Mills, N.; Megson, I.L.; MacNee, W.; Johnston, S.; Lu, S.L.; Tran, L.; Li, R.; et al. Surface Derivatization State of Polystyrene Latex Nanoparticles Determines Both Their Potency and Their Mechanism of Causing Human Platelet Aggregation In Vitro. Toxicol. Sci. 2011, 119, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Li, Y.; Lee, M.; Andrikopoulos, N.; Lin, S.; Chen, C.; Leong, D.T.; Ding, F.; Song, Y.; Ke, P.C. Anionic Nanoplastic Exposure Induces Endothelial Leakiness. Nat. Commun. 2022, 13, 4757. [Google Scholar] [CrossRef]
- Lu, Y.; Cao, M.; Tian, M.; Huang, Q. Internalization and Cytotoxicity of Polystyrene Microplastics in Human Umbilical Vein Endothelial Cells. J. Appl. Toxicol. 2023, 43, 262–271. [Google Scholar] [CrossRef]
- Lu, Y.Y.; Li, H.; Ren, H.; Zhang, X.; Huang, F.; Zhang, D.; Huang, Q.; Zhang, X. Size-Dependent Effects of Polystyrene Nanoplastics on Autophagy Response in Human Umbilical Vein Endothelial Cells. J. Hazard. Mater. 2022, 421, 126770. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Amarakoon, D.; Wei, C.; Choi, K.Y.; Smolensky, D.; Lee, S.H. Adverse Effect of Polystyrene Microplastics (PS-MPs) on Tube Formation and Viability of Human Umbilical Vein Endothelial Cells. Food Chem. Toxicol. 2021, 154, 112356. [Google Scholar] [CrossRef]
- Walczak, A.P.; Hendriksen, P.J.M.; Woutersen, R.A.; Van Der Zande, M.; Undas, A.K.; Helsdingen, R.; Van Den Berg, H.H.J.; Rietjens, I.M.C.M.; Bouwmeester, H. Bioavailability and Biodistribution of Differently Charged Polystyrene Nanoparticles upon Oral Exposure in Rats. J. Nanoparticle Res. 2015, 17, 231. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhu, S.; Liu, Q.; Wei, J.; Jin, Y.; Wang, X.; Zhang, L. Polystyrene Microplastics Cause Cardiac Fibrosis by Activating Wnt/β-Catenin Signaling Pathway and Promoting Cardiomyocyte Apoptosis in Rats. Environ. Pollut. 2020, 265, 115025. [Google Scholar] [CrossRef] [PubMed]
- Liang, B.; Zhong, Y.; Huang, Y.; Lin, X.; Liu, J.; Lin, L.; Hu, M.; Jiang, J.; Dai, M.; Wang, B.; et al. Underestimated Health Risks: Polystyrene Micro- and Nanoplastics Jointly Induce Intestinal Barrier Dysfunction by ROS-Mediated Epithelial Cell Apoptosis. Part. Fibre Toxicol. 2021, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhuan, Q.; Zhang, L.; Meng, L.; Fu, X.; Hou, Y. Polystyrene Microplastics Induced Female Reproductive Toxicity in Mice. J. Hazard. Mater. 2022, 424, 127629. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xie, E.; Du, Z.; Peng, Z.; Han, Z.; Li, L.; Zhao, R.; Qin, Y.; Xue, M.; Li, F.; et al. Detection of Various Microplastics in Patients Undergoing Cardiac Surgery. Environ. Sci. Technol. 2023, 57, 10911–10918. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Wang, C.; Yang, Y.; Du, Z.; Li, L.; Zhang, M.; Ni, S.; Yue, Z.; Yang, K.; Wang, Y.; et al. Microplastics in Three Types of Human Arteries Detected by Pyrolysis-Gas Chromatography/Mass Spectrometry (Py-GC/MS). J. Hazard. Mater. 2024, 469, 133855. [Google Scholar] [CrossRef] [PubMed]
- Marfella, R.; Prattichizzo, F.; Sardu, C.; Fulgenzi, G.; Graciotti, L.; Spadoni, T.; D’Onofrio, N.; Scisciola, L.; La Grotta, R.; Frigé, C.; et al. Microplastics and Nanoplastics in Atheromas and Cardiovascular Events. N. Engl. J. Med. 2024, 390, 900–910. [Google Scholar] [CrossRef]
- Cary, C.M.; Seymore, T.N.; Singh, D.; Vayas, K.N.; Goedken, M.J.; Adams, S.; Polunas, M.; Sunil, V.R.; Laskin, D.L.; Demokritou, P.; et al. Single Inhalation Exposure to Polyamide Micro and Nanoplastic Particles Impairs Vascular Dilation without Generating Pulmonary Inflammation in Virgin Female Sprague Dawley Rats. Part. Fibre Toxicol. 2023, 20, 16. [Google Scholar] [CrossRef]
- Jones, A.E.; Watts, J.A.; Debelak, J.P.; Thornton, L.R.; Younger, J.G.; Kline, J.A. Inhibition of Prostaglandin Synthesis during Polystyrene Microsphere-Induced Pulmonary Embolism in the Rat. Am. J. Physiol. Lung Cell. Mol. Physiol. 2003, 284, L1072–L1081. [Google Scholar] [CrossRef]
- Mason, S.A.; Welch, V.G.; Neratko, J. Synthetic Polymer Contamination in Bottled Water. Front. Chem. 2018, 6, 407. [Google Scholar] [CrossRef]
- Giese, A.; Kerpen, J.; Weber, F.; Prediger, J. A Preliminary Study of Microplastic Abrasion from the Screw Cap System of Reusable Plastic Bottles by Raman Microspectroscopy. ACS EST Water 2021, 1, 1363–1368. [Google Scholar] [CrossRef]
- Schymanski, D.; Goldbeck, C.; Humpf, H.U.; Fürst, P. Analysis of Microplastics in Water by Micro-Raman Spectroscopy: Release of Plastic Particles from Different Packaging into Mineral Water. Water Res. 2018, 129, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Winkler, A.; Santo, N.; Ortenzi, M.A.; Bolzoni, E.; Bacchetta, R.; Tremolada, P. Does Mechanical Stress Cause Microplastic Release from Plastic Water Bottles? Water Res. 2019, 166, 115082. [Google Scholar] [CrossRef] [PubMed]
- Kankanige, D.; Babel, S. Smaller-Sized Micro-Plastics (MPs) Contamination in Single-Use PET-Bottled Water in Thailand. Sci. Total Environ. 2020, 717, 137232. [Google Scholar] [CrossRef] [PubMed]
- Oßmann, B.E.; Sarau, G.; Holtmannspötter, H.; Pischetsrieder, M.; Christiansen, S.H.; Dicke, W. Small-Sized Microplastics and Pigmented Particles in Bottled Mineral Water. Water Res. 2018, 141, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Zuccarello, P.; Ferrante, M.; Cristaldi, A.; Copat, C.; Grasso, A.; Sangregorio, D.; Fiore, M.; Oliveri Conti, G. Exposure to Microplastics (<10 μm) Associated to Plastic Bottles Mineral Water Consumption: The First Quantitative Study. Water Res. 2019, 157, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Vega-Herrera, A.; Llorca, M.; Borrell-Diaz, X.; Redondo-Hasselerharm, P.E.; Abad, E.; Villanueva, C.M.; Farré, M. Polymers of Micro(Nano) Plastic in Household Tap Water of the Barcelona Metropolitan Area. Water Res. 2022, 220, 118645. [Google Scholar] [CrossRef] [PubMed]
- Mintenig, S.M.; Löder, M.G.J.; Primpke, S.; Gerdts, G. Low Numbers of Microplastics Detected in Drinking Water from Ground Water Sources. Sci. Total Environ. 2019, 648, 631–635. [Google Scholar] [CrossRef]
- Bäuerlein, P.S.; Hofman-Caris, R.C.H.M.; Pieke, E.N.; Ter Laak, T.L. Fate of Microplastics in the Drinking Water Production. Water Res. 2022, 221, 118790. [Google Scholar] [CrossRef]
- Strand, J.; Feld, L.; Murphy, F.; Mackevica, A.; Hartmann, N.B. Analysis of Microplastic Particles in Danish Drinking Water–DTU Findit. Available online: https://findit.dtu.dk/en/catalog/5d4166d2d9001d32c978a8c4 (accessed on 6 October 2023).
- Uhl, W.; Eftekhardadkhah, M.; Svendsen, C. Mapping Microplastic in Norwegian Drinking Water, Norsk Vann Report 241/2018; 2018; ISBN 978-82-414-0427-6. [Google Scholar]
- Shen, M.; Zeng, Z.; Wen, X.; Ren, X.; Zeng, G.; Zhang, Y.; Xiao, R. Presence of Microplastics in Drinking Water from Freshwater Sources: The Investigation in Changsha, China. Environ. Sci. Pollut. Res. 2021, 28, 42313–42324. [Google Scholar] [CrossRef]
- Unser Trinkwasser. Mikroplastic. Available online: https://unsertrinkwasser.at/mikroplastik/ (accessed on 28 November 2023).
- Cheung, A.K.; Whelton, P.K.; Muntner, P.; Schutte, A.E.; Moran, A.E.; Williams, B.; Sarafidis, P.; Chang, T.I.; Daskalopoulou, S.S.; Flack, J.M.; et al. International Consensus on Standardized Clinic Blood Pressure Measurement—A Call to Action. Am. J. Med. 2023, 136, 438–445.e1. [Google Scholar] [CrossRef]
- Ogola, B.O.; Zimmerman, M.A.; Clark, G.L.; Abshire, C.M.; Gentry, K.M.; Miller, K.S.; Lindsey, S.H. New Insights into Arterial Stiffening: Does Sex Matter? Am. J. Physiol.-Heart Circ. Physiol. 2018, 315, H1073–H1087. [Google Scholar] [CrossRef]
- Baker, S.E.; Limberg, J.K.; Ranadive, S.M.; Joyner, M.J. Neurovascular Control of Blood Pressure Is Influenced by Aging, Sex, and Sex Hormones. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2016, 311, R1271–R1275. [Google Scholar] [CrossRef]
- Coovadia, Y.; Adler, T.E.; Steinback, C.D.; Fraser, G.M.; Usselman, C.W. Sex Differences in Dynamic Blood Pressure Regulation: Beat-by-Beat Responses to Muscle Sympathetic Nerve Activity. Am. J. Physiol.-Heart Circ. Physiol. 2020, 319, H531–H538. [Google Scholar] [CrossRef]
- Trinity, J.D.; Layec, G.; Hart, C.R.; Richardson, R.S. Sex-Specific Impact of Aging on the Blood Pressure Response to Exercise. Am. J. Physiol.-Heart Circ. Physiol. 2018, 314, H95–H104. [Google Scholar] [CrossRef]
- Ferreira, F.C.; Vaz Padilha, M.C.S.; Rocha, T.M.D.M.S.; Lima, L.S.; Carandina, A.; Bellocchi, C.; Tobaldini, E.; Montano, N.; Soares, P.P.D.S.; Rodrigues, G.D. Cardiovascular Autonomic Modulation during Passive Heating Protocols: A Systematic Review. Physiol. Meas. 2023, 44, 01TR01. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, M.M.; Ouladsmane, M.A.; Aouak, T.A.; ALOthman, Z.A.; Badjah Hadj Ahmed, A.Y. Determination of Phthalates in Bottled Waters Using Solid-Phase Microextraction and Gas Chromatography Tandem Mass Spectrometry. Chemosphere 2022, 304, 135214. [Google Scholar] [CrossRef]
- Vega-Herrera, A.; Garcia-Torné, M.; Borrell-Diaz, X.; Abad, E.; Llorca, M.; Villanueva, C.M.; Farré, M. Exposure to Micro(Nano)Plastics Polymers in Water Stored in Single-Use Plastic Bottles. Chemosphere 2023, 343, 140106. [Google Scholar] [CrossRef]
- Deng, T.; Xie, X.; Duan, J.; Chen, M. Di-(2-Ethylhexyl) Phthalate Induced an Increase in Blood Pressure via Activation of ACE and Inhibition of the Bradykinin-NO Pathway. Environ. Pollut. 2019, 247, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Kupsco, A.; Just, A.; Calafat, A.M.; Oken, E.; Braun, J.M.; Sanders, A.P.; Mercado-Garcia, A.; Cantoral, A.; Pantic, I.; et al. Maternal Phthalates Exposure and Blood Pressure during and after Pregnancy in the PROGRESS Study. Environ. Health Perspect. 2021, 129, 127007. [Google Scholar] [CrossRef] [PubMed]
- Bai, P.Y.; Wittert, G.; Taylor, A.W.; Martin, S.A.; Milne, R.W.; Jenkins, A.J.; Januszewski, A.S.; Shi, Z. The Association between Total Phthalate Concentration and Non-Communicable Diseases and Chronic Inflammation in South Australian Urban Dwelling Men. Environ. Res. 2017, 158, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Shen, Y.; Li, L.; Fan, T.; Wang, Y.; Wei, N. Phthalate Exposure and High Blood Pressure in Adults: A Cross-Sectional Study in China. Environ. Sci. Pollut. Res. 2018, 25, 15934–15942. [Google Scholar] [CrossRef] [PubMed]
- Shiue, I. Higher Urinary Heavy Metal, Arsenic, and Phthalate Concentrations in People with High Blood Pressure: US NHANES, 2009–2010. Blood Press. 2014, 23, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Shiue, I. Higher Urinary Heavy Metal, Phthalate, and Arsenic but Not Parabens Concentrations in People with High Blood Pressure, U.S. NHANES, 2011–2012. Int. J. Environ. Res. Public. Health 2014, 11, 5989–5999. [Google Scholar] [CrossRef] [PubMed]
- Bellavia, A.; Urch, B.; Speck, M.; Brook, R.D.; Scott, J.A.; Albetti, B.; Behbod, B.; North, M.; Valeri, L.; Bertazzi, P.A.; et al. DNA Hypomethylation, Ambient Particulate Matter, and Increased Blood Pressure: Findings from Controlled Human Exposure Experiments. J. Am. Heart Assoc. 2013, 2, e000212. [Google Scholar] [CrossRef] [PubMed]
- Kunovac, A.; Hathaway, Q.A.; Pinti, M.V.; Taylor, A.D.; Hollander, J.M. Cardiovascular Adaptations to Particle Inhalation Exposure: Molecular Mechanisms of the Toxicology. Am. J. Physiol.-Heart Circ. Physiol. 2020, 319, H282–H305. [Google Scholar] [CrossRef]
- Lederer, A.M.; Fredriksen, P.M.; Nkeh-Chungag, B.N.; Everson, F.; Strijdom, H.; De Boever, P.; Goswami, N. Cardiovascular Effects of Air Pollution: Current Evidence from Animal and Human Studies. Am. J. Physiol. Heart Circ. Physiol. 2021, 320, H1417–H1439. [Google Scholar] [CrossRef]

| Unit | Women | Men | |
|---|---|---|---|
| n | 5 | 3 | |
| Age | year | 25 ± 3.5 | 23 ± 1.5 |
| Size | Cm | 167 ± 5.1 | 180 ± 8.7 |
| Weight | Kg | 59 ± 4.7 | 77 ± 9.5 |
| BMI | kg/m2 | 21 ± 0.9 | 24 ± 0.9 |
| Sport activity | <3 h/week | 2 | 1 |
| >3 h/week | 3 | 2 |
| Subjects | Sex | Period Where the Plastic Diet Was Followed (%) | |
|---|---|---|---|
| Day 0–Day 14 | Day 14–Days 28–30 | ||
| P1 | W | 57 | 86 |
| P5 | W | 100 | 93 |
| P6 | M | 86 | 100 |
| P9 | M | 71 | 93 |
| P11 | W | 93 | 93 |
| P12 | M | 86 | 93 |
| P13 | W | 100 | 93 |
| P14 | W | 100 | 100 |
| Subjects | Sex | Systolic BP (mmHg) | ||
|---|---|---|---|---|
| Day 0 | Day 14 | Days 28–30 | ||
| P1 | W | 98 | 92 | 90 |
| P5 | W | 92 | 90 | 88 |
| P6 | M | 102 | 110 | 102 |
| P9 | M | 122 | 124 | 122 |
| P11 | W | 95 | 95 | 100 |
| P12 | M | 122 | 98 | 96 |
| P13 | W | 96 | 94 | 88 |
| P14 | W | 106 | 92 | 92 |
| Subjects | Sex | Systolic BP (mmHg) | ||
|---|---|---|---|---|
| Day 0 | Day 14 | Days 28–30 | ||
| P1 | W | 96 | 90 | 88 |
| P5 | W | 90 | 90 | 88 |
| P6 | M | 102 | 108 | 104 |
| P9 | M | 118 | 122 | 120 |
| P11 | W | 102 | 95 | 98 |
| P12 | M | 114 | 96 | 96 |
| P13 | W | 96 | 94 | 86 |
| P14 | W | 96 | 92 | 92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geppner, L.; Grammatidis, S.; Wilfing, H.; Henjakovic, M. First Evidence of the Possible Influence of Avoiding Daily Liquid Intake from Plastic and Glass Beverage Bottles on Blood Pressure in Healthy Volunteers. Microplastics 2024, 3, 419-432. https://doi.org/10.3390/microplastics3030026
Geppner L, Grammatidis S, Wilfing H, Henjakovic M. First Evidence of the Possible Influence of Avoiding Daily Liquid Intake from Plastic and Glass Beverage Bottles on Blood Pressure in Healthy Volunteers. Microplastics. 2024; 3(3):419-432. https://doi.org/10.3390/microplastics3030026
Chicago/Turabian StyleGeppner, Liesa, Sophie Grammatidis, Harald Wilfing, and Maja Henjakovic. 2024. "First Evidence of the Possible Influence of Avoiding Daily Liquid Intake from Plastic and Glass Beverage Bottles on Blood Pressure in Healthy Volunteers" Microplastics 3, no. 3: 419-432. https://doi.org/10.3390/microplastics3030026
APA StyleGeppner, L., Grammatidis, S., Wilfing, H., & Henjakovic, M. (2024). First Evidence of the Possible Influence of Avoiding Daily Liquid Intake from Plastic and Glass Beverage Bottles on Blood Pressure in Healthy Volunteers. Microplastics, 3(3), 419-432. https://doi.org/10.3390/microplastics3030026








