Abstract
The management of penetrating rectal trauma has evolved from a historic 4-D algorithm (Divert, Drain, Direct repair, and Distal washout) to a more selective approach. This case report describes a patient with multiple wounds, including a high-grade extraperitoneal rectal injury resulting from a pelvic explosive injury. The patient was successfully treated with intraluminal vacuum therapy (ILVT). This case highlights ILVT as a novel method for managing complicated blast-related rectal injuries. While there are limited publications on combat-related penetrating rectal injuries that provide evidence-based guidelines, we suggest an aggressive surgical approach combined with negative pressure wound therapy for optimal patient outcomes.
1. Introduction
The management of rectal injuries resulting from penetrating pelvic trauma or blunt fractures has evolved. Treatment approaches for injuries below peritoneal reflection remain a subject of debate. In 1989, Burch et al. proposed that diversion and pre-sacral drainage were sufficient for these injuries [1]. However, later studies indicated that pre-sacral drainage is ineffective in reducing infections and may even increase the risk of complications [2]. Current guidelines advise against pre-sacral drainage and distal washout [2,3,4]. The modern standard of care for extraperitoneal rectal injuries typically involves trans-anal repair, if feasible, and a loop sigmoid colostomy [3,4,5,6]. The choice of colostomy technique depends on the severity of the injury, the patient’s condition, and the surgeon’s preference. However, these approaches may not be effective for combat-related large defects with poor tissue quality or severe inflammation. Moreover, the exact size and depth of the defect can be unclear, potentially leading to inadequate drainage and persistent abscesses. Therefore, a treatment approach that effectively closes the perforation while controlling the source of infection in a managed manner is often preferred. This case report presents a high-energy rectal injury resulting from explosive pelvic trauma, which was treated with serial debridement, diversion, and ILVT.
2. Detailed Case Description
A 22-year-old male was evacuated from the war zone after sustaining multiple wounds from a pelvic blast caused by an anti-tank-guided missile. Following initial resuscitation at the Hadassah Hebrew University Medical Center in Jerusalem, including the administration of two units of whole blood, a pelvic injury assessment revealed significant wounds, including active bleeding in the right lateral–posterior thigh and a suspected exit wound in the left groin. The patient had intact lower extremity strength, sensation, and peripheral pulses. There was no blood at the urethral meatus, and a rectal examination revealed fresh blood with a preserved sphincter tone. Initially, packing was performed in the thigh wound and rectum. Contrast-enhanced CT imaging revealed an entry wound in the right thigh, a crushed ischium, a rectal injury with free air in adjusted perirectal tissue, and an S4 vertebra fracture (Figure 1). No vascular or bladder injuries were identified. During urgent surgery, the patient was positioned in lithotomy. An examination under anesthesia revealed rectal bleeding and 240-degree circumferential lacerations in the anterior wall 10 cm from the anal verge; hemostasis was achieved with cautery and packing. A loop sigmoid colostomy was performed without distal washout or pre-sacral drainage. Laparoscopic exploration showed minor fluid but no enteric contamination.
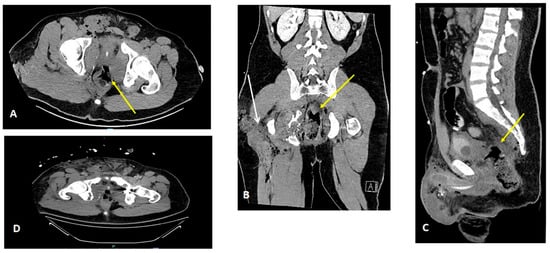
Figure 1.
Initial CT scan findings following resuscitation. A contrast-enhanced CT scan of the abdomen and pelvis showing axial, coronal, and sagittal sections (A–D). Perforation in the lateral–anterior rectal wall, following initial packing ((A–C), yellow arrow). Packing was also conducted for the right thigh wound ((B), white arrow). Complex pelvic fracture with embedded foreign metal bodies is also shown (D).
On postoperative day 1, the patient underwent secondary debridement of the right thigh wound, which extended deeply to the perirectal fat and was temporarily closed using negative pressure wound therapy (NPWT). A rectal examination revealed a full-thickness laceration in the anterior and anterolateral rectal walls, initially repaired with interrupted 1-0 Vicryl sutures. However, the repair failed within three days. By postoperative day 5, the patient developed pelvic sepsis with Escherichia coli bacteremia.
To manage the rectal wall gap, we utilized an endoluminal vacuum-assisted closure (VAC) system. A custom intraluminal NPWT sponge was created over a 12 Fr nasogastric tube, secured with 0-silk sutures, and shaped to fit the cavity while protecting the normal mucosa (Figure 2). We used 75 mm Hg as the controlled pressure for the rectal intraluminal VAC, separately from the NPWT applied to the thigh wound. The intraluminal VAC replacement was performed under general anesthesia in the Jack-knife position every 3 days. After six sponge replacements over a month, wounds in both the thigh and the rectal wall were successfully closed (Figure 3).
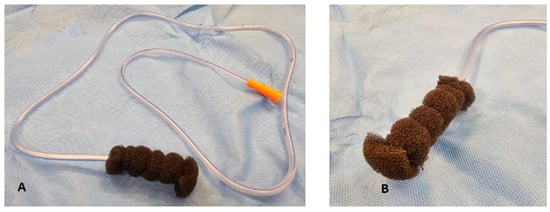
Figure 2.
Sponge preparation for intraluminal vacuum therapy. Intraluminal NPWT sponge constructed with a 12 Fr nasogastric tube (A) and secured at the top and bottom of the tube with a 0-silk suture by transfixing through the NG tube (B). The sponge is cut down and shaped to size according to the dimensions of the cavity to ensure normal mucosa is not subjected to NPWT.
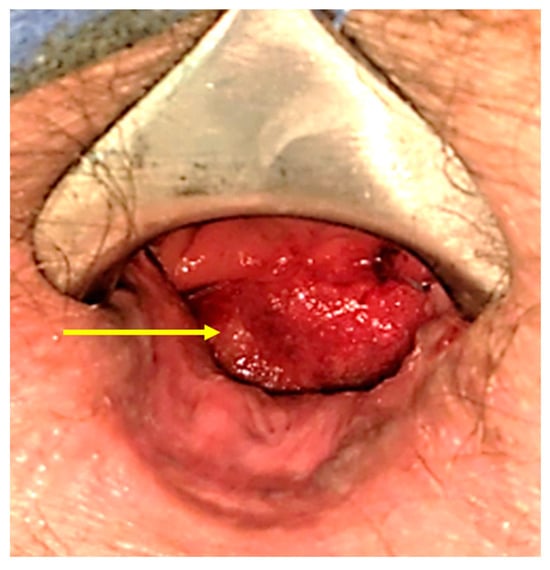
Figure 3.
An examination under anesthesia, conducted after six sessions of intraluminal vacuum therapy, revealed the closure of the anterior–lateral abscess cavity with the presence of granulation tissue (yellow arrow).
The patient received adequate antibiotic therapy. Despite sufficient venous thromboembolism prophylaxis, a pulmonary embolism was diagnosed and treated with a therapeutic Low-Molecular-Weight Heparin dose (Clexane), later converted to direct oral anticoagulant therapy (Apixaban). Following catheter removal, an incomplete urethral injury was observed. Although no leakage was seen on cystography, the Foley catheter was replaced after six weeks. A repeat urogram confirmed bladder and urethral integrity, allowing for the removal of the Foley catheter. The patient was discharged for outpatient follow-up and rehabilitation.
Before stoma reversal, anorectal manometry showed adequate sphincter strength, and transrectal ultrasound revealed a 10% deficiency in the external anal sphincter. A colonoscopy identified a small sinus at the rectal wall (Figure 4A,B). The stoma reversal was performed eight months after the injury and was initially successful. The patient reported good bowel control but experienced a sensation of incomplete evacuation, which improved over the course of biofeedback therapy.
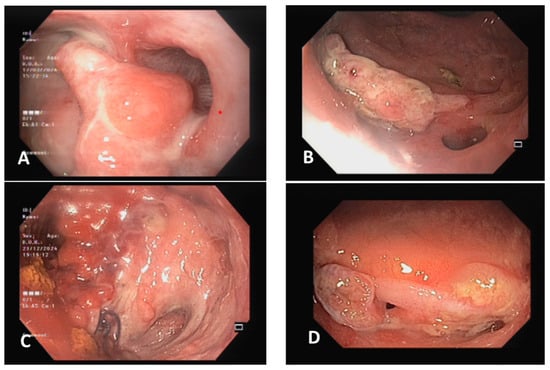
Figure 4.
The evolution of the rectal wall injury. (A) An ulcerated lesion of the anterolateral wall of the distal low rectum following intraluminal vacuum therapy. (B) Healthy granulation tissue and the absence of strictures observed after six endoluminal vacuum therapy sessions and stoma reversal, with two residual sinus openings. (C) Worsening ulceration three months post-reversal, without active bleeding. (D) Progressive granulation tissue formation and no evidence of stenosis or necrosis following hyperbaric oxygen therapy.
After the reversal, the patient, who was on Apixaban for a history of provoked pulmonary embolism, developed rectal bleeding that required a blood transfusion. Examination under anesthesia revealed an ulcer with granulation tissue on the anterolateral rectal wall as the source of bleeding. Hemostasis was achieved with bipolar cautery and sutures. Subsequent sigmoidoscopy showed a deep ulcer with granulation tissue but no active bleeding (Figure 4C).
The patient underwent multiple sessions of hyperbaric oxygen therapy (HBOT). A follow-up sigmoidoscopy three months later revealed that the ulcer had healed, although a small sinus opening was still suspected (Figure 4D). The patient has finished the HBOT treatments and is currently receiving physical therapy with biofeedback to support recovery.
3. Discussion
The VAC Therapy System, also known as NPWT, is effective at managing complex wounds, including diabetic foot ulcers [7], traumatic injuries [8], postoperative infections [9], and perineal wounds [10]. This system employs foam and controls negative pressure to promote healing by removing fluids, reducing edema, increasing blood flow, stimulating granulation tissue formation, and decreasing bacterial contamination [11]. It is also beneficial for local infections in the pelvis following colorectal surgery, with success rates of 75% in improving healing times for rectal anastomotic insufficiencies [12,13,14,15]. On average, complete healing with endoluminal vacuum therapy (EVT) takes about 47 days [14]. Studies have shown that early EVT treatment results in higher success rates compared to delayed treatment (75% versus 38%, respectively) [16], and EVT has been found to limit anastomotic dysfunction better than conservative management [17]. EVT is typically used alongside fecal diversion, as it has shown less success without it due to continued contamination and loss of the seal [14,18].
In civilian practice, most penetrating rectal injuries are caused by low-energy mechanisms and can easily be treated by performing diverting colostomy without the need for further repair of the rectal injury [4]. Data on high-energy blast injuries of the rectum, as encountered in the current case, are rare. The primary phase often includes initial cleaning, packing both the perineal wound and the pre-peritoneal space of the pelvis to control hemorrhage, and diverting colostomy. Repeat operations are required to complete the debridement of soft tissue wounds that heal by secondary intention. The colostomy may only then be closed if the rectum has been repaired with the preservation of anorectal function. This is particularly true for blast-related rectal injuries from anti-personnel-improvised explosive devices [19]. Ashley et al. reported a 15-year-old with a full-thickness anorectal injury successfully managed with 10 weeks of EVT after initial surgery, resulting in a healed defect, restored continuity, and preserved continence. Sozutek et al. described enema-induced rectal perforation treated with EVT, achieving complete resolution in 24 days [20,21].
This case report presents the first instance of using a rectal intraluminal VAC system for the closure of the full-thickness rectal wall defect resulting from penetrating explosive trauma. Our findings demonstrate that the ILVT procedure is both safe and effective in accelerating the healing of extensive extraperitoneal rectal injuries. Although commercial intraluminal NPWT systems are costly and require frequent sponge replacements (averaging 7–10 times), we utilized a more cost-effective alternative that could be easily prepared from VAC sponge material.
VAC therapy is usually effective at −125 mmHg; however, this high pressure can cause tissue necrosis around the sealed mucosa [22]. In our case, we reduced the pressure to −75 mmHg, which was well-tolerated by the patient and led to significant healing of the perforation within 30 days. This approach also potentially shortens hospitalization compared to other techniques.
Adverse events associated with ILVT include sponge dislocation, persistent anal pain, tissue necrosis from high pressure, discomfort from repeated surgeries, and minor bleeding due to granulation tissue ingrowth into the sponge [18,23]. The risks of fecal incontinence, fistula formation, and stricture formation (which occurs in 3–30% of patients following EVT) still have concerns that require long-term monitoring [17]. However, none of these issues were observed during our follow-up except for bleeding from granulation tissue following VAC therapy, which was successfully treated with hemostasis and HBOT.
Oxygen plays a key role in inflammation and wound healing, and HBOT has proven effective in treating complex wound-healing problems in other clinical settings. Oxygen is essential for tissue repair, stimulating collagen synthesis, matrix deposition, angiogenesis, epithelialization, and bacterial eradication [24,25,26].
The use of HBOT, which enhances oxygen supply to tissues, has been incorporated into the treatment of both surgical patients and those with chronic wounds [27,28]. Studies suggest that HBOT may be beneficial for treating colorectal anastomosis dehiscence [29,30].
4. Conclusions
ILVT accelerated recovery and effectively controlled the infection source. While this case is anecdotal and limits our ability to draw definitive conclusions about ILVT’s overall effectiveness for complex penetrating rectal injuries, our results suggest that it is a simple, safe, well-tolerated, and cost-effective alternative when surgical repair fails. Further prospective studies are needed to better understand the benefits and risks of ILVT for trauma patients.
Author Contributions
Conceptualization, M.B.; methodology, M.B.; software, M.B.; validation, M.B.; formal analysis, M.B.; investigation, M.B., O.C.-A., G.M., N.S., M.A.-G. and Y.S.P.; resources, M.B., O.C.-A., G.M., N.S., M.A.-G. and Y.S.P.; data curation, Y.S.P.; writing—original draft preparation, Y.S.P.; writing—review and editing, M.B.; visualization, M.B.; supervision, M.B.; project administration, M.B.; funding acquisition, M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This is not applicable due to the case report format.
Informed Consent Statement
Written informed consent was obtained from the patient.
Data Availability Statement
The data are unavailable due to privacy and stored in hospital medical records.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Burch, J.M.; Feliciano, D.V.; Mattox, K.L. Colostomy and drainage for civilian rectal injuries: Is that all? Ann. Surg. 1989, 209, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.V.R.; Teixeira, P.G.; Furay, E.; Sharpe, J.P.; Musonza, T.; Holcomb, J.; Bui, E.; Bruns, B.; Hopper, H.A.; Truitt, M.S.; et al. Contemporary management of rectal injuries at Level I trauma centers. J. Trauma Acute Care 2018, 84, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Velmahos, G.C.; Gomez, H.; Falabella, A.; Demetriades, D. Operative management of civilian rectal gunshot wounds: Simpler is better. World J. Surg. 2000, 24, 114–118. [Google Scholar] [CrossRef]
- Navsaria, P.H.; Edu, S.; Nicol, A.J. Civilian extraperitoneal rectal gunshot wounds: Surgical management made simpler. World J. Surg. 2007, 31, 1345–1351. [Google Scholar] [CrossRef]
- Bosarge, P.L.; Como, J.J.; Fox, N.; Falck-Ytter, Y.; Haut, E.R.; Dorion, H.A.; Patel, N.J.; Rushing, A.; Raff, L.A.; McDonald, A.A.; et al. Management of penetrating extraperitoneal rectal injuries: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 2016, 80, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Biffl, W.L.; Moore, E.E.; Feliciano, D.V.; Albrecht, R.M.; Croce, M.A.; Karmy-Jones, R.; Namias, N.; Rowell, S.E.; Schreiber, M.A.; Shatz, D.V.; et al. Management of colorectal injuries: A Western Trauma Association critical decisions algorithm. J. Trauma Acute Care Surg. 2018, 85, 1016–1020. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A. Diabetic Foot Study Consortium. Negative pressure wound therapy after partial diabetic foot amputation: A multicentre, randomized controlled trial. Lancet 2005, 12, 1704–1710. [Google Scholar] [CrossRef]
- Labler, L.; Trentz, O. The use of vacuum-assisted closure [VAC [®]] in soft tissue injuries after high energy pelvic trauma. Langenbecks Arch. Surg. 2007, 392, 601–609. [Google Scholar] [CrossRef]
- Fleck, T.M.; Fleck, M.; Moidl, R.; Czerny, M.; Koller, R.; Giovanoli, P.; Hiesmayer, M.J.; Zimpfer, D.; Wolner, E.; Grabenwoger, M.; et al. The vacuum-assisted closure system for the treatment of deep sternal wound infections after cardiac surgery. Ann. Thorac. Surg. 2002, 74, 1596–1600. [Google Scholar] [CrossRef]
- Schaffzin, D.M.; Douglas, J.M.; Stahl, T.J.; Smith, L.E. Vacuum-assisted closure of complex perineal wounds. Dis. Colon. Rectum 2004, 47, 1745–1748. [Google Scholar] [CrossRef]
- Morykwas, M.J.; Argenta, L.C.; Shelton-Brown, E.I.; McGuirt, W. Vacuum-assisted closure: A new method for wound control and treatment: Animal studies and basic foundation. Ann. Plast. Surg. 1997, 38, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Weidenhagen, R.; Spelsberg, F.; Lang, R.A.; Jauch, K.W.; Gruetzner, K.U. New method for sepsis control caused by anastomotic leakage in rectal surgery- the endo-VAC. Int. J. Colorectal Dis. 2003, 5, 1–4. [Google Scholar] [CrossRef]
- Weidenhagen, R.; Gruetzner, K.U.; Wiecken, T.; Spelsberg, F.; Jauch, K.W. Endoscopic vacuum-assisted closure of anastomotic leakage following anterior resection of the rectum. A new method. Surg. Endosc. Other Interv. Tech. 2008, 22, 1818–1825. [Google Scholar] [CrossRef]
- Shalaby, M.; Emile, S.; Elfeki, H.; Sakr, A.; Wexner, S.D.; Sileri, P. Systematic review of endoluminal vacuum-assisted therapy as salvage treatment for rectal anastomotic leakage. BJS Open 2019, 3, 153–160. [Google Scholar] [CrossRef]
- Soliman, F. Intraluminal negative pressure wound therapy and rectal anastomotic leak management: Regular vac sponge and a nasogastric tube. Ann. R. Coll. Surg. Engl. 2024, 106, 461–462. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Runkel, N.S.F.; Birk, M. Endo luminal negative pressure wound therapy [E-NPWT] for anastomotica leakage after rectal resection. Negat. Press. Wound Ther. J. 2014, 1, 1–6. [Google Scholar]
- Abdalla, S.; Cotte, E.; Epin, A.; Karoui, M.; Lefevre, J.H.; Berger, A.; Marchal, F.; Denost, Q.; Penna, C.; Benoist, S.; et al. Short-term and long-term outcome of endo luminal vacuum therapy for colorectal or coloanal anastomotic leakage: Results of a nationwide multicenter cohort study from the French Greccar group. Dis. Colon. Rectum 2020, 6, 371–380. [Google Scholar] [CrossRef]
- de Moura, D.T.H.; de Moura, B.F.B.H.; Manfredi, M.A.; Hathorn, K.E.; Bazarbashi, A.N.; Ribeiro, I.B.; de Moura, E.G.H.; Thompson, C.C. Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects. World J. Gastrointest. Endosc. 2019, 11, 329–344. [Google Scholar]
- Almogy, G.; Makori, A.; Zamir, O.; Pikarsky, A.J.; Rivkind, A.I. Rectal penetrating injuries from blast trauma. Isr. Med. Assoc. J. 2002, 4, 557–558. [Google Scholar]
- Althoff, A. Endoluminal vacuum-assisted closure for penetrating rectal injury in a pediatric patient. J. Pediatr. Surg. Case Rep. 2021, 70, 101885. [Google Scholar] [CrossRef]
- Sozutek, A. Endoluminal Vacuum Therapy (EVT) for the Treatment of Rectal Perforation Following Cleansing Enema Application. Cureus 2023, 15, e35939. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rosati, E.; Valeri, M.; Graziosi, L.; Amato, L.; Avenia, S.; Donini, A. Rectal perforation and perirectal abscess following stapled hemorrhoidectomy for prolapsed hemorrhoids successfully managed with Endo-SPONGE endoluminal vacuum-assisted wound closure system. Ann. Coloproctol. 2022, 38, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Zumblick, M.; Stathopoulos, P.; Gress, T.M.; Denzer, U.W. Endoscopic vacuum therapy for iatrogenic rectal perforation. Case Rep. Gastroenterol. 2022, 16, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Klemetti, E.; Rico-Vargas, S.; Mojon, P. Short duration hyperbaric oxygen treatment effects blood flow in rats: Pilot observations. Lab. Anim. 2005, 39, 116–121. [Google Scholar] [CrossRef]
- Kemik, O.; Adas, G.; Arikan, S.; Gurluler, E.; Dogan, Y.; Toklu, A.S.; Kapran, Y.; Kuntsal, L.; Purisa, S.; Kemik, A. Evaluation of the effects of hyperbaric oxygen treatment and enoxaparin on left colon anastomosis. An experimental study. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 2286–2292. [Google Scholar]
- Hohn, D.C.; MacKay, R.D.; Halliday, B.; Hunt, T.K. Effect of O2 tension on microbicidal function of leukocytes in wounds and in vitro. Surg. Forum. 1976, 27, 18–20. [Google Scholar]
- Dauwe, P.B.; Pulikkottil, B.J.; Lavery, L.; Stuzin, J.M.; Rohrich, R.J. Does hyperbaric oxygen therapy work in facilitating acute wound healing: A systematic review. Plast Reconstr Surg. 2014, 133, 208e–215e. [Google Scholar] [CrossRef]
- Svalestad, J.; Thorsen, E.; Vaagbø, G.; Hellem, S. Effect of hyperbaric oxygen treatment on oxygen tension and vascular capacity in irradiated skin and mucosa. Int. J. Oral. Maxillofac. Surg. 2014, 43, 107–112. [Google Scholar] [CrossRef]
- Brouwer, R.J.; Engberts, A.C.; Borger van der Burg, B.L.B.; van Dongen, T.T.V.; van Hulst, R.A.; Hoencamp, R. Meta-analysis on the effect of hyperbaric oxygen as adjunctive therapy in the outcome of anastomotic healing of experimental colorectal resections in rats. Diving Hyperb. Med. 2018, 48, 173–185. [Google Scholar] [CrossRef]
- Açiksari, K.; Eğin, S.; Hepgül, G.; Mirasoğlu, B.; Tanriverdi, G.; Kanber, D.S.; Demirci, S.; Doğan, H.; Özüçelik, D.N.; Toklu, A.S.; et al. Protective effect of hyperbaric oxygen treatment on rat intestinal mucosa after mesenteric ischemia and reperfusion. Diving Hyperb. Med. 2019, 49, 253–258. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).