Impact of Distal Tibiofibular Joint Anatomy on Reduction Outcome in Dynamic Suture Button Stabilization of the Distal Syndesmosis—A CT Analysis
Abstract
1. Introduction
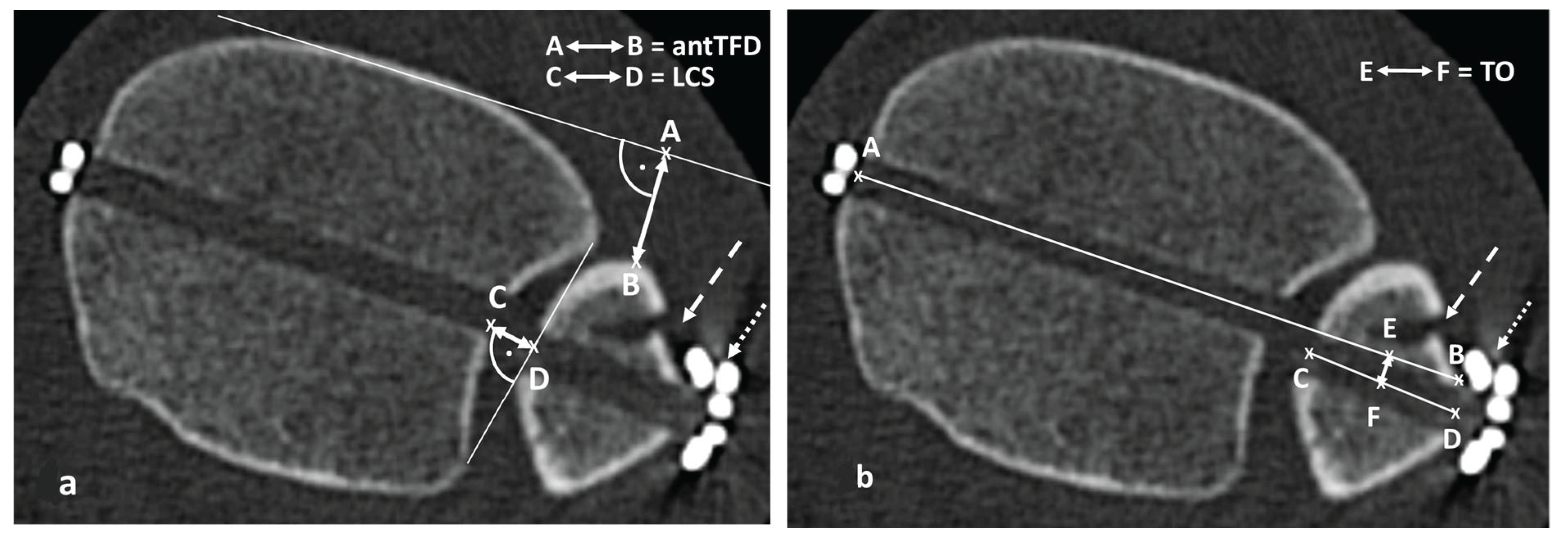
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Patients Overview
3.2. Parameters Describing the Anatomy of the DTFJ
3.3. Correlation Between CT-Morphological Reduction Outcome Parameters and Incisura Parameters
3.4. The Impact of Incisura Anatomy on the “Flexible Nature of Fixation”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burns, W.C.; Prakash, K.; Adelaar, R.; Beaudoin, A.; Krause, W. Tibiotalar Joint Dynamics: Indications for the Syndesmotic Screw—A Cadaver Study. Foot Ankle 1993, 14, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Sagi, H.C.; Shah, A.R.; Sanders, R.W. The Functional Consequence of Syndesmotic Joint Malreduction at a Minimum 2-Year Follow-Up. J. Orthop. Trauma 2012, 26, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.R.; Diep, L.M.; Frihagen, F.; Hellund, J.C.; Madsen, J.E.; Figved, W. Importance of Syndesmotic Reduction on Clinical Outcome After Syndesmosis Injuries. J. Orthop. Trauma 2019, 33, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Hennings, R.; Souleiman, F.; Heilemann, M.; Hennings, M.; Klengel, A.; Osterhoff, G.; Hepp, P.; Ahrberg, A.B. Suture button versus syndesmotic screw in ankle fractures—Evaluation with 3D imaging-based measurements. BMC Musculoskelet. Disord. 2021, 22, 970. [Google Scholar] [CrossRef]
- Spindler, F.T.; Gaube, F.P.; Böcker, W.; Polzer, H.; Baumbach, S.F. Compensation of Dynamic Fixation Systems in the Quality of Reduction of Distal Tibiofibular Joint in Acute Syndesmotic Complex Injuries: A CT-Based Analysis. Foot Ankle Int. 2022, 43, 1393–1401. [Google Scholar] [CrossRef]
- Boszczyk, A.; Kwapisz, S.; Krümmel, M.; Grass, R.; Rammelt, S. Correlation of Incisura Anatomy with Syndesmotic Malreduction. Foot Ankle Int. 2017, 39, 369–375. [Google Scholar] [CrossRef]
- Cherney, S.M.; Spraggs-Hughes, A.G.; McAndrew, C.M.; Ricci, W.M.; Gardner, M.J. Incisura Morphology as a Risk Factor for Syndesmotic Malreduction. Foot Ankle Int. 2016, 37, 748–754. [Google Scholar] [CrossRef]
- Boszczyk, A.; Rammelt, S. Syndesmotic Anatomy as a Risk Factor for Syndesmotic Injury and Syndesmotic Malreduction. Foot Ankle Orthop. 2018, 3, 2473011418S0016. [Google Scholar] [CrossRef]
- Laflamme, M.; Belzile, E.L.; Bédard, L.; Bekerom, M.P.J.v.D.; Glazebrook, M.; Pelet, S. A Prospective Randomized Multicenter Trial Comparing Clinical Outcomes of Patients Treated Surgically With a Static or Dynamic Implant for Acute Ankle Syndesmosis Rupture. J. Orthop. Trauma 2015, 29, 216–223. [Google Scholar] [CrossRef]
- Naqvi, G.A.; Cunningham, P.; Lynch, B.; Galvin, R.; Awan, N. Fixation of Ankle Syndesmotic Injuries: Comparison of TightRope Fixation and Syndesmotic Screw Fixation for Accuracy of Syndesmotic Reduction. Am. J. Sports Med. 2012, 40, 2828–2835. [Google Scholar] [CrossRef]
- Kortekangas, T.; Savola, O.; Flinkkilä, T.; Lepojärvi, S.; Nortunen, S.; Ohtonen, P.; Katisko, J.; Pakarinen, H. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury 2015, 46, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Westermann, R.W.; Rungprai, C.; Goetz, J.E.; Femino, J.; Amendola, A.; Phisitkul, P. The Effect of Suture-Button Fixation on Simulated Syndesmotic Malreduction: A Cadaveric Study. J. Bone Jt. Surg. 2014, 96, 1732–1738. [Google Scholar] [CrossRef] [PubMed]
- Kimura, S.; Yamaguchi, S.; Ono, Y.; Watanabe, S.; Akagi, R.; Sasho, T.; Ohtori, S. Changes in the Syndesmotic Reduction After Syndesmotic Suture-Button Fixation for Ankle Malleolar Fractures: 1-Year Longitudinal Evaluations Using Computed Tomography. Foot Ankle Int. 2021, 42, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- Hennings, R.; Fuchs, C.; Spiegl, U.J.; Theopold, J.; Souleiman, F.; Kleber, C.; Ahrberg, A.B. “Flexible nature of fixation” in syndesmotic stabilization of the inferior tibiofibular joint affects the radiological reduction outcome. Int. Orthop. 2022, 46, 2649–2657. [Google Scholar] [CrossRef]
- Dikos, G.D.; Heisler, J.D.; Choplin, R.H.; Weber, T.G. Normal Tibiofibular Relationships at the Syndesmosis on Axial CT Imaging. J. Orthop. Trauma 2012, 26, 433–438. [Google Scholar] [CrossRef]
- Park, C.H.; Kim, G.B. Tibiofibular relationships of the normal syndesmosis differ by age on axial computed tomography—Anterior fibular translation with age. Injury 2019, 50, 1256–1260. [Google Scholar] [CrossRef]
- Souleiman, F.; Heilemann, M.; Hennings, R.; Hennings, M.; Klengel, A.; Hepp, P.; Osterhoff, G.; Ahrberg, A.B. A standardized approach for exact CT-based three-dimensional position analysis in the distal tibiofibular joint. BMC Med. Imaging 2021, 21, 41. [Google Scholar] [CrossRef]
- Gardner, M.J.; Demetrakopoulos, D.; Briggs, S.M.; Helfet, D.L.; Lorich, D.G. Malreduction of the Tibiofibular Syndesmosis in Ankle Fractures. Foot Ankle Int. 2006, 27, 788–792. [Google Scholar] [CrossRef]
- Ebraheim, N.A.; Mekhail, A.O.; Gargasz, S.S. Ankle Fractures Involving the Fibula Proximal to the Distal Tibiofibular Syndesmosis. Foot Ankle Int. 1997, 18, 513–521. [Google Scholar] [CrossRef]
- Marmor, M.; Hansen, E.; Han, H.K.; Buckley, J.; Matityahu, A. Limitations of Standard Fluoroscopy in Detecting Rotational Malreduction of the Syndesmosis in an Ankle Fracture Model. Foot Ankle Int. 2011, 32, 616–622. [Google Scholar] [CrossRef]
- Kubik, J.F.; Rollick, N.C.; Bear, J.; Diamond, O.; Nguyen, J.T.; Kleeblad, L.J.; Helfet, D.L.; Wellman, D.S. Assessment of malreduction standards for the syndesmosis in bilateral CT scans of uninjured ankles. Bone Jt. J. 2021, 103-B, 178–183. [Google Scholar] [CrossRef]
- Rammelt, S.; Boszczyk, A. Computed Tomography in the Diagnosis and Treatment of Ankle Fractures: A Critical Analysis Review. JBJS Rev. 2018, 6, e7. [Google Scholar] [CrossRef] [PubMed]
- Buckley R., E.; Moran, C.G.; Apivatthakakul, T. (Eds.) AO Principles of Fracture Management: Vol. 1: Principles, Vol. 2: Specific Fractures; Georg Thieme Verlag: Stuttgart, Germany, 2018. [Google Scholar]
- Meinberg, E.; Agel, J.M.; Roberts, C.M.; Karam, M.D.; Kellam, J. Karam Fracture and Dislocation Classification Compendium—2018. J. Orthop. Trauma 2018, 32, S1–S10. [Google Scholar] [CrossRef]
- Pakarinen, H.; Flinkkilä, T.; Ohtonen, P.; Hyvönen, P.; Lakovaara, M.; Leppilahti, J.; Ristiniemi, J. Intraoperative Assessment of the Stability of the Distal Tibiofibular Joint in Supination-External Rotation Injuries of the Ankle: Sensitivity, Specificity, and Reliability of Two Clinical Tests. J. Bone Jt. Surg. 2011, 93, 2057–2061. [Google Scholar] [CrossRef]
- Rüedi, T.P.; Murphy, W.M. AO Principles of Fracture Management; Thieme: Stuttgart, Germany; New York, NY, USA; Davos, Switzerland, 2000. [Google Scholar]
- Cotton, F.J.; Cotton, F.J. Dislocations and Joint-Fractures-Digital Collections-National Library of Medicine. Available online: https://collections.nlm.nih.gov/catalog/nlm:nlmuid-36210580r-bk (accessed on 2 November 2020).
- Matuszewski, P.E.; Dombroski, D.; Lawrence, J.T.R.; Esterhai, J.L.; Mehta, S. Prospective Intraoperative Syndesmotic Evaluation During Ankle Fracture Fixation: Stress External Rotation Versus Lateral Fibular Stress. J. Orthop. Trauma 2015, 29, e157–e160. [Google Scholar] [CrossRef] [PubMed]
- Cottom, J.M.; Hyer, C.F.; Philbin, T.M.; Berlet, G.C. Treatment of Syndesmotic Disruptions with the Arthrex Tightrope™: A Report of 25 Cases. Foot Ankle Int. 2008, 29, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Lepojärvi, S.; Pakarinen, H.; Savola, O.; Haapea, M.; Sequeiros, R.B.; Niinimäki, J. Posterior Translation of the Fibula May Indicate Malreduction: CT Study of Normal Variation in Uninjured Ankles. J. Orthop. Trauma 2014, 28, 205–209. [Google Scholar] [CrossRef]
- Ahrberg, A.B.; Hennings, R.; von Dercks, N.; Hepp, P.; Josten, C.; Spiegl, U.J. Validation of a new method for evaluation of syndesmotic injuries of the ankle. Int. Orthop. 2020, 44, 2095–2100. [Google Scholar] [CrossRef]
- Schon, J.M.; Brady, A.W.; Krob, J.J.; Lockard, C.A.; Marchetti, D.C.; Dornan, G.J.; Clanton, T.O. Defining the three most responsive and specific CT measurements of ankle syndesmotic malreduction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2863–2876. [Google Scholar] [CrossRef]
- Nault, M.-L.; Hébert-Davies, J.; Laflamme, G.-Y.; Leduc, S. CT Scan Assessment of the Syndesmosis: A New Reproducible Method. J. Orthop. Trauma 2013, 27, 638–641. [Google Scholar] [CrossRef]
- Boszczyk, A.; Kwapisz, S.; Krümmel, M.; Grass, R.; Rammelt, S. Anatomy of the tibial incisura as a risk factor for syndesmotic injury. Foot Ankle Surg. 2019, 25, 51–58. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Cosgrove, C.T.; Putnam, S.M.; Cherney, S.M.; Ricci, W.M.; Spraggs-Hughes, A.M.; McAndrew, C.M.M.; Gardner, M.J. Medial Clamp Tine Positioning Affects Ankle Syndesmosis Malreduction. J. Orthop. Trauma 2017, 31, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.N.; Barei, D.P.; Iaquinto, J.M.; Ledoux, W.R.; Beingessner, D.M. Iatrogenic Syndesmosis Malreduction via Clamp and Screw Placement. J. Orthop. Trauma 2013, 27, 100–106. [Google Scholar] [CrossRef] [PubMed]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Parameter Assessing DTFJ | All N = 44 | Range Min–Max | Female N = 21 | Male N = 23 | p |
|---|---|---|---|---|---|
| DI in mm (SD) | 3.8 (1.2) | 1.3–7.2 | 3.3 (1.2) | 4.3 (1.1) | 0.003 1 |
| LCS in mm (SD) | 3.5 (1.1) | 1.2–5.8 | 3.4 (1.2) | 3.6 (1.1) | 0.378 1 |
| FE in mm (SD) | 0.4 (1.4) | −2.6–3.6 | 0.1 (1.3) | 0.7 (1.4) | 0.196 1 |
| ROI in degrees (SD) | 96 (4) | 85–109 | 96 (4) | 96 (4) | 0.878 1 |
| NTDA in degrees (SD) | 8 (5) | −2–18 | 8 (6) | 8 (4) | 0.672 1 |
| antTFD in mm (SD) | 11.2 (2.8) | 4.4–18.7 | 10.8 (2.2) | 11.7 (3.3) | 0.244 1 |
| Parameter assessing the CT-morphological reduction outcome | |||||
| ΔLCS in mm (SD) | 0.7 (1.5) | −2.7–5.5 | 0.7 (1.9) | 0.7 (1.1) | 0.622 1 |
| ΔantTFD in mm (SD) | 0.4 (2.4) | −4.1–9.0 | 0.2 (2.3) | 0.6 (2.8) | 0.689 1 |
| ΔNTDA in degrees (SD) | 2 (1.4) | −11–9 | 2 (4) | 1 (3) | 0.300 1 |
| TO in mm (SD) | 1.2 (1.4) | −2.88–5.7 | 1.4 (1.0) | 0.9 (1.8) | 0.118 1 |
| Native Side | ID | ROI | FE | LCS | NTDA |
|---|---|---|---|---|---|
| DI | −0.197 | 0.662 | 0.218 | 0.159 | |
| ROI | −0.197 | −0.232 | −0.081 | 0.090 | |
| FE | 0.662 | −0.232 | −0.466 | 0.379 | |
| age | 0.128 | −0.073 | 0.401 | −0.444 | 0.128 |
| Congruity | N | DI in mm | ROI in Degrees | FE in mm | NTDA in Degree | LCS in mm | |
|---|---|---|---|---|---|---|---|
| |ΔLCS| in mm | <−1 mm * | N = 8 | 3.4 (1.1) | 97 (5) | 0.1 (1.0) | 6 (4) | 3.9 (1.7) |
| ana | N = 21 | 3.7 (1.2) | 96 (4) | 0.9 (1.4) | 8 (5) | 3.6 (1.0) | |
| >1 mm * | N = 15 | 4.2 (1.4) | 96 (4) | 1.1(1.4) | 8 (4) | 3.1 (1.0) | |
| p | 0.149 1 | 0.681 1 | 0.047 1 | 0.686 1 | 0.238 1 | ||
| |ΔantTFD| in mm | <−1 mm * | N = 14 | 3.4 (1.3) | 95 (4) | 0.5 (0.8) | 7 (5) | 3.2 (1.4) |
| Ana | N = 10 | 3.9 (1.3) | 98 (5) | 0.2 (1.8) | 8 (5) | 3.7 (1.1) | |
| >1 mm * | N = 20 | 4.0 (1.2) | 95 (4) | 0.4 (1.5) | 9 (5) | 3.5 (1.0) | |
| p | 0.3591 | 0.691 1 | 0.743 1 | 0.545 | 0.522 | ||
| |ΔNTDA| in degree | <−5° * | N = 3 | 4 (1) | 95° (9) | 1.0 (0.5) | 10 (8) | 3.2 (1.0) |
| Ana | N = 39 | 4 (1) | 96° (4) | 0.4 (1.4) | 8 (5) | 3.5 (1.2) | |
| >5° * | N = 12 | 4 (1) | 95° (4) | 0.4 (1.5) | 7 (5) | 3.5 (1.1) | |
| P | 0.852 1 | 0.404 1 | 0.617 1 | 0.741 1 | 0.896 1 | ||
| |TO| In mm | <1 mm * | N = 25 | 3.7 (1.2) | 95 (2) | 0.4 (1.5) | 7 (5) | 3.3 (1.0) |
| >1 mm * | N = 20 | 3.9 (1.2 | 96 (6) | 0.4 (1.3) | 9 (4) | 3.8 (1.2) | |
| P | 0.465 1 | 0.568 1 | 0.781 1 | 0.146 1 | 0.121 1 |
| Parameters of Native Incisura | Parameters Assessing the Quality of Reduction of the DTFJ | |||
|---|---|---|---|---|
| ΔLCS | ΔNTDA | ΔantTFD | TO | |
| DI | 0.058 | −0.087 | 0.024 | −0.141 |
| ROI | −0.231 | −0.064 | −0.018 | −0.015 |
| FE | 0.334 | −0.109 | −0.112 | −0.110 |
| LCS | −0.554 | 0.101 | 0.001 | −0.052 |
| NTDA | 0.254 | −0.362 | 0.024 | −0.122 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hennings, R.; Fuchs, C.; Souleiman, F.; Jeanette, H.; Spiegl, U.J.; Kleber, C.; Ahrberg-Spiegl, A.B. Impact of Distal Tibiofibular Joint Anatomy on Reduction Outcome in Dynamic Suture Button Stabilization of the Distal Syndesmosis—A CT Analysis. Trauma Care 2025, 5, 10. https://doi.org/10.3390/traumacare5020010
Hennings R, Fuchs C, Souleiman F, Jeanette H, Spiegl UJ, Kleber C, Ahrberg-Spiegl AB. Impact of Distal Tibiofibular Joint Anatomy on Reduction Outcome in Dynamic Suture Button Stabilization of the Distal Syndesmosis—A CT Analysis. Trauma Care. 2025; 5(2):10. https://doi.org/10.3390/traumacare5020010
Chicago/Turabian StyleHennings, Robert, Carolin Fuchs, Firas Souleiman, Henkelmann Jeanette, Ullrich Joseph Spiegl, Christian Kleber, and Annette B. Ahrberg-Spiegl. 2025. "Impact of Distal Tibiofibular Joint Anatomy on Reduction Outcome in Dynamic Suture Button Stabilization of the Distal Syndesmosis—A CT Analysis" Trauma Care 5, no. 2: 10. https://doi.org/10.3390/traumacare5020010
APA StyleHennings, R., Fuchs, C., Souleiman, F., Jeanette, H., Spiegl, U. J., Kleber, C., & Ahrberg-Spiegl, A. B. (2025). Impact of Distal Tibiofibular Joint Anatomy on Reduction Outcome in Dynamic Suture Button Stabilization of the Distal Syndesmosis—A CT Analysis. Trauma Care, 5(2), 10. https://doi.org/10.3390/traumacare5020010





