Abstract
Background: Injuries of the hip extensors are not uncommon, with those of the hamstrings being frequent among athletes. On the contrary, isolated injuries of the gluteus maximus muscle have been barely reported in the literature. Case Report: We present a case of a 63-year-old male water aerobics trainer with an acute tear of the right gluteus maximus tendon and describe the clinical presentation, imaging studies, surgical treatment, and functional outcome one year after surgery.
1. Introduction
While chronic injuries of the gluteus medius and minimus tendons are frequent among senior middle-aged women and middle-aged men [1], isolated injuries of the gluteus maximus muscle could be incidentally detected through imaging while looking for other pathologies in the gluteal region. The gluteus maximus muscle is the outermost muscle of the posterior part of the pelvic girdle, and it gives the buttocks its bulky and curvy shape [2]. Two-thirds of the proximal part of the muscle insert fibers at the iliotibial band (ITB), while the remaining part inserts at the linea aspera [3]. The distal portion inserts at the gluteal tuberosity [3]. Additionally, being considered the primary extensor of the hip joint, it plays a vital role in maintaining the erect posture of the upper part of the body [2]. To our knowledge, this sort of injury has only been reported twice in the past [4,5].
Considering the identification of the lesion primarily and addressing it adequately important for the functional outcome, we present this case report to raise awareness of these rare injuries. The patient was informed that this case report would be submitted for publication, and he provided consent.
2. Case Report
A 63-year-old male professional water aerobics trainer presented in our emergency department after having noticed a sudden stabbing pain over the proximal right thigh four days earlier during a training session, performing circulatory pelvic muscles strengthening exercises. There was no history of previous illnesses or injuries to the hip or groin, and no medications were taken by him on a regular basis.
On physical examination, inspecting the patient while standing upright, a minimal swelling over the skin at the right greater trochanter compared to the left side was noticed, along with a slightly limping gait. The Trendelenburg sign was negative. The FADIR (Flexion, Adduction, Internal Rotation) test was positive as an indicator of femoroacetabular impingement (FAI) of the right hip joint. With the patient lying in the prone position, pain over the lateral side of the right thigh was triggered while extending the right hip joint against resistance. The neurological and vascular examination was within normal limits.
3. Imaging
In accordance with the clinical findings, the x-ray frog leg view showed CAM deformity of the right hip and signs of osteoarthritis, as shown in Figure 1A. The measurement of the alpha angle on the same radiograph, as first described by Nötzli [6], showed a pathological value of 59° (Figure 1B).
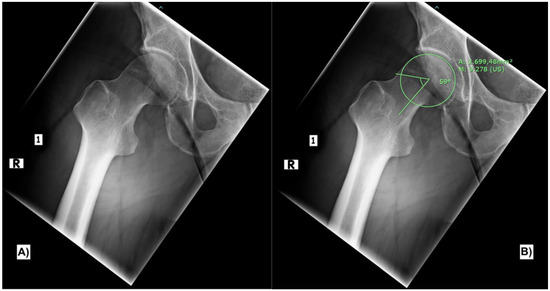
Figure 1.
X-ray frog leg view of the right hip joint showing the CAM deformity (A). Measurement of the alpha angle (B).
The main finding in the MRI was a localized collection of hematoma medial to the iliotibial band, between the iliotibial band and the greater trochanter (Figure 2). Compared to the left side, there was an increased distancing of the fascia lata or the iliotibial tract from the greater trochanter and a redundant, wavy cross-section of the fascia lata at the proximal thigh. Further, hematoma was also detected superficially, subcutaneously at the periphery of the iliotibial band and the gluteus maximus tendon. The insertion of the gluteus maximus muscle at the gluteal tuberosity of the femur was intact. Still, the insertion of the gluteus maximus tendon into the intermuscular septum was elevated and injured (Figure 2). Neither the gluteus medius nor the gluteus minimus tendons were injured. Also, the insertion of the quadratus femoris tendon and the insertion of the iliopsoas tendon at the lesser trochanter were intact. Some fluid was surrounding the tensor fasciae latae muscle. Otherwise, inconspicuous internal signals around the adductors and hip flexors were noticed.
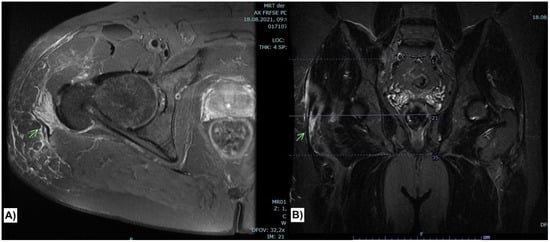
Figure 2.
Axial FRFSE PD sequence (A) showing collection of hematoma medial to the iliotibial band with disruption of the superficial insertion of the gluteus maximus muscle at the iliotibial band and intermuscular septum (Arrow). The injury is again demonstrated in coronal STIR sequence (B).
4. Surgical Intervention
After obtaining informed consent, surgery was done under general anesthesia with the patient lying in the lateral decubitus position. The incision simulated a modified anterolateral approach, as described by Burwell and Scott [7]. First, the anatomical landmarks for the incision were marked as shown in Figure 3. The incision was slightly extended distally along the iliotibial band. After subcutaneous dissection, the posterior border of the tensor fascia latae muscle and the gluteal aponeurosis were identified.

Figure 3.
Anatomical landmarks for the surgical approach.
The tear was located at the intermuscular septum perpendicular to the muscle fibers’ direction, as shown in Figure 4. The distal stump of the tendon was mobilized and released from the surrounding tissue. That required limited dissection. The frayed end of the tendon was debrided, yet the bulk of the tendon was preserved. The tendon was then reattached to the ITB using absorbable number 2 Vicryl sutures. These were tied in 0° extension and neutral rotation of the hip joint. Irrigation of the surgical site then took place followed by wound closure in layers.
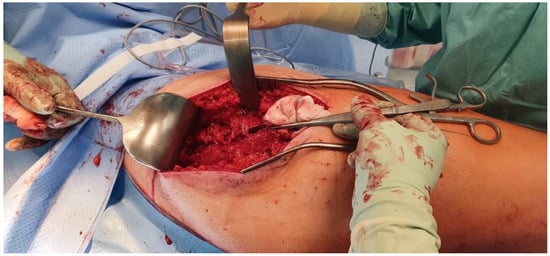
Figure 4.
Torn fibers of the gluteus maximus muscle at the insertion to the iliotibial band pointed with the thumb forceps.
5. Follow Up and Functional Outcome
On the first postoperative day, the patient began with 25% weight-bearing with a crutch-assisted gait, which lasted for four weeks. During that phase, extension and flexion of the hip joint were limited to 0° and 20°, respectively. That limitation aimed to avoid tension at the ITB. Perioperative deep venous thrombosis prophylaxis was administered according to hospital protocol. The postoperative course was uneventful. The wound dressing was removed on the fourth postoperative day, and the patient was discharged two days later. He progressed to weight-bearing at the sixth postoperative week, and the crutches were set aside. Hip-strengthening exercises were initiated in the ninth postoperative week. The patient could return to general activities and work without restrictions three months after surgery.
At the one-year postoperative follow-up, the patient could walk through the examination room without limping. He could stay and get up from the squatting position free from pain (Figure 5). The surgical scar showed no signs of irritation. The range of motion (ROM) of the right hip joint was extension/flexion 0°–0°–130°, abduction/adduction 30°–0°–20°, and external rotation/internal rotation 40°–0°–30°. The Western Ontario University/MacMaster University (WOMAC) Index and the Harris hip score were employed to evaluate the postoperative functional outcome. The result was excellent for both scores, 91.7/100 for the Harris hip score and 95.2/96 for the WOMAC Score.
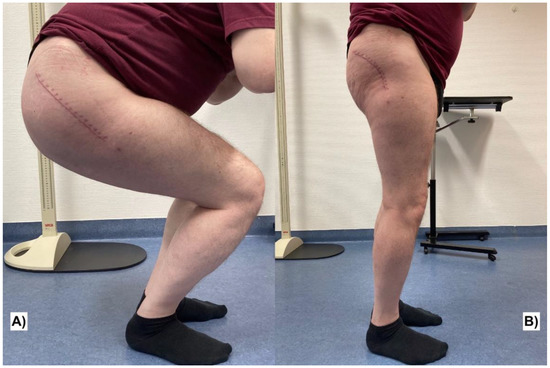
Figure 5.
Documentation of the surgical scar and the function of the hip joint one year postoperatively. Squatting position (A) and standing upright (B).
6. Discussion
After conducting a literature search, only two articles reporting cases of isolated injuries of the gluteus maximus muscle were detected [4,5]. Neither therapeutic strategies nor follow-up results were described in both papers. Those injuries could either result from overuse, misuse, poor posture, or trauma and it can be challenging to determine the exact cause of the injury. Diverse traumatic, degenerative, inflammatory, or idiopathic conditions of anatomical structures in the gluteal region such as injuries of the gluteus medius and minimus tendons [8], gluteal tendinopathy [9], trochanteric bursitis [10], proximal iliotibial band syndrome [11], or snapping hip (coxa saltans) [12] are equally considerable to explain acute as well as chronic pain over the lateral side of the hip. Postoperative muscle herniation [13] could lead to swelling and pain over the surgical scar if the fascia of the thigh was not closed sufficiently. Therefore, obtaining a reliable history of previous surgical procedures is essential. If a history of high-energy trauma to the hip joint is present, residuals of a Morel-Lavallée lesion should be borne in mind [14]. These are degloving injuries that result from the shearing of the hypodermis from the underlying deep fascia and require immediate intervention in the acute phase, whereas the formation of a pseudo capsule could delay its detection [15]. However, it is incontrovertible that Magnetic Resonance Imaging (MRI) is the modality of choice for investigating painful hip conditions [16].
As awareness of FAI increased in the last few years, a recent study proved that FAI is associated with an impairment of the gluteus maximus muscle contraction time, evidenced by tensiomyographic impairment in muscle function [17]. To exclude possibly associated labral tears with FAI [18], we planned an MRI of the right hip joint with radial sequences. Still, these were not obtained due to the apparent injury to the gluteus maximus tendon explaining the patient’s complaint.
In the authors’ opinion, the first step towards reaching the correct diagnosis is considering the muscle injury as a differential diagnosis in the first place, then a careful history taking regarding the location of the pain, radiation, intensity, character, exacerbating and relieving factors along with a thorough physical examination. The diagnosis can be established by a provocation test, as mentioned above. Pain over the lateral side of the thigh after the extension of the hip joint against resistance in the prone position would indicate an injury of the gluteus maximus tendon at the insertion to the ITB.
Though the double insertion of the gluteus maximus muscle might offer some degree of stability to the pelvis and the affected hip joint in mono-insertion injuries, the surgical indication, in this case, was made after careful consideration of multiple factors, including the patient’s age, level of activity, and clinical and radiological findings.
Neglected or mistreated isolated injuries of the gluteus maximus muscle may lead to persistent pain and limited range of motion of the affected hip joint. An adequate understanding of the anatomy of the hip joint will lead to a better perception and proper management of various pathological conditions in the gluteal region. Based on our information, this article revealed the first rehabilitation plan for a gluteus maximus tear following surgical treatment, which yielded an outstanding result. However, regardless of the excellent functional outcome reported, whether surgical intervention is superior to conservative therapy in this instance could not be determined based on one case report. Accordingly, comparing the results of both approaches as part of a prospective study in the future would be of great benefit to both healthcare workers and patients.
7. Conclusions
Isolated injuries of the gluteus maximus tendon are rare and should be considered a differential diagnosis when dealing with painful hip conditions. Surgical decision making in such cases should be patient-centered to achieve the desired outcomes. However, physically active individuals might benefit from early surgical intervention.
Author Contributions
Writing—original draft preparation, A.S.; writing—review and editing, M.P. and M.M.; supervision, W.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent was obtained from the patient for the publication of this case report.
Data Availability Statement
Not applicable.
Acknowledgments
We thank Marceau Tchudjin Chedjou for his assistance in the preparation of this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Domb, B.; Gui, C.; Lodhia, P. How much arthritis is too much for hip arthroscopy: A systematic review. Arthroscopy 2015, 31, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Netter, F.H.; Hansen, J.T.; Lambert, D.R. Netter’s Clinical Anatomy, 6th ed.; Icon Learning Systems: Carlstadt, NJ, USA, 2005; pp. 579–589. [Google Scholar]
- Keith, L.; Anne, M.R. Clinically Oriented Anatomy, 8th ed.; Lippincott Williams & Wilkins: Philidephia, PA, USA, 2015; pp. 337–342. [Google Scholar]
- Gondim Teixeira, P.A. Gluteus Maximus and Surrounding Muscles Injuries. In Muscle Injuries in Sport Athletes; Spring: Cham, Switzerland, 2017; pp. 335–351. [Google Scholar]
- Murat, K.; Tülay, T.; Hatice, Ö.; Bayram, K.; Levent, Ö. Gluteus Maximus Muscle Tear as a Rare Cause of Hip Pain and Sciatica. J. Emerg. Med. 2015, 5, 705–706. [Google Scholar]
- Nötzli, H.; Wyss, T.; Stoecklin, C.; Schmid, M.; Treiber, K.; Hodler, J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J. Bone Jt. Surg. Br. 2002, 84-B, 556–560. [Google Scholar] [CrossRef]
- Burwell, H.; Scott, D. A lateral intermuscular approach to the hip joint for replacement of the femoral head by a prosthesis. J. Bone Jt. Surg. Br. 1954, 36-B, 104–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godshaw, B.; Wong, M.; Ojard, C.; Williams, G.; Suri, M.; Jones, D. Acute Traumatic Tear of the Gluteus Medius and Gluteus Minimus in a Marathon Runner. Ochsner J. 2019, 19, 405–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimaldi, A.; Mellor, R.; Hodges, P.; Bennell, K.; Wajswelner, H.; Vicenzino, B. Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management. Sports Med. 2015, 45, 1107–1119. [Google Scholar] [CrossRef] [PubMed]
- Lustenberger, D.; Ng, V.; Best, T.; Ellis, T. Efficacy of treatment of trochanteric bursitis: A systematic review. Clin. J. Sport Med. 2011, 21, 447–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sher, I.; Umans, H.; Downie, S.; Tobin, K.; Arora, R.; Olson, T. Proximal iliotibial band syndrome: What is it and where is it? Skelet. Radiol. 2011, 12, 1553–1556. [Google Scholar] [CrossRef] [PubMed]
- Badowski, E. Snapping Hip Syndrome. Orthop. Nurs. 2018, 37, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Coleman, W.; Wang, T.; Mathes, S. Muscle Herniation Through a Tensor Fascia Lata Defect. Semin. Plast. Surg. 1987, 1, 144–148. [Google Scholar] [CrossRef]
- Li, H.; Zhang, F.; Lei, G. Morel-Lavallee lesion. Chin. Med. J. 2014, 7, 1351–1356. [Google Scholar]
- Mellado, J.; Pérez del Palomar, L.; Díaz, L.; Ramos, A.; Saurí, A. Long-standing Morel-Lavallée lesions of the trochanteric region and proximal thigh: MRI features in five patients. AJR Am. J. Roentgenol. 2004, 182, 1289–1294. [Google Scholar] [CrossRef] [PubMed]
- Mak, M.S.; Teh, J. Magnetic resonance imaging of the hip: Anatomy and pathology. Polish J. Radiol. 2020, 85, e489–e508. [Google Scholar] [CrossRef] [PubMed]
- Seijas, R.; Alentorn-Geli, E.; Álvarez-Díaz, P.; Marín, M.; Ares, O.; Sallent, A.; Cuscó, X.; Cugat, R. Gluteus maximus impairment in femoroacetabular impingement: A tensiomyographic evaluation of a clinical fact. Arch. Orthop. Trauma Surg. 2016, 136, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Kemp, J.; Makdissi, M.; Schache, A. Hip chondropathy at arthroscopy: Prevalence and relationship to labral pathology, femoroacetabular impingement and patient-reported outcomes. Br. J. Sports Med. 2014, 48, 1102–1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).