Incidence, Trends, and Seasonality of Paediatric Injury-Related Emergency Department Presentations at a Large Level 1 Paediatric Trauma Centre in Australia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Sources
2.3. Data Analysis
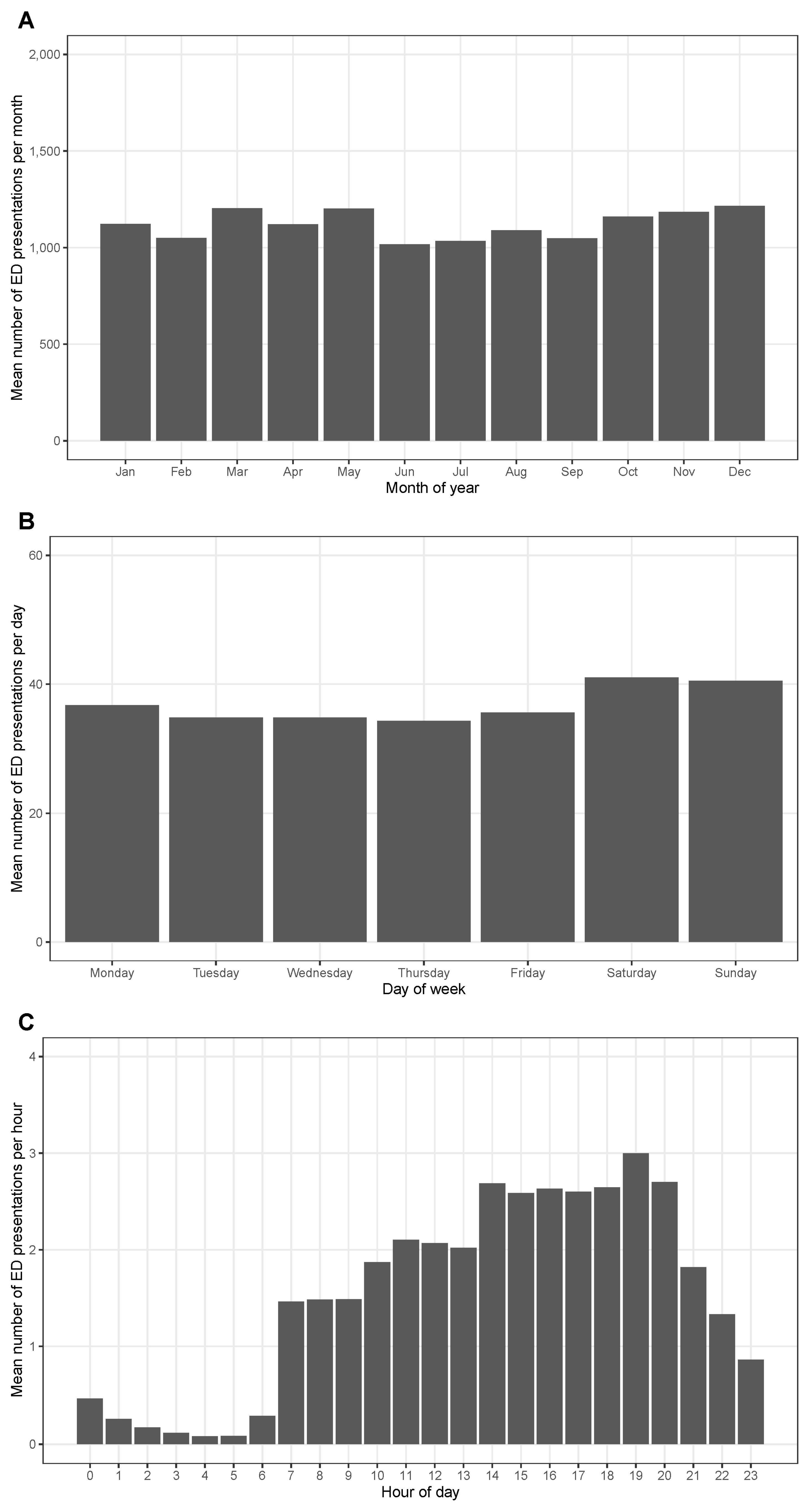
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Report on Child Injury Prevention; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Guice, K.S.; Cassidy, L.D.; Oldham, K.T. Traumatic injury and children: A national assessment. J. Trauma 2007, 63, S68–S80. [Google Scholar] [CrossRef] [PubMed]
- Hedström, E.M.; Bergström, U.; Michno, P. Injuries in children and adolescents—Analysis of 41,330 injury related visits to an emergency department in northern Sweden. Injury 2012, 43, 1403–1408. [Google Scholar] [CrossRef] [PubMed]
- Martinez, T.; Mde, L.; Rocha, C.J.; Clavel-Arcas, C.; Mack, K.A. Nonfatal unintentional injuries in children aged <15 years in Nicaragua. Int. J. Inj. Contr. Saf. Promot. 2010, 17, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Cause of Death Australia. Catalogue No. 3303.0; Australian Bureau of Statistics: Canberra, Australia, 2015.
- Mitchell, R.J.; Curtis, K.; Foster, K. A 10-year review of child injury hospitalisations, health outcomes and treatment costs in Australia. Inj. Prev. 2018, 24, 344–350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehta, S.; Ameratunga, S.N. Prevalence of post-traumatic stress disorder among children and adolescents who survive road traffic crashes: A systematic review of the international literature. J. Paediatr. Child Health 2012, 48, 876–885. [Google Scholar] [CrossRef] [PubMed]
- Foster, K.; Young, A.; Mitchell, R.; Van, C.; Curtis, K. Experiences and needs of parents of critically injured children during the acute hospital phase: A qualitative investigation. Injury 2017, 48, 114–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosta, L.; Harms, L.; Franich-Ray, C.; Anderson, V.; Northam, E.; Cochrane, A.; Menahem, S.; Jordan, B. Parental experiences of their infant’s hospitalization for cardiac surgery. Child Care Health Dev. 2015, 41, 1057–1065. [Google Scholar] [CrossRef] [PubMed]
- Mangelsdorf, S.N.; Conroy, R.; Mehl, M.R.; Norton, P.J.; Alisic, E. Listening to family life after serious pediatric injury: A study of four cases. Fam. Process. 2020, 59, 1191–1208. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.J.; McClure, R.J.; Williamson, A.M.; McKenzie, K. Implementing the national priorities for injury surveillance. Med. J. Aust. 2008, 188, 405–408. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Prehospital Trauma Care Management; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- World Health Organization. Guidelines for Trauma Quality Improvement Programs; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- National Centre for Classification in Health. ICD-10-AM, 5th ed.; National Centre for Classification in Health: Sydney, Australia, 2006.
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016. Catalogue No. 2033.0.55.001; Australian Bureau of Statistics: Canberra, Australia, 2016.
- Do, V.Q.; Ting, H.P.; Curtis, K.; Mitchell, R. Internal validation of models for predicting paediatric survival and trends in serious paediatric hospitalised injury in Australia. Injury 2020, 51, 1769–1776. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.; Ting, H.P. Survival Risk Ratios for ICD-10-AM Injury Diagnosis Classifications for Children [Dataset]. Available online: https://doi.org/10.25949/14852949.v1 (accessed on 13 April 2022).
- Hyndman, R.J.; Athanasopoulos, G. Forecasting: Principles and Practice, 2nd ed.; OTexts: Melbourne, Australia, 2018. [Google Scholar]
- Australian Institute of Health and Welfare. Hospitalised Injury in Children and Young People 2011–12. Injury Research and Statistics Series no. 91. Catalogue No. INJCAT 167; Australian Institute of Health and Welfare: Canberra, Australia, 2014.
- Curtis, K.; Kennedy, B.; Lam, M.K.; Mitchell, R.J.; Black, D.; Burns, B.; White, L.; Loudfoot, A.; D’Amato, A.; Dinh, M.; et al. Cause, treatment costs and 12-month functional outcomes of children with major injury in NSW, Australia. Injury 2020, 51, 2066–2075. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.; Kennedy, B.; Lam, M.K.; Mitchell, R.J.; Black, D.; Burns, B.; Dinh, M.; Holland, A.J. Pathways and factors that influence time to definitive trauma care for injured children in New South Wales, Australia. Injury 2022, 53, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare; Department of Health and Family Services. First Report on the National Health Priority Areas, Full Report; Australian Institute of Health and Welfare: Canberra, Australia, 1997.
- National Public Health Partnership. The National Injury Prevention and Safety Promotion Plan: 2004–2014; National Public Health Partnership: Canberra, Australia, 2004.
- Department of Health. National Injury Prevention Strategy 2020–2030; Commonwealth of Australia Department of Health: Canberra, Australia, 2021.
- Australian Institute of Health and Welfare. Burden of disease [Internet]. Australian Institute of Health and Welfare: Canberra, Australia. 2020. Available online: https://www.aihw.gov.au/reports/australias-health/burden-of-disease (accessed on 7 April 2022).
- Bierbaum, M.; Lystad, R.P.; Curtis, K.; Mitchell, R. Incidence and severity of head injury hospitalisations in Australian children over a 10-year period. Health Promot. J. Austral. 2019, 30, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Adams, S.; Holland, A.J. Furniture injuries in children. J. Paediatr. Child Health 2009, 45, 505–508. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, C.S.; Adams, S.; Tzioumi, D.; Brown, J. Injury from falls in infants under one year. J. Paediatr. Child Health 2017, 53, 754–760. [Google Scholar] [CrossRef] [PubMed]
- Zacay, G.; Dubnov-Raz, G.; Modan-Moses, D.; Tripto-Shkolnik, L.; Levy-Shraga, Y. Epidemiology of childhood fractures in Israel during 2000–2019. Bone 2022, 154, 116174. [Google Scholar] [CrossRef] [PubMed]
- Agar, A.; Sahin, A.; Gunes, O.; Gulabi, D.; Erturk, C. Seasonal variation in paediatric orthopaedic trauma Patients—A single centre experience from Turkey. J. Orthop. Surg. 2022, 30, 23094990211068146. [Google Scholar] [CrossRef] [PubMed]
- Livingston, K.S.; Miller, P.E.; Lierhaus, A.; Matheney, T.H.; Mahan, S.T. Does weather matter? The effect of weather patterns and temporal factors on pediatric orthopedic trauma volume. Open Orthop. J. 2016, 10, 550–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atherton, W.G.; Harper, W.M.; Abrams, K.R. A year’s trauma admissions and the effect of the weather. Injury 2005, 36, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Regional Population. 2022. Available online: https://www.abs.gov.au/statistics/people/population/regional-population (accessed on 7 April 2022).



| Characteristic | N (%) |
|---|---|
| Sex | |
| Male | 80,297 (59.7) |
| Female | 54,187 (40.3) |
| Age group | |
| 0 years | 7852 (5.4) |
| 1–5 years | 60,550 (45.0) |
| 6–10 years | 33,824 (25.2) |
| 11–15 years | 32,258 (24.0) |
| Socioeconomic disadvantage1 | |
| 1 (most disadvantaged) | 32,812 (24.6) |
| 2 | 11,018 (8.3) |
| 3 | 17,963 (13.5) |
| 4 | 32,649 (24.5) |
| 5 (least disadvantaged) | 38,744 (29.1) |
| Mode of arrival | |
| Private car | 115,079 (85.6) |
| Ambulance | 17,885 (13.3) |
| Walk-in | 563 (0.4) |
| Public transport | 428 (0.3) |
| Hospital transport | 335 (0.2) |
| Other | 194 (0.1) |
| Triage category2 | |
| Less urgent condition | 18,706 (13.9) |
| Potentially serious condition | 88,379 (65.7) |
| Potentially life-threatening condition | 22,772 (16.9) |
| Imminently life-threatening condition | 3342 (2.5) |
| Immediately life-threatening condition | 1283 (1.0) |
| Injury severity | |
| Minor (ICISS > 0.99) 3 | 119,376 (88.8) |
| Moderate (ICISS 0.98–0.99) 3 | 13,904 (10.3) |
| Serious (ICISS < 0.98) 3 | 1204 (0.9) |
| Departure status | |
| Discharged | 110,185 (81.9) |
| Admitted | 23,224 (17.3) |
| Departed | 876 (0.7) |
| Transferred | 186 (0.1) |
| Died | 13 (0.0) |
| Diagnosis | N (%) |
|---|---|
| Injuries to the head (S00-S09) | 36,034 (26.8) |
| Superficial injury of head (S00) 1 | 2878 (2.1) |
| Open wound of head (S01) 1 | 13,243 (9.9) |
| Fracture of skull and facial bones (S02) 1 | 4207 (3.1) |
| Dislocation, sprain, and strain of joints and ligaments of head (S03) 1 | 41 (0.0) |
| Injury of eye and orbit (S05) 1 | 2297 (1.7) |
| Intracranial injury (S06) 1 | 2259 (1.7) |
| Other and unspecified injuries of head (S09) 1 | 10,990 (8.2) |
| Injuries to the neck (S10-S19) | 665 (0.5) |
| Injuries to the thorax (S20-S29) | 158 (0.1) |
| Injuries to the abdomen, lower back, lumbar spine and pelvis (S30-S39) | 937 (0.7) |
| Injuries to the shoulder and upper arm (S40-S49) | 9568 (7.1) |
| Injuries to the elbow and forearm (S50-S59) | 20,502 (15.2) |
| Injuries to the wrist and hand (S60-S69) | 14,155 (10.5) |
| Injuries to the hip and thigh (S70-S79) | 1448 (1.1) |
| Injuries to the knee and lower leg (S80-S89) | 8871 (6.6) |
| Injuries to the ankle and foot (S90-S99) | 5895 (4.4) |
| Injuries involving multiple body regions (T00-T07) | 390 (0.3) |
| Injuries to unspecified part of trunk, limb or body region (T08-T14) | 13,486 (10.0) |
| Effects of foreign body entering through natural orifice (T15-T19) | 7518 (5.6) |
| Burns (T20-T31) | 5031 (3.7) |
| Poisoning by drugs, medicaments and biological substances (T36-T50) | 834 (0.6) |
| Toxic effects of substances chiefly nonmedicinal as to source (T51-T65) | 950 (0.7) |
| Other and unspecified effects of external causes (T66-T78) | 5334 (4.0) |
| Certain early complications of trauma (T79) | 85 (0.1) |
| Complications of surgical and medical care (T80-T89) | 2623 (2.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lystad, R.P.; Fyffe, A.; Orr, R.; Browne, G. Incidence, Trends, and Seasonality of Paediatric Injury-Related Emergency Department Presentations at a Large Level 1 Paediatric Trauma Centre in Australia. Trauma Care 2022, 2, 408-417. https://doi.org/10.3390/traumacare2030033
Lystad RP, Fyffe A, Orr R, Browne G. Incidence, Trends, and Seasonality of Paediatric Injury-Related Emergency Department Presentations at a Large Level 1 Paediatric Trauma Centre in Australia. Trauma Care. 2022; 2(3):408-417. https://doi.org/10.3390/traumacare2030033
Chicago/Turabian StyleLystad, Reidar P., Andrew Fyffe, Rhonda Orr, and Gary Browne. 2022. "Incidence, Trends, and Seasonality of Paediatric Injury-Related Emergency Department Presentations at a Large Level 1 Paediatric Trauma Centre in Australia" Trauma Care 2, no. 3: 408-417. https://doi.org/10.3390/traumacare2030033
APA StyleLystad, R. P., Fyffe, A., Orr, R., & Browne, G. (2022). Incidence, Trends, and Seasonality of Paediatric Injury-Related Emergency Department Presentations at a Large Level 1 Paediatric Trauma Centre in Australia. Trauma Care, 2(3), 408-417. https://doi.org/10.3390/traumacare2030033







