Management of Advanced Aged Patients with Rib Fractures: Current Evidence and Review of the Literature
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Data Collection
2.3. Data Extraction and Quality Assessment
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
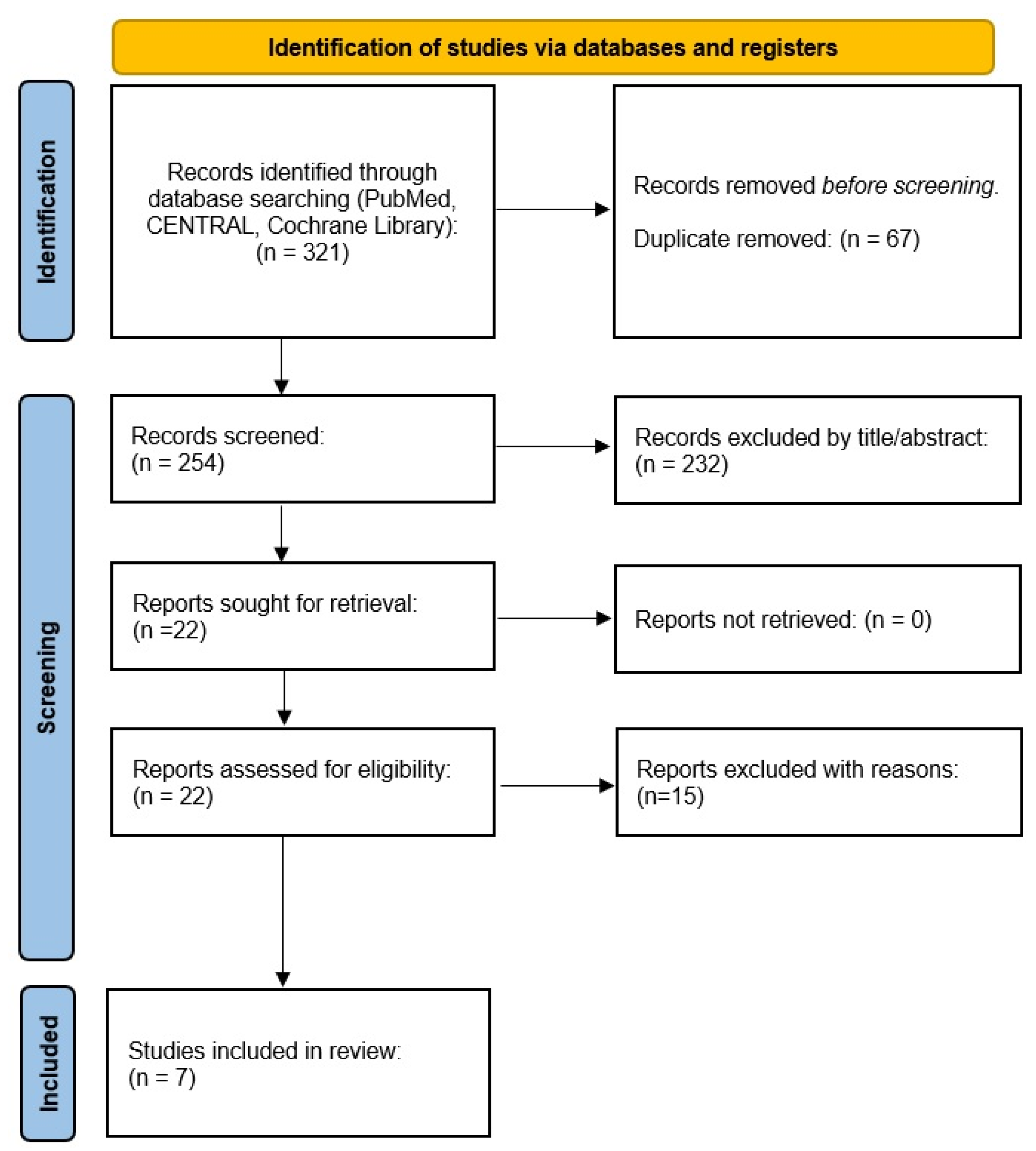
3.1. Study Selection
3.2. Study Characteristics
3.3. Main Findings
3.4. Global Complications Report
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ziegler, D.W.; Agarwal, N.N. The morbidity and mortality of rib fractures. J. Trauma 1994, 37, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.E.; Feliciano, D.V.; Mattox, K.L. Trauma, 5th ed.; McGraw-Hill: New York, NY, USA, 2004; Chap 25. [Google Scholar]
- Caragounis, E.-C.; Olsén, M.F.; Pazooki, D.; Granhed, H. Surgical treatment of multiple rib fractures and flail chest in trauma: A one-year follow-up study. World J. Emerg. Surg. 2016, 11, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordy, S.; Fabricant, L.; Ham, B.; Mullins, R.; Mayberry, J. The contribution of rib fractures to chronic pain and disability. Am. J. Surg. 2014, 207, 659–663. [Google Scholar] [CrossRef]
- Richardson, J.D.; Franklin, G.A.; Heffley, S.; Seligson, D. Operative fixation of chest wall fractures: An underused procedure? Am. Surg. 2007, 73, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Mayberry, J.C.; Ham, L.B.; Schipper, P.H.; Ellis, T.J.; Mullins, R.J. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J. Trauma 2009, 66, 875–879. [Google Scholar] [CrossRef]
- Hoepelman, R.J.; Beeres, F.J.P.; Heng, M.; Knobe, M.; Link, B.-C.; Minervini, F.; Babst, R.; Houwert, R.M.; van de Wall, B.J.M. Rib fractures in the elderly population: A systematic review. Arch. Orthop. Trauma Surg. 2022. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, n71. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Liu, T.; Liu, P.; Chen, J.; Xie, J.; Yang, F.; Liao, Y. A Randomized Controlled Trial of Surgical Rib Fixation in Polytrauma Patients with Flail Chest. J. Surg. Res. 2019, 242, 223–230. [Google Scholar] [CrossRef]
- Khandelwal, G.; Mathur, R.; Shukla, S.; Maheshwari, A. A prospective single center study to assess the impact of surgical stabilization in patients with rib fracture. Int. J. Surg. 2011, 9, 478–481. [Google Scholar] [CrossRef] [Green Version]
- Fitzgerald, M.T.; Ashley, D.W.; Abukhdeir, H.; Christie, D.B., 3rd. Rib fracture fixation in the 65 years and older population: A paradigm shift in management strategy at a Level I trauma center. J. Trauma Acute Care Surg. 2017, 82, 524–527. [Google Scholar] [CrossRef] [PubMed]
- Ali-Osman, F.; Mangram, A.; Sucher, J.; Shirah, G.; Johnson, V.; Moeser, P.; Sinchuk, N.K.; Dzandu, J.K. Geriatric (G60) trauma patients with severe rib fractures: Is muscle sparing minimally invasive thoracotomy rib fixation safe and does it improve post-operative pulmonary function? Am. J. Surg. 2018, 216, 46–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kane, E.D.; Jeremitsky, E.; Bittner, K.R.; Kartiko, S.; Doben, A.R. Surgical Stabilization of Rib Fractures: A Single Institution Experience. J. Am. Coll. Surg. 2018, 226, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Zhu, R.C.; De Roulet, A.; Ogami, T.; Khariton, K. Rib fixation in geriatric trauma: Mortality benefits for the most vulnerable patients. J. Trauma Acute Care Surg. 2020, 89, 103–110. [Google Scholar] [CrossRef]
- Pieracci, F.M.; Leasia, K.; Hernandez, M.C.; Kim, B.; Cantrell, E.; Bauman, Z.; Gardner, S.; Majercik, S.; White, T.; Dieffenbaugher, S.; et al. Surgical stabilization of rib fractures in octogenarians and beyond—what are the outcomes? J. Trauma Acute Care Surg. 2021, 90, 1014–1021. [Google Scholar] [CrossRef]
- Cooper, E.; Wake, E.; Cho, C.; Wullschleger, M.; Patel, B. Outcomes of rib fractures in the geriatric population: A 5-year retrospective, single-institution, Australian study. ANZ J. Surg. 2021, 91, 1886–1892. [Google Scholar] [CrossRef]
- Christie, D.B.; Nowack, T.E.; Nonnemacher, C.J.; Montgomery, A.; Ashley, D.W. Surgical Stabilization of Rib Fractures Improves Outcomes in the Geriatric Patient Population. Am. Surg. 2022, 88, 658–662. [Google Scholar] [CrossRef]
- Zegg, M.; Kammerlander, C.; Schmid, S.; Roth, T.; Kammerlander-Knauer, U.; Gosch, M.; Luger, T.J. Multidisciplinary Approach to Lifesaving Measures in the Elderly Individuals with Flail Chest Injury with ORIF of Rib Fractures. Geriatr. Orthop. Surg. Rehabil. 2012, 3, 164–166. [Google Scholar] [CrossRef] [Green Version]
- Lin, F.C.-F.; Li, R.-Y.; Tung, Y.-W.; Jeng, K.-C.; Tsai, S.C.-S. Morbidity, mortality, associated injuries, and management of traumatic rib fractures. J. Chin. Med Assoc. 2016, 79, 329–334. [Google Scholar] [CrossRef] [Green Version]
- Swart, E.; Laratta, J.; Slobogean, G.; Mehta, S. Operative Treatment of Rib Fractures in Flail Chest Injuries: A Meta-analysis and Cost-Effectiveness Analysis. J. Orthop. Trauma 2017, 31, 64–70. [Google Scholar] [CrossRef]
- Fitzpatrick, D.C.; Denard, P.J.; Phelan, D.; Long, W.B.; Madey, S.M.; Bottlang, M. Operative stabilization of flail chest injuries: Review of literature and fixation options. Eur. J. Trauma Emerg. Surg. 2010, 36, 427–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulman, A.M.; Claridge, J.A.; Young, J.S. Young versus old: Factors affecting mortality after blunt traumatic injury. Am. Surg. 2002, 68, 942. [Google Scholar] [PubMed]
- Christie, D.B., 3rd; Nowack, T.; Drahos, A.; Ashley, D.W. Geriatric chest wall injury: Is it time for a new sense of urgency? J. Thorac. Dis. 2019, 11 (Suppl. S8), S1029–S1033. [Google Scholar] [CrossRef] [PubMed]
- Bulger, E.M.; Arneson, M.A.; Mock, C.; Jurkovich, G.J. Rib fractures in the elderly. J. Trauma 2000, 48, 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Yukioka, T.; Yamaguti, Y.; Shimizu, S.; Goto, H.; Matsuda, H.; Shimazaki, S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J. Trauma 2002, 52, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Marasco, S.F.; Davies, A.R.; Cooper, D.J.; Varma, D.; Bennett, V.; Nevill, R.; Lee, G.; Bailey, M.; Fitzgerald, M. Prospective Randomized Controlled Trial of Operative Rib Fixation in Traumatic Flail Chest. J. Am. Coll. Surg. 2013, 216, 924–932. [Google Scholar] [CrossRef]
- Santiago, M.G.; Valenza, M.C.; Román, E.P.; López, L.L.; Vigueras, N.M.; Martos, I.C.; Cebrià i Iranzo, M.À. Impacts of tailored, rehabilitation nursing care on functional ability and quality of life in hospitalized elderly patients after rib fractures. Clin. Rehabil. 2021, 35, 1544–1554. [Google Scholar] [CrossRef]
- Coary, R.; Skerritt, C.; Carey, A.; Rudd, S.; Shipway, D. New horizons in rib fracture management in the older adult. Age Ageing 2019, 49, 161–167. [Google Scholar] [CrossRef]
| Patient | Hospitalized elderly patients over 60 years old with ribs fractures |
| Intervention | Operative treatment with surgical rib fixation |
| Comparison | Conservative treatment without surgical rib fixation |
| Outcome | Reduced mortality rate |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| The study design was a randomized clinical trial or an observational study | No availability of a full-text |
| Subjects were adult patients over 60 years old age | Conference reports, letters, meeting proceedings, case series with fewer than ten patients |
| Conservative vs. operative treatment of two rib fractures or more was compared | The study was still ongoing |
| Study reporting on mortality rate and secondary outcomes | The study was not written in English |
| Authors (Year, Country) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Outcomes | Fitzgerald et al. (2017, USA) [12] | Ali-Osman et al. (2018, USA) [12] | Kane et al. (2018, USA) [13] | Chen Zhu et al. (2020, USA) [15] | Pieracci et al. (2021, USA) [16] | Cooper et al. (2021, Australia) [17] | Christie et al. (2021, USA) [18] | |
| Subjects (number) | CT | 50 | 135 | 392 | 758 | 227 | 280 | 172 |
| OT | 23 | 64 | 43 | 758 | 133 | 15 | 85 | |
| Male (%) | CT | nr | 73 (54) | nr | 518 (68) | 116 (51) | † 185 (63) | nr nr |
| OT | nr | 41 (61) | nr | 530 (70) | 81 (61) | nr | ||
| Age (IQR/SD) | CT | 75 (65–97) | 72 (66–81) | 75.4 ± 6.8 | 72 (68–79) | 86 (80–90) | 77 (73–84) | 75 (65–100) |
| OT | 68 (63–89) | 69 (63–74) | 71.3 ± 6.0 | 72 (68–78) | 84 (80–100) | 78 (75–83) | 74 (65–69) | |
| Rib fractures (IQR/SD) | CT | nr | 5 (3–7) | nr | nr | 5 (1–7) | 4 (3–6) | nr |
| OT | nr | 7 (5–9) | nr | nr | 9 (1–30) | 8 (6–12) | nr | |
| Flail chest (IQR/SD) | CT | nr | nr | nr | 348 (46) | 36 (16) | 42 (15) | nr |
| OT | nr | nr | nr | 345 (46) | 76 (57) | 7 (50) | nr | |
| ISS (IQR/SD) | CT | 19 (14–23) | 14 (8–24) | 14.1 ± 10.3 | nr | 13 (4–34) | 14 (10–19) | 13 (1–38) |
| OT | 21 (16–26) | 17.5 (9–25) | 20.1 ± 8.5 | nr | 14 (4–57) | 17 (13–29) | 20 (9–59) | |
| Mortality (%) | CT | 2 (4) | 13 (10) | 33 (8) | 55 (7) | 21 (9) | 27 (10) | 18 (10) |
| OT | 0 (0) | 1 (2) | 1 (2) | 32 (4) | 10 (8) | 0 (0) | 4 (5) | |
| Pneumonia (%) | CT | 7 (14) | 16 (12) | 54 (14) | 8 (1) | 9 (4) | 25 (10) | 20 (12) |
| OT | 0 (0) | 5 (8) | 2 (5) | 23 (3) | 16 (12) | 2 (13) | 0 (0) | |
| MVL (IQR/SD) | CT | nr | 4 (1–10) | nr | 7 (3–14) | nr | 5 (2–12) | nr |
| OT | nr | 3 (1–15) | nr | 6 (2–13) | nr | 12 (3–30) | nr | |
| ICU-LOS (IQR/SD) | CT | 12 (7–17) | 4 (3–7) | 0 (0–3) | 4 (2–8) | 0 | 3 (1–6) | 10 (1–32) |
| OT | 8 (5–11) | 6 (3–10) | 5 (0–8) | 7 (4–13) | 4.5 | 6 (2–13) | 8 (1–11) | |
| IH-LOS (IQR/SD) | CT | 17 (10–23) | 4.8 (3–8) | 5 (3–9) | 7 (4–12) | 6 | 6.5 (3–13) | 8 (1–39) |
| OT | 18 (14–23) | 12 (9–16) | 12 (10–16) | 13 (9–18) | 11 | 12 (9–15) | 15 (3–49) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrari, P.A.; Zappadu, S.; Santoru, M.; Riva, L.; Cherchi, R. Management of Advanced Aged Patients with Rib Fractures: Current Evidence and Review of the Literature. Trauma Care 2022, 2, 87-94. https://doi.org/10.3390/traumacare2020008
Ferrari PA, Zappadu S, Santoru M, Riva L, Cherchi R. Management of Advanced Aged Patients with Rib Fractures: Current Evidence and Review of the Literature. Trauma Care. 2022; 2(2):87-94. https://doi.org/10.3390/traumacare2020008
Chicago/Turabian StyleFerrari, Paolo Albino, Sara Zappadu, Massimiliano Santoru, Laura Riva, and Roberto Cherchi. 2022. "Management of Advanced Aged Patients with Rib Fractures: Current Evidence and Review of the Literature" Trauma Care 2, no. 2: 87-94. https://doi.org/10.3390/traumacare2020008
APA StyleFerrari, P. A., Zappadu, S., Santoru, M., Riva, L., & Cherchi, R. (2022). Management of Advanced Aged Patients with Rib Fractures: Current Evidence and Review of the Literature. Trauma Care, 2(2), 87-94. https://doi.org/10.3390/traumacare2020008






