Assessment and Management of Pain in Patients Sustaining Burns at Emergency Department Kenyatta National Hospital, Kenya: A Descriptive Study
Abstract
:1. Introduction
2. Methods
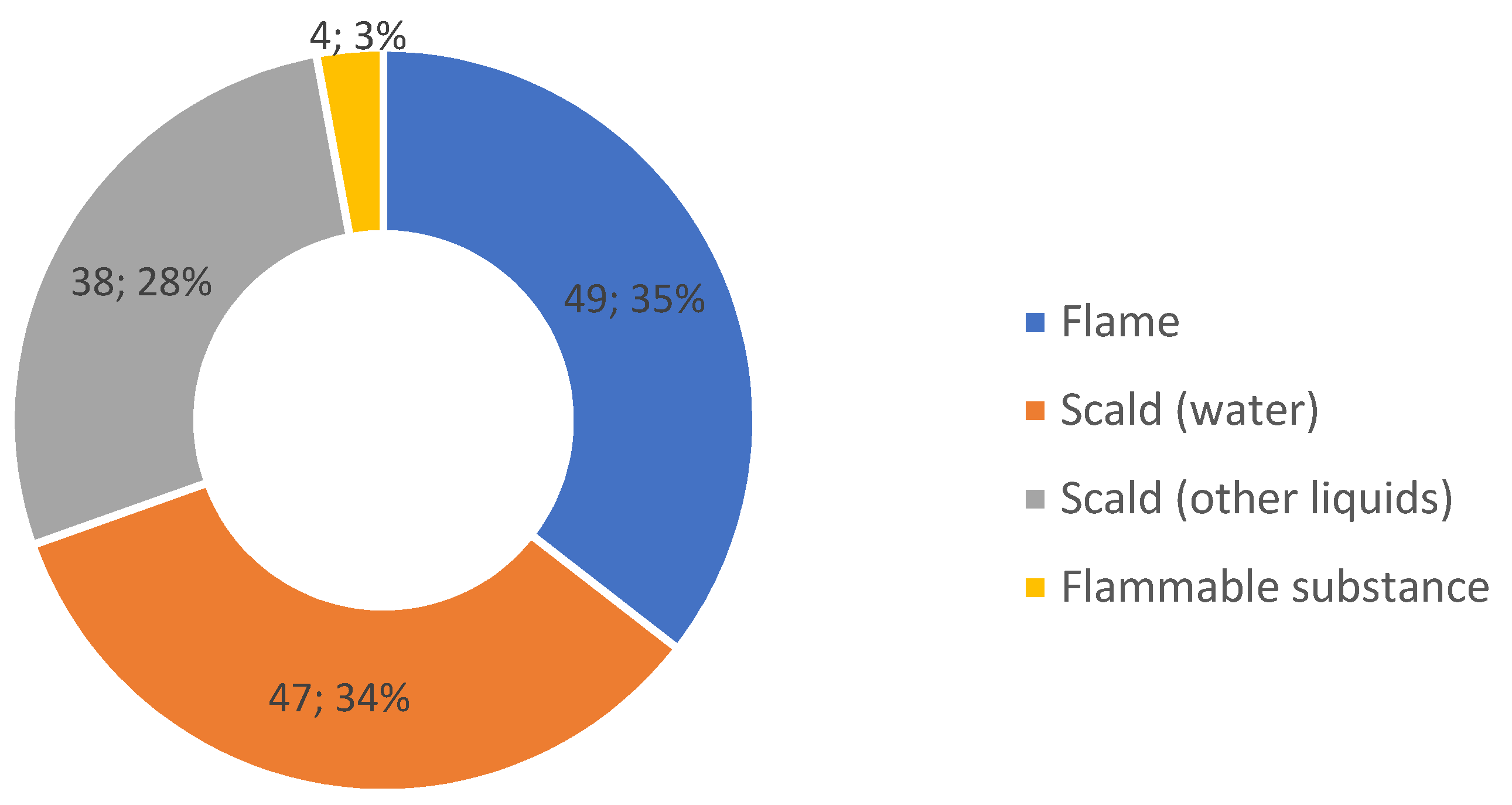
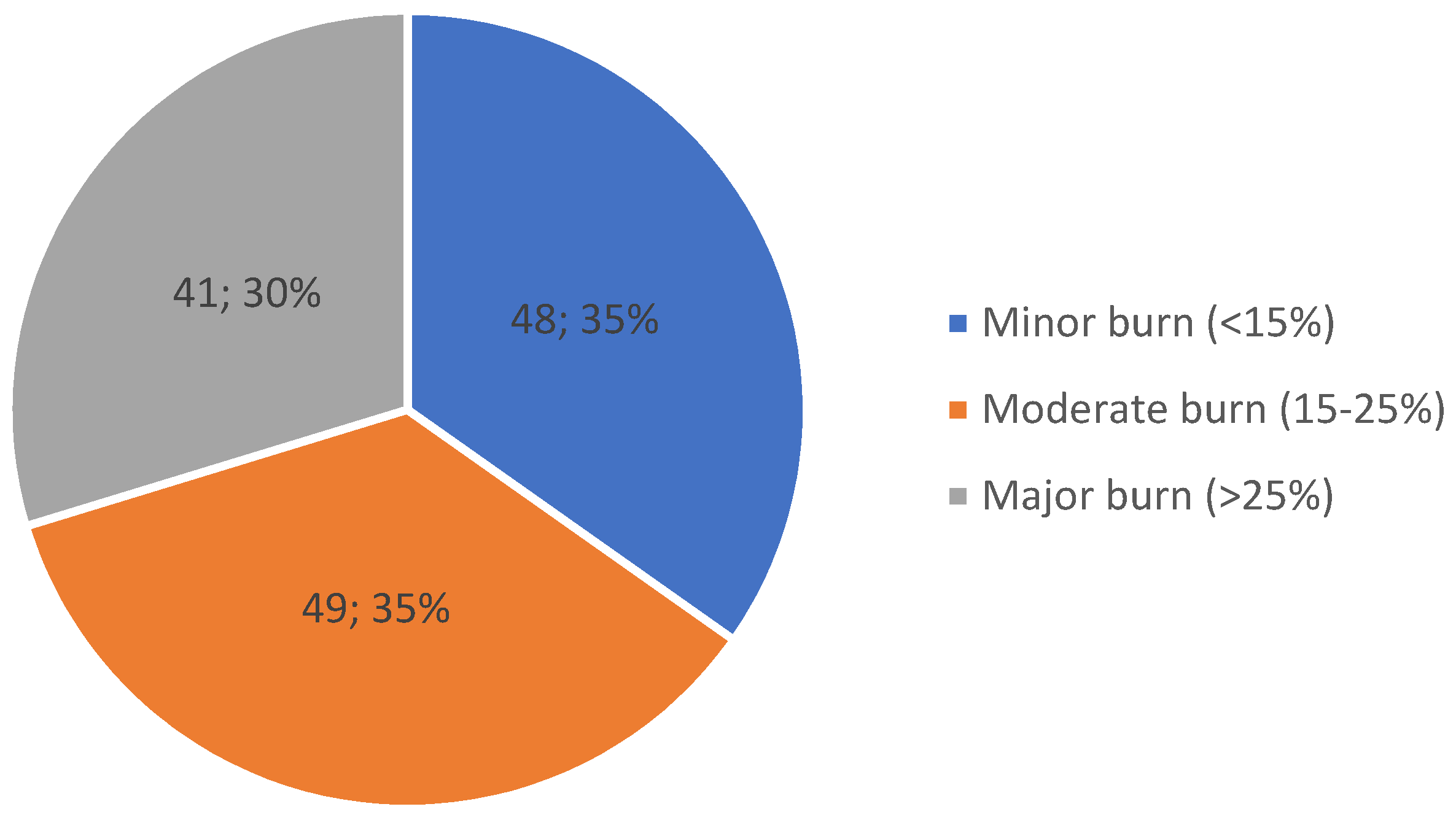
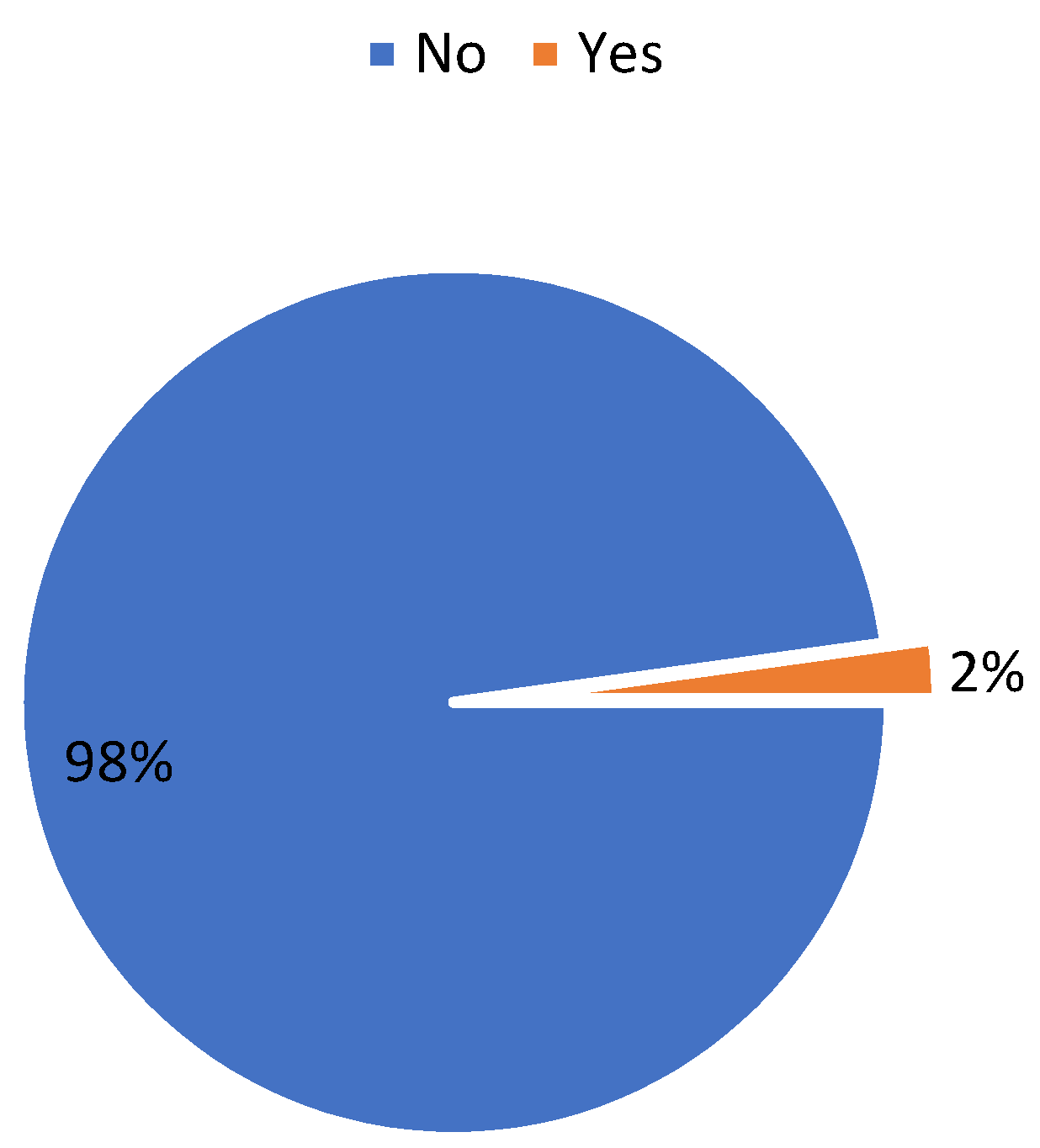
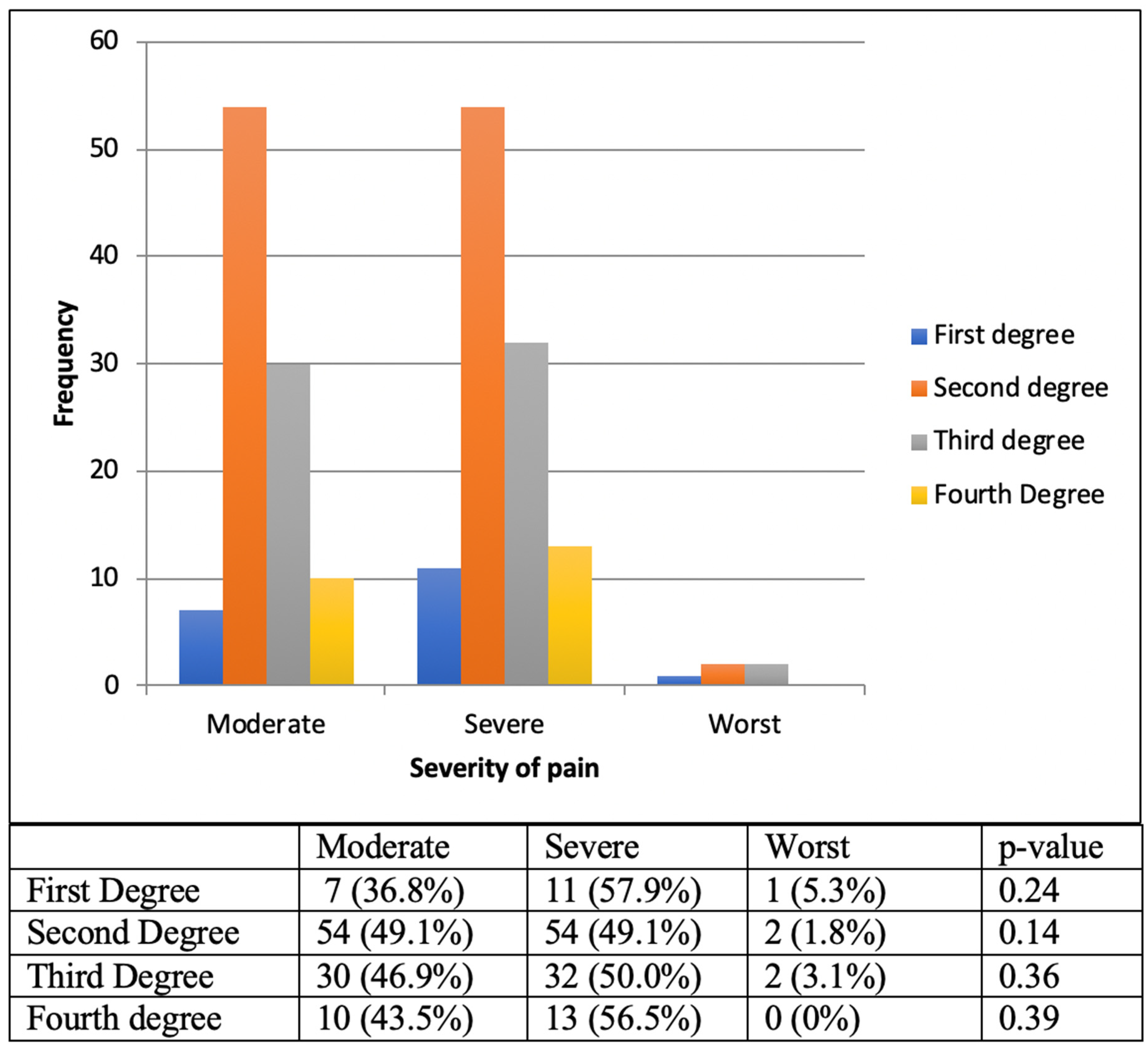
3. Results
4. Discussion
5. Conclusions
6. Limitations
- Burn in jury is common and in adults, the common age group is 22–34.
- Burn injury is associated with severe pain; this entity needs to be assessed to treat appropriately.
- Validated pain assessment tools are available for easy use.
- Pain management is not forgotten, but it could be better managed if it was assessed.
- All front-liners receiving burn victims needs to evaluate pain.
- All healthcare workers need to be taught how to assess the pain.
- Shows a gap in the assessment of pain and treatment of pain.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peck, M.D. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns 2011, 37, 1087–1100. [Google Scholar] [CrossRef] [PubMed]
- WHO. The Global Burden of Disease: 2004 Update; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Odero, W.O.; Kibosia, J.C. Incidence and characteristics of injuries in Eldoret, Kenya. East Afr. Med. J. 1995, 72, 706–710. [Google Scholar] [PubMed]
- Mzezewa, S.; Jonsson, K.; Aberg, M.; Salemark, L. A Prospective study on the epidemiology of burns in patients admitted to the Harare burn units. Burns 1999, 25, 499–504. [Google Scholar] [CrossRef]
- Chalya, P.L.; Mabula, J.B.; Dass, R.M.; Giiti, G.; Chandika, A.B.; Kanumba, E.S.; Gilyoma, J.M. Pattern of childhood burn injuries and their management outcome at Bugando Medical Centre in Northwestern Tanzania. BMC Res. Notes 2011, 4, 485. [Google Scholar] [CrossRef] [Green Version]
- Nthumba, P.M. Outcome of Moderate and Severe Thermal Injuries at Kenyatta National Hospital. Master’s Thesis, Department of Surgery, University of Nairobi, Nairobi, Kenya, 2002. [Google Scholar]
- Lelei, L.; Chebor, A.; Mwangi, H. Burns injuries among in-patients at Moi Teaching and Referral Hospital, Eldoret, Kenya. Ann. Afr. Surg. 2011, 8, 12–15. [Google Scholar]
- Orgill, D.P. Excision and skin grafting of thermal burns. N. Engl. J. Med. 2009, 360, 893–901. [Google Scholar] [CrossRef] [Green Version]
- Richardson, P.; Mustard, L. The management of pain in the burns unit. Burns 2009, 35, 921–936. [Google Scholar] [CrossRef]
- American Pain Society. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 2001, 108, 793–797. [Google Scholar] [CrossRef] [Green Version]
- Summer, G.J.; Puntillo, K.A.; Miaskowski, C.; Green, P.G.; Levine, J.D. Burn injury pain: The continuing challenge. J. Pain 2007, 8, 533–548. [Google Scholar] [CrossRef]
- Hammond, J.; Ward, C. Burns in octogenarians. South Med. J. 1991, 84, 1316–1319. [Google Scholar] [CrossRef]
- Mahar, P.D.; Wasiak, J.; O’Loughlin, C.J.; Christelis, N.; Arnold, C.A.; Spinks, A.B.; Danilla, S. Frequency and use of pain assessment tools implemented irandomiseded controlled trials in the adult burns population: A systematic review. Burns 2012, 38, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Gordon, M.; Greenfield, E.; Marvin, J.; Hester, C.; Lauterbach, S. Use of Pain Assessment Tool: Is There a Preference? J. Burn Care Rehabil. 1998, 19, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Frampton, C.L.; Hughes-Webb, P. The measurement of pain. Clin. Oncol. 2011, 23, 381–386. [Google Scholar] [CrossRef]
- Malenfant, A.; Forget, R.; Papillon, J.; Amsel, R.; Frigon, J.Y.; Choinière, M. Prevalence and characteristics of chronic sensory problems in burn patients. Pain 1996, 67, 493–500. [Google Scholar] [CrossRef]
- Macharia, L.M. The Prevalence of Depression among Patients with Burns. Ph.D. Thesis, University Nairobi Dept Psychiatry, Nairobi, Kenya, 2013. [Google Scholar]
- Dale, E.L.; Mueller, M.A.; Wang, L.; Fogerty, M.D.; Guy, J.S.; Nthumba, P.M. Epidemiology of operative burns at Kijabe Hospital from 2006 to 2010, pilot study of a web-based tool for creation of the Kenya Burn Repository. Burns 2013, 39, 788–795. [Google Scholar] [CrossRef] [Green Version]
- Nthumba, P.M.; Oliech, J.S. Outcome of moderate and severe thermal injuries at Kenyatta National Hospital. East Cent. Afr. J. Surg. 2005, 10, 37–42. [Google Scholar]
- Ulmer, J.F. Burn pain management: A guideline-based approach. J. Burn Care Rehabil. 1998, 19, 151–159. [Google Scholar] [CrossRef]
- Gallagher, G.; Rae, C.P.; Kinsella, J. Treatment of pain in severe burns. Am. J. Clin. Dermatol. 2000, 1, 329–335. [Google Scholar] [CrossRef]
- Castana, O.; Anagiotos, G.; Rempelos, G.; Adalopoulou, A.; Kokkinakis, C.; Giannakidou, M.; Diplas, D.B.; Alexakis, D. Pain response and pain control in burn patients. Ann. Burns Fire Disasters 2009, 22, 88–89. [Google Scholar]
- de Castro, R.J.A.; Leal, P.C.; Sakata, R.K. Pain management in burn patients. Braz. J. Anesthesiol. 2013, 63, 149–153. [Google Scholar] [CrossRef] [Green Version]
- Byers, J.F.; Bridges, S.; Kijek, J.; LaBorde, P. Burn patients’ pain and anxiety experiences. J. Burn Care Rehabil. 2001, 22, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Surgical Stress: The Role of Pain and Analgesia. Br. J. Anaesth. 1989, 63, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Patterson, D.R.; Hoflund, H.; Espey, K.; Sharar, S.R. Pain Management. In Bonica’s Management of Pain, 3rd ed.; Loeser, J., Ed.; Lippincot, Williams & Wilkins: Philadephia, PA, USA, 2001. [Google Scholar]
| Severity of Burns in TBSA | VAS Scores | Total | ||
|---|---|---|---|---|
| Moderate Pain (VAS 4–7) | Severe Pain (VAS 8–9) | Worst Pain (VAS 10) | ||
| Minor burn | 31 (64.6%) | 17 (35.4%) | 0 (0.0%) | 48 (100%) |
| Moderate burn | 28 (57.1%) | 21 (42.9%) | 0 (0.0%) | 49 (100%) |
| Major burns | 14 (34.2%) | 22 (58.5%) | 5 (7.3%) | 41(100%) |
| Total | 73(52.9%) | 62 (44.9%) | 3 (2.2%) | 138(100%) |
| Severity of Burns TBSA | Analgesia Offered | Total | |
|---|---|---|---|
| Multimodal | Unimodal | ||
| Minor | 5 (11.1%) | 40 (88.9%) | 45 (100%) |
| Moderate | 6 (12.8%) | 41 (87.2%) | 47 (100%) |
| Major | 20 (48.8%) | 21 (51.2%) | 41 (100%) |
| Total | 31 (23.3%) | 102 (76.7%) | 133 (100%) |
| Type of Analgesics Used | Burn Severity | Route of Administration | |||
|---|---|---|---|---|---|
| Intravenous | Intramuscular | ||||
| Minor | Moderate | Major | |||
| Opioids (108) | 29 (26.9%) | 40 (37%) | 39 (36.1%) | ||
| Morphine (n = 54) | 7 (13%) | 20 (37%) | 27 (50%) | 28 (51.2) | 26 (50.8) |
| Pethidine (n = 9) | 2 (22.2%) | 4 (44.4%) | 3 (33.2%) | 3 (33.3%) | 6 (66.7%) |
| Tramadol (n = 45) | 20 (44.4%) | 16 (31%) | 9 (20%) | 41 (91.1%) | 4 (8.9%) |
| Diclofenac (n = 24) | 7 (29.2%) | 5 (20.8%) | 12 (50%) | 0 | 24 (100%) |
| Paracetamol (n = 35) | 15 (42.9%) | 8 (22.8%) | 12 (34.3%) | 26 (74%) | * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotecha, V.R.; Opot, N.E.; Nangole, F. Assessment and Management of Pain in Patients Sustaining Burns at Emergency Department Kenyatta National Hospital, Kenya: A Descriptive Study. Trauma Care 2022, 2, 79-86. https://doi.org/10.3390/traumacare2010007
Kotecha VR, Opot NE, Nangole F. Assessment and Management of Pain in Patients Sustaining Burns at Emergency Department Kenyatta National Hospital, Kenya: A Descriptive Study. Trauma Care. 2022; 2(1):79-86. https://doi.org/10.3390/traumacare2010007
Chicago/Turabian StyleKotecha, Vihar R., Nyaim E. Opot, and Ferdinand Nangole. 2022. "Assessment and Management of Pain in Patients Sustaining Burns at Emergency Department Kenyatta National Hospital, Kenya: A Descriptive Study" Trauma Care 2, no. 1: 79-86. https://doi.org/10.3390/traumacare2010007
APA StyleKotecha, V. R., Opot, N. E., & Nangole, F. (2022). Assessment and Management of Pain in Patients Sustaining Burns at Emergency Department Kenyatta National Hospital, Kenya: A Descriptive Study. Trauma Care, 2(1), 79-86. https://doi.org/10.3390/traumacare2010007





