Update of the Potential Treatments for Psychiatric and Neuropsychiatric Symptoms in the Context of the Post-COVID-19 Condition: Still a Lot of Suffering and Many More Things to Learn
Abstract
:1. Introduction
1.1. What Are the Frequent Psychiatric and Neuropsychiatric Symptoms of Post-COVID-19 Syndrome?
1.2. What Are the Mechanisms Involved in Psychiatric and Neuropsychiatric Post-COVID-19?
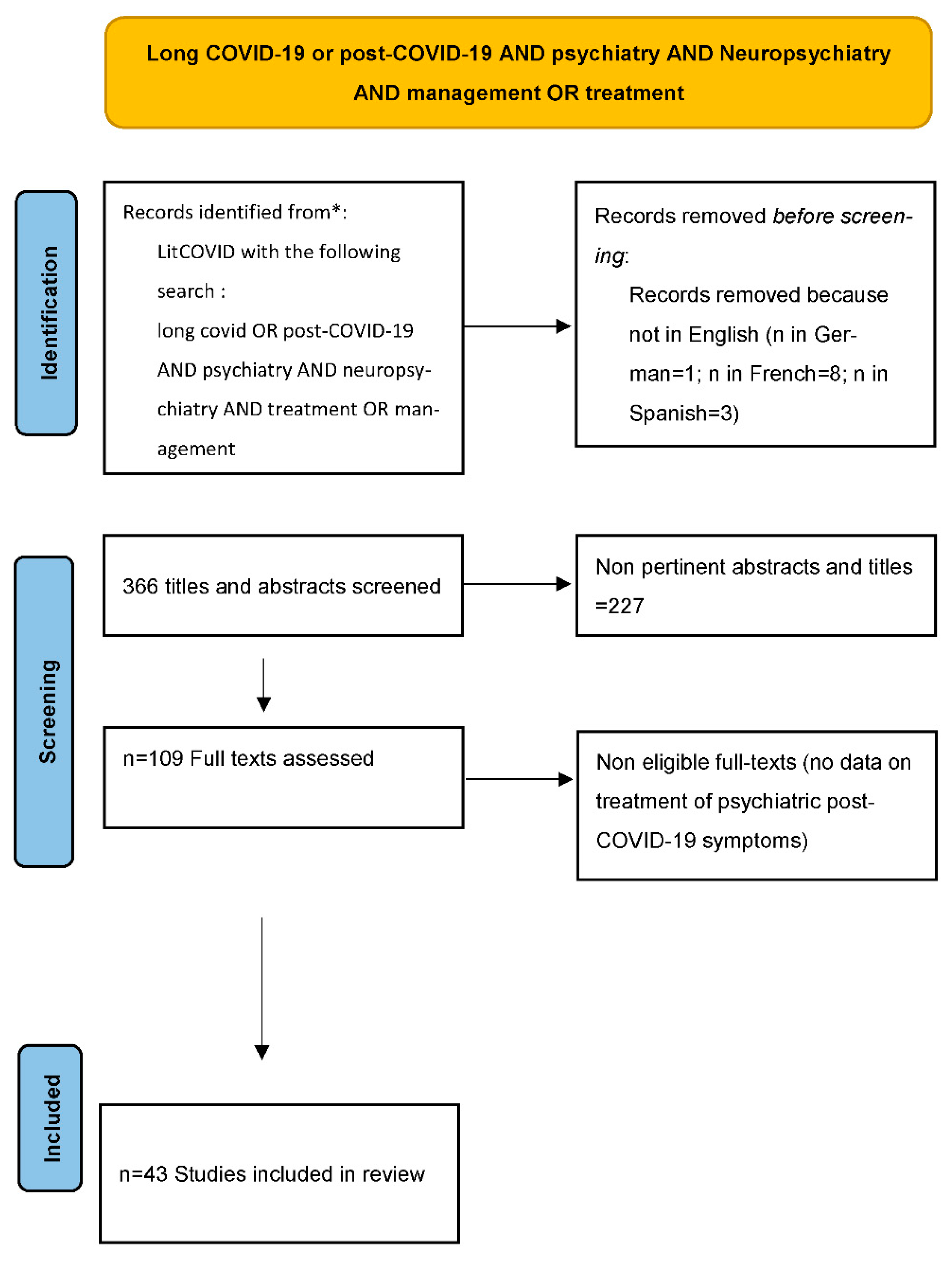
2. Materials and Methods
3. Results
3.1. A Multidisciplinary Approach
3.2. Prevention and Diagnosis Strategies of Psychiatric and Neuropsychiatric Post-COVID-19 Symptoms
3.2.1. A Systematic Screening of Psychiatric Symptoms at the Acute Phase of COVID-19
- In a prospective study with nine months follow-up, the authors assessed the predictive factors of post-COVID-19 syndrome [31]. They found that easy fatigability was the most common symptom (51.04%), followed by anxiety (38.54%), dyspnea (38.54%), and new-onset headache (38.54%) [31]. There was no association between COVID-19 severity in the acute phase and the number of long-COVID-19 symptoms and cognitive function (MoCA) scores at follow-up [31]. They also found that being female, having a higher number of symptoms, and experiencing constitutional neuropsychiatric symptoms in the acute phase were associated with having chronic fatigue syndrome at follow-up. Moreover, constitutional neuropsychiatric symptoms in the acute phase were associated with a lower MoCA score at follow-up [31]. These important results could be used to propose prevention strategies and early treatments to the patients presenting risk factors of developing post-COVID-19 syndrome mainly characterized by chronic fatigue syndrome and cognitive deficits.
- Early detection of psychiatric symptoms at the acute phase of COVID-19 by screening with the depression anxiety stress scale 21 [32] or screening peritraumatic dissociation to detect people at risk of PTSD [9] as well as early management could reduce the risk of symptoms of long psychiatric COVID-19. Some authors suggest follow-up for monitoring early, intermediate, and late complications and also preparation, self-management and supported self-management but no specific recommendation to prevent psychiatric post-COVID-19 symptoms [33].
- Ćosić et coll. maintained that mental health COVID-19 recovery programs at post-COVID-19 clinics based on AI prediction and prevention strategies may significantly improve the global mental health of ex-COVID-19 patients and that they should be developed [34].
- After post-COVID-19 syndrome is diagnosed, customized therapeutic strategies are necessary. Sancak and Kılıç insisted in a letter to the editor that of recognizing suffering and not just considering physical post-acute COVID-19 syndrome is important because somatization could lead to wrong therapeutic choices and worsen the psychic state of the patient [35]. The primary care physician plays a crucial role in the management of patients with long COVID-19. Patients often lack knowledge derived from the medical and scientific community; thus, the first therapeutic step for patients with long COVID-19 is to recognize their suffering and avoid minimization of symptoms, even though more time is needed in the scientific and medical community to clarify its pathophysiology. The primary care physician should systematically look for psychiatric symptoms in the long COVID-19 context and refer the patient for an evaluation by a psychiatrist if there is suspicion of psychiatric disorders, especially in the case of neuropsychological impairment [8].
- A rigorous evaluation and exclusion of medical differential diagnosis is paramount. Suicidal risk must be well evaluated because patients with post-COVID-19 syndrome can experience a period of crisis, making them vulnerable to suicide [66].
- Some authors consider that patients suffering from post-COVID-19 syndrome have an increased risk to initiate or increase addictive behaviors in context and consider this risk should be prevented [36]. These authors invoke the risk of prescribing opioids considering the painful symptoms but also the vulnerability to alcohol and other substances as well as behavioral addictions such as problem gambling or other addictive online behaviors in this context. They suggest systematic assessment of addiction, easy access to specialized staff in addictive behaviors, and studies focusing on the addictive risk. A prospective study concluded that especially patients with mild COVID-19 should be monitored for substance use in the post-COVID-19 period. Preventive interventions for nonmedical analgesic use should be implemented and that focused preventive interventions would be useful, especially for those who reported previous substance use, could be useful [37].
- If the patient develops post-COVID-19 polyphagia, medications which can improve appetite such as psychoactive substances such as cannabis must be looked for and avoided [16].
- Concerning post-COVID-19 fatigue, some authors defined it as a dominant chronic and disabling symptom to that interrupts all or a majority of normal activities.Post-COVID-19 fatigue is persistent for six months or more if an adult (months months in children/adolescents), and emerged during confirmed acute COVID-19 (i.e., with a positive severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2] test) without any symptom-free interval since onset. On the basis on the literature review, these authors suggested systematic brief screening questionnaires such as the Chalder fatigue scale or the SPHERE be administered to characterize the fatigue state. Related physical symptoms, mental health, and other relevant symptom domains as pain and sleep quality could be evaluated using an instrument such as the SF-36 [38].
3.2.2. Predictive Factors of Developing Psychiatric Post-COVID-19 Symptoms
- Some authors concluded that depression significantly interacted with the presence of pain at one month and was predictive of the persistence of pain at three months, with a similar trend for dyspnea [39]. The early detection and management of depression could reduce the risk of persistent pain such as persistent dyspnea. The same team concluded in another study that anxiety and depression symptoms should be systematically screened after a severe COVID-19 episode in patients presenting with cognitive complaints because cognitive impairment is associated with anxiety and depression [40]. A review confirmed standard screening tools should be used to identify patients with anxiety, depression, sleep disturbances, PTSD, dysautonomia, and fatigue [8].
- Some authors proposed looking for biomarkers associated with post-COVID-19 depression. Among the most important that were frequently described in a systematic review were increased levels of interleukin 6 (IL-6), soluble interleukin 6 receptor (sIL-6R), interleukin 1 β (IL-1β), tumor necrosis factor α (TNF-α), interferon gamma (IFN-γ), interleukin 10 (IL-10), interleukin 2 (IL-2), soluble interleukin 2 receptor (sIL-2R), C-reactive protein (CRP), Monocyte Chemoattractant Protein-1 (MCP-1), serum amyloid a (SAA1), and metabolites of the kynurenine pathway Decreased brain-derived neurotrophic factor (BDNF) and tryptophan (TRP) were also noted. The biomarkers identified by these authors indicate the etiopathogenesis of post-COVID-19 depression analogous to the leading inflammatory hypothesis of major depression disorder [41].
- Some authors showed that delayed sleep phase disorder occurs most frequently during the post-COVID-19 period [42]. However, circadian rhythm disorders can enhance affective disorders such as depressive or manic episodes.
3.2.3. Prevention Strategies
- Authors suggest targeting circadian dysfunction. They suggest to develop psychotherapeutic methods taking into account the biological rhythms and changes in working time and schedule in the first six months after the disease [42].
- Some authors conclude in a large prospective study on healthcare workers that physical activity might protect against neurocognitive impairment/fatigue symptoms after COVID-19, suggesting that physical activity could be a good preventive strategy to introduce and encourage [43].
3.3. Biological Treatments of Post-COVID-19 Psychiatric and Neuropsychiatric Symptoms
3.3.1. Usual Psychotropic Treatments
- Some authors suggested on the basis of putative mechanisms underlying post-COVID-19 anxiety, that selective serotonin reuptake inhibitor (SSRI) must be prescribed early because of their efficacy in treating anxiety disorders and COVID-19 infection through several mechanisms [44].
- They suggested avoiding other drugs in COVID-19 context, such as tricyclic antidepressants because of their anticholinergic effects, benzodiazepines because of their respiratory effects, andgabapentinoids, because of cardiac risk [44].
- Other authors investigated the efficacy of SSRI in treating post-COVID-19 depression and concluded that 92% patients of their sample showed a clinical response to antidepressants after four weeks based on a 50% HDRS reduction in the Hamilton depression rating scale (HDRS), defined as [45].
- Some authors tested tofisopam, a 2,3-benzodiazepine (2,3-BDZs) with a common chemical backbone to “classical” 1,4-benzodiazepines that does not interact with the classical benzodiazepine binding site of the GABA receptor, in a case series of three cases of post-COVID-19 patients. The cases showed potential therapeutic properties of tofisopam because of its anxiolytic effects in anxiety and depression, without sedative and muscle relaxant side effects, its antiamnestic properties, and its effects for both positive and negative symptoms of psychosis [47].
- Knowing the frequent cognitive impairment sometimes presented in post-COVID-19 syndrome patients, some treatments must be considered with caution. The American Geriatrics Society created the Beers criteria (updated 2019), a list of potentially inappropriate medications for use in older adults, 65 years and older. The American Academy of Physical Medicine and Rehabilitation (AAPM&R) Multi-Disciplinary PASC Collaborative (PASC Collaborative) warned against these medications in its guidance statement [48]. Decreasing the anticholinergic burden in patients with mild cognitive symptoms has been recommended for older patients. It is important to note that the use of pharmacologic agents and supplements varies across post-COVID-19 syndrome clinics. Prescribing medications or supplements should be considered on a case-by-case basis, recognizing the limited scientific evidence. Additionally, there should be consideration of the out-of-pocket cost of supplements, the risk of medication interactions, lack of federal regulation and oversight of supplements, and possible side effects [48].
3.3.2. Immunopsychiatric Treatments
- Some authors suggest that anticytokine treatments can help mitigate post-COVID-19 and new onset of the OC symptoms [49]. Other authors suggest that immune targeted therapies such as anticytokines and cytokine receptor blockers will not only prevent severe illness but also benefit the brain and mental health [50].
- Monoclonal antibodies blocking IL-6 or IL-17 are expected to have therapeutic effects against COVID-19 associated anxiety, but their efficacy on psychiatric post-COVID-19 symptoms have not been studied [44]. Other authors also proposed the use of anti-inflammatory medications such as minocycline and tumor necrosis factor (TNF)-alpha inhibitors to treat post-COVID-19 depression, but no clinical study exists for these potential treatments at the time of writing this article [51]. Other authors suggest that anticytokine treatments can help mitigate post-COVID-19 and new onset OC symptoms [50]. Some authors considered common mechanisms underlying Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and post-COVID-19 fatigue. They explain that they observed elevations of neurotransmitter receptor antibodies similar to what they have seen in other forms of infection-triggered ME/CFS and think that extracorporeal apheresis or immune adsorption may offer a simple and effective treatment option [52].
- Other authors suggest using an anticholinergic agent such as adamantane for its neuroprotective property to reduce cytokine storm and deposition [53].
3.3.3. Treatments Targeting Redox Imbalance
- Some authors encouraged the study of the connections between redox imbalance, inflammation, and energy metabolism in long COVID-19 and in ME/CFS and suggested some therapeutics such as NO which inhibits the replication of SARS-CoV-2 in vitro and improves oxygenation in people with COVID-19 when administered by inhalation. Ubiquinol and a combination of NADH and CoQ10 and glutathione, N-acetyl cysteine, cysteamine, sulforaphane, nicotinamide, melatonin, selenium, vitamin C, vitamin D, vitamin E, melatonin plus pentoxyfylline, disulfiram, ebselen, and corticosteroids are potential therapeutics. The authors reminded that in two cases of acute COVID-19, glutathione administered therapeutically counteracted dyspnea associated with COVID-19 pneumonia and reduced pulmonary inflammation [54].
3.3.4. Anti-Infectious Treatments
3.3.5. Endogenous Hormones and Natural Molecules
- Some authors suggested oxytocin as an adjunctive treatment in COVID-19 infection because of its proimmune properties and management of stress and anxiety, and also melatonin for its antianxiety, anti-inflammatory, anti-oxidative, neuroprotective, and cardioprotective effects. Concerning the mechanisms of action, oxytocin would counteract the cytokine storm resulting from SARS-CoV-2 infection [44].
- Llach and Vieta proposed some alternative psychotropic treatments such as erythropoietin, but no clinical trial have assessed their efficacy on psychiatric post-COVID-19 symptoms [28].
- One review summarized the potential benefit of natural molecules for treating neuropsychiatric symptoms in post-COVID-19 syndrome patients.to [54]. One is the flavonoid quercetin found in Ginkgo biloba. Quercetin has the potential to inhibit SARS-CoV-2 by blocking TNFα-induced reactive oxygen species from human aortic endothelial cells. The Ginkgo biloba extract EGb 761 has shown efficacy in generalized anxiety disorder and dementia, actions that may be useful for the neuropsychiatric aspects of long-COVID. Other studies have shown that green tea catechins could be useful in COVID-19, especially against entry of SARS-CoV-2. The broccoli extract sulforaphane inhibited expression of IL-6 and IL-8 induced by the SARS-CoV-2 spike protein in bronchial epithelial cells. Such flavonoids are found in green plants and seeds and possess potent antioxidant, anti-inflammatory, and cytoprotective properties, but their consumption as part of the diet does not provide sufficient systemic levels [55].
- Another review suggested luteolin could treat brain fog and prevent neuroinflammation, be neuroprotective, and reduce cognitive dysfunction [55].
- Quercetin has been discussed in a few recent studies, including an open-label clinical study showing good tolerability and benefit. A double-blind, placebo-controlled, randomized study using a liposomal preparation of luteolin (PureLut) in long-COVID-19 patients is underway [55].
- The same author explained combining quercetin with luteolin may provide additional benefits, especially when formulated in olive pomace oil (FibroProtek) that increases oral absorption, that is otherwise quite limited (<10%) and brings additional antiviral and anti-inflammatory benefits. Such liposomal preparations are available and have been successfully used in pilot clinical trials in which they reduced neuropsychiatric symptoms and associated serum IL-6 levels. These molecules could be proposed to patients who suffer from neuropsychiatric symptoms [56].
- L-carnitine is a micronutrient that is in nearly every cell of the body and is useful in energy metabolism and the production of cellular energy, can prevent muscle wasting or reduce muscle breakdown, modulates the composition and decomposition of proteins, and has antiapoptotic, antioxidant, and anti-inflammatory properties [57]. L-cartinine has been imagined as a potential treatment of post-COVID-19 fatigue [57].
3.4. Psychotherapeutic Treatment and Other Nonpharmacological Interventions for Psychiatric and Neuropsychiatric Post-COVID-19 Symptoms
- Some authors proposed adapting an existing cognitive behavioral therapy (CBT) manual for CFS to post-COVID-19 syndrome and called it “Fit after COVID” [58]. This psychotherapy consists of up to nine modules organized over a period of 17 weeks including an introductory module, an evaluation module to set treatment goals, and seven modules that address fatigue-perpetuating factors. Among these, are a disrupted sleep-wake pattern, low or unevenly distributed level of activity, and dysfunctional beliefs about fatigue. The authors plan four optional modules targeting perceived low social support, problems with processing the acute phase of COVID-19, fears and worries regarding COVID-19, and poor coping with pain. A randomized control trial is comparing the “Fit after COVID” program with traditional care regarding fatigue 12 months after the CBT program. Some authors, however, argue that CBT cannot be effective for post-COVID-19 fatigue [59].
- Because psychiatric post-COVID-19 symptoms are integrated with physical issues, a psychotherapeutic approach should consider both realms. Classical psychotherapeutic strategies can be limited for this reason. Taking into account the similarities of chronic fatigue syndrome (CFS), and the fatigue that exists in post-COVID-19 syndrome, some authors proposed cognitive behavioral therapy (CBT) known to be efficient for CFS [48,59,60].
- A rehabilitation team built a protocol for different kinds of chronic illnesses including patients with post-acute COVID-19 syndrome in a non-randomized clinical intervention study that is ongoing at the time of writing this article [63]. The main therapeutic axes of this protocol are: first, to prepare the patient for change prior to treatment; secondly, a focus on health promoting microchoices instead of symptoms; and third, to expect the patient to integrate the changes in everyday living with limited hands-on follow-up [63].
- Some authors suggested giving patients with post-COVID-19 syndrome breathing exercises, known to reduced anxiety; autogenic training, which can change negative views and stress; affirming statements, which help self-esteem, self-enhancement; and activity scheduling to promote physical, social, recreational, and occupational activities and build social support and regulate emotions. These strategies help counter the lack of knowledge on post-COVID-19 syndrome and the stigmatization of people suffering from it [64]. They also have revealed a significant improvement in mental health-related issues after psychological intervention, as assessed by the mental health inventory (MHI) in a sample of 30 patients.
- For polyphagia, behavioral therapies can be useful [16].
3.5. Alternative Therapeutic Devices
- Knowing the important relationship between proinflammatory cytokines and depressive symptoms, some authors suggested using transcutaneous auricular vagus nerve stimulation (taVNS) [57]. This is derived from auricular acupuncture, widely used in China [57]. These authors suggest an efficacy of taVNS on post-COVID-19 depression that involves a cholinergic anti-inflammatory pathway and modulates brain circuits via the hypothalamic-pituitary-adrenal axis [58].
- A multicenter, randomized controlled trial explored the effects of intensive care unit (ICU)-specific virtual reality (VR) on mental health and on patients’ perceived quality of, satisfaction with, and rating of ICU aftercare among COVID-19 ICU survivors. Patients in the ICU-VR group received the ICU-VR intervention once during the visit three months after hospital discharge and did not conclude differences concerning the psychological distress or quality of life but observed a better satisfaction [65].
3.6. Existing Specific Recommendations for Neuropsychiatric Post-COVID-19 Symptoms
- The American Academy of Physical Medicine and Rehabilitation (AAPM&R) Multi-Disciplinary PASC Collaborative (PASC Collaborative) was created and published a guidance statement with a specific focus on the cognitive-related symptoms of PASC that can occur in people who have been diagnosed with acute COVID-19 infection or presumed to have had the infection and initially experienced mild to severe symptoms [42]. This guidance statement defined Cognitive symptom assessment recommendation statements discussion and therapeutic interventions. The five recommendations are as follows: (1) For patients who screen positive for cognitive symptoms, refer to a specialist with expertise in formal cognitive assessment and remediation; (2) Treat, in collaboration with appropriate specialists, underlying medical conditions, such as pain, insomnia/sleep disorders, and mood disorders that may be contributing to cognitive symptoms; (3) Complete, in collaboration with patient primary care provider, medication polypharmacy reduction, weaning or deprescribing medications if medically feasible with emphasis on medications that may impact cognition; (4) Reinforce sleep hygiene techniques including nonpharmacologic approaches as first line of sleep remediation; (5) Similar to patients experiencing “physical” fatigue, patients should be advised to begin an individualized and structured, titrated return to activity program; (5a) For patients who achieve a return to their normal, daily activities, regular exercise (at least 2–3 times/week of aerobic exercise) may be effective in improving cognition and also contribute to improved sleep patterns; (5b) Frequent assessment of the impact of return to normal, daily activities is recommended to ensure that symptoms do not flare and exercise is tolerated [48].
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alwan, N.A.; Johnson, L. Defining long COVID: Going back to the start. Med 2021, 2, 501–504. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health. Available online: https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-COVID-19 (accessed on 5 February 2022).
- Nehme, M.; Braillard, O.; Alcoba, G.; Perone, S.A.; Courvoisier, D.; Chappuis, F.; Guessous, I. COVID-19 Symptoms: Longitudinal Evolution and Persistence in Outpatient Settings. Ann. Intern. Med. 2021, 174, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic dysfunction in ‘long COVID’: Rationale, physiology and management strategies. Clin. Med. 2020, 21, e63–e67. [Google Scholar] [CrossRef]
- World Health Organization. Available online: WHO/2019-nCoV/Post_COVID-19_condition/Clinical_case_definition/2021.1 (accessed on 5 February 2022).
- Taquet, M.; Luciano, S.; Geddes, J.R.; Harrison, P.J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 2020, 8, 130–140. [Google Scholar] [CrossRef]
- Callard, F.; Perego, E. How and why patients made Long COVID. Soc. Sci. Med. 2020, 268, 113426. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Benzakour, L.; Braillard, O.; Mazzola, V.; Gex, D.; Nehme, M.; Perone, S.A.; Agoritsas, T.; Kopp, G.; Cereghetti, S.; Bondolfi, G.; et al. Impact of peritraumatic dissociation in hospitalized patients with COVID-19 pneumonia: A longitudinal study. J. Psychiatr. Res. 2021, 140, 53–59. [Google Scholar] [CrossRef]
- Raman, B.; Cassar, M.P.; Tunnicliffe, E.M.; Filippini, N.; Griffanti, L.; Alfaro-Almagro, F.; Okell, T.; Sheerin, F.; Xie, C.; Mahmod, M.; et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. eClinicalMedicine 2021, 31, 100683. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Taverne, J.; Salvator, H.; Leboulch, C.; Barizien, N.; Ballester, M.; Imhaus, E.; Chabi-Charvillat, M.-L.; Boulin, A.; Goyard, C.; Chabrol, A.; et al. High incidence of hyperventilation syndrome after COVID-19. J. Thorac. Dis. 2021, 13, 3918–3922. [Google Scholar] [CrossRef]
- Culpepper, L.; Lam, R.W.; McIntyre, R.S. Cognitive Impairment in Patients With Depression: Awareness, Assessment, and Management. J. Clin. Psychiatry 2017, 78, 1383–1394. [Google Scholar] [CrossRef] [PubMed]
- Lima, I.M.; Peckham, A.D.; Johnson, S.L. Cognitive deficits in bipolar disorders: Implications for emotion. Clin. Psychol. Rev. 2017, 59, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Gindt, M.; Hot, P. Cognitive impairment in trauma. In Knowledge to Heal; Canini, F., El-Hage, W., Eds.; Mona Edition: Paris, France, 2017; pp. 201–209. [Google Scholar]
- Kaggwa, M.M.; Favina, A.; Najjuka, S.M.; Zeba, Z.; Mamun, M.A.; Bongomin, F. Excessive eating and weight gain:A rare post-acute COVID-19 syndrome. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102252. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Newman, M.; Kunik, M.E. Psychiatric Collaborative Care for Patients With Respiratory Disease. Chest 2019, 155, 1288–1295. [Google Scholar] [CrossRef]
- Troubat, R.; Barone, P.; Leman, S.; DeSmidt, T.; Cressant, A.; Atanasova, B.; Brizard, B.; El Hage, W.; Surget, A.; Belzung, C.; et al. Neuroinflammation and depression: A review. Eur. J. Neurosci. 2020, 53, 151–171. [Google Scholar] [CrossRef]
- van Vuren, E.J.; Steyn, S.F.; Brink, C.B.; Möller, M.; Viljoen, F.P.; Harvey, B.H. The neuropsychiatric manifestations of COVID-19: Interactions with psychiatric illness and pharmacological treatment. Biomed. Pharmacother. 2021, 135, 111200. [Google Scholar] [CrossRef]
- Jackson, J.C.; Pandharipande, P.; Girard, T.; Brummel, N.E.; Thompson, J.L.; Hughes, C.G.; Pun, B.T.; Vasilevskis, E.E.; Morandi, A.; Shintani, A.K.; et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: A longitudinal cohort study. Lancet Respir. Med. 2014, 2, 369–379. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.; Allot, A.; Lu, Z. LitCovid: An open database of COVID-19 literature. Nucleic Acids Res. 2020, 49, D1534–D1540. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, 105906. [Google Scholar] [CrossRef]
- Barker-Davies, R.M.; O’Sullivan, O.; Senaratne, K.P.P.; Baker, P.; Cranley, M.; Dharm-Datta, S.; Ellis, H.; Goodall, D.; Gough, M.; Lewis, S.; et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br. J. Sports Med. 2020, 54, 949–959. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.M.; Brigham, E.; Connolly, B.; McPeake, J.; Agranovich, A.V.; Kenes, M.T.; Casey, K.; Reynolds, C.; Schmidt, K.F.R.; Kim, S.Y.; et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: A multidisciplinary model of care. Lancet Respir. Med. 2021, 9, 1328–1341. [Google Scholar] [CrossRef] [PubMed]
- Horn, M.; Fovet, T.; Vaiva, G.; D’Hondt, F.; Amad, A. Somatic symptom disorders and long COVID: A critical but overlooked topic. Gen. Hosp. Psychiatry 2021, 72, 149–150. [Google Scholar] [CrossRef]
- Llach, C.-D.; Vieta, E. Mind Long COVID: Psychiatric sequelae of SARS-CoV-2 infection. Eur. Neuropsychopharmacol. 2021, 49, 119–121. [Google Scholar] [CrossRef]
- Nakamura, Z.M.; Nash, R.P.; Laughon, S.L.; Rosenstein, D.L. Neuropsychiatric Complications of COVID-19. Curr. Psychiatry Rep. 2021, 23, 25. [Google Scholar] [CrossRef]
- Ahmad, M.; Kim, K.; Indorato, D.; Petrenko, I.; Diaz, K.; Rotatori, F.; Salhany, R.; Lakhi, N. Post-COVID Care Center to Address Rehabilitation Needs in COVID-19 Survivors. Am. J. Med. Qual. 2021. [Google Scholar] [CrossRef]
- Mirfazeli, F.S.; Sarabi-Jamab, A.; Pereira-Sanchez, V.; Kordi, A.; Shariati, B.; Shariat, S.V.; Bahrami, S.; Nohesara, S.; Almasi-Dooghaee, M.; Faiz, S.H.R. Chronic fatigue syndrome and cognitive deficit are associated with acute-phase neuropsychiatric manifestations of COVID-19: A 9-month follow-up study. Neurol. Sci. 2022, 43, 2231–2239. [Google Scholar] [CrossRef]
- Ali, A.M.; Alkhamees, A.A.; Hori, H.; Kim, Y.; Kunugi, H. The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World. Int. J. Environ. Res. Public Health 2021, 18, 10142. [Google Scholar] [CrossRef]
- Garg, M.; Maralakunte, M.; Garg, S.; Dhooria, S.; Sehgal, I.; Bhalla, A.S.; Vijayvergiya, R.; Grover, S.; Bhatia, V.; Jagia, P.; et al. The Conundrum of ‘Long-COVID-19ʹ: A Narrative Review. Int. J. Gen. Med. 2021, 14, 2491–2506. [Google Scholar] [CrossRef]
- Ćosić, K.; Popović, S.; Šarlija, M.; Kesedžić, I.; Gambiraža, M.; Dropuljić, B.; Mijić, I.; Henigsberg, N.; Jovanovic, T. AI-Based Prediction and Prevention of Psychological and Behavioral Changes in Ex-COVID-19 Patients. Front. Psychol. 2021, 12, 782866. [Google Scholar] [CrossRef] [PubMed]
- Sancak, B.; Kılıç, C. A Psychiatrist’s Own Experience of Long COVID: Looking Beyond the Psychosomatic Perspective. Psychiatr. Danub. 2021, 33, 250. [Google Scholar] [PubMed]
- Håkansson, A. Post-COVID syndrome: Need to include risk of addiction in research and multi-disciplinary clinical work. Psychiatry Res. 2021, 301, 113961. [Google Scholar] [CrossRef] [PubMed]
- Ismael, F.; Zaramella, B.; Battagin, T.; Bizario, J.C.S.; Gallego, J.; Villela, V.; de Queiroz, L.B.; Leal, F.E.; Torales, J.; Ventriglio, A.; et al. Substance Use in Mild-COVID-19 Patients: A Retrospective Study. Front. Public Health 2021, 9, 634396. [Google Scholar] [CrossRef]
- Sandler, C.X.; Wyller, V.B.B.; Moss-Morris, R.; Buchwald, D.; Crawley, E.; Hautvast, J.; Katz, B.Z.; Knoop, H.; Little, P.; Taylor, R.; et al. Long COVID and Post-infective Fatigue Syndrome: A Review. Open Forum Infect. Dis. 2021, 8, ofab440. [Google Scholar] [CrossRef]
- Bottemanne, H.; Gouraud, C.; Hulot, J.-S.; Blanchard, A.; Ranque, B.; Lahlou-Laforêt, K.; Limosin, F.; Günther, S.; Lebeaux, D.; Lemogne, C. Do Anxiety and Depression Predict Persistent Physical Symptoms After a Severe COVID-19 Episode? A Prospective Study. Front. Psychiatry 2021, 12, 757685. [Google Scholar] [CrossRef]
- Gouraud, C.; Bottemanne, H.; Lahlou-Laforêt, K.; Blanchard, A.; Günther, S.; El Batti, S.; Auclin, E.; Limosin, F.; Hulot, J.-S.; Lebeaux, D.; et al. Association Between Psychological Distress, Cognitive Complaints, and Neuropsychological Status After a Severe COVID-19 Episode: A Cross-Sectional Study. Front. Psychiatry 2021, 12, 725861. [Google Scholar] [CrossRef]
- Lorkiewicz, P.; Waszkiewicz, N. Biomarkers of Post-COVID Depression. J. Clin. Med. 2021, 10, 4142. [Google Scholar] [CrossRef]
- Boiko, D.I.; Skrypnikov, A.M.; Shkodina, A.D.; Hasan, M.M.; Ashraf, G.M.; Rahman, H. Circadian rhythm disorder and anxiety as mental health complications in post-COVID-19. Environ. Sci. Pollut. Res. 2022, 1–8. [Google Scholar] [CrossRef]
- Strahm, C.; Seneghini, M.; Güsewell, S.; Egger, T.; Leal, O.; Brucher, A.; Lemmenmeier, E.; Kleeb, D.M.; Möller, J.C.; Rieder, P.; et al. Symptoms compatible with long-COVID in healthcare workers with and without SARS-CoV-2 infection—Results of a prospective multicenter cohort. Clin. Infect. Dis. 2022. [Google Scholar] [CrossRef]
- Uzunova, G.; Pallanti, S.; Hollander, E. Presentation and management of anxiety in individuals with acute symptomatic or asymptomatic COVID-19 infection, and in the post-COVID-19 recovery phase. Int. J. Psychiatry Clin. Pract. 2021, 25, 115–131. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; Zanardi, R.; Palladini, M.; Rovere-Querini, P.; Benedetti, F. Rapid response to selective serotonin reuptake inhibitors in post-COVID depression. Eur. Neuropsychopharmacol. 2021, 54, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, L. Lessons from psychiatry for treating post-acute COVID-19 fatigue. Australas. Psychiatry 2021, 29, 560–561. [Google Scholar] [CrossRef]
- Pattnaik, J.I.; Deepthi, R.A.; Dua, S.; Padhan, P.; Ravan, J.R. Role of Tofisopam in Post COVID Neuro-psychiatric Sequelae: A Case Series. Indian J. Psychol. Med. 2021, 43, 174–176. [Google Scholar] [CrossRef] [PubMed]
- Fine, J.S.; Ambrose, A.F.; Didehbani, N.; Fleming, T.K.; Glashan, L.; Longo, M.; Merlino, A.; Ng, R.; Nora, G.J.; Rolin, S.; et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of cognitive symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PM&R 2021, 14, 96–111. [Google Scholar] [CrossRef]
- Nezgovorova, V.; Ferretti, C.J.; Pallanti, S.; Hollander, E. Modulating neuroinflammation in COVID-19 patients with obsessive-compulsive disorder. J. Psychiatr. Res. 2021. [Google Scholar] [CrossRef]
- Mondelli, V.; Pariante, C.M. What can neuroimmunology teach us about the symptoms of long-COVID? Oxf. Open Immunol. 2021, 2, iqab004. [Google Scholar] [CrossRef]
- Penninx, B.W. Psychiatric symptoms and cognitive impairment in “Long COVID”: The relevance of immunopsychiatry. World Psychiatry 2021, 20, 357–358. [Google Scholar] [CrossRef]
- Bornstein, S.R.; Voit-Bak, K.; Donate, T.; Rodionov, R.N.; Gainetdinov, R.R.; Tselmin, S.; Kanczkowski, W.; Müller, G.M.; Achleitner, M.; Wang, J.; et al. Chronic post-COVID-19 syndrome and chronic fatigue syndrome: Is there a role for extracorporeal apheresis? Mol. Psychiatry 2021, 17, 1–4. [Google Scholar] [CrossRef]
- Paul, B.D.; Lemle, M.D.; Komaroff, A.L.; Snyder, S.H. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proc. Natl. Acad. Sci. USA 2021, 118, e2024358118. [Google Scholar] [CrossRef]
- Damiano, R.F.; Guedes, B.F.; de Rocca, C.C.; Serafim, A.D.P.; Castro, L.H.M.; Munhoz, C.D.; Nitrini, R.; Filho, G.B.; Miguel, E.C.; Lucchetti, G.; et al. Cognitive decline following acute viral infections: Literature review and projections for post-COVID-19. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 272, 139–154. [Google Scholar] [CrossRef] [PubMed]
- Theoharides, T.C. Could SARS-CoV-2 Spike Protein Be Responsible for Long-COVID Syndrome? Mol. Neurobiol. 2022, 59, 1850–1861. [Google Scholar] [CrossRef] [PubMed]
- Theoharides, T.C.; Cholevas, C.; Polyzoidis, K.; Politis, A. Long-COVID syndrome-associated brain fog and chemofog: Luteolin to the rescue. BioFactors 2021, 47, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Vaziri-Harami, R.; Delkash, P. Can l-carnitine reduce post-COVID-19 fatigue? Ann. Med. Surg. 2021, 73, 103145. [Google Scholar] [CrossRef]
- Guo, Z.-P.; Sörös, P.; Zhang, Z.-Q.; Yang, M.-H.; Liao, D.; Liu, C.-H. Use of Transcutaneous Auricular Vagus Nerve Stimulation as an Adjuvant Therapy for the Depressive Symptoms of COVID-19: A Literature Review. Front. Psychiatry 2021, 12, 765106. [Google Scholar] [CrossRef]
- Kuut, T.A.; Müller, F.; Aldenkamp, A.; Assmann-Schuilwerve, E.; Braamse, A.; Geerlings, S.E.; Gibney, K.B.; Kanaan, R.A.A.; Nieuwkerk, P.; Hartman, T.C.O.; et al. A randomised controlled trial testing the efficacy of Fit after COVID, a cognitive behavioural therapy targeting severe post-infectious fatigue following COVID-19 (ReCOVer): Study protocol. Trials 2021, 22, 867. [Google Scholar] [CrossRef]
- Vink, M.; Vink-Niese, A. Could Cognitive Behavioural Therapy Be an Effective Treatment for Long COVID and Post COVID-19 Fatigue Syndrome? Lessons from the Qure Study for Q-Fever Fatigue Syndrome. Healthcare 2020, 8, 552. [Google Scholar] [CrossRef]
- Verveen, A.; Müller, F.; Lloyd, A.; Moss-Morris, R.; Omland, T.; Penninx, B.; Raijmakers, R.P.; van der Schaaf, M.; Sandler, C.X.; Stavem, K.; et al. A research agenda for post-COVID-19 fatigue. Psychosomatics 2022, 154, 110726. [Google Scholar] [CrossRef]
- Akbarialiabad, H.; Taghrir, M.H.; Abdollahi, A.; Ghahramani, N.; Kumar, M.; Paydar, S.; Razani, B.; Mwangi, J.; Asadi-Pooya, A.A.; Malekmakan, L.; et al. Long COVID, a comprehensive systematic scoping review. Infection 2021, 49, 1163–1186. [Google Scholar] [CrossRef]
- Kvale, G.; Frisk, B.; Jürgensen, M.; Børtveit, T.; Ødegaard-Olsen, Ø.T.; Wilhelmsen-Langeland, A.; Aarli, B.B.; Sandnes, K.; Rykken, S.; Haugstvedt, A.; et al. Evaluation of Novel Concentrated Interdisciplinary Group Rehabilitation for Patients With Chronic Illnesses: Protocol for a Nonrandomized Clinical Intervention Study. JMIR Res. Protoc. 2021, 10, e32216. [Google Scholar] [CrossRef]
- Priyamvada, R.; Ranjan, R.; Chaudhury, S. Efficacy of psychological intervention in patients with post-COVID-19 anxiety. Ind. Psychiatry J. 2021, 30 (Suppl. S1), S41–S44. [Google Scholar] [CrossRef]
- Vlake, J.H.; van Bommel, J.; Wils, E.-J.; Bienvenu, J.; Hellemons, M.E.; Korevaar, T.I.; Schut, A.F.; Labout, J.A.; Schreuder, L.L.; van Bavel, M.P.; et al. Intensive Care Unit–Specific Virtual Reality for Critically Ill Patients With COVID-19: Multicenter Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e32368. [Google Scholar] [CrossRef] [PubMed]
- Sher, L. The impact of the COVID-19 pandemic on suicide rates. QJM Int. J. Med. 2020, 113, 707–712. [Google Scholar] [CrossRef]
- Sikter, A.; Frecska, E.; Braun, I.M.; Gonda, X.; Rihmer, Z. The role of hyperventilation: Hypocapnia in the pathomechanism of panic disorder. Rev. Bras. Psiquiatr. 2007, 29, 375–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Title | Author | Type of Article | Findings |
|---|---|---|---|
| Post-acute COVID-19 syndrome. | Nalbandian et al., 2021. [8] | Review | Principle of multidisciplinary management. |
| Excessive eating and weight gain: A rare post-acute COVID-19 syndrome. | Kaggwa et al., 2021. [16] | Review | Suggest avoiding medications that improve appetite (cannabis); propose behavioral therapy. |
| The Stanford Hall consensus statement for post-COVID-19 rehabilitation. | Barker-Davies et al., 2020. [25] | Review | Multidisciplinary care consensus. |
| Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. | Parker et al., 2021. [26] | Review | Need for multidisciplinary care. |
| Somatic symptom disorders and long COVID: A critical but overlooked topic. | Horn et al., 2021. [27] | Letter to editor | Usefulness of the SSD scale (SSD-12), designed to assess based on the DSM-5 criteria and importance of consultation-liaison psychiatrists. |
| Mind long COVID: Psychiatric sequelae of SARS-CoV-2 infection. | Llach and Vieta 2021. [28] | Letter to editor | Innovative therapeutics such as cognitive functional remediation for cognitive disorders, psychostimulants or erythropoietin. |
| Neuropsychiatric Complications of COVID-19. | Nakamura, 2021. [29] | Review | Management of post-acute COVID-19 neuropsychiatric symptoms. |
| Post-COVID Care Center to Address Rehabilitation Needs in COVID-19 Survivors: A Model of Care. | Ahmad et al., 2021. [30] | The need for early targeted rehabilitation Post-COVID-19 care centers. | |
| Chronic fatigue syndrome and cognitive deficit are associated with acute-phase neuropsychiatric manifestations of COVID-19: A 9-month follow-up study. | Mirfazeli et al., 2022. [31] | Prospective observational study | Being female, having a higher number of symptoms, and experiencing constitutional neuropsychiatric symptoms in the acute phase were associated with having chronic fatigue syndrome at follow-up. Constitutional neuropsychiatric symptoms in the acute phase were associated with a lower MoCA score at follow-up |
| The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post-COVID-19 World. | Ali et al., 2021. [32] | Review | Prevention by the screening with the depression anxiety stress scale 21. |
| The Conundrum of ‘Long-COVID-19’: A Narrative Review. | Garg et al., 2021. [33] | Narrative review | Close follow-up for monitoring early, intermediate, and late complications but also a preparation and a self-management and supported self-management. |
| AI-Based Prediction and Prevention of Psychological and Behavioral Changes in Ex-COVID-19 Patients. | Ćosić et al., 2021. [34] | Review | Predictive tools based on AI to optimize prevention. |
| A Psychiatrist’s Own Experience of Long COVID: Looking Beyond the Psychosomatic Perspective. | Sancak, B., & Kılıç, C. (2021). [35] | Letter to editor | Importance to recognize suffering and not just consider physical post-acute COVID-19 syndrome as somatization. |
| Post-COVID syndrome: Need to include risk of addiction in research and multi-disciplinary clinical work. | Håkansson, 2021. [36] | Review | Increased risk to initiate or increase addictive behaviors in context and consider this risk should be prevented. |
| Substance Use in Mild-COVID-19 Patients: A Retrospective Study. | Ismael, (2021). [37] | Review | Focused preventive interventions increasing the perceived risks of cannabis and non-medical benzodiazepine and analgesic use. |
| Long COVID and Post-infective Fatigue Syndrome: A Review. | Sandler et al., 2021. [38] | Review | Necessity to precisely assess fatigue and its main factors. |
| Do Anxiety and Depression Predict Persistent Physical Symptoms After a Severe COVID-19 Episode? A Prospective Study. | Bottemanne, H., et al., 2021. [39] | Observational and prospective study | Depression significantly interacted with the presence of pain at one month in predicting the persistence of pain at three months, with a similar trend for dyspnea. |
| Association Between Psychological Distress, Cognitive Complaints, and Neuropsychological Status After a Severe COVID-19 Episode: A Cross-Sectional Study. | Gouraud et al., 2021. [40] | Cross-sectional study | Anxiety and depression symptoms should be systematically screened after a severe COVID-19 episode in patients presenting with cognitive complaints. |
| Biomarkers of Post-COVID Depression. | Lorkiewic et al., 2021. [41] | Review | Biomarkers found to prevent and early manage depression such as IL-6, sIL-6R, IL-1β, TNF-α, IFN-γ, IL-10, IL-2, sIL-2R, CRP, (MCP-1, SAA1,BDNF, TRP. |
| Circadian rhythm disorder and anxiety as mental health complications in post-COVID-19 | Boiko et al., 2022. [42] | Review | Psychotherapeutic methods taking into account the biological rhythms. |
| Symptoms compatible with long-COVID in healthcare workers with and without SARS-CoV-2 infection—results of a prospective multicenter cohort. | Strahm et al., 2022. [43] | Review | Physical activity might be protective against neurocognitive impairment/fatigue symptoms. |
| Presentation and management of anxiety in individuals with acute symptomatic or asymptomatic COVID-19 infection and in the post-COVID-19 recovery phase. | Uzunova et al., 2021. [44] | Review | Overview of pharmacological and innovative treatments. |
| Rapid response to selective serotonin reuptake inhibitors in post-COVID depression. | Mazza et al., 2022. [45] | Clinical trial | N = 60, 92% had a reduction of HDRS >50% with antidepressant after one month. |
| Lessons from psychiatry for treating post-acute COVID-19 fatigue. | Wainwright L. (2021). [46] | Letter to editor. | Lisdexamfetamine efficacy and CBT for fatigue. |
| Role of Tofisopam in Post-COVID Neuro-psychiatric Sequelae: A Case Series. | Pattnaik et al., 2021. [47] | Review | Indicated for psychiatric post-COVID-19 symptoms because its anxiolytic effect on anxiety and depression, without sedative and muscle relaxant side effects, its antiamnestic properties, and its effects for both positive and negative symptoms of psychosis. |
| Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of cognitive symptoms in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). | Fine et al., 2022. [48] | Review | Guidance statement defined Cognitive symptom assessment recommendation statements discussion and therapeutic interventions. The five recommendations are as follow (1) refer to a specialist with expertise in formal cognitive assessment and remediation; (2) Treat, in collaboration with appropriate specialists; (3) Complete, in collaboration with patient primary care provider, medication polypharmacy reduction; (4) Reinforce sleep hygiene techniques including nonpharmacologic approaches; (5) patients should be advised to begin an individualized and structured, titrated return to activity program. |
| Modulating neuroinflammation in COVID-19 patients with obsessive-compulsive disorder. | Nezgovorova et al., 2021. [49] | Review | Suggest that anticytokine treatments can help mitigate post-COVID-19 and new onset of the OC symptoms. |
| What can neuroimmunology teach us about the symptoms of long-COVID?. | Mondelli et al., 2021. [50] | Review | Potential therapeutic efficacy of immune targeted therapies (such as anticytokines and cytokine receptor blockers). |
| Psychiatric symptoms and cognitive impairment in “Long COVID”: the relevance of immunopsychiatry. | Penninx et al., 2021. [51] | Review | Potential immunopsychaitric therapeutic strategies in psychiatric post-COVID-19 symptoms treatment. |
| Chronic post-COVID-19 syndrome and chronic fatigue syndrome: Is there a role for extracorporeal apheresis? | Bornstein et al., 2021. [52] | Review ME/CFS in post-COVID-19 patients and therapeutic options | Potential therapeutic use of extracorporeal apharesis. |
| Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. | Paul et al., 2021. [53] | Review | Potential redox-based therapeutics. |
| Cognitive decline following acute viral infections: literature review and projections for post-COVID-19. | Damiano et al., 2021. [54] | Review | Potential benefit for post-COVID-19 syndrome of natural molecules in post-COVID-19 syndrome to treat neuropsychiatric symptoms. Current randomized controlled trials (RCTs) are investigating the effect of antiviral therapy for the treatment of AD |
| Could SARS-CoV-2 Spike Protein Be Responsible for Long-COVID Syndrome ? | Theoharides, 2022. [55] | Review | Involvement of SARS-CoV-2 in post-COVID-19 and putative treatments of luteolin, quercetin, olive pomace. |
| Long-COVID syndrome-associated brain fog and chemofog: Luteolin to the rescue. | Theoharides, et al., 2021. [56] | Review | Quercetin in combination with luteolin to prevent and reduce cognitive impairment and neuroinflammation. |
| Can l-carnitine reduce post-COVID-19 fatigue? | Vaziri-Harami & Delkash, 2022. [57] | Review | l-carnitine efficacious on psychiatric symptoms treatment and prevention and fatigue. |
| Use of Transcutaneous Auricular Vagus Nerve Stimulation as an Adjuvant Therapy for the Depressive Symptoms of COVID-19: A Literature Review. | Guo et al., 2021. [58] | Review | Propose to use transcutaneous auricular vagus to treat depression knowing effects on cytokine. Involve cholinergic anti-inflammatory pathway and modulates brain circuits via the hypothalamic-pituitary-adrenal axis |
| A randomised controlled trial testing the efficacy of Fit after COVID, a cognitive behavioural therapy targeting severe post-infectious fatigue following COVID-19 (ReCOVer): study protocol. | Kuut et al., 2021. [59] | RCT | Study in progress to assess efficiency of adapted CBT for post-COVID-19 fatigue. |
| Could Cognitive Behavioural Therapy Be an Effective Treatment for Long COVID and Post-COVID-19 Fatigue Syndrome? Lessons from the Qure Study for Q-Fever Fatigue Syndrome. | Vink & vink-niese, 2020. [60] | Review | Potential efficiency of CBT as with Q-Fever Fatigue Syndrome. |
| A research agenda for post-COVID-19 fatigue. Journal of psychosomatic research, 154, 110726. | Verveen et al., 2022. [61] | Review | Treatment of post-COVID-19 fatigue could be CBT or exercize but studies are needed. Prevention strategies must be found. |
| Long COVID, a comprehensive systematic scoping review. | Akbarialiabad et al., 2021. [62] | Review | Few data on treatment for psychiatric post-COVID-19 symptoms but more on fatigue and general state. |
| Evaluation of Novel Concentrated Interdisciplinary Group Rehabilitation for Patients With Chronic Illnesses: Protocol for a Nonrandomized Clinical Intervention Study. | Kvale et al., 2021. [63] | Intervention study a non-randomized clinical intervention study | Study in progress of main therapeutic axes are first to prepare the patient for change prior to treatment; second, a focus on health promoting microchoices instead of symptoms; and third, to expect the patient to integrate the changes in everyday living with limited hands-on follow-up. |
| Efficacy of psychological intervention in patients with post-COVID-19 anxiety. | Priyamvada et al., 2021. [64] | Interventional study | Intervention consisting of breathing exercises, autogenic training activity scheduling, and social support and emotion regulation permitted a significant improvement of the MHI (n = 30). |
| Intensive Care Unit-Specific Virtual Reality (ICU-VR) for Critically Ill COVID-19 Patients: A Multicenter, Randomized Controlled Trial. | Vlake et al., 2021. [65] | Multicenter RCT | No effects of ICU-specific virtual reality on psychological distress nor on quality of life but a better satisfaction. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benzakour, L.; Bondolfi, G. Update of the Potential Treatments for Psychiatric and Neuropsychiatric Symptoms in the Context of the Post-COVID-19 Condition: Still a Lot of Suffering and Many More Things to Learn. Trauma Care 2022, 2, 131-150. https://doi.org/10.3390/traumacare2020011
Benzakour L, Bondolfi G. Update of the Potential Treatments for Psychiatric and Neuropsychiatric Symptoms in the Context of the Post-COVID-19 Condition: Still a Lot of Suffering and Many More Things to Learn. Trauma Care. 2022; 2(2):131-150. https://doi.org/10.3390/traumacare2020011
Chicago/Turabian StyleBenzakour, Lamyae, and Guido Bondolfi. 2022. "Update of the Potential Treatments for Psychiatric and Neuropsychiatric Symptoms in the Context of the Post-COVID-19 Condition: Still a Lot of Suffering and Many More Things to Learn" Trauma Care 2, no. 2: 131-150. https://doi.org/10.3390/traumacare2020011
APA StyleBenzakour, L., & Bondolfi, G. (2022). Update of the Potential Treatments for Psychiatric and Neuropsychiatric Symptoms in the Context of the Post-COVID-19 Condition: Still a Lot of Suffering and Many More Things to Learn. Trauma Care, 2(2), 131-150. https://doi.org/10.3390/traumacare2020011







