The Impact of a Cervical Collar on Intracranial Pressure in Traumatic Brain Injury Patients: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection Process
2.4. Data Extraction and Synthesis
2.5. Quality Assessment and Statistical Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
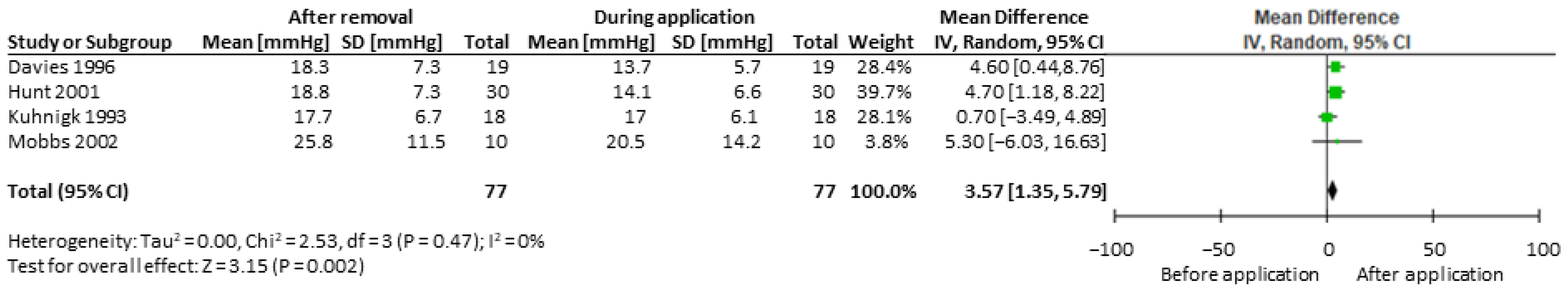
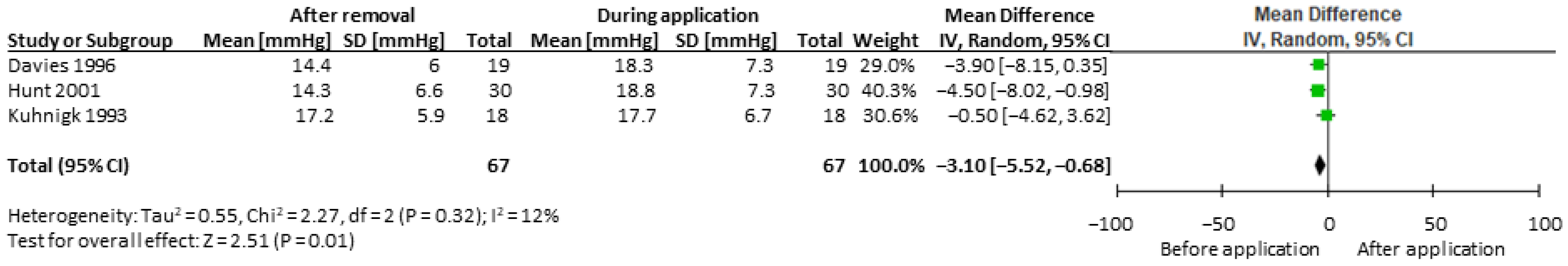
3.4. Meta-Analysis for ICP during and after Collar Application
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blennow, K.; Brody, D.L.; Kochanek, P.M.; Levin, H.; McKee, A.; Ribbers, G.M.; Yaffe, K.; Zetterberg, H. Traumatic brain injuries. Nat. Rev. Dis. Prim. 2016, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, C.; Carretta, A.; Nicolosi, F.; Morselli, C. Epidemiology of severe traumatic brain injury. J. Neurosurg. Sci. 2018, 62, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Stiver, S.I.; Manley, G.T. Prehospital management of traumatic brain injury. Neurosurg. Focus 2008, 25, E5. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.A.; Rojanasarntikul, D.; Jagoda, A. The prehospital management of traumatic brain injury. J. Paramed. Pract. 2015, 127, 367–378. [Google Scholar]
- Boer, C.; Franschman, G.; Loer, S.A. Prehospital management of severe traumatic brain injury: Concepts and ongoing controversies. Curr. Opin. Anesthesiol. 2012, 25, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Theodore, N.; Hadley, M.N.; Aarabi, B.; Dhall, S.S.; Gelb, D.E.; Hurlbert, R.J.; Rozzelle, C.J.; Ryken, T.C.; Walters, B.C. Prehospital cervical spinal immobilization after trauma. Neurosurgery 2013, 72 (Suppl. S3), 22–34. [Google Scholar] [CrossRef] [Green Version]
- Rogers, L. No place for the rigid cervical collar in pre-hospital care. Int. Paramedic Pract. 2017, 7, 12–15. [Google Scholar] [CrossRef]
- Barati, K.; Arazpour, M.; Vameghi, R.; Abdoli, A.; Farmani, F. The effect of soft and rigid cervical collars on head and neck immobilization in healthy subjects. Asian Spine J. 2017, 11, 390. [Google Scholar] [CrossRef] [Green Version]
- Mobbs, R.J.; Stoodley, M.A.; Fuller, J. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J. Surg. 2002, 72, 389–391. [Google Scholar] [CrossRef]
- Sundstrøm, T.; Asbjørnsen, H.; Habiba, S.; Sunde, G.A.; Wester, K. Prehospital use of cervical collars in trauma patients: A critical review. J. Neurotrauma. 2014, 31, 531–540. [Google Scholar] [CrossRef] [Green Version]
- Conner, E.; Moy, H.P. CE Article: Prehospital Use of Cervical Collars. 2020, pp. 1–6. Available online: https://www.hmpgloballearningnetwork.com/site/EMSWorld/1223899/ce-article-prehospital-use-cervical-collars (accessed on 20 November 2021).
- Wampler, D.; Eastridge, B.; Summers, R.; Love, P.; Dharia, A.; Seifi, A. Impact of Cervical Collar and Patient Position on the Cerebral Blood Flow. J. Neurol Res. 2020, 10, 177–182. [Google Scholar] [CrossRef]
- Nunez-Patino, R.A.; Rubiano, A.M.; Godoy, D.A. Impact of cervical collars on intracranial pressure values in traumatic brain injury: A systematic review and meta-analysis of prospective studies. Neurocrit. Care 2020, 32, 469–477. [Google Scholar] [CrossRef]
- Stuke, L.E.; Pons, P.T.; Guy, J.S.; Chapleau, W.P.; Butler, F.K.; McSwain, N.E. Prehospital spine immobilization for penetrating trauma—review and recommendations from the Prehospital Trauma Life Support Executive Committee. J. Trauma Acute Care Surg. 2011, 71, 763–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Hastings, C.; Fisher, C.A. Searching for proof: Creating and using an actionable PICO question. Nurs. Manag. 2014, 45, 9–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, N.; Phillips, M. Rayyan for systematic reviews. J. Electron. Resour. Librariansh. 2018, 30, 46–48. [Google Scholar] [CrossRef] [Green Version]
- Peterson, J.; Welch, V.; Losos, M.; Tugwell, P.J. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2011; pp. 1–2. [Google Scholar]
- Davies, G.; Deakin, C.; Wilson, A. The effect of a rigid collar on intracranial pressure. Injury 1996, 27, 647–649. [Google Scholar] [CrossRef]
- Hunt, K.; Hallworth, S.; Smith, M. The effects of rigid collar placement on intracranial and cerebral perfusion pressures. Anaesthesia 2001, 56, 511–513. [Google Scholar] [CrossRef]
- Kuhnigk, H.; Bomke, S.; Sefrin, P. Effect of external cervical spine immobilization on intracranial pressure. Aktuelle Traumatol. 1993, 23, 350–353. [Google Scholar]
- Porter, K.M.; Allison, K. Semirigid cervical collar and intracranial pressure: A change in pre-hospital emphasis might be indicated. Prehosp. Emerg. Care 1999, 3, 226228. [Google Scholar]
- Craig, G.R.; Nielsen, M.S. Rigid cervical collars and intracranial pressure. Intensive Care Med. 1991, 17, 504–505. [Google Scholar] [CrossRef] [PubMed]
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.L.; Clement, C.M.; Lesiuk, H.; De Maio, V.J.; Laupacis, A.; Schull, M.; McKnight, R.D.; Verbeek, R.; et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001, 286, 1841–1848. [Google Scholar] [CrossRef] [PubMed]
- Hasler, R.M.; Exadaktylos, A.K.; Bouamra, O.; Benneker, L.M.; Clancy, M.; Sieber, R.; Zimmermann, H.; Lecky, F. Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur. Spine J. 2011, 20, 2174–2180. [Google Scholar] [CrossRef] [Green Version]
- Stanton, D.; Hardcastle, T.; Muhlbauer, D.; van Zyl, D. Cervical collars and immobilisation: A South African best practice recommendation. Afr. J. Emerg. Med. 2017, 7, 4–8. [Google Scholar] [CrossRef]
- Horodyski, M.; DiPaola, C.P.; Conrad, B.P.; Rechtine, G.R., II. Cervical collars are insufficient for immobilizing an unstable cervical spine injury. J. Emerg. Med. 2011, 41, 513–519. [Google Scholar] [CrossRef]
- Stocchetti, N.; Carbonara, M.; Citerio, G.; Ercole, A.; Skrifvars, M.; Smielewski, P.; Zoerle, T.; Menon, D. Severe traumatic brain Injury: Targeted management in the intensive care unit. Lancet Neurol. 2017, 16, 452–464. [Google Scholar] [CrossRef] [Green Version]
- Bero, L.; Rennie, D. The Cochrane Collaboration. Preparing, maintaining, and disseminating systematic reviews of the effects of health care. JAMA 1995, 274, 1935–1938. [Google Scholar] [CrossRef]
- Wilson, M. Monro-Kellie 2.0: The dynamic vascular and venous pathophysiological components of intracranial pressure. J. Cereb. Blood Flow Metab. 2016, 36, 1338–1350. [Google Scholar]
- Stone, M.; Tubridy, C.; Curran, R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad. Emerg. Med. 2010, 17, 100–102. [Google Scholar] [CrossRef]
- Godoy, A.D.; Núñez-Patiño, R.A.; Zorrilla-Vaca, A.; Ziai, W.C.; Hemphill, J.C. Intracranial hypertension after spontaneous intracerebral hemorrhage: A systematic review and meta-analysis of prevalence and mortality rate. Neurocrit. Care 2019, 31, 176–187. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Authors | Year | Study Design | Country | Sample Size | Intervention | GRADE Quality | ICP Measurement Device | Findings |
|---|---|---|---|---|---|---|---|---|
| Mobbs et al. [10] | 2002 | A prospective, observational study | Australia | 10 | Laerdal Stifneck collars | Moderate | Medtronic, external ventricular drain, Camino (invasive) | Increase in ICP (mean rise of 4.4 mmHg) following application of the collar. |
| Davies et al. [20] | 1996 | A prospective, observational study | UK | 19 | Laerdal Stifneck collars | Moderate | Camino microventricular catheter (invasive) | Increase in ICP (mean rise of 4.5 mmHg) following application of the collar. |
| Hunt et al. [21] | 2001 | A prospective, observational study | UK | 30 | Laerdal Stifneck collars | Moderate | Codman microsensor (invasive) | Increase in ICP (mean rise of 4.6 mmHg) following application of the collar. |
| Authors | Year | Study Design | Country | Sample Size | Intervention | GRADE Quality | ICP measurement Device | Findings |
|---|---|---|---|---|---|---|---|---|
| Kuhnigk et al. [22] | 1993 | A prospective observational study | Germany | 18 | Speith (n = 12) and Philadelphia cervical collars (n = 6) | Moderate | Epidural transducer (invasive) | No significant change in ICP. |
| Porter et al. [23] | 1993 | A prospective observational study | UK | 9 | * Cervical collar | Not assessed | N/A | Increase in ICP (mean rise of 9.9 mmHg) following application of the collar. |
| Craig and Nielsen [24] | 1991 | Case report | UK | 2 | Laerdal Stifnek collars | Low | ICP monitor (invasive) § | Increase in ICP (18 mmHg and 15 mmHg) following application of the collar. |
| Study | Before Application | During Application | After Removal | Time of Collar Application (min) |
|---|---|---|---|---|
| Mobbs et al. [10] | 20.5 ± 14.2 | 25.8 ± 11.5 | NR | 3–5 |
| Davies et al. [20] | 13.7 ± 5.7 | 18.3 ± 7.3 | 14.4 ± 6.0 | 20 |
| Hunt et al. [21] | 14.1 ± 6.6 | 18.8 ± 8.4 | 14.3 ± 6.6 | 5 |
| Study | Before Application | During Application | After Removal | Time of Collar Application (min) |
|---|---|---|---|---|
| Kuhnigk et al. [22] | 17.0 ± 6.1 | 17.7 ± 6.7 | 17.2 ± 5.9 | 10 |
| Porter et al. [23] | 12.8 (range 6–19) | 22.7 (range 24–36) | NR | 5 * |
| Craig and Nielson [24] | 14 10 | 32 25 | 14 10 | 15 12 |
| Newcastle–Ottawa Scale Results | ||||
|---|---|---|---|---|
| Reference | Selection (4) | Comparability (2) | Outcome (3) | Total (9) |
| Mobbs et al. [10] | 2 | 2 | 3 | 7 |
| Davies et al. [20] | 3 | 2 | 3 | 8 |
| Hunt et al. [21] | 2 | 2 | 3 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bazaie, N.; Alghamdi, I.; Alqurashi, N.; Ahmed, Z. The Impact of a Cervical Collar on Intracranial Pressure in Traumatic Brain Injury Patients: A Systematic Review and Meta-Analysis. Trauma Care 2022, 2, 1-10. https://doi.org/10.3390/traumacare2010001
Bazaie N, Alghamdi I, Alqurashi N, Ahmed Z. The Impact of a Cervical Collar on Intracranial Pressure in Traumatic Brain Injury Patients: A Systematic Review and Meta-Analysis. Trauma Care. 2022; 2(1):1-10. https://doi.org/10.3390/traumacare2010001
Chicago/Turabian StyleBazaie, Naif, Ibrahim Alghamdi, Naif Alqurashi, and Zubair Ahmed. 2022. "The Impact of a Cervical Collar on Intracranial Pressure in Traumatic Brain Injury Patients: A Systematic Review and Meta-Analysis" Trauma Care 2, no. 1: 1-10. https://doi.org/10.3390/traumacare2010001
APA StyleBazaie, N., Alghamdi, I., Alqurashi, N., & Ahmed, Z. (2022). The Impact of a Cervical Collar on Intracranial Pressure in Traumatic Brain Injury Patients: A Systematic Review and Meta-Analysis. Trauma Care, 2(1), 1-10. https://doi.org/10.3390/traumacare2010001







