Association of Unhealthy Behaviors with Self-Harm in Chinese Adolescents: A Study Using Latent Class Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Design of Questionnaires
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Self-Harm
3.2. Latent Class Analysis of Unhealthy Behaviors
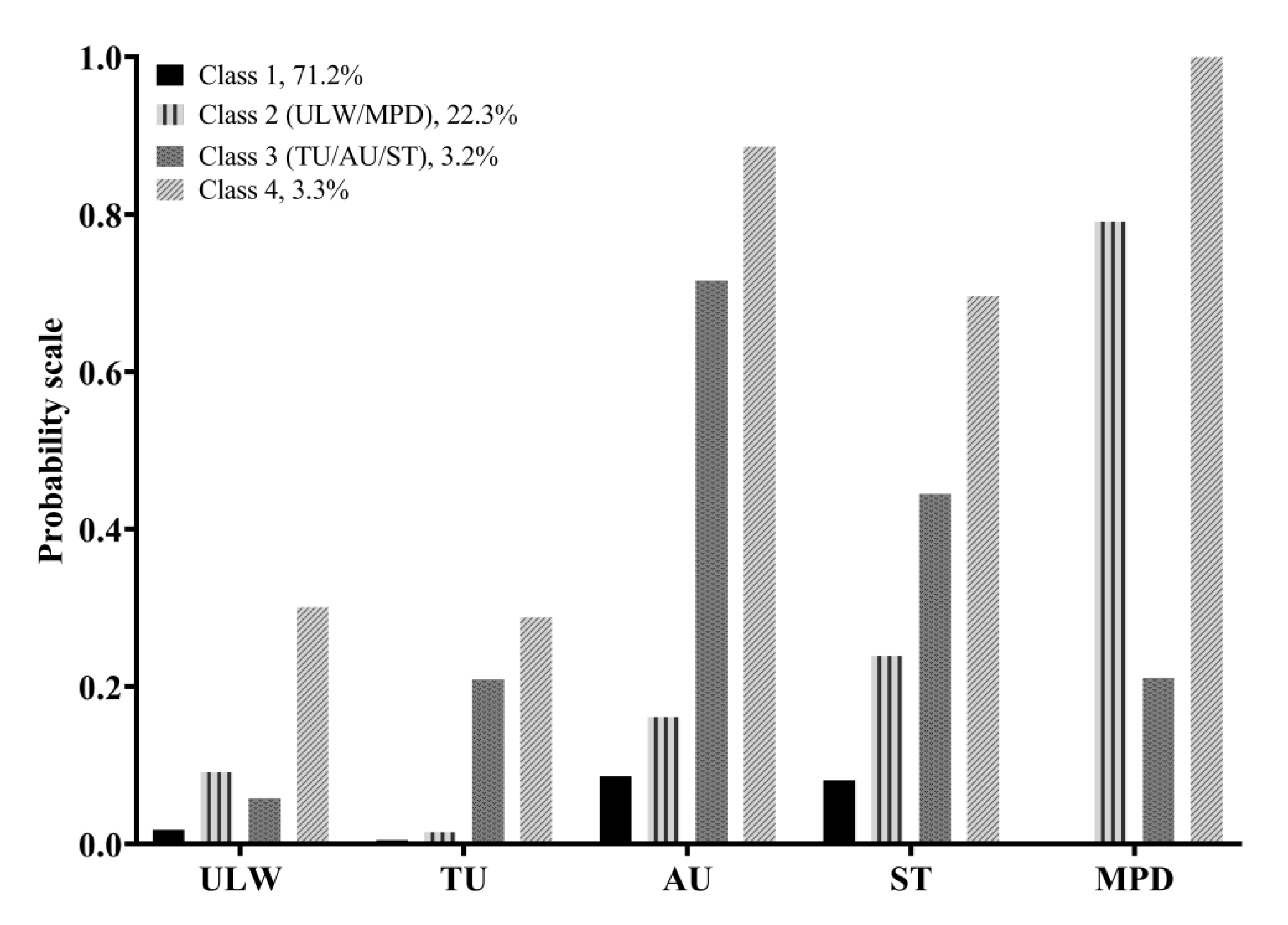
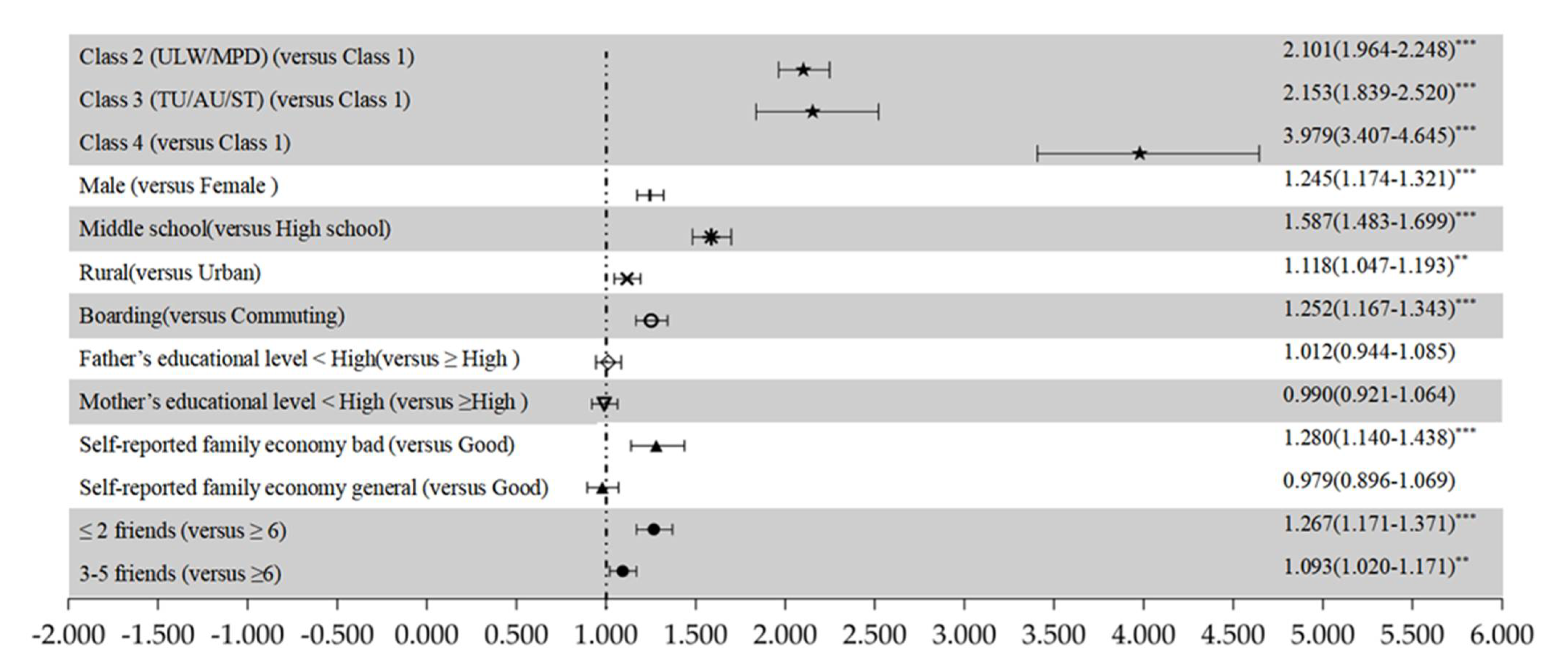
3.3. Multivariate Logistic Regression Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Measures |
| Self-harm | Adolescent Non-suicidal Self-injury Assessment Questionnaire |
| Unhealthy weight loss | During the past 30 days, have you taken any diet pills or diet tea to lose weight? |
| Tobacco use | During the past 30 days, how many days did you smoke cigarettes? |
| Alcohol use | During the past 30 days, on how many days did you have at least one drink of alcohol? |
| Screen time | The average hours on weekdays spent playing games or doing things unrelated to study on the computer every day. |
| Mobile phone dependence | Self-rating Questionnaire for Adolescent Problematic Mobile Phone Use |
References
- Favazza, A.R. Bodies under Siege: Self-Mutilation and Body Modification in Culture and Psychiatry, 2nd ed.; Johns Hopkins: London, UK, 1996. [Google Scholar]
- Guan, K.; Fox, K.R.; Prinstein, M.J. Nonsuicidal self-injury as a time-invariant predictor of adolescent suicide ideation and attempts in a diverse community sample. J. Consult. Clin. Psychol. 2012, 80, 842–849. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association Press: Washington, DC, USA, 2000. [Google Scholar]
- Swannell, S.V.; Martin, G.; Page, A.; Hasking, P.; John, N.J.S. Prevalence of Nonsuicidal Self-Injury in Nonclinical Samples: Systematic Review, Meta-Analysis and Meta-Regression. Suicide Life-Threat. Behav. 2014, 44, 273–303. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.; Yao, Y. Prevalence of nonsuicidal self-injury in chinese middle school and high school students. Medicine 2018, 97, e12916. [Google Scholar] [CrossRef]
- Hawton, K.; Saunders, K.E.A.; O’Connor, R.C. Self-harm and suicide in adolescents. Lancet 2012, 379, 2373–2382. [Google Scholar] [CrossRef]
- World Health Organization. Health Promotion Glossary; World Health Organization: Geneva, Switzerland, 1998; Available online: https://www.who.int/healthpromotion/about/HPR%20Glossary%201998.pdf?ua (accessed on 31 August 2020).
- Ji, C.Y. Adolescent health risk behavior monitoring: An important frontier of school health work. Chin. J. Sch. Health 2009, 30, 99–105, (In Chinese with English abstract). [Google Scholar]
- Li, D.; Yang, R.; Wan, Y.; Tao, F.; Fang, J.; Zhang, S. Interaction of health literacy and Problematic Mobile Phone Use and Their Impact on Non-Suicidal Self-Injury among Chinese Adolescents. Int. J. Environ. Res. Public Health 2019, 16, 2366. [Google Scholar] [CrossRef] [Green Version]
- Throuvala, M.A.; Griffiths, M.D.; Rennoldson, M.; Kuss, D.J. School-based Prevention for Adolescent Internet Addiction: Prevention is the Key. A Systematic Literature Review. Curr. Neuropharmacol. 2019, 17, 507–525. [Google Scholar] [CrossRef]
- Mayne, S.L.; Virudachalam, S.; Fiks, A.G. Clustering of unhealthy behaviors in a nationally representative sample of U.S. children and adolescents. Prev. Med. 2020, 130, 105892. [Google Scholar] [CrossRef]
- Wu, J.; Liu, H. Features of Nonsuicidal Self-Injury and Relationships with Coping Methods among College Students. Iran. J. Public Health 2019, 48, 270–277. [Google Scholar] [CrossRef]
- Martiniuk, A.; Chen, H.-Y.; Glozier, N.; Patton, G.; Senserrick, T.; Williamson, A.; Woodward, M.; Ivers, R. High alcohol use a strong and significant risk factor for repetitive self-harm in female and male youth: A prospective cohort study. Am. J. Drug Alcohol Abus. 2015, 41, 465–473. [Google Scholar] [CrossRef]
- Nagata, J.M.; Garber, A.K.; Tabler, J.; Murray, S.B.; Bibbins-Domingo, K. Differential Risk Factors for Unhealthy Weight Control Behaviors by Sex and Weight Status Among, U.S. Adolescents. J. Adolesc. Health 2018, 63, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Tuisku, V.; Pelkonen, M.; Kiviruusu, O.; Karlsson, L.; Marttunen, M. Alcohol use and psychiatric comorbid disorders predict deliberate self-harm behaviour and other suicidality among depressed adolescent outpatients in 1-year follow-up. Nord. J. Psychiatry 2011, 66, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Tozzi, F.; Thornton, L.M.; Mitchell, J.; Fichter, M.M.; Klump, K.L.; Lilenfeld, L.R.; Reba, L.; Strober, M.; Kaye, W.H.; Bulik, C.M. Features Associated With Laxative Abuse in Individuals With Eating Disorders. Psychosom. Med. 2006, 68, 470–477. [Google Scholar] [CrossRef]
- Çimen, İ.D.; Coşkun, A.; Etiler, N. Non-suicidal self-injury behaviors’ features and relationship with adolescents’ daily life activities and mental status. Turk. J. Pediatrics 2017, 59, 113–121. [Google Scholar] [CrossRef] [Green Version]
- Fu, J.L.; Wan, Y.H.; Sun, Y.; Tao, S.M.; Zu, P.; An, J.; Wang, X.; Tao, F.B. Relation of screen time and psychological sub-health to self-harm behavior in adolescents. Chin. Ment. Health J. 2013, 27, 468–472, (In Chinese with English abstract). [Google Scholar] [CrossRef]
- Choi, S.H.; Duffy, S.A. Analysis of health behavior theories for clustering of health behaviors. J. Addict. Nurs. 2017, 28, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Krokstad, S.; Ding, D.; Grunseit, A.C.; Sund, E.R.; Holmen, T.L.; Rangul, V.; Bauman, A. Multiple lifestyle behaviours and mortality, findings from a large population-based Norwegian cohort study—The HUNT Study. BMC Public Health 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prochaska, J.J.; Prochaska, J.O. A review of multiple health behavior change interventions for primary prevention. Am. J. Lifestyle Med. 2011, 5, 208–221. [Google Scholar] [CrossRef]
- Loef, M.; Walach, H. The combined effects of healthy lifestyle behaviors on all cause mortality: A systematic review and meta-analysis. Prev. Med. 2012, 55, 163–170. [Google Scholar] [CrossRef]
- Ye, Y.-L.; Wang, P.-G.; Qu, G.-C.; Yuan, S.; Phongsavan, P.; He, Q.-Q. Associations between multiple health risk behaviors and mental health among Chinese college students. Psychol. Health Med. 2015, 21, 377–385. [Google Scholar] [CrossRef]
- Dodd, L.J.; Al-Nakeeb, Y.; Nevill, A.; Forshaw, M.J. Lifestyle risk factors of students: A cluster analytical approach. Prev. Med. 2010, 51, 73–77. [Google Scholar] [CrossRef]
- Kwan, M.; Arbour-Nicitopoulos, K.P.; Duku, E.; Faulkner, G. Patterns of multiple health risk–behaviours in university students and their association with mental health: Application of latent class analysis. Health Promot. Chronic Dis. Prev. Can. 2016, 36, 163–170. [Google Scholar] [CrossRef] [Green Version]
- Hagenaars, J.A. Applied Latent Class Analysis; McCutcheons, A.L., Ed.; Cambridge University Press: Cambridge, UK, 2002. [Google Scholar]
- Jessor, R. Risk behavior in adolescence: A psychosocial framework for understanding and action. J. Adolesc. Health 1991, 12, 597–605. [Google Scholar] [CrossRef]
- Elwood, M. Critical Appraisal of Epidemiological Studies and Clinical Trials; Oxford University Press: New York, NY, USA, 2007. [Google Scholar]
- Lv, J.; He, P.P.; Tu, W.X.; Li, L.M. Estimation of sampling error on data from cluster sample survey. Zhonghua Liu Xing Bing Xue Za Zhi 2008, 29, 78–80. [Google Scholar]
- Wan, Y.H.; Liu, W.; Hao, J.H.; Tao, F.B. Development and evaluation on reliability and validity of adolescent non-suicidal self-injury assessment questionnaire. Chin. J. Sch. Health 2018, 39, 170–173, (In Chinese with English abstract). [Google Scholar] [CrossRef]
- Kann, L.; McManus, T.; Harris, W.A.; Shanklin, S.L.; Flint, K.H.; Queen, B.; Lowry, R.; Chyen, D.; Whittle, L.; Thornton, J.; et al. Youth Risk Behavior Surveillance—United States, 2017. MMWR Surveill. Summ. 2018, 67, 1–114. [Google Scholar] [CrossRef] [PubMed]
- Eaton, D.K.; Kann, L.; Kinchen, S.; Shanklin, S.; Ross, J.; Hawkins, J.; Harris, W.A.; Lowry, R.; McManus, T.; Chyen, D.; et al. Youth risk behavior surveillanc, United States, 2009. MMWR Surveill. Summ. 2010, 59, 1–142. [Google Scholar] [PubMed]
- Brener, N.D.; Billy, J.O.; Grady, W.R. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. J. Adolesc. Health 2003, 33, 436–457. [Google Scholar] [CrossRef] [Green Version]
- American Academy of Pediatries. Committee on public education. American Academy of Pediatrics: Children, adolescents, and television. Pediatrics 2001, 107, 423–426. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.; Tao, S.; Zhang, Y.; Zhang, S.; Tao, F. Low Physical Activity and High Screen Time Can Increase the Risks of Mental Health Problems and Poor Sleep Quality among Chinese College Students. PLoS ONE 2015, 10, e0119607. [Google Scholar] [CrossRef] [Green Version]
- Cao, H.; Qian, Q.; Weng, T.; Yuan, C.; Sun, Y.; Wang, H.; Tao, F. Screen time, physical activity and mental health among urban adolescents in China. Prev. Med. 2011, 53, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.M.; Fu, J.L.; Wang, H.; Hao, J.H.; Tao, F.B. Development of self-rating questionnaire for adolescent problematic mobile phone use and the psychometric evaluation in undergraduates. Chin. J. Sch. Health 2013, 34, 26–29, (In Chinese with English abstract). [Google Scholar] [CrossRef]
- Tao, S.; Wu, X.; Zhang, Y.; Zhang, S.; Tong, S.; Tao, F. Effects of sleep quality on the association between problematic mobile phone use and mental health symptoms in Chinese college students. Int. J. Environ. Res. Public Health 2017, 14, 185. [Google Scholar] [CrossRef] [Green Version]
- Tao, S.; Wu, X.; Wan, Y.; Zhang, S.; Hao, J.; Tao, F. Interactions of problematic mobile phone use and psychopathological symptoms with unintentional injuries: A school-based sample of Chinese adolescents. BMC Public Health 2015, 16, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2012; Available online: https://www.statmodel.com/download/usersguide/Mplus%20user%20guide%20Ver_7_r3_web.pdf (accessed on 15 March 2021).
- Carragher, N.; Adamson, G.; Bunting, B.; McCann, S. Subtypes of depression in a nationally representative sample. J. Affect. Disord. 2009, 113, 88–99. [Google Scholar] [CrossRef]
- Nagin, D. Group-Based Modeling of Development; Harvard University Press: London, UK, 2005. [Google Scholar]
- Lim, K.-S.; Wong, C.H.; McIntyre, R.S.; Wang, J.; Zhang, Z.; Tran, B.X.; Tan, W.; Ho, C.S.; Ho, R.C. Global Lifetime and 12-Month Prevalence of Suicidal Behavior, Deliberate Self-Harm and Non-Suicidal Self-Injury in Children and Adolescents between 1989 and 2018: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4581. [Google Scholar] [CrossRef] [Green Version]
- Kidger, J.; Heron, J.; Lewis, G.; Evans, J.; Gunnell, D. Adolescent self-harm and suicidal thoughts in the ALSPAC cohort: A self-report survey in England. BMC Psychiatry 2012, 12, 69. [Google Scholar] [CrossRef] [Green Version]
- Chan, S.; Denny, S.; Fleming, T.; Fortune, S.; Peiris-John, R.; Dyson, B. Exposure to suicide behaviour and individual risk of self-harm: Findings from a nationally representative New Zealand high school survey. Aust. New Zealand J. Psychiatry 2017, 52, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Ceylan, M.F.; Hesapcioglu, S.T.; Kasak, M.; Yavas, C.P. High prevalence of nonsuicidal self-injury, tattoos, and psychiatric comorbidity among male adolescent prisoners and their sociodemographic characteristics. Asian J. Psychiatry 2019, 43, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Ömer, B.; Bildik, T.; Kabukçu-Başay, B.; Güngör, D.; Başay, Ö.; Farmer, R.F. Prevalence of non-suicidal self-injury and distinct groups of self-injurers in a community sample of adolescents. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1163–1171. [Google Scholar] [CrossRef]
- Tørmoen, A.J.; Myhre, M.; Walby, F.A.; Grøholt, B.; Rossow, I. Change in prevalence of self-harm from 2002 to 2018 among Norwegian adolescents. Eur. J. Public. Health 2020, 30, 688–692. [Google Scholar] [CrossRef]
- Barrocas, A.L.; Giletta, M.; Hankin, B.L.; Prinstein, M.; Abela, J.R.Z. Nonsuicidal Self-Injury in Adolescence: Longitudinal Course, Trajectories, and Intrapersonal Predictors. J. Abnorm. Child Psychol. 2014, 43, 369–380. [Google Scholar] [CrossRef]
- Whitlock, J.; Muehlenkamp, J.; Purington, A.; Eckenrode, J.; Barreira, P.; Abrams, G.B.; Marchell, T.; Kress, V.; Girard, K.; Chin, C.; et al. Nonsuicidal Self-injury in a College Population: General Trends and Sex Differences. J. Am. Coll. Health 2011, 59, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K. Self-Injury. Annu. Rev. Clin. Psychol. 2010, 6, 339–363. [Google Scholar] [CrossRef]
- Wan, Y.H.; Hu, C.-L.; Hao, J.-H.; Sun, Y.; Tao, F.-B. Deliberate self-harm behaviors in Chinese adolescents and young adults. Eur. Child Adolesc. Psychiatry 2011, 20, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, L.; Albert, D.; Cauffman, E.; Banich, M.; Graham, S.; Woolard, J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Dev. Psychol. 2008, 44, 1764–1778. [Google Scholar] [CrossRef] [Green Version]
- Markus, H.R.; Kitayama, S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol. Rev. 1991, 98, 224–253. [Google Scholar] [CrossRef]
- Meader, N.; King, K.; Moe-Byrne, T.; Wright, K.; Graham, H.; Petticrew, M.; Power, C.; White, M.; Sowden, A.J. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 2016, 16, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, J.; Agley, J.; Hendryx, M.; Gassman, R.; Lohrmann, D. Risk Patterns Among College Youth. Health Promot. Pract. 2014, 16, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Stephen, E.M.; Rose, J.S.; Kenney, L.; Rosselli-Navarra, F.; Weissman, R.S. Prevalence and correlates of unhealthy weight control behaviors: Findings from the national longitudinal study of adolescent health. J. Eat. Disord. 2014, 2, 16. [Google Scholar] [CrossRef] [Green Version]
- Neumark-Sztainer, D.; Story, M.; French, S.A. Covariations of Unhealthy Weight Loss Behaviors and Other High-Risk Behaviors Among Adolescents. Arch. Pediatrics Adolesc. Med. 1996, 150, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Herpertz, S.C.; Mueller, B.; Qunaibi, M.; Lichterfeld, C.; Konrad, K.; Herpertz-Dahlmann, B. Response to Emotional Stimuli in Boys With Conduct Disorder. Am. J. Psychiatry 2005, 162, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- You, J.; Leung, F. The role of depressive symptoms, family invalidation and behavioral impulsivity in the occurrence and repetition of non-suicidal self-injury in Chinese adolescents: A 2-year follow-up study. J. Adolesc. 2012, 35, 389–395. [Google Scholar] [CrossRef]
- Spring, B.J.; Doran, N.; Pagoto, S.L.; Schneider, K.L.; Pingitore, R.; Hedeker, D. Randomized Controlled Trial for Behavioral Smoking and Weight Control Treatment: Effect of Concurrent Versus Sequential Intervention. J. Consult. Clin. Psychol. 2004, 72, 785–796. [Google Scholar] [CrossRef] [Green Version]
- Joseph, A.M.; Willenbring, M.L.; Nugent, S.M.; Nelson, D.B. A randomized trial of concurrent versus delayed smoking intervention for patients in alcohol dependence treatment. J. Stud. Alcohol. 2004, 65, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Vandelanotte, C.; De Bourdeaudhuij, I.; Sallis, J.F.; Spittaels, H.; Brug, J. Efficacy of sequential or simultaneous interactive computer-tailored interventions for increasing physical activity and decreasing fat intake. Ann. Behav. Med. 2005, 29, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Hyman, D.J.; Pavlik, V.N.; Taylor, W.C.; Goodrick, G.K.; Moye, L. Simultaneous vs Sequential Counseling for Multiple Behavior Change. Arch. Intern. Med. 2007, 167, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Edington, D.W. Emerging research: A view from one research center. Am. J. Health Promot. 2001, 15, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Adlaf, E.M.; Demers, A.; Gliksman, L. Canadian Campus Survey 2004; Centre for Addiction and Mental Health: Toronto, ON, Canada, 2005. [Google Scholar]
| Variable | Hit | Pull Hair | Bang Head | Pinch or Scratch | Bit | Cut | Fire | Toxic Substance | Total |
|---|---|---|---|---|---|---|---|---|---|
| Gender | |||||||||
| Male | 1687 (15.4) | 1558 (14.2) | 2876 (26.2) | 1060 (9.6) | 636 (5.8) | 555 (5.1) | 562 (5.1) | 203 (1.8) | 3871 (35.2) |
| Female | 1516 (13.0) | 1064 (9.1) | 1634 (14.0) | 1650 (14.2) | 948 (8.1) | 796 (6.8) | 374 (3.2) | 93 (0.8) | 3390 (29.1) |
| χ2 | 25.124 | 139.819 | 521.060 | 110.153 | 48.302 | 32.246 | 51.465 | 40.089 | 96.332 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Grade | |||||||||
| Middle school | 1888 (15.7) | 1557 (13.0) | 2516 (21.0) | 1609 (13.4) | 962 (8.0) | 864 (7.2) | 456 (3.8) | 192 (1.6) | 4132 (34.5) |
| High school | 1315 (12.4) | 1065 (10.0) | 1994 (18.7) | 1101 (10.4) | 622 (5.8) | 487 (4.6) | 480 (4.5) | 104 (1.0) | 3129 (29.4) |
| χ2 | 52.921 | 48.482 | 17.556 | 50.182 | 40.873 | 69.183 | 7.189 | 16.948 | 65.487 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.007 | <0.001 | <0.001 |
| Registered residence | |||||||||
| Rural | 1629 (15.0) | 1372 (12.6) | 2264 (20.8) | 1385 (12.7) | 847 (7.8) | 660 (6.1) | 486 (4.5) | 149 (1.4) | 3672 (33.7) |
| Urban | 1574 (13.4) | 1250 (10.6) | 2246 (19.1) | 1325 (11.3) | 737 (6.3) | 691 (5.9) | 450 (3.8) | 147 (1.3) | 3589 (30.6) |
| χ2 | 11.449 | 21.313 | 10.033 | 11.219 | 19.758 | 0.334 | 5.744 | 0.607 | 26.357 |
| p | 0.001 | <0.001 | 0.002 | 0.001 | <0.001 | 0.563 | 0.017 | 0.436 | <0.001 |
| Accommodation type | |||||||||
| Boarding student | 1660 (14.7) | 1353 (12.0) | 2340 (20.7) | 1428 (12.6) | 791 (7.0) | 596 (5.3) | 486 (4.3) | 132 (1.2) | 3725 (32.9) |
| Commuting student | 1543 (13.6) | 1269 (11.2) | 2170 (19.2) | 1282 (11.3) | 793 (7.0) | 755 (6.7) | 450 (4.0) | 164 (1.5) | 3536 (31.3) |
| χ2 | 4.835 | 2.944 | 7.779 | 8.761 | 0.005 | 20.081 | 1.405 | 3.540 | 6.952 |
| p | 0.028 | 0.086 | 0.005 | 0.003 | 0.941 | <0.001 | 0.236 | 0.060 | 0.008 |
| Father’s educational level a | |||||||||
| <High school degree | 1836 (14.1) | 1539 (11.8) | 2665 (20.5) | 1558 (12.0) | 926 (7.1) | 752 (5.8) | 522 (4.0) | 159 (1.2) | 4271 (32.8) |
| ≥High school degree | 1324 (14.0) | 1052 (11.2) | 1795 (19.0) | 1112 (11.8) | 633 (6.7) | 572 (6.1) | 389 (4.1) | 125 (1.3) | 2918 (31.0) |
| χ2 | 0.020 | 2.401 | 7.147 | 0.168 | 1.372 | 0.814 | 0.183 | 0.472 | 8.823 |
| p | 0.886 | 0.121 | 0.008 | 0.682 | 0.242 | 0.367 | 0.669 | 0.492 | 0.003 |
| Mother’s educational level b | |||||||||
| <High school degree | 2020 (14.1) | 1713 (11.9) | 2909 (20.3) | 1749 (12.2) | 1044 (7.3) | 826 (5.8) | 584 (4.1) | 171 (1.2) | 4696 (32.8) |
| ≥High school degree | 1136 (14.0) | 868 (10.7) | 1544 (19.0) | 933 (11.5) | 516 (6.4) | 498 (6.1) | 335 (4.1) | 115 (1.4) | 2491 (30.7) |
| χ2 | 0.024 | 7.825 | 5.029 | 2.339 | 6.722 | 1.362 | 0.046 | 2.102 | 9.751 |
| p | 0.876 | 0.005 | 0.025 | 0.126 | 0.010 | 0.243 | 0.830 | 0.147 | 0.002 |
| Self-reported family economy | |||||||||
| Bad | 628 (19.4) | 510 (15.7) | 802 (24.8) | 524 (16.2) | 296 (9.1) | 230 (7.1) | 169 (5.2) | 63 (1.9) | 1235 (38.1) |
| General | 2107 (12.9) | 1751 (10.7) | 3054 (18.7) | 1816 (11.1) | 1062 (6.5) | 887 (5.4) | 587 (3.6) | 174 (1.1) | 5029 (30.8) |
| Good | 468 (15.4) | 361 (11.9) | 654 (21.5) | 370 (12.2) | 226 (7.4) | 234 (7.7) | 180 (5.9) | 59 (1.9) | 997 (32.8) |
| χ2 | 98.122 | 66.987 | 67.766 | 65.847 | 29.897 | 31.978 | 46.053 | 27.051 | 67.759 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Number of friends | |||||||||
| ≤2 | 965 (17.5) | 735 (13.3) | 1218 (22.1) | 845 (15.3) | 473 (8.6) | 401 (7.3) | 251 (4.6) | 84 (1.5) | 1954 (35.4) |
| 3–5 | 1278 (13.3) | 1042 (10.8) | 1808 (18.8) | 1099 (11.4) | 656 (6.8) | 517 (5.4) | 352 (3.7) | 96 (1.0) | 2998 (31.2) |
| ≥6 | 960 (12.8) | 845 (11.3) | 1484 (19.8) | 766 (10.2) | 455 (6.1) | 433 (5.8) | 333 (4.4) | 116 (1.5) | 2309 (30.8) |
| χ2 | 67.948 | 22.413 | 23.962 | 83.313 | 31.502 | 23.235 | 9.713 | 12.487 | 37.753 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.008 | 0.002 | <0.001 |
| Statistic | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| df | 11 | 17 | 23 | 29 |
| AIC | 77,820.870 | 77,531.146 | 77,470.028 | 77,473.069 |
| BIC | 77,909.166 | 77667.604 | 77,654.647 | 77,705.851 |
| aBIC | 77,874.209 | 77,613.578 | 77,581.554 | 77,613.690 |
| LMR-LRT | <0.0001 | <0.0001 | <0.0001 | 0.0822 |
| BLRT | <0.0001 | <0.0001 | <0.0001 | 0.1935 |
| Entropy | 0.581 | 0.780 | 0.728 | 0.717 |
| Classification probability | 0.16325 0.83675 | 0.21937 0.06633 0.71429 | 0.03301 0.71208 0.03151 0.22340 | 0.09475 0.01039 0.02417 0.83905 0.03164 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, R.; Li, D.; Tian, R.; Hu, J.; Xue, Y.; Huang, X.; Wan, Y.; Fang, J.; Zhang, S. Association of Unhealthy Behaviors with Self-Harm in Chinese Adolescents: A Study Using Latent Class Analysis. Trauma Care 2021, 1, 75-86. https://doi.org/10.3390/traumacare1020008
Yang R, Li D, Tian R, Hu J, Xue Y, Huang X, Wan Y, Fang J, Zhang S. Association of Unhealthy Behaviors with Self-Harm in Chinese Adolescents: A Study Using Latent Class Analysis. Trauma Care. 2021; 1(2):75-86. https://doi.org/10.3390/traumacare1020008
Chicago/Turabian StyleYang, Rong, Danlin Li, Run Tian, Jie Hu, Yanni Xue, Xuexue Huang, Yuhui Wan, Jun Fang, and Shichen Zhang. 2021. "Association of Unhealthy Behaviors with Self-Harm in Chinese Adolescents: A Study Using Latent Class Analysis" Trauma Care 1, no. 2: 75-86. https://doi.org/10.3390/traumacare1020008
APA StyleYang, R., Li, D., Tian, R., Hu, J., Xue, Y., Huang, X., Wan, Y., Fang, J., & Zhang, S. (2021). Association of Unhealthy Behaviors with Self-Harm in Chinese Adolescents: A Study Using Latent Class Analysis. Trauma Care, 1(2), 75-86. https://doi.org/10.3390/traumacare1020008






