A Comprehensive Review on the Management of COVID-19-Associated Mucormycosis (CAM): The New Basics
Abstract
1. Introduction
2. Epidemiology
3. General Mycology
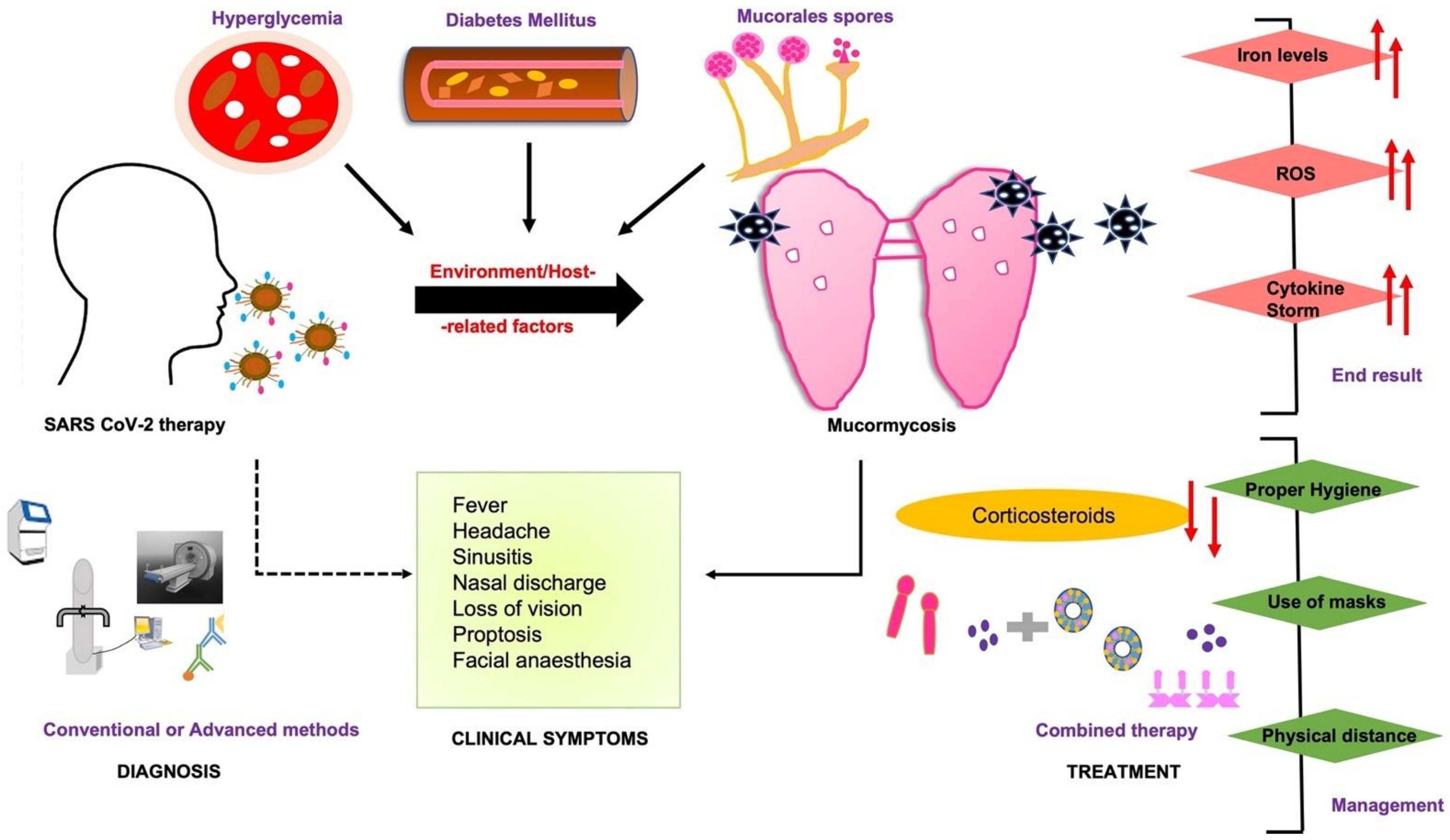
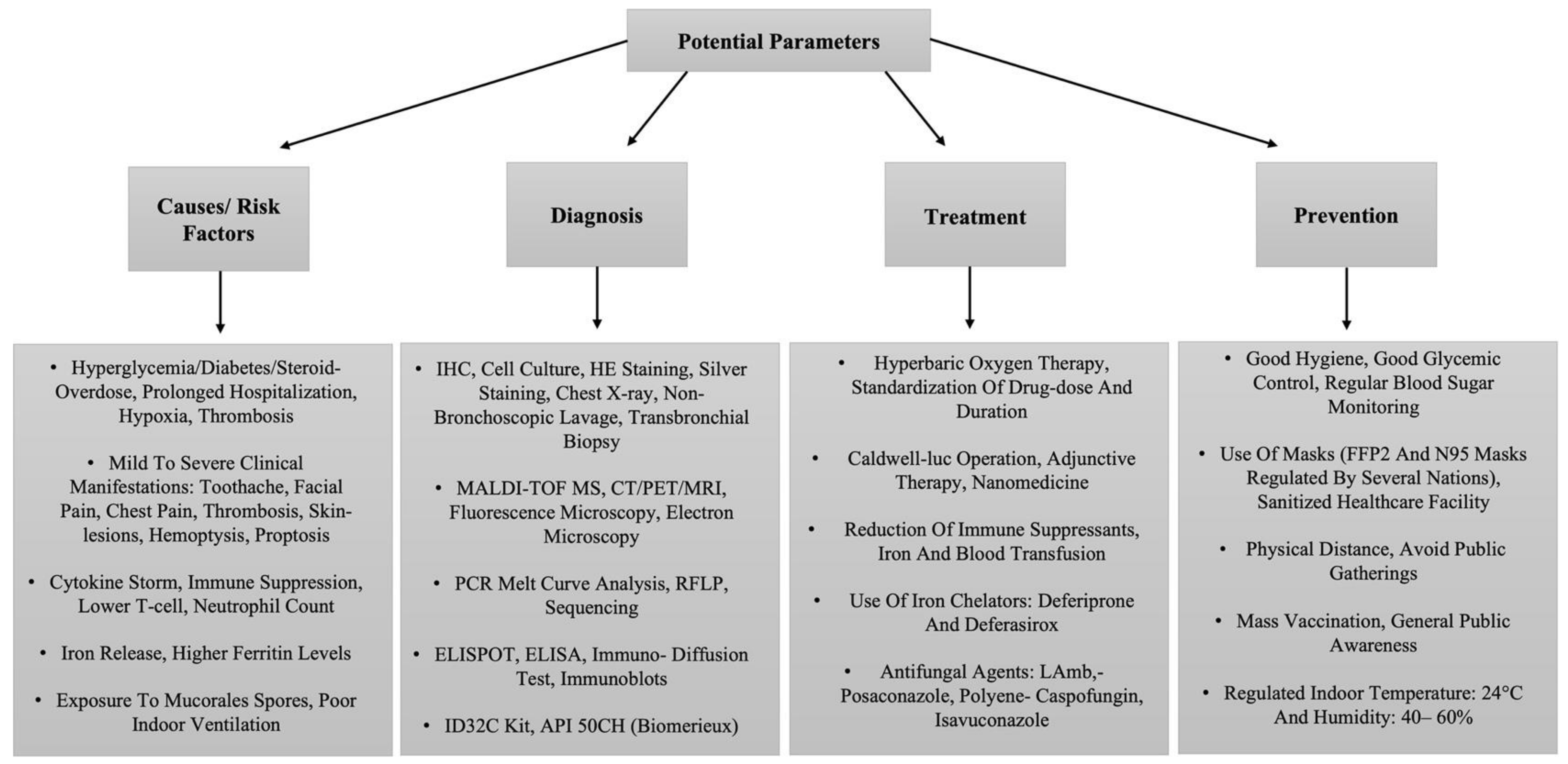
4. Immune System Abnormalities
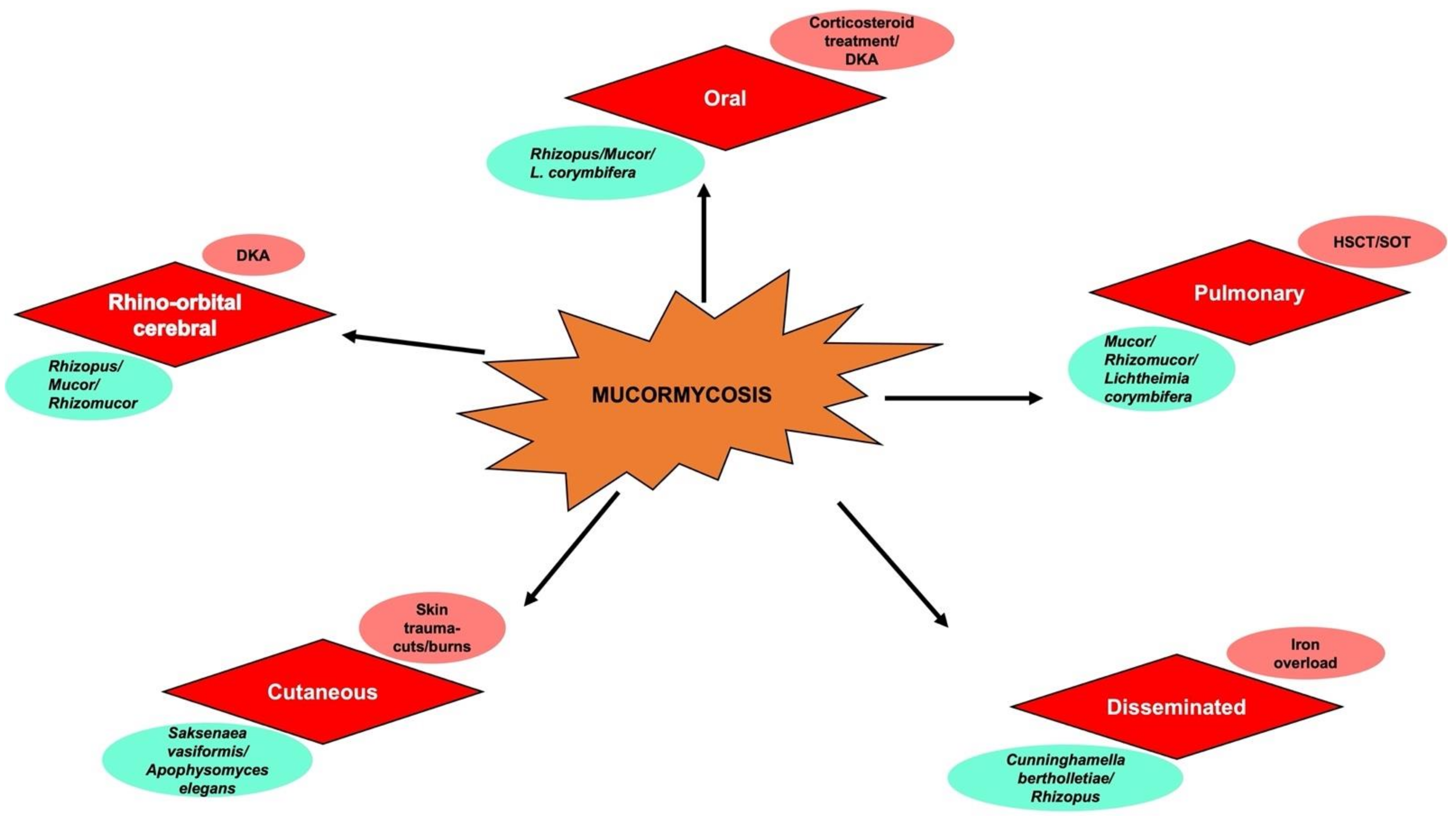
5. Clinical Manifestations
5.1. Rhinocereberal Mucormycosis
5.2. CNS Involvement
5.3. Other Forms of Mucormycosis
5.4. Oral Manifestations: A Dentist’s Perspective
6. Diagnosis
6.1. Microscopic Examination
6.2. Imaging Methods
6.3. Species Identification and Antifungal Susceptibility Testing
6.4. Molecular Assays
6.4.1. Serology Assays
6.4.2. Differential Diagnosis Methods
7. Treatment
7.1. Primary Diagnosis and Prevention
7.2. Antifungal Measures
7.3. Salvage Therapy
7.4. Nanomedicine
8. Link to SARS-CoV-2 Variant
SARS-CoV-2 and Mucormycosis: Underlying Factors
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Richardson, M.; Lass-Flörl, C. Changing epidemiology of systemic fungal infections. Clin. Microbiol. Infect. 2008, 14, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Nagy, E. Changing epidemiology of systemic fungal infections and the possibilities of laboratory diagnostics. Acta Microbiol. Immunol. Hung. 1999, 46, 227–231. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Samaranayake, Y.H.; Samaranayake, L.P. Experimental oral candidiasis in animal models. Clin. Microbiol. Rev. 2001, 14, 398–429. [Google Scholar] [CrossRef] [PubMed]
- Sugar, A.M. Mucormycosis. Clin. Infect. Dis. 1992, 14 (Suppl. 1), S126–S129. [Google Scholar] [CrossRef]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef]
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Y.; Chen, Y.; Qin, Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J. Med. Virol. 2020, 92, 568–576. [Google Scholar] [CrossRef]
- Yang, W.; Cao, Q.; Qin, L.; Wang, X.; Cheng, Z.; Pan, A.; Dai, J.; Sun, Q.; Zhao, F.; Qu, J.; et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): A multi-center study in Wenzhou city, Zhejiang, China. J. Infect. 2020, 80, 388–393. [Google Scholar] [CrossRef]
- Singh, A.K.; Singh, R.; Joshi, S.R.; Misra, A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102146–102146. [Google Scholar] [CrossRef]
- Samson, R.; Dharne, M. COVID-19 associated mucormycosis: Evolving technologies for early and rapid diagnosis. 3 Biotech 2021, 12, 6. [Google Scholar] [CrossRef]
- Skiada, A.; Pavleas, I.; Drogari-Apiranthitou, M. Epidemiology and Diagnosis of Mucormycosis: An Update. J. Fungi 2020, 6, 265. [Google Scholar] [CrossRef] [PubMed]
- Maertens, J.; Demuynck, H.; Verbeken, E.; Zachee, P.; Verhoef, G.; Vandenberghe, P.; Boogaerts, M.A. Mucormycosis in allogeneic bone marrow transplant recipients: Report of five cases and review of the role of iron overload in the pathogenesis. Bone Marrow Transplant. 1999, 24, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Mignogna, M.D.; Fortuna, G.; Leuci, S.; Adamo, D.; Ruoppo, E.; Siano, M.; Mariani, U. Mucormycosis in immunocompetent patients: A case series of patients with maxillary sinus involvement and a critical review of the literature. Int. J. Infect. Dis. 2011, 15, e533–e540. [Google Scholar] [CrossRef] [PubMed]
- Vaezi, A.; Moazeni, M.; Rahimi, M.T.; De Hoog, S.; Badali, H. Mucormycosis in Iran: A systematic review. Mycoses 2016, 59, 402–415. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Zhang, L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Shang, Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Cao, B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef]
- Koehler, P.; Cornely, O.A.; Bottiger, B.W.; Dusse, F.; Eichenauer, D.A.; Fuchs, F.; Shimabukuro-Vornhagen, A. COVID-19 associated pulmonary aspergillosis. Mycoses 2020, 63, 528–534. [Google Scholar] [CrossRef]
- Van Arkel, A.L.E.; Rijpstra, T.A.; Belderbos, H.N.A.; van Wijngaarden, P.; Verweij, P.E.; Bentvelsen, R.G. COVID-19-associated pulmonary aspergillosis. Am. J. Respir. Crit. Care Med. 2020, 202, 132–135. [Google Scholar] [CrossRef]
- Alshahawey, M.G.; El-Housseiny, G.S.; Elsayed, N.S.; Alshahrani, M.Y.; EL Wakeel, L.M.; Aboshanab, K.M. New insights on mucormycosis and its association with the COVID-19 pandemic. Futur. Sci. OA 2022, 8, FSO772. [Google Scholar] [CrossRef] [PubMed]
- Ananthaneni, A.R.; Undavalli, S.B.; Velagapudi, R.P.; Guduru, V.S. Mucormycosis: An atrocious mate of patients with diabetes. BMJ Case Rep. 2013, 2013, bcr2013009600. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Abbo, A.; Bozeman, P.M.; Patrick, C.C. Cunninghamella infections: Review and report of two cases of cunninghamella pneumonia in immunocompromised children. Clin. Infect. Dis. 1993, 17, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Kontoyianis, D.P.; Vartivarian, S.; Anaissie, E.J.; Samonis, G.; Bodey, G.P.; Rinaldi, M. Infections due to cunninghamella bertholletiae in patients with cancer: Report of three cases and review. Clin. Infect. Dis. 1994, 18, 925–928. [Google Scholar] [CrossRef]
- Prakash, H.; Chakrabarti, A. Global Epidemiology of Mucormycosis. J. Fungi 2019, 5, 26. [Google Scholar] [CrossRef]
- Prakash, H.; Chakrabarti, A. Epidemiology of Mucormycosis in India. Microorganisms 2021, 9, 523. [Google Scholar] [CrossRef]
- Hoenigl, M.; Seidel, D.; Carvalho, A.; Rudramurthy, S.M.; Arastehfar, A.; Gangneux, J.-P.; Nasir, N.; Bonifaz, A.; Araiza, J.; Klimko, N.; et al. The emergence of COVID-19 associated mucormycosis: A review of cases from 18 countries. Lancet Microbe 2022, in press. [CrossRef]
- Gil-Lamaignere, C.; Simitsopoulou, M.; Roilides, E.; Maloukou, A.; Winn, R.M.; Walsh, T.J. Interferon- gamma and granulocyte-macrophage colony stimulating factor augment the activity of polymorphonuclear leukocytes against medically important zygomycetes. J. Infect Dis. 2005, 191, 1180–1187. [Google Scholar] [CrossRef]
- Waldorf, A.R. Pulmonary defense mechanisms against opportunistic fungal pathogens. Immunol. Ser. 1989, 47, 243–271. [Google Scholar]
- Dyer, O. COVID-19: Indonesia becomes Asia’s new pandemic epicentre as delta variant spreads. BMJ 2021, 374, n1815. [Google Scholar] [CrossRef]
- Petrikkos, G.; Skiada, A.; Lortholary, O.; Roilides, E.; Walsh, T.J.; Kontoyiannis, D.P. Epidemiology and clinical manifestations of mucormycosis. Clin. Infect. Dis. 2012, 54 (Suppl. 1), S23–S34. [Google Scholar] [CrossRef] [PubMed]
- De Locht, M.; Boelaert, J.R.; Schneider, Y.J. Iron uptake from ferrioxamine and from ferrirhizoferrin by germinating spores of Rhizopus microsporus. Biochem. Pharmacol. 1994, 47, 1843–1850. [Google Scholar] [CrossRef]
- Singh, R.P.; Gupta, N.; Kaur, T.; Gupta, A. Rare case of gastrointestinal mucormycosis with colonic perforation in an immunocompetent patient with COVID-19. BMJ Case Rep. 2021, 14, e244096. [Google Scholar] [CrossRef] [PubMed]
- Chiang, T.-H.; Lee, Y.-W.; Tan, J.-H.; Kao, C.-C.; Chang, C.-C.; Fang, K.-C. Mucormycosis causing massive lower gastrointestinal bleeding: A case report. BMC Gastroenterol. 2021, 21, 272. [Google Scholar] [CrossRef] [PubMed]
- Chikley, A.; Ben-Ami, R.; Kontoyiannis, D.P. Mucormycosis of the Central Nervous System. J. Fungi 2019, 5, 59. [Google Scholar] [CrossRef]
- Ramon, Y.; Oberman, M.; Horowitz, I.; Freedman, A. Extensive maxillary sequestration resulting from rhinocerebral mucormycosis. J. Oral Surg. 1977, 35, 989–991. [Google Scholar]
- Jayachandran, S.; Krithika, C. Mucormycosis presenting as palatal perforation. Indian J. Dent. Res. 2006, 17, 139–142. [Google Scholar] [CrossRef]
- Woo, S.B.; Setterfield, J.F.; Greenberg, M.S. Ulcerative, vesiculous and bullous lesion. In Burket's Oral Medicine, 11th ed.; Greenberg, M.S., Glick, M., Ship, J.A., Eds.; BC Decker Inc.: Hamilton, ON, Canada, 2008; pp. 74–75. [Google Scholar]
- Bonifaz, A.; Macias, B.; Paredes-Farrera, F.; Arias, P.; Ponce, R.; Araiza, J. Palatal zygomycosis: Experience of 21 cases. Oral Dis. 2008, 14, 569–574. [Google Scholar] [CrossRef]
- Cruickshank, G.; Vincent, R.D.; Cherrick, H.M.; Derby, K. Rhinocerebral mucormycosis. J. Am. Dent. Assoc. 1977, 95, 1164–1168. [Google Scholar] [CrossRef]
- Iatta, R.; Napoli, C.; Borghi, E.; Montagna, M.T. Rare mycoses of the oral cavity: A literature epidemiologic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2009, 108, 647–655. [Google Scholar] [CrossRef]
- Tabachnick, T.T.; Levine, B. Mucormycosis of the craniofacial structures. J. Oral. Surg. 1975, 33, 464–469. [Google Scholar]
- Eilderton, T.E. Fatal postextraction cerebral mucormycosis in an unknown diabetic. J. Oral. Surg. 1974, 32, 297–300. [Google Scholar] [PubMed]
- Shetty, S.R.; Punnya, V.A. Palatal mucormycosis: A rare clinical dilemma. Oral. Surg. 2008, 1, 145–148. [Google Scholar] [CrossRef]
- Tugsel, Z.; Sezer, B.; Akalin, T. Facial swelling and palatal ulceration in a diabetic patient. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2004, 98, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Auluck, A. Maxillary necrosis by mucormycosis. a case report and literature review. Med. Oral. Patol. Oral. Cir. Bucal. 2007, 12, E360–E364. [Google Scholar]
- Ahmed, E.; Abou-Bakr, A.; Hussein, R.R.; El-Gawish, A.A.; Ras, A.E.; Ghalwash, D.M. Oral mucormycosis in post-COVID-19 patients: A case series. Oral Dis. 2021. [Google Scholar] [CrossRef]
- Spellberg, B.; Walsh, T.J.; Kontoyiannis, D.P.; Edwards, J.J.; Ibrahim, A.S. Recent Advances in the Management of Mucormycosis: From Bench to Bedside. Clin. Infect. Dis. 2009, 48, 1743–1751. [Google Scholar] [CrossRef]
- Reed, C.; Bryant, R.; Ibrahim, A.S.; Edwards JJr Filler, S.G.; Goldberg, R.; Spellberg, B. Combination polyene caspofungin treatment of rhino-orbital-cerebral mucormycosis. Clin. Infect Dis. 2008, 47, 364–371. [Google Scholar] [CrossRef]
- McDermott, N.E.; Barrett, J.; Hipp, J.; Merino, M.J.; Lee, C.-C.; Waterman, P.; Domingo, D.L.; Walsh, T.J. Successful treatment of periodontal mucormycosis: Report of a case and literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 109, e64–e69. [Google Scholar] [CrossRef]
- Berkow, E.L.; Lockhart, S.R.; Ostrosky-Zeichner, L. Antifungal Susceptibility Testing: Current Approaches. Clin. Microbiol. Rev. 2020, 33, e00069-19. [Google Scholar] [CrossRef]
- Estrem, S.A.; Tully, R.; Davis, W.E. Rhinocerebral mucormycosis: Computed tomographic imaging of cavernous sinus thrombosis. Ann. Otol. Rhinol. Laryngol. 1990, 99, 160–161. [Google Scholar] [CrossRef] [PubMed]
- Lazo, A.; Wilner, H.I.; Metes, J.J. Craniofacial mucormycosis: Computed tomographic and angiographic findings in two cases. Radiology 1981, 139, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Press, G.A.; Weindling, S.M.; Hesselink, J.R.; Ochi, J.W.; Harris, J.P. Rhinocerebral mucormycosis: MR manifestations. J. Comput. Assist. Tomogr. 1988, 12, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Ramani, R.; Gromadzki, S.; Pincus, D.H.; Salkin, I.F.; Chaturvedi, V. Efficacy of API 20C and ID 32C systems for identification of common and rare clinical yeast isolates. J. Clin. Microbiol. 1998, 36, 3396–3398. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, P.; Lortholary, O.; Dromer, F.; Dannaoui, E. Carbon Assimilation Profiles as a Tool for Identification of Zygomycetes. J. Clin. Microbiol. 2007, 45, 1433–1439. [Google Scholar] [CrossRef] [PubMed]
- Schrödl, W.; Heydel, T.; Schwartze, V.U.; Hoffmann, K.; Große-Herrenthey, A.; Walther, G.; Alastruey-Izquierdo, A.; Rodriguez-Tudela, J.L.; Olias, P.; Jacobsen, I.D.; et al. Direct Analysis and Identification of Pathogenic Lichtheimia Species by Matrix-Assisted Laser Desorption Ionization–Time of Flight Analyzer-Mediated Mass Spectrometry. J. Clin. Microbiol. 2012, 50, 419–427. [Google Scholar] [CrossRef]
- Vitale, R.G.; de Hoog, G.S.; Schwarz, P.; Dannaoui, E.; Deng, S.; Machouart, M.; Voigt, K.; van de Sande, W.W.J.; Dolatabadi, S.; Meis, J.F.; et al. Antifungal Susceptibility and Phylogeny of Opportunistic Members of the Order Mucorales. J. Clin. Microbiol. 2012, 50, 66–75. [Google Scholar] [CrossRef]
- Hsiao, C.R.; Huang, L.; Bouchara, J.-P.; Barton, R.; Li, H.C.; Chang, T.C. Identification of medically important molds by an oligonucleotide array. J. Clin. Microbiol. 2005, 43, 3760–3768. [Google Scholar] [CrossRef]
- Larché, J.; Machouart, M.; Burton, K.; Collomb, J.; Biava, M.F.; Gérard, A.; Fortier, B. Diagnosis of cutaneous mucormycosis due to rhizopus microsporus by an innovative PCR-restriction fragment-length polymorphism method. Clin. Infect. Dis. 2005, 41, 1362–1365. [Google Scholar] [CrossRef][Green Version]
- Nyilasi, I.; Papp, T.; Csernetics, A.´.; Krizsa´n, K.; Nagy, E.; Va´gvolgyi, C. Highaffinity iron permease (FTR1) gene sequence-based molecular identification of clinically important Zygomycetes. Clin. Microbiol. Infect. 2008, 14, 393–397. [Google Scholar] [CrossRef]
- Kasai, M.; Harrington, S.M.; Francesconi, A.; Petraitis, V.; Petraitiene, R.; Beveridge, M.G.; Knudsen, T.; Milanovich, J.; Cotton, M.P.; Hughes, J.; et al. Detection of a molecular biomarker for zygomycetes by quantitative pcr assays of plasma, bronchoalveolar lavage, and lung tissue in a rabbit model of experimental pulmonary zygomycosis. J. Clin. Microbiol. 2008, 46, 3690–3702. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, E.; Sutton, D.A.; Cano, J.; Fothergill, A.W.; Stchigel, A.; Rinaldi, M.G.; Guarro, J. Spectrum of zygomycete species identified in clinically significant specimens in the United States. J. Clin. Microbiol. 2009, 47, 1650–1656. [Google Scholar] [CrossRef] [PubMed]
- Lackner, M.; Caramalho, R.; Lass-Florl, C. Laboratory diagnosis of mucormycosis: Current status and future perspectives. Future Microbiol. 2014, 9, 683–695. [Google Scholar] [CrossRef] [PubMed]
- Guinea, J.; Escribano, P.; Vena, A.; Muñoz, P.; Martínez-Jiménez, M.D.C.; Padilla, B.; Bouza, E. Increasing incidence of mucormycosis in a large Spanish hospital from 2007 to 2015: Epidemiology and microbiological characterization of the isolates. PLoS ONE 2017, 12, e0179136. [Google Scholar] [CrossRef] [PubMed]
- Ino, K.; Nakase, K.; Nakamura, A.; Nakamori, Y.; Sugawara, Y.; Miyazaki, K.; Monma, F.; Fujieda, A.; Sugimoto, Y.; Ohishi, K.; et al. Management of Pulmonary Mucormycosis Based on a Polymerase Chain Reaction (PCR) Diagnosis in Patients with Hematologic Malignancies: A Report of Four Cases. Intern. Med. 2017, 56, 707–711. [Google Scholar] [CrossRef]
- Potenza, L.; Vallerini, D.; Barozzi, P.; Riva, G.; Forghieri, F.; Zanetti, E.; Quadrelli, C.; Candoni, A.; Maertens, J.; Rossi, G.; et al. Mucorales-specific T cells emerge in the course of invasive mucormycosis and may be used as a surrogate diagnostic marker in high-risk patients. Blood 2011, 118, 5416–5419. [Google Scholar] [CrossRef]
- Basile, K.; Halliday, C.; Kok, J.; Chen, S.C.-A. Fungal Infections Other Than Invasive Aspergillosis in COVID-19 Patients. J. Fungi 2022, 8, 58. [Google Scholar] [CrossRef]
- Ahmad, S.R.; Ghosh, P. A Systematic Review on Mucormycosis in Corona Patients and its Treatment in India. J. Commun. Dis. 2021, 53, 236–243. [Google Scholar] [CrossRef]
- Christenson, J.C.; Shalit, I.; Welch, D.F.; Guruswamy, A.; Marks, M.I. Synergistic action of amphotericin B and rifampin against Rhizopus species. Antimicrob. Agents Chemother. 1987, 31, 1775–1778. [Google Scholar] [CrossRef][Green Version]
- Ferguson, B.J.; Mitchell, T.G.; Moon, R.E.; Camporesi, E.M.; Farmer, J. Adjunctive hyperbaric oxygen for treatment of rhinocerebral mucormycosis. Clin. Infect. Dis. 1988, 10, 551–559. [Google Scholar] [CrossRef]
- Greenberg, R.N.; Mullane, K.; van Burik, J.-A.H.; Raad, I.; Abzug, M.J.; Anstead, G.; Herbrecht, R.; Langston, A.; Marr, K.A.; Schiller, G.; et al. Posaconazole as Salvage Therapy for Zygomycosis. Antimicrob. Agents Chemother. 2006, 50, 126–133. [Google Scholar] [CrossRef] [PubMed]
- León-Buitimea, A.; Garza-Cervantes, J.A.; Gallegos-Alvarado, D.Y.; Osorio-Concepción, M.; Morones-Ramírez, J.R. Nanomaterial-Based Antifungal Therapies to Combat Fungal Diseases Aspergillosis, Coccidioidomycosis, Mucormycosis, and Candidiasis. Pathogens 2021, 10, 1303. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, M.D. Iron-chelating therapy with the new oral agent ICL670 (Exjade). Best Pract. Res. Clin. Haematol. 2005, 18, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Boelaert, J.R.; Van Cutsem, J.; de Locht, M.; Schneider, Y.J.; Crichton, R.R. Deferoxamine augments growth and pathogenicity of Rhizopus, while hydroxypyridinone chelators have no effect. Kidney Int. 1994, 45, 667–671. [Google Scholar] [CrossRef]
- Walsh, T.J.; Hiemenz, J.W.; Seibel, N.L.; Perfect, J.R.; Horwith, G.; Lee, L.; Silber, J.L.; DiNubile, M.J.; Reboli, A.; Bow, E.; et al. Amphotericin B lipid complex for invasive fungal infections: Analysis of safety and efficacy in 556 cases. Clin. Infect. Dis. 1998, 26, 1383–1396. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.S.; Gebermariam, T.; Fu, Y.; Lin, L.; Husseiny, M.I.; French, S.W.; Schwartz, J.; Skory, C.D.; Edwards, J.E.; Spellberg, B.J. The iron chelator deferasirox protects mice from mucormycosis through iron starvation. J. Clin. Investig. 2007, 117, 2649–2657. [Google Scholar] [CrossRef]
- Rodriȷguez, M.M.; Pastor, F.J.; Calvo, E.; Salas, V.; Sutton, D.A.; Guarro, J. Correlation of in vitro activity, serum levels, and in vivo efficacy of posaconazole against rhizopus microsporus in a murine disseminated infection. Antimicrob. Agents Chemother. 2009, 53, 5022–5025. [Google Scholar] [CrossRef]
- Sahu, R.K.; Salem-Bekhit, M.M.; Bhattacharjee, B.; Almoshari, Y.; Ikbal, A.M.A.; Alshamrani, M.; Bharali, A.; Salawi, A.; Widyowati, R.; Alshammari, A.; et al. Mucormycosis in Indian COVID-19 Patients: Insight into Its Patho-Genesis, Clinical Manifestation, and Management Strategies. Antibiotics 2021, 10, 1079. [Google Scholar] [CrossRef]
- COVID-19 Delta Variant Increases Incidence of Rhinocerebral Mucormycosis. Available online: https://www.enttoday.org/article/covid-19-delta-variant-increases-incidence-of-rhinocerebral-mucormycosis (accessed on 19 July 2021).
- Arakeri, G.; Rao Us, V.; Amaral Mendes, R.; Oeppen, R.S.; Brennan, P.A. COVID-associated mucormycosis (CAM): Is the Delta variant a cause? Br. J. Oral. Maxillofac. Surg. 2021, 16, S0266-4356(21)00335-1. [Google Scholar] [CrossRef]
- Bari, M.; Hossain, M.; Akhter, S.; Emran, T. Delta variant and black fungal invasion: A bidirectional assault might worsen the massive second/third stream of COVID-19 outbreak in South-Asia. Ethic-Med. Public Health 2021, 19, 100722. [Google Scholar] [CrossRef]
- Ravindra, K.; Ahlawat, A. Five probable factors responsible for the COVID-associated mucormycosis outbreak in India. Int. J. Infect. Dis. 2021, 112, 278–280. [Google Scholar] [CrossRef] [PubMed]
- Aranjani, J.M.; Manuel, A.; Razack, H.I.A.; Mathew, S.T. COVID-19–associated mucormycosis: Evidence-based critical review of an emerging infection burden during the pandemic’s second wave in India. PLOS Negl. Trop. Dis. 2021, 15, e0009921. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Grover, M.; Bhargava, S.; Samdani, S.; Kataria, T. Post coronavirus disease mucormycosis: A deadly addition to the pandemic spectrum. J. Laryngol. Otol. 2021, 135, 442–447. [Google Scholar] [CrossRef]
- Sen, M.; Honavar, S.G.; Bansal, R.; Sengupta, S.; Rao, R.; Kim, U.; Sowjanya, Y. Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India-collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1. Indian J. Ophthalmol. 2021, 69, 1670–1692. [Google Scholar] [PubMed]
- Werthman-Ehrenreich, A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am. J. Emerg. Med. 2020, 42, 264.e5–264.e8. [Google Scholar] [CrossRef]
- Placik, D.A.; Taylor, W.L.; Wnuk, N.M. Bronchopleural fistula development in the setting of novel therapies for acute respiratory distress syndrome in SARS-CoV2 pneumonia. Radio Case Rep. 2020, 15, 2378–2381. [Google Scholar] [CrossRef]
- Alekseyev, K.; Didenko, L.; Chaudhry, B. Rhinocerebral Mucormycosis and COVID-19 Pneumonia. J. Med Cases 2021, 12, 85–89. [Google Scholar] [CrossRef]
- Johnson, A.K.; Ghazarian, Z.; Cendrowski, K.D.; Persichino, J.G. Pulmonary aspergillosis and mucormycosis in a patient with COVID-19. Med Mycol. Case Rep. 2021, 32, 64–67. [Google Scholar] [CrossRef] [PubMed]
- Bellanger, A.-P.; Navellou, J.-C.; Lepiller, Q.; Brion, A.; Brunel, A.-S.; Millon, L.; Berceanu, A. Mixed mold infection with Aspergillus fumigatus and Rhizopus microsporus in a severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) patient. Infect Dis. Now. 2021, 51, 633–635. [Google Scholar] [CrossRef]
- Veisi, A.; Bagheri, A.; Eshaghi, M.; Rikhtehgar, M.H.; Kanavi, M.R.; Farjad, R. Rhino-orbital mucormycosis during steroid therapy in COVID-19 patients: A case report. Eur. J. Ophthalmol. 2021, 10, 11206721211009450. [Google Scholar] [CrossRef]
- Pakdel, F.; Ahmadikia, K.; Salehi, M.; Tabari, A.; Jafari, R.; Mehrparvar, G.; Rezaie, Y.; Rajaeih, S.; Alijani, N.; Barac, A.; et al. Mucormycosis in patients with COVID-19: A cross-sectional descriptive multicentre study from Iran. Mycoses 2021, 64, 1238–1252. [Google Scholar] [CrossRef] [PubMed]
- Sargin, F.; Akbulut, M.; Karaduman, S.; Sungurtekin, H. Severe rhinocerebral mucormycosis case developed after COVID 19. J. Bacteriol. Parasitol. 2021, 12, 1000386. [Google Scholar]
- Waizel-Haiat, S.; Guerrero-Paz, J.A.; Sanchez-Hurtado, L.; Calleja-Alarcon, S.; Romero-Gutierrez, L. A Case of fatal rhino-orbital mucormycosis associated with new onset diabetic ketoacidosis and COVID-19. Cureus 2021, 13, e13163. [Google Scholar] [CrossRef] [PubMed]
- Zurl, C.; Hoenigl, M.; Schulz, E.; Hatzl, S.; Gorkiewicz, G.; Krause, R.; Eller, P.; Prattes, J. Autopsy proven pulmonary mucormycosis due to Rhizopus microsporus in a critically Ill COVID-19 patient with underlying hematological malignancy. J. Fungi 2021, 7, 88. [Google Scholar] [CrossRef] [PubMed]
- Garg, D.; Muthu, V.; Sehgal, I.S.; Ramachandran, R.; Kaur, H.; Bhalla, A.; Puri, G.D.; Chakrabarti, A.; Agarwal, R. Coronavirus disease (COVID-19) associated mucormycosis (CAM): Case report and systematic review of literature. Mycopathologia 2021, 186, 289–298. [Google Scholar] [CrossRef]
- Hanley, B.; Naresh, K.; Roufosse, C.; Nicholson, A.G.; Weir, J.; Cooke, G.S.; Thursz, M.; Manousou, P.; Corbett, R.; Goldin, R.; et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: A post-mortem study. Lancet Microbe 2020, 1, e245–e253. [Google Scholar] [CrossRef]
- Kanwar, A.; Jordan, A.; Olewiler, S.; Wehberg, K.; Cortes, M.; Jackson, B. A Fatal case of Rhizopus azygosporus pneumonia following COVID-19. J. Fungi 2021, 7, 174. [Google Scholar] [CrossRef]
- Khatri, A.; Chang, K.-M.; Berlinrut, I.; Wallach, F. Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient–case report and review of literature. J. Mycol. Med. 2021, 31, 101125. [Google Scholar] [CrossRef]
- Jeong, W.; Keighley, C.; Wolfe, R.; Lee, W.L.; Slavin, M.A.; Kong, D.C.M.; Chen, S.C.-A. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin. Microbiol. Infect. Publ. Eur. Soc. Clin. Microbiol. Infect Dis. 2019, 25, 26–34. [Google Scholar] [CrossRef]
- Jain, M.; Tyagi, R.; Tyagi, R.; Jain, G. Post-COVID-19 gastrointestinal invasive mucormycosis. Indian J. Surg. 2021, 1–3. [Google Scholar] [CrossRef]
- Pasero, D.; Sanna, S.; Liperi, C.; Piredda, D.; Branca, G.P.; Casadio, L.; Terragni, P. A challenging complication following SARS-CoV-2 infection: A case of pulmonary mucormycosis. Infection 2021, 49, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- do Monte Junior, E.S.; Dos Santos ME, L.; Ribeiro, I.B.; de Oliveira Luz, G.; Baba, E.R.; Hirsch, B.S.; De Moura EG, H. Rare and fatal gastrointestinal mucormycosis (Zygomycosis) in a COVID-19 patient: A case report. Clin. Endosc. 2020, 53, 746–749. [Google Scholar] [CrossRef] [PubMed]

| Indian States | Number of Cases | Number of Deaths |
|---|---|---|
| Maharashtra | 1500 | 90 |
| Gujarat | 1163 | 61 |
| Madhya Pradesh | 575 | 31 |
| Haryana | 268 | 8 |
| Delhi | 203 | 1 |
| Uttar Pradesh | 169 | 8 |
| Bihar | 103 | 2 |
| Chattisgarh | 101 | 1 |
| Karnataka | 97 | ND |
| Telangana | 90 | 10 |
| CAM-Associated Species | Prevalence | References |
|---|---|---|
| Rhizopus spp. | Mexico, Iran, India 40–50% | [22,23,24,25,26,27] |
| Cunninghamella spp. | Global 40–60% | |
| Lichtheimia spp. | Europe (France) Up to 80% | |
| Rhizomucor spp. | Australia, France, Italy, India 90–100% | |
| R arrhizus | Worldwide 60% | |
| Mucor spp. | USA, Mexico, Iran, Greece 70–90% | |
| Apophysomyces | Asia (India) 90% | |
| Emerging Species | ||
| Rhizopus homothallicus | Asia 7.6% | |
| Thamnostylum lucknowense | Asia | |
| Mucor irregularis | China, India | |
| Saksenaea spp. | France, Australia 60–70% | |
| ToR microspores | India 11% |
| Country | No. of Cases | Affected Organ | References |
|---|---|---|---|
| India | 2849 | Rhino Orbital Cerebral | [85,86] |
| USA | 5 | Rhino Orbital Cerebral | [87,88,89,90] |
| Italy | 1 | Rhino Orbital Cerebral | [91] |
| Iran | 18 | Rhino Orbital Cerebral | [92,93,94] |
| Turkey | 1 | Rhino Orbital Cerebral | [95] |
| Mexico | 1 | Rhino Orbital Cerebral | [96] |
| India | 1 | Pulmonary | [97] |
| UK | 1 | Pulmonary | [98] |
| USA | 2 | Pulmonary | [99,100] |
| Australia | 1 | Pulmonary | [101] |
| India | 2 | Gastro-Intestinal | [33,102] |
| Brazil | 1 | Gastro-Intestinal | [103] |
| USA | 1 | Cutaneous | [104] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Girdhar, D.; Manocha, E. A Comprehensive Review on the Management of COVID-19-Associated Mucormycosis (CAM): The New Basics. BioMed 2022, 2, 181-198. https://doi.org/10.3390/biomed2020017
Girdhar D, Manocha E. A Comprehensive Review on the Management of COVID-19-Associated Mucormycosis (CAM): The New Basics. BioMed. 2022; 2(2):181-198. https://doi.org/10.3390/biomed2020017
Chicago/Turabian StyleGirdhar, Divyam, and Ekta Manocha. 2022. "A Comprehensive Review on the Management of COVID-19-Associated Mucormycosis (CAM): The New Basics" BioMed 2, no. 2: 181-198. https://doi.org/10.3390/biomed2020017
APA StyleGirdhar, D., & Manocha, E. (2022). A Comprehensive Review on the Management of COVID-19-Associated Mucormycosis (CAM): The New Basics. BioMed, 2(2), 181-198. https://doi.org/10.3390/biomed2020017





