Definition
The intensified exposure to high temperature in urban areas, resulting from the combination of heat waves and the urban heat island (UHI) effect, necessitates a deeper understanding of the climate–health relationship. This knowledge directly influences the strategies employed by policy makers and urban planners in their efforts to regenerate cities and protect their population. Nature-based solutions and the widely accepted 15 min city model, characterized by a polycentric structure, should drive the implementation of effective adaptation policies, especially given the persistent delay in mitigation efforts. However, it is less clear whether current or future policies are adequately structured to broadly address the complex forms of social vulnerability. A prime example of this complexity is the demographic shift observed since the mid-20th century, characterized by a relative increase in the elderly population, and a shrinking youth demographic. While extensive literature addresses the physiological impacts of heat wave on human health, evidence regarding the neuro-psychological and cognitive implications for elderly individuals, who frequently suffer from chronic diseases, remains less comprehensive and more fragmented. The purpose of this concise review is to emphasize that crucial findings on the climate–health relationship, particularly concerning the elderly, have often been developed within disciplinary silos. The lack of comprehensive interdisciplinary integration coupled with an incomplete understanding of the full spectrum of vulnerabilities (encompassing both physiological and cognitive) may lead to urban policies that are egalitarian in principle but fail to achieve true equity in practice. This review aims to bridge this gap by highlighting the need for a more integrated approach to urban policy and regeneration.
1. Introduction
The relationship between meteorology and climate on the health and behavior of living beings has been a subject of interest since the earliest days of medicine. Today, influences on health are undeniably linked to rapid urbanization, and the changing demographic structure of high-income countries, particularly the increasing proportion of elderly individuals. Climatic phenomena, both large-scale and local, can lead to significant physical and neurological impairments in large sections of the population. Economic, social, and health determinants of fragility undoubtedly exacerbate these phenomena. Urban climate has been proven to contribute to the onset of pathologies. However, the neuro-psychological aspect of this contribution remains in the specialist sphere, finding few connections in the master plan organization of cities. This literature review aims to highlight which aspects of neurological disorder are attributable to interaction with the local climate, with a particular focus on elderly. This allows for a subsequent analysis of urban regeneration techniques that could mitigate, if not prevent, such impacts on the more vulnerable segments of the population.
A significant number of studies are focusing on urban climates and their impact on the well-being of the resident population. However, despite substantial improvements in our understanding of urban climate since Howard’s pioneering 1833 study (which effectively created the discipline) [1], how urbanization and climate change will interact in the future remains uncertain. Cities are a clear and present danger, a potential source of air, water, and soil pollutants. It is vital to acknowledge the impact of various environmental factors, including heat islands, CO2 domes, particulate matter, and ozone, on human health. The lack of parks and green spaces and the distance urban residents feel from the natural world can have adverse physio-psychological effects [2,3]. Thus, creating a “climate resilient” urban environment requires us to integrate scientific knowledge and management skills.
Addressing urban resilience requires a broader system of governance. This governance must encompass the city’s performance as a built environment, its ability to withstand and absorb the effects of environmental hazards, and its ability to reduce the exposure of the population, especially its most vulnerable members, to health risks [4,5]. Global change presents us with the opportunity to address the problem of understanding and controlling urban processes from the perspective of an “ecology of the city” [6,7,8]. This perspective aligns with international frameworks such as the United Nations Sustainable Development Goal 11 (SDG#11), “Sustainable cities and Communities”, which advocates for inclusive, safe, resilient, and sustainable human settlements (Figure 1) [9].

Figure 1.
Specific targets of Sustainable Development Goal 11 (SDG#11) of U.N. Sustainability Agenda 2020–2030. Adapted from [9].
Specific targets for SDG#11, like enhancing inclusive and sustainable urbanization, are directly relevant to fostering healthier cities and protecting fragile. It is vital to recognize that not all cities can provide an ideal environment for the elderly, especially in large cities. This is the conclusion of the European Commission report on the quality of life in European Cities 2024. In Europe, the proportion of people aged 65 and over went up from 18% in 2012 to 21% in 2022, and is expected to be 24% in 2030 and up to 29% in 2050. It is encouraging to see that the development of elder-friendly cities has become a key urban planning goal. Only 78% of them think that their city is a good place to grow old. This opinion varies widely among European regions. There is higher acceptance in the north and west then in the east and south. Cities’ size is a key factor: smaller cities are clearly more welcoming for the elderly than larger ones. About 83% of elderly in cities with a population of less then 250,000 say they are satisfied, compared with 75% in cities with a population of between 1 and 5 million inhabitants [10]. This demographic trend, which characterizes all industrially advanced countries, suggests a future that will undoubtedly present social and health issues, as well as economic ones. We must consider a comprehensive prevention approach, which could include structural modifications to our cities. This can be done in line with the UN Sustainability Agenda 2020–2030 (Figure 1) and the World Health Organization (WHO) recommendations provided in the One-Health Approach [11].
2. Local Climate Effects on Population Health
Urban air pollution and urban heat waves represent subjects of persistent and significant concern in scientific discourse, political deliberations, and public health considerations.
The relationship between heat waves and a worsened air quality is explained by the fact that the urban structure responds to a higher enthalpy content (heat accumulated in materials) of the city, causing a high degree of mixing of pollutants emitted into the environment and, in fact, trapping them inside it for long periods of time.
The WHO is responsible for the monitoring of the concentration of pollutants in urban areas and the subsequent effects on human health. It is estimated that in 2019, approximately 7 million people died because of exposure to air pollutants [12]. This number underscores that atmospheric contamination represents the most significant threat to public health in the contemporary era.
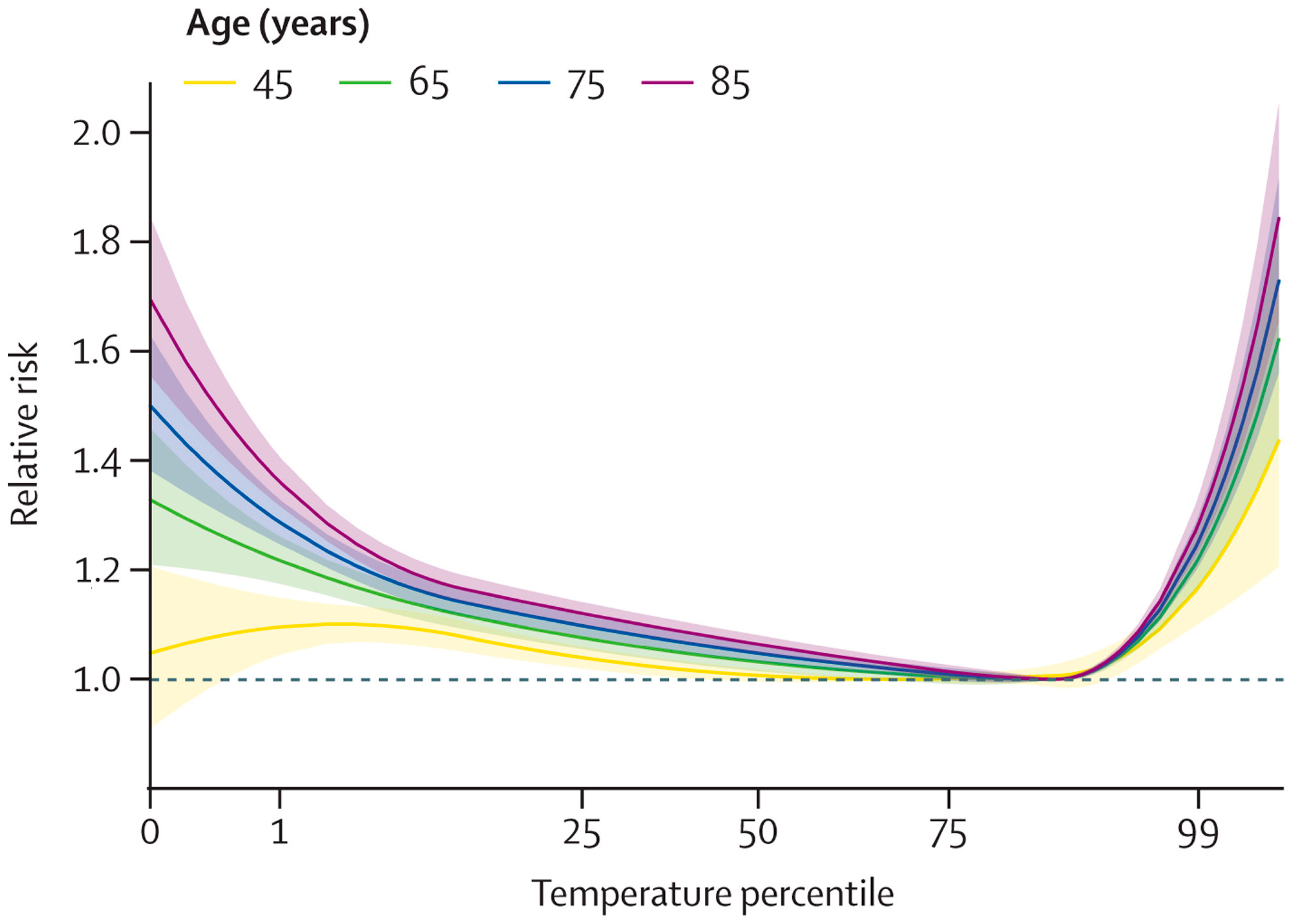
Heat waves are high-temperature spikes lasting a few days and exceeding typical seasonal temperatures. This phenomenon is related to climate change, as they have increased in frequency and intensity. The frequency and intensity of heat waves are extreme events related to climate change, with a regional effect. The 2003 European heatwave, during which Italy, France, Spain, Germany, Portugal, and Switzerland collectively recorded 72,210 heat-related fatalities, serves as a particularly salient exemplar of the potential consequences of inadequate preparedness for climate change. It is evident that elevated and protracted heat waves exert a direct influence on well-being, particularly among vulnerable demographics such as children, the elderly, and the infirm [13,14,15]. More recent data continue to demonstrate the severe health impacts of heatwaves, including substantial excess mortality across Europe in subsequent extreme heat events, such as the summer of 2022 [16,17]. Similar trends are observed in US cities [18]. As Masselot et al. [17] highlighted, a cumulative exposure–response relationship has been identified for several age groups, with an increasing trend of relative risk for increasing age (Figure 2).
Figure 2.
Mortality relative risk as a function of temperature for age groups. Adapted from [17].
In urban areas, the microclimate is known to differ significantly from that of surrounding regions. This discrepancy has been shown to result in an exacerbation of events that engender greater levels of discomfort, in addition to direct impacts on human health. Such impacts may include respiratory difficulties, fatal and non-fatal strokes, and sleep cycle disruption. Kalkstein et al. [19] estimated that, in forty large cities in the United States, there were an additional 1300 deaths per year in the decades 1975–2004 due to Excessive Heat Events (EHEs). More recent analyses continue to highlight persistent heat-related mortality and morbidity in urban settings, especially for vulnerable groups [18].
The social implications of elevated EHE encompass not only mortality but also morbidity, resulting in increased hospital admissions. During the 1995 Chicago heat wave, which persisted for more then a week, a total of 1072 excess admissions were documented, representing an increase of approximately 11% in comparison with typical conditions. Most of these cases (56%) necessitated treatment for dehydration, heatstroke, and heat exhaustion. Semenza et al. (1999) [20] also revealed excess hospital admissions for cardiovascular disease, diabetes, respiratory disease (such as pneumonia, emphysema, asthma, and chronic obstructive), kidney disease, and nervous system disorders through their analysis. As a corollary to the diagnosis of heatstroke, diagnoses of hydro-electrolytic disorders and acid–base imbalances have been made, in addition to acute renal failure following dehydration. A 20% increase in the prevalence of pneumonia and emphysema was observed in the hospital admissions, attributed to the hot and humid climate. As Semenza et al. (1999) [20] have demonstrated, individuals suffering from diabetes are acutely susceptible to the adverse effects of heat waves.
During the summer of 2003, a period of extreme heat characterized by elevated temperatures occurred in western Europe. This EHE was of a magnitude that was unprecedented in historical records. It was estimated that occurrences of this magnitude had not been witnessed in the last 150 years. Temperatures remained well above the climatological average for a period of approximately three months (1 June to 31 August) over a geographical region extending from the Iberian Peninsula to Germany and Italy, with a primary focus on France. In the latter country, temperatures exceeded 38 °C for a period of seven days. As Kalkstein et al. (2008) [21] demonstrate, the maximum daily temperature was 6 °C higher than the average maximum temperature, while the minimum daily temperatures were also extremely above average. It is estimated that the number of heat-related mortalities in France alone exceeded 15,000 cases [22,23].
Conti et al. (2005) [24] conducted an epidemiological study of the 2003 EHE, which strongly emphasized the role of UHI during heat waves. The study demonstrated that the increase in mortality occurred primarily among elderly people living in urban areas.
It is evident that there is an urgent need to formulate urban management strategies that can mitigate the severe impacts on citizens’ health.
The primary adaptation strategies must be initiated by local health authorities, who can act at various levels and provide information on the effects of climate change and its threats to the health of the urban population. Early warning systems have been shown to be valuable instruments in the provision of strategic warnings to residents, with the purpose of informing them of extreme weather events and enabling them to react accordingly. In the long term, tactical measures to be employed to facilitate urban adaptation to climate change may be categorized as follows: the planting of trees, the adoption of green and reflective roofs, and permeable pavements, with a view to reducing the intensity and size of urban heat islands. Health facility measures are important, such as plans to prevent heat stress risks. In addition, the creation of emergency plans in case of flooding is recommended.
3. Neurological and Mental Health Effects of Local Climate
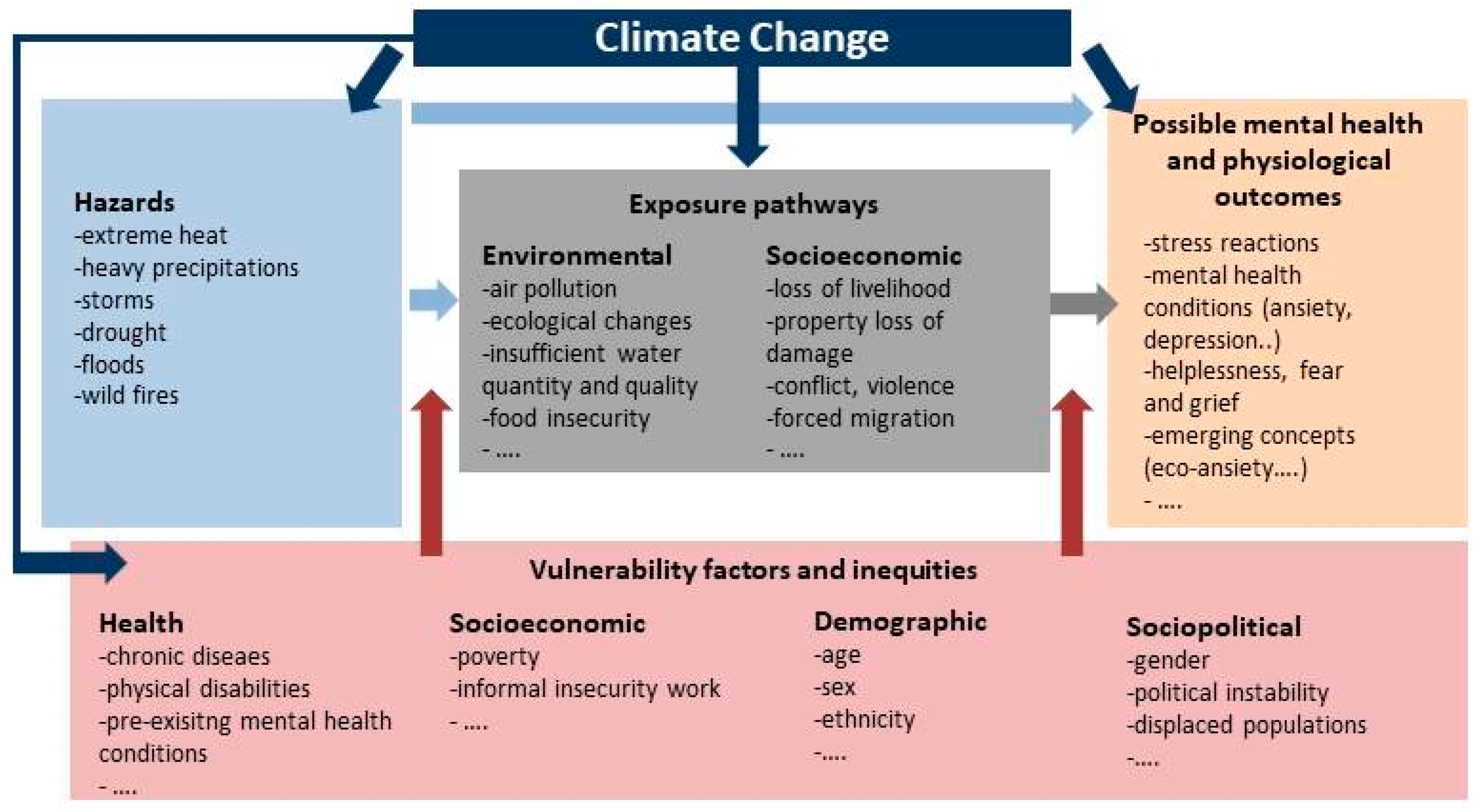
There is a link between climate alteration and our psyche. This manifests itself through complexities that characterize our daily lives. Exploring the origins and consequences of such global phenomena in more depth is the key to understanding their influence on our physical bodies, minds, and emotional states. It is vital to recognize the impact of environmental determinants, which are in a constant state of flux and evolution, on our psychological well-being. These difficulties inevitably lead to a range of reactions, including forms of adaptation and resilience, and in some cases, more profound existential crises. It is vital to consider how these changes in climate impact social relations among individuals. This creates opportunities for a more thoughtful and mindful understanding and management of our natural environment, as well as our mental well-being and psychological health [2,3]. It is important to clarify that while “psychological well-being” encompasses emotional states, stress, and coping mechanisms, “neurological effects” refer to direct impacts on brain function and structure, potentially leading to specific neurological disorders. However, these two domains are intricately linked; prolonged psychological distress can exacerbate or trigger neurological vulnerabilities, and vice-versa: studies have reported significant associations between well-being and various areas of the brain [25]. As Figure 3 shows, climate-related hazards, long-term risks, exposure pathways, and vulnerabilities all intersect to influence mental health through direct and indirect pathways. It is crucial to understand that these factors do not operate in isolation. They can overlap with each other. People are exposed to multiple climate and environmental impacts at the same time. Populations’ existing vulnerabilities can be exacerbated by long-term, large-scale climate risks or short-term, local-scale risks, with all the variability this entails, leading to increased inequalities [8,26]. The resulting impacts have significant implications for mental health and well-being. The Intergovernmental Panel on Climate Change (IPCC) is clear: climate-related diseases, premature deaths, malnutrition in all its forms, and threats to mental health and well-being are increasing. Health systems worldwide are under-resourced and have a minimal capacity to respond to climate change, with particularly little support for mental health [27].
Figure 3.
Main connections between climate change and mental health. Adapted from [28].
Environmental, social, and economic determinants of mental health include air quality, water quantity and quality, food security, income and livelihoods, ecosystem changes, and a range of other social and economic pathways.
Climate change will have an adverse effect on all of us. For instance, during periods of high temperatures, air pollution has been known to cause respiratory illnesses that increase demand for health services, reduce mobility and ability to work, and have mental health impacts ranging from minimal stress and discomfort to the development of mental illness, particularly in low-income settings [29]. In highly urbanized environments, the local climate generates the urban heat island (UHI), which has the potential to produce a re-entrapment or concentration of pollutants within the city fabric. This indicates a clear link between the built environment and the pollutants themselves. The case of prolonged droughts, for example, clearly illustrates the impact of climate change on these determinants. It is vital to recognize the considerable impact of drought on agricultural production and the risk of loss of livelihoods, which can exacerbate the challenges faced by many communities, including the risk of poverty. This has been linked to the development of common mental illnesses [30]. Droughts can contribute to water scarcity and food insecurity, which in turn can have a negative impact on mental health and increase the risk of mental illness [31,32,33].
Food shortages resulting from drought can lead to developmental delays, mental health problems and neurological problems resulting from poor or inadequate nutrition [32,34]. It is vital to understand the impact of climate change on mental health determinants like these. This knowledge is essential for both understanding their impacts and taking climate action.
It is vital to acknowledge that some groups are more vulnerable to the impacts of climate change due to existing inequalities. Disability is a complex phenomenon with many facets, resulting from the interaction between long-term physical, mental, intellectual or sensory impairments, which are often invisible, and environmental barriers, as well as the increased prevalence of age-related disabilities, given that almost half of people over the age of 65 have some form of disability. This is particularly evident in low- and middle-income countries, despite their historically low levels of greenhouse gas emissions [35,36,37,38,39,40]. For instance, indigenous peoples define well-being in terms of harmony with their natural environment, which is subject to significant change in the context of climate change. They are most affected by the loss of even small amounts of land, wildlife, or other climate-related impacts. It is also clear that children and adolescents are particularly affected and will exhibit intense reactions to the scale of the crisis and lack of action [41]. Crucially, older adults represent another highly vulnerable demographic, often facing compounding factors such as reduced mobility, chronic health conditions, social isolation, and lower socioeconomic status, which intensify their susceptibility to climate-related mental and neurological health impacts.
However, understanding vulnerability requires an analysis aimed at identifying contextual factors [42]. It is crucial to understand that vulnerability is not determined by a single factor. However, when there are multiple, often interacting, vulnerability factors, the effects are often multiplied [34,43,44,45]. For instance, an individual may be older, have a lower socioeconomic status, reside in a water-stressed area, or suffer from a chronic disease. However, this does not automatically make them as vulnerable as someone experiencing all these factors concurrently.
The mental health consequences of climate change are well-documented [46,47,48,49,50,51]. They range from minimal stress and symptoms of distress to clinical disorders, including anxiety and sleep disturbances [52], depression, post-traumatic stress, and suicidal thoughts [53,54]. Other consequences include the effect on individuals and communities in their daily lives, perceptions, and experiences. They also have to cope, understand, and respond appropriately to climate change and its implications. It is vital to acknowledge that people exposed to climate- or weather-related natural disasters often experience significant stress and mental health consequences. Climate change will undoubtedly lead to more frequent natural disasters. It is vital to acknowledge that reactions to extreme events involving disruption of life, such as loss of life, resources, social support, and social networks, or extensive relocation, can lead to post-traumatic stress disorder (PTSD), depression, and general anxiety, increased substance use or misuse, and suicidal thoughts. Research has clearly shown a link between peritraumatic experience and acute stress during and immediately after a disaster, which can undoubtedly lead to the onset of PTSD [55].
Both direct and indirect health impacts of extreme heat and extreme precipitation have been identified as part of the relationship between climate and health. Health risks caused by these factors have increased significantly in recent years [56,57].
There is a complex interconnection between physical health, mental health, human well-being, and heat waves. Heat stress, which heat waves can cause, is associated with mood disorders, anxiety, and related consequences [58,59]. People with mental illness are more vulnerable to the consequences of heat waves [53,60] and that exposure to heat waves during pregnancy, particularly in the second and third trimesters, is associated with lower mean birth weight and an increased likelihood of preterm delivery. While the paper primarily focuses on the elderly, it is also important to note that exposure to heatwaves during pregnancy, particularly in the second and third trimesters, is associated with lower mean birth weight and an increased likelihood of preterm delivery. The effects during childhood and adulthood are also clear: reduced education and economic activity, behavioral and motor problems, and reduced IQ [53]. While these specific instances may deviate slightly from the direct elderly focus, they illustrate the broad and pervasive neurological/cognitive impacts of extreme heat. There is clear evidence of a difference in vulnerability between the sexes. The 2003 European heatwave saw a higher death rate in women than in men. The negative outcomes of heatwaves are also related to social factors. Women, young people, and people with low socioeconomic status are more vulnerable to disaster-related anxiety and mood disorders. People enjoy the outdoor environment more during the summer months, which can increase the likelihood of conflict arising. Higher temperatures are associated with increased discomfort, escalating hostility, aggressive thoughts, and possibly even actions. Cities with higher temperatures have a greater propensity for violence. There has been a clear increase in heat-related violence, particularly during the summer months and in warmer years [61].
4. Integrated and Multidisciplinary Approaches for Urban Resilience
The segments of the population most affected by this phenomenon are the elderly, children, people with disabilities, and the chronically ill (the so-called frail population), with whom a low-income condition may also be associated. It is vital to consider the citizen as an individual with specific needs and to understand, assess, and plan protection mechanisms to make the city truly equitable. Mobility impairment can impede an individual’s ability to navigate the city and fulfil their needs and desires. These difficulties result in increased exposure time and, consequently, heightened climate risk for individuals with disabilities. It is therefore imperative that specific policies are implemented to mitigate the urban environment, with a view to reducing the relative risk to people with disabilities by decreasing their exposure to high temperatures. One such measure might be the creation of more shaded areas. The ‘Life Project’, an Italian law [62], is the key to overcoming urban isolation enhancing accessibility during EHEs, including for the most vulnerable members of society, such as individuals living with disabilities. This measure is crucial in reducing their risk of exposure to heat. The law proposes a new definition of disability, moving away from the biomedical model, which focuses on illness and disorder, and adopting a biopsychosocial approach that takes into account the interaction between the individual, their health conditions and environmental and social barriers. For instance, the fundamental evaluation—a compulsory procedure for all individuals seeking recognition of disability—transforms into a multidisciplinary and personalized process that considers all dimensions of the individual’s life, encompassing not only their impairments but also their functionality and capacity to navigate the physical and social environment. The law introduces the obligation of reasonable accommodation for all public and private entities. Reasonable accommodation is defined as a measure aimed at finding a compromise between what is and can be offered by both the public and private entities requesting the Life Project. Every person with a disability must be assured the right to full integration into the community. This means ensuring equal freedom of choice as well as full involvement in the life of society. This concept must be extended to the entire frail population. Cities must be equitable towards the needs of disabled people and the elderly. This is not only a primary need, but also a way of fully satisfying expectations and enabling autonomous decisions [63]. A paradigm shift is needed: we must move from focusing on needs to considering the rights of the frail, valuing the principle of quality of life, and promoting pathways to autonomy. The aim is to create a city of reliable citizenship for all. There are no easy answers when it comes to addressing the challenges of urban climate adaptation. Adaptation is political. Planning is constrained by complex, contextual, and uneven factors. The field of urban climate adaptation planning is still in its early stages, but this will soon change. A truly integrated approach to urban resilience against climate change impacts, particularly concerning neuro-psychological health in vulnerable populations, must encompass several key pillars:
- Health Sector Adaptation and Public Health Interventions: Local health authorities are crucial in initiating primary adaptation strategies. This involves developing and disseminating clear information on climate change impacts and health threats, particularly targeting vulnerable groups. Implementing robust early warning systems for extreme weather events is vital for providing strategic warnings to residents, informing them and enabling timely adaptive behaviors. Beyond warnings, the health sector must proactively adapt its facilities and services. This includes ensuring hospitals and care homes are climate-resilient (e.g., equipped with adequate cooling systems, backup power during heatwaves/power outages), training healthcare professionals on climate-related health risks (both physical and mental), and developing specialized support programs for the elderly and those with chronic conditions to manage heat stress and air pollution impacts.
- Urban Planning and Design: Tactical, long-term measures for urban adaptation are essential to reduce the intensity and size of urban heat islands (UHIs). These include extensive urban greening initiatives, such as widespread tree planting campaigns to increase canopy cover and provide shade; the adoption of green roofs and reflective pavements to reduce heat absorption; and the implementation of permeable surfaces to improve water management and reduce flood risks. Such measures not only mitigate physical climate impacts but also offer significant co-benefits for mental well-being by increasing access to nature and improving urban aesthetics.
- Social and Community Support Systems: Beyond physical infrastructure, strengthening social cohesion and community networks is critical. This involves creating community-based programs that support vulnerable individuals, promoting intergenerational activities, and establishing accessible cooling centers during heatwaves. Digital inclusion initiatives can also help bridge the gap for isolated seniors, ensuring they receive vital information and support.
- Multi-Scalar Governance and Policy Integration: Effective climate adaptation requires collaboration across different governance levels (local, regional, national) and integration across various policy sectors (health, urban planning, social services, environment). This ensures that climate resilience is embedded in all aspects of urban development, not treated as an isolated issue.
- Research and Data-Driven Strategies: Continued application of mixed methods research is needed to explore and refine urban adaptation policies globally [64]. This includes rigorous monitoring and evaluation of implemented strategies to ensure their effectiveness and adaptability to evolving climatic conditions.
By embracing such an integrated and multifaceted approach, cities can move towards becoming truly resilient, equitable, and supportive environments for all citizens, particularly those most susceptible to climate change impacts.
5. Conclusions
This review has underscored the critical and escalating impact of urban climatic phenomena, particularly the urban heat island (UHI) effect and air pollution, on human health. A key focus has been their neuro-psychological consequences for vulnerable populations, especially the elderly. We have highlighted how rapid urbanization and demographic shifts, coupled with extreme weather events, exacerbate pre-existing fragilities, leading to a range of physical and mental health challenges.
The evidence presented reinforces that health systems worldwide are currently under-resourced to address these escalating climate-related health threats, particularly regarding mental health support. Our discussion has emphasized the intricate links between environmental stressors (e.g., extreme heat, air pollution, and indirectly, food insecurity due to drought) and adverse neuro-psychological outcomes, including stress, anxiety, depression, and other physiological disorders.
To effectively mitigate these impacts, this paper advocates for a robust, integrated, and multidisciplinary approach to urban resilience, as detailed in Section 4. This includes crucial actions within the health sector (e.g., enhanced preparedness, early warning systems, adapted facilities), strategic urban planning and design (e.g., widespread green infrastructure, reflective surfaces to counteract UHI), and the reinforcement of social and community support systems. Such a comprehensive strategy is essential to create equitable and supportive urban environments.
Despite significant advancements, further research is still needed to fully comprehend the multifaceted long-term consequences of climate change on mental health, especially in diverse vulnerable groups. Future studies should continue to explore the intricate correlations between climate phenomena and both physiological and neurological disorders. There is also a recognized need for more research on specific psychological reactions to landscape changes (e.g., solastalgia, eco-anxiety) and to develop a deeper understanding of acute, sub-acute, and long-term consequences. It is imperative that future research adopts an increasingly multidisciplinary lens, fostering a common language across fields to better address these complex challenges. Scholars must particularly concentrate on how different vulnerable segments of the population are affected by natural disasters and climate change, and how to effectively deploy protective measures and health resources. Ultimately, urban policy and regeneration initiatives must prioritize vulnerable groups, not as a minority, but as the central focus of intervention, ensuring their autonomy and well-being in the face of evolving climatic conditions.
Author Contributions
Conceptualization, T.G. and L.C.; formal analysis, T.G. and L.C.; methodology, T.G.; data curation, T.G.; resources T.G. and L.C.; writing—original draft preparation T.G. and L.C.; writing—review and editing, T.G. and L.C.; visualization, L.C.; supervision, T.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the European Union under the Horizon Europe Programme, grant number [101137851].
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
This study was conducted in the frame of the project Climate-Resilient Development Pathways in Metropolitan Regions of Europe (CARMINE) funded by the European Union under the Horizon Europe Programme (Grant agreement 101137851).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Howard, L. The Climate of London. 1833. Available online: https://archive.org/details/climatelondonde01howagoog/page/n8/mode/2up (accessed on 9 January 2025).
- Castagna, C. Ecoansia Among College Young Adults: An Analysis of Perceptions and Emotions Related to Climate Change. Master’s Thesis, Università degli Studi di Padova, Padova, Italy, 2024. Available online: https://thesis.unipd.it/bitstream/20.500.12608/75194/1/Castagna%20Caterina.pdf (accessed on 9 January 2025).
- Cipriani, E.; Frumento, S.; Grassini, S.; Gemignani, A.; Menicucci, D. Do Individual Differences in Perception Affect Awareness of Climate Change? Brain Sci. 2024, 14, 266. [Google Scholar] [CrossRef] [PubMed]
- Georgiadis, T. Urban Climate and Risk. In Oxford Handbook Topics in Physical Sciences, Online Ed.; Oxford Academic: Oxford, UK, 2017. [Google Scholar] [CrossRef]
- Georgiadis, T. Climate Change and Effects on Cities, 3rd ed.; Emilia-Romagna Region REnovation of Public Building and Urban Spaces: Bologna, Italy, 2018; Available online: https://territorio.regione.emilia-romagna.it/urbanistica/formazione-ed-eventi/corsi-formazione/rebus-laboratorio-rigeneraz-urbana-cambiam-climatici (accessed on 8 January 2025).
- Vicari, S. Autonomous Children Safe Adolescents; LSWR Editions: Milan, Italy, 2021; p. 285. [Google Scholar]
- Cacioppo, S.; Cacioppo, J.T. Introduction to Social Neuroscience; Raffaello Cortina Editore: Milan, Italy, 2022; p. 298. [Google Scholar]
- Cianconi, P.; Janiri, L. Climate Change and Mental Health: From the Ecology of Mind to the Ecological Mind; Raffaello Cortina Editore: Milan, Italy, 2023; p. 369. [Google Scholar]
- The Sustainable Development Agenda. Available online: https://www.un.org/sustainabledevelopment/development-agenda/ (accessed on 8 January 2025).
- European Commission. Report on the Quality of Life in European Cities. 2023. Available online: https://ec.europa.eu/regional_policy/sources/reports/qol2023/2023_quality_life_european_cities_en.pdf (accessed on 10 January 2025).
- WHO. One Health. 2024. Available online: https://www.who.int/health-topics/one-health#tab=tab_1 (accessed on 8 January 2025).
- World Health Organization (WHO). Ambient (Outdoor) Air Pollution. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 21 July 2025).
- Cardelino, C.A.; Chameides, W.L. Natural hydrocarbons, urbanization, and urban ozone. J. Geoph. Res. 1990, 95, 13971–13979. [Google Scholar] [CrossRef]
- Changnon, S.A.; Kunkel, K.E.; Reinke, B.C. Impacts and responses to the 1995 heat wave: A call to action. Bull. Am. Meteorol. Soc. 1996, 77, 1497–1506. [Google Scholar] [CrossRef]
- McMichael, A.J. The urban environment and health in a world of increasing globalization: Issues for developing countries. Bull. World Health Organ. 2000, 78, 1117–1126. [Google Scholar] [PubMed]
- Ballester, J.; Quijal-Zamorano, M.; Méndez Turrubiates, R.F.; Pegenaute, F.; Herrmann, F.R.; Robine, J.M.; Basagaña, X.; Tonne, C.; Antó, J.M.; Achebak, H. Heat-related mortality in Europe during the summer of 2022. Nat. Med. 2023, 29, 1857–1866. [Google Scholar] [CrossRef] [PubMed]
- Masselot, P.; Mistry, M.; Vanoli, J.; Schneider, R.; Iungman, T.; Garcia-Leon, D.; Ciscar, J.C.; Feyen, L.; Orru, H.; Urban, A.; et al. Excess mortality attributed to heat and cold: A health impact assessment study in 854 cities in Europe. Lancet Planet Health 2024, 8, e531. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.T.; Androne, N.; Alcover, K.C.; Santos-Lozada, A.R. Trends of Heat-Related Deaths in the US, 1999–2023. JAMA 2024, 332, 1203–1204. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kalkstein, L.S.; Greene, S.; Mills, M.D.; Samenow, J. An evaluation of the progress in reducing heat-related human mortality in major U.S. cities. Nat. Hazards 2011, 56, 113–129. [Google Scholar] [CrossRef]
- Semenza, J.C.; McCullogh, J.E.; Flanders, W.D.; McGeehin, M.A.; Lumpkin, J.R. Excess hospital admissions during the July 1995 heat-wave in Chicago. Am. J. Prev. Med. 1999, 16, 269–399. [Google Scholar] [CrossRef]
- Kalkstein, L.S.; Greene, J.S.; Mills, D.M.; Perrin, A.D.; Samenow, J.P.; Cohen, J.-C. Analog European heat waves for U.S. cities to analyze impacts on heat-related mortality. Bull. Am. Meteorol. Soc. 2008, 89, 75–86. [Google Scholar] [CrossRef]
- Koppe, C.; Kovats, S.; Jendritzky, G.; Menne, B. Heat-Waves: Risks and Responses; World Health Organization: Geneva, Switzerland, 2004; Available online: https://iris.who.int/bitstream/handle/10665/107552/9789289010948-eng.pdf?sequence=1&isAllowed=y (accessed on 19 January 2025).
- Poumadère, M.; Mays, C.; Le Mer, S.; Blong, R. The 2003 heat wave in France: Dangerous climate change here and now. Risk Anal. 2005, 25, 1483–1494. [Google Scholar] [CrossRef]
- Conti, S.; Meli, P.; Minelli, G.; Solimini, R.; Toccaceli, V.; Vichi, M.; Beltrano, C.; Perini, L. Epidemiologic study of mortality during the Summer 2003 heat wave in Italy. Environ Res. 2005, 98, 390–399. [Google Scholar] [CrossRef] [PubMed]
- King, M.L. The neural correlates of well-being: A systematic review of the human neuroimaging and neuropsychological literature. Cogn. Affect. Behav. Neurosci. 2019, 19, 779–796. [Google Scholar] [CrossRef]
- WHO. Mental Health Atlas 2020; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240036703 (accessed on 4 January 2025).
- IPCC. Climate Change 2022: Impacts, Adaptation, and Vulnerability; Pörtner, H.-O., Roberts, D.C., Tignor, M., Poloczanska, E.S., Mintenbeck, K., Alegría, A., Craig, M., Langsdorf, S., Löschke, S., Möller, V., et al., Eds.; Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2022; Available online: https://www.ipcc.ch/report/ar6/wg2/ (accessed on 6 January 2025).
- Corvalan, C.; Gray, B.; Villalobos Prats, E.; Sena, A.; Hanna, F.; Campbell-Lendrum, D. Mental health and the global climate crisis. Epidemiol. Psychiatr. Sci. 2022, 31, e86. [Google Scholar] [CrossRef]
- Dodgen, D.; Donato, D.; Kelly, N.; La Greca, A.; Morganstein, J.; Reser, J.; Ruzek, J.; Schweitzer, S.; Shimamoto, M.; Thigpen Tart, K.; et al. Ch. 8: Mental health and well-being. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 217–246. [Google Scholar]
- Lund, C.; Breen, A.; Flisher, A.; Kakuma, R.; Corrigall, J.; Joska, J.; Swartz, L.; Patel, V. Poverty and common mental disorders in low- and middle-income countries: A systematic review. Soc. Sci. Med. 2010, 71, 517–528. [Google Scholar] [CrossRef] [PubMed]
- Stanke, C.; Kerac, M.; Prudhomme, C.; Medlock, J.; Murray, V. Health effects of drought: A systematic review of the evidence. PLoS Curr. 2013, 5, ecurrents.dis.7a2cee9e980f91ad7697b570bcc4b004. [Google Scholar] [CrossRef]
- Vins, H.; Bell, J.; Saha, S.; Hess, J.J. The mental health outcomes of drought: A systematic review and causal process diagram. Int. J. Environ. Res. Public Health 2015, 12, 13251–13275. [Google Scholar] [CrossRef] [PubMed]
- Pourmotabbed, A.; Moradi, S.; Babaei, A.; Ghavami, A.; Mohammadi, H.; Jalili, C.; Symonds, M.E.; Miraghajani, M. Food insecurity and mental health: A systematic review and meta-analysis. Public Health Nutr. 2020, 23, 1778–1790. [Google Scholar] [CrossRef] [PubMed]
- Cianconi, P.; Betrò, S.; Janiri, L. The impact of climate change on mental health: A systematic descriptive review. Front. Psychiatry 2020, 11, 74. [Google Scholar] [CrossRef]
- Berry, H.L.; Bowen, K.; Kjellstrom, T. Climate change and mentalhealth: A causal pathways framework. Int. J. Public Health 2010, 55, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Berry, H.; Hogan, A.; Owen, J.; Rickwood, D. Climate change and farmers’ mental health: Risks and responses. Asia Pac. J. Public Health 2011, 23 (Suppl. S2), 119S–132S. [Google Scholar] [CrossRef]
- Berry, H.L.; Waite, T.; Dear, K.; Capon, A.; Murray, V. The case for systems thinking about climate change and mental health. Nat. Clim. Change 2018, 8, 282–290. [Google Scholar] [CrossRef]
- Bourque, F.; Cunsolo Willox, A. Climate change: The next challenge for public mental health? Int. Rev. Psychiatry 2014, 26, 415–422. [Google Scholar] [CrossRef]
- Hayes, K.; Poland, B. Addressing mental health in a changing climate: Incorporating mental health indicators into climate change and health vulnerability and adaptation assessment. Int. J. Environ. Res. Public Health 2018, 15, 1806. [Google Scholar] [CrossRef]
- Palinkas, L.; Wong, M. Global climate change and mental health. Curr. Opin. Psychol. 2019, 32, 12–16. [Google Scholar] [CrossRef]
- Hickman, C.; Marks, E.; Pihkala, P.; Clayton, S.; Lewandowski, E.; Mayall, E.; Wray, B.; Mellor, C.; van Susteren, L. Climate anxiety in children and young people and their beliefs about government responses to climate change: A global survey. Lancet Planet. Health 2021, 5, e863–e873. [Google Scholar] [CrossRef]
- WHO. Climate Change and Health: Vulnerability and Adaptation Assessment; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240036383 (accessed on 4 January 2025).
- Gamble, J.L.; Balbus, J.; Berger, M.; Bouye, K.; Campbell, V.; Chief, K.; Conton, K.; Criminis, A.; Flanagan, B.; Gonzalez-Maddux, C.; et al. Ch. 9: Populations of Concern. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; Crimmins, A., Balbus, J., Gamble, J.L., Beard, C.B., Bell, J.E., Dodgen, D., Eisen, R.J., Fann, N., Hawkins, M.D., Herring, S.C., et al., Eds.; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 247–285. Available online: https://www.healthandenvironment.org/docs/ImpactsClimageChangeHumanHealthUSGlobalChangeResearchProgramSmall2016.pdf (accessed on 5 January 2025).
- Hayes, K.; Berry, P.; Ebi, K. Factors Influencing the Mental Health Consequences of Climate Change in Canada. Int. J. Environ. Res. Public Health 2019, 16, 1583. [Google Scholar] [CrossRef]
- Ogunbode, C.A.; Bohm, G.; Capstick, S.B.; Demsky, C.; Spence, A.; Tausch, N. The resilience paradox: Flooding experience, coping and climate change mitigation intentions. Clim. Policy 2019, 19, 703–715. [Google Scholar] [CrossRef]
- Obradovich, N.; Migliorini, R.; Paulus, M.P.; Rahwan, I. Empirical evidence of mental health risks posed by climate change. Proc. Natl. Acad. Sci. USA 2018, 115, 10953–10958. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.; Hornigold, R.; Page, L.; Waite, T. Association between high ambient temperatures and heat waves with mental health outcomes: A systematic review. Public Health 2018, 161, 171–191. [Google Scholar] [CrossRef] [PubMed]
- Hayes, K.; Blashki, G.; Wiseman, J.; Burke, S.; Reifels, L. Climate change and mental health: Risks, impacts and priority actions. Int. J. Ment. Health Syst. 2018, 12, 28. [Google Scholar] [CrossRef]
- Zheng, G.; Li, K.; Wang, Y. The effects of high-temperature weather on humanj sleep quality and appetite. Int. J. Environ. Res. Public Health 2019, 16, 270. [Google Scholar] [CrossRef]
- Liu, J.; Varghese, B.M.; Hansen, A.; Xiang, J.; Zhang, Y.; Dear, K.; Gourley, M.; Driscoll, Y.; Morgan, G.; Capon, A.; et al. Is there an association between hot weather and poor mental health outcomes. A systematic review and meta-analysis. Environ. Int. 2021, 153, 106533. [Google Scholar] [CrossRef] [PubMed]
- Pihkala, P. The process of eco-anxiety and ecological grief. A narrative review and new proposal. Sustainability 2022, 14, 16628. [Google Scholar] [CrossRef]
- Blanc, J.; Spruill, T.; Butler, M.; Casimir, G.; Jean-Louis, G. 0885 Is Resilience A Protective Factor for Sleep Disturbances Among Earthquake Survivors? Sleep 2019, 42 (Suppl. 1), A356. [Google Scholar] [CrossRef]
- Ursano, R.J.; Morganstein, J.C.; Cooper, R. Resource Document on Mental Health and Climate Change; APA Committee on Psychiatric Dimensions of Disaster: Washington, DC, USA, 2017; Available online: https://www.psychiatry.org/getattachment/b7fb9e58-86f7-4b54-bd32-59fb50f32d9c/Resource-Document-2017-Mental-Health-Climate-Change.pdf (accessed on 18 January 2025).
- Somoza-Moncada, M.M.; Turrubiates-Herrnandez, F.J.; Munoz-Valle, J.F.; Gutierrez-Brito, J.A.; Diaz-Perez, S.A.; Aguayo-Arelis, A.; Hernandez-Bello, J. Vitamin D in depression: A potential bioactive agent to reduce suicide and suicide attempt risk. Nutrients 2023, 15, 1765. [Google Scholar] [CrossRef] [PubMed]
- Gruebner, O.; Lowe, S.R.; Sykora, M.; Shankardass, K.; Subramanian, S.V.; Galea, S. A novel surveillance approach for disaster mental health. PLoS ONE 2017, 12, e0181233. [Google Scholar] [CrossRef]
- Gronlund, C.J.; Cameron, L.; Shea, C.; O’Neill, M.S. Assessing the magnitude and uncertainties of the burden of selected diseases attributable to extreme heat and extreme precipitation under a climate change scenario in Michigan for the period 2041–2070. Environ. Health 2019, 18, 40. [Google Scholar] [CrossRef]
- Zheng, C.; Yujia, H.; Yuguo, Y. Attention restoration during environmental exposure via alpha-tetha oscillations and synchronization. J. Environ. Psychol. 2020, 68, 101406. [Google Scholar]
- Padhy, S.K.; Sarkar, S.; Panigrahi, M.; Surender, P. Mental health effects of climate change. Indian J. Occup. Environ. Med. 2015, 19, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Repke, M.A.; Berry, M.S.; Conway, L.G.; Metcalf, A.; Hensen, R.M.; Phelan, C. How does nature exposure make people healthier? Evidence for the role of impulsivity and expanded space perception. PLoS ONE 2018, 3, e0202246. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Gavin, L.; Pearson, D.; Ebisu, K.; Malig, B. Examining the association between apparent temperature and mental health-related emergency room visits in California. Am. J. Epidemiol. 2018, 187, 2264. [Google Scholar] [CrossRef] [PubMed]
- Towers, S.; Chen, S.; Malik, A.; Ebert, D. Factors influencing temporal patterns in crime in a large American city: A predictive analytics perspective. PLoS ONE 2018, 13, e0205151. [Google Scholar] [CrossRef]
- Legislative Decree 62/2024—Italian Republic. Official Gazette No. 111, 14 May 24. Available online: https://www.gazzettaufficiale.it/eli/id/2024/05/14/24G00079/SG (accessed on 9 January 2025). (In Italian).
- Mathes, E.W. Maslow’s Hierarchy of Needs as a Guide for Living. J. Humanist. Psychol. 1981, 21, 69–72. [Google Scholar] [CrossRef]
- Meerow, S.; Mitchell, C.L. Weathering the storm: The politics of urban climate change adaptation planning. Environ. Plan. A 2017, 49, 2619–2627. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).