Multi-Modal Approach to Mitigating Hamstring Injuries in Division I College Football Athletes
Definition
1. Introduction or History
2. Description of HSI, Injury Prevention, and HSI Rehabilitation Intervention
2.1. Nature of HSI
2.2. Preventative Considerations
3. Evidence-Based Rehabilitation Interventions/Clinical Practice Guidelines
3.1. Theoretical Models and Factors to Mitigate the Impact of HSI
3.2. Mobile Health Technologies
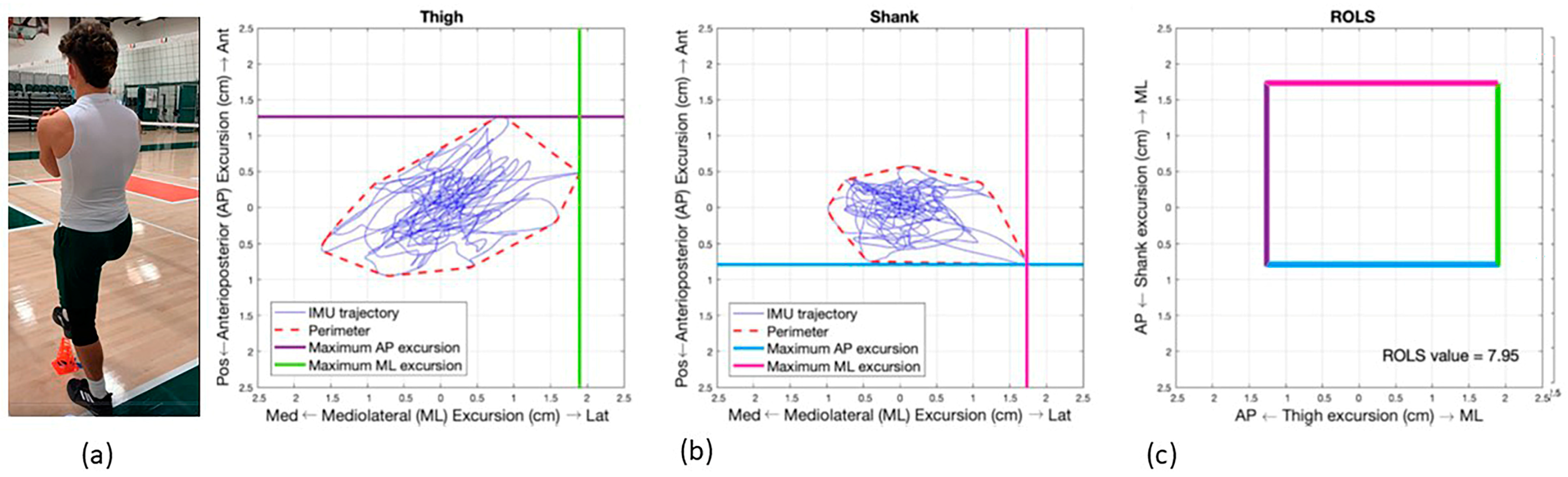
3.3. The Region of Limb Stability (ROLS)
3.4. Alternative Technologies for Assessing Limb Stability
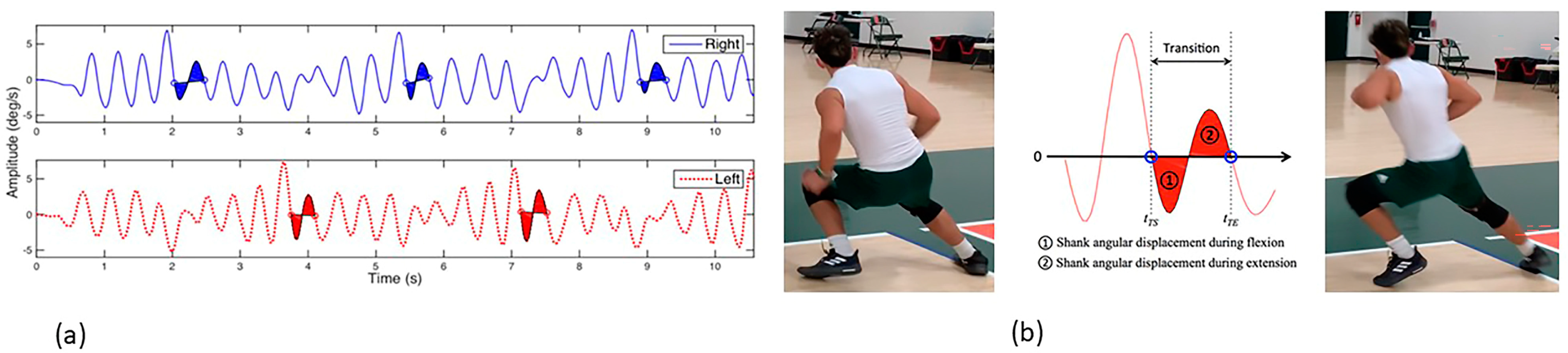
3.5. Transitional Angular Displacement of Segments (TADS)
3.6. Alternative Technologies for Assessing Limb Stability
3.7. GPS Tracking
4. Force Plate Analysis
5. Hamstring-Based Exercise Program (HBEP)
6. Summary/Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al Attar, W.S.A.; Soomro, N.; Sinclair, P.J.; Pappas, E.; Sanders, R.H. Effect of Injury Prevention Programs that Include the Nordic Hamstring Exercise on Hamstring Injury Rates in Soccer Players: A Systematic Review and Meta-Analysis. Sports Med. 2017, 47, 907–916. [Google Scholar] [CrossRef]
- Chandran, A.; Morris, S.N.; Powell, J.R.; Boltz, A.J.; Robison, H.J.; Collins, C.L. Epidemiology of Injuries in National Collegiate Athletic Association Men’s Football: 2014–2015 Through 2018–2019. J. Athl. Train. 2021, 56, 643–650. [Google Scholar] [CrossRef]
- Dalton, S.L.; Kerr, Z.Y.; Dompier, T.P. Epidemiology of Hamstring Strains in 25 NCAA Sports in the 2009–2010 to 2013–2014 Academic Years. Am. J. Sports Med. 2015, 43, 2671–2679. [Google Scholar] [CrossRef]
- Ekstrand, J.; Spreco, A.; Bengtsson, H.; Bahr, R. Injury Rates Decreased in Men’s Professional Football: An 18-Year Prospective Cohort Study of Almost 12,000 Injuries Sustained During 1.8 Million Hours of Play. Br. J. Sports Med. 2021, 55, 1084–1091. [Google Scholar] [CrossRef]
- Green, B.; Bourne, M.N.; van Dyk, N.; Pizzari, T. Recalibrating the risk of hamstring strain injury (HSI): A 2020 systematic review and meta-analysis of risk factors for index and recurrent hamstring strain injury in sport. Br. J. Sports Med. 2020, 54, 1081–1088. [Google Scholar] [CrossRef]
- Mack, C.D.; Kent, R.W.; Coughlin, M.J.; Shiue, K.Y.; Weiss, L.J.; Jastifer, J.R.; Wojtys, E.M.; Anderson, R.B. Incidence of Lower Extremity Injury in the National Football League: 2015 to 2018. Am. J. Sports Med. 2020, 48, 2287–2294. [Google Scholar] [CrossRef]
- Poudel, B.; Pandey, S. Hamstring Injury; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Wing, C.E.; Turner, A.N.; Bishop, C.J. Importance of Strength and Power on Key Performance Indicators in Elite Youth Soccer. J. Strength Cond. Res. 2020, 34, 2006–2014. [Google Scholar] [CrossRef] [PubMed]
- Chumanov, E.S.; Heiderscheit, B.C.; Thelen, D.G. The Effect of Speed and Influence of Individual Muscles on Hamstring Mechanics During the Swing Phase of Sprinting. J. Biomech. 2007, 40, 3555–3562. [Google Scholar] [CrossRef]
- Danielsson, A.; Horvath, A.; Senorski, C.; Alentorn-Geli, E.; Garrett, W.E.; Cugat, R.; Samuelsson, K.; Senorski, E.H. The Mechanism of Hamstring Injuries—A Systematic Review. BMC Musculoskelet Disord. 2020, 21, 641. [Google Scholar] [CrossRef]
- Heiderscheit, B.C.; Sherry, M.A.; Silder, A.; Chumanov, E.S.; Thelen, D.G. Hamstring Strain Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. J. Orthop. Sports Phys. Ther. 2010, 40, 67–81. [Google Scholar] [CrossRef]
- Erickson, L.N.; Sherry, M.A. Rehabilitation and Return to Sport after Hamstring Strain Injury. J. Sport Health Sci. 2017, 6, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Bourne, M.N.; Williams, M.D.; Opar, D.A.; Al Najjar, A.; Kerr, G.K.; Shield, A.J. Impact of Exercise Selection on Hamstring Muscle Activation. Br. J. Sports Med. 2017, 51, 1021–1028. [Google Scholar] [CrossRef]
- Bourne, M.N.; Duhig, S.J.; Timmins, R.G.; Williams, M.D.; Opar, D.A.; Al Najjar, A.; Kerr, G.K.; Shield, A.J. Impact of the Nordic Hamstring and Hip Extension Exercises on Hamstring Architecture and Morphology: Implications for Injury Prevention. Br. J. Sports Med. 2019, 51, 469–477. [Google Scholar] [CrossRef]
- Biz, C.; Nicoletti, P.; Baldin, G.; Bragazzi, N.L.; Crimì, A.; Ruggieri, P. Hamstring Strain Injury (HSI) Prevention in Professional and Semi-Professional Football Teams: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2021, 18, 8272. [Google Scholar] [CrossRef]
- Askling, C.M.; Tengvar, M.; Thorstensson, A. Acute Hamstring Injuries in Swedish Elite Football: A Prospective Randomised Controlled Clinical Trial Comparing Two Rehabilitation Protocols. Br. J. Sports Med. 2013, 47, 953–959. [Google Scholar] [CrossRef] [PubMed]
- Tyler, T.F.; Schmitt, B.M.; Nicholas, S.J.; McHugh, M.P. Rehabilitation After Hamstring-Strain Injury Emphasizing Eccentric Strengthening at Long Muscle Lengths: Results of Long-Term Follow-Up. J. Sport Rehabil. 2017, 26, 131–140. [Google Scholar] [CrossRef]
- Martin, R.L.; Cibulka, M.T.; Bolgla, L.A.; Koc, T.A.; Loudon, J.K.; Manske, R.C.; Weiss, L.; Christoforetti, J.J.; Heiderscheit, B.C. Hamstring Strain Injury in Athletes. J. Orthop. Sports Phys. Ther. 2022, 52, CPG1–CPG44. [Google Scholar] [CrossRef]
- Sherry, M.A.; Best, T.M. A Comparison of 2 Rehabilitation Programs in the Treatment of Acute Hamstring Strains. J. Orthop. Sports Phys. Ther. 2004, 34, 116–125. [Google Scholar] [CrossRef]
- Van Hooren, B.; Bosch, F. Is There Really an Eccentric Action of the Hamstrings During the Swing Phase of High-Speed Running? Part I: A Critical Review of the Literature. J. Sports Sci. 2017, 35, 2313–2321. [Google Scholar] [CrossRef] [PubMed]
- Van Hooren, B.; Bosch, F. Is There Really an Eccentric Action of the Hamstrings During the Swing Phase of High-Speed Running? Part II: Implications for Exercise. J. Sports Sci. 2017, 35, 2322–2333. [Google Scholar] [CrossRef]
- Baroni, B.M.; Costa, L.O.P. Evidence-Based Prevention of Sports Injuries: Is the Sports Medicine Community on the Right Track? J. Orthop. Sports Phys. Ther. 2021, 51, 91–93. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex Systems Approach for Sports Injuries: Moving from Risk Factor Identification to Injury Pattern Recognition—Narrative Review and New Concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed]
- Feigenbaum, L.A.; Gaunaurd, I.A.; Kim, K.J.; Raya, M.A.; Ruiz, J.T.; Rapicavoli, J.; Best, T.M.; Kaplan, L.; Gailey, R.S. Accuracy of the Region of Limb Stability in Predicting Risk for Lower Limb Injury. Med. Sci. Sports Exer. 2020, 11, 2483–2488. [Google Scholar] [CrossRef] [PubMed]
- Feigenbaum, L.A.; Kim, K.J.; Gaunaurd, I.A.; Kaplan, L.D.; Scavo, V.A.; Bennett, C.; Gailey, R.S. Post-Concussive Changes in Balance and Postural Stability Measured with CaneSense and the Balance Error Scoring System (Bess) in Division I Collegiate Football Players: A Case Series. Int. J. Sports Phys. Ther. 2019, 14, 296–307. [Google Scholar] [CrossRef]
- Feigenbaum, L.A.; Kaplan, L.D.; Musto, T.; Gaunaurd, I.A.; Gailey, R.S.; Kelley, W.P.; Alemi, T.J.; Espinosa, B.; Mandler, E.; Scavo, V.A.; et al. A Multidisciplinary Approach in the Rehabilitation of a Collegiate Football Players Following an Ankle Fracture: Case Report. Int. J. Sports Phys. Ther. 2016, 11, 436–449. [Google Scholar] [PubMed]
- Gailey, R.; Gaunaurd, I.; Raya, M.; Kirk-Sanchez, N.; Prieto-Sanchez, L.M.; Roach, K. Effectiveness of an Evidence Based-Amputee Rehabilitation (EBAR) Program: A Pilot Randomized Controlled Trial. Phys Ther. 2020, 100, 773–787. [Google Scholar] [CrossRef]
- Gailey, R.S.; Gaunaurd, I.A.; Raya, M.A.; Roach, K.E.; Linberg, A.A.; Campbell, S.M.; Jayne, D.M.; Scoville, C. The Development and Reliability Testing of the Comprehensive High-level Activity Mobility Predictor (CHAMP) in Service Members with Traumatic Lower Limb Loss. J. Rehabil. Res. Dev. 2013, 50, 905–918. [Google Scholar] [CrossRef] [PubMed]
- Gailey, R.S.; Scoville, C.; Gaunaurd, I.A.; Raya, M.A.; Linberg, A.A.; Stoneman, P.D.; Campbell, S.M.; Roach, K.E. Construct Validity of the Comprehensive High-level Activity Mobility Predictor (CHAMP) for Service Members with Traumatic Lower Limb Loss. J. Rehabil. Res. Dev. 2013, 50, 919–930. [Google Scholar] [CrossRef]
- Gaunaurd, I.; Gailey, R.; Springer, B.; Symsack, A.; Clemens, S.; Lucarevic, J.; Kristal, A.; Bennette, C.; Isaacson, B.; Agrawal, V.; et al. The Utility of the DoD/VA Mobile Device Outcomes Based Rehabilitation Program (MDORP) for Higher Functioning Service Members and Veterans with Lower Limb Amputation. Mil. Med. 2020, 185, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Gaunaurd, I.; Kim, K.J.; Feigenbaum, L.; Raya, M.; Baraga, M.; Fontela, N.; Gailey, R. Construct validation of lower limb segmental excursion as a measure of potential risk for lower limb injury in Division I women’s basketball players. J. Biomech. 2019, 84, 252–256. [Google Scholar] [CrossRef]
- Gaunaurd, I.A.; Gailey, R.S.; Pasquina, P. More than the Final Score: The Development, Application, and Future Research of the Comprehensive High-level Activity Mobility Predictor. J. Rehabil. Res. Dev. 2013, 50, vii–xiii. [Google Scholar] [CrossRef]
- Gaunaurd, I.A.; Roach, K.; Raya, M.A.; Hooper, R.; Linberg, A.A.; Laferrier, J.Z.; Campbell, S.M.; Scoville, C.; Gailey, R.S. Factors Related to High Level Mobility in Service Members with Traumatic Lower Limb Loss. J. Rehabil. Res. Dev. 2013, 50, 969–984. [Google Scholar] [CrossRef]
- Kim, K.J.; Gailey, R.; Agrawal, V.; Gaunaurd, I.; Feigenbaum, L.; Bennett, C.; Felt, V.; Best, T.M. Quantification of Agility Testing with Inertial Sensors after a Knee Injury. Med. Sci. Sports Exerc. 2020, 52, 244–251. [Google Scholar] [CrossRef]
- Kim, K.J.; Agrawal, V.; Bennett, C.; Gaunaurd, I.; Feigenbaum, L.; Gailey, R. Measurement of Lower Limb Segmental Excursion Using Inertial Sensors during Single Limb Stance. J. Biomech. 2018, 71, 151–158. [Google Scholar] [CrossRef]
- Allseits, E.K.; Agrawal, V.; Prasad, A.; Bennett, C.; Kim, K.J. Characterizing the Impact of Sampling Rate and Filter Design on the Morphology of Lower Limb Angular Velocities. IEEE Sens. J. 2019, 19, 4115–4122. [Google Scholar] [CrossRef]
- Allseits, E.; Kim, K.J.; Bennett, C.; Gailey, R.; Gaunaurd, I.; Agrawal, V. A Novel Method for Estimating Knee Angle Using Two Leg-Mounted Gyroscopes for Continuous Monitoring with Mobile Health Devices. Sensors 2018, 22, 2759. [Google Scholar] [CrossRef]
- Allseits, E.; Lučarević, J.; Gailey, R.; Agrawal, V.; Gaunaurd, I.; Bennett, C. The Development and Concurrent Validity of a Real-Time Algorithm for Temporal Gait Analysis Using Inertial Measurement Units. J. Biomech. 2017, 55, 27–33. [Google Scholar] [CrossRef]
- Kim, K.J.; Agrawal, V.; Gaunaurd, I.; Gailey, R.S.; Bennett, C.L. Missing Sample Recovery for Wireless Inertial Sensor-Based Human Movement Acquisition. IEEE Trans. Neural. Syst. Rehabil. Eng. 2016, 24, 1191–1198. [Google Scholar] [CrossRef]
- Kim, K.J.; Lučarević, J.; Bennett, C.; Gaunaurd, I.; Gailey, R.; Agrawal, V. Testing the Assumption of Normality in Body Sway Area Calculations during Unipedal Stance Tests with an Inertial Sensor. Ann. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016, 4987–4990. [Google Scholar]
- Gabbett, T.J.; Whiteley, R. Two Training-Load Paradoxes: Can We Work Harder and Smarter, Can Physical Preparation and Medical Be Teammates? Int. J. Sports Physiol. Perform. 2017, 12, S250–S254. [Google Scholar] [CrossRef]
- Gabbett, T.J. The training-injury prevention paradox: Should athletes be training smarter and harder? Br. J. Sports Med. 2016, 50, 273–280. [Google Scholar] [CrossRef]
- Windt, J.; Gabbett, T.J. How Do Training and Competition Workloads Relate to Injury? The Workload-Injury Aetiology Model. Br. J. Sports Med. 2017, 51, 428–435. [Google Scholar] [CrossRef]
- Hulin, B.T.; Gabbett, T.J.; Lawson, D.W.; Caputi, P.; Sampson, J.A. The Acute:Chronic Workload Ratio Predicts Injury: High Chronic Workload May Decrease Injury Risk in Elite Rugby League Players. Br. J. Sports Med. 2016, 50, 231–236. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Tenan, M.S.; Kempton, T.; Novak, A.; Coutts, A.J. Acute:Chronic Workload Ratio: Conceptual Issues and Fundamental Pitfalls. Int. J. Sports Physiol. Perform. 2020, 15, 907–913. [Google Scholar] [CrossRef]
- Colby, M.J.; Dawson, B.; Peeling, P.; Heasman, J.; Rogalski, B.; Drew, M.K.; Stares, J. Improvement of Prediction of Noncontact Injury in Elite Australian Footballers with Repeated Exposure to Established High-Risk Workload Scenarios. Int. J. Sports Physiol. Perform. 2018, 13, 1130–1135. [Google Scholar] [CrossRef]
- Shah, S.; Collins, K.; Macgregor, L.J. The Influence of Weekly Sprint Volume and Maximal Velocity Exposures on Eccentric Hamstring Strength in Professional Football Players. Sports 2022, 10, 125. [Google Scholar] [CrossRef] [PubMed]
- Suchomel, T.J.; Nimphius, S.; Stone, M.H. The Importance of Muscular Strength in Athletic Performance. Sports Med. 2016, 46, 1419–1449. [Google Scholar] [CrossRef]
- Mitchell, A.; Holding, C.; Greig, M. The Influence of Injury History on Countermovement Jump Performance and Movement Strategy in Professional Soccer Players: Implications for Profiling and Rehabilitation Foci. J. Sport Rehabil. 2021, 30, 768–773. [Google Scholar] [CrossRef]
- McMahon, J.J.; Lake, J.P.; Comfort, P. Reliability of and Relationship between Flight Time to Contraction Time Ratio and Reactive Strength Index Modified. Sports 2018, 6, 81. [Google Scholar] [CrossRef]
- Merrigan, J.J.; Tufano, J.J.; Jones, M.T. Potentiating Effects of Accentuated Eccentric Loading Are Dependent Upon Relative Strength. J. Strength Cond. Res. 2021, 35, 1208–1216. [Google Scholar] [CrossRef]
- Hart, A.S.; Erskine, R.M.; Clark, D.R. The Use of Physical Characteristics to Explain Variation in Ball-Carrying Capability in Elite Rugby Union: A Narrative Review. J. Strength Cond. Res. 2023, 37, 1718–1727. [Google Scholar] [CrossRef] [PubMed]
- Aspe, R.; Swinton, P.A. Electromyographic and Kinetic Comparison of the Back Squat and Overhead Squat. J. Strength Cond. Res. 2014, 28, 2827–2836. [Google Scholar] [CrossRef]
- Delgado, J.; Drinkwater, E.J.; Banyard, H.G.; Haff, G.G.; Nosaka, K. Comparison between Back Squat, Romanian Deadlift, and Barbell Hip Thrust for Leg and Hip Muscle Activities during Hip Extension. J. Strength Cond. Res. 2019, 33, 2595–2601. [Google Scholar] [CrossRef] [PubMed]
- Ishøi, L.; Hölmich, P.; Aagaard, P.; Thorborg, K.; Bandholm, T.; Serner, A. Effects of the Nordic Hamstring Exercise on Sprint Capacity in Male Football Players: Randomized Controlled Trial. J. Sports Sci. 2018, 36, 1663–1672. [Google Scholar] [CrossRef] [PubMed]
- Martin-Fuentes, I.; Oliva-Lozano, J.M.; Muyor, J.M. Electromyographic Activity in Deadlift Exercise and Its Variants: A Systematic Review. PLoS ONE 2020, 15, e0229507. [Google Scholar] [CrossRef]
- Pollard, C.W.; Opar, D.A.; Williams, M.D.; Bourne, M.N.; Timmins, R.G. Razor Hamstring Curls and Nordic Hamstring Exercise Architectural Adaptations: Impact of Exercise Selection and Intensity. Scand. J. Med. Sci. Sports 2019, 29, 706–715. [Google Scholar] [CrossRef]
- Steele, J.; Bruce-Low, S.; Smith, D. A Review of the Specificity of Exercises Designed for Conditioning the Lumbar Extensors. Br. J. Sports Med. 2015, 49, 291–297. [Google Scholar] [CrossRef]
- van der Horst, N.; Smits, D.; Petersen, J.; Geodhart, E.A.; Backx, J.G. The Preventive Effects of the Nordic Hamstring Exercise on Hamstring Injuries in Amateur Soccer Players: A Randomized Controlled Trial. Am. J. Sport Med. 2015, 43, 1316–1323. [Google Scholar] [CrossRef]

| Modifiable |
| Low endurance and strength deficits |
| Lack of core stability and pelvic control |
| Tightness of the hamstrings and surrounding musculature |
| Reduced neuromuscular control due to fatigue |
| Inadequate dynamic stretching, activation, and warm-up |
| Muscle strength imbalances (e.g., quadriceps-to-hamstrings) |
| Incomplete or improper rehab of previous injuries |
| Inefficient sprint mechanics and improper running form |
| Excessive intensity or volume |
| Non-Modifiable |
| Older age |
| Anatomical factors (muscle architecture and fascicle length) |
| Genetic predisposition (collagen properties affecting tissue integrity) |
| Gender (males have a slightly higher risk) |
| History of previous HSI |
| Skeletal structure (pelvic tilt or leg length discrepancies) |
| PBOM | ReLOAD SportTM | GPS | Force Plate | Strength and Conditioning |
|---|---|---|---|---|
| Single-limb stance (s) | Lower limb ROLS value (cm2) | Top speed | Eccentric braking RFD | Daily exercise sets and repetitions (HBEP) |
| Four-meter side-step test (s) | ROLS Symmetry (%) | Player training load | Force at zero velocity asymmetry | Weekly exercise sets and repetitions (HBEP) |
| Countermovement jump | Lower limb TADS (deg/s) | High-speed efforts monitored per position group | Concentric impulse Eccentric impulse | Movement training of running mechanics |
| Depth jump | TADS symmetry (%) | Total distance traveled (day and week) | Landing asymmetry | Movement training of deceleration mechanics |
| Squat jump | Total accelerations and decelerations | Reactive strength index | Movement training of change in direction mechanics | |
| Acute: chronic workload ratio | Peak power | Preventative mobility/exercises |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz, J.T.; Gaunaurd, I.A.; Best, T.M.; Feeley, D.; Mann, J.B.; Feigenbaum, L.A. Multi-Modal Approach to Mitigating Hamstring Injuries in Division I College Football Athletes. Encyclopedia 2024, 4, 1482-1495. https://doi.org/10.3390/encyclopedia4040096
Ruiz JT, Gaunaurd IA, Best TM, Feeley D, Mann JB, Feigenbaum LA. Multi-Modal Approach to Mitigating Hamstring Injuries in Division I College Football Athletes. Encyclopedia. 2024; 4(4):1482-1495. https://doi.org/10.3390/encyclopedia4040096
Chicago/Turabian StyleRuiz, Jeffrey T., Ignacio A. Gaunaurd, Thomas M. Best, David Feeley, J. Bryan Mann, and Luis A. Feigenbaum. 2024. "Multi-Modal Approach to Mitigating Hamstring Injuries in Division I College Football Athletes" Encyclopedia 4, no. 4: 1482-1495. https://doi.org/10.3390/encyclopedia4040096
APA StyleRuiz, J. T., Gaunaurd, I. A., Best, T. M., Feeley, D., Mann, J. B., & Feigenbaum, L. A. (2024). Multi-Modal Approach to Mitigating Hamstring Injuries in Division I College Football Athletes. Encyclopedia, 4(4), 1482-1495. https://doi.org/10.3390/encyclopedia4040096







