Definition
Multiple long-term conditions such as the simultaneous prevalence of obesity, diabetes and cardiovascular disease are becoming increasingly prevalent globally with major consequences of morbidity, mortality and health economy. Lifestyle preventative approaches, especially combining nutrition and physical activity behavioral components, are essential in preventing multiple long-term conditions. However, funded research programs often focus on a single disease or a condition rather than a cluster of conditions. This entry addresses how lifestyle components, especially exercise and nutrition, could target multiple risk reductions associated with preventing multiple long-term conditions, especially diabetes and cardiovascular disease. Innovative exercise prescription should include different intensity-based approaches, which may include intense forms of exercise, but one size does not fit all. Nutritional intake guidelines can also be individualized to target multiple long-term conditions, which all contribute to informing better public health preventative policies.
1. Introduction
Lifestyle related diseases are becoming prevalent globally and non-communicable diseases (NCDs) such as cardiovascular disease (CVD), cancer, respiratory disease and diabetes are now becoming synonymous causes of mortality among adults. Type-2 diabetes (T2D) prevalence figures have almost reached one in ten adults [1], but this figure is on the rise due to the recent COVID-19 lockdown burdens, especially given the reduced healthcare provision and the increased sedentary lifestyle. Multiple NCDs have often been clustered together as the term multimorbidity is coined, which defines the simultaneous existence of two or more chronic conditions in the same individual, such as diabetes, CVD and hypertension [2]. However, lifestyle being the primary cause of such diseases could serve as the primary preventative approach of multimorbidity; hence, it should remain a priority prevention across the healthcare systems.
Interventions involving lifestyle are well established amongst several NCDs. For example, diabetes prevention programs have shown superior or similar effectiveness to medication in individuals with prediabetes [3,4,5,6]. Conventional components of such lifestyle interventions were primarily driven by physical activity, nutrition and education in individuals with high risks of T2D and cardiovascular disease [7,8]. Large prospective cohort studies have consistently demonstrated that lifestyle interventions have significant risk reduction in T2D incidence among populations with impaired glucose tolerance or those with prediabetes [3,4,5,6]. Both the US diabetes prevention program and the Finnish diabetes studies showed 58% reduced T2D incidence in a large cohort who followed combined physical activity and dietary lifestyle behavior changes over a 5-year period [3,4]. Similar benefits of lifestyle interventions have also been shown across other global regions such as those shown in the Indian Diabetes Study and the Di Qing study in China [5,6]. A single-component nutritional lifestyle intervention, focusing on adopting the Mediterranean diet longitudinally, has also shown CVD prevention effectiveness [9,10]. This intervention was retrospectively analyzed for diabetes incidence in older adults with prediabetes as a secondary outcome, and showed that the Mediterranean diet had reversed prediabetes into the remission state [11]. As such, longitudinal and population-based physical activity and nutritional interventions are recommended to prevent multiple long-term conditions.
However, lessons from such largescale interventions across different countries have also shown that widescale interventions require major government, societal and health care systems’ commitment, significant healthcare cost and coordinated efforts, which are not always possible across the globe [12]. Disparities between high-income countries (HICs) and low- and middle-income countries (LMICs), based on countries’ GDP, have been associated with a prevalence of NCDs across different age groups [13,14]. There is also an issue of health inequality in terms of community reach, recruitment, effectiveness and long-term adherence, even with the same country. Preventative healthcare could target a cluster of NCDs via interventions which could be appropriated across different populations. Therefore, whether and how is an important question to answer via this entry, which proposes lifestyle intervention approaches to address multiple long-term conditions, including those appropriate to reduce health disparities, and offers useful tools for public health researchers and healthcare professionals.
2. Optimization Components of Lifestyle Interventions for Multiple Long-Term Conditions
The design of a lifestyle intervention requires significant coordinated efforts from diverse expertise of healthcare professionals, policy makers and funders, and so it is often faced by numerous organizational barriers [15]. In England, current lifestyle prevention guidelines in both exercise and nutrition are disperse, even for a single condition, let alone for multiple long-term conditions [16]. Given the clear benefits of lifestyle disease prevention, it would be important to appropriate the specific components of lifestyle towards making targeted and practical recommendations for multiple long-term conditions.
Targeting multiple risk reduction of NCDs is possible through ameliorating shared disease mechanisms, such as those contained in obesity, diabetes and cardiovascular disease. Each disease or a condition has specific primary (e.g., reduced incidence rate) and secondary outcomes (e.g., glucose and lipid profiles, blood pressure and cardiorespiratory fitness), which can be modified through targeted adjustments in lifestyle behaviors, whether being physical activity, nutritional, dietary or psychological components. However, it is impossible to solely attribute a single lifestyle component to the desired intervention benefits. Meta-analysis and intervention studies have shown that the benefits of physical activity alone, especially in walking exercise, are more effective in terms of compliance than a combined component approach involving diet and exercise [17,18]. However, a combined approach involving exercise and nutrition changes is effective for its preventative benefits in T2D and associated cardiometabolic outcomes when personalized for the targeted risks, and has been justified for cost-effectiveness [7,8]. Sleep patterns and circadian rhythm, which can be modified, have also been implicated in the risk of developing long-term conditions of hypertension, CVD and T2D, and have been recently associated with the metabolic syndrome [19]. Thus, while a combined approach should always be simplified, the effects of each lifestyle component should be carefully reported. A comparison between longitudinal and prospective cohort studies showed that the simpler the intervention is, the better the long-term preventative effects are for multiple outcomes of long-term conditions. Below (Table 1), are four distinct examples showing outcomes relating to T2D glycemic control (fasting blood glucose, HbA1c, Oral glucose tolerance), hypertension (systolic and diastolic blood pressure), obesity (waist circumference, lipid profile of LDL, HDL, TG, total cholesterol) and incidence of T2D, cardiovascular disease, and mortality.

Table 1.
Recommendations based on exercise contribution within lifestyle longitudinal interventions.
2.1. Simplifying Exercise Prescription for Multiple Long-Term Conditions
It is difficult to implement physical activity guidelines for healthy adults, let alone for those with multiple long-term conditions. For example, current guidelines involve low-intensity physical activity of 150–300 min per week or intense physical activity of 75 min per week. More recently, high intensity exercise of 20 min per week was added, while twice per week of resistance exercise is also added [23,24,25]. One should also perform flexibility, balance and interval type exercise [23], or increase the physical activity duration from 150 min to 300 min per week, with at least 10 min bouts [24]. Elsewhere, some recommended performing more intense “HIIT” bouts [25]. Together, impractical advice makes it difficult to achieve adherence. In total, over 10 h weekly seems to be recommended (e.g., 5 h aerobic, 2 h or more, resistance, 3 h light exercise, flexibility, balance) [8], which makes achieving it impractical. An individualized and simplified exercise prescription approach which takes into consideration preventing multiple long-term conditions is needed.
2.2. Addressing Gaps in Prescribing Physical Activity High-Intensity Training
High intensity interval training, or HIIT, involves repeated bouts of a shorter duration exercise with a rest interval in between. HIIT as a training concept has grown in recent years from being a sport-related training to enhance elite athletes’ performance into a public health physical activity strategy prescribed for individuals with long-term conditions especially T2D [25,26,27,28]. However, such recommendation has relied on a number of studies that are acute in nature (e.g., training between one and six sessions only), which is too short of a training duration to indue long-term adaptive physiological response [26,27]. Based on this, the term “HIIT” may not be suitable in the absence of training “T” long-term adaptive response and could perhaps be replaced with a “HI”.
The historic definition of HIIT was intermittent exercise in nature and was not meant to induce long-term recovery in the athletic participants who followed such exercise method due to the performance needs of specific sports training (e.g., repeated sprints in football) [29]. Those needs required training which replicated elite sports performance intensities and were associated with enhancing sport-specific tasks and skills, and so were based on stressing the physiological systems at a higher level than that usually required to perform daily physical activity tasks by the general population. Such sports necessity is absent in individuals who are considered mostly sedentary and even more so in individuals who are living with a long-term condition such as CVD and T2D. Despite this knowledge, HIIT has continued to be promoted for managing and preventing T2D and CVD [26,30,31,32]. Examples of the postulated HIIT benefits include modulated glycemic control and mitochondrial biomarkers in those with early T2D diagnosis, following six sessions of HIIT [26], or even a single session or 1 min cycling at 90% of maximal heart rate [27]. The short term nature of those studies makes it difficult to consider them interventions that can be translated into real lifestyle settings. It has been shown that the smallest change in lifestyle, such as to the diurnal cycle or circadian rhythm, can negate any HIIT effects [33]. Therefore, inducing long-term physiological adaptive responses that are beneficial for several cardiometabolic conditions such as CVD and T2D should be the priority of an individualized exercise prescription, rather than a stiff focus on a specific high intensity or “HIIT” as a public health strategy.
In contrast to short term effects, longer-term effects of HIIT have shown contrasting benefits. High-risk groups such as women who are overweight showed no improvement in insulin sensitivity despite reduction in total and abdominal body fat percentage (BF%) following 18 sessions of HIIT [34]. In a more recent study in women with severe obesity (with total BF% = 40%), we found a similarly modest reduction in BF%, but this was combined with negative response in T2D glycemic control which showed significant elevation in both insulin and glucose following eight weeks of a typical HIIT intervention program [35]. Interestingly, the latter side-effects were also combined with increased metabolic endotoxicity, which could be perceived as a negative HIIT confounder when training individuals with obesity. However, this phenomenon of adverse metabolic response in the early to medium phase (1 session to 18 sessions equivalent to 8 weeks interventions) can be explained by the transient nature of the adaptive metabolic responses induced by HIIT, which are mitigated if long-term adherence is achieved. This suggests that ensuring long-term adherence to such an intense exercise training regime is essential, something that is difficult to achieve in high-risk populations with long-term conditions.
The lack of long-term adherence to HIIT in high-risk groups has been questioned due to concerns over inconsistent intensity definition and adverse physiological side effects especially for those with obesity or prediabetes [35,36,37]. In 411 CVD patients, HIIT was not superior to other types of lower intensity training if the isocaloric exercise protocols were compared [38]. The HIIT vs. moderate adherence records also showed a lower adherence and higher injury record in sedentary individuals with T2D [37,38]. HIIT and strength type exercise trainings have both shown several mitochondrial benefits on the proteomics and transcriptomics of young and older healthy individuals [39]. However, HIIT intervention in individuals with severe obesity can deleteriously elevate metabolic endotoxicity and augment the glucose–insulin action cycle following eight weeks of HIIT, though such adverse metabolic response to HIIT can be reversed by nutritional remedies such as simultaneous caffeine ingestion over the whole intervention period [35]. Despite a plethora of cardiovascular, respiratory and metabolic short-term benefits of HIIT, its metabolic side-effects in those with advanced or multiple long-term conditions should be taken into consideration.
Therefore, it would be premature to promote HIIT for the prevention of multiple long-term conditions. Essentially, HIIT is an already known heavy-exercise-intensity physiological domain, with an associated heavy-intensity-domain physiological responses (e.g., blood lactate concentration, oxygen uptake and respiratory quotient) that are already known in exercise physiology since the turn of the 20th Century [40]. After all, HIIT strategy is not a novel because it is simply a form of training in the heavy exercise intensity domain to induce domain-associated cardiometabolic physiological responses. Such a phenomenon is already known in exercise physiology for a century [40].
2.3. Optimizing Prevention of Multiple Conditions through Targeting Sedentary Behavior
Even minimum amounts of physical activity can be effective in preventing multiple conditions including obesity, T2D, cancer and CVD. Evidence from large meta-analyses from the EPIC study (European Prospective Investigation Into Cancer and Nutrition) has demonstrated an association between the lowest mortality risk for people with diabetes with moderate physical activity (hazard ratios were 0.60 for all-cause mortality) compared with a higher risk for the sedentary and less active individuals [41]. Specific to sedentary behavior, a dose–response relationship has been shown between sedentary behavior and all-cause, CVD, cancer mortality and T2D incidence [42]. Thus, reducing multiple long-term conditions requires addressing sedentary behavior prevention as an integral part of interventions.
Sedentary-related risks can target any lifestyle setting, whether leisure-based behaviors or workplace-based sedentary lifestyle. Thus, targeting workplace settings with interventions aimed at reducing sedentary-related cardiovascular risks through workplace screening and interventions is recommended. We have shown benefits in preventing CVD risks based on enhancing cardiorespiratory fitness, indicated by ventilatory threshold and maximal cardiorespiratory capacity, among white-collar sedentary workers based on their specific job roles and genders, and university community staff and students [43,44,45]. For example, there was a reduction in the cardiovascular and respiratory risks among sedentary university campus employees who followed a three-month intervention of moderate exercise intensity, which was individualized according to their ventilatory threshold (VT). The intervention significantly increased their both VT and its associated velocity, and enhanced [44]. Such benefits were irrespective of weight loss or blood pressure outcomes (Table 2), which is in line with large scale lifestyle interventions aimed at targeted subgroups with specific risks [44].

Table 2.
Sedentary risks reduced following an individualized exercise training intervention.
Populations with diabetes and prediabetes prevalence have reported increased sedentariness. Higher intake of fruit and vegetables, especially those high in fiber (green leafy, yellow and cruciferous vegetables), is associated with a lower risk of T2D [46]. Nonetheless, reducing sedentariness can be achieved by increasing physical activity levels or taking a combined exercise–dietary change approach.
One year interventions targeting sedentary T2D adults with poor glycemic control and reduced insulin sensitivity have shown that increased step count, measured using wrist accelerometry, can be achieved concurrently with continuous glucose monitoring sensor monitoring [47]. High-risk postmenopausal women with CVD risks have also shown enhanced microvascular endothelial activity with individualized exercise training at VT combined with a Mediterranean dietary approach based on main nine nutritional components [48]. A different physical activity approach was used in younger adults who might be at a different workplace risk, such as university students attending campus-based classes. More intense activities or “HIIT” through game sports and intense exercise sessions were tolerated by such a group, resulting in reduced body mass index and fat percentage, lowered blood pressure and higher cardiorespiratory capacity [45]. Individualized sedentary reduction and physical activity approaches are therefore effective in high-risk populations and induce significant risk-reduction benefits in a cluster of long-term conditions.
2.4. Addressing Weight and Fat Loss Prescription
Determining changes in whole body metabolism is essential in health, disease and sports performance. However, achieving weight and fat loss is often simplified by looking into anthropometric changes in BMI, defined as weight in kilograms divided by the square of height in meters. An arbitrary measure of obesity is BMI > 30 kg.m−2, which, although indicative, does not consider metabolic or vascular status or the changes in response to an intervention. It is not uncommon for a lifestyle intervention, whether exercise or diet, to induce minor or no changes in BMI, but significant metabolic and vascular benefits related to CVD and T2D outcomes [34,35,48,49]. Therefore, weight and fat loss outcomes should always consider complementary indicative measures of the individuals’ cardiometabolic profile, especially measures which combine health and fitness profiles, especially in those with multiple long-term conditions. Examples include combined measurements of gaseous exchange data of and which can be used to estimate various thresholds including VT and [43,44].
Data derived from the respiratory gas exchange ratio also allow indirect calorimetry measurements of fatty acid oxidation (FAO) and carbohydrate CHO oxidation (CHO), which provide the main fuel supply for human energy production at rest and during exercise [50,51,52,53]. Impairments in FAO or CHO are known predictors of long-term conditions such as obesity, diabetes and cardiometabolic diseases [50,51]. However, relying on respiratory based calorimetry measures may be insufficient in describing individuals’ metabolic profile, and so adding blood-based biomarkers, especially blood lactate concentration (BLC), to measure metabolism provides a more robust approach in determining metabolic sensitivity and changes in weight and fat loss outcomes and adaptations of multiple cardiometabolic systems [51,52]. Recently validated models of assessing metabolism based on lactate–carbohydrate relationship have sensitively reflected adaptive responses of multiple metabolic characteristics such as muscle fiber composition, glycogen content and activity, gender, diet, aerobic capacity and exercise intensity and duration [52,53]. This model offers an individualized characterization of whole-body metabolism which addresses the large inter-individual and intra-individual variability in fat loss assessment, which are common confounders in measuring adaptations to a lifestyle dietary, or exercise training interventions [52]. Future use of the lactate–carbohydrate predictive model in lifestyle interventions involving multiple long-term conditions merits further research.
3. Conclusions and Prospects
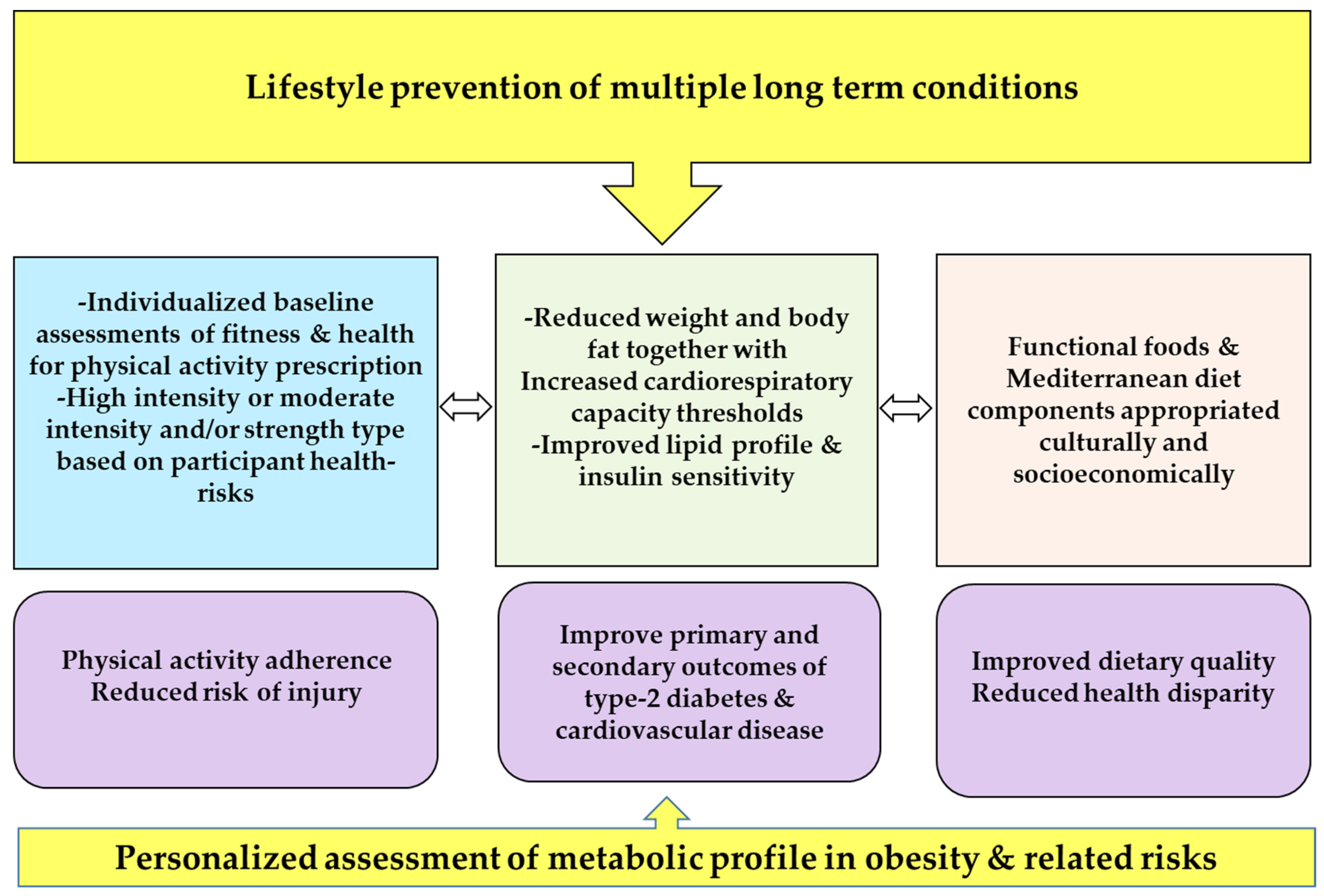
The prevalence of multiple long-term conditions is on the rise across all age groups. The majority of these conditions, including T2D and CVD, can be prevented by lifestyle exercise and nutrition interventions (Figure 1). A person centered lifestyle approach should be adopted and simplified to achieve adherence, especially when intense types of exercise such as HIIT are recommended in high-risk populations. Lifestyle interventions should integrate a component of preventing sedentariness and utilize multiple levels of assessments of both physical fitness and the adaptive metabolic, cardiovascular and respiratory responses. Lifestyle interventions in high-risk children and adolescents with obesity should go beyond achieving weight- and fat-loss outcomes, especially in those with the obesity comorbidity. Predictive models characterizing individuals’ metabolic profiles and the associated whole-body adaptive cardiometabolic responses provide a future scope for the accurate prescription of personalized lifestyle interventions.
Figure 1.
Recommendations for lifestyle prevention of multiple long-term conditions.
Funding
This research received no external funding.
Data Availability Statement
Data are available from the author on request.
Conflicts of Interest
The author declares no conflict of interest.
References
- International Diabetes Federation. Diabetes Atlas, 7th ed.; 2015. Available online: http://www.diabetesatlas.org/ (accessed on 1 April 2019).
- Rokas, N.; Vesna-Kerstin, P.; Andrea, F.; Martin, S. Multimorbidity: What do we know? What should we do? J. Comorbidity 2016, 6, 4–11. [Google Scholar]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [PubMed]
- Tuomilehto, J.; Lindström, J.; Eriksson, J.G.; Valle, T.T.; Hämäläinen, H.; Ilanne-Parikka, P.; Keinänen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Prevention of Type 2 Diabetes Mellitus by Changes in Lifestyle among Subjects with Impaired Glucose Tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, A.; Snehalatha, C.; Mary, S.; Mukesh, B.; Bhaskar, A.D.; Vijay, V.; Indian Diabetes Prevention Programme (IDPP). The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006, 49, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.-R.; Li, G.-W.; Hu, Y.-H.; Wang, J.-X.; Yang, W.-Y.; An, Z.-X.; Hu, Z.-X.; Lin, J.; Xiao, J.-Z.; Cao, H.-B.; et al. Effects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose Tolerance: The Da Qing IGT and Diabetes Study. Diabetes Care 1997, 20, 537–544. [Google Scholar] [CrossRef]
- Herman, W.H. The cost-effectiveness of diabetes prevention: Results from the Diabetes Prevention Program and the Diabetes Prevention Program Outcomes Study. Clin. Diabetes Endocrinol. 2015, 1, 9. [Google Scholar] [CrossRef]
- Alkhatib, A. Personalising Exercise and Nutrition Behaviours in Diabetes Lifestyle Prevention. Eur. Med. J. 2020, 5, 67–77. [Google Scholar] [CrossRef]
- Esposito, K.; Maiorino, M.I.; Petrizzo, M.; Bellastella, G.; Giugliano, D. The Effects of a Mediterranean Diet on the Need for Diabetes Drugs and Remission of Newly Diagnosed Type 2 Diabetes: Follow-up of a Randomized Trial. Diabetes Care 2014, 37, 1824–1830. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Bulló, M.; Estruch, R.; Ros, E.; Covas, M.-I.; Ibarrola-Jurado, N.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; et al. Prevention of Diabetes With Mediterranean Diets. Ann. Intern. Med. 2014, 160, 1–10. [Google Scholar] [CrossRef]
- Tuomilehto, J.; Schwarz, P.E. Preventing Diabetes: Early Versus Late Preventive Interventions. Diabetes Care 2016, 39, S115–S120. [Google Scholar] [CrossRef] [PubMed]
- Alkhatib, A.; Nnyanzi, L.A.; Mujuni, B.; Amanya, G.; Ibingira, C. Preventing Multimorbidity with Lifestyle Interventions in Sub-Saharan Africa: A New Challenge for Public Health in Low and Middle-Income Countries. Int. J. Environ. Res. Public Health 2021, 18, 12449. [Google Scholar] [CrossRef] [PubMed]
- Obita, G.; Alkhatib, A. Disparities in the Prevalence of Childhood Obesity-Related Comorbidities: A Systematic Review. Front. Public Health 2022, 10, 923744. [Google Scholar] [CrossRef]
- Adu, M.D.; Malabu, U.H.; Malau-Aduli, A.E.O.; Malau-Aduli, B.S. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLoS ONE 2019, 14, e0217771. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. A Systematic Review and Metaanalysis Assessing the Effectiveness of Pragmatic Lifestyle Interventions for the Prevention of type 2 Diabetes Mellitus in Routine Practice. 2015. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/733053/PHE_Evidence_Review_of_diabetes_prevention_programmes-_FINAL.pdf (accessed on 1 June 2019).
- Dunkley, A.J.; Bodicoat, D.H.; Greaves, C.J.; Russell, C.; Yates, T.; Davies, M.J.; Khunti, K. Diabetes Prevention in the Real World: Effectiveness of Pragmatic Lifestyle Interventions for the Prevention of Type 2 Diabetes and of the Impact of Adherence to Guideline Recommendations: A systematic review and meta-analysis. Diabetes Care 2014, 37, 922–933. [Google Scholar] [CrossRef] [PubMed]
- Slentz, C.A.; Bateman, L.A.; Willis, L.H.; Granville, E.O.; Piner, L.W.; Samsa, G.P.; Setji, T.L.; Muehlbauer, M.J.; Huffman, K.M.; Bales, C.W.; et al. Effects of exercise training alone vs a combined exercise and nutritional lifestyle intervention on glucose homeostasis in prediabetic individuals: A randomised controlled trial. Diabetologia 2016, 59, 2088–2098. [Google Scholar] [CrossRef] [PubMed]
- Zimmet, P.; Alberti, K.G.M.M.; Stern, N.; Bilu, C.; El-Osta, A.; Einat, H.; Kronfeld-Schor, N. The Circadian Syndrome: Is the Metabolic Syndrome and much more! J. Intern. Med. 2019, 286, 181–191. [Google Scholar] [CrossRef]
- Lamb, M.J.E.; Westgate, K.; Brage, S.; Ekelund, U.; Long, G.H.; Griffin, S.J.; Simmons, R.K.; Cooper, A.J.M.; ADDITION-Plus study team. Prospective associations between sedentary time, physical activity, fitness and cardiometabolic risk factors in people with type 2 diabetes. Diabetologia 2016, 59, 110–120. [Google Scholar] [CrossRef]
- The Look AHEAD Research Group; Wing, R.R.; Bolin, P.; Brancati, F.L.; Bray, G.A.; Clark, J.M.; Coday, M.; Crow, R.S.; Curtis, J.M.; Egan, C.M.; et al. Cardiovascular Effects of Intensive Lifestyle Intervention in Type 2 Diabetes. N. Engl. J. Med. 2013, 369, 145–154. [Google Scholar] [CrossRef]
- Bancks, M.P.; Chen, H.; Balasubramanyam, A.; Bertoni, A.G.; Espeland, M.A.; Kahn, S.E.; Pilla, S.; Vaughan, E.; Wagenknecht, L.E. The Look AHEAD Research Group Type 2 Diabetes Subgroups, Risk for Complications, and Differential Effects Due to an Intensive Lifestyle Intervention. Diabetes Care 2021, 44, 1203–1210. [Google Scholar] [CrossRef]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef] [PubMed]
- World Health organization (WHO). Global Report on Physical Activity. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 31 January 2023).
- Diabetes UK, Living with Diabetes, High-Intensity Interval Training. Available online: https://www.diabetes.co.uk/high-intensity-interval-training.html (accessed on 1 April 2019).
- Little, J.P.; Gillen, J.B.; Percival, M.E.; Safdar, A.; Tarnopolsky, M.A.; Punthakee, Z.; Jung, M.E.; Gibala, M.J. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J. Appl. Physiol. 2011, 111, 1554–1560. [Google Scholar] [CrossRef] [PubMed]
- Shaban, N.; Kenno, K.A.; Milne, K.J. The effects of a 2 week modified high intensity interval training program on the homeostatic model of insulin resistance (HOMA-IR) in adults with type 2 diabetes. J. Sports Med. Phys. Fit. 2014, 54, 203–209. [Google Scholar]
- Laursen, P.B.; Jenkins, D.G. The scientific basis for high-intensity interval training: Optimising training programmes and maximising performance in highly trained endurance athletes. Sports Med. 2002, 32, 53–73. [Google Scholar] [CrossRef]
- Daniels, J.; Scardina, N. Interval Training and Performance. Sports Med. 1984, 1, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Gibala, M.J.; McGee, S. Metabolic Adaptations to Short-term High-Intensity Interval Training: A little pain for a lot of gain? Exerc. Sport Sci. Rev. 2008, 36, 58–63. [Google Scholar] [CrossRef]
- Trapp, E.G.; Chisholm, D.J.; Freund, J.; Boutcher, S.H. The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int. J. Obes. 2008, 32, 684–691. [Google Scholar] [CrossRef]
- Francois, M.E.; Little, J.P. Effectiveness and Safety of High-Intensity Interval Training in Patients With Type 2 Diabetes. Diabetes Spectr. 2015, 28, 39–44. [Google Scholar] [CrossRef]
- Savikj, M.; Gabriel, B.M.; Alm, P.S.; Smith, J.; Caidahl, K.; Björnholm, M.; Fritz, T.; Krook, A.; Zierath, J.R.; Wallberg-Henriksson, H. Afternoon exercise is more efficacious than morning exercise at improving blood glucose levels in individuals with type 2 diabetes: A randomised crossover trial. Diabetologia 2019, 62, 233–237. [Google Scholar] [CrossRef]
- Gillen, J.B.; Percival, M.E.; Ludzki, A.; Tarnopolsky, M.A.; Gibala, M.J. Interval training in the fed or fasted state improves body composition and muscle oxidative capacity in overweight women. Obesity 2013, 21, 2249–2255. [Google Scholar] [CrossRef]
- Alkhatib, A.; Hsieh, M.-J.; Kuo, C.-H.; Hou, C.-W. Caffeine Optimizes HIIT Benefits on Obesity-associated Metabolic Adversity in Women. Med. Sci. Sports Exerc. 2020, 52, 1793–1800. [Google Scholar] [CrossRef]
- Biddle, S.J.; Batterham, A.M. High-intensity interval exercise training for public health: A big HIT or shall we HIT it on the head? Int. J. Behav. Nutr. Phys. Act. 2015, 12, 95. [Google Scholar] [CrossRef]
- Neto, M.G.; Durães, A.R.; Conceição, L.S.R.; Saquetto, M.B.; Ellingsen, Ø.; Carvalho, V. High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with heart failure with reduced ejection fraction: A systematic review and meta-analysis. Int. J. Cardiol. 2018, 261, 134–141. [Google Scholar] [CrossRef]
- Lunt, H.; Draper, N.; Marshall, H.C.; Logan, F.J.; Hamlin, M.J.; Shearman, J.P.; Cotter, J.D.; Kimber, N.E.; Blackwell, G.; Frampton, C.M.A. High Intensity Interval Training in a Real World Setting: A Randomized Controlled Feasibility Study in Overweight Inactive Adults, Measuring Change in Maximal Oxygen Uptake. PLoS ONE 2014, 9, e83256. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.M.; Dasari, S.; Konopka, A.R.; Johnson, M.L.; Manjunatha, S.; Esponda, R.R.; Carter, R.E.; Lanza, I.R.; Nair, K.S. Enhanced protein translation underlies improved metabolic and physical adaptations to different exercise training modes in young and old humans. Cell Metab. 2017, 25, 581–592. [Google Scholar] [CrossRef]
- Hill, A.V.; Furusawa, K.; Long, C.N.H.; Lupton, H. Muscular exercise, lactic acid and the supply and utilisation of oxygen. Parts VII–VIII. Proc. R. Soc. London. Ser. B Boil. Sci. 1924, 97, 155–176. [Google Scholar] [CrossRef]
- Sluik, D.; Buijsse, B.; Muckelbauer, R.; Kaaks, R.; Teucher, B.; Johnsen, N.F.; Tjønneland, A.; Overvad, K.; Østergaard, J.N.; Amiano, P.; et al. Physical Activity and Mortality in Individuals With Diabetes Mellitus: A Prospective Study and Meta-analysis. Arch Intern. Med. 2012, 172, 1285–1295. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.; McNamara, E.; Tainio, M.; De Sá, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef]
- Alkhatib, A. Sedentary Risk Factors across Genders and Job Roles within a University Campus Workplace: Preliminary Study. J. Occup. Health 2013, 55, 218–224. [Google Scholar] [CrossRef]
- Alkhatib, A. High prevalence of sedentary risk factors amongst university employees and potential health benefits of campus workplace exercise intervention. Work 2015, 52, 589–595. [Google Scholar] [CrossRef]
- Kneffel, Z.; Goebel, R.; Alkhatib, A. Cardiovascular Risk Factors and their Responses to a 10 Weeks Training Program in Young Qatari Adults. Obes. Res. Open J. 2015, 2, 57–63. [Google Scholar] [CrossRef]
- Wang, P.-Y.; Fang, J.-C.; Gao, Z.-H.; Zhang, C.; Xie, S.-Y. Higher intake of fruits, vegetables or their fiber reduces the risk of type 2 diabetes: A meta-analysis. J. Diabetes Investig. 2016, 7, 56–69. [Google Scholar] [CrossRef] [PubMed]
- Fritschi, C.; Park, H.; Richardson, A.; Park, C.; Collins, E.G.; Mermelstein, R.; Riesche, L.; Quinn, L. Association Between Daily Time Spent in Sedentary Behavior and Duration of Hyperglycemia in Type 2 Diabetes. Biol. Res. Nurs. 2016, 18, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Alkhatib, A.; Klonizakis, M. Effects of Exercise Training and Mediterranean Diet on Reducing Post-Menopausal Vascular Risk. Clin. Hemorheol. Microcirc. 2014, 57, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Alkhatib, A.; Tsang, C.; Tiss, A.; Bahorun, T.; Arefanian, H.; Barake, R.; Khadir, A.; Tuomilehto, J. Functional Foods and Lifestyle Approaches for Diabetes Prevention and Management. Nutrients 2017, 9, 1310. [Google Scholar] [CrossRef] [PubMed]
- Jeukendrup, A.E.; Wallis, G.A. Measurement of Substrate Oxidation During Exercise by Means of Gas Exchange Measurements. Int. J. Sports Med. 2005, 26, S28–S37. [Google Scholar] [CrossRef]
- Fernández-Verdejo, R.; Bajpeyi, S.; Ravussin, E.; Galgani, J.E. Metabolic flexibility to lipid availability during exercise is enhanced in individuals with high insulin sensitivity. Am. J. Physiol. Endocrinol. Metab. 2018, 315, E715–E722. [Google Scholar] [CrossRef]
- Alkhatib, A. Maximal Fat Metabolism Explained by Lactate-Carbohydrate Model. Physiologia 2022, 2, 121–131. [Google Scholar] [CrossRef]
- Hargreaves, M.; Spriet, L.L. Skeletal muscle energy metabolism during exercise. Nat. Metab. 2020, 2, 817–828. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).