Definition
Synaptosomes are subcellular components isolated from nerve terminations that can be prepared by homogenizing brain tissue in isotonic sucrose solution followed by appropriate centrifugation. Their preparation technique has a long history since synaptosomes were first isolated from nerve endings and described by Gray and Whittaker in 1962. The preparation of synaptosomes produces presynaptic boutons alone or in combination with fragments of postsynaptic membranes. Interestingly, synaptosomes contain organelles and vesicles that express native channels, receptors, and transporters. At 37 °C, these isolated nerve endings are metabolically active and synthesize and release neurotransmitters. They are actively used to investigate neurotransmission, its actors, and the mechanisms of neurotransmitter release. To date, many functional and non-functional applications of synaptosomes have been documented. Due to their versatility, synaptosomes have been actively used to study neuroinflammatory processes.
1. Introduction
Neuroinflammation is a reaction that involves all cells present in the central nervous system (CNS), including neurons, macroglia, and microglia [1,2,3,4]. Immune responses can be beneficial or harmful to the brain, depending on the degree to which they are activated. Inflammation is mediated by the production of cytokines such as interleukin IL-1 and IL-6, TNF-α and TGF-β [5], chemokines, reactive oxygen species, and second messengers [6]. Neuro-inflammatory reactions have immunological, physiological, biochemical, and psychological effects [2]. Additionally, neuroinflammation depends on several conditions (context, duration, and primary stimulus) [7] and can be supported by mechanisms at the synaptic level [8,9,10]. Accordingly, TNF-α is involved in an acute phase of inflammation but is also responsible for several physiological functions and supports synaptic connection [1]. However, uncontrolled expression of TNF-α could lead to synaptic loss and glutamatergic toxicity through modulation of the glutamate receptor [6]. Glutamate release and synaptic plasticity could be inhibited by IL-6 [7]. Therefore, the study of synapses became an important task in several neurodegenerative diseases characterized by high levels of neuroinflammation [11]. There are several models for studying synapses, but one that is largely used is synaptosomal preparation [11,12,13,14].
Synaptosomes are a convenient tool for neurochemical and electrophysiological studies due to the preservation of enzymatic and metabolic activities, as well as being an outstanding research tool for understanding the mechanisms of synaptic dysfunction [15,16,17,18,19,20] (Figure 1). The contribution of ROS to synaptic dysfunction in AD pathogenesis was investigated through synaptosomes from cortices of APP/PS1 mice, observing an increase in septin-3, septin-5, and C1q accumulation [21]. Consequently, an increase in SUMO-1ylation (small ubiquitin-like modifier), which was also present in human AD brains, was observed in cortical synaptosomes from Tg2576 mice. Marcelli and colleagues have shown that increased SUMO-1ylation contributes to the development of synaptic dysfunction in AD [22]. Synaptosomes can be easily prepared using the standard procedure [12]; once the tissue is collected, it is homogenized in 0.32 M sucrose and centrifuged. After the first centrifugation, the supernatant is further centrifuged to obtain the crude synaptosome pellet (P2) [23,24]. In case a higher grade of purity is requested, the samples could be obtained by density gradient (Percoll, Ficoll, or sucrose) centrifugation [25,26,27,28].
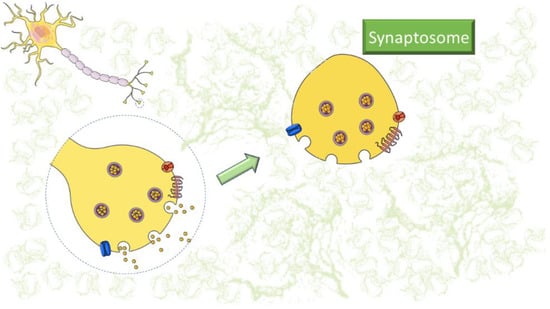
Figure 1.
Representative image of synaptosomes. The figure was partly generated using Servier Medical Art, provided by Servier, licensed under a Creative Commons Attribution 3.0 unported license (https://smart.servier.com/, accessed on 7 February 2023).
Furthermore, synaptosomes could be prepared from post-mortem human brain tissue and used to study disease pathogenesis and neurotransmitter synthesis and release in the brain of patients [15,29]. Several pathologies, such as Huntington’s disease (HD) [30], Parkinson’s disease (PD) [26,31], Alzheimer’s disease (AD) [32,33,34], and amyotrophic lateral sclerosis (ALS) [35], have been studied monitoring synaptic dysfunction through synaptosomes [36]. Additionally, synaptosomes have been observed to undergo functional changes upon acute exposure to receptor ligands/enzyme modulators in vitro. These changes persist after removing the triggering agents, but they can also adapt to and maintain the structure of the tissue of origin chronically exposed to chemicals [37].
Using the entrapping technique, membrane-impermeant agents of different sizes present in the homogenization medium could be internalized for studying intracellular mechanisms [38,39,40]. Recently, synaptosomes were described to release exosomes and extracellular vesicles able to participate in physiological and pathological neurotransmission [41].
This “Entry” paper will briefly summarize the knowledge on the use of synaptosomes for studying neuroinflammation markers (Table 1). In particular, researchers will analyze methods applied to synaptosomes to highlight neuroinflammatory parameters considering mature acquisitions and recent publications.

Table 1.
Summarized overview of the techniques, diseases, and neuroinflammation markers described in this entry.
2. Synaptosomes Applications
2.1. Synaptosomes and Western Blot Analysis
Western blot (WB) analysis is a common laboratory step to study synaptosomal proteins, newly synthesized and misfolded [29], the formation of protein complexes [42], and the detection of autoimmune diseases [73]. Its application in the characterization of synaptosomes or synaptosomal proteins is an established practice in studies related to neuroinflammation [74,75]. This method allows us to easily analyze the presence and amount of specific proteins at the synaptic level [41,76].
Moreover, synaptosomes enriched for synaptic vesicles, synaptic plasma membrane, and synaptic cytosol could be obtained by hypotonic lysis and ultracentrifugation [28]. Biochemical-enrichment analysis, electron microscopy, and WB could be used to confirm the purification of the obtained fractions [28,77,78].
Several biomarkers have been studied using synaptosomes as a protein source. For example, in 2022, Wang and co-workers demonstrated the importance of calcium-dependent cytosolic phospholipase A2 (cPLA2) activation in neuroinflammation and oxidative stress associated with ApoE4 [43]. The activation of cPLA2 is elevated within AD brain plaques, and its activity is regulated by a mitogen-activated protein kinase (MAPK). RTP801/REDD1 is a stress-related protein that could trigger neuronal death. Its involvement has been observed in several neurodegenerative diseases such as AD, HD [79], and PD [80]. Recently, the upregulation of RTP801/REDD1 was linked to neuroinflammation in AD [44]. Pérez-Sisqués and colleagues investigated the role of RTP801 by analyzing the hippocampal synaptosomes obtained from 5xFAD mice (model of Amyloid-β deposition) and the entorhinal cortex from rTg4510 mice (model of tauopathy). Moreover, in this study, human post-mortem AD samples were examined. The researchers confirmed by WB analysis that the levels of RTP801 were higher in both experimental models than in wild-type mice. As previously reported, the use of human tissue to prepare synaptosomes is an important translational paradigm in studies related to neuroinflammation [15,45,81].
Western blot analysis of synaptosomes is also able to show synaptic synthetization of biomarkers such as the amyloid precursor protein (APP) [46]. Cefaliello et al. demonstrated in TgCRND8 mice that APP is synaptically synthesized at the pre-plaque stage, underlining that, in this stage, an increased pro-inflammatory marker such as tumor necrosis factor-α (TNF-α) and an altered redox state are already detectable in synaptosomes through Western blot. The combination of WB and synaptosomes is actively used in the analysis of the gut–brain relationship [47,82]. Several factors could contribute to the neuroinflammatory process; one is a high-fat diet (HFD). HFD-induced neuroinflammation is known to affect BDNF-related pathways in several regions of the brain. BDNF has a pivotal role in brain physiology and pathology. Cavaliere and colleagues have evaluated neuroinflammation in a mouse model of diet-induced obesity with particular attention on the BDNF pathway [62]. Their Western blot results showed that BDNF expression in the synaptosomal fraction of HFD mice decreased significantly compared to controls. Notably, the decrease in the synaptosomal fraction was greater than in the homogenate fraction. The researchers also observed that in synaptosomes, where CREB regulates BDNF gene transcription, the level of CREB phosphorylation was significantly reduced by HFD. Therefore, these results confirm that the neuroinflammation induced by HFD has a substantial effect on the molecular plasticity pathways situated at the synaptic level.
In a similar study with HFD mice, the researchers found that the disruption of hippocampal neurogenesis is driven by the β2-adrenergic receptor-dependent induction of thioredoxin-1 and BDNF [63]. In the dentate gyrus (DG) of the hippocampus, the treadmill exercise inhibited the microglia activation, expression of pro-inflammatory cytokines (TNF-α and IL-1β), and NF-κB activity. The reduction in these parameters was observed through Western blot analysis.
The trigger of neuroinflammation might also be an external factor, such as in sepsis-associated encephalopathy (SAE), a response to pathogen-induced systemic inflammation [59]. A WB and synaptosomes combination can be used to validate an experimental protocol considering, for example, age influences. Two days of consecutive injections of LPS derived from Salmonella enterica or E. coli in middle-aged mice (14–16 months) and young mice (2 months) induced an experimental systemic inflammation. By analyzing the same amount of synaptosome proteins, it was shown that peripheral injections of different LPS serotypes induced different levels of neuroinflammation at 7 and 63 dpi. Manabe and co-workers show a low-grade neuroinflammation present at 7 dpi in middle-aged mice treated with E. coli. In these animals, the CXCL1 levels were significantly higher and even at 63 dpi IL-6 remained elevated. Interestingly, in young animals, at 1 dpi was observed a strong inflammatory response (IFN-γ, IL-1β, IL-10, and TNF-α cytokines), but it was quickly resolved at 7 dpi. In the proposed experimental protocol, all these results underlined that E. coli LPS injection could induce a more sustained neuroinflammation in the brains of older animals than the injection of Salmonella LPS.
An imbalance between inhibitory and excitatory neural activity can lead to seizures and neuronal damage. Several natural compounds, particularly gastrodin from Gastrodia elata, could act on NMDA receptors, consequently achieving neuroprotective effects by preventing NMDA excitotoxicity. This natural compound also has an anti-inflammatory, antiapoptotic, and antioxidant effect [57]. Inflammation and alteration in glutamate neurotransmission contribute to the pathophysiology of several neurodegenerative disorders. However, evidence suggests that N-arachidonoylphenolamine (AM404), a modulator of the cannabinoid system and a metabolite of paracetamol, modulates inflammation and has neuroprotective effects. Pre-treatment with AM404 statistically prevented NMDA-induced IL-1β expression and tended to decrease COX-2 proteins, as shown by Western blot analysis. Levels of the other cytokines, mPGES-1 and iNOS, were not affected by AM404. In addition, AM404 significantly reduced NMDA-induced cell death [55].
2.2. Synaptosomes in Flow Cytometry
Flow cytometric investigation of isolated synaptosomes represents an interesting tool to study synaptic engagement during neuroinflammation, but only a few studies have utilized this approach to assess it [23,81,83,84]. The reason is probably the risk of technical artifacts due to the formation of aggregates. In this regard, Hobson and Sims have performed a critical analysis of synaptosomes in flow cytometry [24]. This paper is probably the most representative example of a synaptosome bias analysis using this technique. The authors described some methods able to minimize the effects of coincidence and aggregation during target detection. One of the most used combinations for the evaluation of neurodegenerative signs in synaptosomes is Annexin-V/Calcein-AM labeling, which allows us to identify early apoptotic and viable particles, respectively [85]. This double staining was successfully applied to investigate synaptic alterations in the EAE mouse model [86], exosomal tau released from Alzheimer’s disease synapses in the presence of beta-amyloid [29], and the synaptotoxicity of the anti-aggregative peptide KLVFF [40]. The advantage of flow cytometry over conventional WB allows the researcher to focus specifically on intact synapses, resulting in high sensitivity with low sample material requirements. In addition, high-throughput acquisition allows the analysis of different markers from the same sample of synaptosomes [61]. It is interesting to note that specific markers for different neuronal populations, such as antibodies for vesicular transporters, can be used to focus the evaluation [87].
Flow cytometry quantified the low-density lipoprotein receptor (LDLR) and ApoE receptor LDLR-related protein 1 (LRP1) in synaptosomes [42], revealing up-regulation of LRP1 in the early and late stages of AD. LDLR and LRP1 contribute to beta-amyloid (Aβ) clearance; this pathway is operated in neurons, astrocytes, and microglia. Enhanced Aβ accumulation driven by ApoE4 has effects on neuroinflammation in the neuronal-synaptic compartment in AD [88].
During the progression of AD, the accumulation of toxic oligomers of beta-amyloid (AβO) and tau (TauO) occurs in the brain [45]. Using synaptosomes isolated from the hippocampus (HP) and frontal cortex (FC) of both mice and post-mortem cognitively intact elderly human brains, Marcatti et al. analyzed by flow cytometry the synaptic binding dynamics of both TauO and AβO. They showed that higher concentrations of TauO effectively displace AβO, becoming the prevalent synaptic-associated species. In contrast, high concentrations of AβO facilitate synaptic TauO recruitment. Due to the excessive accumulation of cytotoxic amyloid oligomers, Györffy et al. studied synaptosomes from an amyloidogenic mouse model of AD (APP/PS1) [21] and investigated the implications of complement (C1q) using flow cytometry. The previously demonstrated activation of local apoptotic-like mechanisms and subsequent synaptic C1q deposition was confirmed by the neurotoxic Aβ accumulation, which induces septin-related alterations and mitochondrial impairment. Flow cytometry could be used to study the progression of pathology-associated proteins and also the loss of specific dopaminergic nerve endings in Alzheimer’s disease and Lewy body disease (LBD) [81]. The interaction of C1q with neuronal pentraxins (NPs) has been investigated [48]. Additionally, growing evidence suggests that NPs may be promising cerebrospinal fluid (CSF) and blood biomarkers for early Alzheimer’s disease. Furthermore, in Alzheimer’s disease, an Aβ-induced rise in the expression of NP1 has been associated with neuronal toxicity. In post-mortem human AD brain samples, however, NP2 is downregulated. A high percentage of co-localization of the C1q tag with NP1/2 on synaptosomes was observed by flow cytometric analysis. These data suggest that NP1 is involved in the selective elimination of C1q-tagged synapses by microglia and that NPs play a regulatory role in C1q synaptic function.
Viral infections can affect the brain. Influenza A virus (IAV) infection causes a prolonged peripheral immune response, followed by a transient disruption of the blood–brain barrier [61]. Flow cytometric analysis uncovered subtle alterations in the activation status of microglial cells. The study highlighted a significant reduction in VGLUT1 in excitatory presynaptic terminals. It should be noted that systemic IAV-induced inflammation affects the central nervous system, causing and promoting neuronal changes.
Recently, using machine intelligence, a new candidate agonist of SH2-containing 5′ inositol phosphatase 1 (SHIP1) was identified, namely K306, which shows selectivity for SHIP1 [89]. Pedicone et al. observed that in macrophages or microglia, K306 could suppress the activation of inflammatory cytokines and iNOS, and, in addition, it reduces TNF-α production in vivo. Through flow cytometry, phagolysosomal degradation of synaptosomes and dead neurons by microglia was shown.
2.3. Synaptosomes and Neurotransmitter Release
Neurotransmitters are key factors in the regulation of neuroinflammation pathways [90]. Historically, synaptosomes have been used to determine changes in neurotransmitter release. Both exocytotic and carrier-mediated release can be efficiently documented using isolated nerve endings [64,91,92,93]. Furthermore, it is possible to functionally analyze all targets present in isolated terminals, considering their regulation on the release of neurotransmitters. A cultural revolution occurred when the immune system became involved in physiological processes, establishing that neuroinflammatory mediators can also modulate cognitive and behavioral mechanisms [94,95]. In the last 20 years, the Roth and Pittaluga groups studied the neurotransmission imbalance in multiple sclerosis (MS) using EAE synaptosomes [65,66,67]. This alteration is coupled either with glutamate and noradrenaline derangements or with overexpression of CCL5, TNF-α, and IL-17. Moreover, Vilcaes et al. have found that only the Ca2+-dependent glutamate release in rat cortical synaptosomes induced by KCl and 4-aminopyridine was considerably reduced at the acute stage of the disease, but not the Ca2+-independent glutamate [68]. In this experimental model, it has been found that a phase-dependent increase in IL-2 and its receptor, IL-1β and IFN-γ, IL-4, and TNF-α indicates that these cytokines are involved in inducing and sustaining brain inflammation in EAE animals. Accordingly, the course of MS in patients is sustained by pro-inflammatory cytokines such as IL-2, IFN-γ, IL-1β, and TNF-α. There was also a marked reduction in GABAergic modulation of glutamate release from synaptosomes isolated from EAE rats during the acute phase of the disease [69]. It has been observed that prostaglandin E2 significantly increases endogenous glutamate and aspartate release in synaptosomes of the rat spinal cord [96] and that the resulting hyperalgesia could be alleviated by the use of non-steroidal anti-inflammatory drugs (NSAID). Anti-inflammatory drugs, such as ibuprofen and aspirin, have increased dopamine transport activity in synaptosomes, while they have shown less intensity in serotonin-transport activity [97]. An analogous overview could be made by studying the ALS genetic mouse model. Indeed, Bonanno and colleagues described in several papers the neurotransmitters’ unbalance in G93A mice [71]. This mouse presents a neuro-muscular pathology with a high involvement of neuroinflammatory processes [72].
Although several cytokines exert an inflammatory effect, IL-6 has been shown to be neuroprotective against ischaemic lesions and glutamate excitotoxicity. In addition, IL-6 has antagonized glutamate release and reduced excitation propagation in rat cortical synaptosomes [98]. The effect of cytokines could be mediated by the activation of protein phosphorylation processes, thereby activating the STAT3, mitogen-activated protein kinase ERK (MAPK/ERK), and stress-associated protein kinase/c-Jun NH2-terminal kinase (SAPK/JNK) pathways. In fact, the results have shown that IL-6 induced a decrease in MAPK/ERK activation. This was concomitant with the stimulation of STAT3 phosphorylation. On the other hand, no involvement of the JNK/SAPK pathway was observed after the activation of IL6.
2.4. Synaptosome and Proteomic Analysis
Recently, different synaptosome isolation methods were investigated, and it was demonstrated that different preparations are suitable for several research directions [25]. During the isolation process, the possibility of contamination must be considered, especially with mitochondrial and glial structures. Synaptosome enrichment can be detected by immunoreactivity for the synapse-specific marker proteins synaptophysin and Psd-95. For proteomic analysis, synaptosomes are ideal targets. The simultaneous qualitative and quantitative analysis of thousands of proteins is possible thanks to recently available separation and protein-detection techniques, which can overcome the reduced complexity of the organelle. These proteins shape the structural and functional properties of the synapse. In addition, using the protein database, synaptic proteins were compared among the different isolations, selecting the suitable one. Interestingly, synaptosomes were proposed to be a mitochondrial transport system that could be used to treat many brain disorders associated with mitochondrial dysfunction [16]. The proteomic approach has demonstrated the presence of proteins that participate in machinery for membrane fusion, including SNARE and SNAP-25 [99]. Moreover, mitochondrial dysfunction plays a crucial role in several neurodegenerative diseases and neuroinflammation due to its involvement in the apoptotic process and ROS production [49].
Wijasa et al. have identified S-nitrosylation as a possible biomarker for neuroinflammation and AD [50]. The generation of NO could be considered a signature of neuroinflammatory brain activity. S-nitrosylation (SNO) of cysteine residues is one of the key biological modifications induced by NO [100]. Consequently, mouse and human synaptosomes were characterized. Synaptosomal proteins were purified from APP/PS1 mice and compared with wild-type and NOS2−/− mice, along with human control, mild cognitive impairment, and Alzheimer’s brain tissue. Proteomic analysis has identified a significant increase in SNO proteins compared to the control. Some of them were modified by NO in response to cerebral amyloidosis [101]. Furthermore, a correlation was observed between age and protein genotype increase; pathological aging led to SNO increase and is related to beta-amyloid deposition and neuroinflammation [102].
Proteomic analysis was also carried out to better understand the progression of PD, which is described by the depletion of neuromelanin-containing dopaminergic neurons within the substantia nigra pars compacta (SNpc) [26]. Plum et al. compared synaptosomes from individuals in advanced stages of PD and controls. Differential analysis between controls and PD subjects indicated that the CD9 antigen was the only protein expressed in PD synaptosomes when compared to controls, while 14 proteins were expressed at a reduced level in PD. All of these proteins are integral parts of biosynthetic pathways. Most of these proteins had not been reported in PD before. Thus, these protein alterations support the hypothesis of impaired mitochondrial function in PD, suggesting an alteration in mitochondrial translation within synaptosomes [103].
Recently, mitochondrial dysfunction has been implicated in the pathogenesis of impaired synaptic function in Unverricht–Lundborg progressive myoclonus epilepsy (EPM1) [58]. EPM1 is a neurodegenerative disorder that occurs as a result of loss-of-function mutations in the cystatin B (CSTB) gene; its deficiency alters GABAergic signaling and causes early neuroinflammation followed by progressive neurodegeneration in the brain of a mouse model, leading to progressive myoclonus and ataxia [104]. Hence, proteomic analysis has highlighted that CSTB−/− synaptosomes are quantitatively and qualitatively distinct. These synaptosomes differ in mitochondrial, ribosomal, and intracellular transport proteins [58,105]. Furthermore, early mitochondrial dysfunction could link ROS signaling and GABAergic inhibition. Therefore, the hypothesis of the role of CSTB in the pathophysiology of synaptic dysfunction and EPM1 was confirmed by the Gorski group.
2.5. Synaptosome and Confocal Microscopy
Confocal microscopy is an advanced microscopy technique. The principal advantage of confocal microscopy over other types of microscopies is its ability to block out-of-focus light from illuminated specimens using pinholes. It is often used with fluorescence optics to produce high-resolution, high-contrast images. Unlike optical microscopes, confocal microscopes use a focused laser beam to scan the entire sample surface at different z-planes. These microscopes are, therefore, ideal for examining thick samples such as biofilms [106], tissue slices [63], and synaptosomes [27]. Using confocal microscopy, it was possible to observe changes in Ca2+ in the cytoplasm and in the endoplasmic reticulum (ER) associated with neuroinflammation in SAE [60]. It is recommended to use fluorescent markers for easy visualization of pre- and postsynaptic terminals of glutamatergic synaptosomes using confocal microscopy. The link between tauopathy and neuroinflammation in AD has been widely demonstrated. Largo-Barrientos and colleagues have also investigated the interaction between Synaptogyrin-3 and tau protein and their involvement in synaptic loss and cognitive decline [51]. The synaptosomes isolated from wild-type and Tau P301S mice were both positive for Synaptoporin and Synaptogyrin-3, but only those from Tau P301S mice were positively stained for Tau. The co-localization of Synaptogyrin-3 and pathogenic tau in synaptosomes of 6-month-old Tau P301S mice confirms the role of these proteins in pathophysiology. In addition, reducing the expression of synaptogyrin-3 has been shown to prevent tau-induced synaptic loss and cognitive decline. AβO and TauO were observed in cortical synaptosomes of elderly patients [45], while plaque-contacted membrane surfaces appeared to lack GABAergic perisomatic synapses, possibly leading to hyperactivity of plaque-contacted neurons [52]. On the other hand, the mice model of AD confocal microscopy has confirmed the presence of the C1q protein in cortical synaptosomes [107]. Similarly, ALS is characterized by neuroinflammation and mitochondrial dysfunction. Therefore, MAP2, GFAP, and LDH were investigated in spinal cord synaptosomes obtained from SOD1G93A mice [71]. MAP2 is a selective marker for neurons, GFAP is a selective marker for astrocytes, and LDH is an enzyme that is localized in the cytosol. LDH-positive particles are thought to represent resealed synaptosomes rather than membrane debris. Synaptosomes at different stages of pathology were characterized. Synaptic structural changes and enhanced glucose catabolism were observed during disease progression [108].
3. Conclusions and Prospects
Synaptosomes are a consolidated preparation in the field of neuroinflammation. Several research groups around the world have contributed to the improvement of their preparation and characterization. Overall, in this entry, researchers have highlighted how a variety of technologies can be adapted to better understand the role of synaptic proteins in inflammatory processes in different neurological diseases using synaptosomes. In this entry, researchers have reviewed some techniques that led to consolidated protocols for assessing neuroinflammatory aspects. It is evident that synaptosomes are a powerful tool with clear advantages such as simple preparation, native targets and biomarkers, and workability, but also some limitations. Briefly, researchers can summarize structural, experimental, and ethical disadvantages. In the first group, there was a small size, lack of structures and signals (i.e., nucleus), the possible presence of postsynaptic membranes, particle pooling, biophase, and survival time. Secondly, synaptosomes can aggregate easily, and some of the compounds used in their protocols, such as Percoll and Ficoll, can exacerbate this tendency. This aspect is crucial when the experimental protocol involves the use of fluorescent agents. Finally, the ethical problems stem from the use of animals, which are still fundamental to neuroscientists. However, in some cases, these limitations have already been effectively overcome, as in the case of introducing perfusion to reduce the biophase or using frozen tissue to reduce the number of animals. All of these considerations, centered on the neuroinflammation tasks, describe the importance of synaptosomes and the need for continuous refinement of their protocols.
Author Contributions
Conceptualization, H.T.; writing—original draft preparation, H.T. and M.G.; supervision, M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Figure 1 was partly generated using Servier Medical Art, provided by Servier, licensed under a Creative Commons Attribution 3.0 Unported License. (https://smart.servier.com/, accessed on 7 February 2023).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rauf, A.; Badoni, H.; Abu-Izneid, T.; Olatunde, A.; Rahman, M.M.; Painuli, S.; Semwal, P.; Wilairatana, P.; Mubarak, M.S. Neuroinflammatory Markers: Key Indicators in the Pathology of Neurodegenerative Diseases. Molecules 2022, 27, 3194. [Google Scholar] [CrossRef]
- Lyman, M.; Lloyd, D.G.; Ji, X.; Vizcaychipi, M.P.; Ma, D. Neuroinflammation: The role and consequences. Neurosci. Res. 2014, 79, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Xanthos, D.N.; Sandkühler, J. Neurogenic neuroinflammation: Inflammatory CNS reactions in response to neuronal activity. Nat. Rev. Neurosci. 2014, 15, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Ji, R.-R.; Xu, Z.-Z.; Gao, Y.-J. Emerging targets in neuroinflammation-driven chronic pain. Nat. Rev. Drug Discov. 2014, 13, 533–548. [Google Scholar] [CrossRef] [PubMed]
- Angelucci, F.; Cechova, K.; Amlerova, J.; Hort, J. Antibiotics, gut microbiota, and Alzheimer’s disease. J. Neuroinflammation 2019, 16, 108. [Google Scholar] [CrossRef]
- Zielinski, M.R.; Gibbons, A.J. Neuroinflammation, Sleep, and Circadian Rhythms. Front. Cell. Infect. Microbiol. 2022, 12, 853096. [Google Scholar] [CrossRef]
- DiSabato, D.J.; Quan, N.; Godbout, J.P. Neuroinflammation: The devil is in the details. J. Neurochem. 2016, 139, 136–153. [Google Scholar] [CrossRef]
- Rao, J.S.; Kim, H.-W.; Kellom, M.; Greenstein, D.; Chen, M.; Kraft, A.D.; Harry, G.J.; Rapoport, S.I.; Basselin, M. Increased neuroinflammatory and arachidonic acid cascade markers, and reduced synaptic proteins, in brain of HIV-1 transgenic rats. J. Neuroinflammation 2011, 8, 101. [Google Scholar] [CrossRef]
- Mottahedin, A.; Ardalan, M.; Chumak, T.; Riebe, I.; Ek, J.; Mallard, C. Effect of Neuroinflammation on Synaptic Organization and Function in the Developing Brain: Implications for Neurodevelopmental and Neurodegenerative Disorders. Front. Cell. Neurosci. 2017, 11, 190. [Google Scholar] [CrossRef]
- Valcarcel-Ares, M.N.; Tucsek, Z.; Kiss, T.; Giles, C.B.; Tarantini, S.; Yabluchanskiy, A.; Balasubramanian, P.; Gautam, T.; Galvan, V.; Ballabh, P.; et al. Obesity in Aging Exacerbates Neuroinflammation, Dysregulating Synaptic Function-Related Genes and Altering Eicosanoid Synthesis in the Mouse Hippocampus: Potential Role in Impaired Synaptic Plasticity and Cognitive Decline. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 290–298. [Google Scholar] [CrossRef]
- Lauderback, C.M.; Kanski, J.; Hackett, J.M.; Maeda, N.; Kindy, M.S.; Butterfield, D.A. Apolipoprotein E modulates Alzheimer’s Abeta(1-42)-induced oxidative damage to synaptosomes in an allele-specific manner. Brain Res. 2002, 924, 90–97. [Google Scholar] [CrossRef] [PubMed]
- GRAY, E.G.; WHITTAKER, V.P. The isolation of nerve endings from brain: An electron-microscopic study of cell fragments derived by homogenization and centrifugation. J. Anat. 1962, 96, 79–88. [Google Scholar] [PubMed]
- Lin, T.Y.; Yang, T.-T.; Lu, C.W.; Wang, S.-J. Inhibition of glutamate release by bupropion in rat cerebral cortex nerve terminals. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 598–606. [Google Scholar] [CrossRef]
- Canas, P.M.; Duarte, J.M.N.; Rodrigues, R.J.; Köfalvi, A.; Cunha, R.A. Modification upon aging of the density of presynaptic modulation systems in the hippocampus. Neurobiol. Aging 2009, 30, 1877–1884. [Google Scholar] [CrossRef]
- Ahmad, F.; Jing, Y.; Lladó, A.; Liu, P. Chemical stimulation of rodent and human cortical synaptosomes: Implications in neurodegeneration. Cells 2021, 10, 1174. [Google Scholar] [CrossRef]
- Picone, P.; Porcelli, G.; Bavisotto, C.C.; Nuzzo, D.; Galizzi, G.; Biagio, P.L.S.; Bulone, D.; Carlo, M.D.; Di Carlo, M. Synaptosomes: New vesicles for neuronal mitochondrial transplantation. J. Nanobiotechnology 2021, 19, 6. [Google Scholar] [CrossRef]
- Wang, C.-C.; Hsieh, P.-W.; Kuo, J.-R.; Wang, S.-J. Rosmarinic Acid, a Bioactive Phenolic Compound, Inhibits Glutamate Release from Rat Cerebrocortical Synaptosomes through GABAA Receptor Activation. Biomolecules 2021, 11, 1029. [Google Scholar] [CrossRef] [PubMed]
- Sellgren, C.M.; Gracias, J.; Watmuff, B.; Biag, J.D.; Thanos, J.M.; Whittredge, P.B.; Fu, T.; Worringer, K.; Brown, H.E.; Wang, J.; et al. Increased synapse elimination by microglia in schizophrenia patient-derived models of synaptic pruning. Nat. Neurosci. 2019, 22, 374–385. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, S.D.; Horng, J.E.; Perlis, R.H. Patient-Derived In Vitro Models of Microglial Function and Synaptic Engulfment in Schizophrenia. Biol. Psychiatry 2022, 92, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Jhou, J.-F.; Tai, H.-C. The Study of Postmortem Human Synaptosomes for Understanding Alzheimer’s Disease and Other Neurological Disorders: A Review. Neurol. Ther. 2017, 6, 57–68. [Google Scholar] [CrossRef]
- Györffy, B.A.; Tóth, V.; Török, G.; Gulyássy, P.; Kovács, R.; Vadászi, H.; Micsonai, A.; Tóth, M.E.; Sántha, M.; Homolya, L.; et al. Synaptic mitochondrial dysfunction and septin accumulation are linked to complement-mediated synapse loss in an Alzheimer’s disease animal model. Cell. Mol. Life Sci. 2020, 77, 5243–5258. [Google Scholar] [CrossRef]
- Marcelli, S.; Ficulle, E.; Iannuzzi, F.; Kövari, E.; Nisticò, R.; Feligioni, M. Targeting SUMO-1ylation Contrasts Synaptic Dysfunction in a Mouse Model of Alzheimer’s Disease. Mol. Neurobiol. 2017, 54, 6609–6623. [Google Scholar] [CrossRef]
- Gylys, K.H.; Fein, J.A.; Cole, G.M. Quantitative characterization of crude synaptosomal fraction (P-2) components by flow cytometry. J. Neurosci. Res. 2000, 61, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Hobson, B.D.; Sims, P.A. Critical analysis of particle detection artifacts in synaptosome flow cytometry. eNeuro 2019, 6, 27. [Google Scholar] [CrossRef] [PubMed]
- Gulyássy, P.; Puska, G.; Györffy, B.A.; Todorov-Völgyi, K.; Juhász, G.; Drahos, L.; Kékesi, K.A. Proteomic comparison of different synaptosome preparation procedures. Amino Acids 2020, 52, 1529–1543. [Google Scholar] [CrossRef] [PubMed]
- Plum, S.; Eggers, B.; Helling, S.; Stepath, M.; Theiss, C.; Leite, R.E.P.P.; Molina, M.; Grinberg, L.T.; Riederer, P.; Gerlach, M.; et al. Proteomic Characterization of Synaptosomes from Human Substantia Nigra Indicates Altered Mitochondrial Translation in Parkinson’s Disease. Cells 2020, 9, 2580. [Google Scholar] [CrossRef]
- Gogoi, P.; Shiozaki, M.; Gouaux, E. Isolation, cryo-laser scanning confocal microscope imaging and cryo-FIB milling of mouse glutamatergic synaptosomes. PLoS ONE 2022, 17, e0271799. [Google Scholar] [CrossRef]
- Massaro Tieze, S.; Chandra, S.S.; Vidyadhara, D.J. Subcellular Fractionation for the Isolation of Synaptic Components from the Murine Brain. J. Vis. Exp. 2022, 2022, 64574. [Google Scholar] [CrossRef]
- Miyoshi, E.; Bilousova, T.; Melnik, M.; Fakhrutdinov, D.; Poon, W.W.; Vinters, H.V.; Miller, C.A.; Corrada, M.; Kawas, C.; Bohannan, R.; et al. Exosomal tau with seeding activity is released from Alzheimer’s disease synapses, and seeding potential is associated with amyloid beta. Lab. Investig. 2021, 101, 1605–1617. [Google Scholar] [CrossRef]
- Sapp, E.; Seeley, C.; Iuliano, M.; Weisman, E.; Vodicka, P.; DiFiglia, M.; Kegel-Gleason, K.B. Protein changes in synaptosomes of Huntington’s disease knock-in mice are dependent on age and brain region. Neurobiol. Dis. 2020, 141, 104950. [Google Scholar] [CrossRef]
- Fonseca-Ornelas, L.; Viennet, T.; Rovere, M.; Jiang, H.; Liu, L.; Nuber, S.; Ericsson, M.; Arthanari, H.; Selkoe, D.J. Altered conformation of α-synuclein drives dysfunction of synaptic vesicles in a synaptosomal model of Parkinson’s disease. Cell Rep. 2021, 36, 109333. [Google Scholar] [CrossRef]
- Sánchez-Sarasúa, S.; Fernández-Pérez, I.; Espinosa-Fernández, V.; Sánchez-Pérez, A.M.; Ledesma, J.C. Can we treat neuroinflammation in alzheimer’s disease? Int. J. Mol. Sci. 2020, 21, 8751. [Google Scholar] [CrossRef] [PubMed]
- Lanni, C.; Fagiani, F.; Racchi, M.; Preda, S.; Pascale, A.; Grilli, M.; Allegri, N.; Govoni, S. Beta-amyloid short- and long-term synaptic entanglement. Pharmacol. Res. 2019, 139, 243–260. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.P.N.; Kumar, M.; Fedele, E.; Bonanno, G.; Bonifacino, T. MicroRNA Alteration, Application as Biomarkers, and Therapeutic Approaches in Neurodegenerative Diseases. Int. J. Mol. Sci. 2022, 23, 4718. [Google Scholar] [CrossRef] [PubMed]
- Obrador, E.; Salvador, R.; López-Blanch, R.; Jihad-Jebbar, A.; Vallés, S.L.; Estrela, J.M. Oxidative Stress, Neuroinflammation and Mitochondria in the Pathophysiology of Amyotrophic Lateral Sclerosis. Antioxidants 2020, 9, 901. [Google Scholar] [CrossRef] [PubMed]
- Raiteri, L.; Raiteri, M. Synaptosomes Still Viable after 25 Years of Superfusion. Neurochem. Res. 2000, 25, 1265–1274. [Google Scholar] [CrossRef]
- Pittaluga, A. Acute functional adaptations in isolated presynaptic terminals unveil synaptosomal learning and memory. Int. J. Mol. Sci. 2019, 20, 3641. [Google Scholar] [CrossRef]
- Raiteri, M.; Sala, R.; Fassio, A.; Rossetto, O.; Bonanno, G. Entrapping of impermeant probes of different size into nonpermeabilized synaptosomes as a method to study presynaptic mechanisms. J. Neurochem. 2000, 74, 423–431. [Google Scholar] [CrossRef]
- Grilli, M.; Summa, M.; Salamone, A.; Olivero, G.; Zappettini, S.; Prisco, S.D.; Feligioni, M.; Usai, C.; Pittaluga, A.; Marchi, M.; et al. In vitro exposure to nicotine induces endocytosis of presynaptic AMPA receptors modulating dopamine release in rat nucleus accumbens nerve terminals. Neuropharmacology 2012, 63, 916–926. [Google Scholar] [CrossRef]
- Trebesova, H.; Olivero, G.; Marchi, M.; Grilli, M. The Anti-Aggregative Peptide KLVFF Mimics Aβ1-40 in the Modulation of Nicotinic Receptors: Implications for Peptide-Based Therapy. Biomedicines 2022, 10, 2231. [Google Scholar] [CrossRef]
- Olivero, G.; Cisani, F.; Marimpietri, D.; Di Paolo, D.; Gagliani, M.C.; Podestà, M.; Cortese, K.; Pittaluga, A. The Depolarization-Evoked, Ca2+-Dependent Release of Exosomes From Mouse Cortical Nerve Endings: New Insights Into Synaptic Transmission. Front. Pharmacol. 2021, 12, 670158. [Google Scholar] [CrossRef]
- Bilousova, T.; Melnik, M.; Miyoshi, E.; Gonzalez, B.L.; Poon, W.W.; Vinters, H.V.; Miller, C.A.; Corrada, M.M.; Kawas, C.; Hatami, A.; et al. Apolipoprotein E/Amyloid-β Complex Accumulates in Alzheimer Disease Cortical Synapses via Apolipoprotein E Receptors and Is Enhanced by APOE4. Am. J. Pathol. 2019, 189, 1621–1636. [Google Scholar] [CrossRef]
- Wang, S.; Li, B.; Solomon, V.; Fonteh, A.; Rapoport, S.I.; Bennett, D.A.; Arvanitakis, Z.; Chui, H.C.; Sullivan, P.M.; Yassine, H.N. Calcium-dependent cytosolic phospholipase A2 activation is implicated in neuroinflammation and oxidative stress associated with ApoE4. Mol. Neurodegener. 2022, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Sisqués, L.; Sancho-Balsells, A.; Solana-Balaguer, J.; Campoy-Campos, G.; Vives-Isern, M.; Soler-Palazón, F.; Anglada-Huguet, M.; López-Toledano, M.-Á.; Mandelkow, E.-M.; Alberch, J.; et al. RTP801/REDD1 contributes to neuroinflammation severity and memory impairments in Alzheimer’s disease. Cell Death Dis. 2021, 12, 616. [Google Scholar] [CrossRef] [PubMed]
- Marcatti, M.; Fracassi, A.; Montalbano, M.; Natarajan, C.; Krishnan, B.; Kayed, R.; Taglialatela, G. Aβ/tau oligomer interplay at human synapses supports shifting therapeutic targets for Alzheimer’s disease. Cell. Mol. Life Sci. 2022, 79, 222. [Google Scholar] [CrossRef] [PubMed]
- Cefaliello, C.; Penna, E.; Barbato, C.; Di Ruberto, G.; Mollica, M.P.; Trinchese, G.; Cigliano, L.; Borsello, T.; Chun, J.T.; Giuditta, A.; et al. Deregulated Local Protein Synthesis in the Brain Synaptosomes of a Mouse Model for Alzheimer’s Disease. Mol. Neurobiol. 2020, 57, 1529–1541. [Google Scholar] [CrossRef]
- Megur, A.; Baltriukien, D.; Bukelskien, V.; Burokas, A. The Microbiota-Gut-Brain Axis and Alzheimer’s Disease: Neuroinflammation Is to Blame? Nutrients 2020, 1, 37. [Google Scholar] [CrossRef]
- Kovács, R.A.; Vadászi, H.; Bulyáki, E.; Török, G.; Tóth, V.; Mátyás, D.; Kun, J.; Hunyadi-Gulyás, E.; Fedor, F.Z.; Csincsi, A.; et al. Identification of Neuronal Pentraxins as Synaptic Binding Partners of C1q and the Involvement of NP1 in Synaptic Pruning in Adult Mice. Front. Immunol. 2021, 11, 599771. [Google Scholar] [CrossRef]
- Bhatti, G.K.; Reddy, A.P.; Reddy, P.H.; Bhatti, J.S. Lifestyle Modifications and Nutritional Interventions in Aging-Associated Cognitive Decline and Alzheimer’s Disease. Front. Aging Neurosci. 2020, 11, 369. [Google Scholar] [CrossRef]
- Wijasa, T.S.; Sylvester, M.; Brocke-Ahmadinejad, N.; Schwartz, S.; Santarelli, F.; Gieselmann, V.; Klockgether, T.; Brosseron, F.; Heneka, M.T. Quantitative proteomics of synaptosome S-nitrosylation in Alzheimer’s disease. J. Neurochem. 2020, 152, 710–726. [Google Scholar] [CrossRef]
- Largo-Barrientos, P.; Apóstolo, N.; Creemers, E.; Callaerts-Vegh, Z.; Swerts, J.; Davies, C.; McInnes, J.; Wierda, K.; De Strooper, B.; Spires-Jones, T.; et al. Lowering Synaptogyrin-3 expression rescues Tau-induced memory defects and synaptic loss in the presence of microglial activation. Neuron 2021, 109, 767–777.e5. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, J.; Grant, S.G.N.N. Synapse pathology in Alzheimer’s disease. Semin. Cell Dev. Biol. 2022, 139, 13–23. [Google Scholar] [CrossRef]
- Sharman, M.J.; Verdile, G.; Kirubakaran, S.; Parenti, C.; Singh, A.; Watt, G.; Karl, T.; Chang, D.; Li, C.G.; Münch, G. Targeting Inflammatory Pathways in Alzheimer’s Disease: A Focus on Natural Products and Phytomedicines. CNS Drugs 2019, 33, 457–480. [Google Scholar] [CrossRef] [PubMed]
- Castelletto, V.; Ryumin, P.; Cramer, R.; Hamley, I.W.; Taylor, M.; Allsop, D.; Reza, M.; Ruokolainen, J.; Arnold, T.; Hermida-Merino, D.; et al. Self-assembly and anti-amyloid cytotoxicity activity of amyloid beta peptide derivatives. Sci. Rep. 2017, 7, 43637. [Google Scholar] [CrossRef] [PubMed]
- Saliba, S.W.; Bonifacino, T.; Serchov, T.; Bonanno, G.; de Oliveira, A.C.P.; Fiebich, B.L. Neuroprotective Effect of AM404 Against NMDA-Induced Hippocampal Excitotoxicity. Front. Cell. Neurosci. 2019, 13, 566. [Google Scholar] [CrossRef]
- Marogianni, C.; Sokratous, M.; Dardiotis, E.; Hadjigeorgiou, G.M.; Bogdanos, D.; Xiromerisiou, G. Neurodegeneration and inflammation—An interesting interplay in parkinson’s disease. Int. J. Mol. Sci. 2020, 21, 8421. [Google Scholar] [CrossRef]
- Lin, C.H.; Hsieh, C.L. Chinese Herbal Medicine for Treating Epilepsy. Front. Neurosci. 2021, 15, 682821. [Google Scholar] [CrossRef]
- Gorski, K.; Spoljaric, A.; Nyman, T.A.; Kaila, K.; Battersby, B.J.; Lehesjoki, A.E. Quantitative Changes in the Mitochondrial Proteome of Cerebellar Synaptosomes From Preclinical Cystatin B-Deficient Mice. Front. Mol. Neurosci. 2020, 13, 570640. [Google Scholar] [CrossRef]
- Manabe, T.; Rácz, I.; Schwartz, S.; Oberle, L.; Santarelli, F.; Emmrich, J.V.; Neher, J.J.; Heneka, M.T. Systemic inflammation induced the delayed reduction of excitatory synapses in the CA3 during ageing. J. Neurochem. 2021, 159, 525–542. [Google Scholar] [CrossRef]
- Jing, G.; Zuo, J.; Fang, Q.; Yuan, M.; Xia, Y.; Jin, Q.; Liu, Y.; Wang, Y.; Zhang, Z.; Liu, W.; et al. Erbin protects against sepsis-associated encephalopathy by attenuating microglia pyroptosis via IRE1α/Xbp1s-Ca2+ axis. J. Neuroinflammation 2022, 19, 237. [Google Scholar] [CrossRef]
- Düsedau, H.P.; Steffen, J.; Figueiredo, C.A.; Boehme, J.D.; Schultz, K.; Erck, C.; Korte, M.; Faber-Zuschratter, H.; Smalla, K.-H.; Dieterich, D.; et al. Influenza A Virus (H1N1) Infection Induces Microglial Activation and Temporal Dysbalance in Glutamatergic Synaptic Transmission. MBio 2021, 12, e01776-21. [Google Scholar] [CrossRef] [PubMed]
- Cavaliere, G.; Trinchese, G.; Penna, E.; Cimmino, F.; Pirozzi, C.; Lama, A.; Annunziata, C.; Catapano, A.; Mattace Raso, G.; Meli, R.; et al. High-Fat Diet Induces Neuroinflammation and Mitochondrial Impairment in Mice Cerebral Cortex and Synaptic Fraction. Front. Cell. Neurosci. 2019, 13, 509. [Google Scholar] [CrossRef] [PubMed]
- Han, T.K.; Leem, Y.H.; Kim, H.S. Treadmill exercise restores high fat diet-induced disturbance of hippocampal neurogenesis through β2-adrenergic receptor-dependent induction of thioredoxin-1 and brain-derived neurotrophic factor. Brain Res. 2019, 1707, 154–163. [Google Scholar] [CrossRef]
- Marte, A.; Cavallero, A.; Morando, S.; Uccelli, A.; Raiteri, M.; Fedele, E. Alterations of glutamate release in the spinal cord of mice with experimental autoimmune encephalomyelitis. J. Neurochem. 2010, 115, 343–352. [Google Scholar] [CrossRef]
- Di Prisco, S.; Merega, E.; Lanfranco, M.; Casazza, S.; Uccelli, A.; Pittaluga, A. Acute desipramine restores presynaptic cortical defects in murine experimental autoimmune encephalomyelitis by suppressing central CCL5 overproduction. Br. J. Pharmacol. 2014, 171, 2457–2467. [Google Scholar] [CrossRef]
- Vallarino, G.; Salis, A.; Lucarini, E.; Turrini, F.; Olivero, G.; Roggeri, A.; Damonte, G.; Boggia, R.; Mannelli, L.D.C.; Ghelardini, C.; et al. Healthy Properties of a New Formulation of Pomegranate-Peel Extract in Mice Suffering from Experimental Autoimmune Encephalomyelitis. Molecules 2022, 27, 914. [Google Scholar] [CrossRef]
- Chanaday, N.L.; Vilcaes, A.A.; de Paul, A.L.; Torres, A.I.; Degano, A.L.; Roth, G.A. Glutamate release machinery is altered in the frontal cortex of rats with experimental autoimmune encephalomyelitis. Mol. Neurobiol. 2015, 51, 1353–1367. [Google Scholar] [CrossRef]
- Vilcaes, A.A.; Furlan, G.; Roth, G.A. Inhibition of Ca2+-dependent glutamate release from cerebral cortex synaptosomes of rats with experimental autoimmune encephalomyelitis. J. Neurochem. 2009, 108, 881–890. [Google Scholar] [CrossRef]
- Fernández Hurst, N.; Chanaday, N.L.; Roth, G.A. GABAergic Agonists Modulate the Glutamate Release from Frontal Cortex Synaptosomes of Rats with Experimental Autoimmune Encephalomyelitis. Inflamm. Allergy Drug Targets 2015, 14, 105–110. [Google Scholar] [CrossRef]
- Di Filippo, M.; De Iure, A.; Giampà, C.; Chiasserini, D.; Tozzi, A.; Orvietani, P.L.; Ghiglieri, V.; Tantucci, M.; Durante, V.; Quiroga-Varela, A.; et al. Persistent activation of microglia and NADPH drive hippocampal dysfunction in experimental multiple sclerosis. Sci. Rep. 2016, 6, 20926. [Google Scholar] [CrossRef]
- Ravera, S.; Torazza, C.; Bonifacino, T.; Provenzano, F.; Rebosio, C.; Milanese, M.; Usai, C.; Panfoli, I.; Bonanno, G. Altered glucose catabolism in the presynaptic and perisynaptic compartments of SOD1G93A mouse spinal cord and motor cortex indicates that mitochondria are the site of bioenergetic imbalance in ALS. J. Neurochem. 2019, 151, 336–350. [Google Scholar] [CrossRef] [PubMed]
- Raiteri, L.; Paolucci, E.; Prisco, S.; Raiteri, M.; Bonanno, G. Activation of a glycine transporter on spinal cord neurons causes enhanced glutamate release in a mouse model of amyotrophic lateral sclerosis. Br. J. Pharmacol. 2003, 138, 1021–1025. [Google Scholar] [CrossRef]
- Meftahi, G.H.; Bahari, Z.; Zarei Mahmoudabadi, A.; Iman, M.; Jangravi, Z. Applications of western blot technique: From bench to bedside. Biochem. Mol. Biol. Educ. A Bimon. Publ. Int. Union Biochem. Mol. Biol. 2021, 49, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.W.; Choe, K.; Park, J.S.; Lee, H.J.; Kang, M.H.; Ahmad, R.; Kim, M.O. Pharmacological Inhibition of Spleen Tyrosine Kinase Suppressed Neuroinflammation and Cognitive Dysfunction in LPS-Induced Neurodegeneration Model. Cells 2022, 11, 1777. [Google Scholar] [CrossRef]
- Zhao, J.; Bi, W.; Xiao, S.; Lan, X.; Cheng, X.; Zhang, J.; Lu, D.; Wei, W.; Wang, Y.; Li, H.; et al. Neuroinflammation induced by lipopolysaccharide causes cognitive impairment in mice. Sci. Rep. 2019, 9, 5790. [Google Scholar] [CrossRef]
- Lu, C.W.; Lin, T.Y.; Huang, S.K.; Wang, S.J. 5-HT1B receptor agonist CGS12066 presynaptically inhibits glutamate release in rat hippocampus. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2018, 86, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Polishchuk, A.; Cilleros-Mañé, V.; Just-Borràs, L.; Balanyà-Segura, M.; Vandellòs Pont, G.; Silvera Simón, C.; Tomàs, M.; Garcia, N.; Tomàs, J.; Lanuza, M.A. Synaptic retrograde regulation of the PKA-induced SNAP-25 and Synapsin-1 phosphorylation. Cell. Mol. Biol. Lett. 2023, 28, 17. [Google Scholar] [CrossRef] [PubMed]
- Morató, X.; López-Cano, M.; Canas, P.M.; Cunha, R.A.; Ciruela, F. Brain Membrane Fractionation: An Ex Vivo Approach to Assess Subsynaptic Protein Localization. J. Vis. Exp. 2017, 123, 55661. [Google Scholar] [CrossRef]
- Martín-Flores, N.; Romaní-Aumedes, J.; Rué, L.; Canal, M.; Sanders, P.; Straccia, M.; Allen, N.D.; Alberch, J.; Canals, J.M.; Pérez-Navarro, E.; et al. RTP801 Is Involved in Mutant Huntingtin-Induced Cell Death. Mol. Neurobiol. 2016, 53, 2857–2868. [Google Scholar] [CrossRef]
- Romaní-Aumedes, J.; Canal, M.; Martín-Flores, N.; Sun, X.; Pérez-Fernández, V.; Wewering, S.; Fernández-Santiago, R.; Ezquerra, M.; Pont-Sunyer, C.; Lafuente, A.; et al. Parkin loss of function contributes to RTP801 elevation and neurodegeneration in Parkinson’s disease. Cell Death Dis. 2014, 5, e1364. [Google Scholar] [CrossRef]
- Postupna, N.O.; Keene, C.D.; Latimer, C.; Sherfield, E.E.; Van Gelder, R.D.; Ojemann, J.G.; Montine, T.J.; Darvas, M. Flow cytometry analysis of synaptosomes from post-mortem human brain reveals changes specific to Lewy body and Alzheimer’s disease. Lab. Investig. 2014, 94, 1161–1172. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, F.; Mao, L.; Feng, T.; Wang, K.; Xu, M.; Lv, B.; Wang, X. Bifico relieves irritable bowel syndrome by regulating gut microbiota dysbiosis and inflammatory cytokines. Eur. J. Nutr. 2023, 62, 139–155. [Google Scholar] [CrossRef] [PubMed]
- Postupna, N.O.; Latimer, C.S.; Keene, C.D.; Montine, K.S.; Thomas, J.; Darvas, M. Synaptosomes; Neuromethods; Murphy, K.M., Ed.; Springer: New York, NY, USA, 2018; Volume 141, ISBN 978-1-4939-8738-2. [Google Scholar]
- Sokolow, S.; Henkins, K.M.; Williams, I.A.; Vinters, H.V.; Schmid, I.; Cole, G.M.; Gylys, K.H. Isolation of synaptic terminals from Alzheimer’s disease cortex. Cytom. Part A 2012, 81A, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Gylys, K.H.; Fein, J.A.; Wiley, D.J.; Cole, G.M. Rapid annexin-V labeling in synaptosomes. Neurochem. Int. 2004, 44, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Centonze, D.; Muzio, L.; Rossi, S.; Cavasinni, F.; Chiara, V.D.; Bergami, A.; Musella, A.; D’Amelio, M.; Cavallucci, V.; Martorana, A.; et al. Inflammation triggers synaptic alteration and degeneration in experimental autoimmune encephalomyelitis. J. Neurosci. 2009, 29, 3442–3452. [Google Scholar] [CrossRef]
- Schaller, S.; Buttigieg, D.; Alory, A.; Jacquier, A.; Barad, M.; Merchant, M.; Gentien, D.; Grange, P.D.L.; Haase, G.; De La Grange, P.; et al. Novel combinatorial screening identifies neurotrophic factors for selective classes of motor neurons. Proc. Natl. Acad. Sci. USA 2017, 114, E2486–E2493. [Google Scholar] [CrossRef]
- Si, Z.-Z.; Zou, C.-J.; Mei, X.; Li, X.-F.; Luo, H.; Shen, Y.; Hu, J.; Li, X.-X.; Wu, L.; Liu, Y. Targeting neuroinflammation in Alzheimer’s disease: From mechanisms to clinical applications. Neural Regen. Res. 2023, 18, 708–715. [Google Scholar] [CrossRef]
- Pedicone, C.; Fernandes, S.; Matera, A.; Meyer, S.T.; Loh, S.; Ha, J.H.; Bernard, D.; Chisholm, J.D.; Paolicelli, R.C.; Kerr, W.G. Discovery of a novel SHIP1 agonist that promotes degradation of lipid-laden phagocytic cargo by microglia. iScience 2022, 25, 104170. [Google Scholar] [CrossRef]
- Abg Abd Wahab, D.Y.; Gau, C.H.; Zakaria, R.; Muthu Karuppan, M.K.; A-Rahbi, B.S.; Abdullah, Z.; Alrafiah, A.; Abdullah, J.M.; Muthuraju, S. Review on Cross Talk between Neurotransmitters and Neuroinflammation in Striatum and Cerebellum in the Mediation of Motor Behaviour. Biomed Res. Int. 2019, 2019, 1767203. [Google Scholar] [CrossRef]
- Pozdnyakova, N.; Krisanova, N.; Pastukhov, A.; Tarasenko, A.; Dudarenko, M.; Chernykh, A.; Pashenko, A.; Ryabukhin, S.; Tolstanova, G.; Volochnyuk, D.; et al. Neuromodulation by selective angiotensin-converting enzyme 2 inhibitors. Neuroscience 2022, 498, 155–173. [Google Scholar] [CrossRef]
- Krisanova, N.; Pozdnyakova, N.; Pastukhov, A.; Dudarenko, M.; Shatursky, O.; Gnatyuk, O.; Afonina, U.; Pyrshev, K.; Dovbeshko, G.; Yesylevskyy, S.; et al. Amphiphilic anti-SARS-CoV-2 drug remdesivir incorporates into the lipid bilayer and nerve terminal membranes influencing excitatory and inhibitory neurotransmission. Biochim. Biophys. Acta. Biomembr. 2022, 1864, 183945. [Google Scholar] [CrossRef] [PubMed]
- Storchak, L.G.; Kravchuk, M.V.; Himmelreich, N.H. Okadaic acid and cyclosporin A modulate [(3)H]GABA release from rat brain synaptosomes. Neurochem. Int. 2001, 38, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Wang, Y.; Zheng, K. Microglial mitophagy integrates the microbiota-gut-brain axis to restrain neuroinflammation during neurotropic herpesvirus infection. Autophagy 2023, 19, 734–736. [Google Scholar] [CrossRef] [PubMed]
- Carlson, S.W.; Dixon, C.E. Lithium Improves Dopamine Neurotransmission and Increases Dopaminergic Protein Abundance in the Striatum after Traumatic Brain Injury. J. Neurotrauma 2018, 35, 2827–2836. [Google Scholar] [CrossRef] [PubMed]
- Nishiham, I.; Toshiaki, M.; Watanabe, Y.; Ito, S.; Hayaishi, O. Prostaglandin E2 stimulates glutamate release from synaptosomes of rat spinal cord. Neurosci. Lett. 1995, 196, 57–60. [Google Scholar] [CrossRef]
- Gagné, F.; Bérubé, E.; Fournier, M.; Blaise, C. Inflammatory properties of municipal effluents to Elliptio complanata mussels—Lack of effects from anti-inflammatory drugs. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2005, 141, 332–337. [Google Scholar] [CrossRef]
- D’arcangelo, G.; Tancredi, V.; Onofri, F.; D’antuono, M.; Giovedì, S.; Benfenati, F. Interleukin-6 inhibits neurotransmitter release and the spread of excitation in the rat cerebral cortex. Eur. J. Neurosci. 2000, 12, 1241–1252. [Google Scholar] [CrossRef]
- Ferreras, S.; Singh, N.P.; Le Borgne, R.; Bun, P.; Binz, T.; Parton, R.G.; Verbavatz, J.-M.; Vannier, C.; Galli, T. A synthetic organelle approach to probe SNARE-mediated membrane fusion in a bacterial host. J. Biol. Chem. 2023, 299, 102974. [Google Scholar] [CrossRef]
- Yang, R.; Gao, Y.; Li, H.; Huang, W.; Tu, D.; Yang, M.; Liu, X.; Hong, J.-S.; Gao, H.-M. Posttranslational S-nitrosylation modification regulates HMGB1 secretion and promotes its proinflammatory and neurodegenerative effects. Cell Rep. 2022, 40, 111330. [Google Scholar] [CrossRef]
- Kummer, M.P.; Hermes, M.; Delekarte, A.; Hammerschmidt, T.; Kumar, S.; Terwel, D.; Walter, J.; Pape, H.-C.; König, S.; Roeber, S.; et al. Nitration of tyrosine 10 critically enhances amyloid β aggregation and plaque formation. Neuron 2011, 71, 833–844. [Google Scholar] [CrossRef]
- Tchaikovskaya, T.; Fraifeld, V.; Urphanishvili, T.; Andorfer, J.H.; Davies, P.; Listowsky, I. Glutathione S-transferase hGSTM3 and ageing-associated neurodegeneration: Relationship to Alzheimer’s disease. Mech. Ageing Dev. 2005, 126, 309–315. [Google Scholar] [CrossRef]
- Giannoccaro, M.P.; La Morgia, C.; Rizzo, G.; Carelli, V. Mitochondrial DNA and primary mitochondrial dysfunction in Parkinson’s disease. Mov. Disord. 2017, 32, 346–363. [Google Scholar] [CrossRef]
- Kälviäinen, R.; Khyuppenen, J.; Koskenkorva, P.; Eriksson, K.; Vanninen, R.; Mervaala, E. Clinical picture of EPM1-Unverricht-Lundborg disease. Epilepsia 2008, 49, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Johannesen, K.M.; Gardella, E.; Linnankivi, T.; Courage, C.; de Saint Martin, A.; Lehesjoki, A.-E.; Mignot, C.; Afenjar, A.; Lesca, G.; Abi-Warde, M.-T.; et al. Defining the phenotypic spectrum of SLC6A1 mutations. Epilepsia 2018, 59, 389–402. [Google Scholar] [CrossRef] [PubMed]
- Marin-Dett, F.H.; Campanella, J.E.M.; Trovatti, E.; Bertolini, M.C.; Vergani, C.E.; Barbugli, P.A. Extracellular lipids of Candida albicans biofilm induce lipid droplet formation and decreased response to a topoisomerase I inhibitor in dysplastic and neoplastic oral cells. J. Appl. Oral Sci. 2023, 30, e20220319. [Google Scholar] [CrossRef] [PubMed]
- Györffy, B.A.; Kun, J.; Török, G.; Bulyáki, É.; Borhegyi, Z.; Gulyássy, P.; Kis, V.; Szocsics, P.; Micsonai, A.; Matkó, J.; et al. Local apoptotic-like mechanisms underlie complementmediated synaptic pruning. Proc. Natl. Acad. Sci. USA 2018, 115, 6303–6308. [Google Scholar] [CrossRef] [PubMed]
- Valbuena, G.N.; Tortarolo, M.; Bendotti, C.; Cantoni, L.; Keun, H.C. Altered Metabolic Profiles Associate with Toxicity in SOD1G93A Astrocyte-Neuron Co-Cultures. Sci. Rep. 2017, 7, 50. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).