Abstract
Background: Vaccination is a crucial public health measure to control infectious diseases, including seasonal influenza. Yet, vaccine uptake varies globally due to sociodemographic factors, misinformation, and access disparities. Objectives: The objective of this study was to assess the prevalence and sociodemographic factors associated with vaccination and the main reasons for vaccine hesitancy in Albania. Methods: A cross-sectional study, conducted in Albania in November–December 2021, included a sample of 1302 individuals aged ≥18 years (≈57% females; mean age: 38.3 ± 15.0 years; response rate: ≈87%). A structured questionnaire was administered inquiring about co-vaccination status against seasonal influenza and COVID-19, reasons for not being vaccinated, and sociodemographic characteristics of participants. Binary logistic regression was used to assess the association of co-vaccination status with sociodemographic factors. Results: Overall, about 28% of individuals were co-vaccinated against seasonal influenza and COVID-19 at least with one dose (25% in males vs. 29% in females; 22% among 18–24-year-olds vs. 54% among those aged ≥65 years). Independent positive and significant correlates of being co-vaccinated included older age (OR = 7.0, 95%CI = 3.7–12.9) and a higher educational attainment (OR = 2.3, 95%CI = 1.4–3.6). The main reasons for vaccine hesitancy among non-vaccinated individuals included the belief that vaccines are: harmful (72%), not effective (66%), weaken the immune system (58%), are not safe (56%), and preference to recover naturally (52%). Conclusions: This study evidenced a relatively low co-vaccination rate in Albania with significant sociodemographic disparities, notwithstanding the availability of vaccines and their free-of-charge provision to the overall population. Older age and higher educational attainment were identified as independent positive predictors of co-vaccination uptake, suggesting the need for targeted public health strategies to address vaccine hesitancy, particularly among younger and less-educated population categories. Our findings emphasize the importance of tailored communication campaigns and community-based interventions to improve vaccine coverage and mitigate the impact of infectious diseases in Albania and elsewhere.
1. Introduction
It has been convincingly demonstrated that vaccination is among the most effective and affordable methods for preventing diseases, including seasonal influenza [1,2]. According to the World Health Organization (WHO), vaccination prevents 2–3 million deaths a year [1], and an additional 1.5 million lives could be saved if global vaccination coverage were increased [1]. Therefore, since 2019, the WHO has listed vaccine hesitancy among the top ten threats to global health [1]. Furthermore, over the past 50 years, over 150 million lives have been saved due to vaccination [3]. In high-income countries, for decades now, routine vaccination has successfully eradicated or controlled several communicable diseases [4,5].
The COVID-19 pandemic posed an unprecedented challenge to public health, the global economy, and nearly every aspect of societies worldwide [2,3]. However, one of the lasting legacies of the COVID-19 pandemic was the rapid development of effective vaccines against seasonal influenza [2]. Mass COVID-19 vaccination began in the United States (US) in December 2020 [6], reducing infections among the vaccinated groups [7]. In 2021, as vaccination programs advanced, a significant decline in cases and deaths led many US regions to ease non-pharmaceutical interventions [2,8,9].
Notably, seasonal influenza and COVID-19 vaccines are distributed annually or biannually across many countries. Since most doses of these two vaccines are sold in high-income countries, this category accounts for a relatively high financial value [3].
Yet, as vaccination campaigns expanded globally, notable vaccine hesitancy—a strong reluctance to embrace vaccination [2,10]—and resistance emerged in the general population [2], as well as among healthcare workers, including also vaccination against seasonal influenza [11]. For example, in 2021, surveys across multiple countries revealed significant variations in seasonal influenza and especially COVID-19 vaccine acceptance between nations, ranging from about 30% to 90% [2,12,13]. Vaccine hesitancy can stem from various factors, including concerns about the vaccine’s safety and potential side effects [2,14], misinformation [15], or distrust in scientific expertise [2,16].
In 2020, there was evidence of lower COVID-19 related mortality and incidence rates in Eastern European countries, including Albania, which has been associated with the delayed start of community circulation [17]. The delayed start of community transmission in Albania [17] was due to the very strict measures introduced on 12 March 2020 upon confirmation of the first cases of COVID-19. A daily curfew was introduced, where individuals were allowed out once a day for 90 min to procure essentials. Private cars and inter-city transport were banned. On the 12th of March 2020, the Albanian Prime Minister declared a “war” on COVID-19. A 72-hour continuous curfew began, during which only food and/or medicine transport was allowed. The lockdown ended on 18 May 2020, and on 1 June 2020, the free movement (24 h) all over the country was restored. However, in 2021, in Eastern European countries and particularly in Albania, there has been an excess death rate from COVID-19, which has been linked to weaker regulation implementation and a lower vaccination coverage [18].
COVID-19 vaccination in Albania began on 11 January 2021, with the Comirnaty® (Pfizer/BioNTech) vaccine, initially targeting healthcare workers, nursing home residents, individuals with chronic diseases or mental health issues, and elderly people, starting with those over 90, then over 80, 70, and 60 years old [19]. As of early December 2021, when the vaccine was already made available free of charge to all population groups, according to the official figures, only about 38% of the Albanian population had received at least one dose of the COVID-19 vaccine, whereas about 34% of the population had received the full series of the vaccine [20].
In this context, the aim of our study was to assess the self-reported prevalence and sociodemographic factors associated with co-vaccination against seasonal influenza and COVID-19 and the main reasons for vaccine hesitancy in the adult population of Albania. We hypothesized a higher co-vaccination uptake among females (due to a greater health awareness than males), older people (due to more health concerns than younger individuals), and highly educated individuals (due to greater access to information and increased trust in scientific research compared to less educated individuals).
2. Materials and Methods
A cross-sectional study was conducted in Albania in November–December 2021.
2.1. Study Population and Sampling
The minimal required sample size was calculated at 840 individuals for different hypotheses related to sociodemographic differences in the prevalence of co-vaccination rates. However, we decided to increase the sample size up to 2000 individuals to increase the power of the study and perform a range of sub-analyses.
A consecutive sample of 1500 individuals aged 18 years and above was targeted for participation in the five biggest regions of Albania: Tirana (the capital), Elbasan, Fier, Vlora, and Shkodra. In each region, individuals were recruited in environments with a significant flow of people, such as shopping malls, bars, and outdoor environments of primary health care centres.
Of 1500 targeted individuals (aimed for a consecutive recruitment), 198 of them (≈13%) refused to participate. Hence, the final sample included in this study consisted of 1302 individuals aged ≥18 years (≈57% females; mean age: 38.3 ± 15.0 years), with an overall response rate of: 1302/1500 = 86.8%.
2.2. Data Collection
A structured and standardized questionnaire was administered to all participants by trained interviewers. The survey instrukent is presented in detail in Supplementary Material. The questionnaire inquired about co-vaccination status against seasonal influenza and COVID-19 (“Have you been co-vaccinated against seasonal influenza and COVID-19 with at least one dose?”). Potential answers consisted of “yes” vs. “no”. Furthermore, non-vaccinated participants were asked whether they had heard about vaccine availability, their willingness to take the vaccines, and the main reasons for vaccine hesitancy.
Sociodemographic characteristics of study participants (Table 1) included gender (males vs. females), age (categorized in the analyses into: 18–24, 25–34, 35–44, 45–54, 55–64, and ≥65 years), marital status (dichotomized into: married vs. not married), educational level (trichotomized into: low, middle, and high), and employment status (dichotomized into: employed vs. not employed and/or retired).
2.3. Ethical Aspects
The study was approved by the Scientific Council of the Albanian Institute of Public Health (Order No. 92/5; date: 4 October 2021). All participants were informed about the aim, objectives, and procedures of the survey and were assured about the confidentiality and anonymity of the study.
2.4. Statistical Analysis
Fisher’s exact test was used to compare the distribution of co-vaccination status by sociodemographic factors of study participants (Table 1).
Conversely, binary logistic regression was employed to assess the association of co-vaccination status with sociodemographic characteristics (Table 2). Firstly, crude (unadjusted) models were conducted (upper panel). Odds ratios (ORs: vaccinated vs. not vaccinated) and their respective 95% confidence intervals (95%CIs) and p-values were calculated. Afterwards, all sociodemographic factors (gender, age, marital status, educational level, and employment status) were entered simultaneously into the logistic regression models (lower panel). Multivariable-adjusted ORs and their respective (95%CIs) and p-values were calculated. Hosmer–Lemeshow test was used to assess the goodness-of-fit of the multivariable-adjusted model [21]. Interaction between age and educational level was assessed by the introduction of a multiplicative term between these two variables.
A p-value of ≤0.05 was considered statistically significant for all tests performed. The Statistical Package for the Social Sciences (SPSS, version 19.0) was used for the data analysis.
3. Results
3.1. Co-Vaccination Rate and Sociodemographic Distribution
Table 1 presents the distribution of seasonal influenza and COVID-19 co-vaccination status (at least one dose) by sociodemographic characteristics of study participants. Overall, about 28% of individuals were co-vaccinated against seasonal influenza and COVID-19. The prevalence of co-vaccination (against seasonal influenza and at least one dose against COVID-19) was non-significantly higher among females than males (about 29% vs. 25%, respectively), and among unemployed individuals than in those who were currently employed (31% vs. 26%, respectively). Conversely, the prevalence of co-vaccination was significantly higher among: older participants (65 years and above) compared to their youngest (18–24 years) counterparts (54% vs. only 22%, respectively); highly-educated participants compared with those with middle education (31% vs. 23%, respectively); and among married participants compared with those who were single, divorced or widowed (30% vs. 25%, respectively).
3.2. Association of Co-Vaccination Status with Sociodemographic Factors
Table 2 presents the association of co-vaccination status (against seasonal influenza and at least one dose against COVID-19) with sociodemographic factors of study participants. In crude (unadjusted) binary logistic regression models (upper panel), co-vaccination against seasonal influenza and COVID-19 was positively and significantly associated with older age (OR = 4.1, 95%CI = 2.4–7.0), and being married (OR = 1.3, 95%CI = 1.0–1.7). Furthermore, there was a significant relationship with educational level (overall p = 0.02), which was nevertheless inconsistent. Also, there was a positive and borderline statistically significant association with unemployment (OR = 1.3, 95%CI = 1.0–1.6).
In multivariable-adjusted binary logistic regression models (lower panel), the associations of co-vaccination status with marital status and employment disappeared, whereas the positive and graded relationship with age was accentuated (OR = 7.0, 95%CI = 3.7–12.9). Additionally, upon simultaneous adjustment for all sociodemographic factors, there was evidence of a strong positive and significant relationship between co-vaccination and high education (OR = 2.3, 95%CI = 1.4–3.6).
There was evidence of a significant interaction between age of participants and their educational level (multivariable-adjusted p-value of the interaction term between age and education: p = 0.018): there was no significant association between older age and co-vaccination among the low-educated participants (p = 0.255), as opposed to a strong positive and significant relationship among individuals with middle and/or high educational attainment (both p < 0.001) (Figure 1).
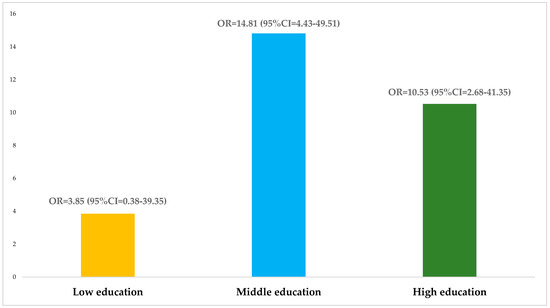
Figure 1.
Multivariable-adjusted association of co-vaccination status with older age (≥65 years) by educational level.
3.3. Reasons for Vaccine Hesitancy
Table 3 presents the level of knowledge about vaccine availability, willingness to take the vaccines against seasonal influenza and COVID-19, and reasons for vaccine hesitancy among non-vaccinated individuals. Among 941 participants who were not co-vaccinated, about 97% of them had heard and were aware of the availability of the vaccines against seasonal influenza and especially the vaccine against COVID-19. However, only around 13% of non-vaccinated individuals were willing to take the vaccines. Approximately 38% of non-vaccinated individuals were discouraged from getting the vaccines.
The main reasons for vaccines hesitancy (in descending order) included the following:
- -
- The belief that vaccines are harmful (72%);
- -
- The belief that vaccines are not effective (66%);
- -
- The belief that vaccines weaken the immune system (58%);
- -
- The belief that vaccines are not safe (56%);
- -
- The belief that it is better to overcome an illness naturally (52%);
- -
- The belief that COVID-19 and especially seasonal influenza are not dangerous diseases (31%);
- -
- The belief that vaccines have a spying device (17%).

Table 1.
Distribution of co-vaccination status by sociodemographic factors in a sample of Albanian adults (N = 1302).
Table 1.
Distribution of co-vaccination status by sociodemographic factors in a sample of Albanian adults (N = 1302).
| Sociodemographic Factors | Total (N = 1302) | Co-Vaccinated (N = 361) | Not Co-Vaccinated (N = 941) | p † |
|---|---|---|---|---|
| Overall sample | 1302 (100.0) * | 361 (27.7) | 941 (72.3) | - |
| Gender: | 0.117 | |||
| Male | 559 (100.0) | 142 (25.4) | 417 (74.6) | |
| Female | 737 (100.0) | 217 (29.4) | 520 (70.6) | |
| Age-group: | <0.001 | |||
| 18–24 years | 258 (100.0) | 57 (22.1) | 201 (77.9) | |
| 25–34 years | 385 (100.0) | 77 (20.0) | 308 (80.0) | |
| 35–44 years | 240 (100.0) | 63 (26.3) | 177 (73.8) | |
| 45–54 years | 178 (100.0) | 56 (31.5) | 122 (68.5) | |
| 55–64 years | 157 (100.0) | 65 (41.4) | 92 (58.6) | |
| ≥65 years | 80 (100.0) | 43 (53.8) | 37 (46.3) | |
| Marital status: | 0.037 | |||
| Married | 761 (100.0) | 229 (30.1) | 532 (69.9) | |
| Other | 529 (100.0) | 131 (24.8) | 398 (75.2) | |
| Educational level: | 0.018 | |||
| Low | 143 (100.0) | 41 (28.7) | 102 (71.3) | |
| Middle | 479 (100.0) | 111 (23.2) | 368 (76.8) | |
| High | 677 (100.0) | 208 (30.7) | 469 (69.3) | |
| Employment status: | 0.074 | |||
| Employed | 861 (100.0) | 225 (26.1) | 636 (73.9) | |
| Unemployed and/or retired | 424 (100.0) | 131 (30.9) | 293 (69.1) |
* Absolute numbers and their respective row percentages (in parentheses). Discrepancies in the totals are due to the missing values for the following variables: gender (n = 6), age (n = 4), marital status (n = 12), educational level (n = 3), and employment status (n = 17). † p-values from Fisher’s exact test.

Table 2.
Association of co-vaccination status with sociodemographic factors in a sample of Albanian adults (N = 1302); unadjusted and multivariable-adjusted results from binary logistic regression models.
Table 2.
Association of co-vaccination status with sociodemographic factors in a sample of Albanian adults (N = 1302); unadjusted and multivariable-adjusted results from binary logistic regression models.
| Upper Panel: Crude (Unadjusted) Binary Logistic Regression Models | |||
|---|---|---|---|
| Sociodemographic Factors | OR * | 95%CI * | p * |
| Gender: | 0.108 | ||
| Male | 1.00 | Reference | |
| Female | 1.23 | 0.96–1.57 | |
| Age-group: | <0.001 (5) † | ||
| 18–24 years | 1.00 | Reference | - |
| 25–34 years | 0.88 | 0.60–1.30 | 0.522 |
| 35–44 years | 1.26 | 0.83–1.89 | 0.279 |
| 45–54 years | 1.62 | 1.05–2.49 | 0.029 |
| 55–64 years | 2.49 | 1.62–3.84 | <0.001 |
| ≥65 years | 4.10 | 2.42–6.95 | <0.001 |
| Marital status: | 0.036 | ||
| Other | 1.00 | Reference | |
| Married | 1.31 | 1.02–1.68 | |
| Educational level: | 0.018 (2) † | ||
| Low | 1.00 | Reference | - |
| Middle | 0.75 | 0.49–1.14 | 0.180 |
| High | 1.10 | 0.74–1.64 | 0.628 |
| Employment status: | 0.073 | ||
| Employed | 1.00 | Reference | |
| Unemployed and/or retired | 1.26 | 0.98–1.63 | |
| Lower panel: multivariable-adjusted binary logistic regression models | |||
| Sociodemographic factors | OR * | 95%CI * | p * |
| Gender: | 0.201 | ||
| Male | 1.00 | Reference | |
| Female | 1.19 | 0.91–1.55 | |
| Age-group: | <0.001 (5) † | ||
| 18–24 years | 1.00 | Reference | - |
| 25–34 years | 1.01 | 0.65–1.56 | 0.967 |
| 35–44 years | 1.72 | 1.04–2.83 | 0.035 |
| 45–54 years | 2.56 | 1.50–4.38 | <0.001 |
| 55–64 years | 4.28 | 2.48–7.37 | <0.001 |
| ≥65 years | 6.95 | 3.74–12.93 | <0.001 |
| Marital status: | 0.882 | ||
| Other | 1.00 | Reference | |
| Married | 0.98 | 0.71–1.34 | |
| Educational level: | <0.001 (2) † | ||
| Low | 1.00 | Reference | - |
| Middle | 0.91 | 0.58–1.42 | 0.664 |
| High | 2.26 | 1.43–3.58 | <0.001 |
| Employment status: | 0.373 | ||
| Employed | 1.00 | Reference | |
| Unemployed and/or retired | 1.15 | 0.85–1.54 | |
* Odds ratios (ORs: co-vaccinated vs. not co-vaccinated) and their respective 95% confidence intervals (95%CIs) and p-values from binary logistic regression models. † Overall p-value and degrees of freedom (in parentheses).

Table 3.
Knowledge about vaccine availability, willingness to take the vaccines, and reasons for vaccine hesitancy among non-vaccinated participants (N = 941).
Table 3.
Knowledge about vaccine availability, willingness to take the vaccines, and reasons for vaccine hesitancy among non-vaccinated participants (N = 941).
| Knowledge about Vaccine Availability, Willingness to Take the Vaccines, and Reasons for Vaccine Hesitancy | Number * | Percentage |
|---|---|---|
| Heard about the availability of the vaccines: | ||
| Yes | 916 | 97.3 |
| No | 21 | 2.2 |
| Not sure | 4 | 0.4 |
| Willingness to take the vaccines: | ||
| Yes | 117 | 12.6 |
| No | 635 | 68.2 |
| Undecided | 179 | 19.2 |
| Has anyone discouraged you from getting the vaccines? | ||
| Yes | 356 | 38.2 |
| No | 562 | 60.4 |
| Not sure | 13 | 1.4 |
| Hesitancy due to the belief that vaccines weaken the immune system: | ||
| Yes | 510 | 58.0 |
| No | 247 | 28.1 |
| Don’t know | 123 | 14.0 |
| Hesitancy based on the belief that vaccines are harmful: | ||
| Yes | 633 | 71.8 |
| No | 142 | 16.1 |
| Don’t know | 107 | 12.1 |
| Hesitancy based on the belief that vaccines are not safe: | ||
| Yes | 483 | 55.9 |
| No | 86 | 10.0 |
| Don’t know | 295 | 34.1 |
| Hesitancy based on the belief that it is better to overcome an illness naturally: | ||
| Yes | 455 | 52.3 |
| No | 289 | 33.2 |
| Don’t know | 126 | 14.5 |
| Hesitancy based on the belief that COVID-19 and especially seasonal influenza are not dangerous diseases: | ||
| Yes | 271 | 31.0 |
| No | 460 | 52.7 |
| Don’t know | 142 | 16.3 |
| Hesitancy based on the belief that vaccines are not effective: | ||
| Yes | 584 | 66.3 |
| No | 137 | 15.6 |
| Don’t know | 160 | 18.2 |
| Hesitancy based on the belief that vaccines have a spying device: | ||
| Yes | 148 | 17.1 |
| No | 461 | 53.1 |
| Don’t know | 259 | 29.8 |
| Hesitancy based on ethical and moral reasons: | ||
| Yes | 50 | 5.8 |
| No | 760 | 88.0 |
| Don’t know | 54 | 6.3 |
| Hesitancy based on religious grounds: | ||
| Yes | 40 | 4.6 |
| No | 795 | 92.3 |
| Don’t know | 26 | 3.0 |
* Discrepancies in the totals are due to the missing values for the following items: heard about the availability of the vaccines (n = 4), willingness to take the vaccines (n = 10), discouraged for taking the vaccines (n = 10), hesitancy due to the belief that vaccines weaken the immune system (n = 61), hesitancy due to the belief that vaccines are harmful (n = 59), hesitancy due to the belief that vaccines are not safe (n = 77), hesitancy due to the belief that it is better to overcome an illness naturally (n = 71), hesitancy based on the belief that COVID-19 and especially seasonal influenza are not dangerous diseases (n = 68), hesitancy based on the belief that vaccines are not effective (n = 60), hesitancy based on the belief that vaccines have a spying device (n = 73), hesitancy based on ethical and moral reasons (n = 77), and hesitancy based on religious grounds (n = 80).
4. Discussion
4.1. Main Findings
A salient finding of our study consists of a low co-vaccination rate against seasonal influenza and COVID-19 in Albania during the first year when the COVID-19 vaccine was made available to the general population. Hence, only slightly more than one in four adults had been co-vaccinated against seasonal influenza and had received at least one dose of the COVID-19 vaccine regardless of its availability free-of-charge. Notably, there were significant sociodemographic disparities with younger participants and less educated individuals exhibiting the lowest levels of vaccine hesitancy.
Among the unvaccinated individuals, the main reasons for vaccine hesitancy were driven by concerns about safety, effectiveness, and potential health risks, with a significant proportion of study participants believing that vaccines are harmful, weaken the immune system, or are unnecessary compared to natural infection.
4.2. Comparison with Other Countries
As of early December 2021, the official COVID-19 vaccination rate for at least one dose in the Western Balkan countries was as follows (in ascending order): about 25% in Bosnia and Herzegovina, 28% in Bulgaria, 40% in North Macedonia, 43% in Montenegro, 47% in Kosovo, 48% in Serbia, and 55% in Croatia [20]. Albania (38%) ranked among the lowest in the region [20]. Furthermore, the official reported vaccination rate for Albania is higher than the self-reported prevalence in our study sample (28%).
Regarding the full series of the COVID-19 vaccine, the official rates in early December 2021 were reported as follows: 22% in Bosnia and Herzegovina, 27% in Bulgaria, 38% in Montenegro, 39% in North Macedonia, 42% in Kosovo, 46% in Serbia, and 50% in Croatia [20]. Similar to the at least one dose, Albania (about 34%) ranked among the lowest countries in the region [20].
On the other hand, in early December 2021, in all countries of the Western Balkan region, including Albania, the vaccination rates for both at least one dose and the full series were higher among the older population subgroups compared with younger categories [20]. This is compatible with our findings based on self-reported information of Albanian adults.
On another note, during July–September 2021, a cross-sectional study on vaccine hesitancy including seasonal influenza and COVID-19 was conducted in a sample of about 1600 adult individuals pertinent to five Western Balkan countries, including Albania, Bosnia and Herzegovina, North Macedonia, Montenegro, and Serbia [22]. This study reported a moderate trust in societal factors and a moderately high level of social responsibility in all five countries [22]. Furthermore, according to this study, the greatest trust relied on health professionals [22].
Another report from a study conducted in these five Western Balkan countries [23] has indicated that the largest proportion of unvaccinated adult individuals willing to get vaccinated in the future was observed in Montenegro and Albania (about 40% in each), whereas the lowest proportion was evident in Serbia (≈23%). According to this study [23], sociodemographic characteristics were not significantly associated with the intention to get vaccinated against seasonal influenza and especially against COVID-19 in most of the countries (23%). On the other hand, the strongest determinant of seasonal influenza and/or COVID-19 vaccination intention in the countries of the Western Balkans was the higher sense of social responsibility [23].
The lower rates of seasonal influenza and especially COVID-19 vaccination in Western Balkan countries compared to Western European countries have been linked to societal distrust, an issue which has jeopardized the sustainability of vaccination programs [24]. In Albania, social distrust has been reported to be the lowest among all countries of the Western Balkan region [24]. In general, a lower educational attainment has been linked to social distrust in Western Balkan countries [24], which is in line with our findings. Yet, predictors of societal trust in the Western Balkans vary across countries, suggesting the need for different approaches in communication campaigns [24].
In Albania, during the season 2020–2021, the flu vaccine coverage was estimated at 86% with a predominance of application in the age group over 60 years (Institute of Public Health, Albania). For the season 2021–2022, the vaccine coverage for seasonal influenza was 91%, again with a predominance of the age group over 60 years, and individuals with concomitant cardiovascular diseases and diabetes (Institute of Public Health, Albania). Hence, on the face of it, the low co-vaccination rates observed in our study are due to the low compliance (hesitancy) related to the COVID-19 vaccine rather than the seasonal influenza vaccine.
According to a survey conducted in 2022 in the European Union (EU) countries [25], about 82% of individuals agreed that vaccines (including seasonal influenza and COVID-19 vaccines) are important; 85% of individuals agreed that vaccines are effective; and 82% of individuals agreed that vaccines are safe [25]. Regarding the specific role of the COVID-19 vaccine [25], around 77% of participants believed that COVID-19 vaccines are effective at preventing severe disease; 67% agreed that COVID-19 vaccines are effective against getting infected with SARS-CoV-2; and 66% agreed that COVID-19 vaccines are effective at preventing transmission of the SARS-CoV-2 virus to others [25]. Our findings indicate a considerably higher level of vaccine hesitancy in the Albanian population compared with the EU public.
Conversely, a study conducted in five countries including Albania on nurses intention to get vaccinated with a COVID-19 vaccine, it was reported that female gender, living in a country with low mortality rate, low knowledge of COVID-19, infection with COVID-19 and non-vaccination with influenza vaccine the last two years were the key reasons for not willing to get vaccinated [26]. Regarding student populations, female gender, working experience in healthcare facilities during the pandemic, lack of trust in doctors, and government experts’ low knowledge of COVID-19 were some key reasons for unwillingness to get vaccinated [27]. Possible long-term effects of vaccines, including seasonal influenza, were mentioned as a key reason for hesitancy among Albanian students [28]. Safety and efficacy were mentioned as key reasons for possible vaccination among Albanian students, including vaccination against seasonal influenza [29]. As for health care workers, a prospective study conducted in Albania in February–May 2021 [30] found that COVID-19 vaccine booster dose uptake was very low, particularly among younger, female, and non-physician health professionals, despite evidence demonstrating the added benefit of boosters in preventing infection and severe disease [31]. Furthermore, a fairly recent publication reported that among Albanian health care workers interviewed in 2022–2023, primary series COVID-19 vaccine coverage was high, but COVID-19 booster doses and seasonal influenza vaccines were low, especially among younger and non-physicians [32].
The finding that over 97% of unvaccinated respondents in our study were aware of the existence of vaccines, yet only approximately 13% expressed willingness to receive them, highlights a critical disconnection between awareness and acceptance—a hallmark of entrenched vaccine hesitancy among Albanian adults. This suggests that lack of information is not the primary barrier in the Albanian context; rather, deep-seated mistrust, misinformation, or value-based opposition may be driving refusal. Such a pattern points to the limitations of awareness-raising campaigns alone and highlights the need for more nuanced, trust-building interventions that directly address underlying fears, beliefs, and misinformation. It also reflects a broader behavioral and sociocultural resistance that public health strategies must confront in Albania, particularly through targeted communication tailored to the psychological and community-level determinants of vaccine acceptance.
Notably, vaccine hesitancy in Albania has been influenced by a complex interplay of cultural and historical factors rooted in the country’s socio-political past. Decades of authoritarian communist rule (1945–1991), during which public trust in government institutions eroded due to censorship and forced compliance, have contributed to enduring skepticism toward state-led public health initiatives [18]. Additionally, Albania’s transition to democracy was marked by political instability and health system underfunding, which further weakened institutional credibility. Culturally, a strong reliance on informal networks and familial advice often outweighs expert recommendations, fostering susceptibility to misinformation, especially via social media [18]. Religious beliefs, though not widespread barriers, and regional disparities—particularly between urban and rural areas—also contribute to differing levels of vaccine acceptance. These historical legacies and cultural dynamics have shaped public perception, making top-down vaccination campaigns less effective without strong community engagement and trust-building efforts.
4.3. Study Limitations
Our study may have several limitations, including sample representativeness and the possibility of information biases. Recruitment of individuals in high-traffic environments such as shopping malls, bars, and outdoor areas of primary health care centres may have systematically excluded certain population groups, e.g., those less socially active, with limited mobility, or those who avoid public spaces due to health concerns or socioeconomic constraints. Thus, the generalizability of the findings of this study should be made with caution.
Another limitation of this study is its exclusive focus on co-vaccination coverage for seasonal influenza and COVID-19, without disaggregating coverage estimates for each vaccine individually. Without separate coverage data, it is difficult to assess differential uptake patterns across subpopulations, understand barriers specific to each vaccine, or evaluate the effectiveness of disease-specific vaccination campaigns. This aggregation may mask important epidemiological insights necessary for optimizing future immunization strategies. On the other hand, by focusing on co-vaccination coverage for seasonal influenza and COVID-19, our study offers valuable insight into the extent to which individuals received both vaccines concurrently, an increasingly important metric for integrated immunization strategies. This approach captures real-world patterns of dual vaccine uptake, which are particularly relevant for optimizing delivery logistics, understanding the reach of co-administration campaigns, and identifying populations that may benefit from streamlined vaccination efforts. Assessing co-coverage, rather than individual vaccine uptake, also reflects the potential impact of bundled public health messaging and can inform the design of interventions aimed at improving the overall efficiency and effectiveness of adult immunization programs.
Also, the study sample had an underrepresented elderly population (80 individuals, or only about 6% of the overall sample). Furthermore, reliance on self-reported data about vaccination status may have resulted in social desirability bias, as individuals might have felt pressured to provide a socially acceptable response in the Albanian context. Additionally, respondents’ answers regarding vaccines hesitancy and awareness may have been influenced by their perceptions of what is expected or acceptable, rather than their actual beliefs or knowledge, potentially distorting the true reasons behind vaccine refusal or hesitancy.
4.4. Suggestions for Further Research
Nonetheless, this study provides useful evidence about co-vaccination rate and the main reasons for vaccine hesitancy in the Albanian population. Longitudinal studies on vaccine uptake are needed to explore the attitude changes over time in the Albanian population. Indeed, longitudinal studies assessing changes in vaccination rates, booster uptake, and shifts in perceptions regarding vaccine safety and effectiveness could provide valuable insights into the long-term impact of public health messaging and policies in Albania. Furthermore, there is a need for qualitative research on vaccine hesitancy determinants to provide deeper insights into the psychological, cultural, and informational factors driving vaccine hesitancy in Albania. From this perspective, in-depth interviews or focus groups with unvaccinated individuals could help uncover underlying concerns, misinformation sources, and potential strategies to improve vaccine acceptance in future public health campaigns in Albania and similar settings.
4.5. Policy Implications
The observed interaction between age and education in our study indicates that educational attainment modified the effect of age on vaccine uptake. Specifically, among Albanian individuals with middle or high education levels, older age was strongly and significantly associated with a higher likelihood of co-vaccination, indicating that as these individuals age, they may become more health-conscious, more trusting of medical recommendations, or more exposed to accurate health information, thereby increasing vaccine acceptance. In contrast, among individuals with low educational attainment, age did not significantly influence co-vaccination rates, suggesting that structural barriers (e.g., access, health literacy) and persistent mistrust or misinformation may override any age-related increases in risk perception or healthcare engagement. This differential pattern implies that educational background conditions how age-related factors—such as increased vulnerability to severe illness or cumulative health system contact—translate into vaccine behavior in the Albanian adult population. This highlights the importance of tailoring public health interventions not only by age but also by education, with targeted outreach needed for older adults with low education who may remain underserved or unconvinced despite their higher risk profile.
This study fills a critical regional research gap by providing the first in-depth, population-based assessment of co-vaccination against seasonal influenza and COVID-19 in Albania—a country for which such data has been notably scarce compared to neighboring Western Balkan countries. While regional counterparts like Serbia, North Macedonia, and Montenegro have reported on vaccine uptake trends and hesitancy drivers, Albania has lacked representative, empirical evidence linking sociodemographic determinants with dual vaccine coverage. By identifying key predictors such as age and education level, and quantifying prevalent misperceptions fueling hesitancy, our study not only informs national public health strategies but also enables more accurate cross-country comparisons within the Western Balkans. The findings thus provide a foundation for harmonized, region-specific interventions aimed at improving vaccination rates and combating misinformation across similar sociopolitical and healthcare contexts.
At a wider international level, there is a need for strengthening global misinformation countermeasures and health communication strategies. This includes developing standardized, evidence-based health communication strategies tailored to different cultural and linguistic contexts, as well as leveraging social media and community-based outreach to address vaccine hesitancy. Indeed, strengthening regulatory frameworks to counteract the spread of false health information, while promoting transparent and accessible scientific communication, is essential to ensuring higher vaccine uptake and preparedness for future public health emergencies. Moreover, it is important to use the current results for managing vaccination hesitancy for other possible infectious diseases. This could help policymakers to undertake the possible measures for the education of the population through awareness-raising campaigns.
5. Conclusions
In conclusion, our study evidenced a relatively low co-vaccination rate against seasonal influenza and COVID-19 in Albania during the first year when the vaccine was available free of charge to the overall population, with significant sociodemographic disparities. Older age and higher educational attainment were identified as independent positive predictors of co-vaccination uptake, suggesting the need for targeted public health strategies to address vaccine hesitancy, particularly among younger and less-educated population categories. Our findings emphasize the importance of tailored communication campaigns and community-based interventions to improve vaccine coverage and mitigate the impact of infectious diseases in Albania and elsewhere.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/covid5080132/s1, Supplementary Material: Survey Instrument.
Author Contributions
Conceptualization, G.Q. and G.B.; methodology, G.Q., E.A.M., S.B. and G.B.; software, G.Q. and G.B.; validation, G.Q., E.A.M., A.F., E.T., S.B. and G.B.; formal analysis, G.B.; investigation, G.Q.; resources, G.Q., A.F. and S.B.; data curation, G.B.; writing—original draft preparation, G.Q. and G.B.; writing—review and editing, G.Q., E.A.M., A.F., E.T., S.B. and G.B.; visualization, G.Q.; supervision, G.B.; project administration, G.Q.; funding acquisition, G.Q. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the United Nations Children’s Fund (UNICEF) Office in Albania.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Scientific Council of the Albanian Institute of Public Health (Order No. 92/5; date: 4 October 2021). All participants were informed about the aim, objectives, and procedures of the survey and were assured about the confidentiality and anonymity of the study.
Informed Consent Statement
All participants were informed about the aim, objectives, and procedures of the survey and were assured of the confidentiality and anonymity of the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
This study was conducted by the National Institute of Public Health in Albania.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019/ (accessed on 13 February 2025).
- Morciglio, A.; Zia, R.K.P.; Hyman, J.M.; Jiang, Y. Understanding the oscillations of an epidemic due to vaccine hesitancy. Math. Biosci. Eng. 2024, 21, 6829–6846. [Google Scholar] [CrossRef]
- World Health Organization. Global Vaccine Market Report 2024; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar] [CrossRef]
- O’Riordan, M.; Fitzpatrick, F. The impact of economic recession on infection prevention and control. J. Hosp. Infect. 2015, 89, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Remy, V.; Largeron, N.; Quilici, S.; Carroll, S. The Economic Value of Vaccination: Why Prevention Is Wealth. Value Health 2014, 17, A450. [Google Scholar] [CrossRef]
- Department of Health and Human Services. COVID-19 Vaccine Distribution: The Process. Available online: https://www.hhs.gov/coronavirus/covid-19-vaccines/index.html (accessed on 13 February 2025).
- Daniel, W.; Nivet, M.; Warner, J.; Podolsky, D.K. Early evidence of the effect of SARS-CoV-2 vaccine at one medical center. N. Engl. J. Med. 2021, 384, 1962–1963. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 13 February 2025).
- Johns Hopkins Coronavirus Resource Center. Impact of Opening and Closing Decisions by State: A Look at How Social Distancing Measures May Have Inffuenced Trends in COVID-19 Cases and Death. Available online: https://coronavirus.jhu.edu/data/state-timeline (accessed on 13 February 2025).
- Murray, C.J.L.; Piot, P. The potential future of the COVID-19 pandemic: Will SARS-CoV-2 become a recurrent seasonal infection? JAMA 2021, 325, 1249–1250. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Goodwin, R.; Ben-Ezra, M.; Takahashi, M.; Luu, L.-A.N.; Borsfay, K.; Kovács, M.; Hou, W.K.; Hamama-Raz, Y. Psychological factors underpinning vaccine willingness in Israel, Japan and Hungary. Sci. Rep. 2022, 12, 439. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Stoler, J.; Klofstad, C.A.; Enders, A.M.; Uscinski, J.E. Sociopolitical and psychological correlates of COVID-19 vaccine hesitancy in the United States during summer 2021. Soc. Sci. Med. 2022, 306, 115112. [Google Scholar] [CrossRef]
- Enders, A.M.; Uscinski, J.; Klofstad, C.; Stoler, J. On the relationship between conspiracy theory beliefs, misinformation, and vaccine hesitancy. PLoS ONE 2022, 17, e0276082. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Ylli, A.; Wu, Y.Y.; Burazeri, G.; Pirkle, C.; Sentell, T. The lower COVID-19 related mortality and incidence rates in Eastern European countries are associated with delayed start of community circulation. PLoS ONE 2020, 15, e0243411. [Google Scholar] [CrossRef] [PubMed]
- Ylli, A.; Burazeri, G.; Wu, Y.Y.; Sentell, T. COVID-19 excess deaths in Eastern European countries associated with weaker regulation implementation and lower vaccination coverage. East. Mediterr. Health 2022, 28, 776–780. [Google Scholar] [CrossRef]
- Council of Ministers of the Republic of Albania. Start of Vaccination Against COVID-19. 11 January 2021. Available online: https://www.kryeministria.al/newsroom/konferenca-per-shtyp-e-kryeministrit-edi-rama-para-nisjes-se-jetesimit-te-fushates-shqiperia-buzeqesh/ (accessed on 13 February 2025).
- World Health Organization. WHO/Europe COVID-19 Vaccine Program Monitor. Available online: https://worldhealthorg.shinyapps.io/EURO_COVID-19_vaccine_monitor/ (accessed on 13 February 2025).
- Hosmer, D.; Lemeshow, S. Applied Logistic Regression; Wiley & Sons: New York, NY, USA, 1989. [Google Scholar]
- Matovic-Miljanovic, S.; Cvjetkovic, S.; Jeremic-Stojkovic, V.; Mandic-Rajcevic, S. COVID-19 vaccine hesitancy in five Western Balkan countries. Eur. J. Public Health 2022, 32, ckac129.736. [Google Scholar] [CrossRef]
- Jeremic-Stojkovic, V.; Cvjetkovic, S.; Jankovic, J.; Mandic-Rajcevic, S.; Matovic-Miljanovic, S.; Stevanovic, A.; Jovic-Vranes, A.; Stamenkovic, Z. Attitudes towards COVID-19 vaccination and intention to get vaccinated in Western Balkans: Cross-sectional survey. Eur. J. Public Health 2023, 33, 496–501. [Google Scholar] [CrossRef]
- Cvjetkovic, S.; Jeremic-Stojkovic, V.; Mandic-Rajcevic, S.; Matovic-Miljanovic, S.; Jankovic, J.; Jovic-Vranes, A.; Stevanovic, A.; Stamenkovic, Z. Societal Trust Related to COVID-19 Vaccination: Evidence from Western Balkans. Sustainability 2022, 14, 13547. [Google Scholar] [CrossRef]
- de Figueiredo, A.; Eagan, R.L.; Hendrickx, G.; Karafillakis, E.; van Damme, P.; Larson, H.J. State of Vaccine Confidence in the European Union; European Commission; Publications Office of the European Union: Luxembourg, 2022. [Google Scholar]
- Patelarou, A.; Saliaj, A.; Galanis, P.; Pulomenaj, V.; Prifti, V.; Sopjani, I.; Mechili, E.A.; Laredo-Aguilera, J.A.; Kicaj, E.; Kalokairinou, A.; et al. Predictors of nurses’ intention to accept COVID-19 vaccination: A cross-sectional study in five European countries. J. Clin. Nurs. 2022, 31, 1258–1266. [Google Scholar] [CrossRef]
- Patelarou, E.; Galanis, P.; Mechili, E.A.; Argyriadi, A.; Argyriadis, A.; Asimakopoulou, E.; Brokaj, S.; Bucaj, J.; Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; et al. Factors influencing nursing students’ intention to accept COVID-19 vaccination: A pooled analysis of seven European countries. Nurse Educ. Today 2021, 104, 105010. [Google Scholar] [CrossRef]
- Buonomo, E.; Cenko, F.; Piunno, G.; Di Giovanni, D.; Gjini, E.; Kërpi, B.; Carestia, M.; Moramarco, S.; Ferrari, C.; Coppeta, L. Vaccine hesitancy, knowledge, and COVID-19 vaccination in a sample of Italian and Albanian healthcare students attending an University in Albania. Trop. Med. Infect. Dis. 2024, 9, 57. [Google Scholar] [CrossRef]
- Kongo, E.; Shpati, K.; Dama, A.; Ymeraj, S.; Murati, E.; Veliaj, U.; Xinxo, S. Determinant Factors of Voluntary or Mandatory Vaccination against COVID-19: A Survey Study among Students at Albanian University. Vaccines 2023, 11, 1215. [Google Scholar] [CrossRef]
- Sridhar, S.; Fico, A.; Preza, I.; Hatibi, I.; Sulo, J.; Kissling, E.; Daja, R.; Ibrahim, R.; Lemos, D.; Rubin-Smith, J.; et al. COVID-19 Vaccine Effectiveness among Healthcare Workers in Albania (COVE-AL): Protocol for a Prospective Cohort Study and Cohort Baseline Data. BMJ Open 2022, 12, e057741. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, P.; Schmid, A.; Sulo, J.; Preza, I.; Hasibra, I.; Kissling, E.; Fico, A.; Sridhar, S.; Rubin-Smith, J.E.; Kota, M.; et al. Factors Associated with Receipt of COVID-19 Vaccination and SARS-CoV-2 Seropositivity among Healthcare Workers in Albania (February 2021–June 2022): Secondary Analysis of a Prospective Cohort Study. Lancet Reg. Health Eur. 2023, 27, 100584. [Google Scholar] [CrossRef] [PubMed]
- Xhaferi, A.; Bino, S.; Daja, R.; Vasili, A.; Sulo, J.; Mebonia, N.; Ndreu, E.; Nika, M.; Jani, N.; Dabaj, E.; et al. Sociodemographic and Occupational Factors Associated with COVID-19 Vaccine and Influenza Vaccine Uptake among Healthcare Workers, in Albania, 2022–2023: A Multicenter Study. Clin. Infect. Dis. 2025, 81, 30–40. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).