Characterization of the SARS-CoV-2 Mutation Pattern Generated In Vitro by the Antiviral Action of Lycorine
Abstract
1. Introduction
2. Materials and Methods
2.1. SARS-CoV-2 Isolates and Cell Culture
2.2. Antiviral Preparation and Concentration Selection
2.3. Serial Passage Protocol
2.4. Viral Quantification
2.5. RNA Extraction and Whole-Genome Sequencing
2.6. Genome Assembly and Analysis
3. Results
3.1. In Vitro Antiviral Activity
3.2. Genome Assembly
3.3. Mutation Patterns
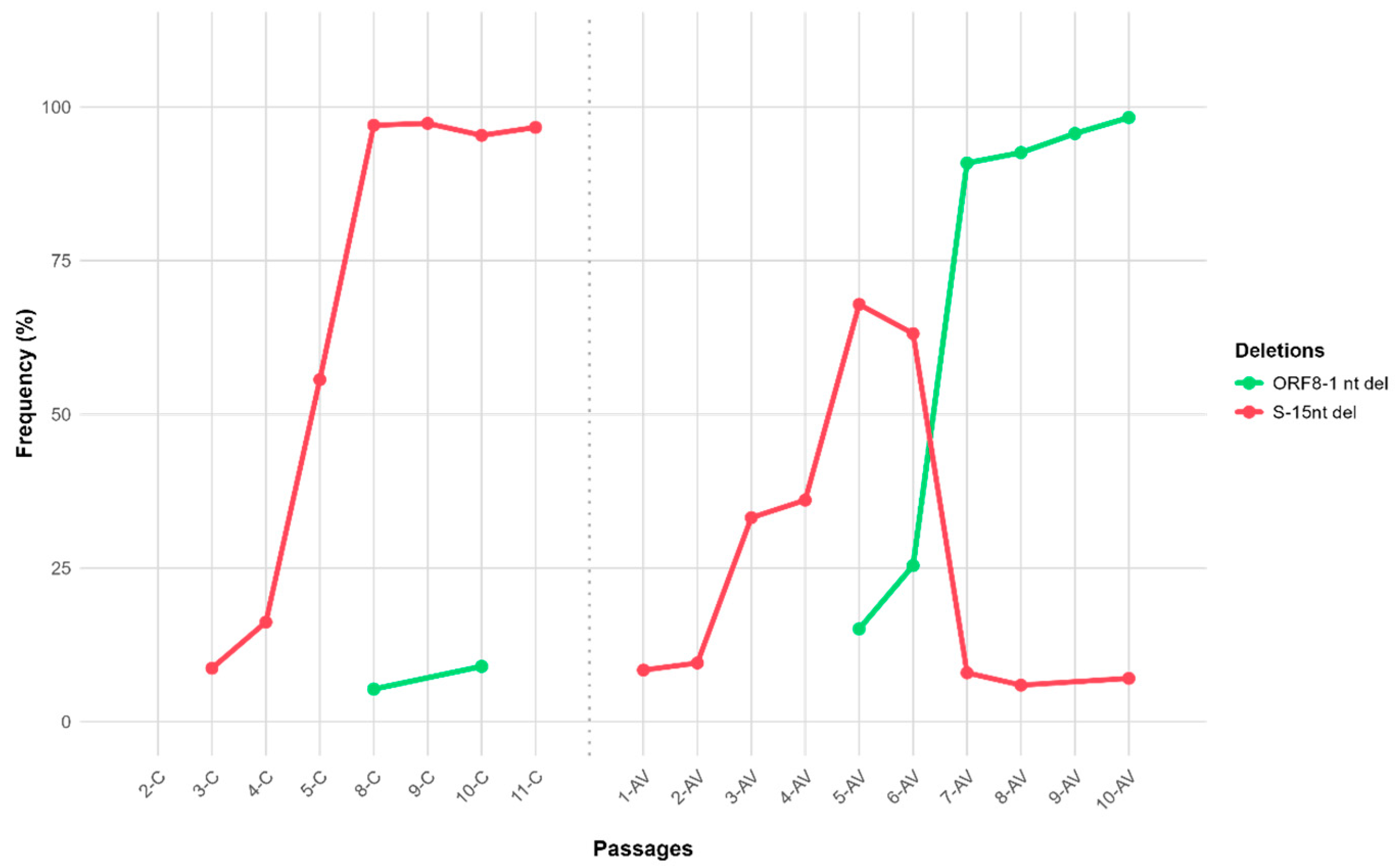
3.3.1. Variants in Untreated Passages
3.3.2. Variants in Lycorine-Treated Passages
3.4. Comparative Analysis
4. Discussion
4.1. Functional Implications of Selected Mutations
4.1.1. Non-Structural Protein Mutations
4.1.2. Structural Proteins
4.1.3. Accessory Proteins
4.2. Lycorine’s Selective Pressure and Mutational Pattern
4.3. Clinical, Surveillance, and Development Implications
4.4. Study Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chung, Y.-S.; Lam, C.-Y.; Tan, P.-H.; Tsang, H.-F.; Wong, S.-C.C. Comprehensive Review of COVID-19: Epidemiology, Pathogenesis, Advancement in Diagnostic and Detection Techniques, and Post-Pandemic Treatment Strategies. Int. J. Mol. Sci. 2024, 25, 8155. [Google Scholar] [CrossRef]
- Kumar, A.; Sharma, A.; Tirpude, N.V.; Thakur, S.; Kumar, S. Combating the Progression of Novel Coronavirus SARS-CoV-2 Infectious Disease: Current State and Future Prospects in Molecular Diagnostics and Drug Discovery. CMM 2023, 23, 127–146. [Google Scholar] [CrossRef]
- Carabelli, A.M.; Peacock, T.P.; Thorne, L.G.; Harvey, W.T.; Hughes, J.; COVID-19 Genomics UK Consortium; Peacock, S.J.; Barclay, W.S.; de Silva, T.I.; Towers, G.J.; et al. SARS-CoV-2 Variant Biology: Immune Escape, Transmission and Fitness. Nat. Rev. Microbiol. 2023, 21, 162–177. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Lee, S.-S. A Detailed Overview of Immune Escape, Antibody Escape, Partial Vaccine Escape of SARS-CoV-2 and Their Emerging Variants with Escape Mutations. Front. Immunol. 2022, 13, 801522. [Google Scholar] [CrossRef]
- Jena, D.; Ghosh, A.; Jha, A.; Prasad, P.; Raghav, S.K. Impact of Vaccination on SARS-CoV-2 Evolution and Immune Escape Variants. Vaccine 2024, 42, 126153. [Google Scholar] [CrossRef]
- Aiello, T.F.; García-Vidal, C.; Soriano, A. Antiviral Drugs Against SARS-CoV-2. Rev. Esp. Quimioter. 2022, 35, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Jayk Bernal, A.; Gomes Da Silva, M.M.; Musungaie, D.B.; Kovalchuk, E.; Gonzalez, A.; Delos Reyes, V.; Martín-Quirós, A.; Caraco, Y.; Williams-Diaz, A.; Brown, M.L.; et al. Molnupiravir for Oral Treatment of COVID-19 in Nonhospitalized Patients. N. Engl. J. Med. 2022, 386, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Maas, B.M.; Strizki, J.; Miller, R.R.; Kumar, S.; Brown, M.; Johnson, M.G.; Cheng, M.; De Anda, C.; Rizk, M.L.; Stone, J.A. Molnupiravir: Mechanism of Action, Clinical, and Translational Science. Clin. Transl. Sci. 2024, 17, e13732. [Google Scholar] [CrossRef] [PubMed]
- Teli, D.; Balar, P.; Patel, K.; Sharma, A.; Chavda, V.; Vora, L. Molnupiravir: A Versatile Prodrug Against SARS-CoV-2 Variants. Metabolites 2023, 13, 309. [Google Scholar] [CrossRef]
- Hashemian, S.M.R.; Sheida, A.; Taghizadieh, M.; Memar, M.Y.; Hamblin, M.R.; Bannazadeh Baghi, H.; Sadri Nahand, J.; Asemi, Z.; Mirzaei, H. Paxlovid (Nirmatrelvir/Ritonavir): A New Approach to COVID-19 Therapy? Biomed. Pharmacother. 2023, 162, 114367. [Google Scholar] [CrossRef]
- Yang, Z. Elucidation of the Pharmacological Development and Action Mechanism of Remdesivir and Paxlovid in Combatting COVID-19. MedScien 2024, 1, 1752. [Google Scholar] [CrossRef]
- Zhang, Y.-N.; Zhang, Q.-Y.; Li, X.-D.; Xiong, J.; Xiao, S.-Q.; Wang, Z.; Zhang, Z.-R.; Deng, C.-L.; Yang, X.-L.; Wei, H.-P.; et al. Gemcitabine, Lycorine and Oxysophoridine Inhibit Novel Coronavirus (SARS-CoV-2) in Cell Culture. Emerg. Microbes Infect. 2020, 9, 1170–1173. [Google Scholar] [CrossRef]
- Jin, Y.-H.; Min, J.S.; Jeon, S.; Lee, J.; Kim, S.; Park, T.; Park, D.; Jang, M.S.; Park, C.M.; Song, J.H.; et al. Lycorine, a Non-Nucleoside RNA Dependent RNA Polymerase Inhibitor, as Potential Treatment for Emerging Coronavirus Infections. Phytomedicine 2021, 86, 153440. [Google Scholar] [CrossRef]
- Kurt, B. Investigation of The Potential Inhibitor Effects of Lycorine On Sars-Cov-2 Main Protease (Mpro) Using Molecular Dynamics Simulations and MMPBSA. Int. J. Life Sci. Biotechnol. 2022, 5, 424–435. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A Simple Method of Estimating FIfty Percent Endpoints. Am. J. Trop. Med. Hyg. 1938, 27, 493–497. [Google Scholar]
- Bhoyar, R.C.; Jain, A.; Sehgal, P.; Divakar, M.K.; Sharma, D.; Imran, M.; Jolly, B.; Ranjan, G.; Rophina, M.; Sharma, S.; et al. High Throughput Detection and Genetic Epidemiology of SARS-CoV-2 Using COVIDSeq Next-Generation Sequencing. PLoS ONE 2021, 16, e0247115. [Google Scholar] [CrossRef]
- Katoh, K.; Standley, D.M. MAFFT Multiple Sequence Alignment Software Version 7: Improvements in Performance and Usability. Mol. Biol. Evol. 2013, 30, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Batool, S.; Chokkakula, S.; Jeong, J.H.; Baek, Y.H.; Song, M.-S. SARS-CoV-2 Drug Resistance and Therapeutic Approaches. Heliyon 2025, 11, e41980. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Kusov, Y.; Hilgenfeld, R. Nsp3 of Coronaviruses: Structures and Functions of a Large Multi-Domain Protein. Antivir. Res. 2018, 149, 58–74. [Google Scholar] [CrossRef]
- Taha, T.Y.; Suryawanshi, R.K.; Chen, I.P.; Correy, G.J.; McCavitt-Malvido, M.; O’Leary, P.C.; Jogalekar, M.P.; Diolaiti, M.E.; Kimmerly, G.R.; Tsou, C.-L.; et al. A Single Inactivating Amino Acid Change in the SARS-CoV-2 NSP3 Mac1 Domain Attenuates Viral Replication in Vivo. PLoS Pathog. 2023, 19, e1011614. [Google Scholar] [CrossRef] [PubMed]
- Roe, M.K.; Junod, N.A.; Young, A.R.; Beachboard, D.C.; Stobart, C.C. Targeting Novel Structural and Functional Features of Coronavirus Protease Nsp5 (3CLpro, Mpro) in the Age of COVID-19. J. General. Virol. 2021, 102, 001558. [Google Scholar] [CrossRef]
- Iketani, S.; Mohri, H.; Culbertson, B.; Hong, S.J.; Duan, Y.; Luck, M.I.; Annavajhala, M.K.; Guo, Y.; Sheng, Z.; Uhlemann, A.-C.; et al. Multiple Pathways for SARS-CoV-2 Resistance to Nirmatrelvir. Nature 2023, 613, 558–564. [Google Scholar] [CrossRef] [PubMed]
- Jochmans, D.; Liu, C.; Donckers, K.; Stoycheva, A.; Boland, S.; Stevens, S.K.; De Vita, C.; Vanmechelen, B.; Maes, P.; Trüeb, B.; et al. The Substitutions L50F, E166A, and L167F in SARS-CoV-2 3CLpro Are Selected by a Protease Inhibitor In Vitro and Confer Resistance to Nirmatrelvir. mBio 2023, 14, e02815-22. [Google Scholar] [CrossRef]
- Zhou, Y.; Gammeltoft, K.A.; Ryberg, L.A.; Pham, L.V.; Tjørnelund, H.D.; Binderup, A.; Duarte Hernandez, C.R.; Fernandez-Antunez, C.; Offersgaard, A.; Fahnøe, U.; et al. Nirmatrelvir-Resistant SARS-CoV-2 Variants with High Fitness in an Infectious Cell Culture System. Sci. Adv. 2022, 8, eadd7197. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, E.M.; Zhang, X.; Tan, H.; Jaskolka-Brown, A.; Kohaal, N.; Frazier, A.; Madsen, J.J.; Jacobs, L.M.C.; Wang, J.; Chen, Y. Distal Protein-Protein Interactions Contribute to Nirmatrelvir Resistance. Nat. Commun. 2025, 16, 1266. [Google Scholar] [CrossRef]
- Tahir, M. Coronavirus Genomic nsp14-ExoN, Structure, Role, Mechanism, and Potential Application as a Drug Target. J. Med. Virol. 2021, 93, 4258–4264. [Google Scholar] [CrossRef] [PubMed]
- Hassan, S.S.; Bhattacharya, T.; Nawn, D.; Jha, I.; Basu, P.; Redwan, E.M.; Lundstrom, K.; Barh, D.; Andrade, B.S.; Tambuwala, M.M.; et al. SARS-CoV-2 NSP14 Governs Mutational Instability and Assists in Making New SARS-CoV-2 Variants. Comput. Biol. Med. 2024, 170, 107899. [Google Scholar] [CrossRef]
- Vu, M.N.; Lokugamage, K.G.; Plante, J.A.; Scharton, D.; Bailey, A.O.; Sotcheff, S.; Swetnam, D.M.; Johnson, B.A.; Schindewolf, C.; Alvarado, R.E.; et al. QTQTN Motif Upstream of the Furin-Cleavage Site Plays a Key Role in SARS-CoV-2 Infection and Pathogenesis. Proc. Natl. Acad. Sci. USA 2022, 119, e2205690119. [Google Scholar] [CrossRef]
- Santos-Mendoza, T. The Envelope (E) Protein of SARS-CoV-2 as a Pharmacological Target. Viruses 2023, 15, 1000. [Google Scholar] [CrossRef]
- Schoeman, D.; Fielding, B.C. Is There a Link Between the Pathogenic Human Coronavirus Envelope Protein and Immunopathology? A Review of the Literature. Front. Microbiol. 2020, 11, 2086. [Google Scholar] [CrossRef]
- Arduini, A.; Laprise, F.; Liang, C. SARS-CoV-2 ORF8: A Rapidly Evolving Immune and Viral Modulator in COVID-19. Viruses 2023, 15, 871. [Google Scholar] [CrossRef] [PubMed]
- Li, J.Y.; Liao, C.H.; Wang, Q.; Tan, Y.J.; Luo, R.; Qiu, Y.; Ge, X.Y. The ORF6, ORF8 and Nucleocapsid Proteins of SARS-CoV-2 Inhibit Type I Interferon Signaling Pathway. Virus Res. 2020, 286, 198074. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, K.; Huang, C.; Makino, S. SARS Coronavirus Accessory Proteins. Virus Res. 2008, 133, 113–121. [Google Scholar] [CrossRef]
- Gong, Y.-N.; Tsao, K.-C.; Hsiao, M.-J.; Huang, C.-G.; Huang, P.-W.P.-N.; Huang, P.-W.P.-N.; Lee, K.-M.; Liu, Y.-C.Y.-C.Y.-C.; Yang, S.-L.; Kuo, R.-L.; et al. SARS-CoV-2 Genomic Surveillance in Taiwan Revealed Novel ORF8-Deletion Mutant and Clade Possibly Associated with Infections in Middle East. Emerg. Microbes Infect. 2020, 9, 1457–1466. [Google Scholar] [CrossRef] [PubMed]
- Hassan, S.S.; Kodakandla, V.; Redwan, E.M.; Lundstrom, K.; Choudhury, P.P.; El-Aziz, T.M.A.; Takayama, K.; Kandimalla, R.; Lal, A.; Serrano-Aroca, Á.; et al. An Issue of Concern: Unique Truncated ORF8 Protein Variants of SARS-CoV-2. PeerJ 2022, 10, e13136. [Google Scholar] [CrossRef]
- Mazur-Panasiuk, N.; Rabalski, L.; Gromowski, T.; Nowicki, G.; Kowalski, M.; Wydmanski, W.; Szulc, P.; Kosinski, M.; Gackowska, K.; Drweska-Matelska, N.; et al. Expansion of a SARS-CoV-2 Delta Variant with an 872 Nt Deletion Encompassing ORF7a, ORF7b and ORF8, Poland, July to August 2021. Euro Surveill. Bull. Eur. Sur Les Mal. Transm. Eur. Commun. Dis. Bull. 2021, 26, 1–6. [Google Scholar] [CrossRef]
- Zinzula, L. Lost in Deletion: The Enigmatic ORF8 Protein of SARS-CoV-2. Biochem. Biophys. Res. Commun. 2020, 54, 251–255. [Google Scholar] [CrossRef]
- Wagner, C.; Kistler, K.E.; Perchetti, G.A.; Baker, N.; Frisbie, L.A.; Torres, L.M.; Aragona, F.; Yun, C.; Figgins, M.; Greninger, A.L.; et al. Positive Selection Underlies Repeated Knockout of ORF8 in SARS-CoV-2 Evolution. Nat. Commun. 2024, 15, 3207. [Google Scholar] [CrossRef]
- Sanderson, T.; Hisner, R.; Donovan-Banfield, I.; Hartman, H.; Løchen, A.; Peacock, T.P.; Ruis, C. A Molnupiravir-Associated Mutational Signature in Global SARS-CoV-2 Genomes. Nature 2023, 623, 594–600. [Google Scholar] [CrossRef]
- Strizki, J.; Murgolo, N.; Gaspar, J.; Howe, J.; Hutchins, B.; Mohri, H.; Ho, D.D.; Hazuda, D.; Grobler, J. 153. Molnupiravir Exhibits a High Barrier to the Development of SARS-CoV-2 Resistance in Vitro. Open Forum Infect. Dis. 2022, 9, ofac492.231. [Google Scholar] [CrossRef]
- Gratteri, C.; Ambrosio, F.A.; Lupia, A.; Moraca, F.; Catalanotti, B.; Costa, G.; Bellocchi, M.; Carioti, L.; Salpini, R.; Ceccherini-Silberstein, F.; et al. Molecular and Structural Aspects of Clinically Relevant Mutations of SARS-CoV-2 RNA-Dependent RNA Polymerase in Remdesivir-Treated Patients. Pharmaceuticals 2023, 16, 1143. [Google Scholar] [CrossRef]
- Stevens, L.J.; Pruijssers, A.J.; Lee, H.W.; Gordon, C.J.; Tchesnokov, E.P.; Gribble, J.; George, A.S.; Hughes, T.M.; Lu, X.; Li, J.; et al. Mutations in the SARS-CoV-2 RNA-Dependent RNA Polymerase Confer Resistance to Remdesivir by Distinct Mechanisms. Sci. Transl. Med. 2022, 14, eabo0718. [Google Scholar] [CrossRef]
- Khater, S.; Kumar, P.; Dasgupta, N.; Das, G.; Ray, S.; Prakash, A. Combining SARS-CoV-2 Proofreading Exonuclease and RNA-Dependent RNA Polymerase Inhibitors as a Strategy to Combat COVID-19: A High-Throughput in Silico Screening. Front. Microbiol. 2021, 12, 647693. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Sacramento, C.Q.; Jockusch, S.; Chaves, O.A.; Tao, C.; Fintelman-Rodrigues, N.; Chien, M.; Temerozo, J.R.; Li, X.; Kumar, S.; et al. Combination of Antiviral Drugs Inhibits SARS-CoV-2 Polymerase and Exonuclease and Demonstrates COVID-19 Therapeutic Potential in Viral Cell Culture. Commun. Biol. 2022, 5, 154. [Google Scholar] [CrossRef] [PubMed]
- Tamama, K. Potential Benefits of Dietary Seaweeds as Protection Against COVID-19. Nutr. Rev. 2021, 79, 814–823. [Google Scholar] [CrossRef]
- Emeny, J.M.; Morgan, M.J. Regulation of the Interferon System: Evidence That Vero Cells Have a Genetic Defect in Interferon Production. J. Gen. Virol. 1979, 43, 247–252. [Google Scholar] [CrossRef]
- Ogando, N.S.; Dalebout, T.J.; Zevenhoven-Dobbe, J.C.; Limpens, R.W.A.L.; Van Der Meer, Y.; Caly, L.; Druce, J.; De Vries, J.J.C.; Kikkert, M.; Bárcena, M.; et al. SARS-Coronavirus-2 Replication in Vero E6 Cells: Replication Kinetics, Rapid Adaptation and Cytopathology. J. Gen. Virol. 2020, 101, 925–940. [Google Scholar] [CrossRef] [PubMed]
- Jureka, A.S.; Basler, C.F. Propagation and Quantification of SARS-CoV-2. In SARS-CoV-2; Chu, J.J.H., Ahidjo, B.A., Mok, C.K., Eds.; Methods in Molecular Biology; Springer: New York, NY, USA, 2022; Volume 2452, pp. 111–129. ISBN 978-1-0716-2110-3. [Google Scholar]
- Matsuyama, T.; Kubli, S.P.; Yoshinaga, S.K.; Pfeffer, K.; Mak, T.W. An Aberrant STAT Pathway Is Central to COVID-19. Cell Death Differ. 2020, 27, 3209–3225. [Google Scholar] [CrossRef]

| Passage | 5 μg/mL | 2.5 μg/mL | Untreated |
|---|---|---|---|
| 1 | 102 | 103 | 106·5 |
| 2 | 0 | 102 | 103 |
| 3 | 0 | 105 | 105·5 |
| 4 | 0 | 102·5 | 103·7 |
| 5 | 0 | 105·5 | 105·25 |
| 6–11 | 0 | 104–106 | 105–107·25 |
| P | Nsp3 T1319A | Nsp3 F1375A | Nsp5 L50F | Nsp5 L67F | Nsp6 L158I | Nsp12 586 (syn) | Nsp14 G265D | Nsp14 H427Y | Nsp16 199 (syn) | Nsp16 273 (syn) | S T76S | S 15nt Del | S D1259H | E-S6L | ORF8 1-nt Del | N-G96N |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2-C | 13.1 | |||||||||||||||
| 3-C | 8.7 | 7.3 | 87.3 | |||||||||||||
| 4-C | 15.9 | 16.2 | 5.8 | 95.1 | ||||||||||||
| 5-C | 23.4 | 55.65 | 99.4 | |||||||||||||
| 8-C | 37.2 | 97.05 | 100 | 5.3 | ||||||||||||
| 9-C | 6.8 | 52.4 | 97.35 | 7.3 | 99.9 | |||||||||||
| 10-C | 18.9 | 18.7 | 66.2 | 95.4 | 7.9 | 99.9 | 9 | |||||||||
| 11-C | 16.4 | 10.2 | 78.5 | 96.7 | 6.3 | 99.7 | ||||||||||
| 1-AV | 8.4 | |||||||||||||||
| 2-AV | 9.55 | |||||||||||||||
| 3-AV | 13.1 | 5.5 | 33.2 | 6.9 | 29.1 | |||||||||||
| 4-AV | 18.9 | 12.8 | 5.8 | 36.05 | 5.4 | 39.3 | ||||||||||
| 5-AV | 26 | 17.9 | 42.9 | 16.1 | 17.3 | 67.9 | 6 | 20.8 | 15.1 | |||||||
| 6-AV | 35.3 | 25 | 44.9 | 25.9 | 33.3 | 63.15 | 6.3 | 22.3 | 25.4 | 5.9 | ||||||
| 7-AV | 87.2 | 89.5 | 12.3 | 7 | 87.1 | 93.3 | 7.95 | 9.7 | 88.2 | 90.9 | 5 | |||||
| 8-AV | 92.3 | 93.6 | 20 | 93.5 | 91 | 5.95 | 7.5 | 92.6 | 92.6 | |||||||
| 9-AV | 95.9 | 96.7 | 36.1 | 96.8 | 97.2 | 6.6 | 95.8 | 95.7 | 10.3 | |||||||
| 10-AV | 92.5 | 94.9 | 34.8 | 95 | 86.4 | 7.05 | 7.5 | 99.4 | 98.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maidana, S.S.; Romera, S.A.; Marandino, A.; Tau, R.L.; Shammas, J.M.; Panzera, Y.; Pérez, R. Characterization of the SARS-CoV-2 Mutation Pattern Generated In Vitro by the Antiviral Action of Lycorine. COVID 2025, 5, 181. https://doi.org/10.3390/covid5110181
Maidana SS, Romera SA, Marandino A, Tau RL, Shammas JM, Panzera Y, Pérez R. Characterization of the SARS-CoV-2 Mutation Pattern Generated In Vitro by the Antiviral Action of Lycorine. COVID. 2025; 5(11):181. https://doi.org/10.3390/covid5110181
Chicago/Turabian StyleMaidana, Silvina Soledad, Sonia Alejandra Romera, Ana Marandino, Rocío Lucia Tau, Juan Mauel Shammas, Yanina Panzera, and Ruben Pérez. 2025. "Characterization of the SARS-CoV-2 Mutation Pattern Generated In Vitro by the Antiviral Action of Lycorine" COVID 5, no. 11: 181. https://doi.org/10.3390/covid5110181
APA StyleMaidana, S. S., Romera, S. A., Marandino, A., Tau, R. L., Shammas, J. M., Panzera, Y., & Pérez, R. (2025). Characterization of the SARS-CoV-2 Mutation Pattern Generated In Vitro by the Antiviral Action of Lycorine. COVID, 5(11), 181. https://doi.org/10.3390/covid5110181






