Geographical Mapping of COVID-19 Testing Rates in St. Louis: Influence of the Socioeconomic Index and Race on Testing in the Early Phase and Peak of the COVID-19 Pandemic
Abstract
1. Introduction
Background
- How do race and socioeconomic status influence COVID-19 testing rates in St. Louis?
- Are there geographical clusters of low testing rates within specific zip codes?
- What are the implications of these findings for public health interventions?
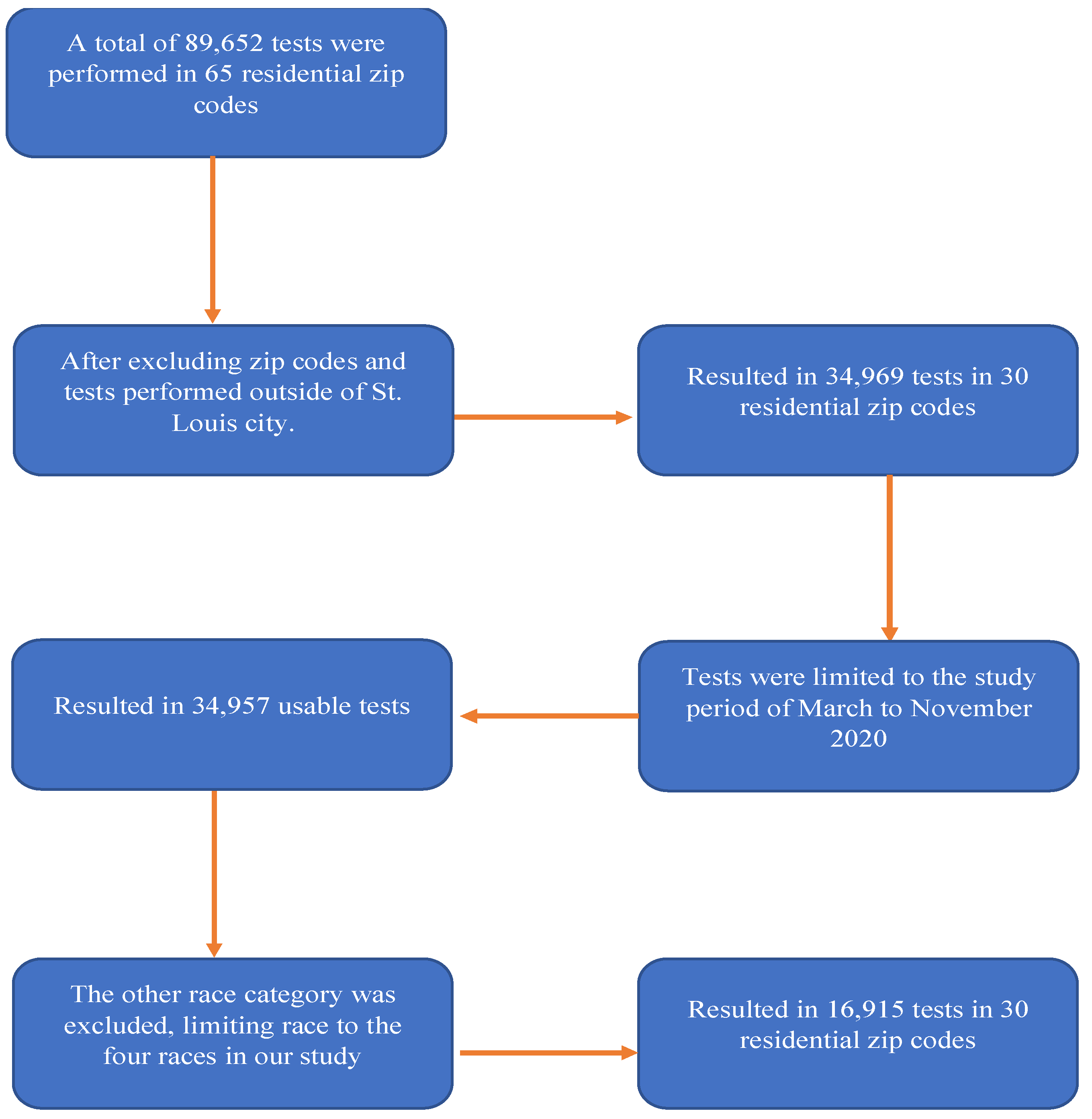
2. Materials and Methods
2.1. Data
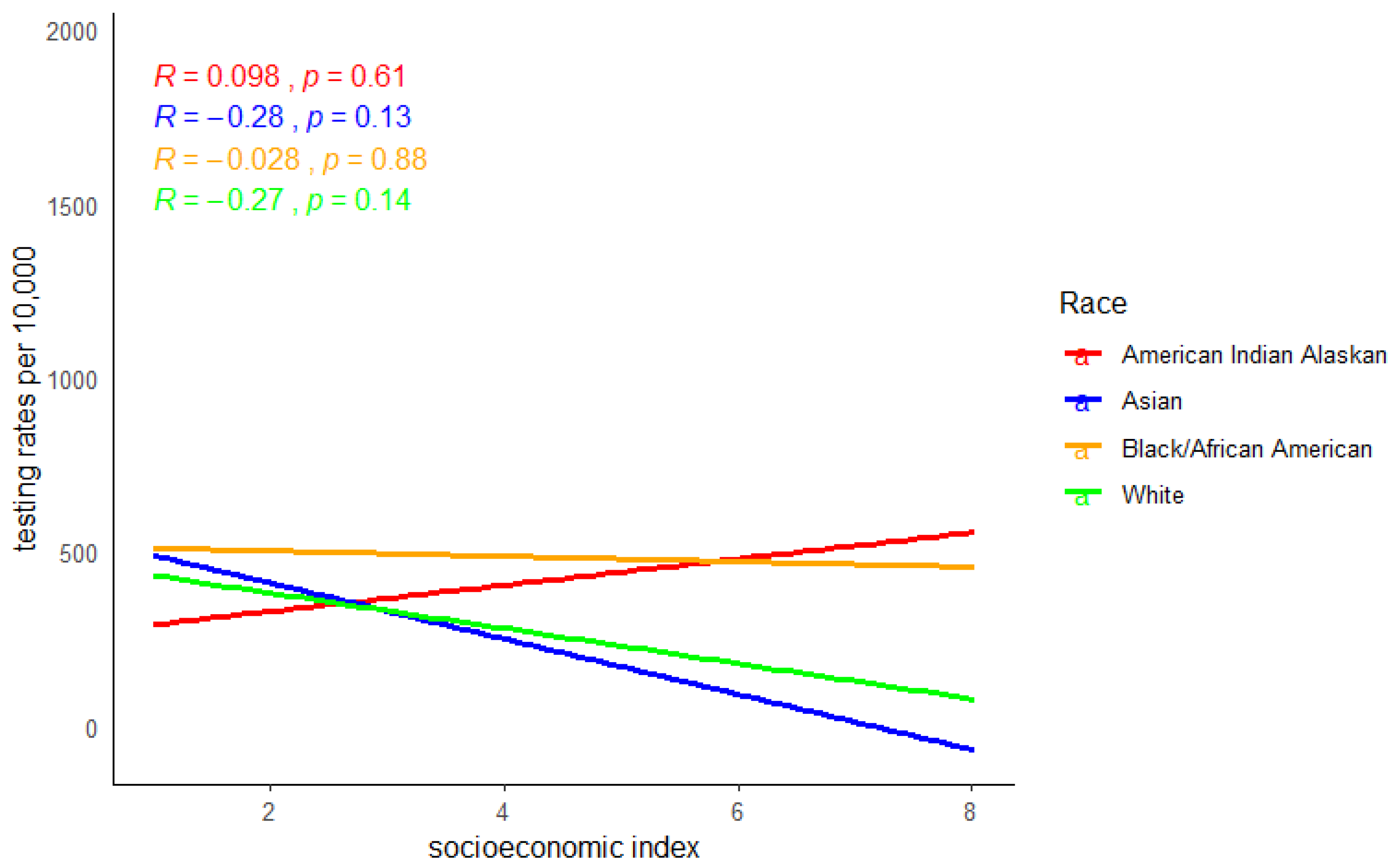
2.2. Statistical Analysis
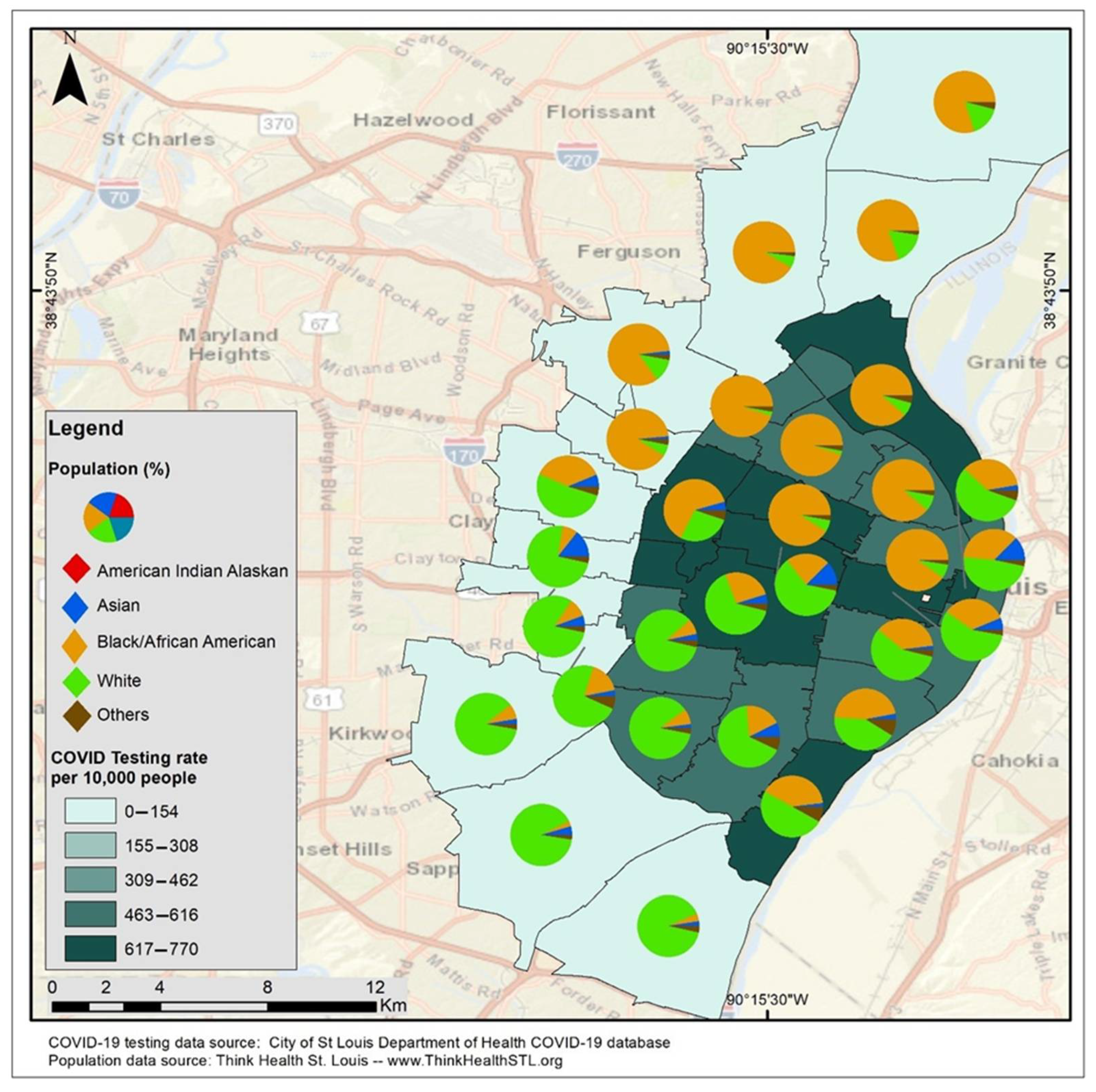
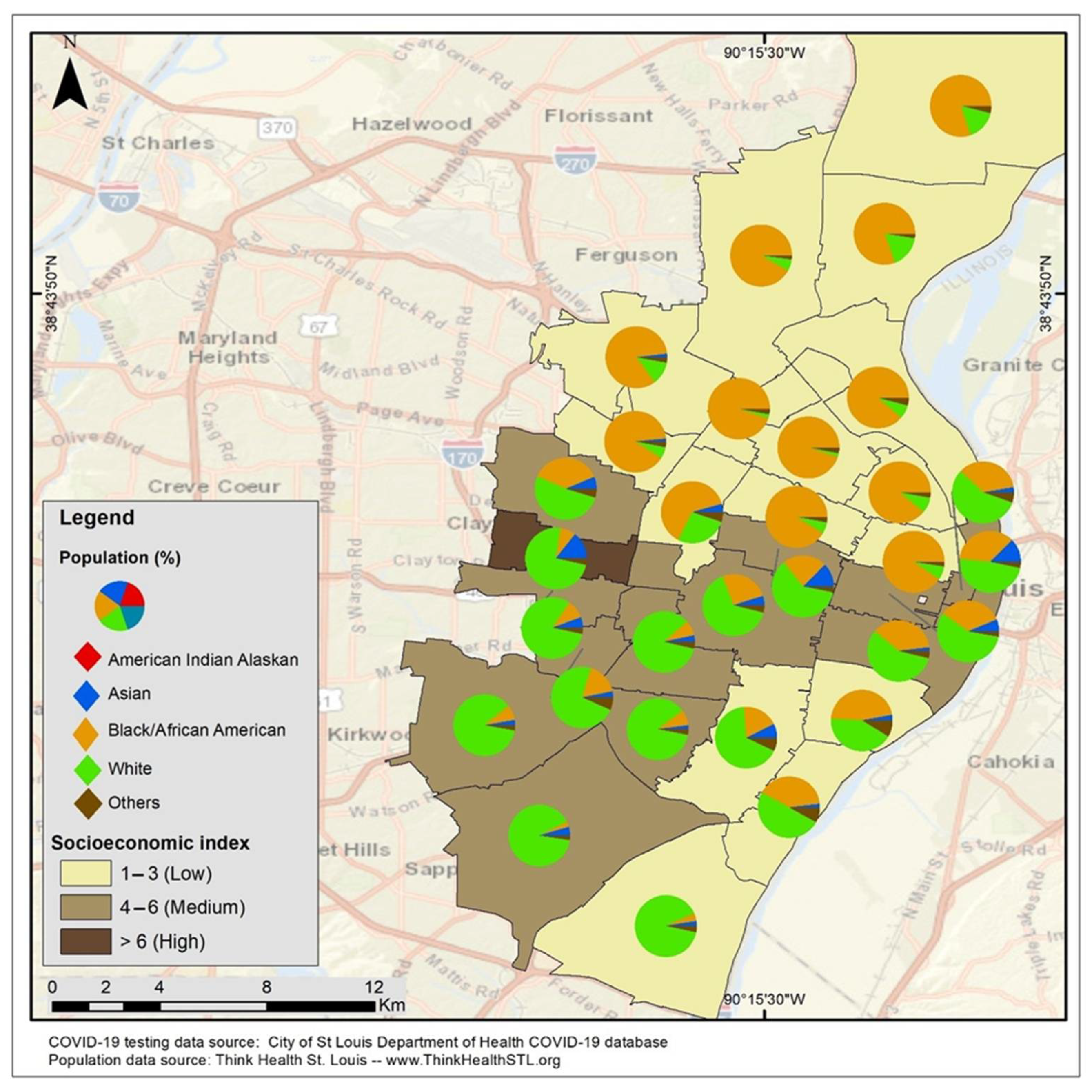
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 20 February 2022).
- COVID-19 Map. Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 29 October 2020).
- CDC. COVID Data Tracker. Centers for Disease Control and Prevention. Published 28 March 2020. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 6 March 2021).
- Tai, D.B.G.; Shah, A.; Doubeni, C.A.; Sia, I.G.; Wieland, M.L. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin. Infect. Dis. 2021, 72, 703–706. [Google Scholar] [CrossRef] [PubMed]
- Sze, S.; Pan, D.; Nevill, C.R.; Gray, L.J.; Martin, C.A.; Nazareth, J.; Minhas, J.S.; Divall, P.; Khunti, K.; Abrams, K.R.; et al. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2020, 29, 100630. [Google Scholar] [CrossRef] [PubMed]
- CDC. Cases, Data, and Surveillance. Centers for Disease Control and Prevention. Published 11 February 2020. Available online: https://archive.cdc.gov/#/details?url=https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed on 6 March 2021).
- Dalva-Baird, N.P.; Alobuia, W.M.; Bendavid, E.; Bhattacharya, J. Racial and Ethnic Inequities in the Early Distribution of U.S. COVID-19 Testing Sites and Mortality. Eur. J. Clin. Investig. 2021, 51, e13669. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.K.T.; Hwang, D.G. Differential Effects of Race/Ethnicity and Social Vulnerability on COVID-19 Positivity, Hospitalization, and Death in the San Francisco Bay Area. J. Racial Ethn. Health Disparities 2023, 10, 834–843. [Google Scholar] [CrossRef] [PubMed]
- Credit, K. Neighbourhood Inequity: Exploring the Factors Underlying Racial and Ethnic Disparities in COVID-19 Testing and Infection Rates Using ZIP Code Data in Chicago and New York. Reg. Sci. Policy Pract. 2020, 12, 1249–1272. [Google Scholar] [CrossRef]
- Capasso, A.; Kim, S.; Ali, S.H.; Jones, A.M.; DiClemente, R.J.; Tozan, Y. Socioeconomic Predictors of COVID-19-Related Health Disparities among United States Workers: A Structural Equation Modeling Study. PLoS Glob. Public Health 2022, 2, e0000117. [Google Scholar] [CrossRef]
- Hsiao, C.J.; Patel, A.G.M.; Fasanya, H.O.; Stoffel, M.R.; Beal, S.G.; Winston-McPherson, G.N.; Campbell, S.T.; Cotten, S.W.; Crews, B.O.; Kuan, K.; et al. The Lines That Held Us: Assessing Racial and Socioeconomic Disparities in SARS-CoV-2 Testing. J. Appl. Lab. Med. 2021, 6, 1143–1154. [Google Scholar] [CrossRef]
- Seto, E.; Min, E.; Ingram, C.; Cummings, B.; Farquhar, S.A. Community-Level Factors Associated with COVID-19 Cases and Testing Equity in King County, Washington. Int. J. Environ. Res. Public Health 2020, 17, 9516. [Google Scholar] [CrossRef]
- Lieberman-Cribbin, W.; Tuminello, S.; Flores, R.M.; Taioli, E. Disparities in COVID-19 Testing and Positivity in New York City. Am. J. Prev. Med. 2020, 59, 326–332. [Google Scholar] [CrossRef]
- National Public Radio (NPR). In Large Texas Cities, Access to Coronavirus Testing May Depend on Where You Live. Available online: https://www.npr.org/sections/health-shots/2020/05/27/862215848/across-texas-black-and-hispanic-neighborhoods-have-fewer-coronavirus-testing-sit (accessed on 3 September 2024).
- The Lost Month: How a Failure to Test Blinded the U.S. to COVID-19. Aggressive Screening Might Have Helped Contain the Coronavirus in the United States. But Technical Flaws, Regulatory Hurdles and Lapses in Leadership Let It Spread Undetected for Weeks. New York Times. Available online: https://www.nytimes.com/2020/03/28/us/testing-coronaviruspandemic.htmlextracted (accessed on 11 July 2022).
- Farley, J.E. Black-White Housing Segregation in the City of St. Louis: A 1988 Update. Urban Aff. Q. 1991, 26, 442–450. [Google Scholar] [CrossRef]
- The COVID Racial Data Tracker. The COVID Tracking Project. Available online: https://covidtracking.com/race (accessed on 28 October 2020).
- Available online: https://usafacts.org/data/topics/people-society/population-and-demographics/our-changing-population/state/missouri/county/st-louis-city?endDate=2021-01-01&startDate=2010-01-01 (accessed on 22 September 2022).
- Logan, J.R. The Persistence of Segregation in the 21st Century Metropolis. City Community 2013, 12, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.bbc.com/news/ay/magazine-17361995 (accessed on 22 September 2022).
- Divided Cities Lead to Differences in Health. Available online: https://forthesakeofall.files.wordpress.com/2013/11/policy-brief-4.pdf (accessed on 22 September 2022).
- Block, J.P.; Scribner, R.A.; DeSalvo, K.B. Fast food, race/ethnicity, and income: A geographic analysis. Am. J. Prev. Med. 2004, 27, 211–217. [Google Scholar]
- Acevedo-Garcia, D.; Lochner, K.A.; Osypuk, T.L.; Subramanian, S.V. Future directions in residential segregation and health research: A multilevel approach. Am. J. Public Health 2003, 93, 215. [Google Scholar] [CrossRef] [PubMed]
- Goodman, M.S.; Gaskin, D.J.; Si, X.; Stafford, J.D.; Lachance, C.; Kaphingst, K.A. Self-reported segregation experience throughout the life course and its association with adequate health literacy. Health Place 2012, 18, 1115–1121. [Google Scholar] [CrossRef]
- Kaphingst, K.A.; Goodman, M.; Pyke, O.; Stafford, J.; Lachance, C. Relationship between self-reported racial composition of high school and health literacy among community health center patients. Health Educ. Behav. 2012, 39, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://medicine.wustl.edu/news/early-covid-19-shutdowns-helped-st-louis-area-avoid-thousands-of-deaths/ (accessed on 23 September 2022).
- Available online: https://www.ksdk.com/article/news/health/coronavirus/st-louis-county-coronavirus-timeline-travel-quarantine/63-f81d92d8-dd20-4557-a487-101ce826418f (accessed on 23 September 2022).
- Available online: https://www.stlouis-mo.gov/government/departments/health/news/first-death-related-covid-19-city-of-st-louis.cfm (accessed on 27 September 2022).
- Available online: https://www.stlouis-mo.gov/covid-19/data/ (accessed on 27 September 2022).
- Available online: https://exploremohealth.org/reports/zip-health-report/ (accessed on 26 September 2022).
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S, 4th ed.; Springer: New York, NY, USA, 2002; ISBN 0-387-95457-0. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 2 January 2023).
- Palsky, G. Connections and exchanges in European thematic cartography. The case of 19th century choropleth maps. Rev. Belg. Géogr. 2008, 3–4, 413–426. [Google Scholar] [CrossRef]
- Al-Ghamdi, A.M. Optimising the Selection of a Number of Choropleth Map Classes. In Thematic Cartography for the Society; Bandrova, T., Konecny, M., Zlatanova, S., Eds.; Lecture Notes in Geoinformation and Cartography; Springer: Cham, Switzerland, 2014. [Google Scholar] [CrossRef]
- Martin, C.A.; Jenkins, D.R.; Minhas, J.S. Socio-demographic heterogeneity in the prevalence of COVID-19 during lockdown is associated with ethnicity and household size: Results from an observational cohort study. EClinicalMedicine 2020, 25, 100466. [Google Scholar] [CrossRef]
- Jing, Q.-L.; Liu, M.-J.; Zhang, Z.-B. Household secondary attack rate of COVID-19 and associated determinants in Guangzhou, China: A retrospective cohort study. Lancet Infect. Dis. 2020, 20, 1141–1150. [Google Scholar] [CrossRef]
- Hawkins, D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am. J. Ind. Med. 2020, 63, 817–820. [Google Scholar] [CrossRef]
- McClure, E.S.; Vasudevan, P.; Bailey, Z.; Patel, S.; Robinson, W.R. Racial Capitalism within Public Health—How Occupational Settings Drive COVID-19 Disparities. Am. J. Epidemiol. 2020, 189, 1244–1253. [Google Scholar] [CrossRef]
- Do, D.P.; Frank, R. Using Race- and Age-Specific COVID-19 Case Data to Investigate the Determinants of the Excess COVID-19 Mortality Burden among Hispanic Americans. Demogr. Res. 2021, 44, 699–718. [Google Scholar] [CrossRef]
- Gaitens, J.; Condon, M.; Fernandes, E.; McDiarmid, M. COVID-19 and Essential Workers: A Narrative Review of Health Outcomes and Moral Injury. Int. J. Environ. Res. Public Health 2021, 18, 1446. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.stlouis-mo.gov/government/departments/health/communicable-disease/COVID-19/documents/upload/COVID-19-One-Year-Report-City-of-St-Louis.pdf (accessed on 26 September 2022).
- Post-Dispatch Article. Available online: https://www.stltoday.com/lifestyles/health-med-fit/coronavirus/what-s-working-in-public-health-cdcdirector-finds-reason-for-hope-in-st-louis/article_9ae68eba-4fe8-55d6-be7a-1e7ee44f7bee.html (accessed on 23 October 2022).
- Brandt, K.; Goel, V.; Keeler, C.; Bell, G.J.; Aiello, A.E.; Corbie-Smith, G.; Wilson, E.; Fleischauer, A.; Emch, M.; Boyce, R.M. SARS-CoV-2 Testing in North Carolina: Racial, Ethnic, and Geographic Disparities. Health Place 2021, 69, 102576. [Google Scholar] [CrossRef] [PubMed]
- Rentsch, C.T.; Kidwai-Khan, F.; Tate, J.P.; Park, L.S.; King Jr, J.T.; Skanderson, M.; Justice, A.C. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLoS Med. 2020, 17, e1003379. [Google Scholar] [CrossRef] [PubMed]
- Baquero, B.; Gonzalez, C.; Ramirez, M.; Chavez Santos, E.; Ornelas, I.J. Understanding and Addressing Latinx COVID-19 Disparities in Washington State. Health Educ. Behav. 2020, 47, 845–849. [Google Scholar] [CrossRef]
- Gil, M.R.; Marcelin, J.R.; Zuniga-Blanco, B.; Marquez, C.; Mathew, T.; Piggott, D.A. COVID-19 Pandemic: Disparate Health Impact on the Hispanic/Latinx Population in the United States. J. Infect. Dis. 2020, 222, 1592–1595. [Google Scholar] [CrossRef]
- New York Fatalities COVID-19 by Race/Ethnicity. New York Department of Health. Published 2020. Available online: https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-race-ethnicity-05142020-1.pdf (accessed on 11 July 2022).


| Covariates | Average Testing Rates Per 10,000 (sd) |
|---|---|
| Overall Testing in St. Louis | 303.97 (57.28) |
| Race | |
| American Indian/Alaskan native | 360.63 (12.14) |
| Asian | 242.41 (3.52) |
| Blacks/African Americans | 374.26 (34.94) |
| White | 247.77 (4.14) |
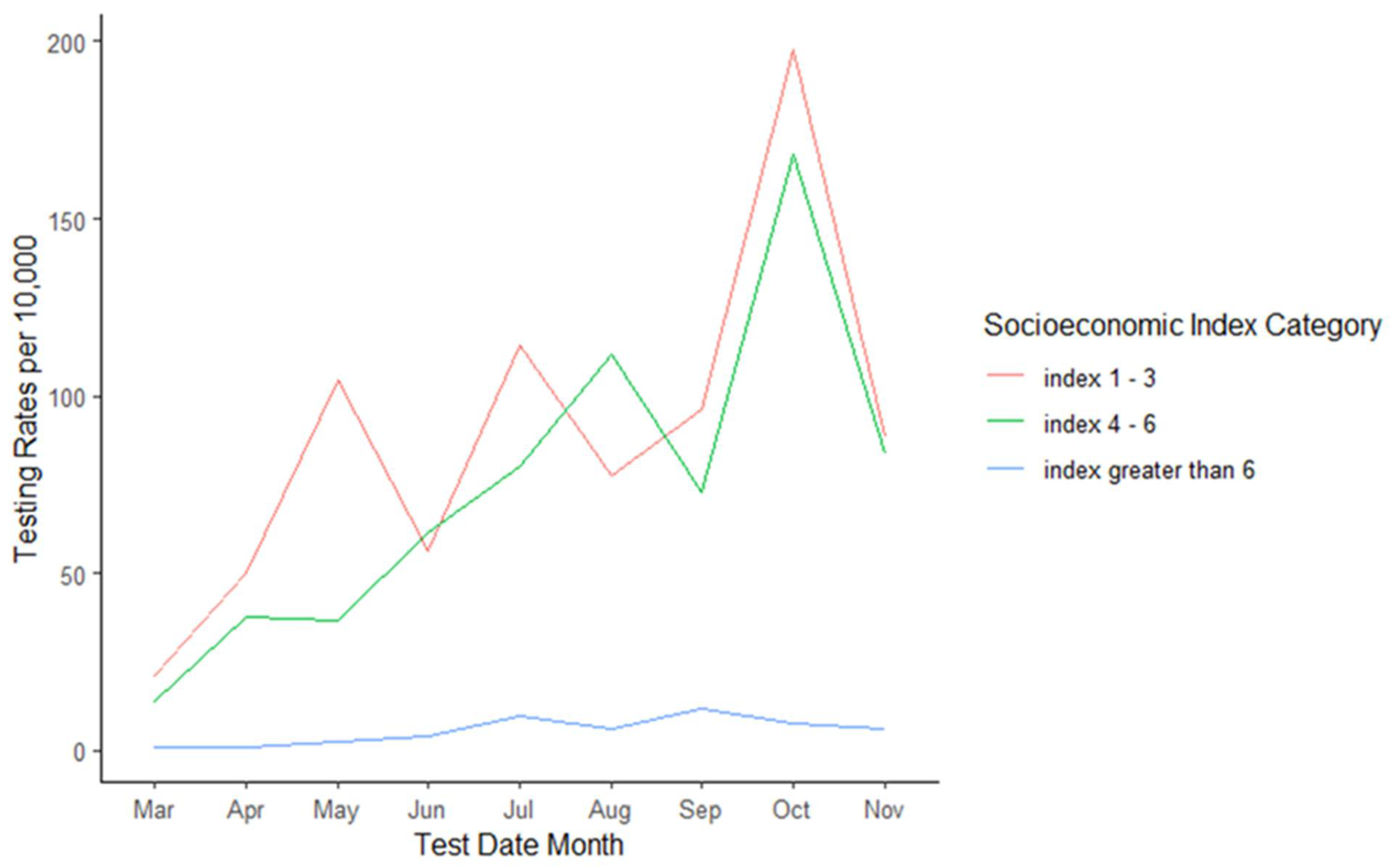
| Socioeconomic Index Category | |
| Index 1–3 (low SES) | 363.23 (17.20) |
| Index 4–6 (medium SES) | 259.53 (14.69) |
| Index > 6 (high SES) | 33.57 (51.56) |
| Characteristics | Beta | CI (95%) | p-Value |
|---|---|---|---|
| Intercept | 538 | 318, 759 | 0.000 |
| Race | |||
| White | ref | ref | ref |
| American Indian Alaskan | 448 | 188, 707 | 0.000 |
| Asian | 32 | −184, 247 | 0.773 |
| Black/African American | 125 | −75, 325 | 0.222 |
| Socioeconomic index | −56 | −110, −2.4 | 0.040 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Governor, S.B.; Effah, W.O.; Ntajal, J.; Nartey, C.N.O.; Voytovych, V.; Sam, H.; Ulanja, M.B.; Tutlam, N.T.; Otchere, P. Geographical Mapping of COVID-19 Testing Rates in St. Louis: Influence of the Socioeconomic Index and Race on Testing in the Early Phase and Peak of the COVID-19 Pandemic. COVID 2024, 4, 1463-1475. https://doi.org/10.3390/covid4090103
Governor SB, Effah WO, Ntajal J, Nartey CNO, Voytovych V, Sam H, Ulanja MB, Tutlam NT, Otchere P. Geographical Mapping of COVID-19 Testing Rates in St. Louis: Influence of the Socioeconomic Index and Race on Testing in the Early Phase and Peak of the COVID-19 Pandemic. COVID. 2024; 4(9):1463-1475. https://doi.org/10.3390/covid4090103
Chicago/Turabian StyleGovernor, Samuel B., William O. Effah, Joshua Ntajal, Cecilia Naa Ometse Nartey, Viktoriya Voytovych, Htu Sam, Mark B. Ulanja, Nhial T. Tutlam, and Prince Otchere. 2024. "Geographical Mapping of COVID-19 Testing Rates in St. Louis: Influence of the Socioeconomic Index and Race on Testing in the Early Phase and Peak of the COVID-19 Pandemic" COVID 4, no. 9: 1463-1475. https://doi.org/10.3390/covid4090103
APA StyleGovernor, S. B., Effah, W. O., Ntajal, J., Nartey, C. N. O., Voytovych, V., Sam, H., Ulanja, M. B., Tutlam, N. T., & Otchere, P. (2024). Geographical Mapping of COVID-19 Testing Rates in St. Louis: Influence of the Socioeconomic Index and Race on Testing in the Early Phase and Peak of the COVID-19 Pandemic. COVID, 4(9), 1463-1475. https://doi.org/10.3390/covid4090103







