Psychological Determinants of COVID-19 Vaccination Uptake among Pregnant Women in Kenya: A Comprehensive Model Integrating Health Belief Model Constructs, Anticipated Regret, and Trust in Health Authorities
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Sample
2.3. Measures
2.3.1. Dependent Variable
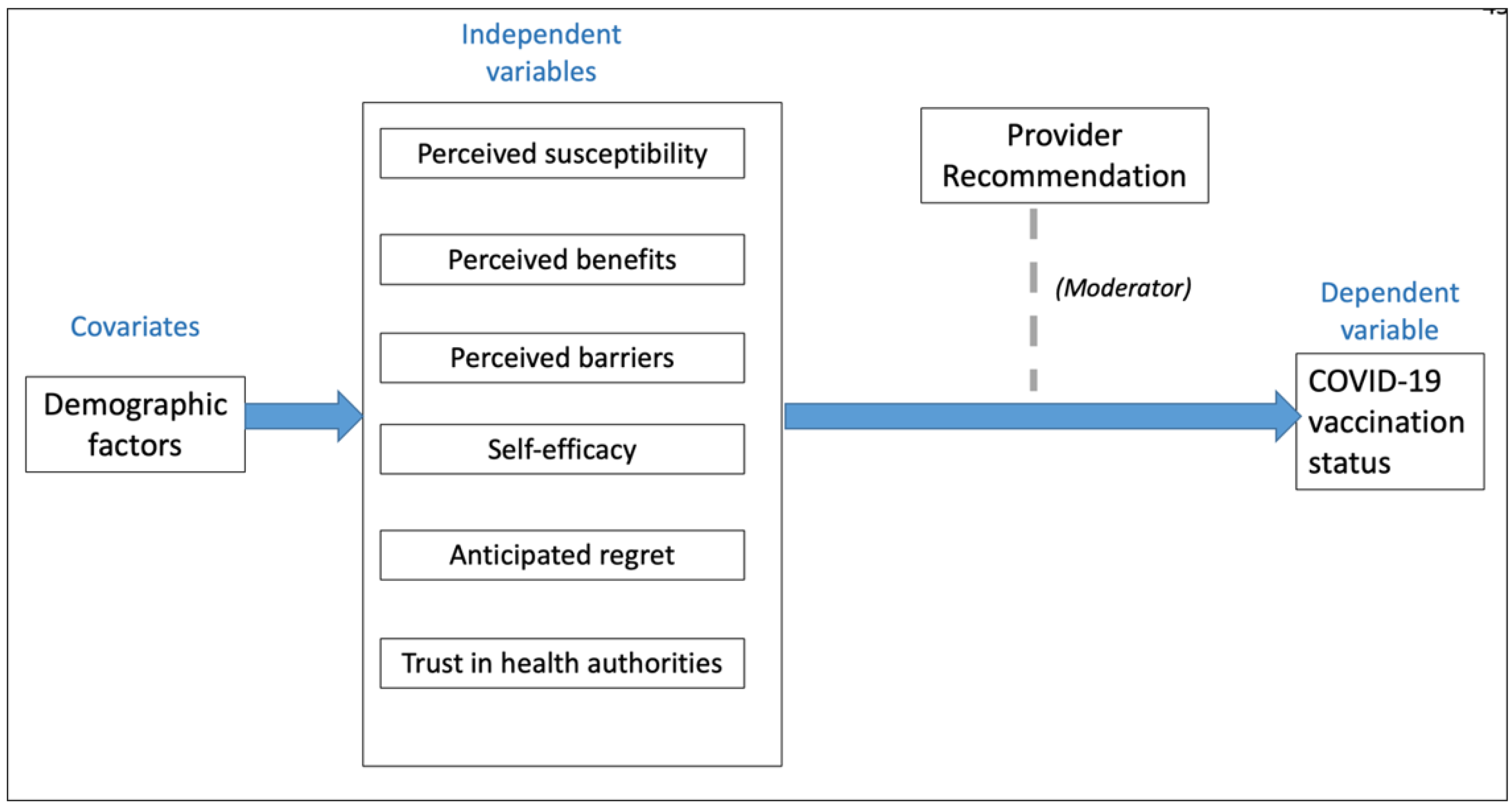
2.3.2. Independent Variables
2.3.3. Covariates
2.3.4. Effect Modification
2.4. Ethics
2.5. Statistical Analysis
3. Results
3.1. Descriptive Characteristics
3.2. Socio-Psychological Factors among Pregnant Women in Kenya
3.3. Correlation Analyses
3.4. Associations between Psychological Factors Associated with COVID-19 Vaccination and Vaccination Status among Pregnant Women in Kenya
3.5. Effect of Provider Recommendation on COVID-19 Vaccination by Psychological Factors
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 25 April 2024).
- US Food and Drug Administration. Coronavirus Disease 2019 (COVID-19) EUA Information. Available online: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization#covid19euas (accessed on 20 April 2024).
- European Medicines Agency. Comirnaty. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/comirnaty (accessed on 2 May 2023).
- World Health Organization (WHO). COVID-19 Advice for the Public: Getting Vaccinated. 2023. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice (accessed on 9 August 2023).
- Zheng, C.; Shao, W.; Chen, X.; Zhang, B.; Wang, G.; Zhang, W. Real-world effectiveness of COVID-19 vaccines: A literature review and meta-analysis. Int. J. Infect. Dis. 2022, 114, 252–260. [Google Scholar] [CrossRef]
- Sharif, N.; Alzahrani, K.J.; Ahmed, S.N.; Dey, S.K. Efficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. Front. Immunol. 2021, 12, 714170. [Google Scholar] [CrossRef]
- Mohammed, I.; Nauman, A.; Paul, P.; Ganesan, S.; Chen, K.H.; Jalil, S.M.S.; Jaouni, S.H.; Kawas, H.; Khan, W.A.; Vattoh, A.L.; et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: A systematic review. Hum. Vaccin. Immunother. 2022, 18, 2027160. [Google Scholar] [CrossRef]
- Allotey, J.; Stallings, E.; Bonet, M.; Stallings, E.; Yap, M.; Kew, T.; Zhou, D.; Coomar, D.; Sheikh, J.; Lawson, H.; et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020, 370, m3320. [Google Scholar] [CrossRef]
- Smith, D.D.; Pippen, J.L.; Adesomo, A.A.; Rood, K.M.; Landon, M.B.; Costantine, M.M. Exclusion of Pregnant Women from Clinical Trials during the Coronavirus Disease 2019 Pandemic: A Review of International Registries. Am. J. Perinatol. 2020, 37, 792–799. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Countering COVID-19 Misinformation in Africa. 2021. Available online: https://www.afro.who.int/news/countering-covid-19-misinformation-africa-continent-13-billion-people-who-and-partners-are (accessed on 25 April 2024).
- Van Spall, H.G.C. Exclusion of pregnant and lactating women from COVID-19 vaccine trials: A missed opportunity. Eur. Heart J. 2021, 42, 2724–2726. [Google Scholar] [CrossRef]
- Blakeway, H.; Prasad, S.; Kalafat, E.; Heath, P.T.; Ladhani, S.N.; Le Doare, K.; Magee, L.A.; O’Brien, P.; Rezvani, A.; van Dadalszen, P.; et al. COVID-19 vaccination during pregnancy: Coverage and safety. Am. J. Obstet. Gynecol. 2022, 226, 236. [Google Scholar] [CrossRef]
- Fell, D.B.; Dhinsa, T.; Alton, G.D.; Török, E.; Dimanlig-Cruz, S.; Regan, A.K.; Sprague, A.E.; Buchan, S.A.; Kwong, J.C.; Wilson, S.E.; et al. Association of COVID-19 Vaccination in Pregnancy with Adverse Peripartum Outcomes. JAMA 2022, 327, 1478–1487. [Google Scholar] [CrossRef]
- Ministry of Health-Kenya. Kenya COVID-19 Vaccination Program—Daily Situation Report. 2022. Available online: https://www.health.go.ke/covid-19 (accessed on 10 January 2024).
- Kyobutungi, C. The Ins and Outs of Kenya’s COVID-19 Vaccine Rollout Plan. The Conversation. 2021. Available online: https://theconversation.com/the-ins-and-outs-of-kenyas-covid-19-vaccine-rollout-plan-156310 (accessed on 15 March 2024).
- Kenya Obstetrical and Gynaecological Society, K. KOGS Statement on COVID-19 Vaccine among Pregnant & Breastfeeding Women. 2021. Available online: https://kogs.or.ke/2021/08/13/kogs-statement-covid19-vaccine-pregnant-breastfeeding-women/ (accessed on 15 March 2024).
- Cervi, L.; Calvo, S.T.; Robledo-Dioses, K. Digital communication and the city. Analysis of the websites of the most visited cities in the world in the COVID-19 era. Rev. Lat. Comun. Soc. 2023, 81, 81–107. [Google Scholar]
- Goncu Ayhan, S.; Oluklu, D.; Atalay, A.; Menekse Beser, D.; Tanacan, A.; Moraloglu Tekin, O.; Sahin, D. COVID-19 vaccine acceptance in pregnant women. Int. J. Gynaecol. Obstet. 2021, 154, 291–296. [Google Scholar] [CrossRef]
- Pairat, K.; Phaloprakarn, C. Acceptance of COVID-19 vaccination during pregnancy among Thai pregnant women and their spouses: A prospective survey. Reprod. Health 2022, 19, 74. [Google Scholar] [CrossRef]
- Gunawardhana, N.; Baecher, K.; Boutwell, A.; Pekwarake, S.; Kifem, M.; Ngong, M.G.; Fondzeyuf, A.; Halle-Ekane, G.; Mbah, R.; Tih, P.; et al. COVID-19 vaccine acceptance and perceived risk among pregnant and non-pregnant adults in Cameroon, Africa. PLoS ONE 2022, 17, e0274541. [Google Scholar] [CrossRef]
- Mohan, S.; Reagu, S.; Lindow, S.; Alabdulla, M. COVID-19 vaccine hesitancy in perinatal women: A cross-sectional survey. J. Perinat. Med. 2021, 49, 678–685. [Google Scholar] [CrossRef]
- Skirrow, H.; Barnett, S.; Bell, S.; Riaposova, L.; Mounier-Jack, S.; Kampmann, B.; Holder, B. Women’s views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: A multi-methods study in the UK. BMC Pregnancy Childbirth 2022, 22, 33. [Google Scholar] [CrossRef]
- Naqvi, S.; Saleem, S.; Naqvi, F.; Billah, S.M.; Nielsen, E.; Fogleman, E.; Peres-da-Silva, N.; Figueroa, L.; Mazariegos, M.; Garces, A.L.; et al. Knowledge, attitudes, and practices of pregnant women regarding COVID-19 vaccination in pregnancy in 7 low- and middle-income countries: An observational trial from the Global Network for Women and Children’s Health Research. BJOG 2022, 129, 2002–2009. [Google Scholar] [CrossRef]
- Tao, L.; Wang, R.; Han, N.; Liu, J.; Yuan, C.; Deng, L.; Sun, F.; Liu, M.; Liu, J. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: A multi-center cross-sectional study based on health belief model. Hum. Vaccin. Immunother. 2021, 17, 2378–2388. [Google Scholar] [CrossRef]
- Limbu, Y.B.; Gautam, R.K.; Pham, L. The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 973. [Google Scholar] [CrossRef]
- Glanz, K.E.; Rimer, B.K.; Viswanath, K. Health Behavior: Theory, Research, and Practice, 5th ed.; Jossey-Bass: San Francisco, CA, USA, 2015. [Google Scholar]
- Karimy, M.; Bastami, F.; Sharifat, R.; Heydarabadi, A.B.; Hatamzadeh, N.; Pakpour, A.H.; Cheraghian, B.; Zaman-Alavijeh, F.; Jasemzadeh, M.; Araban, M. Factors related to preventive COVID-19 behaviors using health belief model among general population: A cross-sectional study in Iran. BMC Public Health 2021, 21, 1934. [Google Scholar] [CrossRef]
- Carico, R.R.; Sheppard, J.; Thomas, C.B. Community pharmacists and communication in the time of COVID-19: Applying the health belief model. Res. Social. Adm. Pharm. 2021, 17, 1984–1987. [Google Scholar] [CrossRef]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccin. Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef]
- Limaye, R.J.; Paul, A.; Gur-Arie, R.; Zavala, E.; Lee, C.; Fesshaye, B.; Singh, P.; Njagi, W.; Odila, P.; Munyao, P.; et al. A socio-ecological exploration to identify factors influencing the COVID-19 vaccine decision-making process among pregnant and lactating women: Findings from Kenya. Vaccine 2022, 40, 7305–7311. [Google Scholar] [CrossRef]
- Ayieko, S.; Jaoko, W.; Opiyo, R.O.; Orang’o, E.O.; Messiah, S.E.; Baker, K.; Markham, C. Knowledge, Attitudes, and Subjective Norms Associated with COVID-19 Vaccination among Pregnant Women in Kenya: An Online Cross-Sectional Pilot Study Using WhatsApp. Int. J. Environ. Res. Public Health 2024, 21, 98. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Ghamri, R.A.; Othman, S.S.; Alhiniah, M.H.; Alelyani, R.H.; Badawi, A.M.; Alshahrani, A.A. Acceptance of COVID-19 Vaccine and Associated Factors Among Pregnant Women in Saudi Arabia. Patient Prefer. Adherence 2022, 16, 861–873. [Google Scholar] [CrossRef]
- Statista. Number of Internet Users in Selected Countries in Africa as of December 2020, by Country. Available online: https://www.statista.com/statistics/505883/number-of-internet-users-in-african-countries/ (accessed on 23 July 2023).
- Alkandari, D.; Herbert, J.A.; Alkhalaf, M.A.; Yates, C.; Panagiotou, S. SARS-CoV-2 vaccines: Fast track versus efficacy. Lancet Microbe. 2021, 2, 89–90. [Google Scholar] [CrossRef]
- Nasimiyu, C.; Audi, A.; Oduor, C.; Ombok, C.; Oketch, D.; Aol, G.; Ouma, A.; Osoro, E.; Ngere, I.; Njoroge, R.; et al. COVID-19 Knowledge, Attitudes and Practices and Vaccine Acceptability in Rural Western Kenya and an Urban Informal Settlement in Nairobi, Kenya: A Cross-Sectional Survey. COVID 2022, 2, 1491–1508. [Google Scholar] [CrossRef]
- Anino, C.O.; Wandera, I.; Masimba, Z.O.; Kirui, C.K.; Makero, C.S.; Omari, P.K.; Sanga, P. Determinants of COVID-19 vaccine uptake among the elderly aged 58 years and above in Kericho County, Kenya: Institution based cross-sectional survey. PLOS Glob. Public Health 2023, 3, e0001562. [Google Scholar] [CrossRef]
- Becker, M. The health belief model and sick role behavior. Health Educ. Monogr. 1974, 2, 409–419. [Google Scholar] [CrossRef]
- Skinner, C.; Tiro, J.; Champion, V. The health belief model. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K.R.B., Viswanath, K.V., Eds.; Jossey-Bass: San Francisco, CA, USA, 2015; pp. 75–94. [Google Scholar]
- Nazzal, Z.; Mohammad, A.; Qub, L.; Masri, H.; Abdullah, I.; Qasrawi, H.; Maraqa, B. Coverage and Determinants of COVID-19 Vaccination Among Pregnant Women: An Experience from a Low-Income Country. Am. J. Health Promot. 2023, 37, 222–227. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ten Threats to Global Health in 2019. 2021. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 April 2024).
- Best, A.L.; Fletcher, F.E.; Kadono, M.; Warren, R.C. Institutional Distrust among African Americans and Building Trustworthiness in the COVID-19 Response: Implications for Ethical Public Health Practice. J. Health Care Poor Underserved 2021, 32, 90–98. [Google Scholar] [CrossRef]
- Anraad, C.; Lehmann, B.A.; Visser, O.; van Empelen, P.; Paulussen, T.G.; Ruiter, R.A.; Kamp, L.; van der Maas, N.A.T.; Barug, D.; Rujis, W.L.M.; et al. Social-psychological determinants of maternal pertussis vaccination acceptance during pregnancy among women in the Netherlands. Vaccine 2020, 38, 6254–6266. [Google Scholar] [CrossRef]
- Liu, P.L.; Ao, S.H.; Zhao, X.; Zhang, L. Associations Between COVID-19 Information Acquisition and Vaccination Intention: The Roles of Anticipated Regret and Collective Responsibility. Health Commun. 2023, 38, 2198–2209. [Google Scholar] [CrossRef]
- Okuhara, T.; Shirabe, R.; Kagawa, Y.; Okada, H.; Kiuchi, T. Encouraging COVID-19 vaccination by focusing on anticipated affect: A scoping review. Heliyon 2023, 9, 22655. [Google Scholar] [CrossRef]
- Nan, X.; Zhao, X.; Briones, R. Parental cancer beliefs and trust in health information from medical authorities as predictors of HPV vaccine acceptability. J. Health Commun. 2014, 19, 100–114. [Google Scholar] [CrossRef]
- Ebrahimi, O.V.; Johnson, M.S.; Ebling, S.; Amundsen, O.M.; Halsøy, Ø.; Hoffart, A.; Skjerdingstad, N.; Johnson, S.U. Risk, Trust, and Flawed Assumptions: Vaccine Hesitancy During the COVID-19 Pandemic. Front. Public Health 2021, 9, 700213. [Google Scholar] [CrossRef]
- Wang, P.H.; Lee, W.L.; Yang, S.T.; Tsui, K.H.; Chang, C.C.; Lee, F.K. The impact of COVID-19 in pregnancy: Part II. Vaccination to pregnant women. J Chin. Med. Assoc. 2021, 84, 903–910. [Google Scholar] [CrossRef]
- Kilich, E.; Dada, S.; Francis, M.R.; Tazare, J.; Chico, R.M.; Paterson, P.; Larson, H.J. Factors that influence vaccination decision-making among pregnant women: A systematic review and meta-analysis. PLoS ONE 2020, 15, 0234827. [Google Scholar] [CrossRef]
- Kola-Palmer, S.; Keely, A.; Walsh, J. ‘It has been the hardest decision of my life’: A mixed-methods study of pregnant women’s COVID-19 vaccination hesitancy. Psychol. Health 2023, 1–21. [Google Scholar] [CrossRef]
| Variable | N (%) |
|---|---|
| Vaccination Status | |
| Vaccinated | 31 (27) |
| Unvaccinated | 84 (73) |
| Age | |
| 18–24 years | 19 (17) |
| 25–29 years | 45 (39) |
| 30–39 years | 45 (39) |
| 40–49 years | 6 (5) |
| Education level | |
| Primary school | 3 (3) |
| Secondary School | 34 (29) |
| College/University | 78 (68) |
| Region | |
| Nairobi | 59 (51) |
| Uasin Gishu | 56 (49) |
| Insurance Status | |
| Insured | 85 (74) |
| Uninsured | 30 (26) |
| Health Provider Recommendation | |
| Yes | 72 (64) |
| No | 40 (36) |
| Variable | Mean (SD) | ||||
|---|---|---|---|---|---|
| Vaccinated | Unvaccinated | t | Mean Difference | p-Value | |
| Perceived susceptibility | 3.64 ± 0.72 | 3.52 ± 0.93 | −0.77 | −0.13 | 0.44 |
| Perceived barriers | 5.19 ± 2.50 | 5.03 ± 3.36 | −0.27 | −0.16 | 0.78 |
| Perceived benefits | 2.67 ± 0.55 | 2.45 ± 0.81 | −1.63 | −0.22 | 0.11 |
| Self-efficacy | 3.02 ± 0.80 | 2.86 ± 0.83 | −0.93 | −0.16 | 0.35 |
| Anticipated regret | 2.65 ± 1.01 | 1.76 ± 0.91 | −4.21 | −0.89 | 0.01 * |
| Trust | 6.61 ± 1.60 | 5.13 ± 2.40 | −3.81 | −1.48 | 0.01 * |
| Perceived Susceptibility | Perceived Barriers | Perceived Benefits | Self-Efficacy | Anticipated Regret | Trust | |
|---|---|---|---|---|---|---|
| Perceived Susceptibility | 1 | |||||
| Perceived barriers | 0.01 | 1 | ||||
| Perceived benefits | 0.13 | 0.10 | 1 | |||
| Self-efficacy | −0.11 | −0.15 | −0.01 | 1 | ||
| Anticipated regret | 0.05 | 0.17 | 0.17 | 0.24 | 1 | |
| Trust | 0.06 | 0.13 | 0.01 | 0.36 * | 0.34 * | 1 |
| Variable | OR (95% CI) | aOR (95% CI) |
|---|---|---|
| Perceived susceptibility | 1.42 (0.44–4.55) | 1.54 (0.38–6.30) |
| Perceived barriers | 2.12 (0.88–5.09) | 1.58 (0.53–4.75) |
| Perceived benefits | 1.30 (0.54–3.10) | 1.14 (0.40–3.23) |
| Self-efficacy | 1.77 (0.71–4.45) | 0.96 (0.28–3.29) |
| Anticipated regret | 4.46 (1.55–12.83) * | 4.27 (1.23–14.85) * |
| Trust | 4.19 (1.60–10.96) * | 2.27 (0.61–8.41) |
| Age | ||
| 18–24 years | 2.5 (0.71–8.75) | 4.87 (0.99–23.86) |
| 25–29 years | Ref | Ref |
| 30–39 years | 3.08 (1.17–8.13) * | 2.84 (0.96–8.42) |
| 40–49 years | 3.33 (0.36–30.95) | ** |
| Education level | ||
| Primary school | 0.17 (0.01–2.01) | 0.68 (0.22–2.13) |
| Secondary School | 0.96 (0.38–2.39) | 1.02 (0.02–66.83) |
| College/University | Ref | Ref |
| Region | ||
| Nairobi | Ref | Ref |
| Uasin Gishu | 1.17 (0.51–2.68) | 1.06 (0.38–2.94) |
| Insurance Status | ||
| Insured | 1.22 (0.49–3.08) | 1.89 (0.54–6.62) |
| Uninsured | Ref | Ref |
| Health Provider Recommendation | ||
| Yes | 3.70 (1.53–8.92) * | 3.22 (1.27–8.16) a |
| No | Ref | Ref |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayieko, S.; Markham, C.; Baker, K.; Messiah, S.E. Psychological Determinants of COVID-19 Vaccination Uptake among Pregnant Women in Kenya: A Comprehensive Model Integrating Health Belief Model Constructs, Anticipated Regret, and Trust in Health Authorities. COVID 2024, 4, 749-760. https://doi.org/10.3390/covid4060050
Ayieko S, Markham C, Baker K, Messiah SE. Psychological Determinants of COVID-19 Vaccination Uptake among Pregnant Women in Kenya: A Comprehensive Model Integrating Health Belief Model Constructs, Anticipated Regret, and Trust in Health Authorities. COVID. 2024; 4(6):749-760. https://doi.org/10.3390/covid4060050
Chicago/Turabian StyleAyieko, Sylvia, Christine Markham, Kimberly Baker, and Sarah E. Messiah. 2024. "Psychological Determinants of COVID-19 Vaccination Uptake among Pregnant Women in Kenya: A Comprehensive Model Integrating Health Belief Model Constructs, Anticipated Regret, and Trust in Health Authorities" COVID 4, no. 6: 749-760. https://doi.org/10.3390/covid4060050
APA StyleAyieko, S., Markham, C., Baker, K., & Messiah, S. E. (2024). Psychological Determinants of COVID-19 Vaccination Uptake among Pregnant Women in Kenya: A Comprehensive Model Integrating Health Belief Model Constructs, Anticipated Regret, and Trust in Health Authorities. COVID, 4(6), 749-760. https://doi.org/10.3390/covid4060050









