Abstract
Purpose: The post-pandemic management of COVID-19 infections and any emergent outbreaks is because this endemic disease remains a public health concern. Vaccine hesitancy may continue to hamper efforts to respond to any new disease outbreaks and future epidemics. This qualitative study aimed to explore the factors influencing COVID-19 vaccine acceptance and hesitancy in Kenya to gain deeper insights into this issue. Methods: This study was implemented in western Kenya using key informant interviews. Fourteen (14) key informants were purposively selected for this study. All interviews were transcribed and analyzed using thematic analysis. The interpretation of findings was conducted within the framework of the Health Belief Model. Key findings: Knowledge was a critical factor in combatting misinformation and fostering vaccine acceptance among participants in this study. Misinformation included rumors that the vaccine lowers immunity and was intended for population control. Cues to action included influence from political and opinion leaders and observing the loss of life among unvaccinated individuals. Perceived barriers to vaccine uptake included fear of vaccine safety, side effects, long waiting times at the time of our study, fear of contracting COVID-19 at vaccination sites, family/spousal influence on vaccine uptake and fear of the unknown with the vaccine. Conclusions: The findings from this study provide insight into areas for targeted strategies for managing COVID-19 vaccinations and future pandemics. Within the framework of the Health Belief Model, this study identified salient barriers and facilitators of COVID-19 vaccine hesitancy that may be helpful to inform future pandemic responses.
1. Introduction
The post-pandemic management of COVID-19 infections, emergent outbreaks and surges as an endemic disease is of major public health concern [1]. While the World Health Organization (WHO) declared COVID-19 no longer a public health emergency (PHE) in May 2023, there are still daily infections and deaths caused by the disease in varying numbers around the world [1]. Experts predict that the disease will transition to an endemic phase because no vaccine has yet been developed that can provide lasting immunity or eliminate or eradicate the virus; hence, the virus continues to evolve into new strains [1,2]. Against this backdrop, addressing current and future potential COVID-19 vaccine hesitancy is critical in increasing vaccinations.
The endemic phase is characterized by continued infections by the virus but in lesser numbers, though it is not synonymous with COVID-19 infections becoming safe or the mortality and morbidity becoming less of a problem [3]. According to another study [4], the disease burden and prevalence in the endemic phase will be influenced by different factors beyond the endemicity itself. These include how quickly new variants emerge, the development of efficacious COVID-19 vaccines, uptake of vaccines, characteristics of people’s immunity at the individual level and herd immunity at the population level.
COVID-19 garnered unprecedented magnitudes of misinformation, disinformation and conspiracy theories in the history of recorded epidemics and pandemics that necessitated the World Health Organization to declare this a major public health problem, known as an infodemic [5]. This infodemic will continue to influence the current and future perceptions of vaccines and efforts of vaccination around the world, continually contributing to vaccine acceptance, hesitancy and refusal [6,7,8]. A myriad number of other factors significantly contributed to COVID-19 vaccine hesitancy globally and may still be difficult to deal with in the post-pandemic endemic phase [9,10]. While the world continues to learn more and apply lessons learned from the management of COVID-19 pandemic, countries must continually strive to maintain the significant gains that have been made during the past 4 years through active surveillance, reporting and data collection [1].
Vaccine hesitancy (VH), defined as the reluctance or refusal to get vaccinated despite the availability of vaccines, is among the ten main threats to global health [11]. In the early phase of a devastating global pandemic like COVID-19, vaccine hesitancy can greatly hamper efforts to respond effectively and control the outbreak, prolonging the battle with the disease. Earlier studies during the outbreak and spread of the pandemic demonstrated that COVID-19 vaccine hesitancy exists at varying levels across populations, from a low of 3% in Ecuador to as high as 72% in Kuwait [12]. Surprisingly, high levels of hesitancy are also reported even among health professionals with medical knowledge. According to recent studies [13,14], more than one-fifth of healthcare workers globally were hesitant about receiving a COVID-19 vaccine. The prevalence of vaccine hesitancy among healthcare workers worldwide ranged from about 4% to 72%, with an average of 22% [13]. Factors, such as vaccine safety, efficacy, potential side effects, fear of vaccine driven by conspiracy theories, the novelty of the COVID-19 vaccines and the urgency with which they were developed, have been identified as the top reasons for vaccine hesitancy among healthcare workers and members of the general population [14,15]. Health professionals, among others, have a crucial role in disseminating information, providing health education and attempting to convince people to follow vaccination schedules. Health professionals themselves may have doubts about the vaccines, resulting from many factors including mistrust of the healthcare system of their country, and this influences their own perceptions and decisions on vaccine acceptance as well as openly expressing their reservations, hence impacting the preventative behaviors and decisions of the general population.
As Orenstein and Ahmed [16] point out, it is often said that vaccines save lives, which is not strictly true; it is vaccination that saves lives because a vaccine that remains in a vial is 0% effective, even if it is the best in the world. Hence, it is imperative that there are concerted efforts to assure that high levels of vaccination coverage are attained among targeted populations for whom vaccines are recommended. The historical trajectory of VH traverses many vaccine-recommended diseases, and vaccine skeptics have been present since the smallpox vaccination exercise carried out in the 19th century [17,18,19,20,21]. However, the phenomenon of VH has been magnified in the technological advancement era of the internet and social media, with exponential communications and interaction strategies and platforms globally [17,20,22,23,24,25]. As studies consistently point out, VH and the under-utilization of accessible vaccination services contribute to the continued and/or increasing burden of diseases from vaccine-preventable diseases (VPDs) around the world, which stymies decades of public health efforts and desired progress [11,26,27,28,29,30].
For example, in the United States, Canada and Europe, the resurgence of measles due to vaccine reluctance resulted in increased vulnerability in unimmunized children in large urban centers [31]. Additionally, such occurrences in developed countries influence the decisions and actions of people in other parts of the world, including developing countries and the African continent [32]. This speaks to the urgency of addressing vaccine hesitancy as a top priority in public health towards effective vaccination programs [11].
VH is a complex phenomenon, context specific, varies between time periods and within a given period and ranges as a continuum, from overt acceptance to uncertainty, delay and outright refusal [33,34]. While VH is embedded in individual and collective behaviors and decisions influenced by a wide range of factors in different people or communities, the phenomenon should always be examined in broader lenses and multiple perspectives that incorporate historical, political, socio-cultural and global forces, as people live and concurrently interact at multiple levels in society [34]. Globally, the drivers of VH are as complex as the phenomenon itself, numerous, vary and evolve over time as well as within any given period [12,34,35]. According to the study findings in [36], some concerns are perennial, while others may be new as each vaccine is introduced in a different context, and some concerns may be unfounded, though others may be valid. The updated WHO model [37] provides the 5Cs as a framework by which to assess VH, which are as follows: confidence, complacency, constraints including structural and psychological barriers; calculation (decision making); and collective responsibility (communal orientation). In recent years [26], many VH models and frameworks have been developed [38,39,40], which reveal and further emphasize that VH is not captured in simple dichotomies of acceptance/refusal, pro-vaccine/anti-vaccine and confident or hesitant about vaccines.
Further, as reported by one study [41], addressing VH is not a singular focus on the provision of more information to fil gaps without consideration of how the information may be used or interpreted by recipients, among other issues. For example, an earlier study identified over 70 factors that drive or influence VH towards influenza vaccines globally [42]. Some of the challenges limiting the acceptance of COVID-19 vaccines [12] have been observed in other vaccines, such as flu vaccines [43], the HPV vaccine [44] and other vaccines [18]. The consensus, based on findings from decades of research and policy strategies, is that addressing VH should be multi-sectoral, multi-disciplinary and consistently entrenched in evidenced-based findings and ongoing research, with rigorous evaluation of their impact on desired outcomes in different contexts and groups.
The development and spread of anti-vaccination movements over the years demonstrate that public concerns are not merely a distrust of science but a mix of scientific, psychological, sociocultural and political factors [17,23]. As posited by [26,32,45], in addition to other structural and logistical considerations, feedback mechanisms for the acknowledgement of community efforts in previous health interventions should be improved upon to encourage the acceptance of the prospective COVID-19 vaccine. A systematic review [46] on vaccine hesitancy in Sub-Saharan Africa (SSA) in the context of a COVID-19 vaccination exercise reported that vaccine hesitancy occurs against a colonial backdrop of inequities in global health research, social–cultural complexities, poor community involvement and public distrust. There is a large body of anecdotal evidence from Africa regarding mistrust in medicine, which often leads to an underutilization of healthcare [19,47,48,49,50]. The legacy of colonial practices in medicine on the African continent remains a barrier to vaccinations, with embedded mistrust of the motives of Western developed countries [32]. Widespread and strongly entrenched perceptions and rumors exist that SSA is a testing ground for new vaccines and that Africans are used as guinea pigs for vaccine trials. In Kenya, studies [51,52] corroborate such findings. More recently two French doctors suggested testing C19 vaccines in Africa, which was not taken positively by the people on the African continent [53]. As noted by [54], there is no vaccine against resistance or refusals that are rooted in social, cultural, religious and political contexts; no supply chain can overcome some of the barriers. Medical approaches alone cannot address certain community concerns.
We adopted the Health Belief Model (HBM) as our conceptual framework to guide our study in the data we sought to collect. The HBM was developed in the early 1950s by social scientists in the US Public Health Service to understand people’s failure to adopt disease prevention strategies [55,56]. The six constructs of the HBM are perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action and self-efficacy. Over the years, as it evolved, this framework has been extensively applied in different ways in understanding behavioral health decisions and applied for different outcomes, with varied findings, some positive while others were inconclusive [56,57,58].
The HBM is an important tool for public health professionals and others involved in policy and decision making on the health and health outcomes of populations because it provides a framework for understanding how people perceive health risks and how these perceptions may contribute to how they respond to those risks [55,56,57,58,59]. The HBM framework suggests that people’s beliefs and self-efficacy explain engagement (or lack of engagement) in health-promoting behaviors. With an understanding of these perceptions, it is assumed that public health professionals can design interventions that are more effective in promoting healthy behaviors, influencing communication, campaigns and policy for motivating individuals towards effective behavior changes for desired better outcomes [59,60,61].
While much success is attributed to the use of the framework, it is important to note that, like all other theories and models/frameworks, the HBM has limitations. Notable among these are not accounting for habitual behaviors, where individuals are not rational but more impulsive in their decision making; not accounting for broader organizational, community, population or structural factors that are not necessarily health-related but affect people’s decisions; and assumes that cues to action are widely prevalent in encouraging people to act, and that “health” actions are the main goal in the decision-making process in everyday lives, or decisions made will be sustained [59,60,61,62]. However, despite the limitations, the HBM is still a widely applied framework for application in today’s public health work and studies and contributes to generating relevant information and knowledge.
The majority of studies on vaccine hesitancy are largely quantitative, with few qualitative available across the world and particularly in Kenya. Qualitative studies, especially for healthcare research, are useful in understanding health behaviors by eliciting rich narratives on a phenomenon and deeper understanding of the lived experiences of the target population [63]. Against this backdrop, this qualitative study aimed to explore the factors influencing COVID-19 vaccine acceptance and hesitancy in Kenya to capture the lived experiences and other attributes of VH that numbers alone may not highlight. At the time of this study, such data help gain a deeper understanding of the context-specific factors associated with vaccine uptake and hesitancy, which would contribute to efforts towards health promotion for vaccinations, policy implementation and ways to manage the COVID-19 pandemic and other future pandemics. Findings from this study may be helpful in designing effective intervention strategies as we deal with COVID-19 as an endemic disease.
2. Materials and Methods
2.1. Research Design
We utilized an exploratory qualitative cross-sectional research design by conducting key informant interviews (KII) on purposefully selected participants, mainly because of ease of access and the population segments they are part of in the community. This study was conducted in May–August 2021, at the peak of COVID-19 globally. Our primary aim for the qualitative strategy through open-ended structured interview questions was to understand the factors associated with vaccine hesitancy, acceptance, motivators and barriers to COVID-19 vaccine uptake among adults aged 18+ years. This study focused on eliciting information guided by the most salient elements of the model (perceived susceptibility, perceived severity, perceived benefits, perceived barriers to action, cues to action and self-efficacy) to identify factors influencing vaccine acceptance and hesitancy.
2.2. Study Setting
This study was carried out in Kakamega, Vihiga and Kisumu Counties in western Kenya.
Kakamega County is located in the former Western Province of Kenya and borders Vihiga County to the south, Siaya County to the west, Bungoma and Trans-Nzoia counties to the north and Nandi and Uasin Gishu counties to the east. Its capital, and largest town, is Kakamega, and it has a population of over 1.8 million people and an area of 3033.8 km2. The county has twelve sub-counties, eighty-three locations, two hundred and fifty sub-locations, one hundred and eighty-seven Village Units and four hundred Community Administrative Areas. There are 433,207 households, with an average size of 4.3 persons per household [64].
Vihiga County lies in the Lake Victoria Basin and covers an area of 531.0 km2, around 80 km northwest of Eldoret, around 60 km north of Kisumu and approximately 350 km west of Nairobi City, the capital city of Kenya. It is in the western region of Kenya and borders Nandi County to the east, Kisumu County to the south, Siaya County to the west and Kakamega County to the north. Its headquarters are in Mbale, and it is one of the four counties in the former Western Province. The county has a population of over 600,000 people, of which 51.9% are females, while males constitute 48.1%; 64.4% of the total population are under the age of 30 [64]. The county has five administrative sub-counties. The county is further subdivided into 38 locations and 131 sub-locations.
Located in the western part of Kenya, Kisumu County is one of the 47 counties in the country. It borders Lake Victoria to the east and is home to the third-largest city in Kenya, Kisumu City. The county has a population of over 1.1 million people and covers an area of 2085.9 km. The county is bordered to the north by Nandi County and to the north east by Kericho County. Women make up 50.1% of Kisumu’s population, and men represent 49.9%. Sixty-four percent of the total population are under the age of 25. Administratively, the county is divided into 7 sub-counties, and these are further divided into 35 wards [64].
2.3. Study Population and Participants
Our study targeted key informants who were all adults 18+ years residing in Kisumu, Vihiga and Kakamega counties in western Kenya. Key informants are individuals with unique expertise and understanding in each area. This was to collect information from a wide range of people who have firsthand knowledge about the community. There were 14 key informants, who included Assistant Chief, motorcycle rider, community health volunteer, medical officer, nurse, gospel minister, youth mentor, security officer, lawyer, Islamic religious leader, women’s group leader, community health promoter and Evangelist.
2.4. Sampling Procedure
Purposive sampling was used to select the three counties and study participants. Purposive sampling is a technique widely used in qualitative research for the identification and selection of information-rich cases for the most effective use of limited resources [65]. This involves identifying and selecting individuals or groups of individuals that are especially knowledgeable about or experienced with a phenomenon of interest. The fourteen (14) key informants were selected purposively from the three counties. Key informant interviews are qualitative in-depth interviews with people who know what is going on in the community or given region based on their experiences, interactions or the nature of their work/vocations and position in the community [66,67]. The purpose of using key informant interviews (KIIs) is to collect in-depth and/or expert information from a wide range of people, including community leaders, professionals, residents, stakeholder representatives, experts of various kinds including teachers, health professionals and community health workers, shopkeepers, market traders, transporters, drivers, faith leaders, farmers, community elders, and many more, who have firsthand knowledge about the community or prevailing issues from a broader perspective. These community experts, with their knowledge and understanding, can provide insight into the nature of problems and give recommendations for solutions. They often speak of their own opinions, though much of it is often influenced by broader sentiments in a subtle way [68,69]. The sample size for KIIs depends on various factors, such as the topic, aim/study focus, size of the community or region and existing community structures and study duration, among others. While most studies using KIIs use between 10 and 16 participants, there have been some below 10 and with as few as 4–6 participants, while some have been as large as over 40 and others with over 50 participants, especially in national- or global-level studies [66,67,70]. The authors of this study considered the selection of 14 participants a good representation across the 3 counties as well as many relevant sectors for broader views of the everyday lives, opinions of the public and insights of the prevailing attitudes and beliefs of the community on COVID-19 vaccines. This would be different for a quantitative study in the same area and on the same topic.
2.5. Data Collection Tools
A semi-structured interview guide was developed through discussion depending on the antecedent knowledge and previous studies [65]. A semi-structured interview guide was utilized so that flexibility during the interview would be ensured. The interview guide was anchored on the Health Belief Model, including the perceived severity, perceived susceptibility, perceived benefits and barriers such as misinformation. Open-ended questions and prompts guided the interview to form a colloquial manner to generate rich descriptions.
2.6. Data Collection Procedure
This was a qualitative study conducted in western Kenya using the key informant interview (KII) approach. Fourteen key informants were purposively selected to participate in this study. Data were recorded verbatim using an audio recording device and transcribed into Microsoft Word processor.
A semi-structured interview guide was used for data collection. The interview guide was piloted among four (4) participants to determine if it elicited the requisite and desired responses from the study participants. The four informants who participated in the pilot were excluded from the study. Each participant was interviewed alone after making appropriate appointments in their offices or in a secluded area, as appropriate. The interview guide was utilized throughout the interview to guarantee uniformity and standardization of the whole interview process, at the same time as permitting extensive probe of the phenomenon in question. The interviewer delved into emerging ideas depending on the participants’ responses. Each interview session took between 15 and 20 min and was recorded using a tape recorder with permission from the study participants. In each interview, field notes were also taken.
2.7. Data Analysis
Data from the key informant interviews (KII) were analyzed using the principles of thematic analysis process [71,72,73]. Data were categorized and frameworks identified based on the issues in the interview guide, and coding plan was developed to explore interactions. Each segment of the transcript (text file) was coded. The coded transcripts were then exported to QSR NVIVO 12.5 statistical software to analyze qualitative data; this software give the opportunity to organize, store, retrieve and process data, with 90% level of output accuracy (QSR NVIVO 12.5 full version). The analysis was then accomplished by familiarizing with data by reading verbatim and noting significant themes. Emerging themes were identified, and coding categories were developed according to the views of the respondent [74,75,76]. Each segment of the transcript (text file) was coded according to each category to describe the factors influencing COVID-19 vaccine acceptance and hesitancy based on the Health Belief Model’s salient concepts of relevance to this study. The interpretation was conducted within the framework of the Health Belief Model (HBM).
2.8. Ethical Approval
The research protocol was reviewed and approved by the institution ethics review committee of University of Eastern Africa Baraton (Approval Code: (UEAB/REC/50/03/2021)).
3. Results
3.1. Study Participants
A total of 14 respondents participated in this study, drawn from diverse occupations, as indicated in Table 1 below.

Table 1.
Occupation distribution of key informant study participants.
3.2. Factors Influencing the Uptake of COVID-19 Vaccine
3.2.1. Low Perceived Severity of COVID-19
Respondents indicated that observing the devastating effects of COVID-19 among those who were unvaccinated, particularly the loss of life, locally and internationally, influenced the uptake of the COVID-19 vaccine. As a participant mentioned, “I think the most relevant is the fear of death” (R13, Evangelist occupation). People were willing to get vaccinated so that they could avoid being infected by COVID-19. For example, a participant mentioned a reason why people get vaccinated: “people take the vaccine to be safe and due to fear for infection from others” (R8, Youth mentor occupation). More so, participants highlighted the role that international travelling played in inducing COVID-19 vaccine uptake, as noted by one of the participants:
“We are living in a society where people do with the international travelling, so this influences them to take the vaccine as you can see people are really losing their lives, yes as you can see even in our country here”(R1, Assistant chief).
It also emerged that another factor crucial in fostering COVID-19 vaccine uptake was the perceived severity of the disease, particularly the social consequences, such as isolation and stigmatization. One respondent mentioned the following:
“People fear being infected, because if you are positive of COVID-19 you will be isolated, so you will be away from your family members, also there is fear of stigmatization.”(R3, CHV).
3.2.2. Perceived Benefits
Respondents indicated that vaccine acceptance was fostered by the benefits that are perceived to accrue from getting vaccinated. These benefits included the belief that the vaccine prevented the disease and improved their immunity. One of the motorbike (Boda Boda) riders said the following:
“Me I think, people go to get the vaccine because they believe that the vaccine prevents COVID-19, so I think it is because they don’t want to get that virus also they’ll get immunity boost towards the virus”(R2, Boda Boda Rider).
A community health volunteer (CHV) said, “We normally say, prevention is better than cure, so people go for prevention… Another issue is that they see that if you get vaccinated early, the chance of getting the virus is low, and you can live longer as for example the measles vaccine.” (R3, CHV).
Further benefits were cited, including the fact that the vaccination is free of charge:
“One is to improve the immunity, also to be free from corona virus, and also to be healthy and… also to add the service is cost free.”(R5, security officer).
3.2.3. Low Perceived Susceptibility
One of the factors reported as influencing hesitancy was a low perception of susceptibility to COVID-19. This particularly affected uptake among the youth, who did not perceive themselves to be at risk of the disease. As one of the respondents stated:
“people say that vaccine is for the elderly not for the young or the youths… people say that the elderly are the once who are at risks, we as the energetics ones we are just ok”(R14, Women Group Leader).
This belief stems from the idea that younger people have a higher immunity compared to older populations. As identified by another of the study participants,
“there is misconception among the youth about the age, whereby they think that they have strong immunity, whereby they believe that the elderly are at risk than them”(R4, Lawyer).
In addition to the belief that younger populations are not as susceptible to COVID-19 compared to elderly ones, there was also the belief that COVID-19 susceptibility varied by geographical location. As explained by a study participant,
“our people believe that COVID-19 is for the cities, it is not found in the villages, hence there is reluctances in us who are in rural areas or rural small towns”(R12, Gospel minister).
3.3. Barriers
3.3.1. Lack of Knowledge
Participants identified the lack of knowledge as a barrier to COVID-19 vaccine uptake. Respondents indicated that proper knowledge of vaccines and their purpose was critical in fostering vaccine acceptance. This knowledge was fostered by public sensitization, as one participant highlighted:
“Once proper knowledge [is gained], those who have knowledge [have] a proper uptake of the vaccine.”(R1, Assistant Chief).
Particularly, knowledge was important for dispelling rumors about the COVID-19 vaccine. According to another participant:
“In my opinion you know if you inform the people about the drugs, you know they will be aware and willing, so that they can do away with the rumors of witchcraft and myths that is going around her in the community”(R7, Community health worker).
To inform the public about the vaccine study, participants reported that political and opinion leaders’ actions and words motivated or influenced the general population to take the COVID-19 vaccine. A nurse, who was one of the respondents, stated that:
“the people who are in power are a major factor, because the people are seeing them as an example, hence they feel motivated to go and receive the jab”(R11, Nurse).
The other factor cited to influence COVID-19 vaccine hesitancy was a lack of knowledge of what respondents termed “the basics of the vaccine.” This included its efficacy and side effects. As one respondent explained,
“There is lack of knowledge, people do not have the basics of the vaccine.” (R5, Security officer). Another added that, “…also others still don’t know the effects of the vaccine to them” (R2, Boda Boda Rider).
Overall, a lack of awareness was a significant barrier to vaccine uptake, as highlighted by a study participant, “lack of sensitization, there is lack of sensitization in the areas we are living in” (R8, Youth Mentor).
3.3.2. Misinformation
Another barrier was reported to be the perceived side effects of the vaccines, some of which arose from misinformation while others from lived experiences. The perceived side effects of the vaccine included the fear of blood clotting, trembling, and shaking and even death. According to a respondent, people’s willingness to take the vaccine was impacted by rumors of side effects:
“some are willing but there are some side effects of vaccine as in the rumors they normally hear from their friends and fellows.”(R3, CHV).
Some of the rumors that were shared about the side effects of the vaccine included trembling and shaking after vaccination, pain, nose bleeds and issues of blood clotting, as a respondent indicated: “there is also rumor that when you get the vaccine, there are issues of blood clotting and so on…” (R2, Boda Boda rider). And yet another participant highlighted,
“the issue of nose bleeding which some people saw in vaccinated people, this really affected the uptake, and hence people fear”.(R13, Evangelist).
Rumors also included the perceived inefficacy of the COVID-19 vaccine. As one respondent stated:
“there is a rumor that these vaccines does not treat, and also people now see it that even if you get vaccinated you will still get the virus if you are exposed”(R13, Evangelist).
Death was identified as one of the side effects of taking the vaccine, and, surprisingly, this was noted by a health professional:
“I fear that one can get abnormal side effects and also deaths, people fear death”(R9, Medical officer).
While some participants expressed perceptions of side effects, others highlighted side effects shared by those who had received the vaccine. For example, one of the participants explained that:
“we have cases that emerged, like for example people whom have been vaccinated will tell the rest on how they feel like the signs and symptoms like headache, tiredness and so on, also you have there are this category of people whom do not want to be injected, in that they prefer oral drugs, they are afraid of the injection”(R11, Nurse).
Other misinformation about the vaccine included rumors such as the COVD-19 vaccine being about population control of African populations by people from the West, with some asserting that those who get vaccinated ended up dead and that the vaccine would lower one’s immunity rather than boost it or even cause impotency among men and infertility in women. According to one respondent, “some people argue that it is a way of controlling the population, as a way of suppressing the African population.” (R1, Assistant chief).
Another participant echoed that, “some believe that it may lower the immunity for the oppressed.” (R5, security officer).
There were also rumors that the vaccine may impact reproduction. According to a study participant,
“I have heard people say that when you get vaccine, you may lose you fertility, so you may end up not giving birth”(R6, Islamic Religious Educator).
3.3.3. Access Issues
Barriers influencing COVID-19 uptake hesitancy included access issues, such as long queues, initially typical of vaccination centers, poor accessibility due to scarcity of vaccination sites and the fear of contracting the disease from the ensuing crowd. According to one of the participants,
“People fear to make a queue morning hour because they fear infected when they go to the crowd…”(R2, boda boda rider).
To highlight structural accessibility issues, one of the respondents stated that: “I can say the accessibility, so you know the transportation is very key and people are coming from very far, and people normally say that they are very committed with their daily activities so this is hard on them” (R3, CHV).
Particularly, the combination of distance and fear of side effects of the vaccine served as barriers to taking the COVID-19 vaccine. As a respondent explained,
“Number one I can say, those already vaccinated goes on talking about side effects, and these side effects makes people to fear to go and take the vaccine… number two, is the issue of the distance, you know many people come from far, and this will make people to board a motorbike and pay the service for transportation, so this is a factor”.(R8, Youth mentor).
3.3.4. Spousal Influence
It was also reported that COVID-19 vaccine hesitancy was influenced by spousal influence, particularly for women. One respondent posited that in certain circumstances, a husband could refuse to let his wife get vaccinated out of fear, especially if he does not want the vaccine himself. According to this participant,
“you find that on the side of pregnant women, her spouse may deny her a chance to go and take the vaccine because of fear of unknown effects”(R2, Boda Boda Rider).
Below is a conceptual illustration of our key findings (Figure 1).
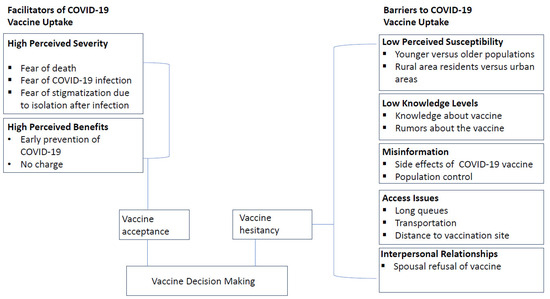
Figure 1.
A conceptual illustration of our key findings.
4. Discussion
This qualitative study explored the factors influencing COVID-19 vaccine uptake and hesitancy in Kenya. Upon analysis, the findings were found to fit within the framework of the Health Belief Model and were, thus, interpreted. Knowledge was a critical factor in fostering vaccine acceptance among participants in this study, which is consistent with findings from other studies, indicating that knowledge about the COVID-19 vaccine facilitates vaccine acceptance among Sub-Saharan African populations [77,78]. A lack of knowledge on the efficacy and side effects of the vaccine was highlighted as factors that influence vaccine uptake in the current study and other studies with African populations [35]. Misinformation in the current study included rumors about population control and that the vaccine lowers immunity. Misinformation about COVID-19 has been found to be particularly prevalent among varying African populations, leading to significant levels of vaccine hesitancy [7,79,80,81]. However, in the current study, participants also highlighted the fact that the COVID-19 vaccine did not prevent infection as a barrier to vaccine acceptance (and also people now see that, even if you get vaccinated, you will still get the virus if you are exposed” (R13)). Swan and colleagues posited that a vaccine’s population impacts depend on three factors, namely (1) reducing the likelihood of acquiring infection upon exposure (VESUSC), (2) reducing the likelihood of symptoms upon infection (VESYMP) and (3) decreasing the infectiousness of individuals who become infected (VEINF). However, the widely used COVID-19 vaccines at the time had either low or unknown VESUSC, VESYMP and VEINF [81]. The present study indicates that participants place a high premium on VESUSC and, therefore, constitutes important feedback for vaccine developers. Participants in this study suggested that public sensitization may increase knowledge about COVID-19 vaccines and combat vaccine-related misinformation. Although the Kenyan government engaged in the dissemination of COVID-19-related information to dispel misinformation, the extent to which these campaigns were effective is uncertain [82]. However, there is evidence suggesting that low levels of trust in the government may have reduced the acceptance of COVID-19-related government initiatives and information in Kenya [82].
A systematic review of the HBM applied to COVID-19 vaccine hesitancy indicated that cues to action have an inverse association with vaccine hesitancy [83]. Cues to action in this study included influence from political and opinion leaders, which aligns with findings from other studies examining the factors that impact COVID-19 vaccine acceptance across several countries [84,85]. Participants in this study reported that observing the loss of life among unvaccinated individuals served as a cue to action. This aligns with findings from the literature, suggesting that severity is positively associated with COVID-19 vaccine uptake [86,87].
The current study observed vaccine acceptance because of the perceived benefits, including that the vaccine prevents COVID-19 and improves immunity and the perceived severity of COVID-19, particularly the social consequences resulting from isolation and stigmatization. This is consistent with other findings from a quantitative study, showing an inverse association between the perceived benefits and severity of the COVID-19 vaccine and vaccine hesitancy [83]. The findings from this study indicated that younger populations did not perceive themselves to be at risk of COVID-19, which is consistent with findings from another study on the risk perceptions of COVID-19 among younger versus older populations in Sub-Saharan Africa (SSA) [88]. More so, perceived susceptibility to COVID-19 has shown negative associations with COVID-19 vaccine hesitancy, which supports the findings from this study, wherein vaccine uptake was reported to be lower among youths with reduced perceived susceptibility to COVID-19 [83].
Perceived barriers to COVID-19 vaccine uptake in this study included fear of vaccine safety and side effects, which align with evidence from the literature, highlighting factors associated with COVID-19 vaccine refusal in Kenya and other African countries [89,90,91]. Uniquely, in the present study, this fear was not merely driven by misinformation but particularly by the experience of others (people whom have been vaccinated will tell others how they feel, like the signs and symptoms of headache, tiredness and so on, R11… the issue of nose bleeding which some people saw in vaccinated people, this really affected the uptake, and hence people’s fear, R13). Another study characterized these side effects as mild to moderate in severity, with no significant influence or interference in individual daily activities [92]. These studies, however, were conducted in developed countries, where citizens have a greater understanding and awareness of vaccine adverse reactions, particularly among healthcare workers [93,94,95,96]. Our study indicates that they had an impact on vaccine hesitancy; thus, addressing them would be critical in fostering vaccine acceptance. Public health communication campaigns can focus more effort on educating the public on the side effects of vaccines. More particularly, vaccine developers should consider the impact that so-called mild to moderate reactions have on vaccine acceptance, alongside the more fundamental aspects of efficacy and safety, especially during a pandemic of a novel disease. Participants in the current study also identified the scarcity of vaccines and long waiting times at vaccination sites as barriers to vaccine uptake, which is consistent with results showing poor accessibility to COVID-19 vaccines in SSA countries, such as Ghana, South Africa and Zimbabwe [81,90]. The fear of contracting COVID-19 from crowds at vaccination sites is a unique finding in the current study that has not been reported elsewhere. Spousal influence on vaccine uptake resulted from fear of the vaccine, as reported by participants in this study. No other studies have reported on marital partners preventing the other from accessing COVID-19 vaccines among African populations. However, the concept of fear of the vaccine and its association with vaccine hesitancy have been found among some African populations [10,81]. This may be an area for further exploration in research in many more populations across the continent.
Recommendations
The establishment of a virtual system for mass education is crucial in improving vaccine-related knowledge in the general population, especially in the face of a pandemic, and should, therefore, be adopted by the Kenyan government. Such as system was instrumental in the COVID-19 response in Brazil and over 55 countries across the world [97,98].
Furthermore, a previous study reported a lack of proper reporting of adverse events following immunization in Kenya [99]. We recommend the establishment of a robust system for the surveillance of adverse events following immunization, which is important not only for monitoring but also the response, which can contribute to allaying public fears and fostering vaccine acceptance.
5. Conclusions
This study is not without limitations. As this was a qualitative study, it was impossible to draw any conclusions regarding causal associations between the variables determining vaccine hesitancy within the target population. The use of the KII approach fostered the possibility of bias in the selection of study participants. However, the KII also offers significant benefits in gathering key insights on the determinants of vaccine hesitancy from strategic community members with a deeper understanding of this phenomenon. The findings from this study will provide important guidance for implementing post-pandemic management interventions and informing future pandemic prevention strategies, with contextual considerations on the impact of the interventions to the targeted groups/populations and effectiveness towards desired outcomes.
Author Contributions
F.J.N.—conceptualized the study and significantly worked on the manuscript, revised and provided approval for submission. C.K.N.—conceptualized the study, data collection, manuscript preparation and revisions. W.C.—conceptualized the study, methods, data analysis, and reporting and manuscript revision. W.A.—data collection, manuscript preparation and revisions, T.A.—manuscript preparation and revision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the University of Eastern Africa, Baraton. Approval Code: (UEAB/REC/50/03/2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study by signing a consent form that had an explanation of the voluntary participation and purpose of the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are contained within this article. Any additional data or clarifications are available upon reasonable request.
Acknowledgments
We are grateful to all the research assistants and field coordinators who helped with the study. We acknowledge the participation of those who agreed to be interviewed for their time and shared experiences with us.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. From Emergency Response to Long-Term COVID-19 Disease Management: Sustaining Gains Made during the COVID-19 Pandemic. Available online: https://www.who.int/publications/i/item/WHO-WHE-SPP-2023.1 (accessed on 10 October 2023).
- Cohen, L.E.; Spiro, D.J.; Viboud, C. Projecting the SARS-CoV-2 transition from pandemicity to endemicity: Epidemiological and immunological considerations. PLoS Pathog. 2022, 18, e1010591. [Google Scholar] [CrossRef] [PubMed]
- Katzourakis, A. COVID-19—Endemic doesn’t mean harmless. Nature 2022, 601, 485. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.M.; Doster, J.M.; Landwehr, E.H.; Kumar, N.P.; White, E.J.; Beachboard, D.C.; Stobart, C.C. Evaluating the Virology and Evolution of Seasonal Human Coronaviruses Associated with the Common Cold in the COVID-19 Era. Microorganisms 2023, 11, 445. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Managing the COVID-19 Infodemic: A Call to Action. 2020. Available online: https://www.who.int/news/item/11-12-2020-call-for-action-managing-the-infodemic (accessed on 10 October 2023).
- Zarocostas, J. How to fight an infodemic. Lancet 2020, 395, 676. [Google Scholar] [CrossRef]
- Okereke, M.; Ukor, N.A.; Ngaruiya, L.M.; Mwansa, C.; Alhaj, S.M.; Ogunkola, I.O.; Jaber, H.M.; Isa, M.A.; Ekpenyong, A.; Lucero-Prisno III, D.E. COVID-19 Misinformation and Infodemic in Rural Africa. Am. J. Trop. Med. Hyg. 2020, 104, 453–456. [Google Scholar] [CrossRef] [PubMed]
- United Nations. UN Tackles Infodemic of Misinformation and Cybercrime in COVID-19 Crisis. 2020. Available online: https://www.un.org/en/un-coronavirus-communications-team/un-tackling-%E2%80%98infodemic%E2%80%99-misinformation-and-cybercrime-covid-19 (accessed on 15 October 2023).
- Fajar, J.K.; Sallam, M.; Soegiarto, G.; Sugiri, Y.J.; Anshory, M.; Wulandari, L.; Kosasih, S.A.P.; Ilmawan, M.; Kusnaeni, K.; Fikri, M.; et al. Global prevalence, and potential influencing factors of COVID-19 vaccination hesitancy: A meta-analysis. Vaccines 2022, 10, 1356. [Google Scholar] [CrossRef] [PubMed]
- Ngangue, P.; Pilabré, A.H.; Barro, A.; Pafadnam, Y.; Bationo, N.; Soubeiga, D. Public attitudes towards COVID-19 vaccines in Africa: A systematic review. J. Public Health Afr. 2022, 13, 2181. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report of The Sage Working Group on Vaccine Hesitancy. 2014. Available online: https://www.asset-scienceinsociety.eu/sites/default/files/sage_working_group_revised_report_vaccine_hesitancy.pdf (accessed on 4 November 2023).
- Sallam, M. COVID-19 Vaccine hesitancy worldwide: A systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef]
- McCready, J.L.; Nichol, B.; Steen, M.; Unsworth, J.; Comparcini, D.; Tomietto, M. Understanding the barriers and facilitators of vaccine hesitancy towards the COVID-19 vaccine in healthcare workers and healthcare students worldwide: An Umbrella Review. PLoS ONE 2023, 18, e0280439. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Orenstein, W.A.; Ahmed, R. Vaccination saves lives. Proc. Natl. Acad. Sci. USA 2017, 114, 4031–4033. [Google Scholar] [CrossRef] [PubMed]
- Blume, S. Anti-Vaccination Movements and Their Interpretations. Soc. Sci. Med. 2006, 62, 628–642. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Nuwarda, R.F.; Ramzan, I.; Weekes, L.; Kayser, V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines 2022, 10, 1595. [Google Scholar] [CrossRef] [PubMed]
- Spier, R.E. Perception of risk of vaccine adverse events: A historical perspective. Vaccine 2002, 20 (Suppl. S1), S78–S84. [Google Scholar] [CrossRef]
- Wolfe, R.M.; Sharp, L.K. Anti-vaccinationists past and present. BMJ 2002, 325, 430–432. [Google Scholar] [CrossRef] [PubMed]
- Galagali, P.M.; Kinikar, A.A.; Kumar, V.S. Vaccine Hesitancy: Obstacles and Challenges. Curr. Pediatr. Rep. 2022, 10, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Hassan, R.S.; Yousaf, M.; Zaman, U.; Waheed, K.S.; Core, R.; Malik, A. Unlocking infodemics and mysteries in COVID-19 vaccine hesitancy: Nexus of conspiracy beliefs, digital informational support, psychological Well-being, and religious fatalism. Vaccine 2023, 41, 1703–1715. [Google Scholar] [CrossRef]
- Wilson, S.L.; Wiysonge, C. Social Media and Vaccine Hesitancy. BMJ Glob. Health 2020, 5, e004206. [Google Scholar] [CrossRef]
- Hicks, A.; Lloyd, A. Agency and liminality during the COVID-19 pandemic: Why information literacy cannot fix vaccine hesitancy. J. Inf. Sci. 2022, 1–16. [Google Scholar] [CrossRef]
- Bednarczyk, R.A.; Dew, M.A.; Hart, T.A.; Freedland, K.E.; Kaufmann, P.G. Introduction to the special issue on vaccine hesitancy and refusal. Health Psychol. 2023, 42, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Dubé, È.; Ward, J.K.; Verger, P.; MacDonald, N.E. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu. Rev. Public Health 2012, 42, 175–191. [Google Scholar] [CrossRef]
- Malone, K.M.; Alan, R.; Hinman, A.R. Vaccine Mandates: The Public Health Imperative and Individual Rights. n.d. Available online: https://www.cdc.gov/vaccines/imz-managers/guides-pubs/downloads/vacc_mandates_chptr13.pdf (accessed on 3 February 2024).
- Omer, S.B.; Salmon, D.A.; Orenstein, W.A.; de Hart, M.P.; Halsey, N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N. Engl. J. Med. 2009, 360, 1981–1988. [Google Scholar] [CrossRef]
- Salmon, D.A.; Omer, S.B. Individual freedoms versus collective responsibility: Immunization decision-making in the face of occasionally competing values. Emerg. Themes Epidemiol. 2006, 3, 13. [Google Scholar] [CrossRef]
- Patel, M.; Lee, A.; Redd, S.; Clemmons, N.; McNaiill, R.; Cohn, A.; Gastañaduy, P. Increase in Measles Cases-United States, 1 January–26 April 2019. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 402–404. [Google Scholar] [CrossRef]
- Afolabi, A.A.; Ilesanmi, O.S. Dealing with vaccine hesitancy in Africa: The prospective COVID-19 vaccine context. Pan Afr. Med. J. 2021, 38, 3. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 August 2023).
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope, and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Oliveira, I.S.; Cardoso, L.S.; Ferreira, I.G.; Alexandre-Silva, G.M.; Jacob BC, D.S.; Cerni, F.A.; Monteiro, W.M.; Zottich, U.; Pucca, M.B. Anti-vaccination movements in the world and in Brazil. Rev. Da Soc. Bras. De Med. Trop. 2022, 55, e05922021. [Google Scholar] [CrossRef] [PubMed]
- Nihlén Fahlquist, J. Vaccine hesitancy and trust: Ethical aspects of risk communication. Scand. J. Public Health 2017, 46, 182–188. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Dube, E.; Comeau, J.L. Have vaccine hesitancy models oversimplified a complex problem to our detriment? The Adapted Royal Society of Canada vaccine uptake framework. Vaccine 2022, 40, 3927–3930. [Google Scholar] [CrossRef]
- Frew, P.M.; Murden, R.; Mehta, C.C.; Chamberlain, A.T.; Hinman, A.R.; Nowak, G.; Mendel, J.; Aikin, A.; Randall, L.A.; Hargreaves, A.L.; et al. Development of a US trust measure to assess and monitor parental confidence in the vaccine system. Vaccine 2019, 37, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Gust, D.; Brown, C.; Sheedy, K.; Hibbs, B.; Weaver, D.; Nowak, G. Immunization attitudes and beliefs among parents: Beyond a dichotomous perspective. Am. J. Health Behav. 2005, 29, 81–92. [Google Scholar] [CrossRef]
- Opel, D.J.; Taylor, J.A.; Zhou, C.; Catz, S.; Myaing, M.; Mangione-Smith, R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: A validation study. JAMA Pediatr. 2013, 167, 1065–1071. [Google Scholar] [CrossRef]
- Rossen, I.; Hurlstone, M.J.; Lawrence, C. Going with the Grain of Cognition: Applying Insights from Psychology to Build Support for Childhood Vaccination. Front. Psychol. 2016, 7, 1483. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of influenza vaccination intention and behavior—A systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Welch, V.L.; Metcalf, T.; Macey, R.; Markus, K.; Sears, A.J.; Enstone, A.; Langer, J.; Srivastava, A.; Cane, A.; Wiemken, T.L. Understanding the Barriers and Attitudes toward Influenza Vaccine Uptake in the Adult General Population: A Rapid Review. Vaccines 2023, 11, 180. [Google Scholar] [CrossRef]
- Ver, A.T.; Notarte, K.I.; Velasco, J.V.; Buac, K.M.; Nazareno, J., 3rd; Lozañes, J.A.; Antonio, D.; Bacorro, W. A systematic review of the barriers to implementing human papillomavirus vaccination programs in low- and middle-income countries in the Asia-Pacific. Asia-Pac. J. Clin. Oncol. 2021, 17, 530–545. [Google Scholar] [CrossRef] [PubMed]
- Ilesanmi, O.; Afolabi, A. Perception and practices during the COVID-19 pandemic in an urban community in Nigeria: A cross-sectional study. PeerJ 2020, 8, e10038. [Google Scholar] [CrossRef] [PubMed]
- Ochola, E.A. Vaccine Hesitancy in Sub-Saharan Africa in the Context of COVID-19 Vaccination Exercise: A Systematic Review. Diseases 2023, 11, 32. [Google Scholar] [CrossRef]
- Ackah, B.B.B.; Woo, M.; Stallwood, L.; Fazal, Z.A.; Okpani, A.; Ukah, U.V.; Adu, P.A. COVID-19 vaccine hesitancy in Africa: A scoping review. Glob. Health Res. Policy 2022, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Archibong, B.; Annan, F. ‘We Are Not Guinea Pigs’: The Effects of Disclosure of Medical Misconduct on Vaccine Compliance. JEL Classification: I12, I14, I18, D83, O12, Z12. 2021, 10. Available online: https://www.brookings.edu/wp-content/uploads/2021/12/We-are-not-guinea-pigs_final.pdf (accessed on 6 January 2024).
- Cooper, S.; Betsch, C.; Sambalaa, E.Z.; Mchizaa, N.; Wiysongea, C.S. Vaccine hesitancy—A potential threat to the achievements of vaccination programmes in Africa. Hum. Vaccines Immunother. 2018, 14, 2355–23571. [Google Scholar] [CrossRef] [PubMed]
- Lowes, S.; Montero, E. The Legacy of Colonial Medicine in Central Africa. Am. Econ. Rev. 2021, 111, 1284–1314. [Google Scholar] [CrossRef]
- Orangi, S.; Mbuthia, D.; Chondo, E.; Ngunu, C.; Kabia, E.; Ojal, J.; Barasa, E. A qualitative inquiry on drivers of COVID-19 vaccine hesitancy among adults in Kenya. PLOS Glob. Public Health 2024, 4, e0002986. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Combatting Antivaccination Rumours: Lessons Learned from Case Studies in East Africa. n.d. Available online: https://www.comminit.com/unicef/content/combatting-antivaccination-rumours-lessons-learned-case-studies-east-africa (accessed on 6 January 2024).
- BBC. Coronavirus: France Racism Row over Doctors’ Africa Testing Comments. Available online: https://www.bbc.com/news/world-europe-52151722 (accessed on 24 February 2024).
- Obregón, R.; Chitnis, K.; Morry, C.; Feek, W.; Bates, J.; Galway, M.; Ogden, E. Achieving polio eradication: A review of health communication evidence and lessons learned in India and Pakistan. Bull. World Health Organ. 2009, 87, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.J.; Smith, H.; Llewellyn, C. Evaluating the effectiveness of health belief model interventions in improving adherence: A systematic review. Health Psychol. Rev. 2014, 8, 253–269. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. Why people use health services. Milbank Meml. Fund Q. 1966, 44, 94–127. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The health belief model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef]
- Harrison, J.A.; Mullen, P.D.; Green, L.W. A meta-analysis of studies of the health belief model with adults. Health Educ. Res. 1992, 7, 107–116. [Google Scholar] [CrossRef]
- Sohl, S.J.; Moyer, A. Tailored interventions to promote mammography screening: A meta-analytic review. Prev. Med. 2007, 45, 252–261. [Google Scholar] [CrossRef]
- Carpenter, C.J. A meta-analysis of the effectiveness of Health Belief Model Variables in predicting behavior. Health Commun. 2010, 25, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Orji, R.; Vassileva, J.; Mandryk, R. Towards an effective health interventions design: An Extension of the Health Belief Model. Online J. Public Health Inform. 2012, 4, ojphi.v4i3.4321. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.; Campbell, R.; Hildona, Z.; Hobbs, L.; Michie, S. Theories of behaviour and behaviour change across the social and behavioral sciences: A scoping review. Health Psychol. 2015, 9, 323–344. [Google Scholar] [CrossRef] [PubMed]
- Renjith, V.; Yesodharan, R.; Noronha, J.A.; Ladd, E.; George, A. Qualitative methods in healthcare research. Int. J. Prev. Med. 2021, 12, 20. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://en.wikipedia.org/wiki/Counties_of_Kenya (accessed on 26 April 2023).
- Muellmann, S.; Brand, T.; Jürgens, D.; Gansefort, D.; Zeeb, H. How many key informants are enough? Analysing the validity of the community readiness assessment. BMC Res. Notes 2021, 14, 85. [Google Scholar] [CrossRef] [PubMed]
- Pahwa, M.; Cavanagh, A.; Vanstone, M. Key Informants in Applied Qualitative Health Research. Qual. Health Res. 2023, 33, 1251–1261. [Google Scholar] [CrossRef] [PubMed]
- McKenna, S.A.; Main, D.S. The role and influence of key informants in community-engaged research: A critical perspective. Action Res. 2013, 11, 113–124. [Google Scholar] [CrossRef]
- Neergaard, M.A.; Olesen, F.; Andersen, R.S.; Sondergaard, J. Qualitative description—The poor cousin of health research? BMC Med. Res. Methodol. 2009, 9, 52. [Google Scholar] [CrossRef]
- Donnelly, C.; Janssen, A.; Shah, K.; Harnett, P.; Vinod, S.; Shaw, T.J. Qualitative study of international key informants’ perspectives on the current and future state of healthcare quality measurement and feedback. BMJ Open 2023, 13, e073697. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Javadi, M.; Zarea, M. Understanding Thematic Analysis and its Pitfalls. J. Client Care 2016, 1, 33–39. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Research and Evaluation Methods, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Cresswell, J.W.; Plano Clark, V.L. Designing and Conducting Mixed Method Research, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Furber, C. Framework analysis: A method for analyzing qualitative data. AJM 2010, 4, 97–100. [Google Scholar] [CrossRef]
- Miner, C.A.; Timothy, C.G.; Percy, K.; Mashige Osuagwu, U.L.; Envuladu, E.A.; Amiebenomo, O.M.A.; Ovenseri-Ogbomo, G.; Charwe, D.D.; Goson, P.C.; Ekpenyong, B.N. Acceptance of COVID-19 vaccine among sub-Saharan Africans (SSA): A comparative study of residents and diasporan dwellers. BMC Public Health 2023, 23, 191. [Google Scholar] [CrossRef] [PubMed]
- Osuagwu, U.L.; Miner, C.A.; Bhattarai, D.; Mashige, K.P.; Oloruntoba, R.; Abu, E.K.; Ekpenyong, B.; Chikasirimobi, T.G.; Goson, P.C.; Ovenseri-Ogbomo, G.O.; et al. Misinformation About COVID-19 in Sub-Saharan Africa: Evidence from a Cross-Sectional Survey. Health Secur. 2021, 19, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Afrifa-Anane, G.F.; Larbi, R.T.; Addo, B.; Agyekum, M.W.; Kyei-Arthur, F.; Appiah, M.; Agyemang, C.O.; Sakada, I.G. Facilitators and barriers to COVID-19 vaccine uptake among women in two regions of Ghana: A qualitative study. PLoS ONE 2022, 17, e0272876. [Google Scholar] [CrossRef] [PubMed]
- Adebisi, Y.A.; Rabe, A.; Lucero-Prisno Iii, D.E. Risk communication and community engagement strategies for COVID-19 in 13 African countries. Health Promot. Perspect. 2021, 11, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Swan, D.A.; Bracis, C.; Janes, H.; Moore, M.; Matrajt, L.; Reeves, D.B.; Burns, E.; Donnell, D.; Cohen, M.S.; Schiffer, J.T.; et al. COVID-19 vaccines that reduce symptoms but do not block infection need higher coverage and faster rollout to achieve population impact. Sci. Rep. 2021, 11, 15531. [Google Scholar] [CrossRef]
- Ireri, E.M.; Mutugi, M.W.; Falisse, J.B.; Mwitari, J.M.; Atambo, L.K. Influence of conspiracy theories and distrust of community health volunteers on adherence to COVID-19 guidelines and vaccine uptake in Kenya. PLOS Glob. Public Health 2023, 3, e0001146. [Google Scholar] [CrossRef]
- Limbu, Y.B.; Gautam, R.K.; Pham, L. The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 973. [Google Scholar] [CrossRef]
- Patwary, M.M.; Alam, M.A.; Bardhan, M.; Disha, A.S.; Haque, M.Z.; Billah, S.M.; Kabir, M.P.; Browning, M.H.E.M.; Rahman, M.M.; Parsa, A.D.; et al. COVID-19 Vaccine Acceptance among Low- and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines 2022, 10, 427. [Google Scholar] [CrossRef] [PubMed]
- Kerr, J.R.; Schneider, C.R.; Recchia, G.; Dryhurst, S.; Sahlin, U.; Dufouil, C.; Arwidson, P.; Freeman, A.L.; van der Linden, S. Correlates of intended COVID-19 vaccine acceptance across time and countries: Results from a series of cross-sectional surveys. BMJ Open 2021, 11, e048025. [Google Scholar] [CrossRef]
- Yang, X.; Wei, L.; Liu, Z. Promoting COVID-19 Vaccination Using the Health Belief Model: Does Information Acquisition from Divergent Sources Make a Difference? Int. J. Environ. Res. Public Health 2022, 19, 3887. [Google Scholar] [CrossRef] [PubMed]
- Rani MD, M.; Mohamed, N.A.; Solehan, H.M.; Ithnin, M.; Ariffien, A.R.; Isahak, I. Assessment of acceptability of the COVID-19 vaccine based on the health belief model among Malaysians-A qualitative approach. PLoS ONE 2022, 17, e0269059. [Google Scholar] [CrossRef]
- Abu, E.K.; Oloruntoba, R.; Osuagwu, U.L.; Bhattarai, D.; Miner, C.A.; Goson, P.C.; Langsi, R.; Nwaeze, O.; Chikasirimobi, T.G.; Ovenseri-Ogbomo, G.O.; et al. Risk perception of COVID-19 among sub-Sahara Africans: A web-based comparative survey of local and diaspora residents. BMC Public Health 2021, 21, 1562. [Google Scholar] [CrossRef] [PubMed]
- Rego, R.T.; Kenney, B.; Ngugi, A.K.; Espira, L.; Orwa, J.; Siwo, G.H.; Sefa, C.; Shah, J.; Weinheimer-Haus, E.; Delius, A.J.S.; et al. COVID-19 vaccination refusal trends in Kenya over 2021. Vaccine 2023, 41, 1161–1168. [Google Scholar] [CrossRef]
- Myburgh, N.; Mulaudzi, M.; Tshabalala, G.; Beta, N.; Gutu, K.; Vermaak, S.; Lau, C.; Hill, C.; Stanberry, L.; James, W.; et al. A Qualitative Study Exploring Motivators and Barriers to COVID-19 Vaccine Uptake among Adults in South Africa and Zimbabwe. Vaccines 2023, 11, 729. [Google Scholar] [CrossRef]
- Naidoo, D.; Meyer-Weitz, A.; Govender, K. Factors Influencing the Intention and Uptake of COVID-19 Vaccines on the African Continent: A Scoping Review. Vaccines 2023, 11, 873. [Google Scholar] [CrossRef]
- Acheampong, T.; Akorsikumah, E.A.; Osae-Kwapong, J.; Khalid, M.; Appiah, A.; Amuasi, J.H. Examining Vaccine Hesitancy in Sub-Saharan Africa: A Survey of the Knowledge and Attitudes among Adults to Receive COVID-19 Vaccines in Ghana. Vaccines 2021, 9, 814. [Google Scholar] [CrossRef]
- Dhamanti, I.; Suwantika, A.A.; Adlia, A.; Yamani, L.N.; Yakub, F. Adverse Reactions of COVID-19 Vaccines: A Scoping Review of Observational Studies. Int. J. Gen. Med. 2023, 16, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Sakong, J.; Jo, S.; Kim, M.; Baek, K. Adverse effects on work and daily life interference among healthcare workers after the first and second chadox1 and bnt162b2 COVID-19 vaccine doses. Vaccines 2021, 9, 926. [Google Scholar] [CrossRef] [PubMed]
- Kadali, R.A.K.; Janagama, R.; Peruru, S.; Malayala, S.V. Side effects of BNT162b2 mRNA COVID-19 vaccine: A randomized, cross-sectional study with detailed self-reported symptoms from healthcare workers. Int. J. Infect Dis. 2021, 106, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Bsoul, E.A.; Loomer, P.M.; Patel, S.K.S. COVID-19 vaccination experience among United States dental professionals and students: Safety, confidence, concerns, and side effects. PLoS ONE 2022, 17, e0264323. [Google Scholar] [CrossRef] [PubMed]
- Valentim, R.A.D.M.; Lima, T.S.; Cortez, L.R.; Barros, D.M.D.S.; Silva, R.D.D.; Paiva, J.C.D.; Andrade, F.R.D. The relevance a technology ecosystem in the Brazilian National Health Service’s COVID-19 response: The case of Rio Grande do Norte, Brazil. Ciência Saúde Coletiva 2021, 26, 2035–2052. [Google Scholar]
- Valentim, J.L.; Dias-Trindade, S.; Oliveira, E.S.; Moreira, J.A.; Fernandes, F.; Romão, M.H.; Morais, P.S.; Caitano, A.R.; Dias, A.P.; Oliveira, C.A.; et al. The relevancy of massive health education in the Brazilian prison system: The course “health care for people deprived of freedom” and its impacts. Front. Public Health 2022, 10, 935389. [Google Scholar] [CrossRef]
- Malande, O.O.; Munube, D.; Afaayo, R.N.; Chemweno, C.; Nzoka, M.; Kipsang, J.; Musyoki, A.M.; Meyer, J.C.; Omayo, L.N.; Owino-Okongo, L. Adverse events following immunization reporting and impact on immunization services in informal settlements in Nairobi, Kenya: A prospective mixed-methods study. Pan Afr. Med. J. 2021, 40, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).