1. Introduction
In Fall 2020, the sociopolitical landscape of the United States was one of collective anxiety and uncertainty, driven by the evolving COVID-19 disease dynamics. Vaccines against the virus first became available in the US in December 2020 when the Food and Drug Administration (FDA) granted Emergency Use Authorization (EUA) to the Pfizer-BioNTech vaccine on 11 December 2020. Shortly thereafter, the Moderna vaccine received emergency authorization. Since then, several vaccines and boosters have received authorization and full approval, expanding the range of options available for vaccination in the US and around the world. By March 2024, 81.4% of the US population had received at least one dose of a COVID-19 vaccine, with 69.5% of them completing a primary series and 17% receiving an updated (bivalent) booster dose which was later introduced to boost and sustain immunity against a rapidly evolving virus [
1]. More recently (in September 2023), the FDA approved and authorized an updated COVID-19 vaccine to coincide with the 2023-24 flu season, formulated to target the latest variants of COVID-19 [
2].
In retrospect, vaccine development and deployment may be seen largely as a success story, based on the sheer number of people who have received at least one dose of a COVID-19 vaccine. Yet, the human responses to the crisis have been far from ideal. Recognizing that many of the failures were in the realm of human dynamics, social scientists have identified a complex interplay of social, psychological, political, economic, and cultural factors that have contributed to the still unfolding story of the pandemic. These include attitudes towards COVID-19 and behaviors pertaining to pharmaceutical and nonpharmaceutical interventions to mitigate it. Scholars, public health experts, and others with an interest in the area remain keen on learning and applying lessons from the first pandemic of the information age towards future pandemic preparedness.
Factors driving COVID-19 attitudes and behaviors have evolved over time as our understanding of the virus and the pandemic itself has developed. Yet, within the rich extant scholarship, a few clear patterns have emerged. In particular, this work suggests that a range of individual-level factors, contextual factors, and demographics shape COVID-19 attitudes and behavior. These include knowledge, risk perception, media and information access, peer influence, employment, education, healthcare access, trust, and demographic characteristics, such as age, political orientation, and gender [
3,
4,
5].
As far as vaccination intention and intake are concerned, extant scholarship identifies several individual and demographic factors as well as contextual factors driving these attitudes and behaviors. Individual-level factors include affective constructs, such as risk perception, where research finds that those who have higher risk perceptions regarding contracting and spreading COVID-19 tend to exhibit lower vaccine hesitancy [
6]. Prominent demographic and ideological factors that shape vaccine attitudes include racial/ethnic background, socioeconomic status (SES), gender, and political ideology. For instance, COVID-19 vaccine intake and intention differ between Black and White residents in the US due to concerns over safety and efficacy, but also importantly due to structural barriers related to knowledge, access, and precarious occupational conditions, which disproportionately affect Black residents [
7]. Elsewhere, extant scholarship has demonstrated SES, education, age, and gender to be variably associated with COVID-19 vaccine attitudes [
8]. Peer influence matters too, to the extent that one’s attitudes towards a contentious topic constitute an important part of one’s social identity [
9]. These identity dynamics suggest that we are influenced by an affinity to and behavior of those in our “in-group”.
In a recent meta-analysis of demographic variability of vaccine attitudes in the US, Dhanani and Franz [
10] found the highest variability across race and political affiliation. Black respondents and Republicans reported higher vaccine hesitancy than their White and Democrat counterparts. In fact, political ideology is a well-documented determinant of vaccine attitudes in the US where conservatives tend to be more vaccine hesitant than liberals [
11,
12,
13,
14]. Recent research does not support earlier contentions that both conservatives and liberals harbor biases against vaccines due to different concerns, e.g., individual rights in the case of conservatives and distrust of “Big Pharma” in the case of liberals [
11].
Among contextual factors, media coverage and media polarization emerge as important factors that confound vaccine attitudes. Consider recent Gallup polls that show that while 70% of Democrats agree that they have a “great deal/fair amount of trust and confidence in the mass media to report the news fully, accurately and fairly”, only 14% of Republicans agreed with the same. This compares to 27% of those who identified as politically independent [
15]. This level of polarization in attitudes towards mainstream media is indicative of an “echo chamber” effect: a phenomenon described as an outcome of social groups limiting themselves to only receiving information that matches their pre-established ideological foundations [
16,
17]. As people isolate themselves into selective information ecosystems, these systems evolve into “filter bubbles.” This sorting is accelerated by social media algorithms which predict and selectively expose participants to more of what they may desire [
18]. Partisan media feeds into this mechanism, compelling those who are at the receiving end to engage in “motivated reasoning” when presented with new information or information that does not align with their prior beliefs. Motivated reasoning may lead to several outcomes: the recipient may outright reject the new information, they may intensify their prior views, or they may believe mis/disinformation driven by their identity/ideology [
19,
20]. Prior work demonstrates that political orientation (both political party identification and political ideology) is the primary cause of motivated reasoning [
21]. In the current media ecosystem, Altman et al. [
22] argue that “Polarizing viewpoints are inevitable, but they have been heightened as social media has become the main source of information for many, and misinformation about vaccines has flooded platforms in the wake of COVID-19”. In short, extant research suggests that closely held ideologies, such as political views, in combination with mis/disinformation, have continued to shape vaccine attitudes in the US, leading to more conservative/Republican vaccine hesitancy, even though the vaccine launch itself was primarily associated with a conservative administration [
5,
23,
24].
2. The Current Research
In Fall 2020, our research team developed a survey to collect data on attitudes and behavior towards COVID-19. Data collection occurred between October and December 2020 and concluded just before the first COVID-19 vaccine was administered in the US, on 14 December 2020, when a nurse in New York was given the vaccine [
25]. Given this timeline, our survey asks about vaccination intention: “If a vaccine against COVID-19 is approved by the FDA (Food and Drug Administration) and becomes available, would you get vaccinated?” Consequently, our data pertain to the development stage, prior to the vaccine rollout in the US, where there was no safety and efficacy data available, yet there was widespread media reporting about the expected vaccine rollout with political polarization of the issue already beginning to take shape. This fracturing was visible when survey data from a Kaiser Family Foundation’s COVID-19 Vaccine Monitor as early as December 2020 found that, amidst “promising news about several COVID-19 vaccine candidates, vaccine hesitancy remained the highest among Republicans (42%), followed by those aged 30–49 (36%) and rural residents (35%)” [
26]. Glaring implications of the politicization of vaccines and the polarization of attitudes towards it is seen in recent research that reports higher excess mortality for Republican voters than Democratic voters “after COVID-19 vaccines were available to all adults, but not before” [
27].
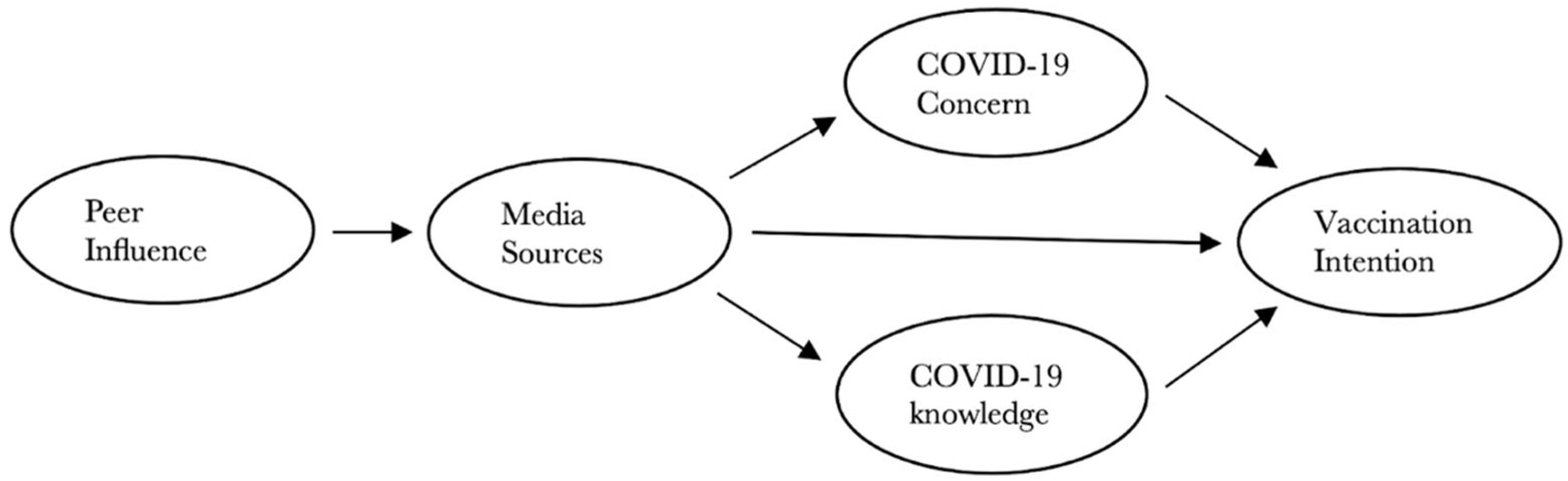
To understand how sociodemographic and contextual factors shaped COVID-19 vaccination intention in the early phase of the pandemic, we test a conceptual model using structural equation modeling (SEM). Our model posits a causal relationship between COVID-19 knowledge, concern, peer influence, media access, and vaccination intention. We further determine how five exogenous variables (political ideology, gender, age, race, and rurality) factor into behavioral intention. Given the ensuing political polarization of attitudes towards COVID-19 vaccines, we test our conceptual model for three different conditions based on primary media sources: a conservative media model (A), a mainstream media model (B), and a mainstream and liberal media model (C). The factors considered in our conceptual model draw from two foundational theories of health promotion and health behavior—the health belief model (HBM) and the theory of planned behavior (TPB). Specifically, COVID-19 concern aligns with “perceived severity” and COVID-19 knowledge aligns with “self-efficacy” from the HBM. Peer influence aligns with “subjective norms” from the TPB. Media access falls under “perceived barriers” and “supplemental self-efficacy” from the HBM [
28].
We believe that our study sheds important light on emerging social dynamics that would subsequently change the nature of one of the most significant public health crises/campaigns in the US, and ultimately the world. In particular, the empirical findings regarding the impacts of political ideology and the role of media/information in reinforcing ideologically driven behaviors and attitudes should be essential considerations for future pandemic preparedness. As vaccine hesitancy has remained an important public health issue, better understanding the hesitant groups, their ideological foundations, and their levels of openness to public health interventions is essential to developing communication and policy around these target groups.
4. Results
The sample demographics table in
Supplementary Materials (S4) includes the demographic distributions for ID, TX, and VT samples, as well as the full survey sample. Of the full sample, 55% identify as female, 44% identify as male, and 0.6% do not identify with a binary gender category. Our sample is skewed for education in that 66% have a bachelor’s degree or a higher level of education. Further, 16% have obtained some college, while 9% have completed an associate’s degree. Only 0.4% of the sample identified as having less than a high school degree. The mean age of the sample is 55 years, with ages ranging from 18–96, (SD = 16.42). In terms of race, the majority of respondents identify as white (85%), while the second highest category (7%) did not provide a response to this question. In terms of ethnicity, only 4% of our respondents identified as Hispanic or Latino. About equal percentages of survey respondents identify as politically moderate (29.6%), liberal (28.5%), or conservative (28.2%), followed by 7.9% that identify as non-political, 3.6% libertarian, and 2.2% other. When considering race, education, and age, the disproportionate representation of respondents identifying as white, having higher levels of education, and being older, are trends observed frequently in mail surveys [
31].
We calculated individual model fit statistics and performed pairwise comparisons for all three SEM models. AIC values for the conservative media model (A), mainstream media model (B), and mainstream and liberal media model (C) are 12,590, 14,973, and 17,171, respectively. This indicates that model A has the lowest predictive error. Additionally, the lavaan test statistic for the models was calculated and compared pairwise using the
lavtestLRT function in the
lavaan package. With this test, model A performs better than models B and C, with a
p-value less than 0.001 for each comparison. Based on the results of these model fit measures, model A (conservative media model) appears to be the best-supported model (
Supplementary Materials, S6).
We also considered additional models which included mainstream and conservative media (
Supplementary Materials, S10) and all of the media sources (
Supplementary Materials, S11). However, the fit for these models was substantially worse than the models presented here (e.g., a combined conservative media and mainstream media model resulted in significantly lower fit measures than our best-fit model (A) with a chi-squared difference of 219.7). Additionally, results from exploratory factor analysis indicate that a two-factor decomposition is appropriate for decomposing the information sources (see
Supplementary Materials, S3). Combining this with the correlations for media sources (see
Supplementary Materials, S2) led us to design the models with the information sources of conservative media, mainstream media, and mainstream and liberal media.
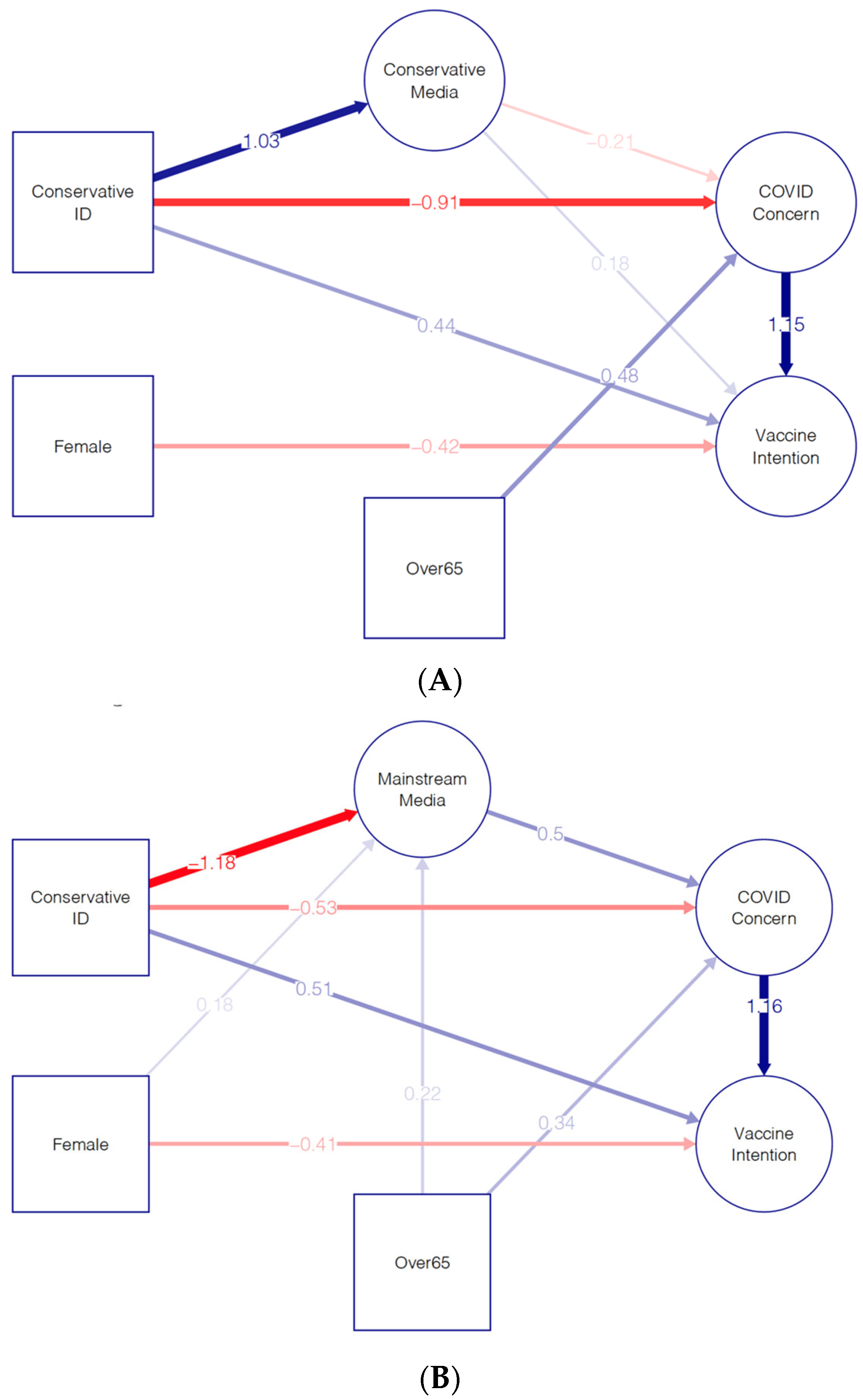
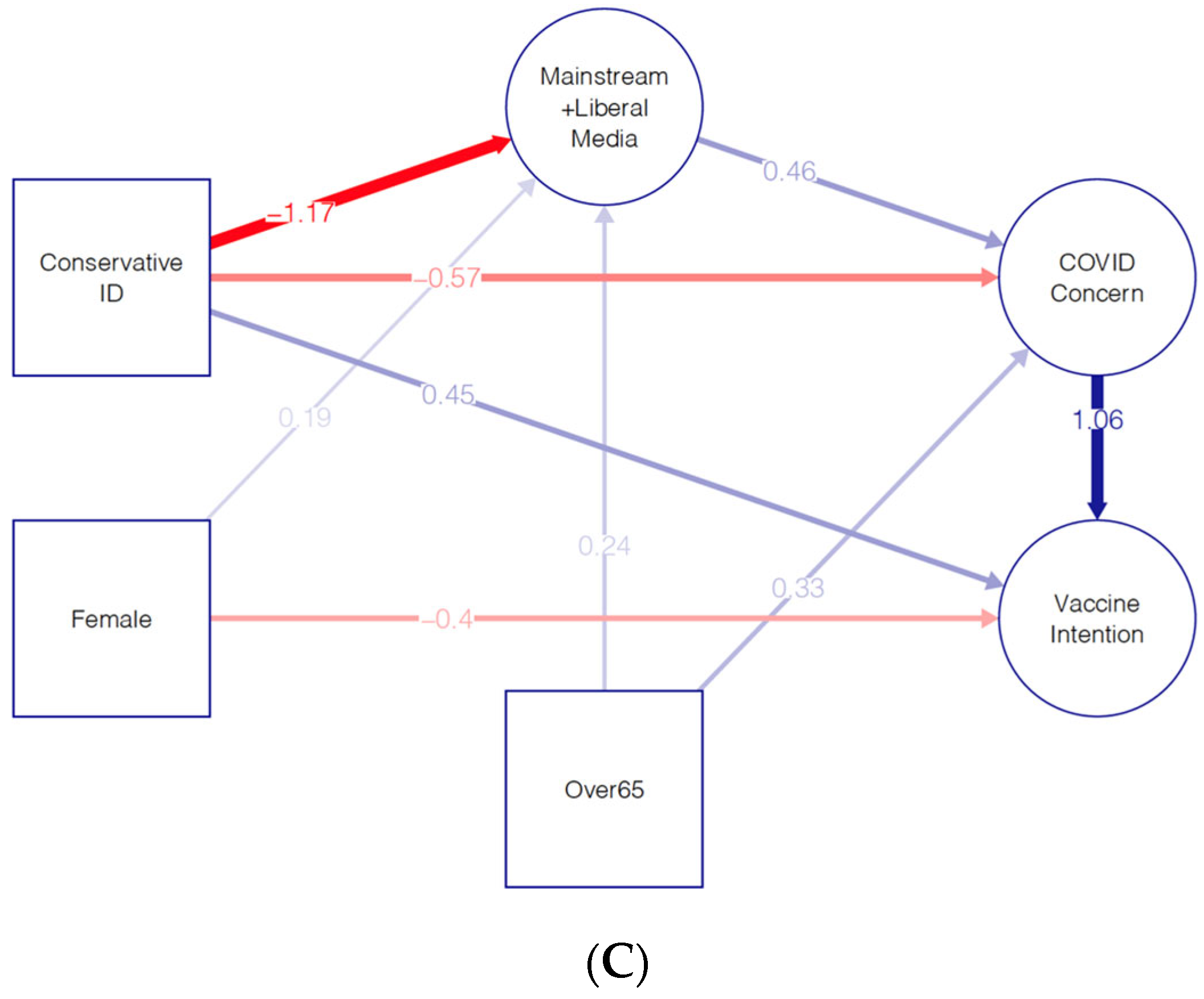
The three path diagrams in
Figure 2 show the significant direct effects of the three tested SEM models. In all three models, we see that COVID-19 concern is the primary driver of vaccine intention, with those more concerned about the impact of the disease showing more interest in receiving the vaccine once it became available. While all of the political identities were significant predictors for the latent variables, as shown in the
Supplementary Tables (S6, S8, S9), the strongest effect was uniformly associated with conservative ideology, so this is the political identity that is depicted in the three diagrams.
Figure 2A shows that respondents who identify as conservative showed a strong preference for conservative media and were less concerned about COVID-19. In fact, the ideology of the respondent was the most significant predictor of COVID-19 concern. Respondents over age 65 showed an increased concern for the effects of COVID-19, consistent with the increased risk for those in this age group. Perhaps surprisingly, consuming conservative media was only marginally significant in lowering COVID-19 concern. This can be explained by the large effect of ideology on COVID-19 concern and the fact that many who do not identify as conservative still consume at least some conservative media. The positive direct effect of conservative identity on vaccine intention shows that conservatives were more likely to indicate that they would receive the vaccine than their concern about the coronavirus disease would imply alone. Similarly, the positive direct effect of conservative media consumption on intention to be vaccinated should be understood as saying that conservatives were more likely to be vaccinated than would be expected given their very low levels of concern about COVID-19. Finally, women expressed more vaccine hesitancy than would be expected from the expressed level of concern about COVID-19.
We note that
Figure 2B,C are very close to being identical, with only a small variation in the sizes of the estimated effects. The primary difference between these and the results in
Figure 2A is that those who identify as conservative express a strong avoidance of liberal and mainstream media sources. We note that this aversion is an even stronger effect than the positive effect of consuming conservative media. As consuming both mainstream and liberal media was associated with an increase in concern about COVID-19, the direct effect of identifying as conservative on reducing COVID-19 concern has a lower estimate for these models. Finally, we see that there is also an effect of gender on media consumption, with women marginally more likely to consume mainstream and liberal media than men.
The overall path effects on vaccine intention are also calculated and shown in the
Supplementary Tables for all three models (S6, S8, S9). For model A, we see that conservative identity has the most significant effect (Std.lv = −0.669,
p < 0.001) on vaccine intention. The next most significant exogenous variable is age, with a significant positive effect (Std.lv= 0.342,
p < 0.001) of being over 65 on vaccine intention. Finally, women were significantly (Std.lv = −0.274,
p < 0.00) less likely to express an intention to receive the vaccine.
Additionally, our results indicate that some demographic variables have significant effects on several of the latent variables considered in models A, B, and C (see regression statistics in
Supplementary Tables, S6, S8, S9). Those who are older (over 65 years of age) express more COVID-19 concern in all models (pA < 0.001, pB < 0.001, pC < 0.001) compared to their younger counterparts. Furthermore, COVID-19 concern had a significant positive effect on vaccination intention in all models (pA < 0.001, pB < 0.001, pC < 0.001). Notably, COVID-19 knowledge did not appear to be a significant predictor of vaccination intention. Women expressed lower vaccination intention than men in models A and C (pA < 0.001, pC < 0.001). Rurality and race did not emerge as significant variables in any of the models considered. The most significant sociodemographic factor in our models is political ideology. Compared to respondents identifying as politically moderate, self-identified liberals and conservatives expressed less peer influence in all three models (pA, pB, pC < 0.001 for all). Conservatives, libertarians, and those who are politically non-aligned all expressed less COVID-19 concern compared to moderates; yet, those who identified as politically liberal expressed more concern (pA, pB, pC < 0.001 for all). Political ideology is also significantly associated with vaccination intention in all of our models.
Overall, it appears that conservative political ideology is the most significant and robust predictor of latent variables across the three models. Effects of demographic variables, in combination with our SEM results for the best-fit model, suggest that political ideology and media sources were primarily responsible for driving vaccination intention in the early phase of the COVID-19 pandemic through their combined effects on COVID-19 concern. This was particularly true for those who were leaning politically conservative and relied on conservative media as their primary source of information regarding the pandemic.
5. Discussion
Vaccine hesitancy is not a new phenomenon in the United States. In fact, when one of the founding fathers, Benjamin Franklin, lost the youngest of his two sons to smallpox, Franklin penned: “In 1736, I lost one of my sons, a fine boy of four years old, by the small-pox, taken in the common way. I long regretted bitterly, and still regret that I had not given it to him by inoculation. This I mention for the sake of parents who omit that operation, on the supposition that they should never forgive themselves if the child died under it: my example showing that the regret may be the same either way, and that, therefore, the safer should be chosen” [
32]. And yet, concerns about vaccine safety and efficacy have prevailed.
A well-known contemporary example is the infamous 1998 paper by Andrew Wakefield which generated widespread concern about a potential link between MMR vaccines and autism. Though researchers have widely debunked this study, concerns remain and continue to affect parents’ vaccination decisions [
33]. To make matters worse, in recent decades, some thought leaders (e.g., politicians, the business community, religious leaders) have taken public positions that are at odds with the scientific consensus on a range of topics, from climate change and evolution to biomedical research and vaccines [
11]. For COVID-19, the early stages of vaccine deployment were ripe for such attitude polarization, both due to the sustaining politicization of vaccines as well as the relative unfamiliarity of the new mRNA vaccines. While mRNA technology and mRNA vaccines were based on well-established science, contrarians continued to question the technology, even going as far as to advocate for alternatives, such as ivermectin. In this context, and lacking first-hand knowledge about the safety and efficacy of COVID-19 vaccines, most people turned to their trusted information sources.
Overall, while our results show that COVID-19 concern was the primary driver of vaccination intention, political ideology and media consumption patterns were the main factors that shaped people’s concern. Ideology and media habits were much more important in affecting concern for those who leaned politically conservative, as opposed to those who leaned liberal or remained politically moderate. In sum, it appears from the SEM models that the information politically conservative respondents were receiving reinforced the effects of their ideology, leading to a greater reduction in their COVID-19 concern. Overall path effects affirm this, demonstrating that conservative political ideology has the single most significant effect on vaccine intention.
Our results suggest that, in the early phase of the pandemic, amidst the ensuing social upheavals, people who were politically conservative have largely congregated in a conservative “echo chamber”, In particular, results suggest that politically motivated selective exposure to partisan information was especially severe for those who identified as politically conservative, which led to large decreases in their COVID-19 concern. That a “conservative echo chamber” existed, and that it affected attitudes and behavior around COVID-19 in the early stages of the pandemic in the US, is further affirmed by our model comparison, which shows strong avoidance of mainstream and liberal media by those who identified as politically conservative. As noted above, this aversion to non-ideologically aligned media was even stronger than the affinity to ideologically aligned media for conservatives. While we cannot further disentangle specific mechanisms from our analysis, it is possible that conservatives embed themselves in echo chambers not only as an outcome of algorithmic exposure to selective information but also due to active avoidance of information that they disagree with, driven by psychological processes, such as confirmation bias and identity protective cognition [
34].
Looking back at the period of 2020 to 2023, and in the ensuing politicization and polarization of the pandemic response, we are not surprised to uncover that political ideology was the most significant predictor of COVID-19 concern or to find that ideology had the strongest effect on vaccine intention. The new insight gleaned from these results is how quickly this effect had taken place in the US. Keeping in mind the timing of our survey, these results indicate that partisan polarization was already well entrenched by the time vaccines were rolled out across the country. Ideologically motivated individuals had embedded themselves in information ecosystems of like-minded others, bonded through their shared lack of concern and hesitancy/refusal to vaccinate themselves. These attitudes were likely aggravated through powerful messaging from trusted leaders, such as former President Donald Trump, who did not publicly encourage Americans to take the vaccine while in office [
35]. In fact, when Trump attempted to tout the success of his vaccine development program, he received backlash from his supporters. The message of vaccine efficacy was not welcome in that echo chamber [
36]. In the end, individual decisions had variable, real-life consequences on the health and safety of the public where, according to one study conducted in Florida and Ohio between March 2020 and December 2021, the excess mortality rate for Republicans was 43% higher than the excess mortality rate for Democrats [
27].
In addition to political ideology (and its connection to media), age and gender emerged as two other significant exogenous variables in our path analysis models. Age (over 65) increased vaccination intention, and women were less likely to express their intention to vaccinate than men. As the pandemic unfolded, there was less ambiguity and disagreement regarding age as a COVID-19 risk factor. Many people experienced this through firsthand exposure to severe illness and/or loss of older friends and family members, but also via media reporting regarding disproportionate impacts on unique populations, such as nursing home residents. These trends have since been affirmed by research that shows that age operated as an independent risk factor for COVID-19 mortality [
37]. The gender difference in the intention to get vaccinated against COVID-19 is not unique to our study. In a meta-analysis of 46 studies conducted between November 2020 and January 2021, Zintel et al. [
38] found that 58% of studies report women’s lower intention to get vaccinated. However, they argue, that the actual vaccination rates for women were much higher, creating an intention–behavior gap, which these researchers explain as a result of rising infections, increased mortality, positive experience of vaccination by those who received it, and some effective vaccination campaigns. It is also plausible that the initial high efficacy of the vaccine persuaded many women who were making decisions for themselves and their families.
An important implication from our research for future pandemic preparedness is recognizing the significance of political ideology in shaping concern, which drives prophylactic behavior. Given ideological motivations that drive information access, future vaccination campaigns should consider the framing of the message as well as who is leveraged as messengers. When it comes to controversial, health-related topics, people are more likely to listen to others who they see as sharing similar values and concerns. In this vein, pro-vaccine conservative political and religious leaders may be better advocates for vaccination campaigns than technical experts (e.g., CDC, WHO, scientists) who are often viewed with skepticism by those who occupy the US political right [
11]. On topics where people are ideologically motivated to dismiss information, it is also important that communication is clear, concise, unambiguous, and consistent. With COVID-19, this became especially challenging due to the dynamic nature of the epidemic itself, the variable messaging about face masks, the introduction of a new type of vaccines (m-RNA vaccines), the complexities in schedules, availability, and access, the changing scientific knowledge regarding the extent of protection offered by vaccines, questions on whether or not vaccines prevent long-COVID, lack of comprehensive knowledge on vaccine side effects, etc. While we cannot do much to forecast and reduce all complexities—new infectious diseases will take hold and new pandemics will ravage populations in the future, in yet unknown ways—we now know to anticipate that complexities related to human dynamics will most likely arise and will likely have disproportionately large impacts on fractions of the American public ideologically motivated to distrust scientific expertise. As far as vaccine messaging is concerned, these dynamics make it even more pertinent that scholars and health communicators pay attention to frames that rise above political divisions and connect us via shared concerns regarding our local communities and/or the tendency to protect the vulnerable. Where hearts and minds cannot be changed through public health campaigns, it may be necessary to use policies such as vaccine mandates.
While our research generated valuable insights on social, psychological, and contextual factors that shaped vaccination attitudes during the early stages of the pandemic, this research is not without limitations. First, in spite of concerted efforts to increase coverage and reduce response biases (e.g., reminder postcards and mail), we received a low response rate and a non-representative sample. Our final sample turned out to be highly educated (61% of the sample had a bachelor’s degree or higher level of education), skewed towards older respondents (55% of the sample was aged over 55 years), and overwhelmingly white (83.5%). Second, in spite of efforts to increase the number of rural respondents (e.g., a stratified sampling strategy targeting equal proportions of rural and non-rural samples), the overall percentage of rural respondents was lower than intended at 36%. Furthermore, our survey covers only three US states, is cross-sectional, and cannot account for any changes in attitudes over time or be generalized to other US states. These challenges expose some common limitations of survey research (e.g., funding, resources, time) exacerbated by the challenges of conducting social science research in an ensuing pandemic scenario. In spite of our best efforts, it is plausible that social vulnerabilities exacerbated by the unequal effects of the pandemic made it even less likely for already marginalized communities (lower educated, economically marginalized, and rural for instance) to respond to calls for research participation. Yet, we see attitude polarization and hesitancy among a sample of respondents skewed towards the older and the more educated—people who we expect to be more open to vaccines—indicating that the phenomena uncovered here are important considerations for future pandemic preparedness and prevention.
Future research should consider oversampling economically marginalized, socially vulnerable, lower educated, and rural populations in order to conduct meaningful subgroup analyses. Retrospective analysis of media content, media framing, misinformation, and disinformation would also provide valuable insights into strategic communication for pandemic prevention. Other factors that have subsequently emerged as important predictors of COVID-19 behavioral responses include factors such as the presence of children and the pregnancy status of women [
39]. While polarization of the pandemic was a significant predictor of attitudinal and behavioral response in the United States [
5], international comparative analysis points towards other cultural, social, psychological, and contextual factors. For instance, the International Collaboration on the Social and Moral Psychology of COVID-19 (ICSMP COVID-19) project, examining survey data from 69 countries, identifies several social, psychological, and cognitive factors that predict COVID-19 responses. In their analysis, internalized moral identity (i.e., a measure of participants’ concern about right and wrong done towards those they care about) emerged as the most consistent predictor, while individual characteristics related to information processing and self-control were also identified as important determinants. Notably, this multi-national analysis reaffirms that cultural context and stage of the pandemic are critical considerations when determining predictive contributions of various psychosocial and contextual factors [
40]. For example, collaborators of ICSMP COVID-19 from Bulgaria who examined psychological predictors of COVID-19 policy support at the beginning of the pandemic found that people’s likelihood of following physical distancing guidelines were predicted by fewer conspiracy theory beliefs, open-mindedness, higher levels of self-control, moral identity, risk perception, and psychological well-being [
41]. The authors argue that these findings must be understood in the context of Bulgaria at the time of data collection, which occurred in April-May 2020, prior to the first wave of illness in Bulgaria. This period overlapped with the first long-term lockdown in Bulgaria where people were facing the stress and anxiety of potential job loss and economic collapse [
41]. Similar retrospective and cross-cultural analyses at different stages of the pandemic would shed light on the determinants of COVID-19 public responses, including factors that shaped vaccine intention and intake.