Mortality of Laryngeal Cancer before and during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Database Search
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parker, D.A.; Robin, P.E. Investigation of laryngeal pathology: A review of diagnostic techniques. Clin. Otolaryngol. Allied Sci. 1989, 14, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Adriaansen, A.; Van Lierde, K.; Meerschman, I.; Claeys, S.; D’haeseleer, E. The Occurrence of Laryngeal Pathologies in a Treatment-Seeking Pediatric Population. J. Voice 2023. [Google Scholar] [CrossRef] [PubMed]
- Koroulakis, A.; Agarwal, M. Laryngeal Cancer. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK526076/ (accessed on 9 May 2024).
- Itamura, K.; Hsue, V.B.; Barbu, A.M.; Chen, M.M. Diagnostic Assessment (Imaging) and Staging of Laryngeal Cancer. Otolaryngol. Clin. N. Am. 2023, 56, 215–231. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Wekking, D.; Senevirathne, T.H.; Pearce, J.L.; Aiello, M.; Scartozzi, M.; Lambertini, M.; De Silva, P.; Solinas, C. The impact of COVID-19 on cancer patients. Cytokine Growth Factor. Rev. 2024, 75, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Allahqoli, L.; Mazidimoradi, A.; Salehiniya, H.; Alkatout, I. Impact of COVID-19 on cancer screening: A global perspective. Curr. Opin. Support. Palliat. Care 2022, 16, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.D.; Cabrera, C.I.; Fowler, N.M.; Li, S.; Thuener, J.E.; Lavertu, P.; Teknos, T.N.; Rezaee, R.P.; Tamaki, A. Incidence and medical complications of COVID-19 in the total laryngectomy population: A population-based study. Oral. Oncol. 2023, 139, 106353. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention; National Center for Health Statistics. National Vital Statistics System, Mortality 2018–2022 on CDC WONDER Online Database, Released in 2024. Data are from the Multiple Cause of Death Files, 2018–2022, as Compiled from Data Provided by the 57 Vital Statistics Jurisdictions through the Vital Statistics Cooperative Program. Available online: http://wonder.cdc.gov/ucd-icd10-expanded.html (accessed on 4 May 2024).
- Nocini, R.; Molteni, G.; Mattiuzzi, C.; Lippi, G. Updates on larynx cancer epidemiology. Chin. J. Cancer Res. 2020, 32, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Igissin, N.; Zatonskikh, V.; Telmanova, Z.; Tulebaev, R.; Moore, M. Laryngeal Cancer: Epidemiology, Etiology, and Prevention: A Narrative Review. Iran. J. Public Health 2023, 52, 2248–2259. [Google Scholar] [CrossRef] [PubMed]
- Richards, M.; Anderson, M.; Carter, P.; Ebert, B.L.; Mossialos, E. The impact of the COVID-19 pandemic on cancer care. Nat. Cancer 2020, 1, 565–567. [Google Scholar] [CrossRef] [PubMed]
- Heer, E.; Ruan, Y.; Boyne, D.J.; Jarada, T.N.; Heng, D.; Henning, J.-W.; Morris, D.M.; O’sullivan, D.E.; Cheung, W.Y.; Brenner, D.R. Impact of the COVID-19 pandemic on cancer diagnoses, stage and survival in Alberta. CMAJ 2023, 195, E804–E812. [Google Scholar] [CrossRef] [PubMed]
- Pennisi, F.; Odelli, S.; Borlini, S.; Morani, F.; Signorelli, C.; Renzi, C. Impact of the COVID pandemic on timely cancer diagnosis across European healthcare settings: A scoping review. Ann. Ig. 2024, 36, 194–214. [Google Scholar] [CrossRef] [PubMed]
- Mattiuzzi, C.; Lippi, G. Timeline analysis of clinical severity of COVID-19 in the general population. Eur. J. Intern. Med. 2023, 110, 97–98. [Google Scholar] [CrossRef] [PubMed]
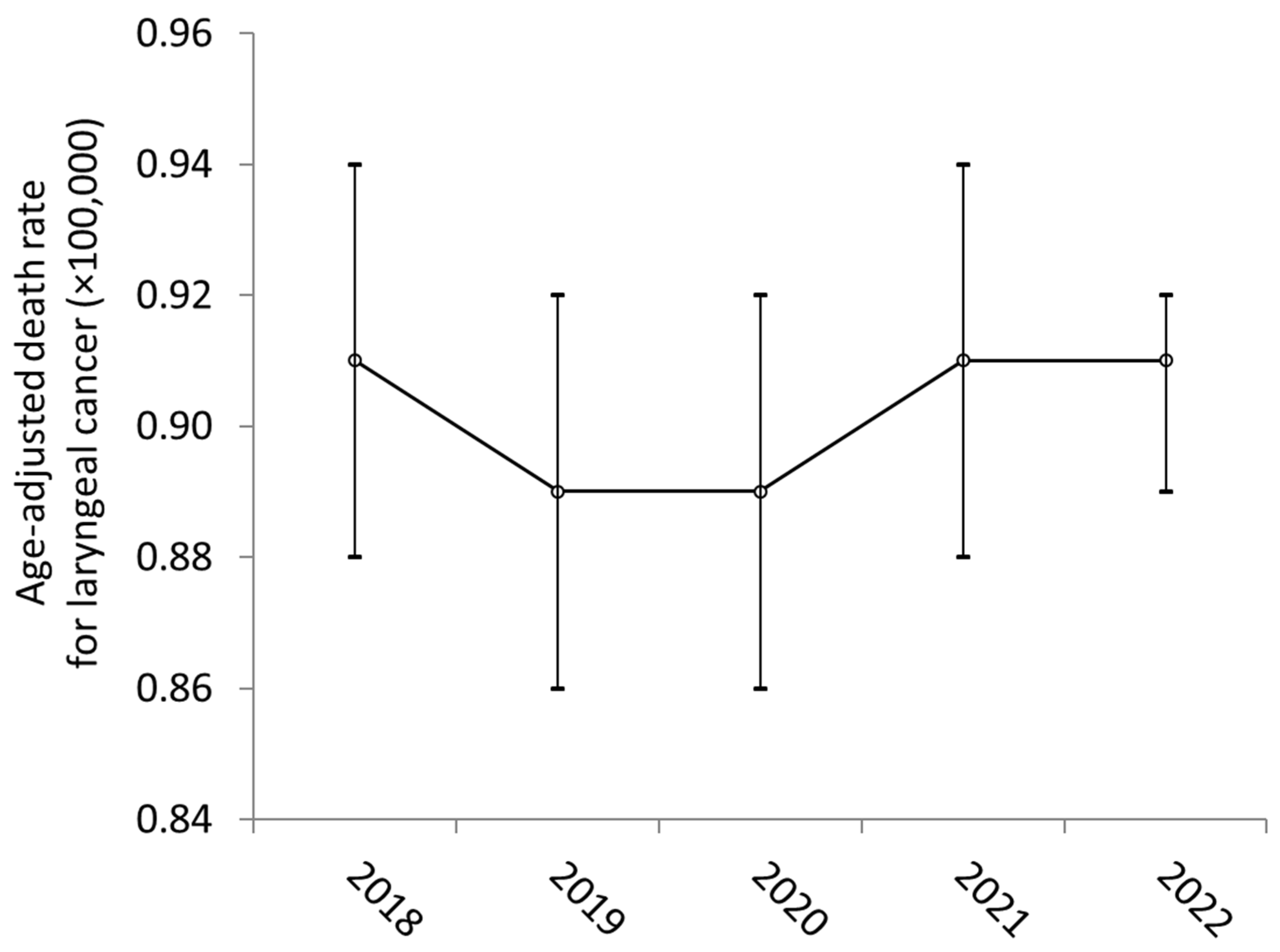
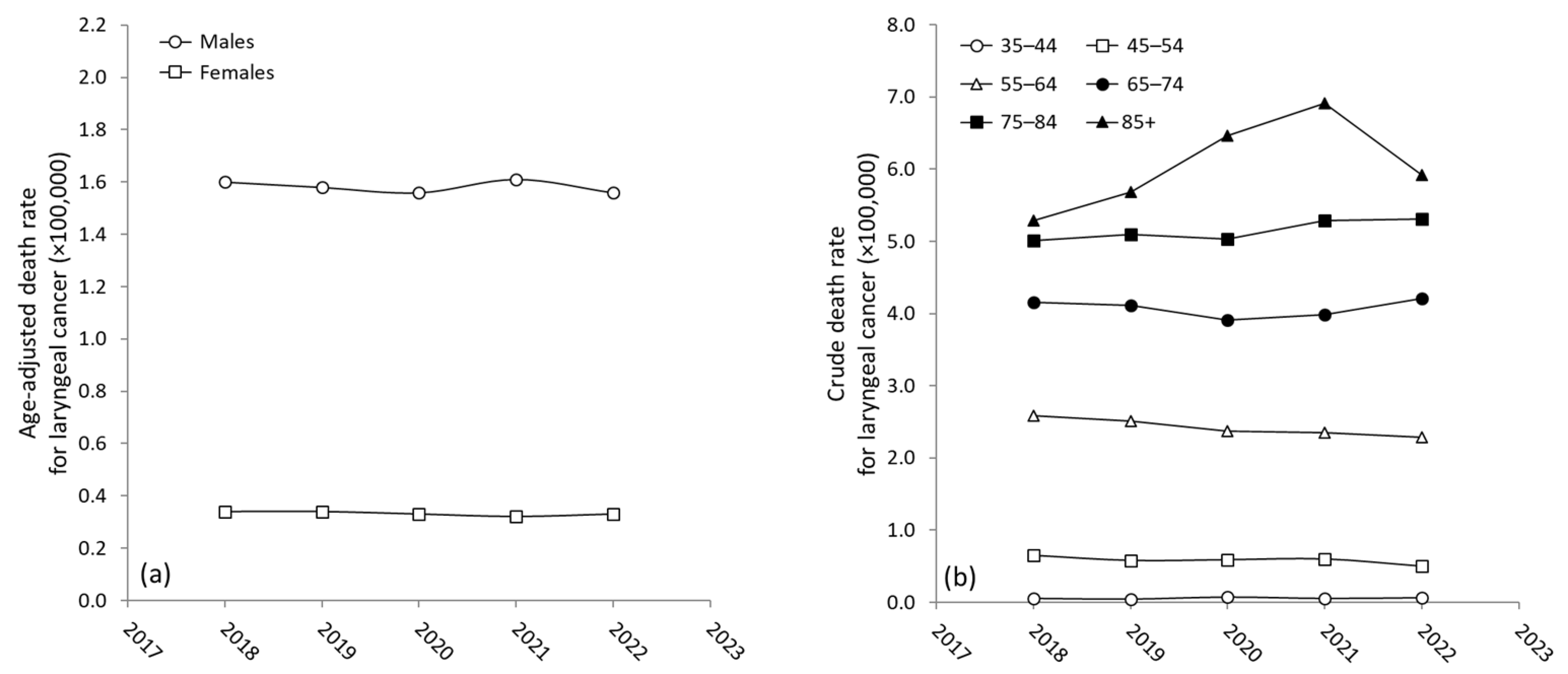
| Years | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|
| Overall | 0.91 (0.84–0.94) | 0.89 (0.86–0.92) | 0.89 (0.86–0.92) | 0.91 (0.88–0.94) | 0.91 (0.89–0.92) |
| Gender | |||||
| - Males | 1.60 (1.54–1.66) | 1.58 (1.64–1.52) | 1.56 (1.62–1.51) | 1.61 (1.67–1.55) | 1.56 (1.61–1.50) |
| - Females | 0.34 (0.31–0.36) | 0.34 (0.31–0.36) | 0.33 (0.31–0.35) | 0.32 (0.34–0.30) | 0.33 (0.31–0.35) |
| - Ratio (M/F) | 4.7 | 4.6 | 4.7 | 5.0 | 4.7 |
| Age (years) | |||||
| - 35–44 | 0.05 (0.03–0.08) | 0.04 (0.02–0.06) | 0.07 (0.04–0.10) | 0.05 (0.03–0.08) | 0.06 (0.04–0.08) |
| - 45–54 | 0.65 (0.57–0.73) | 0.58 (0.51–0.66) | 0.59 (0.52–0.67) | 0.60 (0.53–0.68) | 0.50 (0.43–0.57) |
| - 55–64 | 2.58 (2.43–2.74) | 2.51 (2.36–2.66) | 2.37 (2.22–2.52) | 2.35 (2.20–2.49) | 2.29 (2.15–2.44) |
| - 65–74 | 4.15 (3.92–4.38) | 4.11 (3.89–4.33) | 3.91 (3.69–4.12) | 3.98 (3.77–4.19) | 4.21 (3.99–4.43) |
| - 75–84 | 5.01 (4.66–5.37) | 5.10 (4.75–5.45) | 5.03 (4.68–5.37) | 5.29 (4.94–5.65) | 5.31 (4.97–5.66) |
| - ≥85 | 5.39 (4.83–5.96) | 5.68 (5.10–6.25) | 6.46 (5.85–7.07) | 6.91 (6.24–7.58) | 5.92 (5.33–6.51) |
| f-Value | p-Value | |
|---|---|---|
| All age classes | 0.76 | 0.553 |
| 35–44 years | 1.24 | 0.300 |
| 45–54 years | 1.72 | 0.142 |
| 55–64 years | 2.63 | 0.052 |
| 65–74 years | 1.23 | 0.269 |
| 75–84 years | 0.668 | 0.614 |
| ≥85 years | 3.90 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nocini, R.; Lippi, G.; Mattiuzzi, C. Mortality of Laryngeal Cancer before and during the COVID-19 Pandemic. COVID 2024, 4, 652-657. https://doi.org/10.3390/covid4050044
Nocini R, Lippi G, Mattiuzzi C. Mortality of Laryngeal Cancer before and during the COVID-19 Pandemic. COVID. 2024; 4(5):652-657. https://doi.org/10.3390/covid4050044
Chicago/Turabian StyleNocini, Riccardo, Giuseppe Lippi, and Camilla Mattiuzzi. 2024. "Mortality of Laryngeal Cancer before and during the COVID-19 Pandemic" COVID 4, no. 5: 652-657. https://doi.org/10.3390/covid4050044
APA StyleNocini, R., Lippi, G., & Mattiuzzi, C. (2024). Mortality of Laryngeal Cancer before and during the COVID-19 Pandemic. COVID, 4(5), 652-657. https://doi.org/10.3390/covid4050044








