Abstract
We provide policy lessons for governments across Latin America by drawing on an original dataset of daily national and subnational non-pharmaceutical interventions (NPIs) during the COVID-19 pandemic for eight Latin American countries: Argentina, Bolivia, Brazil, Chile, Colombia, Ecuador, Mexico, and Peru. Our analysis offers lessons for health system decision-making at various levels of government and highlights the impact of subnational policy implementation for responding to health crises. However, subnational responses cannot replace coordinated national policy; governments should emphasize the vertical integration of evidence-based policy from national to local levels while tailoring local policies to local conditions as they evolve. Horizontal policy integration across sectors and jurisdictions will also improve coordination at each level of government. The Latin American experiences with policy and politics during the COVID-19 pandemic project glocal health policy recommendations that connect global considerations with local needs.
1. Introduction
This article draws policy lessons from Latin America via an analysis of non-pharmaceutical interventions (NPIs) through the first two years of the COVID-19 pandemic [,,,,]. We constructed a large, unique dataset of daily national and subnational NPIs for eight Latin American countries: Argentina, Bolivia, Brazil, Chile, Colombia, Ecuador, Mexico, and Peru. These NPIs, such as stay-at-home orders or restrictions on the size of gatherings, travel, and mask use, were some of the main policy responses to the pandemic in countries with limited or slow vaccine rollout.
Our analysis of NPI implementation, adoption, and sustainability can inform health system decision-making at multiple levels of government. We describe individual countries’ experiences and then provide a regional policy perspective for Latin America that can aid the global understanding of the pandemic.
Our results showcase the importance of national leadership and coordination across the health system with the vertical integration of evidence-based policy in funding, designing, coordinating, implementing, and evaluating programs from national to local levels while tailoring local policies to local conditions as they evolve. We also highlight the importance of social welfare policies to mitigate the pandemic’s impact on vulnerable populations []. Next, we show how the absence of leadership can undermine public health policy and exacerbate fragmented public health responses. Finally, we situate our lessons from Latin America in a global context. The result is a set of GLOCAL health policy recommendations stemming from our analysis of policy and politics in Latin America at the national and sub-national levels during the COVID-19 pandemic. The Latin American experiences with policy and politics during the COVID-19 pandemic generate “glocal” health policy recommendations that connect global considerations with local needs.
2. Literature Review
A large strain of literature now highlights the importance of NPIs such as social distancing, mask-wearing, and lockdowns in curbing the transmission of COVID-19 in Latin America [,,,,,,,,]. For example, early scholarship emphasized the crucial role of early and strict lockdown measures in reducing the spread of the virus in several Latin American countries, including Argentina, Brazil, Chile, and Mexico [,,,,]. Additionally, parallel research demonstrated that mask-wearing mandates and public awareness campaigns in Mexico and Panama significantly contributed to the decline in COVID-19 cases [,]. While NPIs were effective in slowing the virus’s spread, challenges such as limited healthcare infrastructure and economic vulnerabilities posed unique hurdles in the Latin American context, making it vital for policymakers to strike a balance between health and socio-economic considerations.
Furthermore, the implementation and enforcement of NPIs varied widely across Latin American countries, leading to heterogeneous outcomes. For instance, these included early and coordinated governmental responses in countries such as Uruguay and Costa Rica, which led to successful pandemic control compared to that of nations with delayed responses []. In contrast, countries facing political and social unrest, such as Venezuela, struggled to enforce NPIs effectively, resulting in higher case burdens. Additionally, research demonstrates the necessity of culturally sensitive and community-driven interventions in indigenous populations, such as those in Bolivia, Brazil, Ecuador, and Peru [].
By the end of March 2020, many countries had implemented at least some national restrictions, yet the rigor and types of NPI waxed and waned over the entire pandemic period and continue to do so []. In Brazil and Mexico, accounting for 55% of the region’s population, federal governments delegated or “punted” NPI responsibility to state governments, leading to large-scale variation within each country with no central, evidence-based planning []. In other countries, national leaders relaxed policies at the sub-national level to balance health imperatives, economic outcomes, and limited compliance due to lockdown fatigue. Countries in the region struggled to gather adequate evidence to guide their subnational policymaking. Only Uruguay—now also a country with very high per capita deaths—and Chile focused on access to testing. However, access to diagnostic tests was often scarce and unequally distributed between rich and poor []. This produced a patchwork of NPIs within and across countries, sometimes reactively yet seldom proactively responding to the geographic variation in risk based on evidence given the limited testing and contact tracing.
Few studies have analyzed subnational variation in the use of NPIs in the COVID-19 response, even though variation exists in all countries, and almost no data are available for low- and middle-income countries (LMICs) [,]. Our analysis is based on a unique dataset that records the daily adoption of NPIs at the state or departmental level for Argentina, Bolivia, Brazil, Chile, Colombia, Ecuador, Mexico, and Peru since the first case in each country. These data come from the Observatory for the Containment of COVID-19 in the Americas (the Observatory), which provides data on the adoption of public policies at the national and subnational levels in Latin America []. We selected these NPIs by reviewing the literature in early 2020 on public policy choices that might influence COVID-19 cases and deaths [,,,,,,,,].
3. Materials and Methods
We collected data on NPIs related to physical distancing and the containment of COVID-19 for national and subnational territories in Argentina, Bolivia, Brazil, Chile, Colombia, Ecuador, Mexico, and Peru, beginning with each country’s first case. We focus on the national and mid-levels of government, such as the province, state, or department. Our data begin on 25 February 2020, and end in December 2021, covering roughly the first two years of the pandemic in the region.
Our data cover school closures, work suspensions, public event cancellations, public transportation suspensions, information campaigns, intra-state travel restrictions, international travel restrictions, stay-at-home mandates, restrictions on gatherings, and mask mandates.
We summarize our coding here and describe it more thoroughly in the appendix as well as in other publications [,,,,]. We first created country-teams with local research assistants to review government websites, official documents, and news reports of NPI implementation. These teams then assessed whether or not each NPI had been implemented each day, beginning with each country’s first case. We then coded the NPIs as partially or fully implemented to measure policy rigor with an internal review of inter-coder reliability. In Appendix A Table A1, we present the 10 policy variables and their values [].
We analyzed our NPI data individually as well as when combined into an aggregate policy index. Our previous research covers the comparative analysis of the timing and rigor of policy implementation [,,,,]. In turn, this paper focuses on a reanalysis of that data from a policy perspective. We accomplish this by synthesizing the results from earlier research and emphasizing their policy implications. The online appendix contains a detailed discussion of the measure’s construction [].
4. Results
The following section describes the results of the analysis of the NPI combination, timing, and rigor for each country as well as the policy lessons stemming from each. Exhibit 1 presents each country’s NPI policy index scores at the national level over the course of the 300 days since the first reported case in each country.
4.1. Argentina
Argentina implemented a relatively stringent early response to the COVID-19 pandemic, primarily driven by localized lockdowns. Instead of independent and sometimes contradictory subnational policies, Argentina’s national government set a high policy standard for NPIs, and subnational government compliance was generally high, though with more variation in Argentina than in Bolivia, Chile, Ecuador, or Peru. These lockdowns varied significantly at the subnational level from very strict in Buenos Aires, to more relaxed in less densely populated areas. Argentina maintained strict NPIs during the re-opening phase of the pandemic, which continued from the ending phase of the world’s longest lockdown in late 2020 into 2021 [].
One of the most important policy lessons from Argentina’s COVID-19 experience is the need for strong public health infrastructure and coordination across different levels of government. The pandemic exposed weaknesses in Argentina’s health system, including inadequate investment in public health and primary care services []. The government responded by increasing funding for healthcare and expanding its public health workforce, which was immediately necessary to combat the pandemic, but was not always forthcoming across Latin America [].
A second lesson from Argentina is the importance of data-driven decision-making and transparency in communicating with the public. The government’s decision to provide daily updates on COVID-19 cases and deaths helped to build public trust and facilitate compliance with public health measures []. Finally, the pandemic underscored the need for social protection programs to support vulnerable populations during times of crisis. The government’s emergency income support program, known as Ingreso Familiar de Emergencia (IFE), is credited with reducing poverty and inequality during the pandemic [].
4.2. Bolivia
Bolivia’s COVID-19 response offers lessons on health system performance and subnational NPI implementation as well as support for informal workers without social protection []. Similar to Argentina, Bolivia’s national government implemented stringent nation-wide NPIs to combat COVID-19. Bolivia acted early, only trailing Colombia in NPI implementation in response to the WHO’s recommendations. Bolivia also stands out as having one of the strictest overall responses to the first stage of the COVID-19 pandemic, along with Peru and Ecuador.
The Bolivian government faced increasing political and economic pressure to relax its NPIs and hold repeatedly delayed elections. After ending a national quarantine, daily deaths from COVID-19 rose dramatically from June 2020 as quarantines ended [,]. Bolivia’s government relaxed its policies significantly on 1 September 2020, when national policies that had prohibited most travel relaxed, and containment policies became even more varied sub-nationally.
The government created intergovernmental commissions to coordinate the pandemic response at different levels of government [,]. Coordinating across governments using the authority of an unpopular, unelected government was a serious challenge, as we might expect. Governments, at minimum, must be perceived as legitimate to elicit cooperation from subnational units. An additional lesson is the importance of investing in healthcare infrastructure and strengthening primary healthcare services. The pandemic exposed longstanding weaknesses in Bolivia’s healthcare system, including inadequate funding and an inadequate provision of primary healthcare services []. The government responded by increasing healthcare funding and expanding primary healthcare services [].
Finally, the pandemic highlighted the need for social protection programs to support vulnerable populations during crises, particularly in a country where 80% of workers have informal employment. Bolivia’s national government increased benefits for its cash transfer programs in March 2020 and expanded the programs to reach new, previously unprotected workers []. These expansions were logistically difficult during the crisis, but the Bono Familia program reduced poverty and inequality during the pandemic []. Nevertheless, pervasive poverty, inequity and precarious work are all structural and comprise part of a syndemic []. Meeting these challenges requires a comprehensive syndemic approach to implement NPIs and deliver employment-based financial benefits.
4.3. Brazil
Brazil’s COVID-19 cases and deaths were consistently the highest in Latin America in absolute terms and represent the second highest toll globally; per capita COVID-19 deaths were third in the region, behind Peru and Argentina []. One of the causes of this public health crisis was the country’s populist leadership and resulting governance failures. Like other populist presidents in the region, Jair Bolsonaro denied the pandemic’s severity and mounted only a limited campaign to combat the disease. Bolsonaro cycled through three Health Ministers since the pandemic began. He fired the first minister on 17 April 2020, for promoting and defending subnational governments’ “stay-at-home” orders. The replacement minister resigned after only one month when Bolsonaro ordered gymnasiums to reopen. Finally, the third and current Health Minister during the first year of the COVID-19 pandemic was a general from the army, with no prior public health experience. On 6 June 2020, Bolsonaro ordered the Ministry of Health to stop releasing data on COVID-19 cases and deaths, which also highlights Bolsonaro’s disdain for the free press and evidence-based policies.
The Bolsonaro Administration’s actions left subnational governments in states and municipalities to take the lead in delivering COVID-19-related services and generally protect their populations from the virus. Many subnational governments in Brazil engaged in this, but with limited authority and resources relative to those of the national government. The result was a confusing patchwork of public health messaging and partial NPI implementation [,,].
Brazil, along with Mexico, exhibited the least stringent early responses to the pandemic, with considerable variation across both country’s states []. Brazil implemented the least stringent NPIs among the countries examined in this paper; Brazil was the last country to implement lockdowns and many other NPIs, which were quite limited compared to NPIs in other countries. Brazil was the first country in our dataset to relax its limited NPIs and re-open, followed by Mexico [,].
The COVID-19 pandemic showcases the need for coordinated, consistent public health policies and effective governance in Brazil. One lesson learned is the importance of early and decisive action in controlling the spread of the virus. Brazilian states that implemented strict social distancing measures earlier had lower mortality rates compared to those of states that implemented them later []. Additionally, the pandemic exposed the need for Brazil to invest more in its public healthcare system. The World Health Organization (WHO) found that Brazil’s healthcare system was underfunded and lacked the necessary resources to respond to the pandemic adequately []. Moving forward, policymakers in Brazil should prioritize investing in public health infrastructure and implementing evidence-based policies to prevent future outbreaks. The country should also empower subnational governments to take the lead to safeguard the public in the face of national government inaction.
4.4. Chile
Chile’s response to the pandemic featured localized lockdowns and a quick, centralized response effort at the national level with little subnational variation in other NPIs []. Following the first major COVID-19 transmission wave (May–June 2020), the government implemented a five-tiered strategy that adapted NPIs (e.g., localized lockdowns, school closures, and limited gatherings) to local epidemiological conditions, health system capacity, and contact tracing, beginning on 19 July 2020 []. As a result, NPIs were more stringent for many of Chile’s sub-national regions during its reopening phase than early in the pandemic.
The COVID-19 pandemic in Chile shows the importance of public health policies, effective governance, and adaptation to local conditions. In contrast to uncoordinated responses in larger, more populous federal countries, such as in Brazil and Mexico, Chile’s early response to the pandemic, which included aggressive testing, contact tracing measures, and early mass vaccination, contributed to a lower mortality rate compared to that of other countries in the region after the first year of the pandemic [].
The Chilean experience also highlights the importance of ensuring an equitable allocation of resources. The Ministry of Health took administrative control of all hospital beds in the public and private sector and diverted resources to significantly expand the health system’s capacity, for example by bringing new beds, ventilators, and quarantine hotels into service. The centralized prioritization of resources for the pandemic response led to a temporary deferral of elective surgeries and non-urgent care, and a major increase in testing capabilities.
A final lesson is the need for robust social welfare policies to support vulnerable populations affected by the pandemic. Chile’s social welfare policies, such as cash transfers and food assistance, were effective in mitigating the pandemic’s economic impact when implemented [].
4.5. Colombia
Colombia had a stringent early response to the COVID-19 pandemic with significant subnational variation. Colombia was the first to act of all countries in our analysis, enacting school closures, severe stay-at-home measures, workplace closures and travel bans on 22 March 2020, even before the WHO recommended a pandemic response. Colombia began reopening in September 2020 with a significant relaxation of NPIs, which was after Brazil and Mexico but before the other countries in the analysis [].
COVID-19 policy lessons from Colombia mirror those of some of the other countries discussed above. Colombia’s timely and coordinated actions in terms of NPIs likely prevented the spread of the virus relative to that in other countries in the region. Colombia’s early response and strict measures were key to strengthening the health system, particularly in areas without intensive care units. However, no robust testing and tracing system was put in place. These aspects likely contributed to a lower mortality rate compared to that of other countries in the region during the first months of the pandemic. However, Colombia experienced one of the worst COVID-19 peaks in the region, and the mortality rate over the course of the pandemic was in the middle range of the countries analyzed here []. As described for Chile and Bolivia, social welfare policies, such as emergency cash transfers to four million households, were important for many in the country affected by the pandemic [].
4.6. Ecuador
Ecuador’s national government established a stringent set of COVID-19 restrictions. Subnational governments typically complied with these restrictions, but Ecuador delayed somewhat in implementing these stringent NPIs relative to Peru, Bolivia, and Chile. Ecuador re-opened earlier than did Peru and Bolivia by several months as well, relaxing its NPIs by August 2020, with subnational policies becoming more heterogeneous [].
Ecuador’s experience with the COVID-19 pandemic offers several policy lessons. Like Bolivia and Peru, Ecuador demonstrates a need to promote effective health governance along with social welfare policies. Timing is also of the essence, as Ecuador’s somewhat delayed response to the pandemic may have contributed to a higher mortality rate compared to that of other countries in the region []. Like in other highly unequal Latin American countries, supporting vulnerable populations through social welfare policies is paramount. Similar to those of other countries in the analysis, Ecuador’s social welfare programs, such as cash transfers and food assistance, also helped vulnerable populations whose livelihoods were impacted during the pandemic [].
4.7. Mexico
Mexico’s total COVID-19 cases and deaths are second only to those of Brazil in Latin America. The large populations in both countries led to proportional expectations for a high total of cases and deaths. However, Mexico’s national policy response to the COVID-19 pandemic was slow and limited, like that in Brazil, which likely exacerbated the pandemic’s impact. Mexico and Brazil were the last to enter the lockdown phase, and their lockdowns were brief and limited compared to those of other countries. Mexico was the second of the eight countries to reopen, following Brazil. State and local governments in Mexico also initiated policy responses to fill the void left by the federal government []. However, Mexico’s patchwork of policy responses allowed the virus to spread rapidly throughout the country.
The timing of Mexico’s pandemic response was especially challenging because it occurred during a transition from Seguro Popular, which had dramatically expanded insurance coverage prior to 2018, to a new, untested system []. The Mexican government’s replacement was implemented chaotically just prior to the pandemic, which exacerbated COVID-19′s impact on a population left vulnerable by health disparities and comorbidities. Similar to Brazil’s President Bolsonaro, Mexico’s President Lopez Obrador also consistently denied and downplayed the COVID-19 threat, encouraging the population to continue to maintain daily activities and interactions. Additionally, the Mexican government eliminated basic social support programs, such as a wide-reaching conditional cash transfer program, and replaced it, too, with an untested system that made supporting marginalized populations difficult [].
Mexico’s policy lessons showcase the need for coordination across federal entities, the need for health system stewardship, and the inadvisability of large-scale health system reforms during a pandemic. Instead of retaining a proven system, the government chose to continue with one of the largest health system shifts in decades, which created delays and confusion in terms of authorities and responsibilities to combat COVID-19 []. The delayed response may have also raised the death toll from the pandemic, as in Brazil []. Finally, Mexico’s experience with the COVID-19 pandemic highlights the need to expand support programs and not eliminate effective support infrastructure on the cusp of the population’s greatest need [].
4.8. Peru
Peru had a stringent overall response to the emergence of COVID-19 and acted early in the pandemic. However, Peru still experienced the highest per capita COVID-19 death toll in the region and in the world. Peru’s national government implemented NPIs that its provinces followed with minimal variation. In comparison to that of other countries in the dataset, Peru’s government opted for a longer wait before reopening, finally doing so in October 2020 [].
Peru’s strategy for easing the COVID-19 lockdown and restarting economic operations was incremental and occurred in four distinct phases. The initial phase, which began in May 2020, focused on resuming activities such as mining, construction, commerce, and tourism-related services such as those of restaurants and hotels. The second phase followed a month later, with agriculture, manufacturing, and professional services resuming. A month after that, retail stores reopened, most lockdowns ended, and domestic travel resumed. By 15 July, lockdowns had been lifted in 18 out of 25 regions, while the remaining 7 regions, primarily in the Highland area, maintained lockdowns due to increasing infection rates. International air travel resumed in October of 2020, while restaurant and retail capacity continued to rise [].
This incremental approach was coupled with maintaining or reinstituting lockdowns in regions experiencing rising infection rates, and schools remained closed until 2021. Despite Peru’s high death toll, several policies, including incremental reopening, lockdown reinforcements in provinces experiencing outbreaks, mask mandates, cash transfers, and vaccination, may have prevented even worse health outcomes and therefore serve as important lessons [].
Figure 1 below presents the policy index in each country since the first reported case in the country as well as the facemask index. Figure 2 shows the subnational variation on these policies for each country in the dataset.
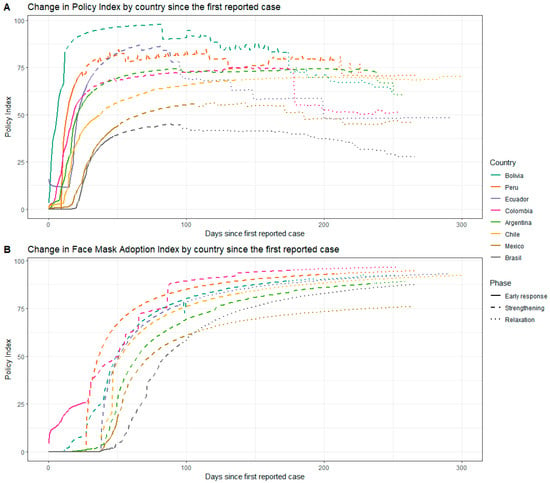
Figure 1.
Change in Policy Index and Facemask Index by country since the first COVID-19 case. These trends are presented separately in (A,B) because the facemask index has unique characteristics relative to the other NPI indices.
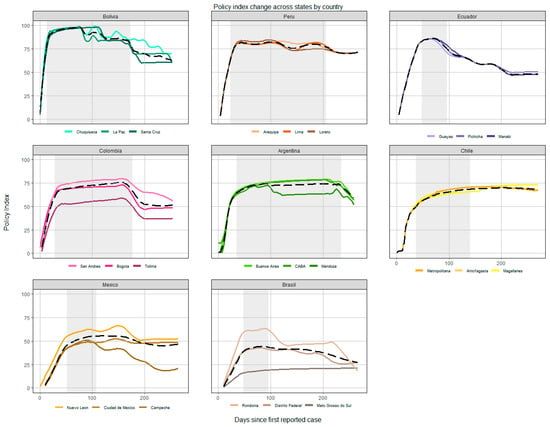
Figure 2.
NPI policy index scores over the first 300 days since a case was reported in each country, but with subnational variation across states, provinces, departments, and regions.
5. Discussion
Several themes emerge from Latin American countries’ experience with COVID-19 and policy efforts to control the spread of the virus. The lessons from these experiences apply to the rest of the world, both for the COVID-19 pandemic as well as future public health crises. First, coordination across the health system with subnational units was essential to controlling and then treating COVID-19 and will be for future pandemics and global emergencies. Collaboration and coordination among healthcare professionals, public health officials, and policymakers aids efforts to deliver health services at all levels, especially in a public health crisis. This includes sharing information, resources, and expertise, as well as implementing consistent measures and guidelines to prevent the spread of the virus. Coordination also enables healthcare systems to better prepare for and respond to future pandemics as well as to natural disasters, an influx of refugees, or other crises that might overwhelm health systems.
Second, balancing the health benefits of large-scale NPIs with the social and economic costs they impose is critical to maintaining the well-being of the population and sustaining them beyond the pandemic. The countries in our dataset experienced tradeoffs between slowing the spread of the disease and supporting livelihoods, especially in lower-income countries; wealthy countries across the globe often provide income support to their populations, but many Latin American countries do not. Countries that bolstered and expanded social welfare programs cushioned the economic impact of lockdowns and other NPIs on vulnerable populations. In contrast, countries that did not expand cash transfers or other financial support programs allowed unnecessary economic suffering that exacerbated other health problems during the pandemic and beyond, particularly in countries with strict, lengthy lockdowns.
The need to act with expediency is another important lesson that emerges from Latin America. Many governments quickly implemented NPIs to respond to early COVID-19 cases. Most countries in this analysis implemented a wide array of stringent national and international travel restrictions, had closed schools, and locked down populations. However, Brazil and Mexico implemented NPIs slowly and in a frequently decentralized fashion [,,]. Brazil and Mexico’s NPIs for COVID-19 are sub-nationally heterogeneous, more so in Brazil, and reflect an uncoordinated national response. Additionally, even rapid, strict responses may be counterproductive. For example, lockdowns serve only to delay disease transmission when they are not coupled with extensive testing and contract tracing upon reopening, as well as increased health system capacity to treat patients. Moreover, lockdowns delay the treatment of other diseases and as discussed earlier, impose economic costs that can easily undermine the health of vulnerable groups.
Finally, Latin America’s experience with the COVID-19 pandemic demonstrates the perils of populist leadership and ensuing poor governance and/or poor stewardship of the health system. Lacking a cohesive or evidence-based national policy, populist leaders in the region understated the risk of the virus and relied on or defaulted to state governments to design, organize, and implement NPIs. These actions confused and endangered the population and limited governments’ capacity to respond to the pandemic, despite previously capable, effective health systems [,,,,].
6. Conclusions
Implementing widespread NPIs imposed large costs on countries. Simultaneously, many countries failed to prevent COVID-19 transmission without these NPIs. In Latin America, there are clear tradeoffs between ensuring citizens’ income and controlling COVID-19 transmission; high-income countries have financing and systems in place to do both, but most LMICs do not. Our data are unique and allow us to draw different policy lessons by comparing subnational NPIs during each day of the COVID-19 pandemic. Most Latin American countries implemented NPIs rapidly to contain the spread of COVID-19 at the beginning of the pandemic, but we show that the Latin American NPIs implemented to combat COVID-19 demonstrate critical subnational and national variation. It is clear from the analysis above that subnational governments’ COVID-19 responses, however stringent they may be, cannot compensate for limited national policies.
It is also important to discuss the limitations of this research. First and foremost, this is a descriptive analysis with inferences drawn from non-causal data trends. Descriptive studies are important, especially in the absence of covariates to allow for more comprehensive causal modeling. Nevertheless, our policy lessons should be taken with the caveat that they are not based on causal logic, but rather descriptions of NPIs and broad associations between NPIs and health outcomes. Second, we produced a unique dataset of NPI, but enforcement and compliance fall beyond the scope of this paper and of our data collection. Compliance with COVID-19 restrictions is important for achieving positive health outcomes, however, and has been fraught with numerous challenges in Latin America. One of the foremost obstacles to compliance has been the economic disparities and informal labor sectors common in many countries across the region. Millions of Latin America’s residents rely on daily wages, making it exceedingly difficult for them to adhere to lockdowns and stay-at-home orders without an economic safety net to fall back on. Additionally, the lack of robust healthcare infrastructure and unequal access to healthcare services exacerbated the crisis. Moreover, misinformation and mistrust in government institutions hindered compliance efforts, as some segments of the population were reluctant to follow health guidelines or get vaccinated. The region’s vast geographic and cultural diversity also posed challenges for uniform enforcement of restrictions, with rural and indigenous communities often facing unique obstacles. These multifaceted challenges made it arduous for Latin American nations to effectively contain the spread of the virus and protect public health. As stated above, we do not have data on policy compliance and leave this topic for future researchers to address. Finally, our data are coded as a partial implementation of policy when policies exist but are targeted toward a specific group. For example, stay-at-home orders are partial when only the elderly must remain at home; school closures are partial when only younger children are kept home. In retrospect, evidence on NPIs and health outcomes suggests that these targeted NPIs may have been more effective, efficient, and appropriate from a socioeconomic perspective than the blunt NPIs that were stringently enforced in some cases. Protecting the elderly while reopening the economy may have been a better policy than lengthy lockdowns for all []. Nevertheless, some partial NPIs, such as closing schools for young children, carried good intentions, but were ineffective from a health standpoint and counterproductive from a socioeconomic standpoint. Hence, it is a limitation of our research that we do not distinguish between positive and negative targeted NPIs and could not do so at the original time of data collection and coding.
Future research should disaggregate data and address NPIs, compliance, and health outcomes at the most granular level possible. In some countries, causal, municipal-level exploration of relationships between NPIs and health outcomes may become possible. Equipped with these analyses, scholars and practitioners can better target recommendations for national and subnational policymaking. Future research should also address the issue of targeted NPIs that carry much lower economic costs and higher health benefits for the target population. This strategy was not immediately open to policymakers without knowledge of the effects of a novel virus. However, the scientific evidence quickly suggested the possibility of targeted approaches, which most governments ignored for more than a year in many cases. Understanding why and how health policies that were designed to be responsive to scientific evidence were not responsive in practice is also an important step toward better performance during the next global pandemic. The result would be an evidence base that could be vertically integrated across government units, from the municipal to the state to the national level in a way that is responsive to local conditions and that is coordinated at all levels of government.
Author Contributions
Conceptualization, F.M.K., M.M.T. and H.A.-O.; methodology, H.A.-O., R.C.-A., C.H. and O.M.-C.; validation, J.I., S.O.-B., F.P., P.J.G., C.B., V.X.V.G., J.N.-N. and P.P.-C.; investigation, H.A.-O., R.C.-A., T.P., C.H., O.M.-C., J.I., S.O.-B., F.P., P.J.G., C.B., V.X.V.G., J.N.-N. and P.P.-C.; writing—original draft preparation, M.M.T.; writing—review and editing, F.M.K., H.A.-O., R.C.-A., C.H., O.M.-C., J.I., S.O.-B., F.P., P.J.G., C.B., V.X.V.G., J.N.-N. and P.P.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Institute for Advanced Study of the Americas, University of Miami, grant number 2020-009. The APC was funded by the Institute for Advanced Study of the Americas, University of Miami.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting reported results can be found on the Harvard Dataverse: https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/NFSXTR (accessed on 15 August 2023).
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Appendix A.1. Learning from Latin America: Coordinating Policy Responses across National and Subnational Levels to Combat COVID-19
Appendix A.1.1. Description of NPI Variables
The variables “school closings”, “suspension of work”, “cancellation of public events”, “suspension of public transport and/or closure of public transport systems” are categorical and take values of 0 when not implemented, 0.5 when partially implemented, and 1 when fully implemented. The variable “development of information campaigns” records whether or not governments implemented campaigns to inform the public about the virus, the disease, its consequences, and containment measures. It takes a value of 0 for no campaigns, 0.5 for only a federal campaign, and 1 for a subnational government campaign. The variable “travel restrictions within the state” registers the implementation of internal movement restrictions in the state or department, such as bans on interstate and intercity travel. It takes values of 0 when there are no restrictions; 0.5 when restriction of movement is recommended; and 1 when the state restricts all movement.
The variable “international travel control” records international movement restrictions, taking a value of 0 when no action was taken; 0.33 when only screening and/or monitoring was applied to international travelers; 0.66 when mandatory quarantines were required for travelers in high-risk regions; and 1 when the state implemented a travel ban to and from high-risk regions. States without a seaport, international airport, or border received the value of the national mean for this variable to not penalize them for their lack of entry points.
The “stay-at-home order” measures requirements to shelter in place or confine oneself to the home and takes a value of 0 when no order was issued; 0.33 when the state-level recommendation was not to leave the house; 0.66 when the instruction was not to leave home except in “essential” cases; and 1 when the lockdown was fully enforced and required not leaving the home, with minimal exceptions.
The variable “restrictions on the size of gatherings” refers to the cut-off size on the prohibitions of private gatherings, taking a value of 0 in the absence of any gathering size restriction; 0.25 when events of more than 1000 people were prohibited; 0.5 when events of more than 100 people were banned; 0.75 when gatherings were banned consisting above 50 people; and 1 when only gatherings of 10 people or less were permitted.
We also include a variable to describe mask mandates in each state. This variable takes a value of 0 if no mask requirement was in place for people in public places; 0.5 when mask use was recommended or only required in specific locations; and 1 when states implemented a full mask mandate. The World Health Organization (WHO) did not release general guidance about the public’s use of face coverings until 5 June []. However, many countries, and subnational units, began recommending or requiring their use months earlier.

Table A1.
Public policy variables.
Table A1.
Public policy variables.
| Variable Name | Description | Coding |
|---|---|---|
| Stay at Home Orders | Record orders to “shelter-in-place” | 0—No measures 0.33—Recommend not leaving the house 0.66—Partial requirements (specified groups or times) 1—Require not leaving the house with minimal exceptions (e.g., allowed to leave only once a week, or only one person can leave at a time, etc.) |
| School Closure | Closure of in-person classes | 0—No measures 0.5—Recommend closing 1—Require closing all levels |
| Workplace Closure | Workplaces closures, restrict working hours, and/or closure of specific economic activities/sectors | 0—No measures 0.5 Partial (or work from home) for some activities, sectors or categories of workers, and times 1—Require closing |
| Public Event Cancellations | Prohibition of events, social, cultural, or religious activities and sports | 0—No measures 0.5—Recommend canceling 1—Require canceling |
| Restrictions on gatherings | Restrictions on crowds of people | 0—No restrictions 0.33—Restrict very large gatherings (limit is above 1000) 0.66—Restrict gatherings between 11 and 100 people 1—Restrict gatherings of 10 people or less. |
| Public transit suspensions | Traffic restrictions, schedules, types, or routes of travel in each state/department | 0—No measures 0.33—Recommended closing 0.66—Significantly reduce volume/route/means of transport available 1—Require closing (or prohibit most citizens from using it) |
| Information campaigns | Measures to disseminate information on health, contagions, prevention measures, tests, and laws | 0—No COVID-19 public information campaign 0.5—Public officials urge caution about COVID-19 1—Coordinated public information campaign (e.g., across traditional and social media) |
| Mask mandates | Use of masks and face coverings | 0—No measure 0.33—Recommended 0.66—Partial and mandatory 1—Total/mandatory implementation |
| Internal travel controls | Traffic restrictions, schedules, types, or routes of travel within each state/department | 0—No measures 0.33—Recommend not to travel between regions/cities 0.66—Relax moving restrictions 1—Internal moving restrictions in place |
| International travel ban | Movement restrictions on international travel including air, land, water | 0—No measure 0.33—Quarantine arrivals from high-risk regions 0.66—Ban on arrivals from some regions 1—Ban on all regions or total border closure |
Appendix A.1.2. Public Policy Adoption Index
The Public Policy Adoption Index is constructed as presented in the Equation (A1) below:
where by:
IPPit = Public policy adoption index in country/state i in time t
Ij = Public Policy Index j, where j changes from 1 to n = 9.
Dt = Days from the first registered case until time t.
Dt = Days from the implementation of policy j until time t.
The index sums up the values of 9 of the 10 variables weighted by the day each policy was implemented in relation to the appearance of the first case []. The ratio is continuous and goes from 0, when policy j has not yet been implemented in state i at time t, up to 1, in instances where public policy has been implemented at the same time t in which the first case appears. The PPAI is different than Oxford’s Stringency Index in the way it treats the timeliness of policy adoption. The approach considers that public containment policies have diminishing power to contain the virus the later they are adopted. To this end, we raise the ratio to the power of 0.5, to reflect decreasing policy efficacy with delays in policy implementation. For more detail, please review the online appendix.
In the aggregate, each state, i, receives a daily score between 0 and 10, which reflects the sum of the different policy dimensions and is then normalized to 100. The maximum value of the index is 100 but obtaining a score of 100 would not be realistic or desirable since it would imply a total closure of the state the day after the first case in the country.
Our Public Policy Adoption (PPA) Index measure sums up daily scores for each policy variable. The index takes time since implementation into account by multiplying the sum of policy scores by a ratio of the days since implementation to the days since a country’s first case.
For each country and policy implementation phase, we first estimate the mean PPA score by weighting PPA by the population of each state, province, or department. Then, we document and describe subnational heterogeneity in the stringency of NPIs and compare the country responses against each other. We consider variation in NPI policies using PPA to measure the timeliness and intensity of implementing a standard set of policies.
We analyze mask mandates separately because the use of face masks resulted in different outcomes from those of the other measures. Mask recommendations or requirements tended to be a reopening feature and were not designed to restrict movement. Instead, they modulated distancing and facilitated closer, safer contacts among the population. They were often implemented much later than were the other indicators we have collected based on the WHO’s release of general guidance about the use of face coverings by the public on 5 June 2020 [].
References
- Knaul, F.M.; Touchton, M.; Arreola-Ornelas, H.; Atun, R.; Anyosa, R.J.C.; Frenk, J.; Martínez-Valle, A.; McDonald, T.; Porteny, T.; Sánchez-Talanquer, M.; et al. Punt Politics as Failure of Health System Stewardship: Evidence from the COVID-19 Pandemic Response in Brazil and Mexico. Lancet Reg. Health Am. 2021, 4, 100086. [Google Scholar] [CrossRef]
- Hummel, C.; Knaul, F.M.; Touchton, M.; Guachalla, V.X.V.; Nelson-Nuñez, J.; Boulding, C. Poverty, precarious work, and the COVID-19 pandemic: Lessons from Bolivia. Lancet Glob. Health 2021, 9, e579–e581. [Google Scholar] [CrossRef] [PubMed]
- Touchton, M.; Knaul, F.M.; Arreola-Ornelas, H.; Porteny, T.; Sánchez, M.; Méndez, O.; Faganello, M.; Edelson, V.; Gygi, B.; Hummel, C.; et al. A partisan pandemic: State government public health policies to combat COVID-19 in Brazil. BMJ Glob. Health 2021, 6, e005223. [Google Scholar] [CrossRef] [PubMed]
- Knaul, F.; Arreola-Ornelas, H.; Porteny, T.; Touchton, M.; Sánchez-Talanquer, M.; Méndez, O.; Chertorivski, S.; Ortega, S.; Chudnovsky, M.; Kuri, P.; et al. Not far enough: Public health policies to combat COVID-19 in Mexico’s states. PLoS ONE 2021, 16, e0251722. [Google Scholar] [CrossRef]
- Knaul, F.M.; Touchton, M.M.; Arreola-Ornelas, H.; Calderon-Anyosa, R.; Otero-Bahamón, S.; Hummel, C.; Pérez-Cruz, P.; Porteny, T.; Patino, F.; Atun, R.; et al. Strengthening Health Systems to Face Pandemics: Subnational Policy Responses To COVID-19 In Latin America: Study examines policy responses to COVID-19 in Latin America. Health Aff. 2022, 41, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Blofield, M.; Giambruno, C.; Filguiera, F. Policy Expansion in Compressed Time: Assessing the Speed, Breadth and Sufficiency of Post-COVID-19 Social Protection Measures in 10 Latin American Countries; CEPAL: Santiago, Chile, 2020. [Google Scholar]
- Stanford, V.; Gresh, L.; Toledo, J.; Méndez, J.; Aldighieri, S.; Reveiz, L. Evidence in decision-making in the context of COVID-19 in Latin America. Lancet Reg. Health Am. 2022, 14, 100322. [Google Scholar] [CrossRef]
- Fernández-Marín, H.; Bruner-Montero, G.; Portugal-Loayza, A.; Miranda, V.; Villarreal Dominguez, A.E.; Ortega-Barría, E.; Kosagisharaf, J.R. Dynamics of mask use as a prevention strategy against SARS-CoV-2 in Panama. Int. J. Environ. Res. Public Health 2021, 18, 12982. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Gallego, V.; Escalera-Antezana, J.P.; Méndez, C.A.; Zambrano, L.I.; Franco-Paredes, C.; Suárez, J.A.; Rodriguez-Enciso, H.D.; Balbin-Ramon, G.J.; Savio-Larriera, E.; et al. COVID-19 in Latin America: The implications of the first confirmed case in Brazil. Travel Med. Infect. Dis. 2020, 35, 101613. [Google Scholar] [CrossRef]
- Machado, F.C.G.; Ferron, M.M.; Barddal, M.T.d.M.; Nascimento, L.A.; Rosalen, J.; Avelino-Silva, V.I. COVID-19 vaccination, incidence, and mortality rates among indigenous populations compared to the general population in Brazil: Describing trends over time. Lancet Reg. Health Am. 2022, 13, 100319. [Google Scholar] [CrossRef]
- Garcia, P.J.; Alarcón, A.; Bayer, A.; Buss, P.; Guerra, G.; Ribeiro, H.; Rojas, K.; Saenz, R.; de Snyder, N.S.; Solimano, G.; et al. COVID-19 Response in Latin America. Am. J. Trop. Med. Hyg. 2020, 103, 1765–1772. [Google Scholar] [CrossRef]
- Burki, T. COVID-19 in Latin America. Lancet Infect. Dis. 2020, 20, 547. [Google Scholar] [CrossRef]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021, 372, eabg5298. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Observatory [Internet]. University of Miami. 2021. Available online: http://observcovid.miami.edu/ (accessed on 15 September 2021).
- Vardavas, R.; de Lima, P.N.; Baker, L. Modeling COVID-19 Nonpharmaceutical Interventions: Exploring periodic NPI Strategies. MedRxiv 2021, 3, 439–463. [Google Scholar] [CrossRef]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef] [PubMed]
- Haushofer, J.; Metcalf, C.J.E. Which interventions work best in a pandemic? Science 2020, 368, 1063–1065. [Google Scholar] [CrossRef]
- Rowan, N.J.; Moral, R.A. Disposable face masks and reusable face coverings as non-pharmaceutical interventions (NPIs) to prevent transmission of SARS-CoV-2 variants that cause coronavirus disease (COVID-19): Role of new sustainable NPI design innovations and predictive mathematical modelling. Sci. Total Environ. 2021, 772, 145530. [Google Scholar] [PubMed]
- McCoy, L.G.; Smith, J.; Anchuri, K.; Berry, I.; Pineda, J.; Harish, V.; Lam, A.T.; Yi, S.E.; Hu, S.; Rosella, L.; et al. Characterizing early Canadian federal, provincial, territorial and municipal nonpharmaceutical interventions in response to COVID-19: A descriptive analysis. CMAJ Open 2020, 8, E545–E553. [Google Scholar] [CrossRef]
- Davies, N.G.; Kucharski, A.J.; Eggo, R.M.; Gimma, A.; Edmunds, W.J.; Jombart, T.; O’Reilly, K.; Endo, A.; Hellewell, J.; Nightingale, E.S.; et al. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: A modelling study. Lancet Public Health 2020, 5, e375–e385. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S. Variation in Government Responses to COVID-19 Version 10.0. Blavatnik School of Government Working Paper. Available online: https://www.bsg.ox.ac.uk/sites/default/files/2020-12/BSG-WP-2020-032-v10.pdf (accessed on 15 September 2020).
- Walker, P.G.T.; Whittaker, C.; Watson, O.J.; Baguelin, M.; Winskill, P.; Hamlet, A.; Djafaara, B.A.; Cucunubá, Z.; Mesa, D.O.; Green, W.; et al. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science 2020, 369, 413–422. [Google Scholar] [CrossRef]
- Li, Y.; Undurraga, E.A.; Zubizarreta, J.R. Effectiveness of Localized Lockdowns in the COVID-19 Pandemic. Am. J. Epidemiol. 2022, 191, 812–824. [Google Scholar] [CrossRef]
- Gemelli, N.A. Management of COVID-19 Outbreak in Argentina: The Beginning. Disaster Med. Public Health Prep. 2020, 14, 815–817. [Google Scholar] [CrossRef]
- Kaplan, L.J.; Delfino, A. Pandemia, políticas públicas y sectores vulnerables: Un análisis del Ingreso Familiar de Emergencia en Argentina. Política. Rev. De Cienc. Política 2021, 59, 81–104. [Google Scholar] [CrossRef]
- Saletti-Cuesta, L.; Berra, S.; Tumas, N.; Johnson, C.; Carbonetti, A. Argentina COVID-19 Snapshot Monitoring (COSMO Argentina): Monitoring Knowledge, Risk Perceptions, Preventive Behaviours, and Public Trust in the Current Coro-Navirus Outbreak in Argentina; Government of Argentina: Buenos, Argentina, 2020.
- Institute for Health Metrics and Evaluation. COVID-19 Projections: Daily Deaths, Bolivia. 19 November 2020. Available online: https://covid19.healthdata.org/bolivia-(plurinational-state-of)?view=total-deaths&tab=trend (accessed on 29 November 2020).
- Gobierno del Estado Plurinacional de Bolivia. Ministerio de Salud y Deportes. 2020. Available online: https://www.minsalud.gob.bo/ (accessed on 25 November 2020).
- Birbuet, J.C.; López, R. Dinámica de Expansión del COVID-19 en Bolivia Durante las Primeras 6 Semanas; Documento de trabajo, Fundacion Avina: La Paz, Bolivia, 2020. [Google Scholar]
- Velasco-Guachalla, V.X.; Hummel, C.; Nelson-Nuñez, J.; Boulding, C. Legitimacy and policy during crises: Subna-tional Covid-19 responses in Bolivia. Perspect. Politics 2022, 20, 528–546. [Google Scholar] [CrossRef]
- Blofield, M.; Filgueira, F. COVID-19 and Latin America: Social Impact, Policies and a Fiscal Case for an Emergency Social Protection Floor. 5 April 2020. Available online: https://www.cippec.org/wp-content/uploads/2020/04/Blofield-Filgueira-2020-1.pdf (accessed on 29 November 2020).
- Romero, C.A.; Romero, F.D.M. Política Social y Reactivación Económica Ante el COVID-19: Bolivia y su Apuesta por los Bonos; Government of Bolivia: La Paz, Bolivia, 2021.
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef] [PubMed]
- Pires de Oliveira, M.; Barcellos, C.; Ferreira, J. Social distancing measures in the Brazilian context: What was the contribution of healthcare capacity in reducing mortality? J. Am. Med. Assoc. 2021, 4, e214054. [Google Scholar]
- World Health Organization. WHO Mission Report: COVID-19 Preparedness and Response in Brazil. 2020. Available online: https://www.who.int/publications/m/item/who-mission-report-covid-19-preparedness-and-response-in-brazil (accessed on 29 November 2020).
- West, R.; Michie, S.; Rubin, G.J.; Amlot, R. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat. Hum. Behav. 2020, 4, 451–459. [Google Scholar] [CrossRef]
- Borquez, A.; Atalaya, R.; Romero, M.; Gomez, D.; Cerna, F. Early response to COVID-19 in Chile: Key lessons and unresolved questions. Lancet Reg. Health Am. 2021, 1, 100017. [Google Scholar]
- Inter-American Development Bank. Social Welfare Policies in Chile’s Response to the COVID-19 Crisis. 2020. Available online: https://publications.iadb.org/publications/english/document/Social-Welfare-Policies-in-Chiles-Response-to-the-COVID-19-Crisis.pdf (accessed on 15 August 2023).
- Sarmiento-Ospina, A.; Barona-Vilar, C.; Mora-García, G.; Rodríguez-Morales, A.J.; Rojas-Vélez, A.F. Colombia’s response to COVID-19: A framework for analysis and lessons to be learned. J. Public Health Policy 2021, 42, 192–206. [Google Scholar]
- World Bank. Colombia—Emergency COVID-19 Response Project. 2021. Available online: https://projects.worldbank.org/en/projects-operations/project-detail/P173738 (accessed on 15 August 2023).
- Villacrés-Granda, I.; García-Almeida, D.; Sandoval-Ramírez, J.; Guamán-Ramón, E. Ecuador’s response to COVID-19: Analysis of national surveillance data. Int. J. Infect. Dis. 2021, 102, 318–324. [Google Scholar] [CrossRef]
- United Nations Development Programme. COVID-19 and Human Development in Ecuador: Assessing the Impacts and Defining Policy Responses. 2020. Available online: https://www.ec.undp.org/content/ecuador/es/home/library/crisis_prevention_and_recovery/COVID-19-and-Human-Development-in-Ecuador.html (accessed on 15 August 2023).
- Knaul, F.M.; Arreola-Ornelas, H.; Touchton, M.; McDonald, T.; Blofield, M.; Burgos, L.A.; Gómez-Dantés, O.; Kuri, P.; Martinez-Valle, A.; Méndez-Carniado, O.; et al. Setbacks in the quest for universal health coverage in Mexico: Polarised politics, policy upheaval, and pandemic disruption. Lancet 2023, 402, 731–746. [Google Scholar] [CrossRef]
- Ruiz-Sánchez, A.; Alavez-Ramírez, J.R.; García-Rodríguez, R.I.; Villagrana-Bañuelos, K.E. COVID-19 pandemic in Mexico: Lessons learned and future directions. J. Glob. Health 2020, 10, 020346. [Google Scholar] [CrossRef]
- World Bank. Mexico—COVID-19 Emergency Cash Transfer Project. 2021. Available online: https://projects.worldbank.org/en/projects-operations/project-detail/P173830 (accessed on 15 August 2023).
- Calderon-Anyosa, R.J.; Bilal, U.; Kaufman, J.S. Focus: Preventive medicine: Variation in non-external and external causes of death in Peru in relation to the COVID-19 lockdown. Yale J. Biol. Med. 2021, 94, 23. [Google Scholar]
- International Labour Organization. Peru–Mitigating the Impact of COVID-19 on Employment and Incomes in Peru: An Assessment of Policy Responses. 2020. Available online: https://www.ilo.org/wcmsp5/groups/public/---americas/---ro-lima/documents/publication/wcms_760696.pdf (accessed on 15 August 2023).
- Daoust, J.F. Elderly people and responses to COVID-19 in 27 Countries. PLoS ONE 2020, 15, e0235590. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).