A Mediation Model of Self-Efficacy and Depression between Burnout and Alcohol Consumption among Health Workers during the COVID-19 Pandemic
Abstract
1. Introduction
1.1. Job Demands and Resources Model
1.2. Alcohol Consumption
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.2.1. Burnout Scale
2.2.2. Depression Scale
2.2.3. Self-Efficacy Index
2.2.4. Alcohol Consumption
2.3. Procedure
2.4. Data Analyses
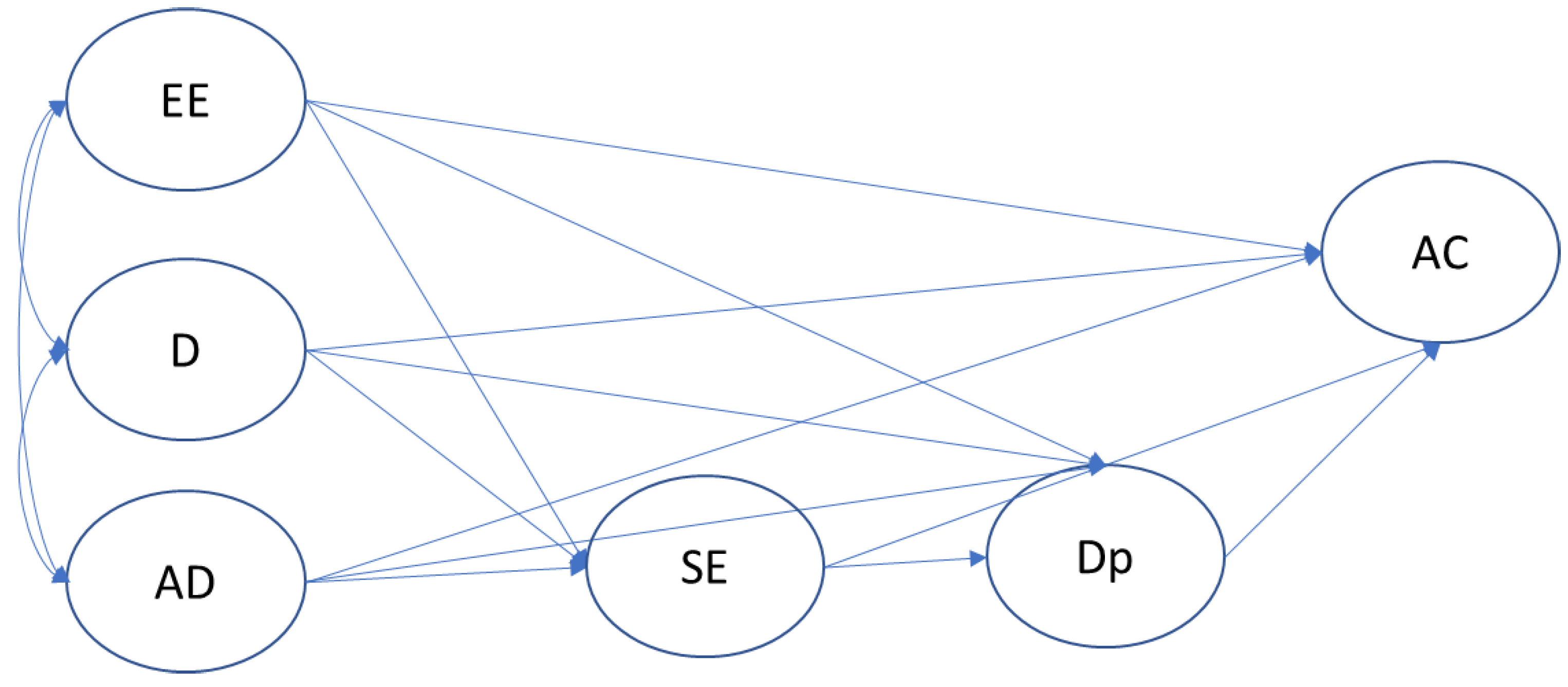
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kniffin, K.M.; Narayanan, J.; Anseel, F.; Antonakis, J.; Ashford, S.P.; Bakker, A.B.; Bamberger, P.; Bapuji, H.; Bhave, D.P.; Choi, V.K.; et al. COVID-19 and the workplace: Implications, issues, and insights for future research and action. Am. Psychol. 2021, 76, 63–77. [Google Scholar] [CrossRef]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Curr. Psychiatry Rep. 2020, 22, 22. [Google Scholar] [CrossRef] [PubMed]
- Sultana, A.; Sharma, R.; Hossain, M.M.; Bhattacharya, S.; Purohit, N. Burnout among healthcare providers during COVID-19: Challenges and evidence-based interventions. Indian J. Med. Ethics 2020, 5, 308–311. [Google Scholar] [CrossRef] [PubMed]
- White, E.M.; Wetle, T.F.; Reddy, A.; Baier, R.R. Front-line nursing home staff experiences during the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Young, K.P.; Kolcz, D.L.; O’Sullivan, D.M.; Ferrand, J.; Fried, J.; Robinson, K. Health care workers’ mental health and quality of life during COVID-19: Results from a mid-pandemic, national survey. Psychiatr. Serv. 2021, 72, 122–128. [Google Scholar] [CrossRef]
- Zerden, L.D.S.; Richman, E.L.; Lombardi, B.; Forte, A.B. Frontline, essential, and invisible: The needs of low-wage workers in hospital settings during COVID-19. Workplace Health Saf. 2022, 70, 509–514. [Google Scholar] [CrossRef]
- Tipa, R.O.; Tudose, C.; Pucarea, V.L. Measuring burnout among psychiatric residents using the Oldenburg Burnout Inventory (OLBI) Instrument. J. Med. Life 2019, 12, 354–360. [Google Scholar] [CrossRef]
- Bakker, A.; Demerouti, E.; Schaufeli, W. Dual processes at work in a call centre: An application of the job demands–resources model. Eur. J. Work. Organ. Psychol. 2003, 12, 393–417. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands-resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E.; Euwema, M.C. Job resources buffer the impact of job demands on burnout. J. Occup. Health Psychol. 2005, 10, 170–180. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job demands–resources theory: Taking stock and looking forward. J. Occup. Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Njim, T.; Mbanga, C.M.; Tindong, M.; Fonkou, S.; Makebe, H.; Toukam, L.; Fondungallah, J.; Fondong, A.; Mulang, I.; Kika, B. Burnout as a correlate of depression among medical students in Cameroon: A cross-sectional study. BMJ Open 2019, 9, e027709. [Google Scholar] [CrossRef]
- Talih, F.; Daher, M.; Daou, D.; Ajaltouni, J. Examining burnout, depression, and attitudes regarding drug use among Lebanese medical students during the 4 years of medical school. Acad. Psychiatry 2018, 42, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Walkiewicz, M.; Tartas, M. Vulnerability of medical students and professionals to extreme work stress: A select review of the literature. Commun. Med. 2017, 14, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Hyman, S.A.; Shotwell, M.S.; Michaels, D.R.; Han, X.; Card, E.B.; Morse, J.L.; Weinger, M.B. A survey evaluating burnout, health status, depression, reported alcohol and substance use, and social support of Anesthesiologists. Anesth. Analg. 2017, 125, 2009–2018. [Google Scholar] [CrossRef]
- Sklar, M.; Ehrhart, M.G.; Aarons, G.A. COVID-related work changes, burnout, and turnover intentions in mental health providers: A moderated mediation analysis. Psychiatr. Rehabil. J. 2021, 44, 219. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122–147. [Google Scholar] [CrossRef]
- Bandura, A. Social Cognitive Theory of self-regulation. Organ. Behav. Hum. Decis. Process. 1991, 50, 248–287. [Google Scholar] [CrossRef]
- Bandura, A. Cultivate self-efficacy for personal and organizational effectiveness. In Handbook of Principles of Organization Behavior; Locke, E.A., Ed.; Blackwell: Oxford, UK, 2000; pp. 120–135. [Google Scholar]
- Abdelsadig Mohammed, H.; Elamin, S.A.; El-Awaisi, A.; El Hajj, M.S. Use of the job demands-resource model to understand community pharmacists’ burnout during the COVID-19 pandemic. Res. Soc. Adm. Pharm. 2022, 18, 3568–3579. [Google Scholar] [CrossRef]
- Albergo, J.I.; Fernández, M.C.; Zaifrani, L.; Giunta, D.H.; Albergo, L. ¿Cómo afecta la privación de sueño durante una guardia de 24 horas las funciones cognitivas de los residentes de ortopedia y traumatología? [How does sleep deprivation during 24 hours on call duty affect the cognitive performance orthopaedic residents?]. Rev. Esp. Cir. Ortop. Traumatol. 2016, 60, 113–118. [Google Scholar] [CrossRef]
- Dewa, C.; Loong, D.; Bonato, S.; Trojanowski, L.; Rea, M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: A systematic literature review. BMC Med. Educ. 2017, 17, 195. [Google Scholar] [CrossRef] [PubMed]
- An, T.W.; Henry, J.K.; Igboechi, O.; Wang, P.; Yerrapragada, A.; Lin, C.A.; Paiement, G.D. How are orthopaedic surgery residencies responding to the COVID-19 pandemic? An assessment of resident experiences in cities of major virus outbreak. J. Am. Acad. Orthop. Surg. 2020, 28, 679–685. [Google Scholar] [CrossRef]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, e113129. [Google Scholar] [CrossRef] [PubMed]
- García-Torres, M.; Aguilar-Castro, J.; García-Méndez, M. Psychological weelbeing and burnout in health care providers during the COVID-19 pandemic [Bienestar psicológico y burnout en personal de salud durante la pandemia de COVID-19]. Escr. Psicol. 2021, 14, 96–106. [Google Scholar] [CrossRef]
- Torres-Muñoz, V. Riesgos y daños en la salud mental del personal sanitario por la atención a pacientes con COVID-19 [Risks and damage to the mental health of health personnel due to the care of patients with COVID-19]. Rev. Mex. Urol. 2020, 80, 1–9. [Google Scholar] [CrossRef]
- Killikelly, C.; Lenferink, L.I.M.; Xie, H.; Maercker, A. Rapid systematic review of psychological symptoms in health care workers COVID-19. J. Loss Trauma 2021, 26, 638–655. [Google Scholar] [CrossRef]
- Robles, R.; Rodríguez, E.; Vega-Ramírez, H.; Álvarez-Icaza, D.; Madrigal, E.; Durand, S.; Astudillo, C.; Becerra, C.; Escamilla, R.; Diaz, D.; et al. Mental health problems among healthcare workers involved with the COVID-19 outbreak. Braz. J. Psychiatry 2020, 43, 494–503. [Google Scholar] [CrossRef]
- Mahase, E. Coronavirus COVID-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ 2020, 368, m641. [Google Scholar] [CrossRef]
- Pan American Health Organization/World Health Organization. Epidemiological Alert: COVID-19 among Healthcare Workers; Pan American Health Organization: Washington, DC, USA, 2020. [Google Scholar]
- Muñoz del Carpio-Toia, A.; Begazo Muñoz del Carpio, L.; Mayta-Tristan, P.; Alarcón-Yaquetto, D.E.; Málaga, G. Workplace violence against physicians treating COVID-19 patients in Peru: A cross-sectional study. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Rzymski, P.; Mamzer, H.; Nowicki, M. The main sources and potential effects of COVID-19-related discrimination. In Coronavirus Disease—COVID-19; Rezaei, N., Ed.; Advances in Experimental Medicine and Biology; Springer: Cham, Swizerland, 2021; Volume 1318, pp. 705–725. [Google Scholar]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Scheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15. [Google Scholar] [CrossRef] [PubMed]
- Freudenberger, H.J. Staff burn-out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Maslach, C. Burned-out. Can. J. Psychiatr. Nurs. 1979, 20, 5–9. [Google Scholar] [PubMed]
- Maslach, C. Burnout: The Cost of Caring; Prentice-Hall: Englewood Cliffs, NJ, USA, 1982. [Google Scholar]
- Leiter, M.; Maslach, C. Latent burnout profiles: A new approach to understanding the burnout experience. Burn. Res. 2016, 3, 89–100. [Google Scholar] [CrossRef]
- Uribe Prado, J.F. La Escala de Desgaste Ocupacional (EDO) y sus propiedades psicométricas con trabajadores en precariedad laboral de la Ciudad de México [The Occupational Burnout Scale (EDO) and its psychometric properties with precarious workers in Mexico City]. Rev. Interam. Psicol. Ocup. 2013, 32, 38–55. [Google Scholar]
- Maslach, C.; Leiter, M. Early predictors of job burnout and engagement. J. Appl. Psychol. 2008, 93, 498–512. [Google Scholar] [CrossRef]
- Drüge, M.; Schladitz, S.; Wirtz, M.A.; Schleider, K. Psychosocial burden and strains of pedagogues-using the Job Demands-Resources Theory to predict burnout, job satisfaction, general state of health, and life satisfaction. Int. J. Environ. Res. Public Health 2021, 18, 7921. [Google Scholar] [CrossRef]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef]
- Rodriguez, R.M.; Medak, A.J.; Baumann, B.M.; Lim, S.; Chinnock, B.; Frazier, R.; Cooper, R.J. Academic emergency medicine physicians' anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID-19 Pandemic. Acad. Emerg. Med. 2020, 27, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Andrade, G.; Menolli, P.; Clemente, P.; Eumann, A.; Silva, D.; Girotto, E. Burnout syndrome and consumption of alcohol and illicit substances in university students. Sch. Educ. Psychol. 2021, 31, e3134. [Google Scholar] [CrossRef]
- Bonini, A.D.; Campos, J.S.; Valéria Salloume Sampaio Bonafé, F.; Velez Oliveira, R.; Maroco, J. Burnout syndrome and alcohol consumption in prison employees. Rev. Bras. Epidemiol. 2016, 19, 205–216. [Google Scholar] [CrossRef]
- Jackson, E.R.; Shanafelt, T.D.; Hasan, O.; Satele, D.V.; Dyrbye, L.N. Burnout and alcohol abuse/dependence among U.S. medical students. Acad. Med. 2016, 91, 1251–1256. [Google Scholar] [CrossRef] [PubMed]
- Ahola, K.; Pulkki-Råback, L.; Kouvonen, A.; Rossi, H.; Aromaa, A.; Lönnqvist, J. Burnout and behavior-related health risk factors: Results from the population-based Finnish Health 2000 study. J. Occup. Environ. Med. 2012, 54, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Olivares-Faúndez, V.E.; Gil-Monte, P.R.; Figueiredo-Ferraz, H. The mediating role of feelings of guilt in the relationship between burnout and the consumption of tobacco and alcohol. Jpn. Psychol. Res. 2014, 56, 340–348. [Google Scholar] [CrossRef]
- Aaker, J.L. Dimensions of Brand Personality. J. Mark. Res. 1997, 34, 347–356. [Google Scholar] [CrossRef]
- Wiesner, M.; Windle, M.; Freeman, A. Work stress, substance use, and depression among young adult workers: An examination of main and moderator effect model. J. Occup. Health Psychol. 2005, 10, 83–96. [Google Scholar] [CrossRef]
- Frone, M.R. Are work stressors related to employee substance use? The importance of temporal context assessments of alcohol and illicit drug use. J. Appl. Psychol. 2008, 93, 199–206. [Google Scholar] [CrossRef]
- Beiter, K.J.; Wiedemann, R.P.; Thomas, C.L.; Conrad, E.J. Alcohol consumption and COVID-19–Related stress among health care workers: The need for continued stress-management mnterventions. Public Health Rep. 2022, 137, 326–335. [Google Scholar] [CrossRef]
- Medina-Mora, M.E.; Cordero-Oropeza, M.; Rafful, C.; Real, T.; Villatoro-Velazquez, J.A. COVID-19 and alcohol in Mexico: A serious health crisis, strong actions on alcohol in response—Commentary on Stockwell et al. Drug Alcohol Rev. 2021, 40, 13–16. [Google Scholar] [CrossRef]
- Raman, B.; Cassar, M.P.; Tunnicliffe, E.M.; Filippini, N.; Griffanti, L.; Alfaro-Almagro, F.; Okell, T.; Sheerin, F.; Xie, C.; Mahmod, M.; et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine 2021, 31, 100683. [Google Scholar] [CrossRef]
- Nesoff, E.D.; Gutkind, S.; Sirota, S.; McKowen, A.L.; Veldhuis, C.B. Mental health and economic stressors associated with high-risk drinking and increased alcohol consumption early in the COVID-19 pandemic in the United States. Prev. Med. 2021, 153, 106854. [Google Scholar] [CrossRef] [PubMed]
- Pocuca, N.; London-Nadeau, K.; Geoffroy, M.-C.; Chadi, N.; Séguin, J.R.; Parent, S.; Boivin, M.; Tremblay, R.E.; Cote, S.M.; Costellanos-Ryan, N. Changes in emerging adults’ alcohol and cannabis use from before to during the COVID-19 pandemic: Evidence from a prospective birth cohort. Psychol. Addict. Behav. 2022, 36, 786–797. [Google Scholar] [CrossRef] [PubMed]
- Shield, K.D.; Chrystoja, B.R.; Ali, S.; Sohi, I.; Rehm, J.; Nigatu, Y.T.; Elton-Marshall, T.; Hamilton, H.; Jankowicz, D.; Wells, S. Changes in alcohol consumption in Canada during the COVID-19 Pandemic: Associations with anxiety and self-perception of depression and loneliness. Alcohol Alcohol. 2021, 57, 190–197. [Google Scholar] [CrossRef]
- Turaev Bobir, T. Patients with alcoholism functional changes in the liver after COVID-19 disease. Peerian J. 2023, 15, 38–47. [Google Scholar]
- Ji, D.; Qin, E.; Xu, J.; Zhang, D.; Cheng, G.; Wang, Y.; Lau, G. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J. Hepatol. 2020, 73, 451–453. [Google Scholar] [CrossRef]
- Xu, L.; Liu, J.; Lu, M.; Yang, D.; Zheng, X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020, 40, 998–1004. [Google Scholar] [CrossRef]
- Singh, A.; Hussain, S.; Antony, B. Non-alcoholic fatty liver disease and clinical outcomes in patients with COVID-19: A comprehensive systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 813–822. [Google Scholar] [CrossRef]
- Nielsen, M.B.; Finne, L.B.; Christensen, J.O.; Knardahl, S. Job demands and alcohol use: Testing a moderated mediation model. Scand. J. Work. Environ. Health 2015, 41, 43–53. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; W H Freeman/Times Books/Henry Holt & Co.: New York, NY, USA, 1997; Volume 9, p. 604. [Google Scholar]
- Bandura, A. Social Cognitive Theory: An agentic perspective. Annu. Rev. Psychol. 2001, 52, 21–41. [Google Scholar] [CrossRef]
- Makara-Studzińska, M.; Golonka, K.; Izydorczyk, B. Self-efficacy as a moderator between stress and professional burnout in firefighters. Int. J. Environ. Res. Public Health 2019, 16, 183. [Google Scholar] [CrossRef]
- Alessandri, G.; Perinelli, E.; De Longis, E.; Schaufeli, W.B.; Theodorou, A.; Borgogni, L.; Caprara, G.V.; Cinque, L. Job burnout: The contribution of emotional stability and emotional self-efficacy beliefs. J. Occup. Organ. Psychol. 2018, 91, 823–851. [Google Scholar] [CrossRef]
- Brown, C.G. A systematic review of the relationship between self-efficacy and burnout in teachers. Educ. Child Psychol. 2012, 29, 47–63. [Google Scholar] [CrossRef]
- Shoji, K.; Cieslak, R.; Smoktunowicz, E.; Rogala, A.; Benight, C.C.; Luszczynska, A. Associations between job burnout and self-efficacy: A meta-analysis. Anxiety Stress Coping 2016, 29, 367–386. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Franco-Díaz, K.L.; Fernández-Niño, J.A.; Astudillo-García, C.I. Prevalencia de síntomas depresivos e invarianza factorial de la Escala de Depresión del Centro de Estudios Epidemiológicos (CES-D) en población indígena mexicana [Prevalence of depressive symptoms and factorial invariance of the Center for Epidemiologic Studies (CES-D) Depression Scale in a group of Mexican indigenous population]. Biomédica 2018, 38, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Herrero, J.; Gracia, E. Una medida breve de la sintomatología depresiva (CESD-7). Salud Ment. 2007, 30, 40–46. [Google Scholar]
- Balasubramanian, A.; Paleri, V.; Bennett, R.; Paleri, V. Impact of COVID-19 on the mental health of surgeons and coping strategies. Head Neck 2020, 42, 1638–1644. [Google Scholar] [CrossRef]
- Babor, T.F.; Higgins-Bidle, J.C.; Saunders, J.B.; Monteiro, M.G. Audit. Cuestionario de Identificación de los Trastornos Debidos al Consumo de Alcohol. Pautas para su Utilización en Atención Primaria [AUDIT. Questionnaire for the Identification of Disorders due to Alcohol Consumption. Guidelines for Its Use in Primary Care]; Sustancias, S.M., Ed.; Organización Mundial de la Salud/World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, e103208. [Google Scholar] [CrossRef]
- IBM SPSS. AMOS. for Windows, 26.0.0 ed.; IBM Corporation: Wexford, PA, USA, 2019. [Google Scholar]
- IBM SPSS. For Windows, 26th ed.; IBM Corporation: Armonk, NY, USA, 2019. [Google Scholar]
- Cho, G.; Hwang, H.; Sarstedt, M.; Ringle, C.M. Cutoff criteria for overall model fit indexes in generalized structured component analysis. J. Mark. Anal. 2020, 8, 189–202. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural equation modeling with AMOS, EQS, and LISREL: Comparative approaches to testing for the factorial validity of a measuring instrument. Int. J. Test. 2001, 1, 55–86. [Google Scholar] [CrossRef]
- Collier, J.E. Applied Structural Equation Modeling Using AMOS; Basic to Advanced Techniques; Routledge: New York, NY, USA, 2020. [Google Scholar]
- Mache, S.; Vitzthum, K.; Groneberg, D.A. Prevention of study-related stress symptoms: Health-promoting behavior among dental students. Wien. Med. Wochenschr. 2015, 165, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E.; Leiter, M. The Maslach Burnout Inventory-Test Manual, 3rd ed.; Consulting Psychologist Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- Pietrowski, D.L.; Cardoso, N.D.O.; Bernardi, C.C.D.N. Estratégias de coping frente à síndrome de burnout entre os professores: Uma revisão integrativa da literatura nacional [Coping strategies for burnout syndrome between teachers: A national integrative literature review]. Contextos Clín. 2018, 11, 397–409. [Google Scholar] [CrossRef]
- Tsutsumi, A.; Kayaba, K.; Theorell, T.; Siegrist, J. Association between job stress and depression among Japanese employees threatened by job loss in a comparison between two complementary job-stress models. Scand. J. Work. Environ. Health 2001, 27, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Airagnes, G.; Lemogne, C.; Even-Baisse, M.-A.; Le Faou, A.-L.; Limosin, F. Work conditions are associated with alcohol use after taking into account life conditions outside of work: Findings from a french occupational health service. Subst. Use Misuse 2021, 56, 2259–2263. [Google Scholar] [CrossRef]
- Hruska, B.; Barduhn, M.S. Dynamic psychosocial risk and protective factors associated with mental health in Emergency Medical Service (EMS) personnel. J. Affect. Disord. 2021, 282, 9–17. [Google Scholar] [CrossRef]
- Bardhoshi, G.; Um, B. The effects of job demands and resources on school counselor burnout: Self-efficacy as a mediator. J. Couns. Dev. 2021, 99, 289–301. [Google Scholar] [CrossRef]
- Kumar, N.; Gupta, M.; Gupta, D.; Tiwari, S. Novel deep transfer learning model for COVID-19 patient detection using X-ray chest images. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 469–478. [Google Scholar] [CrossRef]
- Reis, H.C.; Turk, V. COVID-DSNet: A novel deep convolutional neural network for detection of coronavirus (SARS-CoV-2) cases from CT and Chest X-Ray images. Artif. Intell. Med. 2022, 134, 102427. [Google Scholar] [CrossRef]
- Calina, D.; Hartung, T.; Mardare, I.; Mitroi, M.; Poulas, K.; Tsatsakis, A.; Rogoveanu, I.; Docea, A.O. COVID-19 pandemic and alcohol consumption: Impacts and interconnections. Toxicol. Rep. 2021, 8, 529–535. [Google Scholar] [CrossRef]
- Valencia, P.D.; Torres-Quispe, M.A.; Sánchez-Cayo, S.; Reyes-Aguilar, R.F.; Acevedo-Cahuana, A.G. Factors associated with depressive symptomatology during the COVID-19 pandemic in Mexico: A 2021 national survey. J. Affect. Disord. 2022, 317, 212–220. [Google Scholar] [CrossRef]
| Relationships | B | S.E. | C.R. | β | p |
|---|---|---|---|---|---|
| Emotional Exhaustion → | |||||
| Self-Efficacy at Work | −0.20 | 0.03 | −7.07 | −0.18 | <0.001 |
| Depression | 0.60 | 0.03 | 24.59 | 0.54 | <0.001 |
| Alcohol Consumption | −0.02 | 0.02 | −1.08 | −0.04 | 0.279 |
| Depersonalization → | |||||
| Self-Efficacy at Work | −0.21 | 0.03 | −6.25 | −0.15 | <0.001 |
| Depression | 0.14 | 0.03 | 5.33 | 0.10 | <0.001 |
| Alcohol Consumption | 0.10 | 0.02 | 5.89 | 0.15 | <0.001 |
| Achievement Dissatisfaction → | |||||
| Self-Efficacy at Work | −0.19 | 0.04 | −4.86 | −0.12 | <0.001 |
| Depression | 0.18 | 0.03 | 5.79 | 0.12 | <0.001 |
| Alcohol Consumption | 0.00 | 0.02 | 0.21 | 0.01 | 0.835 |
| Self-Efficacy at Work → | |||||
| Depression | −0.11 | 0.02 | −7.53 | −0.11 | <0.001 |
| Alcohol Consumption | −0.02 | 0.01 | −2.19 | −0.04 | 0.029 |
| Depression → | |||||
| Alcohol Consumption | 0.08 | 0.01 | 6.19 | 0.18 | <0.001 |
| B | Confidence Interval | p | ||
|---|---|---|---|---|
| Low | High | |||
| EE -> D -> AC | 0.049 | 0.035 | 0.066 | 0.006 |
| EE -> SE -> AC | 0.004 | 0.001 | 0.007 | 0.030 |
| EE -> SE -> D -> AC | 0.002 | 0.001 | 0.003 | 0.004 |
| DEP -> D -> AC | 0.011 | 0.007 | 0.017 | 0.012 |
| DEP -> SE -> AC | 0.004 | 0.002 | 0.009 | 0.014 |
| DEP -> SE -> D -> AC | 0.002 | 0.001 | 0.003 | 0.004 |
| AD -> D -> AC | 0.014 | 0.009 | 0.020 | 0.008 |
| AD -> SE ->AC | 0.004 | 0.001 | 0.009 | 0.013 |
| AD -> SE -> D -> AC | 0.002 | 0.001 | 0.003 | 0.002 |
| SE-> D ->AC | −0.009 | −0.013 | −0.006 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domínguez-Espinosa, A.d.C.; Laborda Sánchez, F.; Polo Velázquez, A.M.; Polanco Hernández, G. A Mediation Model of Self-Efficacy and Depression between Burnout and Alcohol Consumption among Health Workers during the COVID-19 Pandemic. COVID 2023, 3, 643-654. https://doi.org/10.3390/covid3040046
Domínguez-Espinosa AdC, Laborda Sánchez F, Polo Velázquez AM, Polanco Hernández G. A Mediation Model of Self-Efficacy and Depression between Burnout and Alcohol Consumption among Health Workers during the COVID-19 Pandemic. COVID. 2023; 3(4):643-654. https://doi.org/10.3390/covid3040046
Chicago/Turabian StyleDomínguez-Espinosa, Alejandra del Carmen, Fátima Laborda Sánchez, Alma Mireya Polo Velázquez, and Graciela Polanco Hernández. 2023. "A Mediation Model of Self-Efficacy and Depression between Burnout and Alcohol Consumption among Health Workers during the COVID-19 Pandemic" COVID 3, no. 4: 643-654. https://doi.org/10.3390/covid3040046
APA StyleDomínguez-Espinosa, A. d. C., Laborda Sánchez, F., Polo Velázquez, A. M., & Polanco Hernández, G. (2023). A Mediation Model of Self-Efficacy and Depression between Burnout and Alcohol Consumption among Health Workers during the COVID-19 Pandemic. COVID, 3(4), 643-654. https://doi.org/10.3390/covid3040046






