Early Discharge from a Newborn Nursery in the United States during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Population
2.2. Outcomes and Study Definitions
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Demographics
3.2. Early Discharge (Less Than or Equal to 24 h of Age)
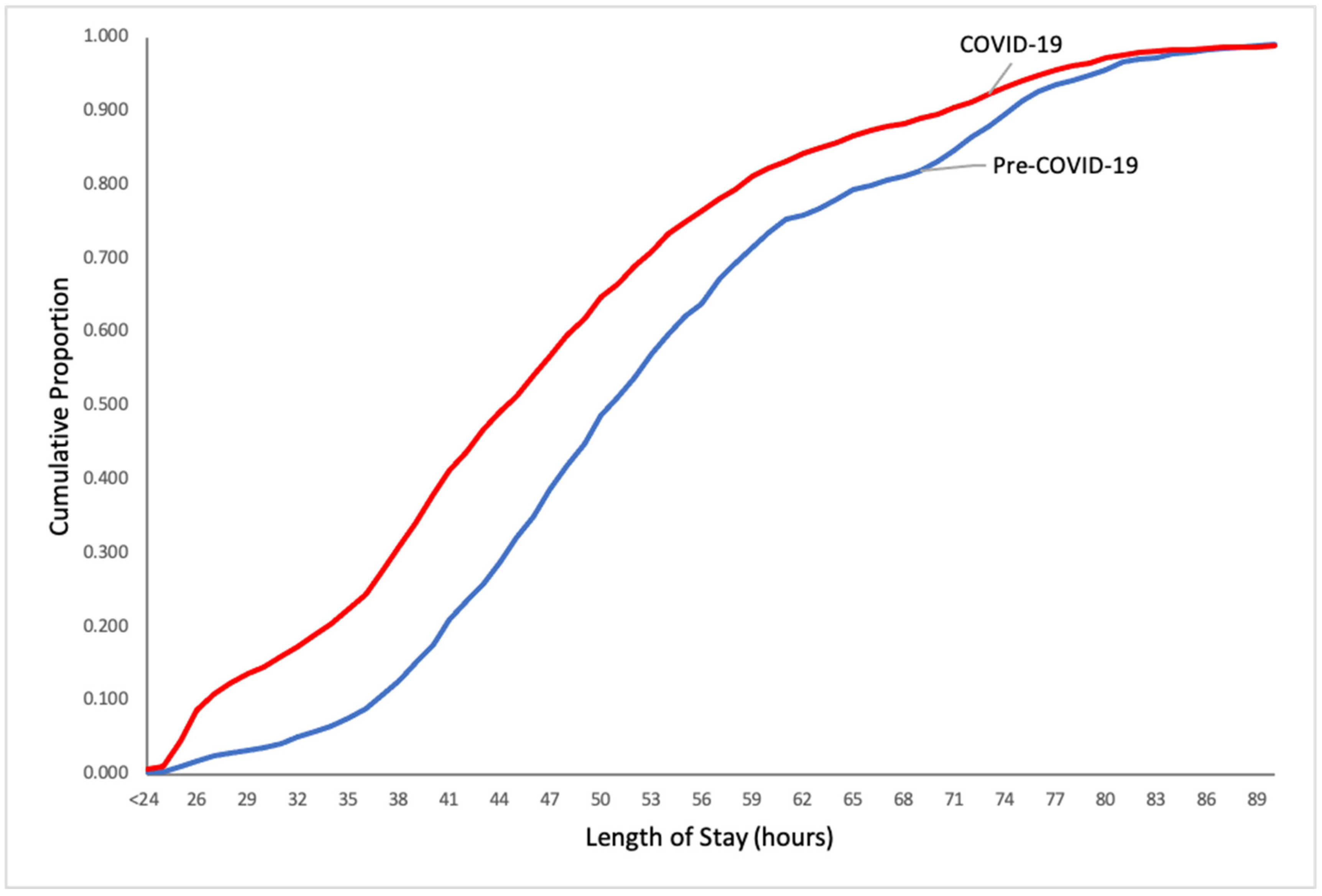
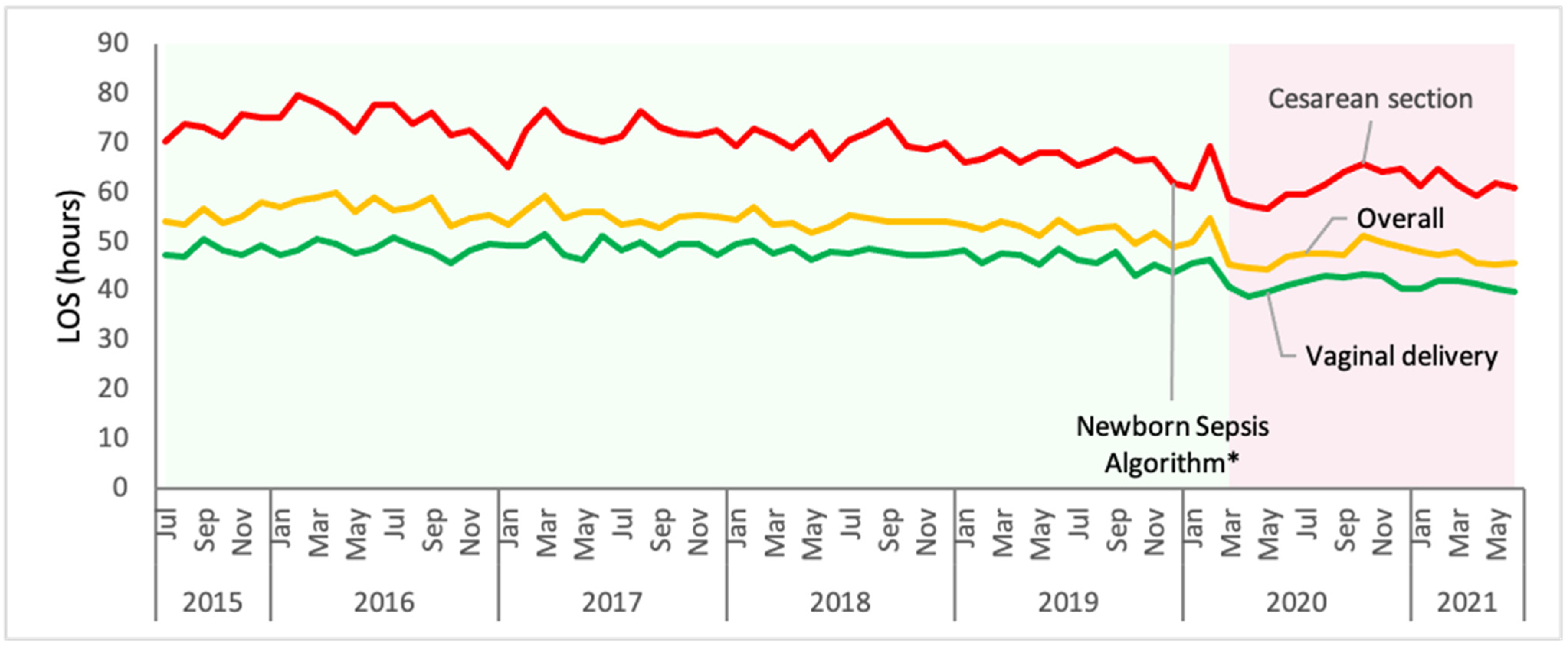
3.3. Length of Stay
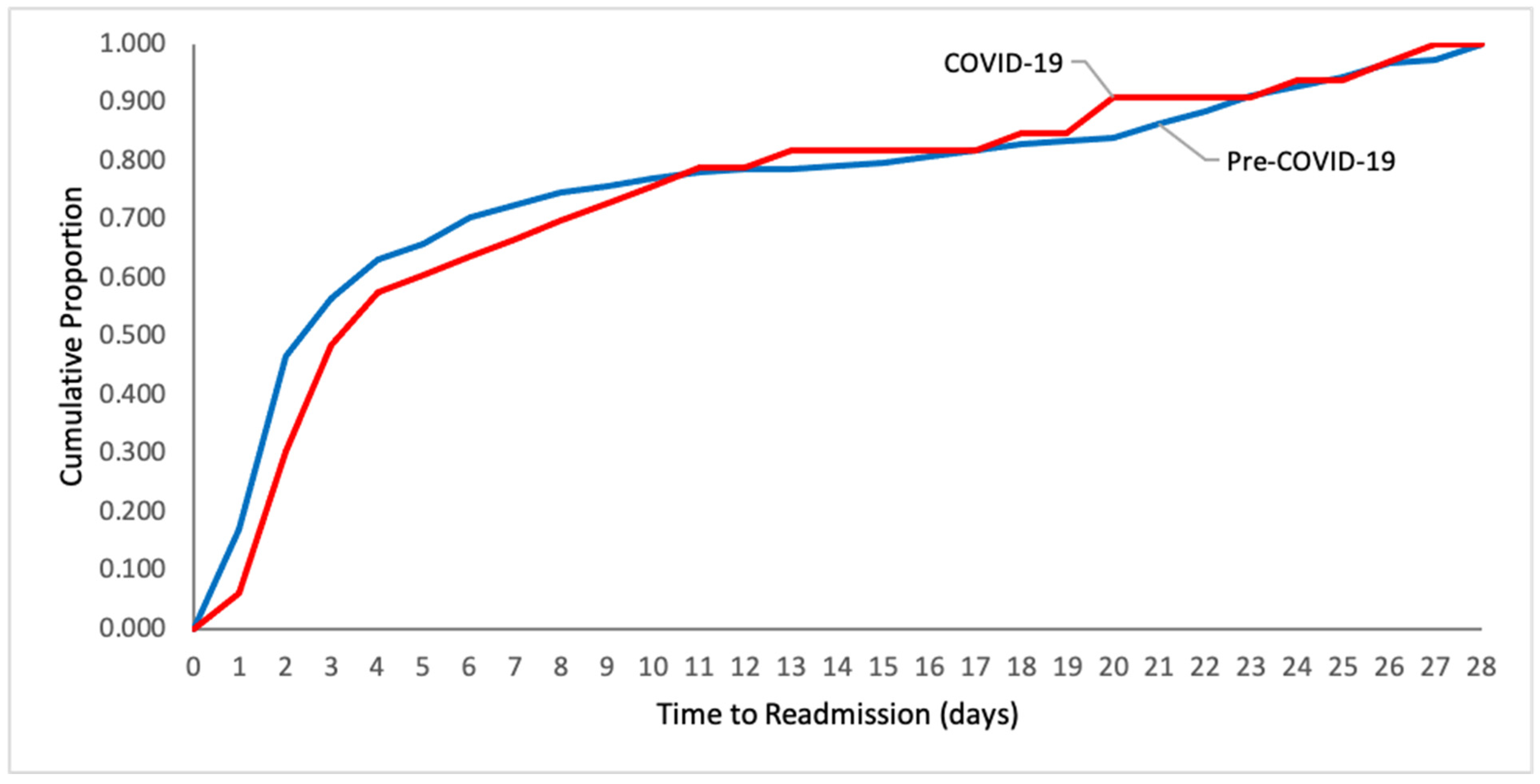
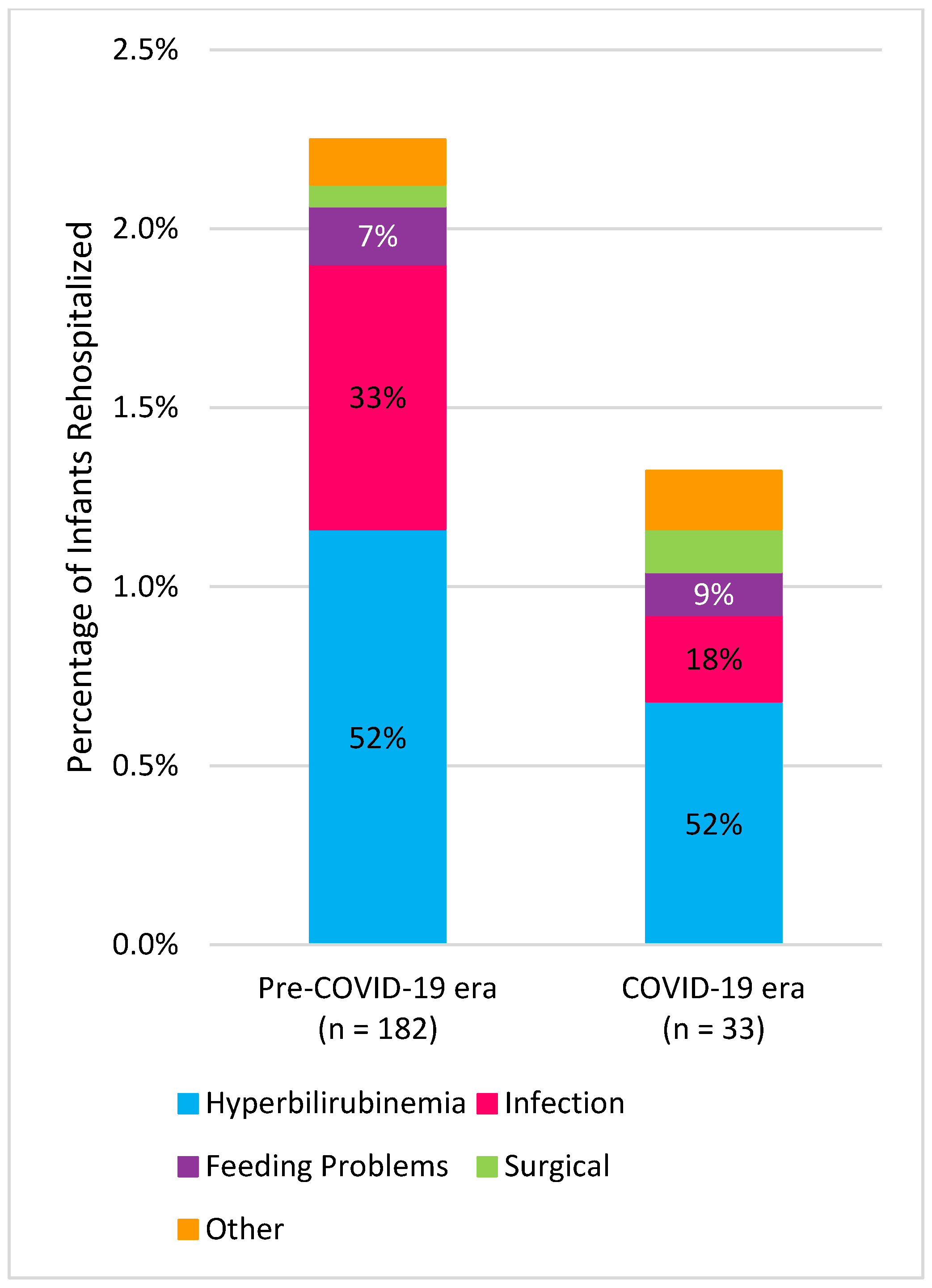
3.4. Readmissions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Datar, A.; Sood, N. Impact of Postpartum Hospital-Stay Legislation on Newborn Length of Stay, Readmission, and Mortality in California. Pediatrics 2006, 118, 63–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, E.; Taylor, B.; MacArthur, C.; Bradshaw, S.; Hope, L.; Cummins, C. Early Postnatal Discharge for Infants: A Meta-analysis. Pediatrics 2020, 146, e20193365. [Google Scholar] [CrossRef] [PubMed]
- Kotagal, U.R.; Atherton, H.D.; Eshett, R.; Schoettker, P.J.; Perlstein, P.H. Safety of Early Discharge for Medicaid Newborns. JAMA J. Am. Med. Assoc. 1999, 282, 1150–1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, I.M.; Lehman, E.B.; Hollenbeak, C.S.; Maisels, M.J. Preventable Newborn Readmissions Since Passage of the Newborns’ and Mothers’ Health Protection Act. Pediatrics 2006, 118, 2349–2358. [Google Scholar] [CrossRef] [PubMed]
- Committee on Fetus and Newborn. Hospital Stay for Healthy Term Newborns. Pediatrics 2004, 113, 1434–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benitz, W.E.; Committee on Fetus and Newborn; Watterberg, K.L.; Aucott, S.; Benitz, W.E.; Cummings, J.J.; Eichenwald, E.C.; Goldsmith, J.; Poindexter, B.B.; Puopolo, K.; et al. Hospital Stay for Healthy Term Newborn Infants. Pediatrics 2015, 135, 948–953. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. 2014. Available online: https://apps.who.int/iris/handle/10665/97603 (accessed on 20 December 2021).
- U.S. Department of Labor. Newborns’ and Mothers’ Portections. Available online: https://www.dol.gov/general/topic/health-plans/newborns (accessed on 20 December 2021).
- Mosen, D.M.; Clark, S.L.; Mundorff, M.B.; Tracy, D.M.; McKnight, E.C.; Zollo, M.B. The medical and economic impact of the newborns’ and mothers’ health protection act. Obstet. Gynecol. 2002, 99, 116–124. [Google Scholar] [CrossRef]
- Watt, S.; Sword, W.; Krueger, P. Longer postpartum hospitalization options—Who stays, who leaves, what changes? BMC Pregnancy Childbirth 2005, 5, 13. [Google Scholar] [CrossRef] [Green Version]
- Norton, A.; Wilson, T.; Geller, G.; Gross, M.S. Impact of Hospital Visitor Restrictions on Racial Disparities in Obstetrics. Health Equity 2020, 4, 505–508. [Google Scholar] [CrossRef]
- Davis-Floyd, R.; Gutschow, K.; Schwartz, D.A. Pregnancy, Birth and the COVID-19 Pandemic in the United States. Med. Anthropol. 2020, 39, 413–427. [Google Scholar] [CrossRef]
- Altman, M.R.; Eagen-Torkko, M.K.; Mohammed, S.A.; Kantrowitz-Gordon, I.; Khosa, R.M.; Gavin, A.R. The impact of COVID-19 visitor policy restrictions on birthing communities of colour. J. Adv. Nurs. 2021, 77, 4827–4835. [Google Scholar] [CrossRef] [PubMed]
- Associated Press News. Iowa Governor Announces First 3 COVID-19 Cases in State. 2020. Available online: https://apnews.com/article/virus-outbreak-science-iowa-kim-reynolds-ia-state-wire-4fed9d219a5c62f884f4eae081ddfa9b (accessed on 20 December 2021).
- Campbel, M.J.; Swinscow, T. Statistics at Square One, 6th ed.; BMJ: London, UK, 2002. [Google Scholar]
- Jones, E.; Taylor, B.; MacArthur, C.; Pritchett, R.; Cummins, C. The effect of early postnatal discharge from hospital for women and infants: A systematic review protocol. Syst. Rev. 2016, 5, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, E.; Stewart, F.; Taylor, B.; Davis, P.G.; Brown, S.J. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst. Rev. 2021, 6, Cd002958. [Google Scholar] [CrossRef] [PubMed]
- Campbell, O.M.; Cegolon, L.; Macleod, D.; Benova, L. Length of Stay After Childbirth in 92 Countries and Associated Factors in 30 Low- and Middle-Income Countries: Compilation of Reported Data and a Cross-sectional Analysis from Nationally Representative Surveys. PLoS Med. 2016, 13, e1001972. [Google Scholar] [CrossRef] [Green Version]
- Farhat, R.; Rajab, M. Length of postnatal hospital stay in healthy newborns and re-hospitalization following early discharge. N. Am. J. Med. Sci. 2011, 3, 146–151. [Google Scholar] [CrossRef]
- Harriel, K.L.; Nolt, D.; Moore, S.; Kressly, S.; Bernstein, H.H. Management of neonates after postpartum discharge and all children in the ambulatory setting during the coronavirus disease 2019 (COVID-19) pandemic. Curr. Opin. Pediatr. 2020, 32, 610–618. [Google Scholar] [CrossRef]
- Metcalfe, A.; Mathai, M.; Liu, S.; Leon, J.A.; Joseph, K.S. Proportion of neonatal readmission attributed to length of stay for childbirth: A population-based cohort study. BMJ Open 2016, 6, e012007. [Google Scholar] [CrossRef]
- Handley, S.C.; Gallagher, K.; Breden, A.; Lindgren, E.; Lo, J.Y.; Son, M.; Murosko, D.; Dysart, K.; Lorch, S.A.; Greenspan, J.; et al. Birth Hospital Length of Stay and Rehospitalization During COVID-19. Pediatrics 2021, 149, e2021053498. [Google Scholar] [CrossRef]
- Greene, N.H.; Kilpatrick, S.J.; Wong, M.S.; Ozimek, J.A.; Naqvi, M. Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM 2020, 2, 100234. [Google Scholar] [CrossRef]
- Bornstein, E.; Gulersen, M.; Husk, G.; Grunebaum, A.; Blitz, M.J.; Rafael, T.J.; Rochelson, B.L.; Schwartz, B.; Nimaroff, M.; Chervenak, F.A. Early postpartum discharge during the COVID-19 pandemic. J. Perinat. Med. 2020, 48, 1008–1012. [Google Scholar] [CrossRef]
- Vazquez-Vazquez, A.; Dib, S.; Rougeaux, E.; Wells, J.C.; Fewtrell, M.S. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the UK: Preliminary data from the COVID-19 New Mum Study. Appetite 2021, 156, 104985. [Google Scholar] [CrossRef] [PubMed]
- Escobar, G.J.; Greene, J.D.; Hulac, P.; Kincannon, E.; Bischoff, K.; Gardner, M.N.; Armstrong, M.A.; France, E.K. Rehospitalisation after birth hospitalisation: Patterns among infants of all gestations. Arch. Dis. Child. 2005, 90, 125. [Google Scholar] [CrossRef] [PubMed]
- Dinleyici, E.C.; Borrow, R.; Safadi, M.A.P.; van Damme, P.; Munoz, F.M. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum. Vaccin. Immunother. 2021, 17, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Puopolo, K.M.; Benitz, W.E.; Zaoutis, T.E.; Committee on Fetus and Newborn; Committee on Infectious Diseases; Cummings, J.; Juul, S.; Hand, I.; Eichenwald, E.; Poindexter, B.; et al. Management of Neonates Born at ≥35 0/7 Weeks’ Gestation With Suspected or Proven Early-Onset Bacterial Sepsis. Pediatrics 2018, 142, e20182894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barfield, W.D. Social disadvantage and its effect on maternal and newborn health. Semin. Perinatol. 2021, 45, 151407. [Google Scholar] [CrossRef] [PubMed]
| Pre-COVID-19 Era * (n = 8094) | COVID-19 Era * (n = 2495) | p Value | |
|---|---|---|---|
| Gestational age, mean (SD), weeks | 39.2 (1.3) | 39.0 (1.3) | <0.001 |
| Maternal age, mean (SD), years | 29.8 (5.3) | 29.7 (5.4) | 0.35 |
| Birth weight, mean (SD), grams | 3381 (503) | 3354 (488) | 0.02 |
| Race, n (%) ** | |||
| White | 5387 (66.6) | 1579 (63.3) | 0.003 |
| African American/Black | 998 (12.3) | 273 (10.9) | 0.06 |
| American Indian/Alaska Native | 24 (0.3) | 9 (0.4) | 0.62 |
| Asian | 393 (4.9) | 96 (3.8) | 0.04 |
| Hispanic | 502 (6.2) | 175 (7.0) | 0.15 |
| Native Hawaiian/Pacific Islander | 8 (0.1) | 5 (0.2) | 0.21 |
| Multiracial/two or more races | 690 (8.5) | 241 (9.7) | 0.08 |
| Declined | 92 (1.1) | 117 (4.7) | <0.001 |
| Mode of Delivery, n (%) | |||
| Vaginal delivery | 5761 (71.2) | 1780 (71.3) | 0.87 |
| Cesarean section | 2333 (28.8) | 715 (28.7) |
| Pre-COVID-19 Era * (n = 19) | COVID-19 Era * (n = 24) | p Value | |
|---|---|---|---|
| Gestational age, mean (SD), weeks | 39.8 (1.1) | 39.7 (0.6) | 0.57 |
| Maternal age, mean (SD), years | 31.8 (3.9) | 29.1 (4.3) | 0.04 |
| Birth weight, mean (SD), grams | 3407 (332) | 3464 (381) | 0.60 |
| Mode of Delivery, n (%) | |||
| Vaginal delivery | 19 (100) | 24 (100) | |
| Cesarean section | - | - | |
| 28-day Readmission, n (%) | 1 (5) | 0 (0) | 0.44 |
| Shortened Pre-COVID-19 Era * (n = 2268) n (%) | COVID-19 Era * (n = 2495) n (%) | Incidence Rate Ratio (95% CI) | |
|---|---|---|---|
| Discharges ≤24 h | 7 (0.31) | 24 (0.96) | 3.1 (1.3–7.2) |
| Discharges from 25 to 30 h | 73 (3.2) | 338 (13.5) | 4.2 (3.3–5.4) |
| Discharges from 31 to 36 h | 120 (5.3) | 245 (9.8) | 1.9 (1.5–2.3) |
| Discharges from 37 to 48 h | 750 (33.1) | 881 (35.3) | 1.1 (1.0–1.2) |
| Discharges >48 h | 1318 (58.1) | 1007 (40.4) | 0.7 (0.6–0.8) |
| Pre-COVID-19 Era * (n = 182) | COVID-19 Era * (n = 33) | p Value | |
|---|---|---|---|
| Gestational age, mean (SD), weeks | 38.6 (1.5) | 38.6 (1.3) | 0.90 |
| Maternal age, mean (SD), years | 30.2 (5.1) | 30.6 (5.3) | 0.65 |
| Birth weight, mean (SD), grams | 3379 (486) | 3227 (555) | 0.15 |
| Mode of Delivery, n (%) | |||
| Vaginal delivery | 144 (79) | 27 (82) | 0.82 |
| Cesarean section | 38 (21) | 6 (18) | |
| Length of Stay, n (%) | |||
| Discharges ≤24 h | 1 (1) | 0 (0) | 0.07 |
| Discharges from 25 to 30 h | 4 (2) | 5 (15) | |
| Discharges from 31 to 36 h | 8 (4) | 1 (3) | |
| Discharges from 37 to 48 h | 64 (35) | 11 (33) | |
| Discharges >48 h | 105 (58) | 16 (49) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wood, K.E.; Schmitz, A.; Bhoojhawon, G. Early Discharge from a Newborn Nursery in the United States during the COVID-19 Pandemic. COVID 2022, 2, 379-388. https://doi.org/10.3390/covid2030026
Wood KE, Schmitz A, Bhoojhawon G. Early Discharge from a Newborn Nursery in the United States during the COVID-19 Pandemic. COVID. 2022; 2(3):379-388. https://doi.org/10.3390/covid2030026
Chicago/Turabian StyleWood, Kelly E., Anna Schmitz, and Guru Bhoojhawon. 2022. "Early Discharge from a Newborn Nursery in the United States during the COVID-19 Pandemic" COVID 2, no. 3: 379-388. https://doi.org/10.3390/covid2030026
APA StyleWood, K. E., Schmitz, A., & Bhoojhawon, G. (2022). Early Discharge from a Newborn Nursery in the United States during the COVID-19 Pandemic. COVID, 2(3), 379-388. https://doi.org/10.3390/covid2030026






