Abstract
The COVID-19 pandemic changed birth hospitalization, with many hospitals implementing restrictions. Little is known about the impact of the COVID-19 pandemic on rates of early newborn discharge and length of stay (LOS). The primary objective was to compare rates of early discharge before and after the start of the COVID-19 pandemic. Secondary objectives included 28-day readmissions and LOS. A single-center retrospective cohort study was undertaken of all live newborns discharged from a well newborn nursery in the United States between 1 July 2015 and 18 June 2021. The pre-COVID-19 era was defined as 1 July 2015 to 29 February 2020, and the COVID-19 era as 1 March 2020 to 18 June 2021, based on the first case reported in our state. Early discharge was defined as less than or equal to 24 h. A total of 10,589 newborns were included: 8094 before and 2495 after the COVID-19 pandemic started. Overall, 43 newborns (0.41%) were discharged early. In the COVID-19 era, early discharges significantly increased from 0.23% (n = 19) to 0.96% (n = 24) (p < 0.001). Median LOS declined from 52.0 (IQR, 43.0–64.0) to 45.0 (IQR, 37.0–56.0) hours (p < 0.001). The 28-day readmission rate decreased from 2.3% (n = 182) to 1.3% (n = 33) (p < 0.01). Since the start of the COVID-19 pandemic, the number of early discharges has significantly increased at our institution without an increase in readmissions. Additionally, overall decrease in length of stay for the birth hospitalization was observed. Potential reasons include changes in hospital unit policies including visitor limitations to reduce COVID-19 infection risk to patients and staff and/or parental concern for iatrogenic acquisition of the virus.
1. Introduction
Early discharge of a newborn infant has been shown in some studies to be associated with increased risk of readmission [1,2,3,4]. In 2004, the American Academy of Pediatrics (AAP) in the United States (U.S.) defined early discharge as less than or equal to 48 h [5]. In 2015, the AAP outlined minimum discharge criteria for term healthy infants, recognizing that timing of discharge should be individualized to the mother-infant dyad and involve shared decision-making with the parents [6]. In 2015, the World Health Organization (WHO) published updated guidelines increasing the recommended minimum length of stay (LOS) after an uncomplicated vaginal delivery from 12 to 24 h [7].
In 1996, the U.S. Congress passed the Newborns’ and Mothers’ Health Protection Act [8]. This federal law mandates insurers to pay for at least a 48 h hospital stay following vaginal delivery and 96 h after a Cesarean delivery [8]. After passage, several studies demonstrated an increased length of hospital stay [4,9,10]. With guaranteed insurance coverage, shorter length of stay may still occur if the practitioner, in agreement with the parent, elects for early discharge [4].
The arrival of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 virus), the causative agent for Coronavirus-19 Disease (COVID-19), brought changes to the birth experience and hospitalization in general in the United States. Many hospitals adopted restricted visitor policies [11,12]. These policies may have enhanced preexisting socioeconomic disparities in the neonatal and post-partum period [13]. Little is known as to how these policies have affected newborn and maternal health outcomes.
The primary objective of our study was to evaluate the incidence of early discharges from our newborn nursery and compare rates before and after the start of the COVID-19 pandemic. We hypothesized that the number of early discharges would increase after the start of the COVID-19 pandemic. Secondary objectives include LOS over time and rates of readmission after discharge.
2. Materials and Methods
2.1. Study Design and Patient Population
We performed a retrospective cohort study at a single academic institution in the Midwestern United States. Our medical center has the state’s only Level IV Neonatal Intensive Care Unit (NICU), Level 1 trauma center, and is affiliated with the state’s medical school. It is the major referral center for high-risk obstetrics and serves a large catchment area due to the closing of regional birthing centers. The catchment area for our academic institution is the eastern half of the state as well as the far western portion of the neighboring state, an area of approximately 25,000 square miles. In 2020, approximately 2100 newborns were admitted to the nursery.
All live newborns discharged from the well-newborn nursery between 1 July 2015 and 18 June 2021 were included. At our institution, newborns of 35 weeks gestation or greater weighing at least 1900 g may be admitted to the well-newborn nursery. Nursery capabilities include intravenous (IV) antibiotics, phototherapy, and hypoglycemia management, including dextrose gel and a single IV dextrose bolus. Newborns requiring respiratory support or cardiopulmonary monitoring are admitted to the NICU. At our institution, standard discharge is on day of life two for vaginal deliveries and day of life three for cesarean section (C-section). We divided the cohorts into two groups based on the first reported COVID-19 case in our state [14]. The pre-COVID-19 group included patients discharged between 1 July 2015 and 29 February 2020. The COVID-19 group comprised patients discharged between 1 March 2020 and 18 June 2021.
2.2. Outcomes and Study Definitions
The primary endpoint of the study was the proportion of newborns with early discharge. The secondary endpoints were LOS and all-cause 28-day readmissions for patients within our system. Early discharge was defined as a hospital stay less than or equal to 24 h of age. This definition was chosen based upon institutional practice, where newborns are discharged based upon day of life rather than by hours of age. Standard institutional practice is to discharge in the morning on day of life two after a vaginal or uncomplicated C-section delivery and in the morning on day of life three for all other C-section deliveries. LOS was calculated in hours using the date and time of birth and discharge. Time to readmission was calculated from the date and time of the rehospitalization and newborn nursery discharge.
2.3. Data Collection
All data were collected from the electronic medical record (EMR) and included date and time of birth, hospital discharge, and readmission. Additional data collected included gestational age, maternal age, mode of delivery, infant race, infant sex, birth weight, and reason for readmission. Race was parent-reported and based upon predefined EMR racial categories including White, African American/Black, American Indian/Alaska Native, Asian, Hispanic, Native Hawaiian/Pacific Islander, Multiracial/two or more races, or declined. LOS was categorized into five groups: less than or equal to 24 h, 25 to 30 h, 31 to 36 h, 37 to 48 h, and greater than 48 h.
2.4. Statistical Analysis
Descriptive statistics were used to describe the study cohorts [15]. Bivariable statistical procedures included the two-tailed Student’s t-test and Mann-Whitney-Wilcoxon test for numerical variables. Chi-square tests and Fisher’s exact tests were calculated for categorical variables. Column proportions were compared using the Z-test and a Bonferroni correction was applied. To control for seasonal and temporal differences in LOS, focused analysis was performed for patients discharged between 1 March 2018 and 18 June 2019 (Shortened pre-COVID-19 group) and between 1 March 2020 and 18 June 2021 (COVID-19 group). The two-sample Kolmogorov-Smirnov test was used to compare the cumulative distribution functions of LOS and time to readmissions. Incidence rate ratios were computed for each individual LOS group using the shortened pre-pandemic rates as reference. A significance value of 0.05 was used. No data was missing. We performed statistical analyses with IBM SPSS Statistics for Windows, Version 27.0 (Armonk, NY, USA).
3. Results
3.1. Demographics
A total of 10,589 newborns were included, with 8094 in the pre-COVID-19 and 2495 in the COVID-19 cohorts. For the entire population, 65.8% (n = 6966) of infants identified as White, 12.0% (n = 1271) African American/Black, 8.8% (n = 931) Multiracial/Two or More Races, 6.4% (n = 677) Hispanic, 4.6% (n = 489) Asian, 0.3% (n = 33) American Indian/Alaska Native, 0.1% (n = 13) Native Hawaiian/Pacific Islander, and 2.0% (n = 209) declined categorization. Baseline characteristics for each cohort are described in Table 1.

Table 1.
Baseline characteristics of newborns born before and during the COVID-19 pandemic.
Mean gestational age was significantly higher in the pre-COVID-19 era, 39.2 vs. 39.0 weeks (p < 0.001). Mean birth weight was significantly higher in the pre-COVID-19 era, 3381 vs. 3354 g (p = 0.02). For race, the pre-COVID-19 cohort had a significantly lower proportion decline categorization (1.1% vs. 4.7%, p < 0.001), and a higher proportion of White newborns (66.6% vs. 63.3%, p = 0.003). There was no significant difference in maternal age or mode of delivery between the two cohort groups (Table 1).
3.2. Early Discharge (Less Than or Equal to 24 h of Age)
Early discharge occurred at a significantly lower rate during the pre-COVID-19 period, 0.23% vs. 0.96% (p < 0.001). During the pre-pandemic era, 19 newborns were discharged at less than or equal to 24 h of age over a 56-month period compared to 24 newborns over almost 14 months during the pandemic era. Mothers of early discharged newborns were significantly older in the pre-pandemic era compared to the pandemic era, 31.8 vs. 29.1 years, (p = 0.04). There were no significant differences in gestational age or birth weight. All newborns discharged early were born by vaginal delivery (Table 2). In addition, discharges before 24 h of age also significantly increased during the COVID-19 era, 0.11% (n = 9) vs. 0.60% (n = 15) (p < 0.001).

Table 2.
Characteristics of newborns discharging early (less than or equal to 24 h) before and during the COVID-19 pandemic.
3.3. Length of Stay
The median (interquartile range) LOS was significantly higher during the pre-COVID-19 pandemic era at 52.0 (43.0–64.0) vs. 45.0 (37.0–56.0) hours (p < 0.001). A two-sample Kolmogorov-Smirnov test showed a significant difference towards earlier discharge across the entire population (p < 0.001).
To control for seasonal and temporal trends in length of stay, a focused data analysis was performed for discharges across the same months of the year in different years. Table 3 demonstrates the incidence rate ratios of discharges grouped in five LOS categories. In the COVID-19 era, a discharge at less or equal to 24 h of age was 3.1 times (95% CI, 1.3–7.2) more likely to occur compared to the pre-pandemic levels. Similarly, a discharge at 25–30 h of age was 4.2 times more likely (95% CI, 3.3–5.4) to occur in the COVID-19 era. Figure 1 illustrates the shift in distribution of LOS over the same periods (1 March–18 June). Figure 2 showcases the trends in LOS for our institution for cesarean, and vaginal deliveries over the six-year period.

Table 3.
Proportion of Discharges by length of stay before and during the COVID-19 pandemic.
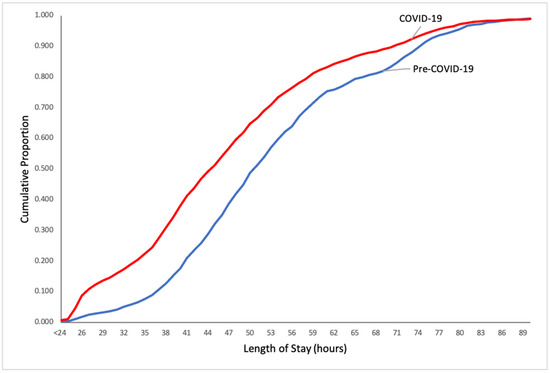
Figure 1.
Cumulative proportion of newborn discharges by length of stay in hours before and during the COVID-19 pandemic.
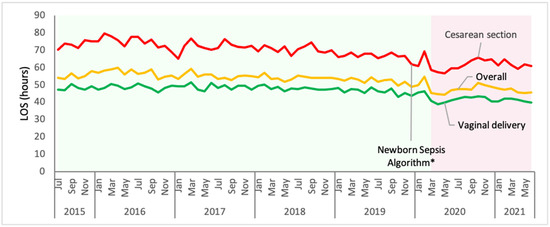
Figure 2.
Mean length of stay in hours for overall, cesarean, and vaginal deliveries before and during the COVID-19 pandemic Footnote—Pre-COVID-19 era (1 July 2015–29 February 2020) is shaded in light green. COVID-19 era (1 March 2020–18 June 2021) is shaded in light pink. * A new newborn sepsis algorithm was implemented in December 2019.
3.4. Readmissions
Readmissions included all causes within the first 28 days after the day of newborn nursery discharge. For newborns with more than one readmission, only the first readmission was included. Readmissions occurred in 2% (n = 182) of the pre-COVID-19 cohort compared to 1% (n = 33) of the COVID-19 cohort (p = 0.004). There was no association between study cohorts and LOS for readmitted patients (p = 0.07). There was also no association between study cohorts and race for readmitted patients (p = 0.05). Only one newborn discharged early was readmitted. The newborn failed the critical congenital heart disease screen at a follow-up appointment one day after discharge and was found to have pulmonary hypertension on an echocardiogram (Table 4).

Table 4.
Characteristics of infants readmitted within 28 days of hospital discharge.
Figure 3 shows the cumulative proportion of readmissions by time to hospitalization. There was no difference in the cumulative distribution function, with a Kolmogorov-Smirnov test D(215) = 0.997, (p = 0.27) indicating no difference between time to readmission between the cohorts.
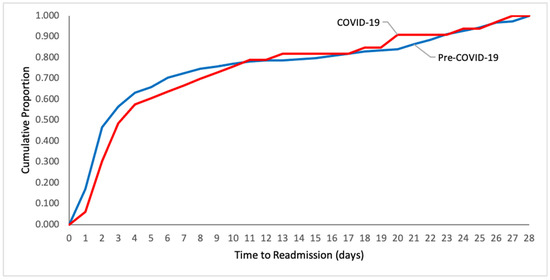
Figure 3.
Cumulative proportion of infant readmissions by time to readmission in days.
The reasons for readmission were categorized as hyperbilirubinemia, infection (included documented or suspected, fever, and hypothermia), feeding problems (included dehydration), surgical, and other. Less common reasons included in the category of “other” included but was not limited to fall, cardiac or respiratory issues, and suspected child abuse. Hyperbilirubinemia was the most common reason for readmission, accounting for over 50% of readmissions in both groups. For the pre-COVID-19 cohort, 52% (n = 94) were readmitted for hyperbilirubinemia, 33% (n = 60) infection, 7% (n = 13) feeding problems, 3% (n = 5) surgical, and 6% (n = 10) other. In the COVID-19 cohort, 52% (n = 17) were readmitted for hyperbilirubinemia, 18% (n = 6) infection, 9% (n = 3) feeding problems, 9% (n = 3) surgical, and 12% (n = 4) other. There was no significant difference in readmission diagnosis between the cohorts (p = 0.177). Eleven newborns were admitted twice within first 28 days. Figure 4 shows the breakdown of readmission by indication.
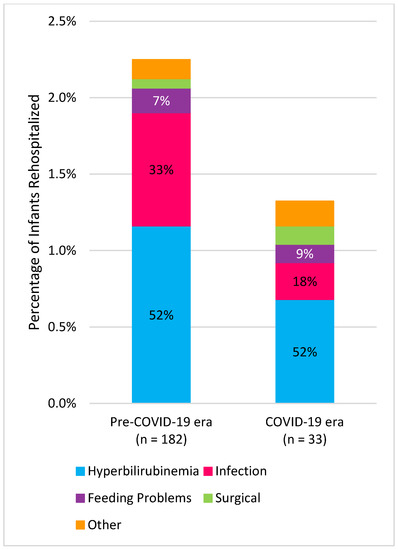
Figure 4.
Readmitted infants and reason for readmission during first 28 days after discharge. Footnote—Infection includes confirmed or suspected fever and hypothermia. Feeding problems include dehydration. The distribution of readmission reason in the pre-COVID-19 era included 52% hyperbilirubinemia, 33% infection, 7% feeding problems, 3% surgical, and 6% other. The distribution of readmission reason in the COVID-19 era included 52% hyperbilirubinemia, 18% infection, 9% feeding problems, 9% surgical, and 12% other.
4. Discussion
The length of birth hospitalization after an uncomplicated delivery has decreased in several countries worldwide, including the U.S., United Kingdom (U.K.), and Canada [16,17]. Currently, in these countries the average length of stay after a singleton vaginal delivery ranges between 1.5 and 2.0 days [18]. Cited benefits for earlier discharge include improved family bonding, decreased risk of iatrogenic infection, and potentially decreased healthcare cost [17,19,20]. Little is known about the impact of COVID-19 on the birth hospitalization. In our study in the U.S., we found that rates of early newborn discharge, at less than or equal to 24 h of age, increased without an increase in 28 day readmissions.
The definition of early discharge varies significantly among studies resulting in conflicting and challenging results in terms of interpretation [17,21]. In 2021, a Cochrane review looking at early postnatal discharge of term infants weighing 2500 g or more at birth found that the definition of “early” varied from 6 h to four to five days [17]. The authors concluded that early discharge probably leads to a higher risk of infant readmission within 28 days of birth [17]. A 2020 meta-analysis by Jones et al. pooled readmission data from seven randomized controlled studies and found that infants discharged early were more likely to be readmitted within 28 days compared to standard discharge [2].
Our results are consistent with recently published studies since the onset of the pandemic. In a study of 35 health systems in the U.S. including over 200,000 healthy term singleton infants, Handley et al. reported early postnatal discharge increased from 28.5% to 43% for all births during the COVID-19 era, defined as less than two midnights for vaginal and three midnights for cesarean births [22]. They looked at readmission rates in the first seven days of life, and reported a slight decrease during the pandemic, 1.2% versus 1.1% [22]. After modification of unit policy in response to COVID-19, one U.S. hospital reported that almost half of newborns born vaginally were discharged home after one midnight compared to a quarter prior to implementation [23]. Similarly, 42.5% versus 12.5% of newborns born via C-section were discharged after less than or equal to two midnights. Rates of newborn readmission within 28 days decreased from 2.1% to 1.3% postimplementation [23]. In a study of seven New York hospitals, a significant decrease in postnatal hospital LOS in the COVID-19 era was observed for both vaginal and C-section deliveries [24]. Similarly, in the U.K. the COVID-19 New Mum Study reported a significant decrease in postnatal length of stay after implementation of lockdown measures [25].
During the COVID-19 era, data from U.S. healthcare systems discussed above showed that early discharge has not been shown to increase readmissions; in fact, a decrease in readmissions has been observed [22,23]. The reason for this is unclear, and contradicts the findings of a pre-pandemic meta-analysis which found infants discharged early were more likely to be readmitted within 28 days [2]. In the meta-analysis, early was defined as less than 48 h for vaginal and 96 h for cesarean delivery, which exceeds the average postnatal LOS in several developed countries [2,18]. Five of the included studies from Canada, Spain, Sweden, Switzerland, and the U.S. were published 15 or more years ago [2]. A single study from Egypt of cesarean deliveries only accounted for 86.9% of the readmissions [2]. A study by Hadley et al. found that a large and diverse population of healthy newborns, including over 57,000 born during the COVID-19 pandemic, were discharged earlier without an increase in readmission. This suggests that families and practitioners were appropriately assessing discharge readiness based upon the outcome of readmission. Time-based definitions of early discharge do not allow for individualization; therefore, discharge checklists may be a better assessment of optimal discharge timing for the mother-infant dyad [6].
Since the beginning of the COVID-19 pandemic, reasons for readmission remain similar, with jaundice, dehydration, and feeding difficulties being most common [4,22,26]. Hyperbilirubinemia was the most common, accounting for over 50% of rehospitalizations prior to and during the pandemic in both our study and in Handley et al. [22]. With the anticipated release of the updated AAP hyperbilirubinemia guideline, the number of readmissions for jaundice may decrease. Similar to a prior report, we found that readmissions due to documented or suspected infection decreased after the start of the pandemic [22]. This may be related to increased mask wearing, school closures, less travel, and heightened awareness and practice of infection prevention. The pandemic also brought changes in healthcare utilization as evidenced by delayed immunizations and other health maintenance [27]. We chose a 28-day readmission window to ensure that delays in seeking care did not mask readmission rates. We found no difference in time to readmission between the cohorts.
The reasons for increase in early newborn discharge since COVID-19 are unknown and can only be speculated on. Potential reasons for the increase include changes in labor and delivery unit policies, including visitor limitations, in order to reduce SARS-CoV-2 infection risk to patients and staff and/or parental concern for iatrogenic acquisition of COVID-19. Prior to the pandemic, our nursery postnatal LOS had already been decreasing. The reasons for this are multifactorial and have accompanied an increase in patient volumes. This may have led to changes in staff practice habits and families being aware that early discharge is possible. Three months prior to the pandemic, our institutional management of infants with suspected sepsis was updated to align with the AAP’s 2018 recommendations [28]. This was likely another contributing factor.
Social disadvantage and healthcare inequities disproportionately affect minorities [29]. Identifying and addressing such inequities is imperative. In the U.S. studies of changes in LOS during the pandemic, 43% to 61% of women were White [22,23,24]. In our study, almost two-thirds of infants were White. Additional studies involving a more diverse population are needed to assess any differences among ethnic groups, especially in larger metropolitan areas. Globally, studies in low-income countries, where infant and maternal mortality may be higher, are needed. In the 2021 Cochrane Review of early postnatal discharge, none of the evidence came from low-income countries [17].
5. Conclusions
Since the start of the COVID-19 pandemic, the number of newborns discharging early at 24 h or less has significantly increased without an increase in readmissions. In addition, overall postnatal length of stay has decreased. Potential explanations for these observations include changes in hospital and unit policies including visitor and labor support restrictions and parental concern about iatrogenic acquisition of COVID-19. In addition to rehospitalization, more trials exploring expanded outcomes including unplanned healthcare visits, breastfeeding rates, caregiver wellbeing, and timeliness of follow-up are needed.
Author Contributions
Conceptualization, Methodology, Investigation, Writing—Review & Editing: K.E.W., A.S. and G.B.; Writing-Original Draft Preparation, Visualization: K.E.W. and G.B.; Data curation, formal analysis, validation: G.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study received institutional review board (HawkIRB) approval (IRB ID. 202107147) on 14 July 2021.
Informed Consent Statement
Patient consent was waived due to study involving no more than minimal risk to the subjects or their privacy, waiver of consent would not adversely affect the subjects’ right and welfare, and lack of feasibility.
Data Availability Statement
The data presented in this study are available in in this article.
Acknowledgments
We thank the nursery personnel for care of the newborns described in this study. We thank Charles Grose for his mentorship.
Conflicts of Interest
Schmitz and Bhoojhawon have no conflict of interest relevant to this article to disclose. Wood receives royalties from McGraw Hill Professionals for a textbook she co-edited. That relationship did not influence the work presented.
References
- Datar, A.; Sood, N. Impact of Postpartum Hospital-Stay Legislation on Newborn Length of Stay, Readmission, and Mortality in California. Pediatrics 2006, 118, 63–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, E.; Taylor, B.; MacArthur, C.; Bradshaw, S.; Hope, L.; Cummins, C. Early Postnatal Discharge for Infants: A Meta-analysis. Pediatrics 2020, 146, e20193365. [Google Scholar] [CrossRef] [PubMed]
- Kotagal, U.R.; Atherton, H.D.; Eshett, R.; Schoettker, P.J.; Perlstein, P.H. Safety of Early Discharge for Medicaid Newborns. JAMA J. Am. Med. Assoc. 1999, 282, 1150–1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, I.M.; Lehman, E.B.; Hollenbeak, C.S.; Maisels, M.J. Preventable Newborn Readmissions Since Passage of the Newborns’ and Mothers’ Health Protection Act. Pediatrics 2006, 118, 2349–2358. [Google Scholar] [CrossRef] [PubMed]
- Committee on Fetus and Newborn. Hospital Stay for Healthy Term Newborns. Pediatrics 2004, 113, 1434–1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benitz, W.E.; Committee on Fetus and Newborn; Watterberg, K.L.; Aucott, S.; Benitz, W.E.; Cummings, J.J.; Eichenwald, E.C.; Goldsmith, J.; Poindexter, B.B.; Puopolo, K.; et al. Hospital Stay for Healthy Term Newborn Infants. Pediatrics 2015, 135, 948–953. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. 2014. Available online: https://apps.who.int/iris/handle/10665/97603 (accessed on 20 December 2021).
- U.S. Department of Labor. Newborns’ and Mothers’ Portections. Available online: https://www.dol.gov/general/topic/health-plans/newborns (accessed on 20 December 2021).
- Mosen, D.M.; Clark, S.L.; Mundorff, M.B.; Tracy, D.M.; McKnight, E.C.; Zollo, M.B. The medical and economic impact of the newborns’ and mothers’ health protection act. Obstet. Gynecol. 2002, 99, 116–124. [Google Scholar] [CrossRef]
- Watt, S.; Sword, W.; Krueger, P. Longer postpartum hospitalization options—Who stays, who leaves, what changes? BMC Pregnancy Childbirth 2005, 5, 13. [Google Scholar] [CrossRef] [Green Version]
- Norton, A.; Wilson, T.; Geller, G.; Gross, M.S. Impact of Hospital Visitor Restrictions on Racial Disparities in Obstetrics. Health Equity 2020, 4, 505–508. [Google Scholar] [CrossRef]
- Davis-Floyd, R.; Gutschow, K.; Schwartz, D.A. Pregnancy, Birth and the COVID-19 Pandemic in the United States. Med. Anthropol. 2020, 39, 413–427. [Google Scholar] [CrossRef]
- Altman, M.R.; Eagen-Torkko, M.K.; Mohammed, S.A.; Kantrowitz-Gordon, I.; Khosa, R.M.; Gavin, A.R. The impact of COVID-19 visitor policy restrictions on birthing communities of colour. J. Adv. Nurs. 2021, 77, 4827–4835. [Google Scholar] [CrossRef] [PubMed]
- Associated Press News. Iowa Governor Announces First 3 COVID-19 Cases in State. 2020. Available online: https://apnews.com/article/virus-outbreak-science-iowa-kim-reynolds-ia-state-wire-4fed9d219a5c62f884f4eae081ddfa9b (accessed on 20 December 2021).
- Campbel, M.J.; Swinscow, T. Statistics at Square One, 6th ed.; BMJ: London, UK, 2002. [Google Scholar]
- Jones, E.; Taylor, B.; MacArthur, C.; Pritchett, R.; Cummins, C. The effect of early postnatal discharge from hospital for women and infants: A systematic review protocol. Syst. Rev. 2016, 5, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, E.; Stewart, F.; Taylor, B.; Davis, P.G.; Brown, S.J. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst. Rev. 2021, 6, Cd002958. [Google Scholar] [CrossRef] [PubMed]
- Campbell, O.M.; Cegolon, L.; Macleod, D.; Benova, L. Length of Stay After Childbirth in 92 Countries and Associated Factors in 30 Low- and Middle-Income Countries: Compilation of Reported Data and a Cross-sectional Analysis from Nationally Representative Surveys. PLoS Med. 2016, 13, e1001972. [Google Scholar] [CrossRef] [Green Version]
- Farhat, R.; Rajab, M. Length of postnatal hospital stay in healthy newborns and re-hospitalization following early discharge. N. Am. J. Med. Sci. 2011, 3, 146–151. [Google Scholar] [CrossRef]
- Harriel, K.L.; Nolt, D.; Moore, S.; Kressly, S.; Bernstein, H.H. Management of neonates after postpartum discharge and all children in the ambulatory setting during the coronavirus disease 2019 (COVID-19) pandemic. Curr. Opin. Pediatr. 2020, 32, 610–618. [Google Scholar] [CrossRef]
- Metcalfe, A.; Mathai, M.; Liu, S.; Leon, J.A.; Joseph, K.S. Proportion of neonatal readmission attributed to length of stay for childbirth: A population-based cohort study. BMJ Open 2016, 6, e012007. [Google Scholar] [CrossRef]
- Handley, S.C.; Gallagher, K.; Breden, A.; Lindgren, E.; Lo, J.Y.; Son, M.; Murosko, D.; Dysart, K.; Lorch, S.A.; Greenspan, J.; et al. Birth Hospital Length of Stay and Rehospitalization During COVID-19. Pediatrics 2021, 149, e2021053498. [Google Scholar] [CrossRef]
- Greene, N.H.; Kilpatrick, S.J.; Wong, M.S.; Ozimek, J.A.; Naqvi, M. Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM 2020, 2, 100234. [Google Scholar] [CrossRef]
- Bornstein, E.; Gulersen, M.; Husk, G.; Grunebaum, A.; Blitz, M.J.; Rafael, T.J.; Rochelson, B.L.; Schwartz, B.; Nimaroff, M.; Chervenak, F.A. Early postpartum discharge during the COVID-19 pandemic. J. Perinat. Med. 2020, 48, 1008–1012. [Google Scholar] [CrossRef]
- Vazquez-Vazquez, A.; Dib, S.; Rougeaux, E.; Wells, J.C.; Fewtrell, M.S. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the UK: Preliminary data from the COVID-19 New Mum Study. Appetite 2021, 156, 104985. [Google Scholar] [CrossRef] [PubMed]
- Escobar, G.J.; Greene, J.D.; Hulac, P.; Kincannon, E.; Bischoff, K.; Gardner, M.N.; Armstrong, M.A.; France, E.K. Rehospitalisation after birth hospitalisation: Patterns among infants of all gestations. Arch. Dis. Child. 2005, 90, 125. [Google Scholar] [CrossRef] [PubMed]
- Dinleyici, E.C.; Borrow, R.; Safadi, M.A.P.; van Damme, P.; Munoz, F.M. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum. Vaccin. Immunother. 2021, 17, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Puopolo, K.M.; Benitz, W.E.; Zaoutis, T.E.; Committee on Fetus and Newborn; Committee on Infectious Diseases; Cummings, J.; Juul, S.; Hand, I.; Eichenwald, E.; Poindexter, B.; et al. Management of Neonates Born at ≥35 0/7 Weeks’ Gestation With Suspected or Proven Early-Onset Bacterial Sepsis. Pediatrics 2018, 142, e20182894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barfield, W.D. Social disadvantage and its effect on maternal and newborn health. Semin. Perinatol. 2021, 45, 151407. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).