A Descriptive Analysis of the Impact of COVID-19 on Emergency Department Attendance and Visit Characteristics in Singapore
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Source and Extraction
2.3. Patient Acuity Category Scale (PACS)
2.4. SNOMED CT to ICD-10-CM Conversion for ED Diagnosis
2.5. Statistical Analysis
3. Results
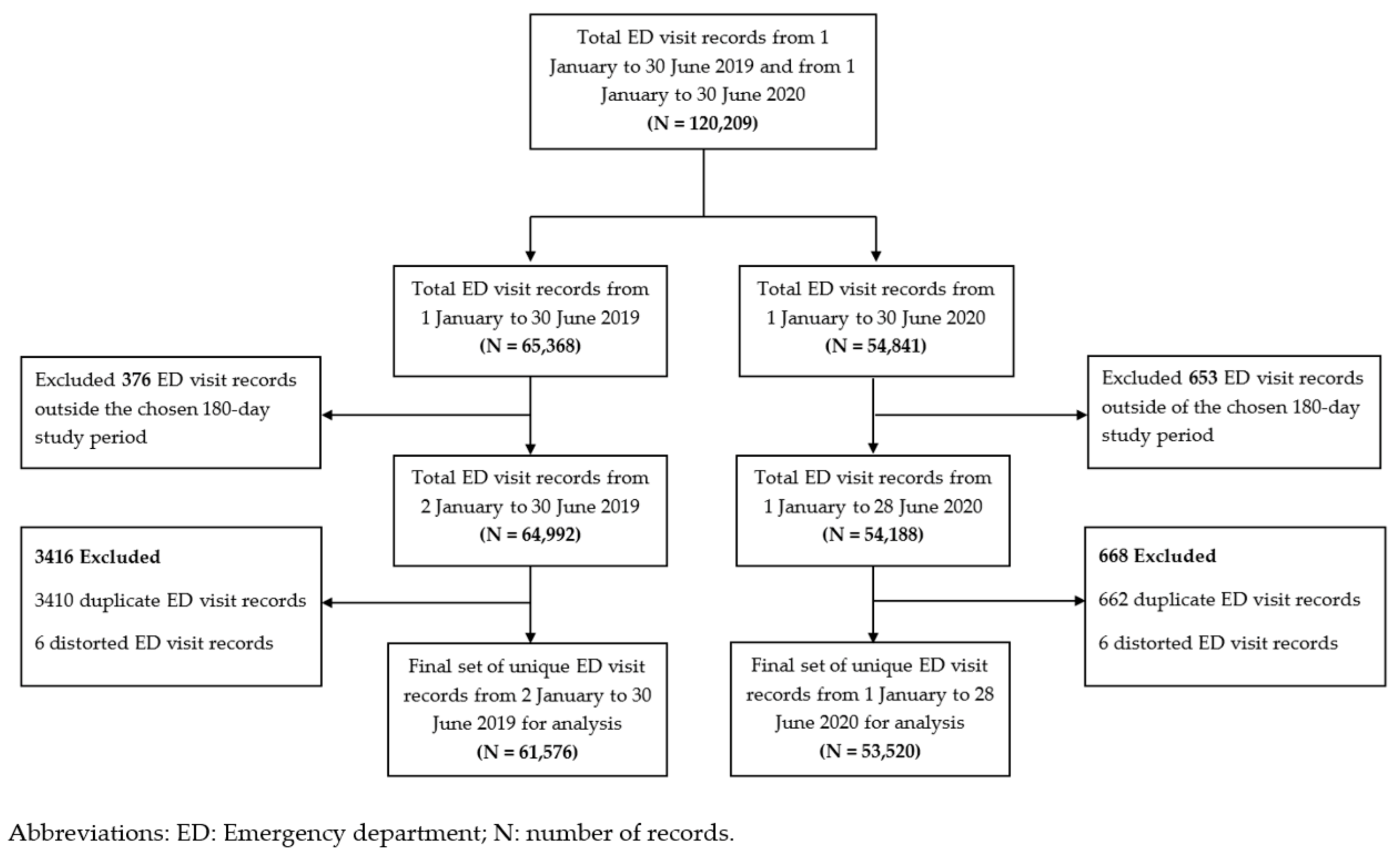
3.1. ED Visit Records Selected for the Analysis
3.2. Patient Demographics and Visit Characteristics
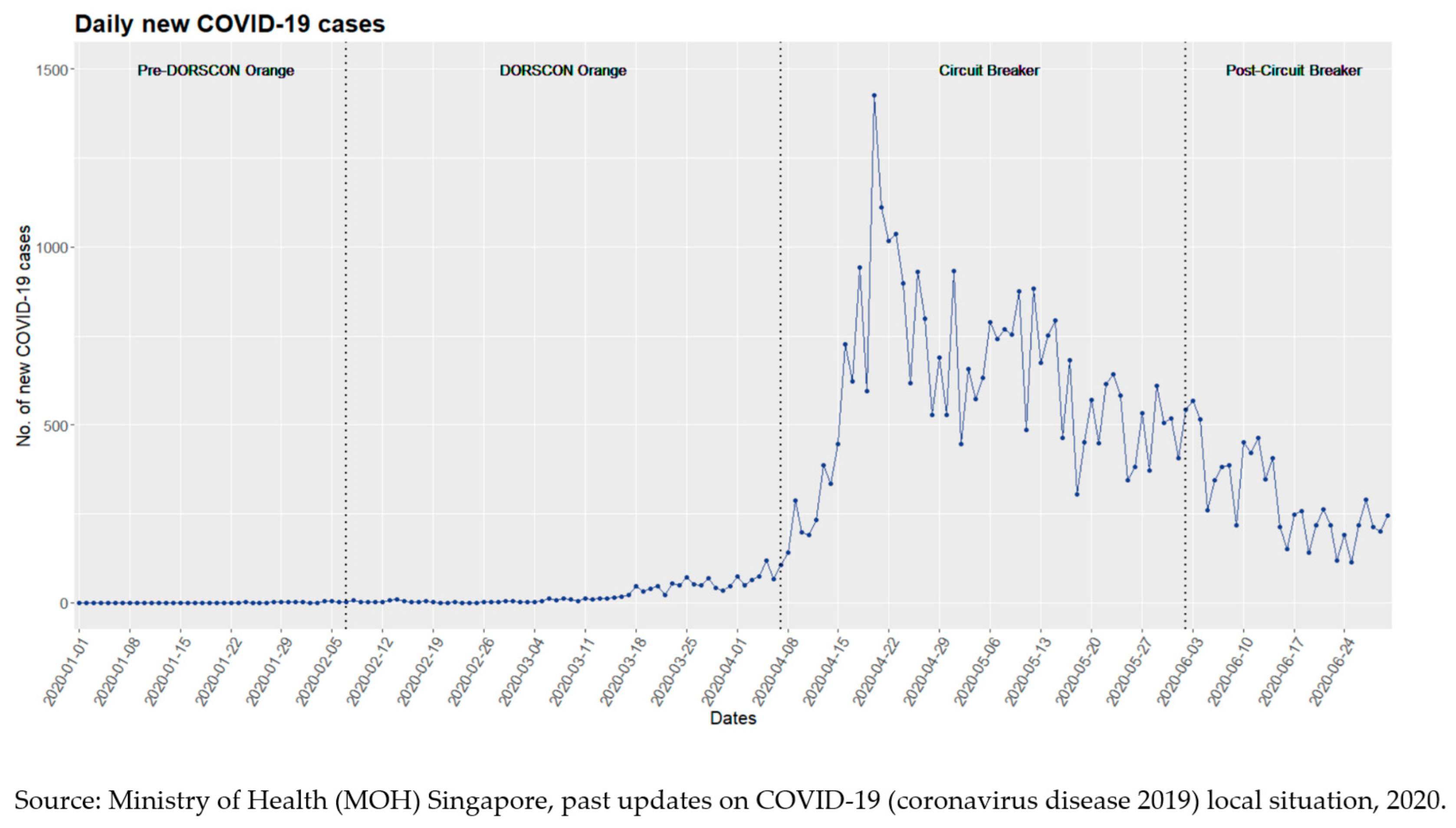
3.3. Two-Phase ED Attendance Trend
3.3.1. First Phase of the ED Attendance Trend
3.3.2. Second Phase of the ED Attendance Trend
3.4. Sub-Group Analysis of the ED Attendance by ‘Non-Fever’ and ‘Fever’ Triage Categories
3.5. Clinical Reasons for ED Attendance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V.; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, 1 January 2019–30 May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Cella, A.; Marchetti, F.; Iughetti, L.; Di Biase, A.R.; Graziani, G.; De Fanti, A.; Valletta, E.; Vaienti, F.; Vergine, G.; Viola, L.; et al. Italian COVID-19 Epidemic: Effects on Paediatric Emergency Attendance—A Survey in the Emilia Romagna Region. BMJ Paediatr. Open 2020, 4, e000742. [Google Scholar] [CrossRef] [PubMed]
- Leow, S.H.; Dean, W.; MacDonald-Nethercott, M.; MacDonald-Nethercott, E.; Boyle, A.A. The Attend Study: A Retrospective Observational Study of Emergency Department Attendances During the Early Stages of the COVID-19 Pandemic. Cureus 2020, 12, e9328. [Google Scholar] [CrossRef] [PubMed]
- Walline, J.H.; Song, P.P.; Lim, A.M.; Hung, K.K.; Graham, C.A. Hong Kong Emergency Department Attendance Plummets during COVID-19. Emerg. Med. Australas. 2020, 32, 1093–1094. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A.; et al. Potential Indirect Effects of the COVID-19 Pandemic on Use of Emergency Departments for Acute Life-Threatening Conditions—United States, January–May 2020. Am. J. Transplantation 2020, 20, 2612–2617. [Google Scholar] [CrossRef] [PubMed]
- Nagamine, M.; Chow, D.S.; Chang, P.D.; Boden-Albala, B.; Yu, W.; Soun, J.E. Impact of COVID-19 on Acute Stroke Presentation at a Comprehensive Stroke Center. Front. Neurol. 2020, 11, 850. [Google Scholar] [CrossRef] [PubMed]
- Khalik, S. Surge in Coronavirus Infections Strains Healthcare System. The Straits Times Singapore, 18 April 2020. [Google Scholar]
- What Do the Different DORSCON Levels Mean. Available online: http://www.gov.sg/article/what-do-the-different-dorscon-levels-mean (accessed on 15 August 2020).
- Shorey, S.; Ang, E.; Yamina, A.; Tam, C. Perceptions of Public on the COVID-19 Outbreak in Singapore: A Qualitative Content Analysis. J. Public Health 2020, 42, 665–671. [Google Scholar] [CrossRef] [PubMed]
- Comprehensive Medical Strategy for COVID-19. Available online: https://www.moh.gov.sg/news-highlights/details/comprehensive-medical-strategy-for-covid-19 (accessed on 15 August 2020).
- Tay, T.F. Coronavirus: Community Cases Remain Low but Singapore Should Prepare for Second Wave, Says Gan Kim Yong. The Straits Times Singapore, 17 July 2020. [Google Scholar]
- Singapore Starts Booster Shots as COVID Cases Hit 1-Year High. Available online: https://asia.nikkei.com/Spotlight/Coronavirus/COVID-vaccines/Singapore-starts-booster-shots-as-COVID-cases-hit-1-year-high (accessed on 14 September 2021).
- Govt Won’t Rule out Return to Circuit Breaker or Heightened Alert If COVID-19 Cases in ICUs Rise Sharply: Lawrence Wong. Available online: https://www.todayonline.com/singapore/govt-wont-rule-out-return-circuit-breaker-or-heightened-alert-if-covid-19-cases-icus-rise (accessed on 6 September 2021).
- Quah, L.J.J.; Tan, B.K.K.; Fua, T.-P.; Wee, C.P.J.; Lim, C.S.; Nadarajan, G.; Zakaria, N.D.; Chan, S.-E.J.; Wan, P.W.; Teo, L.T.; et al. Reorganising the Emergency Department to Manage the COVID-19 Outbreak. Int. J. Emerg. Med. 2020, 13, 32. [Google Scholar] [CrossRef] [PubMed]
- Fong, R.Y.; Glen, W.S.S.; Mohamed Jamil, A.K.; Tam, W.W.S.; Kowitlawakul, Y. Comparison of the Emergency Severity Index versus the Patient Acuity Category Scale in an Emergency Setting. Int. Emerg. Nurs. 2018, 41, 13–18. [Google Scholar] [CrossRef] [PubMed]
- SNOMED CT to ICD-10-CM Map. Available online: https://www.nlm.nih.gov/research/umls/mapping_projects/snomedct_to_icd10cm.html (accessed on 27 September 2020).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 30 April 2020).
- Past Updates on COVID-19 Local Situation. Available online: https://www.moh.gov.sg/covid-19/past-updates (accessed on 15 August 2020).
- Singaporeans Are Confident in the Government Amidst Fears of the COVID-19 Outbreak. Available online: https://www.ipsos.com/en-sg/singaporeans-are-confident-government-amidst-fears-covid-19-outbreak (accessed on 16 August 2020).
- Wong, L.E.; Hawkins, J.E.; Langness, S.; Iris, P.; Sammann, A. Where Are All the Patients? Addressing Covid-19 Fear to Encourage Sick Patients to Seek Emergency Care. NEJM Catalyst Innov. Care Deliv. 2020, 1, 1–12. [Google Scholar] [CrossRef]
- Lin, R.J.; Lee, T.H.; Lye, D.C. From SARS to COVID-19: The Singapore journey. Med. J. Aust. 2020, 212, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishna, G.; Choo, P.; Leo, Y.S.; Tay, B.K.; Lim, Y.T.; Khan, A.S.; Tan, C.C. SARS transmission and hospital containment. Emerg. Infect. Dis. 2004, 10, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.W.X.; Coleman, K.K.; Chia, P.Y.; Thoon, K.C.; Pada, S.; Venkatachalam, I.; Fisher, D.; Tan, Y.K.; Tan, B.H.; Ng, O.T.; et al. Transmission modes of severe acute respiratory syndrome coronavirus 2 and implications on infection control: A review. Singap. Med. J. 2020, 1, 21. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.É.; Marynak, K.; Clarke, K.E.N.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns—United States, June 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef] [PubMed]
- Inside Singapore’s COVID-19 Screening Centre, on the Front Line against the Disease. Available online: https://www.channelnewsasia.com/cnainsider/inside-singapore-covid-19-screening-centre-defence-disease-ncid-765381 (accessed on 19 April 2020).
- Stretched but Coping: How Singapore’s Healthcare System Has Cranked up Efforts to Deal with COVID-19. Available online: https://www.channelnewsasia.com/singapore/covid-19-singapore-health-capacity-hospitals-treatment-935336 (accessed on 4 May 2020).

| Time Periods Studied | Pre-COVID-19 Period | COVID-19 Period | % Change in ED Attendances Compared with the Pre-COVID-19 Period |
|---|---|---|---|
| 2 January–30 June 2019 | 1 January–28 June 2020 | ||
| Total number of ED visits | 61,576 | 53,520 | −8056 (−13.1%) |
| Mean ED attendance (SD, range) | 342 (44.9, 277–427) | 297 (31.8, 207–445) | |
| Demographics | N (%) | N (%) | |
| Gender | |||
| Male | 31,707 (51.5%) | 28,942 (54.1%) | −2765 (−8.7%) |
| Female | 29,869 (48.5%) | 24,578 (45.9%) | −5291 (−17.7%) |
| Age (year) | |||
| Median (Q1–Q3, range) | 56 (36–70, 0–106) | 55 (35–70, 0–105) | |
| 0–10 | 386 (0.6%) | 216 (0.4%) | −170 (−44.0%) |
| 11–14 | 213 (0.3%) | 108 (0.2%) | −105 (−49.3%) |
| 15–24 | 5172 (8.4%) | 3970 (7.4%) | −1202 (−23.2%) |
| 25–34 | 8448 (13.7%) | 8407 (15.7%) | −41 (−0.5%) |
| 35–44 | 7008 (11.4%) | 6916 (12.9%) | −92 (−1.3%) |
| 45–54 | 7856 (12.8%) | 6757 (12.6%) | −1099 (−14.0%) |
| 55–64 | 10,736 (17.4%) | 8884 (16.6%) | −1852 (−17.3%) |
| ≥65 | 21,757 (35.3%) | 18,261 (34.1%) | −3496 (−16.1%) |
| Missing | 0 | 1 | |
| Citizenship status | |||
| Singapore citizen | 49,592 (80.5%) | 41,099 (76.8%) | −8493 (−17.1%) |
| Non-citizen | 11,984 (19.5%) | 12,421 (23.2%) | +437 (+3.6%) |
| Ethnicity | |||
| Chinese | 39,663 (64.4%) | 33,137 (61.9%) | −6525 (−16.5%) |
| Indian | 8034 (13.0%) | 7605 (14.2%) | −429 (−5.3%) |
| Malay | 6603 (10.7%) | 5811 (10.9%) | −792 (−12.0%) |
| Others | 7276 (11.8%) | 6967 (13.0%) | −309 (−4.2%) |
| Visit characteristics | N (%) | N (%) | |
| Mode of arrival | |||
| Non-ambulance | 52,585 (85.4%) | 43,239 (80.8%) | −9346 (−17.8%) |
| SCDF ambulance | 6432 (10.4%) | 7384 (13.8%) | +952 (+14.8%) |
| Private ambulance | 2559 (4.2%) | 2897 (5.4%) | +338 (+13.2%) |
| Patient acuity category status | |||
| P1 | 9049 (14.7%) | 5336 (10.0%) | −3713 (−41.0%) |
| P2 | 33,550 (54.5%) | 28,608 (53.5%) | −4942 (−14.7%) |
| P3 | 16,874 (27.4%) | 10,486 (19.6%) | −6388 (−37.9%) |
| P4 | 345 (0.6%) | 138 (0.3%) | −207 (−60.0%) |
| P1F | 144 (0.2%) | 178 (0.3%) | +34 (+23.6%) |
| P2F | 714 (1.2%) | 1138 (2.1%) | +424 (+59.4%) |
| P3F | 900 (1.5%) | 7636 (14.3%) | +6736 (+748.4%) |
| Disposition | |||
| Admitted from ED | 25,422 (41.3%) | 23,422 (43.8%) | −2000 (−7.9%) |
| General ward | 21,958 (86.4%) | 20,000 (85.4%) | −1958 (−8.9%) |
| High dependency ward | 1190 (4.7%) | 872 (3.7%) | −318 (−26.7%) |
| Intermediate care area | 387 (1.5%) | 231 (1.0%) | −156 (−40.3%) |
| Intensive care unit | 372 (1.5%) | 302 (1.3%) | −70 (−18.8%) |
| Infectious disease/isolation ward | 857 (3.4%) | 1891 (8.1%) | +1034 (+120.7%) |
| Unknown | 658 (2.6%) | 126 (0.5%) | −532 (−80.9%) |
| Not admitted | 36,126 (58.7%) | 30,054 (56.2%) | −6072 (−16.8%) |
| Missing | 28 | 44 |
| Time Periods Studied | Pre-COVID-19 Period | COVID-19 Period | % Change in Frequency Compared with the Pre-COVID-19 Period |
|---|---|---|---|
| 2 January–30 June 2019 | 1 January–28 June 2020 | ||
| Total number of ED visits | 61,576 | 53,520 | |
| Number of ED visits with ≥1 recorded diagnosis | 60,166 | 52,385 | |
| Total number of documented diagnoses | 73,545 (100%) | 67,444 (100%) | |
| ICD-10-CM diagnosis categories | N (% total documented diagnoses) | N (% total documented diagnoses) | |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 19,196 (25.5%) | 16,883 (24.5%) | −2313 (−12.0%) |
| Injury, poisoning and certain other consequences of external causes | 9358 (12.5%) | 6779 (9.9%) | −2579 (−27.6%) |
| Diseases of the musculoskeletal system and connective tissue | 5932 (7.9%) | 3995 (5.8%) | −1937 (−32.7%) |
| Diseases of the circulatory system | 5810 (7.7%) | 4723 (6.9%) | −1087 (−18.7%) |
| Diseases of the respiratory system | 5594 (7.4%) | 11,842 (17.2%) | +6248 (+111.7%) |
| Diseases of the digestive system | 4971 (6.6%) | 4367 (6.4%) | −604 (−12.2%) |
| Diseases of the genitourinary system | 3821 (5.1%) | 3141 (4.6%) | −680 (−17.8%) |
| Certain infectious and parasitic diseases | 3799 (5.1%) | 3095 (4.5%) | −704 (−18.5%) |
| Endocrine, nutritional and metabolic diseases | 2976 (4.0%) | 2735 (4.0%) | −241 (−8.1%) |
| Diseases of the skin and subcutaneous tissue | 2937 (3.9%) | 2360 (3.4%) | −577 (−19.6%) |
| Diseases of the eye and adnexa | 2493 (3.3%) | 1805 (2.6%) | −688 (−27.6%) |
| Diseases of the nervous system | 1265 (1.7%) | 1074 (1.6%) | −191 (−15.1%) |
| Neoplasms | 1227 (1.6%) | 1069 (1.6%) | −158 (−12.9%) |
| Mental, behavioural and neurodevelopmental disorders | 1012 (1.3%) | 899 (1.3%) | −113 (−11.2%) |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 943 (1.3%) | 860 (1.2%) | −83 (−8.8%) |
| External causes of morbidity | 699 (0.9%) | 636 (0.9%) | −63 (−9.0%) |
| Diseases of the ear and mastoid process | 640 (0.9%) | 537 (0.8%) | −103 (−16.1%) |
| Factors influencing health status and contact with health services | 557 (0.7%) | 405 (0.6%) | −152 (−27.3%) |
| Pregnancy, childbirth and the puerperium | 220 (0.3%) | 174 (0.3%) | −46 (−20.9%) |
| Congenital malformations, deformations and chromosomal abnormalities | 62 (0.1%) | 36 (0.1%) | −26 (−41.9%) |
| Certain conditions originating in the perinatal period | 33 (0.0%) | 29 (0.0%) | −4 (−12.1%) |
| Total number of P1 visits | 9049 | 5336 | |
| Number of P1 visits with ≥1 recorded diagnosis | 9012 | 5313 | |
| Total number of recorded diagnoses | 11,510 (100%) | 7519 (100%) | |
| ICD-10-CM diagnosis categories | N (% total documented diagnoses) | N (% total documented diagnoses) | |
| Severe diseases | |||
| Stroke | 704 (6.1%) | 516 (6.9%) | −188 (−26.7%) |
| Acute myocardial infarction | 508 (4.4%) | 440 (5.9%) | −68 (−13.4%) |
| STEMI | 226 (2.0%) | 187 (2.5%) | −39 (−17.3%) |
| NSTEMI | 282 (2.5%) | 253 (3.4%) | −29 (−10.3%) |
| Other acute ischemic heart diseases | 109 (0.9%) | 95 (1.3%) | −14 (−12.8%) |
| Heart failure | 337 (2.9%) | 231 (3.1%) | −106 (−31.5%) |
| Cardiac arrest | 92 (0.8%) | 102 (1.4%) | +10 +(10.9%) |
| Paralytic ileus and intestinal obstruction without hernia | 337 (2.9%) | 277 (3.7%) | −60 (−17.8%) |
| Appendicitis | 173 (1.5%) | 157 (2.1%) | −16 (−9.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, M.Q.; Saffari, S.E.; Ho, A.F.W.; Liew, J.N.M.H.; Tan, B.K.K.; Sim, N.S.; Shen, Y.; Siddiqui, F.J.; Ong, M.E.H. A Descriptive Analysis of the Impact of COVID-19 on Emergency Department Attendance and Visit Characteristics in Singapore. COVID 2021, 1, 739-750. https://doi.org/10.3390/covid1040059
Lim MQ, Saffari SE, Ho AFW, Liew JNMH, Tan BKK, Sim NS, Shen Y, Siddiqui FJ, Ong MEH. A Descriptive Analysis of the Impact of COVID-19 on Emergency Department Attendance and Visit Characteristics in Singapore. COVID. 2021; 1(4):739-750. https://doi.org/10.3390/covid1040059
Chicago/Turabian StyleLim, Mei Qiu, Seyed Ehsan Saffari, Andrew Fu Wah Ho, Johannes Nathaniel Min Hui Liew, Boon Kiat Kenneth Tan, Nicole Simin Sim, Yuzeng Shen, Fahad Javaid Siddiqui, and Marcus Eng Hock Ong. 2021. "A Descriptive Analysis of the Impact of COVID-19 on Emergency Department Attendance and Visit Characteristics in Singapore" COVID 1, no. 4: 739-750. https://doi.org/10.3390/covid1040059
APA StyleLim, M. Q., Saffari, S. E., Ho, A. F. W., Liew, J. N. M. H., Tan, B. K. K., Sim, N. S., Shen, Y., Siddiqui, F. J., & Ong, M. E. H. (2021). A Descriptive Analysis of the Impact of COVID-19 on Emergency Department Attendance and Visit Characteristics in Singapore. COVID, 1(4), 739-750. https://doi.org/10.3390/covid1040059









