Brucella Diagnostics in Endemic Areas: Evaluation of Point-of-Care Kits and the Need for Alternative Diagnostic Tests
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Samples and Testing Procedures
2.3. Training and Capacity Building
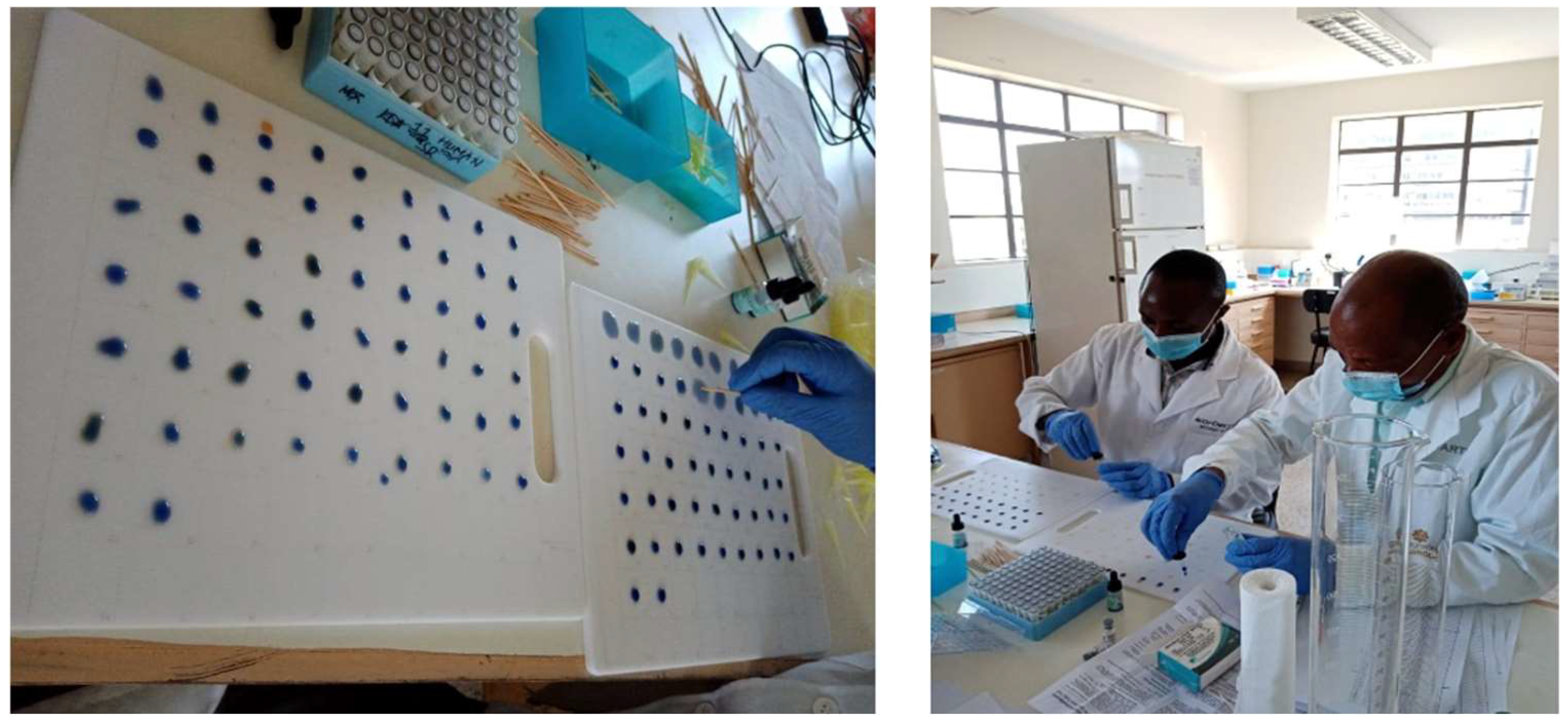
- Sample selection and blinding: Use of 100 ELISA-positive and 100 ELISA-negative samples, blinded to the operator. The serum samples were allowed to thaw at room temperature before analysis, and the test kits’ reagents were removed from the refrigerator and allowed to attain room temperature. A plastic board with a white background was used because of the many samples to be tested (Figure 1).
- The routine qualitative procedure, as detailed in the kit’s inserts, was strictly adhered to and is summarized as follows:
- Two areas of the demarcated board were labelled positive and negative. The other regions were labelled with the unique serum sample numbers, ensuring each sample had a pair representation, including the labels ‘A’ for abortus and ‘M’ for melitensis.
- 50 μL of the paired serum samples were put in areas labelled A and B with their respective unique sample numbers.
- A drop of the antigen was added to the serum samples and mixed using an applicator stick.
- The whiteboard was then manually rocked and observed for agglutination over a period, as indicated in the manufacturer’s kit insert.
2.4. Data Processing and Statistical Analyses
3. Results
4. Discussion and Conclusions
- Adopt and scale up the use of validated alternatives such as the Rose Bengal test, where culture and molecular diagnostics are unavailable.
- Invest in molecular diagnostic platforms, including LAMP, alongside structured laboratory training for in-country validation.
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FBAT | Febrile Brucella Agglutination Test |
| FN | False Negative |
| FP | False Positive |
| TN | True Negative |
| TP | True Positive |
| CI | Confidence Interval |
References
- Dagnaw, G.G.; Mamuye, Y.; Dejene, H. Human and animal brucellosis and risk factors for human infection in Ethiopia: A systematic review and meta-analysis (2015–2024). BMC Public Health 2024, 24, 3495. [Google Scholar] [CrossRef]
- Mwatondo, A.; Muturi, M.; Akoko, J.; Nyamota, R.; Nthiwa, D.; Maina, J.; Omolo, J.; Gichuhi, S.; Mureithi, M.W.; Bett, B. Seroprevalence and related risk factors of Brucella spp. in livestock and humans in Garbatula subcounty, Isiolo county, Kenya. PLoS Negl. Trop. Dis. 2023, 17, e0011682. [Google Scholar] [CrossRef]
- Munyua, P.; Bitek, A.; Osoro, E.; Pieracci, E.G.; Muema, J.; Mwatondo, A.; Kungu, M.; Nanyingi, M.; Gharpure, R.; Njenga, K.; et al. Prioritization of Zoonotic Diseases in Kenya, 2015. PLoS ONE 2016, 11, e0161576. [Google Scholar] [CrossRef]
- Akoko, J.M.; Mwatondo, A.; Muturi, M.; Wambua, L.; Abkallo, H.M.; Nyamota, R.; Bosire, C.; Oloo, S.; Limbaso, K.S.; Gakuya, F.; et al. Mapping brucellosis risk in Kenya and its implications for control strategies in sub-Saharan Africa. Sci. Rep. 2023, 13, 20192. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.B.; Khatkar, M.S.; Aulakh, R.S.; Gill, J.P.S.; Dhand, N.K. Estimation of the health and economic burden of human brucellosis in India. Prev. Vet. Med. 2018, 154, 148–155. [Google Scholar] [CrossRef]
- Kiiza, D.; Denagamage, T.; Serra, R.; Maunsell, F.; Kiker, G.; Benavides, B.; Hernandez, J.A. A systematic review of economic assessments for brucellosis control interventions in livestock populations. Prev. Vet. Med. 2023, 213, 105878. [Google Scholar] [CrossRef] [PubMed]
- Freire, M.L.; Machado de Assis, T.S.; Silva, S.N.; Cota, G. Diagnosis of human brucellosis: Systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2024, 181, e0012030. [Google Scholar] [CrossRef] [PubMed]
- Dadar, M.; Al-Khaza’leh, J.; Fakhri, Y.; Akar, K.; Ali, S.; Shahali, Y. Human brucellosis and associated risk factors in the Middle East region: A comprehensive systematic review, meta-analysis, and meta-regression. Heliyon 2024, 10, e34324. [Google Scholar] [CrossRef]
- Lokamar, P.N.; Kutwah, M.A.; Munde, E.O.; Oloo, D.; Atieli, H.; Gumo, S.; Akoko, J.M.; Ouma, C. Prevalence of brucellosis in livestock keepers and domestic ruminants in Baringo County, Kenya. PLOS Glob. Public Health 2022, 2, e0000682. [Google Scholar] [CrossRef]
- Kiambi, S.G.; Fèvre, E.M.; Omolo, J.; Oundo, J.; de Glanville, W.A. Risk factors for acute human brucellosis in Ijara, north-eastern Kenya. PLoS Negl. Trop. Dis. 2020, 14, e0008108. [Google Scholar] [CrossRef]
- Njeru, J.; Wareth, G.; Melzer, F.; Henning, K.; Pletz, M.W.; Heller, R.; Neubauer, H. Systematic review of brucellosis in Kenya: Disease frequency in humans and animals and risk factors for human infection. BMC Public Health 2016, 16, 853. [Google Scholar] [CrossRef]
- Rahman, M.T.; Sobur, M.A.; Islam, M.S.; Ievy, S.; Hossain, M.J.; El Zowalaty, M.E.; Rahman, A.T.; Ashour, H.M. Zoonotic Diseases: Etiology, Impact, and Control. Microorganisms 2020, 8, 1405. [Google Scholar] [CrossRef]
- Pereira, C.R.; Cotrim de Almeida, J.V.F.; Cardoso de Oliveira, I.R.; Faria de Oliveira, L.; Pereira, L.J.; Zangerônimo, M.G.; Lage, A.P.; Dorneles, E.M.S. Occupational exposure to Brucella spp.: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2020, 14, e0008164. [Google Scholar] [CrossRef]
- Waringa, N.M.A.; Waiboci, L.W.; Bebora, L.; Kinyanjui, P.W.; Kosgei, P.; Kiambi, S.; Osoro, E. Human brucellosis in Baringo County, Kenya: Evaluating the diagnostic kits used and identifying infecting Brucella species. PLoS ONE 2023, 18, e0269831. [Google Scholar] [CrossRef]
- de Glanville, W.A.; Conde-Álvarez, R.; Moriyón, I.; Njeru, J.; Díaz, R.; Cook, E.A.J.; Morin, M.; Bronsvoort, B.M.D.C.; Thomas, L.F.; Kariuki, S.; et al. Poor performance of the rapid test for human brucellosis in health facilities in Kenya. PLoS Negl. Trop. Dis. 2017, 11, e0005508. [Google Scholar] [CrossRef] [PubMed]
- Alumasa, L.; Thomas, L.F.; Amanya, F.; Njoroge, S.M.; Moriyón, I.; Makhandia, J.; Rushton, J.; Fèvre, E.M.; Falzon, L.C. Hospital-based evidence on cost-effectiveness of brucellosis diagnostic tests and treatment in Kenyan hospitals. PLoS Negl. Trop. Dis. 2021, 15, e0008977. [Google Scholar] [CrossRef]
- Vered, O.; Simon-Tuval, T.; Yagupsky, P.; Malul, M.; Cicurel, A.; Davidovitch, N. The Price of a Neglected Zoonosis: Case-Control Study to Estimate Healthcare Utilization Costs of Human Brucellosis. PLoS ONE 2015, 10, e0145086. [Google Scholar] [CrossRef] [PubMed]
- Lukambagire, A.S.; Mendes, Â.J.; Bodenham, R.F.; McGiven, J.A.; Mkenda, N.A.; Mathew, C.; Rubach, M.P.; Sakasaka, P.; Shayo, D.D.; Maro, V.P.; et al. Performance characteristics and costs of serological tests for brucellosis in a pastoralist community of northern Tanzania. Sci. Rep. 2021, 11, 5480. [Google Scholar] [CrossRef]
- McNemar, Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 1947, 12, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Fagerland, M.W.; Lydersen, S.; Laake, P. The McNemar test for binary matched-pairs data: Mid-p and asymptotic are better than exact conditional. BMC Med. Res. Methodol. 2013, 13, 91. [Google Scholar] [CrossRef]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.M.; Lijmer, J.G.; Moher, D.; Rennie, D.; de Vet, H.C.; et al. Standards for Reporting of Diagnostic Accuracy. Towards complete and accurate reporting of studies of diagnostic accuracy: The STARD initiative. Standards for Reporting of Diagnostic Accuracy. Clin. Chem. 2003, 49, 1–6. [Google Scholar] [CrossRef]
- Brown, N.; Wilson, G. Ten quick tips for teaching programming. PLoS Comput. Biol. 2018, 14, e1006023. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Li, M.; Gao, Q.; Yu, T. Kappa statistic considerations in evaluating inter-rater reliability between two raters: Which, when and context matters. BMC Cancer 2023, 23, 799. [Google Scholar] [CrossRef]
- Power, M.; Fell, G.; Wright, M. Principles for high-quality, high-value testing. Evid. Based Med. 2013, 18, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Wang, W.; Chen, F.; Li, W.; Wang, G. ELISA is superior to bacterial culture and agglutination test in the diagnosis of brucellosis in an endemic area in China. BMC Infect. Dis. 2020, 20, 11. [Google Scholar] [CrossRef]
- Di Bonaventura, G.; Angeletti, S.; Ianni, A.; Petitti, T.; Gherardi, G. Microbiological Laboratory Diagnosis of Human Brucellosis: An Overview. Pathogens 2021, 10, 1623. [Google Scholar] [CrossRef] [PubMed]
- Loubet, P.; Magnan, C.; Salipante, F.; Pastre, T.; Keriel, A.; O’Callaghan, D.; Sotto, A.; Lavigne, J.P. Diagnosis of brucellosis: Combining tests to improve performance. PLoS Negl. Trop. Dis. 2024, 18, e0012442. [Google Scholar] [CrossRef]
- Macharia, Z.; Ogoti, B.; Otieno, M.; Gitonga, P.; Bosco-Lauth, A.; Maritim, M.; Lemarkoko, E.; Keya, A.; Sankok, J.; Gitao, G.; et al. Transmission of SARS-CoV-2 among underserved pastoralist communities in Kajiado County, Kenya: 2020–2022. PLoS ONE 2024, 19, e0308318. [Google Scholar] [CrossRef] [PubMed]
- Hajia, M.; Fallah, F.; Angoti, G.; Karimi, A.; Rahbar, M.; Gachkar, L.; Mokhtari, B.; Sanaei, A.; Lari, A.R. Comparison of methods for diagnosing brucellosis. Lab. Med. 2013, 44, 29–33. [Google Scholar] [CrossRef]
- Moeini-Zanjani, A.; Pournajaf, A.; Ferdosi-Shahandashti, E.; Gholami, M.; Masjedian, F.; Khafri, S.; Rajabnia, R. Comparison of loop-mediated isothermal amplification and conventional PCR tests for diagnosis of common Brucella species. BMC Res. Notes 2020, 13, 533. [Google Scholar] [CrossRef] [PubMed]
- Karthik, K.; Rathore, R.; Thomas, P.; Arun, T.R.; Viswas, K.N.; Agarwal, R.K.; Manjunathachar, H.; Dhama, K. Loop-mediated isothermal amplification (LAMP) test for specific and rapid detection of Brucella abortus in cattle. Vet. Q. 2014, 34, 174–179. [Google Scholar] [CrossRef] [PubMed]
| Source of Kit | Product Description | Controls Provided | Diagnostic Performance Claims |
|---|---|---|---|
| Atlas Medical | Lot 19072705/Ref 8.01.15.1.0010 | Yes | Sensitivity: 100%. Specificity: 98% |
| Accucare (Lab-Care Diagnostics) | Lot BAM 200101 Ref-Not Available | No | 70% specificity and sensitivity |
| Expert Diagnostics | Lot 20062203 Ref FA-16.0010 | Yes | Not indicated in the insert |
| Shubam Diagnostics | Lot BAM 200302 Ref-Not Available | No | Not indicated in the insert |
| Fortress Diagnostics Limited | Lot FC-1904-4 Ref FEBAMP05 | Yes | Not indicated in the insert |
| ELISA Test Result | FBAT Positive for Either B. abortus or B. melitensis | FBAT Negative for Both B. abortus and B. melitensis |
| Positive | True positive | False negative |
| Negative | False positive | True negative |
| FBAT Kit * | FN | FP | TN | TP | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| Atlas | 32 | 38 | 62 | 68 | 0.68 | 0.62 |
| Expert | 55 | 32 | 68 | 45 | 0.45 | 0.68 |
| Fortress | 38 | 77 | 23 | 62 | 0.62 | 0.23 |
| Shubham | 59 | 37 | 63 | 41 | 0.41 | 0.63 |
| Labcare | 49 | 45 | 55 | 51 | 0.51 | 0.55 |
| FBAT Kit | Sensitivity (95% CI) | Specificity (95% CI) | McNemar p-Value |
|---|---|---|---|
| Atlas | 0.68 (0.58–0.76) | 0.62 (0.52–0.71) | 0.550 |
| Labcare | 0.51 (0.41–0.61) | 0.56 (0.46–0.66) | 0.678 |
| Expert | 0.45 (0.35–0.55) | 0.68 (0.58–0.77) | 0.018 * |
| Shubham | 0.41 (0.31–0.51) | 0.63 (0.53–0.72) | 0.032 * |
| Fortress | 0.62 (0.52–0.71) | 0.23 (0.15–0.33) | 0.0004 * |
| FBAT Kit | Cohen’s Kappa (95% CI) | p-Value |
|---|---|---|
| Atlas | 0.30 (0.18–0.42) | 0.0003 * |
| Labcare | 0.07 (−0.05–0.19) | 0.25 |
| Expert | 0.14 (0.02–0.26) | 0.08 |
| Shubham | 0.04 (−0.008–0.16) | 0.39 |
| Fortress | −0.15 (−0.27–0.03) | 0.91 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keya, A.; Gitonga, P.; Wanjohi, D.; Lemarkoko, E.; Sankok, J.; Ogoti, B.; Bosco-Lauth, A.; Maritim, M.; Gitao, G.; Onono, J.; et al. Brucella Diagnostics in Endemic Areas: Evaluation of Point-of-Care Kits and the Need for Alternative Diagnostic Tests. Appl. Microbiol. 2025, 5, 104. https://doi.org/10.3390/applmicrobiol5040104
Keya A, Gitonga P, Wanjohi D, Lemarkoko E, Sankok J, Ogoti B, Bosco-Lauth A, Maritim M, Gitao G, Onono J, et al. Brucella Diagnostics in Endemic Areas: Evaluation of Point-of-Care Kits and the Need for Alternative Diagnostic Tests. Applied Microbiology. 2025; 5(4):104. https://doi.org/10.3390/applmicrobiol5040104
Chicago/Turabian StyleKeya, Aggrey, Pauline Gitonga, Daniel Wanjohi, Esther Lemarkoko, Joseph Sankok, Brian Ogoti, Angela Bosco-Lauth, Marybeth Maritim, George Gitao, Joshua Onono, and et al. 2025. "Brucella Diagnostics in Endemic Areas: Evaluation of Point-of-Care Kits and the Need for Alternative Diagnostic Tests" Applied Microbiology 5, no. 4: 104. https://doi.org/10.3390/applmicrobiol5040104
APA StyleKeya, A., Gitonga, P., Wanjohi, D., Lemarkoko, E., Sankok, J., Ogoti, B., Bosco-Lauth, A., Maritim, M., Gitao, G., Onono, J., Oyugi, J., & Bowen, R. (2025). Brucella Diagnostics in Endemic Areas: Evaluation of Point-of-Care Kits and the Need for Alternative Diagnostic Tests. Applied Microbiology, 5(4), 104. https://doi.org/10.3390/applmicrobiol5040104







