State Anxiety in People Living with Disability and Visual Impairment during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Participants and Procedure
2.3. Analysis
3. Results
3.1. Participant Characteristics
3.2. Subgroup Differences in State Anxiety
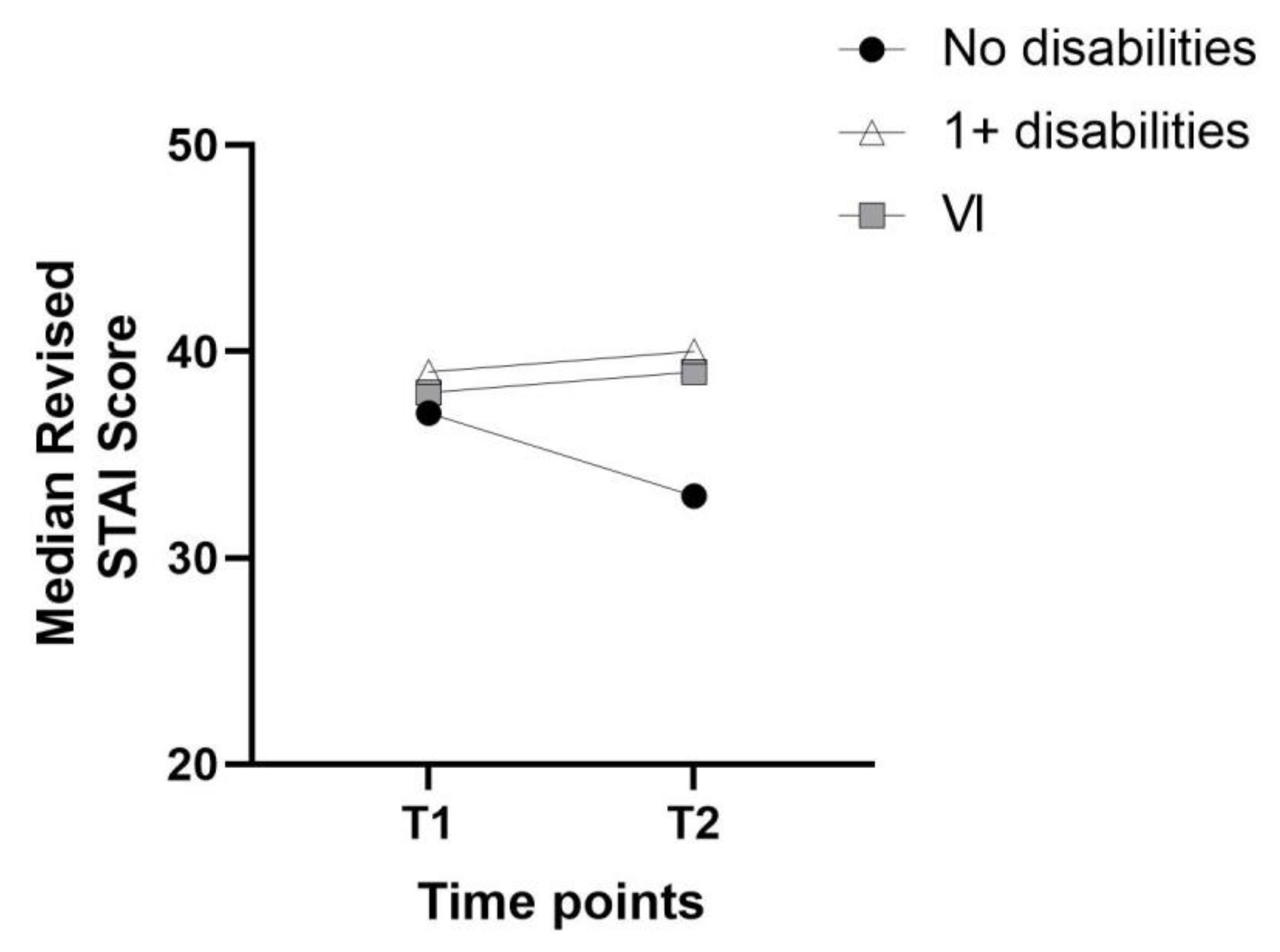
3.3. Changes in State Anxiety over Time
3.4. Factors Predicting State Anxiety
4. Discussion
Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schimmenti, A.; Billieux, J.; Starcevic, V. The four horsemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clin. Neuropsychiatry 2020, 17, 41–45. [Google Scholar] [PubMed]
- Pedrosa, A.L.; Bitencourt, L.; Fróes, A.C.F.; Cazumbá, M.L.B.; Campos, R.G.B.; de Brito, S.B.C.S.; Silva, A.C.S. Emotional, behavioral, and psychological Impact of the COVID-19 Pandemic. Front. Psychol. 2020, 11, 566212. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.M.; Lee, J.; Fitzgerald, H.N.; Oosterhoff, B.; Sevi, B.; Shook, N.J. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J. Occup. Environ. Med. 2020, 62, 686–691. [Google Scholar] [CrossRef] [PubMed]
- McDowell, C.P.; Herring, M.P.; Lansing, J.; Brower, C.S.; Meyer, J.D. Associations between employment changes and mental health: US data from during the COVID-19 pandemic. Front. Psychol. 2021, 12, 631510. [Google Scholar] [CrossRef] [PubMed]
- Malesza, M.; Kaczmarek, M.C. Predictors of anxiety during the COVID-19 pandemic in Poland. Pers. Individ. Dif. 2021, 170, 110419. [Google Scholar] [CrossRef] [PubMed]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Bu, F.; Mak, H.W.; Paul, E.; Steptoe, A. COVID-19 Social Study Results Release 32; University College London: London, UK, 2021. [Google Scholar]
- Guo, Y.; Cheng, C.; Zeng, Y.; Li, Y.; Zhu, M.; Yang, W.; Xu, H.; Li, X.; Leng, J.; Monroe-Wise, A. Mental health disorders and associated risk factors in Quarantined adults during the COVID-19 outbreak in China: Cross-sectional study. J. Med. Internet Res. 2020, 22, e20328. [Google Scholar] [CrossRef]
- Brenner, M.H.; Bhugra, D. Acceleration of anxiety, depression, and suicide: Secondary effects of economic disruption related to COVID-19. Front. Psychiatry 2020, 11, 592467. [Google Scholar] [CrossRef]
- Banerjee, D.; Rai, M. Social isolation in COVID-19: The impact of loneliness. Int. J. Soc. Psychiatry 2020, 66, 525–527. [Google Scholar] [CrossRef]
- Hoffart, A.; Johnson, S.U.; Ebrahimi, O.V. Loneliness and Social Distancing During the COVID-19 Pandemic: Risk Factors and Associations With Psychopathology. Front. Psychiatry 2020, 11, 589127. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Lund, E.M.; Forber-Pratt, A.J.; Wilson, C.; Mona, L.R. The COVID-19 pandemic, stress, and trauma in the disability community: A call to action. Rehabil. Psychol. 2020, 65, 313. [Google Scholar] [CrossRef] [PubMed]
- Emerson, E.; Stancliffe, R.; Hatton, C.; Llewellyn, G.; King, T.; Totsika, V.; Aitken, Z.; Kavanagh, A. The impact of disability on employment and financial security following the outbreak of the 2020 COVID-19 pandemic in the UK. J. Public Health 2021, 43, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Szmuda, T.; Ali, S.; Słoniewski, P. Telemedicine in neurosurgery during the novel coronavirus (COVID-19) pandemic. Neurol. I Neurochir. Pol. 2020, 54, 207–208. [Google Scholar]
- Jayaram, H.; Strouthidis, N.G.; Gazzard, G. The COVID-19 pandemic will redefine the future delivery of glaucoma care. Eye 2020, 34, 1203–1205. [Google Scholar] [CrossRef]
- Steptoe, A.; Di Gessa, G. Mental health and social interactions of older people with physical disabilities in England during the COVID-19 pandemic: A longitudinal cohort study. Lancet Public Health 2021, 6, e365–e373. [Google Scholar] [CrossRef]
- Ting, D.S.J.; Krause, S.; Said, D.G.; Dua, H.S. Psychosocial impact of COVID-19 pandemic lockdown on people living with eye diseases in the UK. Eye 2020, 35, 2064–2066. [Google Scholar] [CrossRef]
- Kempen, G.I.J.M.; Ballemans, J.; Ranchor, A.V.; van Rens, G.H.M.B.; Zijlstra, G.A.R. The impact of low vision on activities of daily living, symptoms of depression, feelings of anxiety and social support in community-living older adults seeking vision rehabilitation services. Qual. Life Res. 2012, 21, 1405–1411. [Google Scholar] [CrossRef] [Green Version]
- van der Aa, H.P.; Comijs, H.C.; Penninx, B.W.; van Rens, G.H.; van Nispen, R.M. Major depressive and anxiety disorders in visually impaired older adults. Investig. Ophthalmol. Vis. Sci. 2015, 56, 849–854. [Google Scholar] [CrossRef] [Green Version]
- Frank, C.R.; Xiang, X.; Stagg, B.C.; Ehrlich, J.R. Longitudinal Associations of Self-reported Vision Impairment With Symptoms of Anxiety and Depression Among Older Adults in the United States. JAMA Ophthalmol. 2019, 137, 793–800. [Google Scholar] [CrossRef]
- Fenwick, E.K.; Pesudovs, K.; Khadka, J.; Dirani, M.; Rees, G.; Wong, T.Y.; Lamoureux, E.L. The impact of diabetic retinopathy on quality of life: Qualitative findings from an item bank development project. Qual. Life Res. 2012, 21, 1771–1782. [Google Scholar] [CrossRef]
- Schliermann, R.; Heydenreich, P.; Bungter, T.; Anneken, V. Health-related quality of life in working-age adults with visual impairments in Germany. Disabil. Rehabil. 2017, 39, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Bullard, K.M.; Cotch, M.F.; Wilson, M.R.; Rovner, B.W.; McGwin, G.; Owsley, C.; Barker, L.; Crews, J.E.; Saaddine, J.B. Association between depression and functional vision loss in persons 20 years of age or older in the United States, NHANES 2005–2008. JAMA Ophthalmol. 2013, 131, 573–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyman, S.R.; Gosney, M.A.; Victor, C.R. Psychosocial impact of visual impairment in working-age adults. Br. J. Ophthalmol. 2010, 94, 1427–1431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vancampfort, D.; Koyanagi, A.; Hallgren, M.; Probst, M.; Stubbs, B. The relationship between chronic physical conditions, multimorbidity and anxiety in the general population: A global perspective across 42 countries. Gen. Hosp. Psychiatry 2017, 45, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Heinze, N.; Hussain, S.F.; Castle, C.L.; Godier-McBard, L.R.; Kempapidis, T.; Gomes, R.S. The long-term impact of the COVID-19 pandemic on loneliness in people living with disability and visual impairment. Front. Public Health 2021, 9, 738304. [Google Scholar] [CrossRef]
- Hussain, S.F.; Heinze, N.; Castle, C.L.; Godier-McBard, L.R.; Kempapidis, T.; Gomes, R.S.M. The Impact of COVID-19 on Health-Related Behaviours in People Living with Disabilities; BRAVO VICTOR: London, UK, 2021; manuscript submitted for publication. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Personal. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Heinze, N.; Hussain, S.F.; Castle, C.L.; Godier-McBard, L.R.; Kempapidis, T.; Ftouni, S.; Espie, C.A.; Gomes, R.S. The Impact of COVID-19 on Sleep Quality in People Living With Disabilities. Front. Psychol. 2021, 12, 786904. [Google Scholar] [CrossRef]
- Agorastos, A.; Skevas, C.; Matthaei, M.; Otte, C.; Klemm, M.; Richard, G.; Huber, C.G. Depression, anxiety, and disturbed sleep in glaucoma. J. Neuropsychiatry Clin. Neurosci. 2013, 25, 205–213. [Google Scholar] [CrossRef]
- Department for Work & Pensions. The Employment of Disabled People 2021. Available online: https://www.gov.uk/government/statistics/the-employment-of-disabled-people-2021/the-employment-of-disabled-people-2021 (accessed on 1 March 2022).
- Kahlon, M.K.; Aksan, N.; Aubrey, R.; Clark, N.; Cowley-Morillo, M.; Jacobs, E.A.; Mundhenk, R.; Sebastian, K.R.; Tomlinson, S. Effect of layperson-delivered, empathy-focused program of telephone calls on loneliness, depression, and anxiety among adults during the COVID-19 pandemic: A randomized clinical trial. JAMA Psychiatry 2021, 78, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Frontini, R.; Rebelo-Gonçalves, R.; Amaro, N.; Salvador, R.; Matos, R.; Morouço, P.; Antunes, R. The Relationship Between Anxiety Levels, Sleep, and Physical Activity During COVID-19 Lockdown: An Exploratory Study. Front. Psychol. 2021, 12, 659599. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Carbonell, L.; Meurling, I.J.; Wasserman, D.; Gnoni, V.; Leschziner, G.; Weighall, A.; Ellis, J.; Durrant, S.; Hare, A.; Steier, J. Impact of the novel coronavirus (COVID-19) pandemic on sleep. J. Thorac. Dis. 2020, 12, S163–S175. [Google Scholar] [CrossRef] [PubMed]
- Necho, M.; Birkie, M.; Gelaye, H.; Beyene, A.; Belete, A.; Tsehay, M. Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PLoS ONE 2020, 15, e0244530. [Google Scholar] [CrossRef]
- Office for National Statistics. 2011 Census Analysis: Ethnicity and Religion of the Non-UK Born Population in England and Wales: 2011; Office for National Statistics: Newport, UK, 2015. [Google Scholar]
- Redwood, S.; Gill, P.S. Under-representation of minority ethnic groups in research—Call for action. Br. J. Gen. Pract. 2013, 63, 342–343. [Google Scholar] [CrossRef] [Green Version]
- Zimdars, A.; Nazroo, J.; Gjonca, E. The circumstances of older people in England with self-reported visual impairment: A secondary analysis of the English Longitudinal Study of Ageing (ELSA). Br. J. Vis. Impair. 2012, 30, 22–30. [Google Scholar] [CrossRef]
| T1T2 % (n) | T1 % (n) | T2 % (n) | ||
|---|---|---|---|---|
| Gender | Female | 52.2 (83) | ||
| Male | 47.8 (76) | |||
| Ethnicity | Asian | 1.3 (2) | ||
| Black/African/Caribbean | 0.6 (1) | |||
| Hispanic/Latino/Spanish origin | 1.9 (3) | |||
| Mixed/Multiple Ethnic groups | 1.3 (2) | |||
| White/Other White | 95.0 (151) | |||
| Country of residence 1 | Canada | 0.6 (1) | ||
| France | 1.3 (2) | |||
| Germany | 1.9 (3) | |||
| Greece | 0.6 (1) | |||
| Malta | 5.6 (9) | |||
| Portugal | 3.1 (5) | |||
| Thailand | 0.6 (1) | |||
| UK | 76.9 (123) | |||
| USA | 9.4 (15) | |||
| Age | 18–25 | 1.9 (3) | 1.9 (3) | |
| 26–35 | 13.9 (22) | 11.4 (18) | ||
| 36–45 | 13.9 (22) | 17.7 (28) | ||
| 46–55 | 34.8 (55) | 31.0 (49) | ||
| 56–65 | 25.9 (41) | 24.1 (38) | ||
| 66–75 | 6.3 (10) | 10.8 (17) | ||
| 76–85 | 3.2 (5) | 3.2 (5) | ||
| 86+ | - | - | ||
| Employment status | In paid employment | 73.5 (111) | 69.6 (110) | |
| Employed but furloughed | - | 1.3 (2) | ||
| Retired | 16.6 (25) | 17.7 (28) | ||
| Unemployed, not looking for work | 7.9 (12) | 9.5 (15) | ||
| Unemployed, but looking for work | 2.0 (3) | 1.9 (3) | ||
| Time spent self-isolating | I am not self-isolating. | 24.5 (39) | 70.9 (112) | |
| 0–2 weeks | 5.7 (9) | 0.6 (1) | ||
| 2–4 weeks | 42.1 (67) | - | ||
| 4–8 weeks | 27.0 (43) | 0.6 (1) | ||
| 8–12 weeks | 1.3 (2) | 1.3 (2) | ||
| 3–4 months | 0.6 (1) | 0.6 (1) | ||
| 4–5 months (T2 only) | - | 1.3 (2) | ||
| Over 6 months (T2 only) | - | 24.7 (39) | ||
| Living status | I live on my own. | 23.9 (38) | 23.9 (38) | |
| I live with others. | 76.1 (121) | 76.1 (121) | ||
| Disability | No disability | 66.5 (105) | ||
| One or more disabilities | 33.5 (53) | |||
| VI or blindness | VI not reported | 76.9 (123) | ||
| VI reported | 23.1 (37) |
| T1 | T2 | VI | ||||
|---|---|---|---|---|---|---|
| No Disabilities | 1+ Disabilities | VI | No Disabilities | 1+ Disabilities | ||
| n | 104 | 50 | 35 | 105 | 51 | 35 |
| M | 37.54 | 41.52 | 38.89 | 35.67 | 42.67 | 40.49 |
| SD | 13.54 | 15.12 | 13.92 | 13.12 | 15.19 | 13.65 |
| Mdn | 37.00 | 39.00 | 38.00 | 33.00 | 40.00 | 39.00 |
| IQR | 20 | 24 | 16 | 20 | 27 | 21 |
| Variable | T1 | T2 | |||
|---|---|---|---|---|---|
| B | β | B | β | ||
| Model 1 | Constant | 52.127 *** | 51.839 *** | ||
| Age | −0.251 ** | −0.233 | −0.216 * | −0.200 | |
| Sex | −1.085 | −0.039 | −5.573 * | −0.197 | |
| Model 2 | Constant | 14.154 ** | 11.444 * | ||
| Age | −0.095 | −0.088 | −0.047 | −0.044 | |
| Sex | −6.131 ** | −0.222 | −0.361 | −0.013 | |
| Loneliness | 0.547 *** | 0.527 | 0.511 *** | 0.517 | |
| Sleep quality | 1.066 *** | 0.335 | 0.928 *** | 0.298 | |
| Self-isolation | −0.239 | −0.019 | 0.377 | 0.094 | |
| Living situation | 4.167 * | 0.130 | −0.781 | −0.024 | |
| Model 3 | Constant | 13.217 * | 11.805 * | ||
| Age | −0.086 | −0.080 | −0.014 | −0.013 | |
| Sex | −5.429 ** | −0.196 | −1.464 | −0.052 | |
| Loneliness | 0.551 *** | 0.531 | 0.503 *** | 0.508 | |
| Sleep quality | 1.174 *** | 0.369 | 1.033 *** | 0.332 | |
| Self-isolation | −0.239 | −0.019 | 0.359 | 0.089 | |
| Living situation | 3.778 | 0.117 | −2.499 | −0.076 | |
| Hearing impairment | 2.703 | 0.054 | −3.755 | −0.083 | |
| Mobility impairment | −6.118 * | −0.157 | −6.279 * | −0.164 | |
| Medical condition | 1.905 | 0.043 | 4.262 | 0.099 | |
| Mental health | 0.028 | 0.001 | 2.078 | 0.050 | |
| Model 4 | Constant | 13.187 * | 11.834 * | ||
| Age | −0.088 | −0.081 | −0.014 | −0.013 | |
| Sex | −5.539 ** | −0.200 | −1.497 | −0.053 | |
| Loneliness | 0.552 *** | 0.532 | 0.503 *** | 0.508 | |
| Sleep quality | 1.173 *** | 0.369 | 1.031 *** | 0.331 | |
| Self-isolation | −0.231 | −0.019 | 0.361 | 0.090 | |
| Living situation | 3.841 | 0.119 | −2.511 | −0.076 | |
| Hearing impairment | 2.503 | 0.050 | −3.671 | −0.081 | |
| Mobility impairment | −6.261 * | −0.160 | −6.237 * | −0.163 | |
| Medical condition | 1.851 | 0.042 | 4.277 | 0.099 | |
| Mental health | 0.029 | 0.001 | 2.074 | 0.050 | |
| VI | 0.485 | 0.014 | −0.168 | −0.005 | |
| Model 1 | Model 2 | Model 3 | Model 4 | ||
| T1 | R2 | 0.061 | 0.556 | 0.576 | 0.576 |
| F | 4.58 * | 28.40 *** | 17.94 *** | 16.20 *** | |
| ΔR2 | 0.061 | 0.495 | 0.020 | 0.000 | |
| ΔF | 4.58 * | 37.90 *** | 1.56 | 0.03 | |
| T2 | R2 | 0.050 | 0.562 | 0.587 | 0.587 |
| F | 3.77 * | 29.98 *** | 19.29 *** | 17.41 *** | |
| ΔR2 | 0.050 | 0.513 | 0.024 | 0.000 | |
| ΔF | 3.77 * | 41.00 *** | 1.99 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinze, N.; Castle, C.L.; Hussain, S.F.; Godier-McBard, L.R.; Kempapidis, T.; Gomes, R.S.M. State Anxiety in People Living with Disability and Visual Impairment during the COVID-19 Pandemic. Disabilities 2022, 2, 235-246. https://doi.org/10.3390/disabilities2020017
Heinze N, Castle CL, Hussain SF, Godier-McBard LR, Kempapidis T, Gomes RSM. State Anxiety in People Living with Disability and Visual Impairment during the COVID-19 Pandemic. Disabilities. 2022; 2(2):235-246. https://doi.org/10.3390/disabilities2020017
Chicago/Turabian StyleHeinze, Nikki, Claire L. Castle, Syeda F. Hussain, Lauren R. Godier-McBard, Theofilos Kempapidis, and Renata S. M. Gomes. 2022. "State Anxiety in People Living with Disability and Visual Impairment during the COVID-19 Pandemic" Disabilities 2, no. 2: 235-246. https://doi.org/10.3390/disabilities2020017
APA StyleHeinze, N., Castle, C. L., Hussain, S. F., Godier-McBard, L. R., Kempapidis, T., & Gomes, R. S. M. (2022). State Anxiety in People Living with Disability and Visual Impairment during the COVID-19 Pandemic. Disabilities, 2(2), 235-246. https://doi.org/10.3390/disabilities2020017






