Level of Inclusiveness of People with Disabilities in Ghanaian Health Policies and Reports: A Scoping Review
Abstract
:1. Introduction
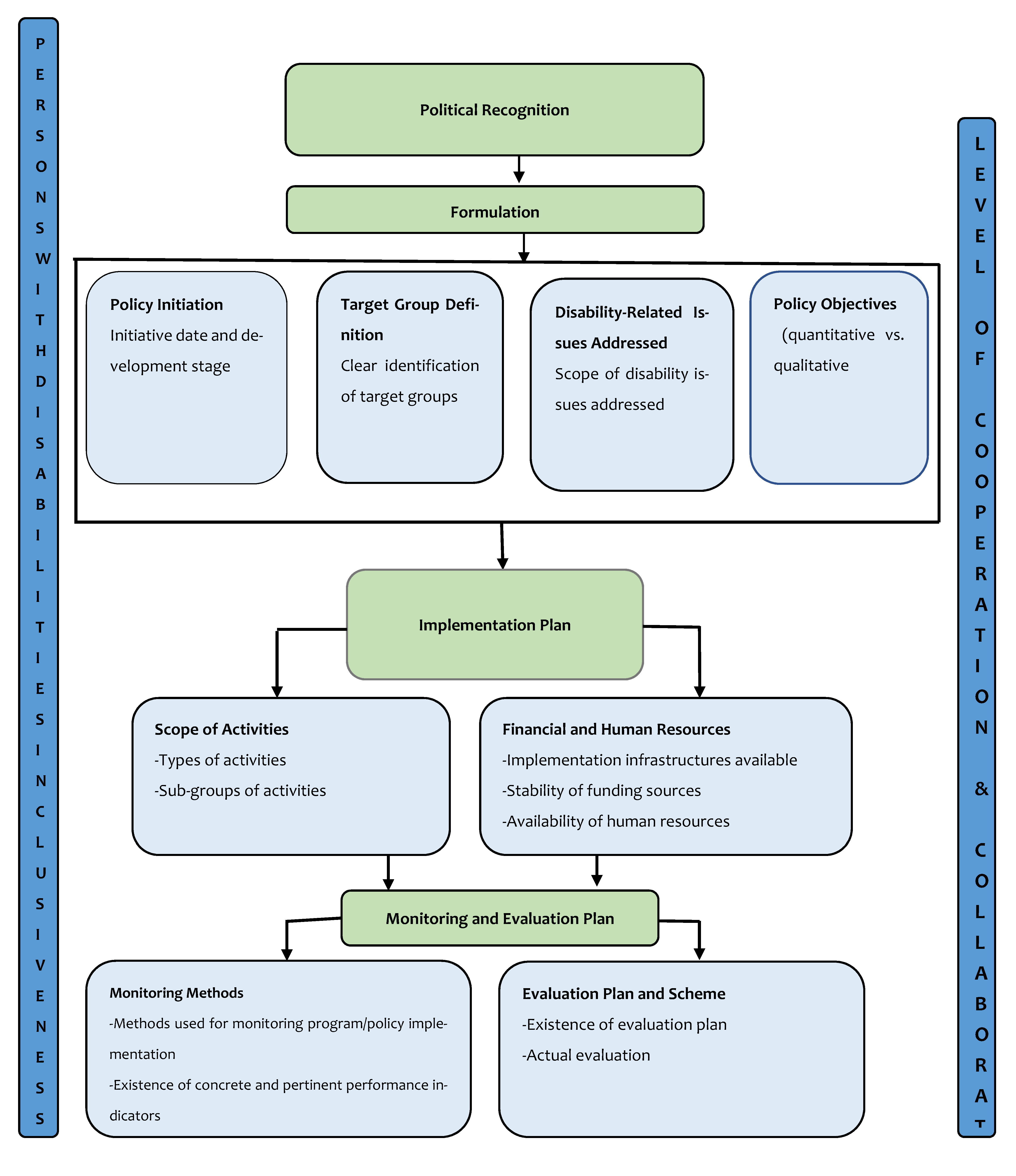
2. Materials and Methods
2.1. Phase 1: The Review/Research Question
- (1)
- What are the health policies/reports in Ghana?
- (2)
- To what extent do these policies/reports include PWDs?
2.2. Phase 2: Identifying Relevant Policies
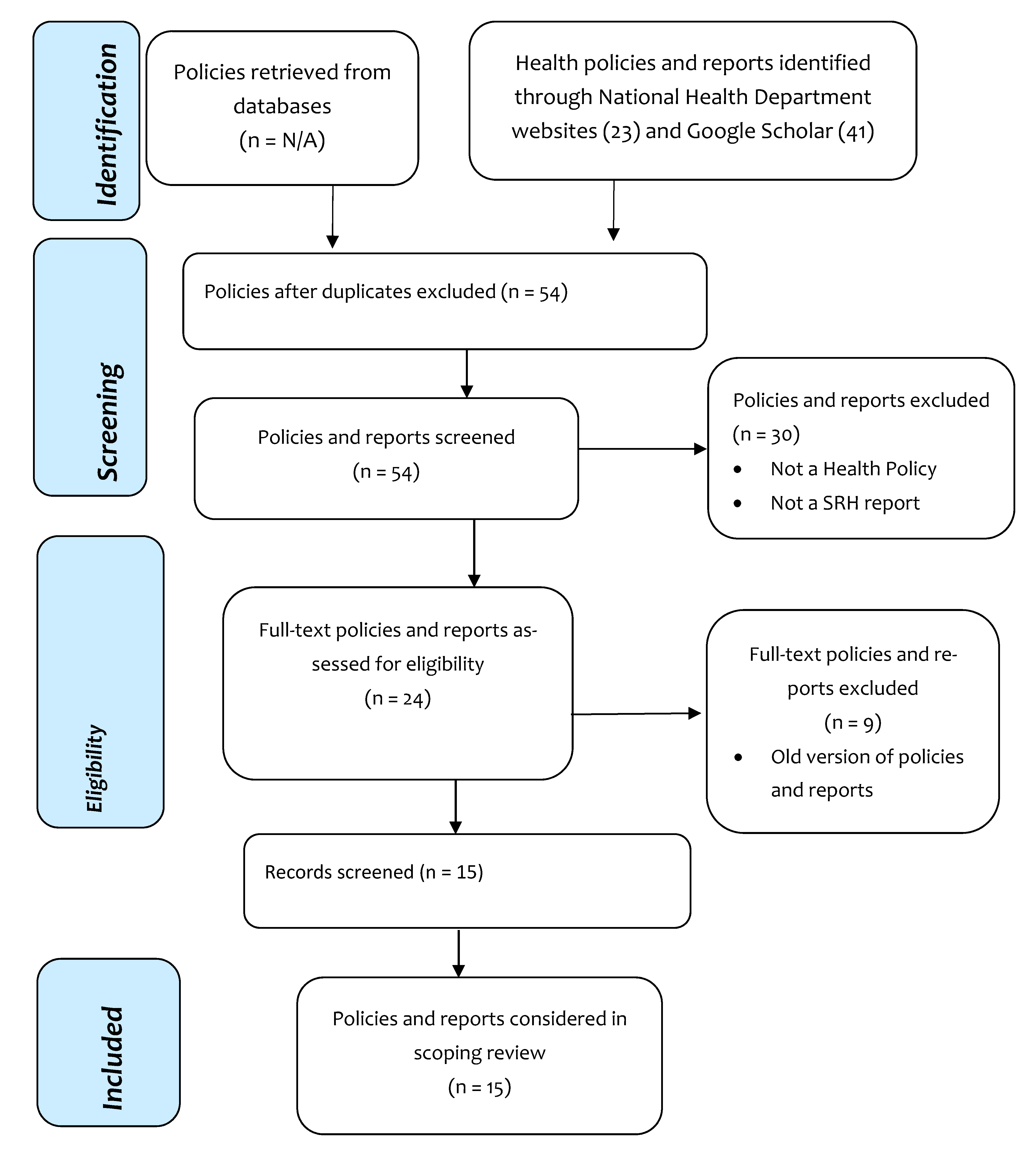
2.3. Phase 3: Study Selection
2.4. Phase 4: Charting the Data
2.5. Phase 5: Collating, Summarizing and Reporting the Results
3. Results
3.1. Political Recognition
“there is the need to create a safe and supportive environment, ensure access to appropriate information, ensure that health facilities provide goods and services including counselling on mental health, nutrition, sexual and reproductive health, ensure the active participation of young people in programmes affecting them and their protection from all forms of violence, harmful practices especially focusing on the more vulnerable such as pre adolescents, younger adolescents, pregnant adolescents, adolescents practising prostitution directly or indirectly and adolescents living with HIV and AIDS”.
“…The Policy has been inspired by the overall national medium-term policy framework, set out in the Coordinated Programme of Economic and Social Development Policies (2017–2024), and recognises several global, continental and regional compacts and policy frameworks, such as SDGS, the International Health Regulations, the African Union Vision 2063: The Africa We Want, the ECOWAS Vision 2020 and the African Health Strategy (2016–2030)”.
3.2. Policy Initiation
3.3. Target Group Definition
3.4. Composition of the People Who Developed the Policy/Advisory Panel
3.5. Disability Issues Addressed
“…States/parties shall ensure that all measures that relate to the exercise of legal capacity provide for appropriate and effective safeguards to prevent abuse in accordance with international human rights law. Such safeguards shall ensure that measures relating to the exercise of legal capacity respect the rights, will and preferences of the person, are free of conflict of interest and undue influence, are proportional and tailored to the person’s circumstances, apply for the shortest time possible and are subject to regular review by a competent, independent, and impartial authority or judicial body. The safeguards shall be proportional to the degree to which such measures affect the person’s rights and interests”.[4] (p. 10–11).
3.6. Policy Objectives
“…The overarching goal of this Policy is to mainstream gender equality concerns into the national development processes by improving the social, legal, civic, political, economic and socio-cultural conditions of the people of Ghana particularly women, girls, children, the vulnerable and people with special needs; persons with disability and the marginalized”.
3.7. Scope of Activities
3.8. Financial and Human Resources
3.9. Monitoring and Evaluation Plan
“The importance of reliable and timely collection of demographic data for formulation, monitoring and evaluation of development programmes cannot be over emphasized. Different strategies such as timely collection of data, strengthening the capacity of the Ghana health service and all training and research institutions and the enactment of laws governing the registration of vital events”.
3.10. Level of Coordination and Collaboration
3.11. Level of Disability Involvement
“The issue of disability in our society also deserves serious consideration. Although official figures of registered persons with disabilities in the country in 1990 was 47, 397, it is believed, that unofficial figures might be well over 1 million. The proper sustenance and rehabilitation of these disabled persons demands serious attention”.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. World Report on Disability; WHO: Geneva, Switzerland, 2011; Available online: https://apps.who.int/iris/handle/10665/44575 (accessed on 1 June 2021).
- Mitra, S.; Yap, J. The Disability Data Report: Disability Data Initiative; Fordham Research Consortium on Disability: New York, NY, USA, 2021; pp. 1–69. [Google Scholar]
- WHO. Disability and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 1 June 2021).
- UN. Convention on the Rights of Persons with Disabilities; United Nations: New York, NY, USA, 2006. [Google Scholar]
- Ghana Disability Data Disaggregation Pilot Project: Results of Integrating Disability into Routine Data Collection Systems; Sightsavers: Chippenham, UK, 2018.
- OHCHR. Status of Ratification Interactive Dashboard; Office of the High Commissioner for Human Rights Retrieved: Geneva, Switzerland, 2021; Available online: https://indicators.ohchr.org/ (accessed on 1 May 2021).
- WHO. Disability-Inclusive Health Services Toolkit: A Resource for Health Facilities in the Western Pacific Region; World Health Organization Regional Office for the Western Pacific: Manila, Philippines, 2020; pp. 1–234. [Google Scholar]
- UN. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015. [Google Scholar]
- Asuman, D.; Ackah, C.G.; Agyire-Tettey, F. Disability and household welfare in Ghana: Costs and correlates. J. Fam. Econ. Issues 2020, 2020, 1–7. [Google Scholar]
- Gichane, M.W.; Heap, M.; Fontes, M.; London, L. “They must understand we are people”: Pregnancy and maternity service use among signing Deaf women in Cape Town. Disabil. Health J. 2017, 10, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Madans, J.H.; Loeb, M.E.; Altman, B.M. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health 2011, 11, 1–4. [Google Scholar] [CrossRef] [Green Version]
- SSharma, S.; Sivakami, M. Sexual and reproductive health concerns of persons with disability in India: An issue of deep-rooted silence. J. Biosoc. Sci. 2018, 51, 225–243. [Google Scholar] [CrossRef] [PubMed]
- Esmail, S.; Darry, K.; Walter, A.; Knupp, H. Attitudes and perceptions towards disability and sexuality. Disabil. Rehabil. 2010, 32, 1148–1155. [Google Scholar] [CrossRef] [PubMed]
- Badu, E.; Gyamfi, N.; Opoku, M.P.; Mprah, W.K.; Edusei, A.K. Enablers and barriers in accessing sexual and reproductive health services among visually impaired women in the Ashanti and Brong Ahafo regions of Ghana. Reprod. Health Matters 2018, 26, 51–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groce, N.; Kett, M.; The Disability and Development Gap. Leonard Cheshire Disability and Inclusive Development Centre Working Paper Series. 2013. Available online: https://www.academia.edu/download/51014735/WP21_Disability_and_Development_Gap.pdf (accessed on 1 May 2021).
- Badu, E.; Opoku, M.P.; Appiah, S.C.Y. Attitudes of health service providers: The perspective of people with disabilities in the kumasi metropolis of ghana. Afr. J. Disabil. 2016, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Badu, E.; Mensah, I.; Gyamfi, N.; Agyei-Okyere, E.; Abodey, E.; Adusei-Nkrumah, J. Knowledge and sources of accessing sexual and reproductive health information among visually impaired women in Ghana. BMC Res. Notes 2019, 12, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Saulo, B.; Walakira, E.; Darj, E. Access to healthcare for disabled persons. How are blind people reached by HIV services? Sex. Reprod. Healthc. 2012, 3, 49–53. [Google Scholar] [CrossRef]
- Burke, E.; Kébé, F.; Flink, I.; Van Reeuwijk, M.; Le May, A. A qualitative study to explore the barriers and enablers for young people with disabilities to access sexual and reproductive health services in Senegal. Reprod. Health Matters 2017, 25, 43–54. [Google Scholar] [CrossRef]
- Holdsworth, E.; Trifonova, V.; Tanton, C.; Kuper, H.; Datta, J.; MacDowall, W.; Mercer, C. Sexual behaviours and sexual health outcomes among young adults with limiting disabilities: Findings from third British National Survey of Sexual Attitudes and Lifestyles (Natsal-3). BMJ Open 2018, 8, e019219. [Google Scholar] [CrossRef] [Green Version]
- Frohmader, C.; Ortoleva, S. The Sexual and Reproductive Rights of Women and Girls with Disabilities. 2013. Available online: https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=21.%09Frohmader%2C+C.%3B+Ortoleva%2C+S.+The+Sexual+and+Reproductive+Rights+of+Women+and+Girls+with+Disabilities%3B+Publisher%3A+city%2C+country%2C+2013.&btnG= (accessed on 1 May 2021).
- Bremer, K.; Cockburn, L.; Ruth, A. Reproductive health experiences among women with physical disabilities in the Northwest Region of Cameroon. Int. J. Gynecol. Obstet. 2009, 108, 211–213. [Google Scholar] [CrossRef]
- UNFPA. A Deeper Silence: The Unheard Experiences of Women With Disabilities and their Sexual and Reproductive Health Experiences: Kiribati, the Solomon Islands and Tonga; United Nations Population Fund Pacific Sub-Regional Office: Suva, Fiji, 2013. [Google Scholar]
- Addlakha, R.; Price, J.; Heidari, S. Disability and sexuality: Claiming sexual and reproductive rights. Reprod. Health Matters 2017, 25, 4–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahinkorah, B.O.; Kang, M.; Perry, L.; Brooks, F. Prevention of adolescent pregnancy in Anglophone sub-Saharan Africa: A scoping review of national policies. Int. J. Health Policy Manag. 2020. [Google Scholar] [CrossRef] [PubMed]
- Agbenu, I. Evaluation of the Implementation of Adolescent Health Service Policy and Strategy (2016-2020) in the Tema Metropolis; University of Ghana: Accra, Ghana, 2019; pp. 1–157. [Google Scholar]
- GAC. National HIV and AIDS, STI Policy; Ghana AIDS Commission: Accra, Ghana, 2013; pp. 1–67. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjBosL48IfxAhWIsRQKHWCzCKwQFjAAegQIAhAD&url=https%3A%2F%2Fwww.healthpolicyproject.com%2Fpubs%2F153_Policyfinal.pdf&usg=AOvVaw3h4sEOigw2Vj4R6OIoe5Tj (accessed on 1 May 2021).
- Lang, R.; Schneider, M.; Kett, M.; Cole, E.; Groce, N. Policy development: An analysis of disability inclusion in a selection of African Union policies. Dev. Policy Rev. 2018, 37, 155–175. [Google Scholar] [CrossRef] [Green Version]
- Kwadwo, W.; Anafi, P.; Sekyere, F.O. Does disability matter? Disability in sexual and reproductive health policies and research in Ghana. Int. Q. Community Health Educ. 2014, 35, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Karimu, A.T.F.A. Disabled persons in Ghanaian health strategies: Reflections on the 2016 adolescent reproductive health policy. Reprod. Health Matters 2018, 26, 20–24. [Google Scholar] [CrossRef]
- Mfoafo-M’Carthy, M.; Grischow, J.D.; Stocco, N. Cloak of invisibility: A literature review of physical disability in Ghana. SAGE Open 2020, 10. [Google Scholar] [CrossRef]
- Hashemi, G.; Kuper, H.; Wickenden, M. SDGs, Inclusive health and the path to universal health coverage. Disabil. Glob. South 2017, 4, 1088–1111. [Google Scholar]
- Jamali, M.Z. Disability Measurement and Uptake of Sexual and Reproductive Health Services in Malawi. Ph.D. Thesis, University of Southampton, Southampton, UK, 2020. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Jones, C.M.; Gautier, L.; Ridde, V. A scoping review of theories and conceptual frameworks used to analyse health financing policy processes in sub-Saharan Africa. Health Policy Plan. 2021. [Google Scholar] [CrossRef] [PubMed]
- Calves, A. Assessing Adolescent Reproductive Health Policies and Programs. In Policy Working Paper Series; USAID: Washington, DC, USA, 2002; pp. 1–33. Available online: https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Calves%2C+A.+%282002%29.+Assessing+adolescent+reproductive+health+policies+and+programs.+Retrieved+from+Washington%2C+DC%3A+&btnG= (accessed on 1 May 2021).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Int. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MOH. National Health Policy: Ensuring Healthy Lives for All; Ministry of Health: Accra, Ghana, 2020; pp. 1–46. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjXoLbz8YfxAhVJ5uAKHQXZC0MQFjAAegQIAxAD&url=https%3A%2F%2Fwww.moh.gov.gh%2Fwpcontent%2Fuploads%2F2020%2F07%2FNHP_12.07.2020.pdf-13072020-FINAL.pdf&usg=AOvVaw1G--5Y2AsC0xcGkqx6Dv_U (accessed on 1 May 2021).
- GOG. National Population Policy (Revised Edition, 1994). 1994. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjSb76qtPxAhWBoVwKHebHCCoQFjABegQIBBAD&url=https%3A%2F%2Fnpc.gov.gh%2Fwp-content%2Fuploads%2F2019%2F01%2FNational-Population-PolicyRevised-Edition-1994.pdf&usg=AOvVaw0PI2IHJYnyOhqKL4RVxfGI (accessed on 1 May 2021).
- GHS. Adolescent Health Service Policy and Strategy (2016–2020); Ghana Health Service: Accra, Ghana, 2020; Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwiG3_zZydDyAhUmQEEAHYnzCRYQFnoECAQQAQ&url=https%3A%2F%2Fwww.afro.who.int%2Fsites%2Fdefault%2Ffiles%2F2017-10%2FADOLESCENT%2520HEALTH%2520SERVICE%2520POLICY%2520%2520AND%2520STRATEGY.pdf&usg=AOvVaw3bBY-GRD6_kQnXb-4Bno9A (accessed on 1 May 2021).
- GHS. Reproductive Health Strategic Plan 2007–2011. 2007. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiwsNyT9YfxAhUM0uAKHSZ3CykQFjABegQIBBAD&url=http%3A%2F%2Fwww.moh.gov.gh%2Fwp-content%2Fuploads%2F2016%2F02%2FGHS-Reproductive-Health-Strategic-Plan-FINAL.pdf&usg=AOvVaw35xjp5uCQ-rpwmCmF-EKQ3 (accessed on 1 May 2021).
- IDS; GSS and Associates. Domestic Violence in Ghana: Incidence, Attitudes, Determinants and Consequences. 2016. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwipnfKC9ofxAhVuA2MBHdSvA6cQFjACegQIAxAE&url=https%3A%2F%2Fwww2.statsghana.gov.gh%2Fdocfiles%2Fpublications%2FDV_Ghana_Report_FINAL.pdf&usg=AOvVaw2ybOzhhduAH5Td0CFYGk6T (accessed on 1 May 2021).
- GOG. Criminal Code 1960 (ACT, 29). 1960. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiW4tKZq9PxAhXahVwKHQrrAewQFjADegQIBRAD&url=https%3A%2F%2Fhome.gis.gov.gh%2Fwp-content%2Fuploads%2F2020%2F05%2FCriminal-Offences-Act-1960-Act-29.pdf&usg=AOvVaw1A7R-yWgXvCFI5o2PodrGW (accessed on 1 May 2021).
- Awusabo-Asare, K.; Abane, A.M.; Kumi-Kyereme, A. Adolescent Sexual and Reproductive Health in Ghana: A Synthesis of Research Evidence, Occasional Report; The Alan Guttmacher Institute: New York, NY, USA, 2004; Volume 13, pp. 1–37. [Google Scholar]
- MOH. National Health Insurance Policy; MOH: Accra, Ghana, 2004; Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiC_56nqNPxAhU1olwKHcHqA3QQFjAAegQIBRAD&url=https%3A%2F%2Fextranet.who.int%2Fnutrition%2Fgina%2Fen%2Fnode%2F8121&usg=AOvVaw2rz6rYKnEFrXhiKrJgkaOX (accessed on 1 May 2021).
- GOG. National Gender Policy. 2015. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiP0OnO94fxAhVR7OAKHXdAFoQFjAMegQIFRAD&url=https%3A%2F%2Fwww.mogcsp.gov.gh%2Fmdocs-posts%2Fnational-gender-policy%2F&usg=AOvVaw1qlYJiNL4OULY97kmD94tr (accessed on 1 May 2021).
- GSS. Multiple Indicator Cluster Survey (MICS2017/18), Survey Findings Report; GSS: Accra, Ghana, 2018; Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiFp6aTfxAhXgBmMBHfQABYkQFjABegQIBBAD&url=https%3A%2F%2Fwww.unicef.org%2Fghana%2Freports%2Fghana-multiple-indicator-cluster-survey&usg=AOvVaw2Qyn1V1D8SM9oRnT2AE6Ky (accessed on 1 May 2021).
- MOH. National Reproductive Health Policy and Standards. 2003. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwij7_7BqNPxAhVVglwKHXysCNUQFjAKegQIMRAD&url=https%3A%2F%2Fwww.ghanahealthservice.org%2Fdownloads%2FNHI_policy%2520framework.pdf&usg=AOvVaw1MJE_i5eIFLOz9YmRIBNOP (accessed on 1 May 2021).
- GOG. Ghana Family Planning Costed Implementation Plan 2016–2020; Ghana Health Service: Accra, Ghana, 2015. [Google Scholar]
- GSS; GHS; ICF. Ghana Demographic and Health Survey 2014; GSS, GHS, and ICF: Rockville, MD, USA, 2015. [Google Scholar]
- GSS; GHS; ICF. Ghana Maternal Health Survey 2017; GSS, GHS, and ICF: Accra, Ghana, 2018. [Google Scholar]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Bloor, M.; Wood, F. Phenomenological methods. Keywords Qual. Methods 2006, 56, 128–130. [Google Scholar]
- Dye, T.R. Understanding Public Policy; Pearson: Upper Saddle River, NJ, USA, 1998. [Google Scholar]
- Stover, J.; Johnston, A.; The Art of Policy Formulation: Experiences from Africa in Developing National HIV. AIDS Policies. 1999. Available online: http://www.plicyprogect.com/pubs/occasional/op-03PDF (accessed on 1 May 2021).
- Birdthistle, I.; Vince-Whitman, C. Reproductive Health Programs for Young Adults: School-Based Programs; Pathfinder International, Focus on Young Adults Project: Watertown, MA, USA, 1997. [Google Scholar]
- Walsham, M.; Kuper, H.; Banks, L.M.; Blanchet, K. Social protection for people with disabilities in Africa and Asia: A review of programmes for low-and middle-income countries. Oxf. Dev. Stud. 2018, 47, 97–112. [Google Scholar] [CrossRef] [Green Version]
- MOH. Health Sector Policy; Ministry of Health: Kigali, Rwanda, 2015; pp. 1–41. Available online: https://www.moh.gov.rw/news-detail/health-sector-policy-2015 (accessed on 1 July 2021).
- Njelesani, J.; Siegel, J.; Ullrich, E. Realization of the rights of persons with disabilities in Rwanda. PLoS ONE 2018, 13, 1–15. [Google Scholar] [CrossRef] [Green Version]
- DOH. National Health Promotion Policy and Strategy, 2015-2019; Department of Health: Pretoria, South Africa, 2015; Available online: https://www.health-e.org.za/wp-content/uploads/2015/09/The-National-Health-Promotion-Policy-and-Strategy.pdf (accessed on 1 July 2021).
- FMOH. National Health Promotion Policy; FMOH: Abuja, Nigeria, 2019; pp. 1–33. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiR4abcltLxAhXBQkEAHd1nBIgQFjABegQIBRAD&url=https%3A%2F%2Fwww.health.gov.ng%2Fdoc%2FNHPP_2019.pdf&usg=AOvVaw3nsSO9pb2yHTuomf_b_0ez (accessed on 1 July 2021).
- MHSS. National Health Policy Framework, 2010–2020. In Ministry of Health and Social Services, Windhoek, Namibia; 2010; pp. 1–40. Available online: https//www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjI1YHD48vyAhVymVwKHZGbBPEQFnoECAIQAQ&url=https%3A%2F%2Fextranet.who.int%2Fcountryplanningcycles%2Fsites%2Fdefault%2Ffiles%2Fcountry_docs%2FNamibia%2Fnamibia_national_health_policy_framework_2010-2020.pdf&usg=AOvVaw3pmJVGOWC_V4f-iqW67SA0 (accessed on 1 July 2021).
| Policy/Report Title | Political Recognition | Policy/ Report Initiation | Disability/Issues Addressed Concerning Persons with Disabilities | Target Group Definition | Composition of the People who Developed It/ Advisory Panel | Policy Objective (Qualitative/Quantitative) | Scope of Activities/ Strategies to Include PWDs | Resources (Financial and Human) | M and E Plan and Performance Indicators | Cooperation & Collaboration (Number of Partners Involved) | Involvement of Persons with Disabilities | How Accessible Is It? | Mention of Disability |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| National Health Policy: Ensuring healthy lives for all, revised version, January 2020 [38] | yes | 01/01/2020 | access to healthcare, discrimination and stigmatisation and empowerment | general | multi-disciplinary group, no disability organisation present | qualitative | X | human and financial resources | √ | √ | √ | online (English version) | yes |
| Ghana Demographic and Health Survey (2014) [50] | yes | 2014 | X | men (15–64), women (15–49), children (under five) | multi-disciplinary group, no disability organisation present | qualitative | X | human and financial resources | N/A | √ | X | online (English version) | yes |
| Ghana Maternal Health Survey(2017) [51] | yes | 2017 | health care access, insurance, and disability, family planning, ANC, skilled delivery, place of delivery, problems in accessing healthcare | women aged 15–49 | multi-disciplinary group, no disability organisation present | qualitative | X | human and financial resources | N/A | √ | X | online (English version) | yes |
| National Population Policy [39] | yes | 1994 | creating opportunities for participation. | general | multi-disciplinary, no disability organisation present | qualitative | Education, form a national coordinating committee on disability, enactment of laws and enforcement of existing ones, provision of assistance | human and financial resources | √ | √ | X | online (English version) | yes |
| National HIV and AIDS, STI policy [27] | yes | 01/02/2013 | X | general population with much emphasis on persons living with HIV and AIDS | multi-disciplinary group, no disability organisation present | qualitative | IEC (social and behavioural change, including most at risk populations. Social protection | human and financial resources | √ | √ | X | online (English version) | yes |
| Adolescent Health Service Policy and Strategy [40] | yes | 2016 | creating opportunities for participation | young people aged 10–24 years | multi-disciplinary group, disability organisation present (National Commission for Persons with Disabilities) | qualitative | IEC (Social and Behavioural Change Communication strategy) Health Services (increase access for adolescents) Training (needs assessment of staff, and capacity building of staff) | human and financial resources | √ | √ | √ | online (English version) | yes |
| Reproductive health strategic plan [41] | yes | 07/04/2007 | X | general | multi-disciplinary group, no disability organisation present | qualitative | IEC (Information, education and communication, Behavioural Change Communication), improving access to MHS (ANC, Skilled delivery, PNC), Promotion of access to contraceptive prevalence, using community based volunteers | human and financial resources | √ | √ | X | online (English version) | no |
| Domestic Violence Report [42] | yes | 01/07/2016 | X | men, women, boys and girls between the ages of 15 and 60 years | multi-disciplinary group, no disability organisation present | qualitative | X | human and financial resources | N/A | √ | X | online (English version) | yes |
| Criminal offences code [43] | yes | 12/01/1961 | abortion | general | not stated | qualitative | X | human and financial resources | N/A | X | X | online (English version) | yes |
| National Survey of Adolescents [44] | not described | 01/06/2004 | X | adolescents (10–19 years) | group of researchers without inputs from persons with disabilities | qualitative | X | human and financial resources | N/A | X | X | online (English version) | no |
| National Health Insurance Scheme Policy [45] | yes | August, 2004 | exemption from payment | general | multi-disciplinary group, no disability organisation present | qualitative | Exemptions of payment for Poor and Vulnerable groups | human and financial resources | X | √ | X | online (English version) | yes |
| National Gender Policy [46] | yes | May, 2015 | opportunities for participation | general | multi-disciplinary group, no disability organisation present | qualitative | Information Education and Communication (Social and Behavioural Change Communication strategy), Health Services, Training (needs assessment of staff, and capacity building of staff) | human and financial resources | √ | √ | √ | online (English version) | yes |
| Multiple indicator cluster survey [47] | yes | 2018 | functioning based on the WHO functional disability module/questionnaire | men and women, children aged 5–17 years as well as children under 5 | not clearly stated | qualitative | Adding the functional disability module to the survey | human and financial resources | N/A | √ | Yes | online (English version) | yes |
| National Reproductive health service policy and standards [48] | yes | 2014 | abortion and contraception | general | not clearly stated | qualitative | Birth control for “mentally disabled” women. | human and financial resources | √ | √ | Yes | online (English version) | yes |
| Ghana Family Planning Costed Implementation Plan [40] | yes | 01/09/2015 | X | women | not clearly stated | qualitative and quantitative | X | human and financial resources | √ | √ | X | online (English version) | yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seidu, A.-A.; Malau-Aduli, B.S.; McBain-Rigg, K.; Malau-Aduli, A.E.O.; Emeto, T.I. Level of Inclusiveness of People with Disabilities in Ghanaian Health Policies and Reports: A Scoping Review. Disabilities 2021, 1, 257-277. https://doi.org/10.3390/disabilities1030019
Seidu A-A, Malau-Aduli BS, McBain-Rigg K, Malau-Aduli AEO, Emeto TI. Level of Inclusiveness of People with Disabilities in Ghanaian Health Policies and Reports: A Scoping Review. Disabilities. 2021; 1(3):257-277. https://doi.org/10.3390/disabilities1030019
Chicago/Turabian StyleSeidu, Abdul-Aziz, Bunmi S. Malau-Aduli, Kristin McBain-Rigg, Aduli E. O. Malau-Aduli, and Theophilus I. Emeto. 2021. "Level of Inclusiveness of People with Disabilities in Ghanaian Health Policies and Reports: A Scoping Review" Disabilities 1, no. 3: 257-277. https://doi.org/10.3390/disabilities1030019
APA StyleSeidu, A.-A., Malau-Aduli, B. S., McBain-Rigg, K., Malau-Aduli, A. E. O., & Emeto, T. I. (2021). Level of Inclusiveness of People with Disabilities in Ghanaian Health Policies and Reports: A Scoping Review. Disabilities, 1(3), 257-277. https://doi.org/10.3390/disabilities1030019







