1. Introduction
AI and machine learning have made a great impact in most areas of modern society, from entertainment, to commerce, to healthcare. All these data can be used to predict certain behaviours in society (
Arvai et al., 2025). In the health area, there is a great potential for this type of tool to predict trends and behaviours with the purpose of improving the responsiveness of health professionals and managers (
Catalina et al., 2023).
There are several studies that prove that Artificial Intelligence (AI) algorithms can add value to various healthcare units (
Nelson et al., 2020). AI can actively contribute to the improvement of care delivery, for example, through the analysis of medical images, through the correlation of symptoms that allow characterising and performing a prognosis regarding a given pathology, through the prediction of the level of demand for a given service, or through the improvement of the management processes inherent to a health unit (
Bohr & Memarzadeh, 2020;
Hassan et al., 2024).
The demand for healthcare has been increasing and was particularly aggravated by the COVID-19 pandemic. In this sense, several countries have faced a shortage of healthcare professionals and struggle daily against the scarcity of resources and the lack of adaptive measures in the face of this new reality (
Liu et al., 2021). The healthcare ecosystem is increasingly aware of the importance that AI tools may have in future generations. Beyond the improvement in terms of performance, it is estimated that AI could have a huge impact on cost reduction with fewer hospitalisations, fewer doctor visits and fewer treatments (
Eigner et al., 2019).
During the research period, three main factors were considered: the perception and knowledge, the benefits, and the challenges associated with the implementation of smart systems.
The main motivation for the development of this research study was due to the need to understand how Portuguese health professionals and managers envision the implementation of AI tools (
Asan et al., 2020). Understanding the main motivations and concerns of health professionals and managers is essential to understand how to act so as to enhance the implementation of these systems over the coming years.
The number of challenges facing health institutions has been increasing. The pandemic crisis has posed huge challenges to the response capacity of the NHS. It is therefore necessary to reformulate the strategy of action and find innovative ways to address its different weaknesses (
Public Finance Council, 2020).
Despite the recognition of several benefits associated with the implementation of AI tools, there are several reasons that lead to the failure of their implementation (
Gerke et al., 2020). According to
Panch et al. (
2019), the main causes of failure are due to several factors such as the complexity of AI algorithms, the integrity and quality of the stored data, the level of trust of health professionals, the level of user perception and acceptance, user reliability, the violation of ethical and privacy issues, legal liability, the purpose for adopting these tools, and the attitude of medical students towards these new technologies. To contribute to the process of implementation of these systems, it is necessary to understand which factors mostly contribute to the failure of AI adoption in the health area. In this sense, this study aims to understand how health professionals and managers face the challenge of integrating AI tools (
Henzler et al., 2025).
This research presents in its literature review several articles that exemplify how institutions make use of AI systems. The main problem identified is associated with the lack of knowledge about AI of healthcare professionals and managers.
To fulfil this purpose, the following objective was defined: to understand which factors influence the possibility of applying intelligent systems in the health area. In this sense, it will be possible to identify which factors favour (or not) the intentionality of implementing this type of system in context.
Despite the growing interest in AI adoption in healthcare, previous research applying the TAM/UTAUT models has rarely focused on healthcare professionals and managers (
Chan & Zary, 2019) simultaneously, and few studies explore the Portuguese context. Portugal’s centralised public healthcare system, combined with relatively low levels of digital maturity and limited training on AI, makes it a distinctive environment for analysing adoption behaviour. This study aims to fill these gaps by (1) extending technology adoption models to explore the mediating roles of knowledge and perceived benefits, (2) offering empirical insights from both clinical and managerial actors, and (3) contributing data from a Portuguese context that remains underrepresented in the literature.
2. Materials and Methods
According to
Vilelas (
2009), the main objective of research methodology is to study the scientific method that enables the validation and confirmation of a given theory. According to the author, we may classify methodology in two ways: ends and means. The ends refer to applied research of an exploratory nature, while the means are related to field study and bibliographical research. Regarding the means of the present study, as a primary source, the study relied on the application of questionnaires, and as a secondary source, bibliographical research was conducted through the analysis of several scientific articles present in books, newspapers and magazines.
Based on the objectives of this study, a quantitative methodology was chosen through the creation of a questionnaire. It should be noted that this approach had an inductive nature, since it was conducted through a non-probability convenience sample, considering that the intention was to obtain a sample with members from the health area and the health management area with an interest in AI. It is also important to mention that the convenience sample is more likely to be influenced by variables that are not under the researcher’s control, thus not allowing general and rigorous statements to be made about the population. As regards external validity, this study reinforced some existing theory and deepened the knowledge about the impact that Artificial Intelligence may have in the area of health.
2.1. Research Model
To answer the study objective, a quantitative approach was carried out through the creation of a questionnaire. According to
Vilelas (
2009), this method aims to obtain standardised answers with closed and easily interpretable questions and is mostly used when the unit of analysis is people. According to
Vilelas (
2009), the use of a questionnaire has some advantages in terms of costs, data processing, and reduction in the margin of error.
The questionnaire had a section with identification questions and information questions. The document developed addressed the topics previously described in the literature review and was structured using the Google Forms tool. After being validated by the advisor, it was assessed and tested by three health professionals who suggested that one of the questions be reformulated. Their validation aimed to ensure that the questionnaire was error-free. Subsequently, the document was shared through the LinkedIn network.
The document was divided into four sections. The first section contained a multiple-answer question aimed at performing an initial screening to ensure that only people connected to health or health management and with an interest in the area of AI could complete the questionnaire. The same section had three additional questions to characterise the respondent. Sections two, three, and four were intended to answer the research question through Likert-type scales with seven levels, in which each extreme would have an opposite position. Responses were collected between 7 January 2021 and 7 February 2022, where 100 responses were obtained. Subsequently, the extracted data were entered in Excel format in the SmartPLS 3 software platform. Thus, the research question—what are the factors that influence the intentionality of healthcare professionals and managers in implementing Artificial Intelligence systems in order to promote greater efficiency and more significant health gains?—was answered through a quantitative methodology, namely through structural equation modelling (SEM).
In the field of social sciences, there has been an exponential growth of data analysis in terms of technological and computational development. SEM has been one of the most studied data analysis techniques over the last few years and the model is based on a statistical method increasingly used in the field of social sciences for its ability to be able to explain and predict specific behaviours of individuals, groups, or organisations (
Tarka, 2018). The technique behind the SEM methodology results from the dichotomy between an exploratory and predictive character. Additionally, the user-friendly software, SmartPLS, requires little technical knowledge for model development and testing (
Hair et al., 2019). This methodology allows estimation of how causal relationships are established, defined from a single model. The objective involves being able to analyse the complexity of a system through a set of concepts and indicators obtained with latent variables and observed/manifested variables (
Civelek, 2018). The methodology developed enables multivariate data analysis to be performed and the behaviour of multiple variables to be studied simultaneously.
SEM represents the link between Path Analysis (PA) and Confirmatory Factor Analysis (CFA). CFA is based on the idea that a set of variables can be expressed differently for the same concept; on the other hand, PA consists of a model that evaluates the relationship between the variables measured in a direct or indirect way.
The partial least squares approach (PLS-SEM), also known as Path Modelling, seeks to maximise the variance between the dependent variables in the model and is used in an exploratory research context. With the linear relationships established, it is possible to study the complex links between the latent variables and the observed variables. To simplify this analysis, it is possible to perform a graphical representation from a diagram called Path Model (PL) (
Civelek, 2018).
The measurement of latent constructs is performed indirectly, mainly using a set of observable variables and by observing the causal effects on SEM between the respective latent variables (
Tarka, 2018). According to this approach, there are two steps that are important to highlight. The first tests the credibility, factor loading, and quality of fit for each scale in the study. The second step focuses on the structural model and the relationship between constructs, describing the details of each construct in the model (
Tarka, 2018).
SEM is a tool that allows the measurement of the direct or indirect effect of the explanatory variable on the dependent one, while factor analysis cannot establish these causal relationships (
Civelek, 2018). According to
Hair et al. (
2019), the reasons behind the growth in demand for PLS-SEM models is due to the ability of this methodology to understand the complexity inherent in models that include several constructs, indicators and possible relationships between these indicators, without imposing a particular distribution on the data, and to the fact that structural equation models take measurement errors into particular consideration (
Hair et al., 2019).
The PLS-SEM methodology does not merely recognise individual factors or behaviours but also seeks to determine the cause–effect links between scientific areas of interest, as well as understand the complexity inherent in social reality (
Tarka, 2018). SEM is used to test partial least squares models and is based on a variance-based structural equation modelling technique. The 3.3.9. version of the SmartPLS 3 software (
Tarka, 2018) was used to perform this analysis along with a bootstrap with 5000 resamples and bias-corrected and accelerated 95% confidence intervals. To reach the results interpretation phase, the reliability and validity of the measurement model were assessed in the first instance and, subsequently, the structural model was assessed. To assess the quality of the measurement model, the following criteria were assessed: individual indicators of reliability, convergent validity, internal consistency reliability, and discriminant validity (
Hair et al., 2019).
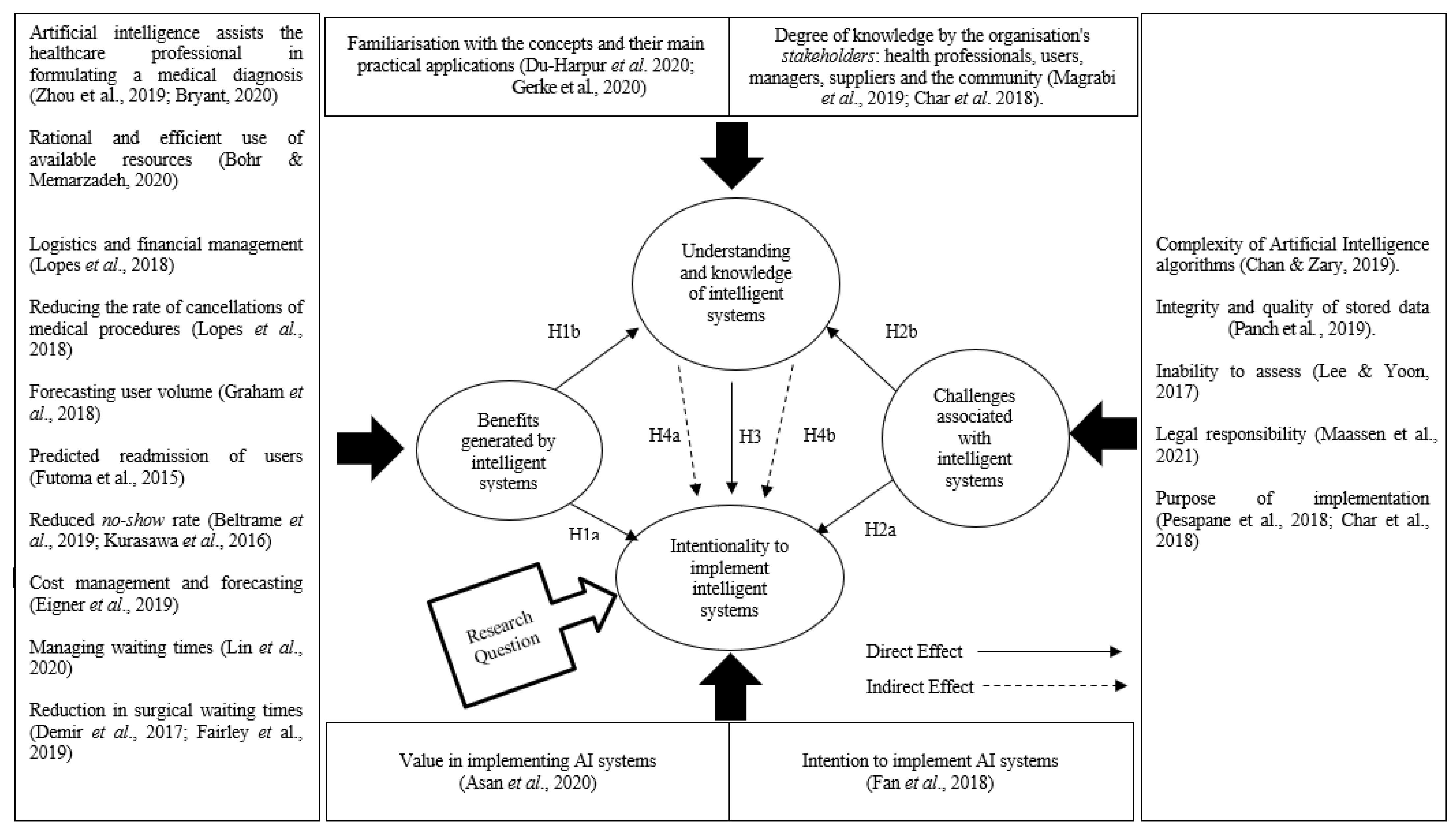
In
Figure 1, it is possible to analyse in detail the information that the integrated conceptual model created to answer this research question. According to the same, the following hypotheses were formulated:
H1a. The benefits generated by intelligent systems positively impact the intention to implement this type of system.
H1b. Benefits generated by intelligent systems positively impact perceptions and knowledge about intelligent systems.
H2a. The challenges associated with the use of intelligent systems negatively impact the intention to implement these types of systems.
H2b. The challenges associated with the use of intelligent systems negatively impact perceptions and knowledge about intelligent systems.
H3. Perception and knowledge about intelligent systems positively impacts the intention to implement this type of system.
H4a. Perception and knowledge about intelligent systems mediates the effect between the benefits generated by intelligent systems and the intention to implement this type of system.
H4b. Perception and knowledge about intelligent systems mediates the effect between the challenges associated with the use of intelligent systems and the intention to implement these types of systems.
2.2. Characterisation of the Sample
The sample was composed of 100 respondents. Participants were recruited via professional networks, including LinkedIn and direct institutional contacts. Out of approximately 240 eligible professionals invited, 100 completed the survey, resulting in a 41.7% response rate.
Initially, the variables that could characterise the sample regarding their professional activity, age group, and professional experience were analysed. In the end, a quantitative analysis of the answers was performed to obtain the data necessary to draw theoretical and empirical conclusions.
Out of a total of 100 respondents, 61% are health professionals and 39% hold management positions in the health area. Regarding the age range, 46% of respondents are less than 35 years old, 44% are between 35 and 45 years old, and 10% are over 45 years old. With regard to professional experience, 25% of the respondents have professional experience of less than 5 years, 22% have professional experience of more than 5 years, and 53% have professional experience of more than 10 years.
On the health professionals’ side, 38% of these health professionals are doctors, 18% are senior technicians in diagnosis and therapy, 21% are nurses, 6% are medical students, and 17% are pharmacists.
Regarding management, 15% of the respondents are hospital administrators, 10% are members of a hospital administration board, 5% are infrastructure and safety managers, 12% are service directors, 15% are hospital production managers, 28% are responsible for the quality department, 14% are operating room managers, and 11% perform supply and logistics functions.
3. Results
The results presented in this chapter aim to answer the previously formulated research question—what are the factors that influence the intentionality of health professionals and managers in implementing Artificial Intelligence systems to promote greater efficiency and more significant health gains?
Through an approach with two distinct phases, it was possible to analyse and interpret the results obtained. To answer the aforementioned question, the SEM-PLS methodology was used, through which the degree of reliability and validity of the measurement model was tested. Subsequently, the evaluation of the structural model was carried out (
Tarka, 2018). Four individual indicators allowed us to evaluate the quality of the measurement model, namely composite reliability, convergent validity, internal consistency reliability, and discriminant validity (
Hair et al., 2019).
The results obtained showed that the standardised factor loadings presented a value close to or greater than 0.6 and were significant when
p < 0.05, which demonstrates the reliability of the individual indicators (
Hair et al., 2019). The internal reliability was confirmed since all the composite reliability values of the constructs showed a value greater than 0.7 (
Hair et al., 2019), as represented in
Table 1.
According to the table, it is possible to verify that convergent validity was confirmed by respecting the minimum values for the three criteria (
Tarka, 2018). The first criterion needs all items to have positive and significant values, as is indeed observable (
Hair et al., 2019). For the second criterion to be properly validated, all constructs must have composite reliability (CR) values greater than 0.70, which is also observed (
Hair et al., 2019). The last criterion, average variance extracted (AVE), is represented on the diagonal of the table in bold and should have a value close to or greater than 0.50 (
Hair et al., 2019).
Discriminant validity was assessed through two approaches. Initially, we used the
Fornell and Larcker (
1981) criterion, which requires the value of the square root of the AVE to be higher than the value of the highest correlation established between constructs. Subsequently, the HTMT (heterotrait–monotrait ratio) criterion was used. According to
Hair et al. (
2019), these values should be lower than 0.85 for the model to be more robust as to its discriminant validity, and these values are also reflected in the table above.
Before performing the structural model assessment, the collinearity was checked. It was concluded that all items of the structural model did not present collinearity among themselves, as the VIF values ranged between 1.303 and 4.313, which is below the indicative critical value of 5 proposed by
Hair et al. (
2019). As far as the evaluation of the structural model is concerned, three main points were considered. In the first instance, the sign, magnitude, and significance of the structural path coefficients were analysed. Subsequently, the magnitude of the value of R2 for each of the endogenous variables was assessed as a measure of the model’s predictive accuracy. Finally, through Stone–Geisser’s Q2 values, the extent of the model’s predictive relevance was assessed (
Hair et al., 2019). The values for R2, the coefficient of determination, for the endogenous variables “Perception and knowledge about smart systems” and “Intention to implement smart systems” were 17.3% and 46.8%, respectively, a value that is higher than the minimum value of 10% (
Falk, 2014). Stone–Geisser’s Q values2 for each endogenous variable, 0.063 and 0.349, respectively, were shown to be above zero, indicating the predictive relevance of the model (
Hair et al., 2019).
As mentioned earlier, through SEM it is possible to measure the direct or indirect effect of variables. The following table illustrates how these relationships are established.
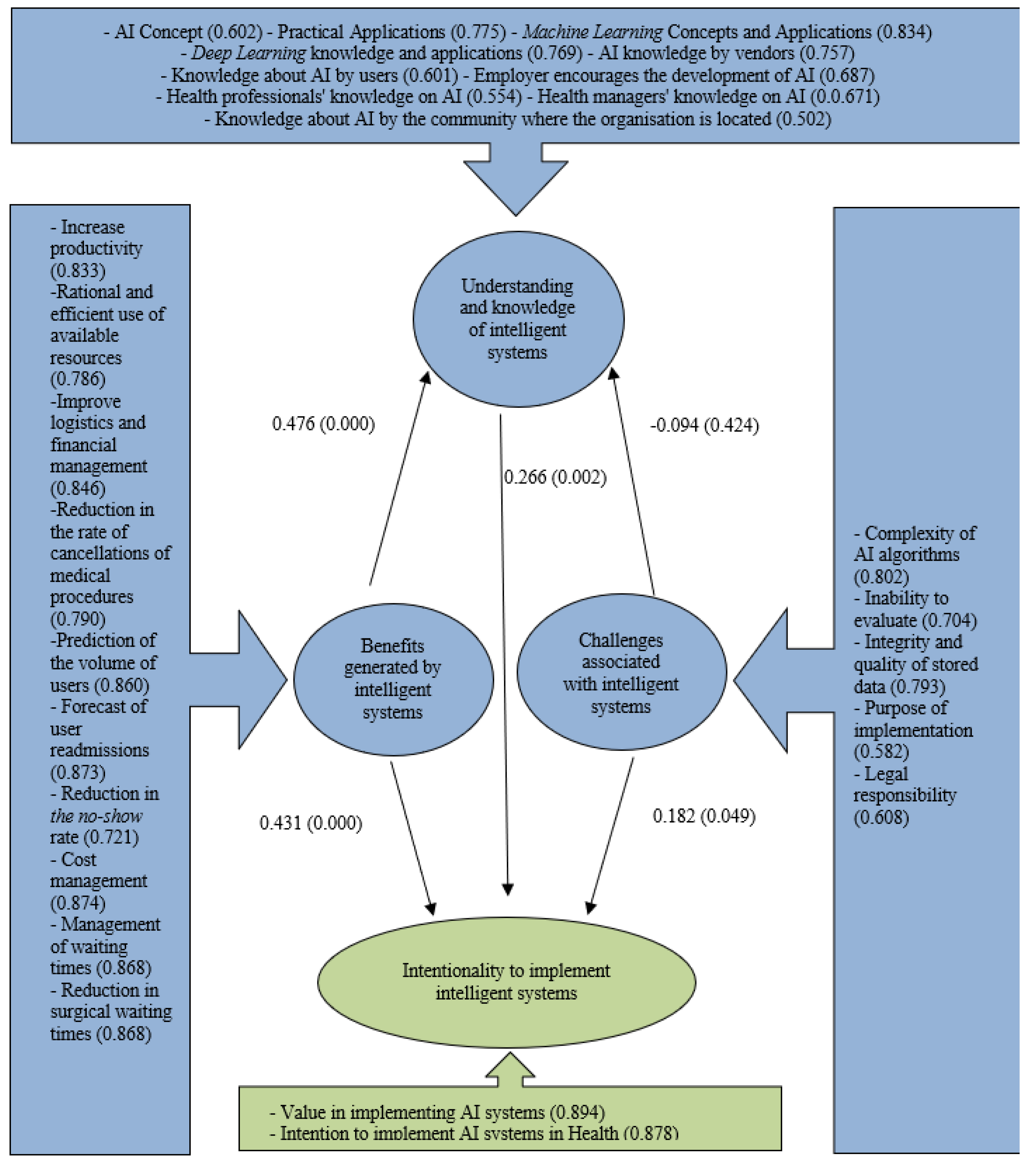
The results in
Table 2 show that the benefits generated by intelligent systems have a significantly positive effect on the intention to implement these systems in the health area (ß = 0.431,
p < 0.05), as well as on the perception associated with this type of technology (ß = 0.476,
p < 0.05).
Table 2 also shows that, contrary to what the authors argue, the challenges in implementing this type of system have a significantly positive relationship in relation to the intention to apply them, demonstrating that the identified challenges are not seen as a barrier to the intention to apply AI systems in the health area (ß = 0.182,
p < 0.05).
Regarding hypothesis H2b, it is not possible to determine whether the challenges associated with the use of intelligent systems negatively impact the perception and knowledge about intelligent systems, since the tested hypothesis is not statistically significant as it has a p-value greater than 0.05 (ß = −0.025, p value = 0.448). Thus, it is not possible to prove hypothesis H2b.
Finally, it can be proven by the figures in
Table 2 that perception and knowledge about intelligent systems has a significantly positive relationship with the intention to implement the same systems (ß = 0.266,
p < 0.05), thus supporting hypothesis H3.
To test the mediation hypotheses (H4a and H4b) and using the SmartPLS 3 tool, the bootstrapping method was used to test the level of significance of indirect effects through a mediator (
Tarka, 2018).
Table 3 shows the mediation effects.
Through the table it is possible to verify that the indirect effects of the benefits generated by intelligent systems on the intention to implement this type of system through the mediators perception or knowledge have a significantly positive relationship (ß = 0.127, p < 0.05), supporting hypothesis H4a.
According to the same table, it is not possible to determine whether perception and knowledge about smart systems mediates the effect between the challenges associated with the implementation of smart systems and the intention to implement them, since the tested hypothesis is not statistically significant as it presents a p-value greater than 0.05 (ß = −0.025, p Value = 0.458). Thus, it is not possible to prove hypothesis H4b.
Following on from the result analysis, it is possible to verify which of the research model hypotheses were accepted.
Table 4 summarises the value of ß and its statistical significance for each of the hypotheses tested, supporting the decision to accept or reject each of the hypotheses.
4. Discussion
The findings and their implications should be discussed in the broadest context possible. Future research directions may also be as shown in
Figure 1; the conceptual model was subjected to several tests using the SmartPLS 3 tool. According to the model figure, three factors were identified that foster the possibility of implementing AI systems in the health area, namely the perception and knowledge about intelligent systems (
Char et al., 2018;
Magrabi et al., 2019;
Nelson et al., 2020), the benefits generated by smart systems (
Letourneau-Guillon et al., 2020;
Dossou et al., 2021), and the challenges associated with the implementation of smart systems (
Gerke et al., 2020;
Panch et al., 2019).
In order to arrive at the three factors identified, the indicators of each of the factors were individually assessed through the questionnaire (
Figure 2). In the vast majority, the indicators proved to be relevant to the study by obtaining scores above 0.6, which tells us that the chosen indicators are reliable indicators when
p < 0.05 (
Hair et al., 2019).
The benefits generated by intelligent systems have also been shown to be aligned with the theories advocated by the authors, insofar as the main benefits include increasing productivity through case prioritisation (
Bryant, 2020), using the available resources rationally and efficiently (
Bohr & Memarzadeh, 2020), improving logistics and financial management (
Lopes et al., 2018), reducing the cancellation rates of certain medical procedures (
Lopes et al., 2018); predicting user volume (
Graham et al., 2018), predicting the level of user readmissions (
Futoma et al., 2015), reducing the no-show rate (
Beltrame et al., 2019;
Kurasawa et al., 2016), managing costs (
Eigner et al., 2019), managing waiting times (
Lin et al., 2020), and reducing surgical waiting times (
Demir et al., 2017;
Fairley et al., 2019).
Finally, the result of the challenges generated by the implementation of intelligent systems is not in full agreement with the authors studied. According to the conceptual model, the level of trust of healthcare professionals (
Maassen et al., 2021), the level of user perception and acceptance, as well as user trustworthiness (
Zhang et al., 2021), the violation of ethical and privacy issues (
Gerke et al., 2020;
Maassen et al., 2021), and medical students’ attitudes towards AI systems (
Sit et al., 2020) proved to be of little significance when it comes to influencing the intentionality of managers and health professionals in the process of implementing intelligent systems, so they were excluded from the model.
After identifying the three categories with an impact on the intention to implement AI systems in the health area, the hypotheses were tested. Concerning the direct effects, the results show that the benefits generated by intelligent systems positively impact the intention of managers and health professionals to implement these systems, confirming hypothesis H1a of this study. According to the authors studied, the benefits that AI systems bring, whether in terms of clinical practice, through aiding the formulation of diagnoses (
Letourneau-Guillon et al., 2020), or in terms of health management (
Dossou et al., 2021), through logistical planning and the optimisation of available resources, increase the likelihood that these professionals will adopt intelligent systems.
In addition, based on the results, it can be concluded that the benefits generated by intelligent systems have a positive impact on the perception and knowledge about this type of technology, thus confirming hypothesis H1b. This hypothesis reflects the importance of making public the advances that AI systems have been causing in the health area, serving as a stimulus for the scientific community, which includes these professionals, to deepen their knowledge so as to promote the use of these technologies in Portuguese health institutions (
Nelson et al., 2020).
Regarding the challenges associated with the implementation of intelligent systems, the results do not support what the authors argue (
Panch et al., 2019;
Gerke et al., 2020). In other words, one would expect challenges to be an obstacle in the face of the intention to implement AI systems; however, this is not the case. According to the results obtained, challenges do not constitute a barrier to the intention to adopt these systems. The rejection of hypothesis H2a demonstrates that the challenges identified by users do not decrease the incentives to use AI systems. According to
Schwendicke et al. (
2020), despite the recognition of several challenges in the implementation of these systems, the authors believe that AI has the potential to revolutionise the health area and overcome concerns about data protection and security, as well as to help managers and health professionals make decisions that promote better healthcare.
Regarding the impacts that perception and knowledge have on the intention to implement AI systems, it was possible to confirm through the results that the higher the level of knowledge by all stakeholders, the higher the intention to implement intelligent systems. According to
Magrabi et al. (
2019), it is necessary to involve the various stakeholders, namely nurses, physicians, computer scientists, mathematicians, managers, and investors, in the process of implementing an AI tool. It therefore becomes pivotal to establish communication bridges so that everyone understands what is being accomplished (
Char et al., 2018).
Finally, considering the indirect effects of the benefits generated by intelligent systems on the intention to implement them, through the mediators of perception and knowledge, the results showed that the impact generated is positive, thus confirming the mediation hypothesis H4b. Thus, it is possible to state that the increase in benefits could arouse people’s interest and encourage them to deepen their knowledge about these types of technologies, and, consequently, positively impact the intention to move towards their implementation (
Asan et al., 2020). According to
Fan et al. (
2020), the expectations of the performance of smart systems and the initial trust that is placed in smart systems impact the intention to adopt these technologies. The same authors state that the people who have higher levels of confidence in AI are precisely the people who have a higher perception of these matters and who end up showing greater intention to implement AI tools.
The findings should be interpreted in light of the Portuguese healthcare context, characterised by a centralised public system, slow digital transformation, and cautious regulatory frameworks. These structural characteristics may limit generalizability to more privatised or technologically mature healthcare systems.
5. Conclusions
The present research indicates a higher intention to adopt AI tools by healthcare professionals and managers. The question developed from the literature review sought to understand which factors contribute to the implementation of AI tools by health professionals and managers. The variables identified were divided into three groups, namely the perception and knowledge about intelligent systems, the benefits generated by intelligent systems, and the challenges associated with the implementation of these systems.
In turn, the answers to the questionnaire allowed us to draw some conclusions about the possibility of implementing intelligent systems in the health area and to discuss, in agreement with the authors found, which were the main benefits and challenges encountered, according to the perception and knowledge of each of the respondents.
With regard to the benefits, as addressed throughout the literature review, it was possible to verify that the main motivations for the implementation of AI systems in the health area are related to the aid of these systems in the formulation of a medical diagnosis (
Zhou et al., 2019;
Bryant, 2020), in the rational and efficient use of available resources (
Bohr & Memarzadeh, 2020), in the improvement of logistics and financial management (
Lopes et al., 2018), in predicting user volume (
Graham et al., 2018), in predicting user readmissions (
Futoma et al., 2015), in reducing the no-show rate (
Beltrame et al., 2019;
Kurasawa et al., 2016), in managing costs (
Eigner et al., 2019), in managing waiting times (
Lin et al., 2020), and in reducing surgical waiting times (
Demir et al., 2017;
Fairley et al., 2019).
Although the introduction of AI in healthcare is at an early stage, respondents recognise that the implementation of such systems will enhance the responsiveness provided by healthcare professionals and managers. Respondents recognise that the available data can be used to predict certain behaviours and generate value for healthcare institutions. According to
Dossou et al. (
2021), there is widespread optimism from the scientific community that the application of AI tools will provide substantial improvements in all areas of healthcare.
According to
Bohr and Memarzadeh (
2020), the health ecosystem is increasingly aware of the impact that technology can generate in healthcare. It is estimated that AI applications can reduce the costs associated with healthcare by increasingly focusing on the process of disease prevention and prediction. In practical terms, this is expected to result in fewer hospitalisations and a reduced number of treatments. Respondents also believe that this technology will play an important role in users’ health, as it will help people to be diagnosed earlier and with more personalised follow-ups (
Letourneau-Guillon et al., 2020).
On the other hand, for the same group of respondents, it was possible to identify the main challenges. These challenges are related to the complexity of the Artificial Intelligence algorithms (
Issa et al., 2024), the integrity and quality of the stored data (
Panch et al., 2019), the inability to evaluate (
Lee & Yoon, 2017), the legal liability (
Maassen et al., 2021), and the purpose of the implementation (
Pesapane et al., 2018;
Char et al., 2018). In this sense, and according to the authors studied, there are several implications from the challenges associated with the implementation of these systems which end up creating barriers that do not encourage the intention to use this type of technology to improve care delivery; however, according to the conceptual model developed, these challenges have not been shown to have a negative impact on this same intention.
In a first instance, the conclusion may be drawn that the benefits outweigh the challenges and that it will be difficult to counter the impact that AI tools are already demonstrating in healthcare; however, the respondents’ non-valuation of the challenges may also be related to a low level of perception and knowledge of them (
Wood et al., 2021).
According to the degree of perception of each of the respondents, it should be noted that respondents who claimed to have more knowledge have a greater intention to implement this type of systems (
Du-Harpur et al., 2020;
Gerke et al., 2020). However, in order to make use of AI tools it is necessary to involve all the stakeholders. According to
Manne and Kantheti (
2021), governmental support will be crucial. It is therefore important to invest in training, not only of health professionals and managers, but also of people who have the necessary capacity to regulate this type of technology and overcome issues related to ethical and legal violations (
Magrabi et al., 2019). This research aims to contribute to the introduction of intelligent systems in healthcare. The practical examples are based on two main strands of action, namely the strand connected to clinical practice and the strand connected to the health management area. Thus, it is possible to make known the main benefits and challenges of the adoption of intelligent systems.
6. Theoretical and Practical Implications
This study contributes to the theoretical understanding of technology adoption in healthcare by confirming the mediating role of knowledge and perception in the relationship between perceived benefits and the intention to implement AI systems. The findings support prior theoretical models that emphasise the importance of cognitive and affective constructs in the adoption of innovations, particularly in complex and highly regulated environments such as healthcare. Additionally, the study extends the literature by highlighting that perceived challenges do not necessarily hinder intention, suggesting a potential shift in how professionals cognitively appraise barriers when benefits are sufficiently salient.
For clinicians, the research results underscore the importance of AI literacy training, as familiarity and understanding of intelligent systems positively influence intention to adopt. AI solutions should also be aligned with clinical routines to reduce resistance.
Practical implications for managerial staff include investing in communication strategies to promote perceived benefits, as well as creating implementation plans that consider the strategic alignment between AI systems and health service goals. Managers should also prioritise stakeholder involvement during the adoption process.