A Biomechanical Comparison of Therapeutic Footwear and Athletic and Low-Cost Generic Shoes: Effects on Plantar Pressure, Lower Extremity Kinematics, and Kinetics
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Materials and Instruments
2.3. Procedures
2.4. Data Analysis
3. Results
3.1. Gait Temporospatial Characteristics
3.2. Gait Kinematics and Kinetics
3.3. Peak Plantar Pressure
3.4. Relation Between Peak Plantar Pressure (PPP) and Gait Parameters
3.5. Comfort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MTP | Metatarsophalangeal |
| MBT | Masai Barefoot Technology |
| EVA | ethyl vinyl acetate |
| GRFz | vertical ground reaction force |
| PPP | peak plantar pressure |
Appendix A
| Type of Shoes | Insole |
|---|---|
| Generic |  |
| Orthofeet—Athletic |  |
| Orthofeet—Dress |  |
| Participants’ shoes (Nike) |  |
| Shoe Type | Upper Material | Midsole Material | Outsole Material | Weight (Men’s Shoe Size) |
|---|---|---|---|---|
| OrthoFeet Dress | Leather | EVA | Rubber | 365 g (9M) |
| OrthoFeet Athletic | Synthetic mesh | EVA | Rubber | 387 g (9M) |
| Low-cost Generic | Synthetic mesh | EVA | Rubber | 298 g (9M) |
| Participants’ shoes (Nike) | Synthetic mesh | EVA | Rubber | 286 g (9M) |
| Participants’ shoes (New Balance) | Synthetic mesh | EVA | Rubber | 280 g (9M) |
| Participant # | Body Height (cm) | Body Mass (kg) | Shoe Size | Age (yrs) | Gender | Type of Participant’s Shoes |
|---|---|---|---|---|---|---|
| 1 | 172 | 68 | 8 | 36 | F | New balance |
| 2 | 170 | 65 | 8 | 41 | F | New balance |
| 3 | 165 | 57 | 7.5 | 27 | F | New balance |
| 4 | 152 | 78 | 7.5 | 26 | F | Nike |
| 5 | 159 | 53 | 7.5 | 26 | F | Nike |
| 6 | 161 | 49 | 8 | 28 | F | Nike |
| 7 | 167 | 61 | 8.5 | 30 | F | Nike |
| 8 | 170 | 65 | 8 | 39 | F | New balance |
| 9 | 172 | 54 | 8 | 24 | M | Addidas |
| 10 | 174 | 78 | 7.5 | 35 | M | Nike |
| 11 | 175 | 73 | 9.5 | 36 | M | Nike |
| 12 | 186 | 86 | 10.5 | 26 | M | Nike |
| 13 | 172 | 70 | 9.5 | 48 | M | Addidas |
| 14 | 180 | 78 | 10.5 | 39 | M | New balance |
| 15 | 177 | 73 | 10.5 | 34 | M | New balance |
| 16 | 177 | 85 | 9.5 | 33 | M | Nike |
| 17 | 163 | 61 | 7.5 | 36 | M | Nike |
| 18 | 178 | 73 | 9.5 | 28 | M | Nike |
| 19 | 180 | 75 | 9.5 | 32 | M | New balance |
| 20 | 180 | 80 | 10.5 | 38 | M | New balance |
| Mean (SD) | 171.5 (8.4) | 69.1 (10.7) | 8.8 (1.2) | 33.1 (6.2) |
References
- Pecoraro, R.E.; Reiber, G.E.; Burgess, E.M. Pathways to diabetic limb amputation: Basis for prevention. Diabetes Care 1990, 13, 513–521. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A. Clinical Care of the Diabetic Foot; American Diabetes Association: Alexandria, Virginia, 2005. [Google Scholar]
- Singh, N.; Armstrong, D.G.; Lipsky, B.A. Preventing foot ulcers in patients with diabetes. JAMA 2005, 293, 217–228. [Google Scholar] [CrossRef]
- Chamberlain, R.C.; Fleetwood, K.; Wild, S.H.; Colhoun, H.M.; Lindsay, R.S.; Petrie, J.R.; McCrimmon, R.J.; Gibb, F.; Philip, S.; Sattar, N.; et al. Foot Ulcer and Risk of Lower Limb Amputation or Death in People With Diabetes: A National Population-Based Retrospective Cohort Study. Diabetes Care 2022, 45, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Boyko, E.J.; Zelnick, L.R.; Braffett, B.H.; Pop-Busui, R.; Cowie, C.C.; Lorenzi, G.M.; Gubitosi-Klug, R.; Zinman, B.; de Boer, I.H. Risk of Foot Ulcer and Lower-Extremity Amputation Among Participants in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study. Diabetes Care 2022, 45, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Arts, M.L.; Waaijman, R.; de Haart, M.; Keukenkamp, R.; Nollet, F.; Bus, S.A. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet. Med. 2012, 29, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Alkhatieb, M.T.; Alkhalifah, H.A.; Alkhalifah, Z.A.; Aljehani, K.M.; Almalki, M.S.; Alqarni, A.A.; Alqurashi, S.Z.; Alzahrani, R.A. The effect of therapeutic footwear on the recurrence and new formation of foot ulcers in previously affected diabetic patients in Jeddah, Saudi Arabia. J. Tissue Viability 2023, 32, 417–422. [Google Scholar] [CrossRef]
- Janisse, D.J. Shoes and shoe modifications. In AAOS Atlas of Orthoses and Assistive Devices, 4th ed.; Mosby: Philadelphia, PA, USA, 2008; pp. 325–333. [Google Scholar]
- Bowling, F.L.; Reeves, N.D.; Boulton, A.J. Gait-related strategies for the prevention of plantar ulcer development in the high risk foot. Curr. Diabetes Rev. 2011, 7, 159–163. [Google Scholar] [CrossRef]
- Praet, S.F.; Louwerens, J.W. The influence of shoe design on plantar pressures in neuropathic feet. Diabetes Care 2003, 26, 441–445. [Google Scholar] [CrossRef]
- van Schie, C.; Ulbrecht, J.S.; Becker, M.B.; Cavanagh, P.R. Design criteria for rigid rocker shoes. Foot Ankle Int. 2000, 21, 833–844. [Google Scholar] [CrossRef]
- Haworth, L.; Booth, N.; Chohan, A.; Chapman, G.; Richards, J. How does orthotic walker boot design influence lower limb and trunk function during gait? Prosthet. Orthot. Int. 2025, 49, 66–75. [Google Scholar] [CrossRef]
- Hutchins, S.; Bowker, P.; Geary, N.; Richards, J. The biomechanics and clinical efficacy of footwear adapted with rocker profiles—Evidence in the literature. Foot 2009, 19, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, M.M.; Nourani, A. Testing the effects of footwear on biomechanics of human body: A review. Heliyon 2025, 11, e42870. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, M.; Tateuchi, H.; Takeoka, T.; Ichihashi, N. Kinematic and kinetic characteristics of Masai Barefoot Technology footwear. Gait Posture 2012, 35, 567–572. [Google Scholar] [CrossRef]
- Chang, B.C.; Liu, D.H.; Chang, J.L.; Lee, S.H.; Wang, J.Y. Plantar pressure analysis of accommodative insole in older people with metatarsalgia. Gait Posture 2014, 39, 449–454. [Google Scholar] [CrossRef]
- Lin, S.C.; Chen, C.P.; Tang, S.F.; Wong, A.M.; Hsieh, J.H.; Chen, W.P. Changes in windlass effect in response to different shoe and insole designs during walking. Gait Posture 2013, 37, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, A.K.; John, M.C.; Arnold, G.P.; Cochrane, L.; Abboud, R.J. The effects of off-the-shelf in-shoe heel inserts on forefoot plantar pressure. Gait Posture 2008, 28, 533–537. [Google Scholar] [CrossRef]
- Zhang, X.; Li, B. Influence of in-shoe heel lifts on plantar pressure and center of pressure in the medial-lateral direction during walking. Gait Posture 2014, 39, 1012–1016. [Google Scholar] [CrossRef]
- Shuang, J.; Haron, A.; Massey, G.; Mansoubi, M.; Dawes, H.; Bowling, F.L.; Reeves, N.D.; Weightman, A.; Cooper, G. The effect of calcaneus and metatarsal head offloading insoles on healthy subjects’ gait kinematics, kinetics, asymmetry, and the implications for plantar pressure management: A pilot study. PLoS ONE 2024, 19, e0303826. [Google Scholar] [CrossRef]
- Malki, A.; Hajibozorgi, M.; Verkerke, G.J.; Dekker, R.; Hijmans, J.M. Plantar pressure reduction in the heel region through self-adjusting insoles with a heel cup in standard and individualized rocker shoes. Clin. Biomech. 2024, 116, 106281. [Google Scholar] [CrossRef]
- Lavery, L.A.; Vela, S.A.; Fleischli, J.G.; Armstrong, D.G.; Lavery, D.C. Reducing plantar pressure in the neuropathic foot. A comparison of footwear. Diabetes Care 1997, 20, 1706–1710. [Google Scholar] [CrossRef]
- Uccioli, L.; Faglia, E.; Monticone, G.; Favales, F.; Durola, L.; Aldeghi, A.; Quarantiello, A.; Calia, P.; Menzinger, G. Manufactured shoes in the prevention of diabetic foot ulcers. Diabetes Care 1995, 18, 1376–1378. [Google Scholar] [CrossRef] [PubMed]
- Bus, S.A.; Waaijman, R.; Arts, M.; de Haart, M.; Busch-Westbroek, T.; van Baal, J.; Nollet, F. Effect of custom-made footwear on foot ulcer recurrence in diabetes: A multicenter randomized controlled trial. Diabetes Care 2013, 36, 4109–4116. [Google Scholar] [CrossRef] [PubMed]
- Myers, K.A.; Long, J.T.; Klein, J.P.; Wertsch, J.J.; Janisse, D.; Harris, G.F. Biomechanical implications of the negative heel rocker sole shoe: Gait kinematics and kinetics. Gait Posture 2006, 24, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Van Bogart, J.J.; Long, J.T.; Klein, J.P.; Wertsch, J.J.; Janisse, D.J.; Harris, G.F. Effects of the toe-only rocker on gait kinematics and kinetics in able-bodied persons. IEEE Trans. Neural Syst. Rehabil. Eng. 2005, 13, 542–550. [Google Scholar] [CrossRef]
- Nouman, M.; Apiputhanayut, R.; Narungsri, T.; Tipchatyotin, S.; Dissaneewate, T. Comparative Analysis of Three Types of Therapeutic Offloading Diabetic Shoes With Custom Made Insole on Plantar Pressure Distribution in Severe Diabetic Charcot Foot. Can. Prosthet. Orthot. J. 2024, 7, 41780. [Google Scholar] [CrossRef]
- Chung, M.J.; Wang, M.J. Gender and walking speed effects on plantar pressure distribution for adults aged 20–60 years. Ergonomics 2012, 55, 194–200. [Google Scholar] [CrossRef]
- Drew Shoes. Available online: https://www.drewshoe.com/ (accessed on 2 April 2025).
- OrthoFeet Therapeutic Shoes. Available online: https://www.orthofeet.com/collections/men-shoes (accessed on 2 April 2025).
- Low Cost Therapeutic Shoes. Available online: https://tinyurl.com/535bz648 (accessed on 2 April 2025).
- Rabi, D.M.; Edwards, A.L.; Southern, D.A.; Svenson, L.W.; Sargious, P.M.; Norton, P.; Larsen, E.T.; Ghali, W.A. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv. Res. 2006, 6, 124. [Google Scholar] [CrossRef]
- Arin-Bal, G.; Livanelioglu, A.; Leardini, A.; Belvedere, C. Correlations between plantar pressure and postural balance in healthy subjects and their comparison according to gender and limb dominance: A cross-sectional descriptive study. Gait Posture 2024, 108, 124–131. [Google Scholar] [CrossRef]
- Putti, A.B.; Arnold, G.P.; Abboud, R.J. Foot pressure differences in men and women. Foot Ankle Surg. 2010, 16, 21–24. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef]
- Leardini, A.; Sawacha, Z.; Paolini, G.; Ingrosso, S.; Nativo, R.; Benedetti, M.G. A new anatomically based protocol for gait analysis in children. Gait Posture 2007, 26, 560–571. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Biomechanics and Motor Control of Human Movement; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Castro, M.; Abreu, S.; Sousa, H.; Machado, L.; Santos, R.; Vilas-Boas, J.P. Ground reaction forces and plantar pressure distribution during occasional loaded gait. Appl. Ergon. 2013, 44, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Perry, J. Gait Analysis: Normal and Pathological Function; SLACK Incorporated: Thorofare, NJ, USA, 1992. [Google Scholar]
- Wu, W.L.; Rosenbaum, D.; Su, F.C. The effects of rocker sole and SACH heel on kinematics in gait. Med. Eng. Phys. 2004, 26, 639–646. [Google Scholar] [CrossRef]
- Boulton, A.J.; Hardisty, C.A.; Betts, R.P.; Franks, C.I.; Worth, R.C.; Ward, J.D.; Duckworth, T. Dynamic foot pressure and other studies as diagnostic and management aids in diabetic neuropathy. Diabetes Care 1983, 6, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; Armstrong, D.G.; Wunderlich, R.P.; Tredwell, J.; Boulton, A.J. Predictive value of foot pressure assessment as part of a population-based diabetes disease management program. Diabetes Care 2003, 26, 1069–1073. [Google Scholar] [CrossRef]
- Urry, S. Plantar pressure-measurement sensors. Meas. Sci. Technol. 1999, 10, 16–32. [Google Scholar] [CrossRef]
- Bryant, A.; Tinley, P.; Singer, K. Plantar pressure distribution in normal, hallux valgus and hallux limitus feet. Foot 1999, 9, 115–119. [Google Scholar] [CrossRef]
- Amemiya, A.; Noguchi, H.; Oe, M.; Ohashi, Y.; Ueki, K.; Kadowaki, T.; Mori, T.; Sanada, H. Elevated plantar pressure in diabetic patients and its relationship with their gait features. Gait Posture 2014, 40, 408–414. [Google Scholar] [CrossRef]
- Rao, S.R.; Saltzman, C.L.; Wilken, J.; Yak, H.J. Increased passive ankle stiffness and reduced dorsiflexion range of motion in individuals with diabetes mellitus. Foot Ankle Int. 2006, 27, 617–622. [Google Scholar] [CrossRef]
- Lavery, L.A.; Armstrong, D.G.; Boulton, A.J. Ankle equinus deformity and its relationship to high plantar pressure in a large population with diabetes mellitus. J. Am. Podiatr. Med. Assoc. 2002, 92, 479–482. [Google Scholar] [CrossRef]
- Ouattas, A.; Finco, M.G.; Dehghan Rouzi, M.; Azarian, M.; Rojas, A.Z.; Ochoa, M.B.; El-Refaei, N.; Momin, A.; Najafi, B. The role of therapeutic footwear to increase daily physical activity in older adults with chronic foot pain. Clin. Biomech. 2024, 123, 106373. [Google Scholar] [CrossRef] [PubMed]
- Finco, M.G.; Ouattas, A.; El-Refaei, N.; Momin, A.S.; Azarian, M.; Najafi, B. Assessing the Acceptability and Effectiveness of a Novel Therapeutic Footwear in Reducing Foot Pain and Improving Function among Older Adults: A Crossover Randomized Controlled Trial. Gerontology 2024, 70, 842–854. [Google Scholar] [CrossRef] [PubMed]
- Nurse, M.A.; Hulliger, M.; Wakeling, J.M.; Nigg, B.M.; Stefanyshyn, D.J. Changing the texture of footwear can alter gait patterns. J. Electromyogr. Kinesiol. 2005, 15, 496–506. [Google Scholar] [CrossRef] [PubMed]



| Category | Parameter | Athletic 1 | Dress 2 | Generic 3 | Own 4 |
|---|---|---|---|---|---|
| Temporospatial | Speed (m/s) | 1.25 (0.13) | 1.23 (0.12) | 1.27 (0.13) | 1.24 (0.11) |
| Stride length (m) | 1.39 (0.12) | 1.37 (0.17) | 1.38 (0.18) | 1.36 (0.10) | |
| Double support time (s) | 0.27 (0.08) | 0.27 (0.07) | 0.25 (0.06) | 0.23 (0.08) | |
| Joint kinematics (o) | Ankle dorsiflexion | 13.0 (3.5) 3,4 | 12.9 (3.4) 3,4 | 10.5 (3.4) 1,2 | 10.1 (2.6) 1,2 |
| Ankle plantar flexion | 14.7 (4.9) 2–4 | 16.4 (4.8) 1,3,4 | 17.8 (4.9) 1,2 | 19.2 (5.4) 1,2 | |
| Ankle range of motion | 27.8 (3.7) 2,4 | 29.3 (4.2) 1 | 28.4 (4.2) | 29.3 (3.6) 1 | |
| Knee 1st peak flexion | 18.0 (5.4) | 16.8 (5.0) | 16.9 (5.6) | 16.2 (7.3) | |
| Knee 2nd peak flexion | 65.0 (5.8) | 66.4 (6.1) | 65.8 (6.2) | 65.3 (7.0) | |
| Hip 1st peak flexion | 29.0 (3.9) | 28.7 (4.3) | 29.7 (3.6) 4 | 28.4 (3.6) 3 | |
| Hip peak extension | 15.5 (3.1) | 15.6 (4.0) | 15.3 (2.9) | 15.2 (3.5) | |
| Joint kinetics (Nm/kg) | Ankle plantar flexor | 1.41 (0.24) | 1.43 (0.24) 3 | 1.38 (0.24) 2 | 1.39 (0.24) |
| Knee flexor | 0.28 (0.12) | 0.25 (0.12) | 0.27 (0.10) | 0.28 (0.11) | |
| Knee extensor | 0.64 (0.27) | 0.63 (0.25) | 0.62 (0.26) | 0.64 (0.28) | |
| Hip flexor | 0.87 (0.20) | 0.83 (0.23) | 0.85 (0.22) | 0.86 (0.25) | |
| Hip extensor | 0.74 (0.32) | 0.67 (0.27) | 0.67 (0.27) | 0.66 (0.23) | |
| GRFz (BW) | 1st peak | 1.16 (0.11) | 1.15 (0.13) | 1.15 (0.12) | 1.15 (0.13) |
| 2nd peak | 1.12 (0.07) | 1.12 (0.08) | 1.12 (0.07) | 1.13 (0.08) | |
| Impulse (BW.GC%) | Propulsive | 4.19 (0.97) | 4.36 (1.2) | 4.33 (1.06) | 4.56 (1.08) |
| Braking | 4.37 (0.65) | 4.49 (0.76) | 4.5 (0.66) | 4.55 (0.69) | |
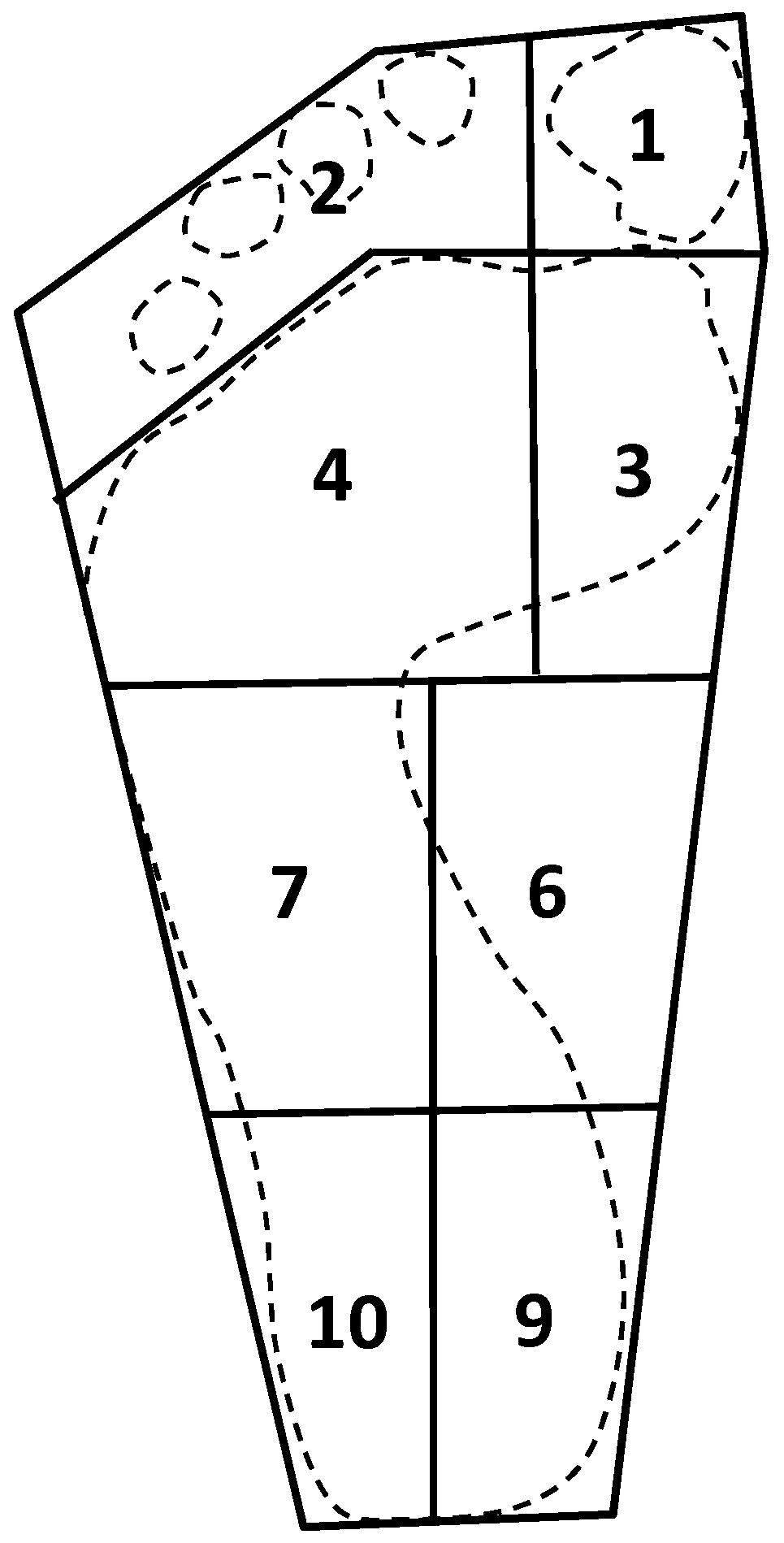
| Peak plantar pressure (kPa) | 1: Big toe | 294.5 (121.1) 2 | 400.0 (182.9) 1,3,4 | 270.1 (137.6) 2,4 | 330.0 (153.2) 2,3 |
| 2: Other toes | 134.8 (58.9) | 129.2 (64.8) | 131.3 (66.7) | 128.3 (56.8) | |
| 3: Medial forefoot | 267.6 (105.0) | 280.7 (118.8) | 261.2 (77.9) | 302.7 (116.4) | |
| 4: Lateral forefoot | 273.1 (97.2) | 292.5 (88.5) | 299.1 (97.3) | 309.0 (103.4) | |
| 5: Forefoot | 328.5 (97.3) | 352.5 (107.2) | 339.4 (89.7) | 355.6 (125.5) | |
| 6: Medial midfoot | 79.2 (49.9) | 106.9 (78.1) 3 | 52.3 (31.6) 2 | 83.0 (68.8) | |
| 7: Lateral midfoot | 99.1 (43.2) | 101.4 (32.7) | 111.8 (46.8) | 118.9 (46.6) | |
| 8: Midfoot | 113.3 (55.7) | 133.0 (70.9) | 117.4 (46.1) | 135.4 (74.8) | |
| 9: Medial hindfoot | 240.2 (79.1) 3 | 266.9 (99.7) | 290.6 (76.6) 1 | 267.2 (92.2) | |
| 10: Lateral hindfoot | 250.6 (92.3) | 247.5 (79.6) | 260.3 (64.1) | 263.6 (116.2) | |
| 11: Hindfoot | 272.7 (91.4) | 281.9 (100.1) | 304.0 (75.6) | 291.9 (115.8) | |
| Survey | Comfort rating (%) | 56.3 (20.8) 4 | 65.6 (16.4) 3,4 | 49.4 (17.5) 2,4 | 82.4 (15) 1,2,3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Liu, H.; Gao, F. A Biomechanical Comparison of Therapeutic Footwear and Athletic and Low-Cost Generic Shoes: Effects on Plantar Pressure, Lower Extremity Kinematics, and Kinetics. Biomechanics 2025, 5, 29. https://doi.org/10.3390/biomechanics5020029
Wang Q, Liu H, Gao F. A Biomechanical Comparison of Therapeutic Footwear and Athletic and Low-Cost Generic Shoes: Effects on Plantar Pressure, Lower Extremity Kinematics, and Kinetics. Biomechanics. 2025; 5(2):29. https://doi.org/10.3390/biomechanics5020029
Chicago/Turabian StyleWang, Qiu, Haibin Liu, and Fan Gao. 2025. "A Biomechanical Comparison of Therapeutic Footwear and Athletic and Low-Cost Generic Shoes: Effects on Plantar Pressure, Lower Extremity Kinematics, and Kinetics" Biomechanics 5, no. 2: 29. https://doi.org/10.3390/biomechanics5020029
APA StyleWang, Q., Liu, H., & Gao, F. (2025). A Biomechanical Comparison of Therapeutic Footwear and Athletic and Low-Cost Generic Shoes: Effects on Plantar Pressure, Lower Extremity Kinematics, and Kinetics. Biomechanics, 5(2), 29. https://doi.org/10.3390/biomechanics5020029






