Reliability of the Hip Extension Lower Exercise as a Measure of Eccentric Hamstring Strength
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
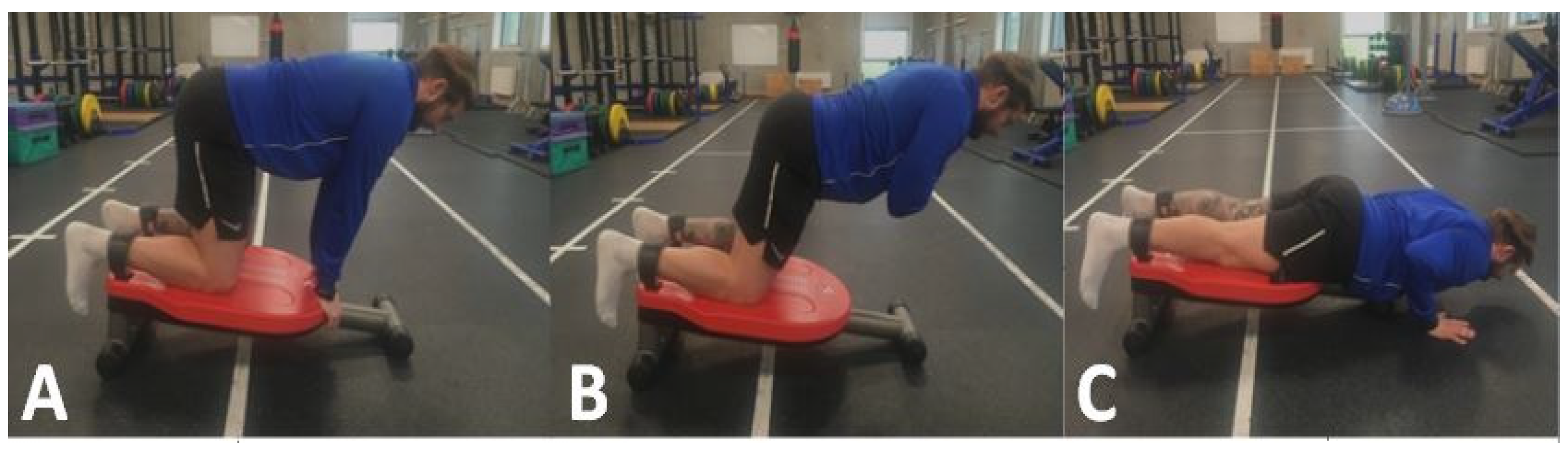
2.3. Methods and Materials
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, H.; Garrett, W.E.; Moorman, C.T.; Yu, B. Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J. Sport Health Sci. 2012, 1, 92–101. [Google Scholar] [CrossRef] [Green Version]
- Verrall, G.M.; Kalairajah, Y.; Slavotinek, J.P.; Spriggins, A.J. Assessment of player performance following return to sport after hamstring muscle strain injury. J. Sci. Med. Sport 2006, 9, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Hickey, J.; Shield, A.J.; Williams, M.D.; Opar, D.A. The financial cost of hamstring strain injuries in the Australian Football League. Br. J. Sports Med. 2014, 48, 729–730. [Google Scholar] [CrossRef] [Green Version]
- Ekstrand, J.; Hägglund, M.; Waldén, M. Epidemiology of muscle injuries in professional football (soccer). Am. J. Sports Med. 2011, 39, 1226–1232. [Google Scholar] [CrossRef] [Green Version]
- Ekstrand, J.; Hägglund, M.; Waldén, M. Injury incidence and injury patterns in professional football: The UEFA injury study. Br. J. Sports Med. 2011, 45, 553–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekstrand, J.; Waldén, M.; Hägglund, M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: A 13-year longitudinal analysis of the UEFA Elite Club injury study. Br. J. Sports Med. 2016, 50, 731–737. [Google Scholar] [CrossRef] [Green Version]
- Woods, C.; Hawkins, R.D.; Maltby, S.; Hulse, M.; Thomas, A.; Hodson, A. The Football Association Medical Research Programme: An audit of injuries in professional football—Analysis of hamstring injuries. Br. J. Sports Med. 2004, 38, 36–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Askling, C.M.; Karlsson, J.; Thorstensson, A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand. J. Med. Sci. Sports 2003, 13, 244–250. [Google Scholar] [CrossRef]
- Thelen, D.G.; Chumanov, E.S.; Best, T.M.; Swanson, S.C.; Heiderscheit, B.C. Simulation of biceps femoris musculotendon mechanics during the swing phase of sprinting. Med. Sci. Sport Exerc. 2005, 37, 1931–1938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Opar, D.A.; Williams, M.D.; Shield, A.J. Hamstring strain injuries: Factors that lead to injury and re-injury. Sports Med. 2012, 42, 209–226. [Google Scholar] [CrossRef] [PubMed]
- Opar, D.A.; Williams, M.D.; Timmins, R.G.; Hickey, J.; Duhig, S.J.; Shield, A.J. Eccentric hamstring strength and hamstring injury risk in Australian footballers. Med. Sci. Sport Exerc. 2015, 47, 857–865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, J.; Thorborg, K.; Nielsen, M.B.; Budtz-Jørgensen, E.; Hölmich, P. Preventive Effect of Eccentric Training on Acute Hamstring Injuries in Men’s Soccer: A cluster-randomized controlled trial. Am. J. Sports Med. 2011, 39, 2296–2303. [Google Scholar] [CrossRef] [PubMed]
- Hibbert, O.; Cheong, K.; Grant, A.; Beers, A.; Moizumi, T. A systematic review of the effectiveness of eccentric strength training in the prevention of hamstring muscle strains in otherwise healthy individuals. N. Am. J. Sports Phys. Ther. 2008, 3, 67–81. [Google Scholar] [PubMed]
- Petersen, J.; Hölmich, P. Evidence based prevention of hamstring injuries in sport. Br. J. Sports Med. 2005, 39, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Bourne, M.; Opar, D.; Williams, M.D.; Shield, A.J. Eccentric Knee Flexor Strength and Risk of Hamstring Injuries in Rugby Union. Am. J. Sports Med. 2015, 43, 2663–2670. [Google Scholar] [CrossRef] [PubMed]
- Croisier, J.-L.; Ganteaume, S.; Binet, J.; Genty, M.; Ferret, J.-M. Strength imbalances and prevention of hamstring injury in professional soccer players. Am. J. Sports Med. 2008, 36, 1469–1475. [Google Scholar] [CrossRef] [PubMed]
- Fousekis, K.; Tsepis, E.; Poulmedis, P.; Athanasopoulos, S.; Vagenas, G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: A prospective study of 100 professional players. Br. J. Sports Med. 2011, 45, 709–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vicens-Bordas, J.; Esteve, E.; Fort-Vanmeerhaeghe, A.; Clausen, M.B.; Bandholm, T.; Opar, D.; Shields, A.; Thorborg, K. Eccentric hamstring strength is associated with age and duration of previous season hamstring injury in male soccer players. Int. J. Sports Phys. Ther. 2020, 15, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Cholley, Y.; Nagel, M.; Poulos, N. The effect of body mass on eccentric knee-flexor strength assessed with an instrumented Nordic hamstring device (Nordbord) in football players. Int. J. Sports Physiol. Perform. 2016, 11, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Opar, D.A.; Piatkowski, T.; Williams, M.D.; Shield, A.J. A Novel Device Using the Nordic Hamstring Exercise to Assess Eccentric Knee Flexor Strength: A Reliability and Retrospective Injury Study. J. Orthop. Sports Phys. Ther. 2013, 43, 636–640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lodge, C.; Tobin, D.; O’Rourke, B.; Thorborg, K. Reliability and validity of a new eccentric hamstring strength measurement device. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100034. [Google Scholar] [CrossRef] [PubMed]
- Van Der Horst, N.; Smits, D.W.; Petersen, J.; Goedhart, E.A.; Backx, F.J. The Preventive Effect of the Nordic Hamstring Exercise on Hamstring Injuries in Amateur Soccer Players. Am. J. Sports Med. 2015, 43, 1316–1323. [Google Scholar] [CrossRef]
- Presland, J.D.; Timmins, R.G.; Bourne, M.N.; Williams, M.D.; Opar, D.A. The effect of Nordic hamstring exercise training volume on biceps femoris long head architectural adaptation. Scand. J. Med. Sci. Sports 2018, 28, 1775–1783. [Google Scholar] [CrossRef]
- Bahr, R.; Thorborg, K.; Ekstrand, J. Evidence-based hamstring injury prevention is not adopted by the majority of Champions League or Norwegian Premier League football teams: The Nordic Hamstring survey. Br. J. Sports Med. 2015, 49, 1466–1471. [Google Scholar] [CrossRef] [Green Version]
- Oliver, G.D.; Dougherty, C.P. The razor curl: A functional approach to hamstring training. J. Strength Cond. Res. 2009, 23, 401–405. [Google Scholar] [CrossRef] [Green Version]
- Pollard, C.W.; Opar, D.A.; Williams, M.D.; Bourne, M.N.; Timmins, R.G. Razor hamstring curl and Nordic hamstring exercise architectural adaptations: Impact of exercise selection and intensity. Scand. J. Med. Sci. Sports 2019, 29, 706–715. [Google Scholar] [CrossRef]
- Lahti, J.; Mendiguchia, J.; Ahtiainen, J.; Anula, L.; Kononen, T.; Kujala, M.; Matinlauri, A.; Peltonen, V.; Thibault, M.; Toivonen, R.-M.; et al. Multifactorial individualised programme for hamstring muscle injury risk reduction in professional football: Protocol for a prospective cohort study. BMJ Open Sport Exerc. Med. 2020, 6, 758–772. [Google Scholar] [CrossRef]
- Oakley, A.J.; Jennings, J.; Bishop, C.J. Holistic hamstring health: Not just the Nordic hamstring exercise. Br. J. Sports Med. 2018, 52, 816–817. [Google Scholar] [CrossRef]
- Hopkins, W.G. Spreadsheets for analysis of validity and reliability. Sportscience 2015, 19, 36–42. [Google Scholar]
- Hills, M.; Fleiss, J.L. The Design and Analysis of Clinical Experiments. J. R. Stat. Soc. Ser. A 1987, 150, 400. [Google Scholar] [CrossRef]
- Hopkins, W.G. Measures of Reliability in Sports Medicine and Science. Sports Med. 2000, 30, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cuthbert, M.; Comfort, P.; Ripley, N.; McMahon, J.J.; Evans, M.; Bishop, C. Unilateral vs. bilateral hamstring strength assessments: Comparing reliability and inter-limb asymmetries in female soccer players. J. Sports Sci. 2021, 39, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
| Trial 1 | Trial 2 | ICC (95% CI) | TE (N) | CV% | MDC(N) | |
|---|---|---|---|---|---|---|
| Average Left (N) | 375.73 ± 36.27 | 381.38 ± 41.62 | 0.9 (0.7–0.97) | 14.10 | 1.87 | 39.06 |
| Average Right (N) | 382.07 ± 58.87 | 382.20 ± 65.10 | 0.91 (0.73–0.97) | 20.89 | 3.26 | 57.87 |
| Peak Left (N) | 392.99 ± 39.18 | 395.93 ± 37.80 | 0.91 (0.71–0.97) | 13.55 | 1.61 | 37.53 |
| Peak Right (N) | 395.48 ± 57.88 | 394.97 ± 63.37 | 0.9 (0.7–0.97) | 21.70 | 3.31 | 60.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Brien, J.; Browne, D.; Earls, D.; Lodge, C. Reliability of the Hip Extension Lower Exercise as a Measure of Eccentric Hamstring Strength. Biomechanics 2022, 2, 1-6. https://doi.org/10.3390/biomechanics2010001
O’Brien J, Browne D, Earls D, Lodge C. Reliability of the Hip Extension Lower Exercise as a Measure of Eccentric Hamstring Strength. Biomechanics. 2022; 2(1):1-6. https://doi.org/10.3390/biomechanics2010001
Chicago/Turabian StyleO’Brien, Joey, Declan Browne, Des Earls, and Clare Lodge. 2022. "Reliability of the Hip Extension Lower Exercise as a Measure of Eccentric Hamstring Strength" Biomechanics 2, no. 1: 1-6. https://doi.org/10.3390/biomechanics2010001
APA StyleO’Brien, J., Browne, D., Earls, D., & Lodge, C. (2022). Reliability of the Hip Extension Lower Exercise as a Measure of Eccentric Hamstring Strength. Biomechanics, 2(1), 1-6. https://doi.org/10.3390/biomechanics2010001





