Comparative Finite Element Analysis of Fixation Techniques for APC II Open-Book Injuries of the Pelvis
Abstract
1. Introduction
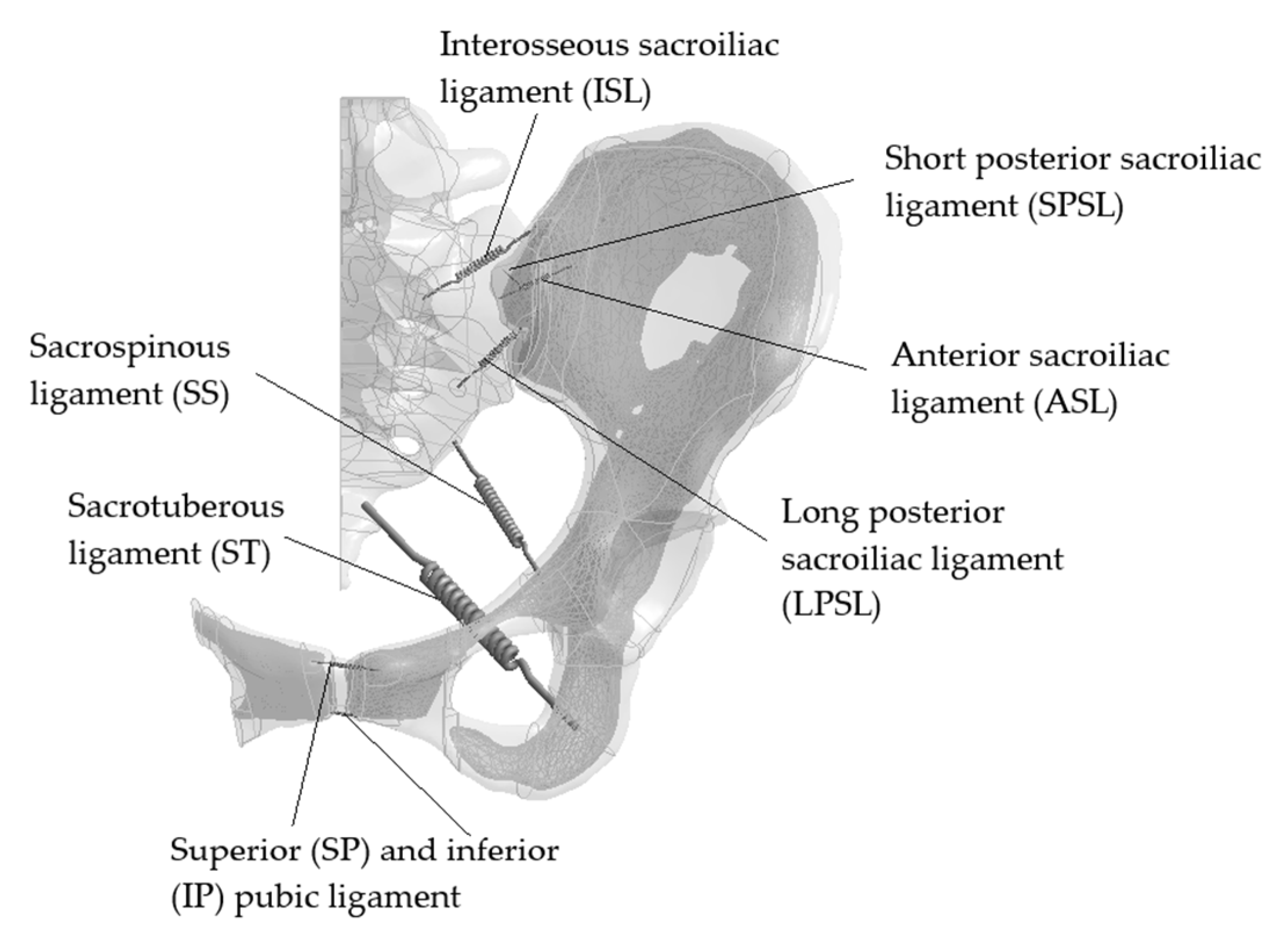
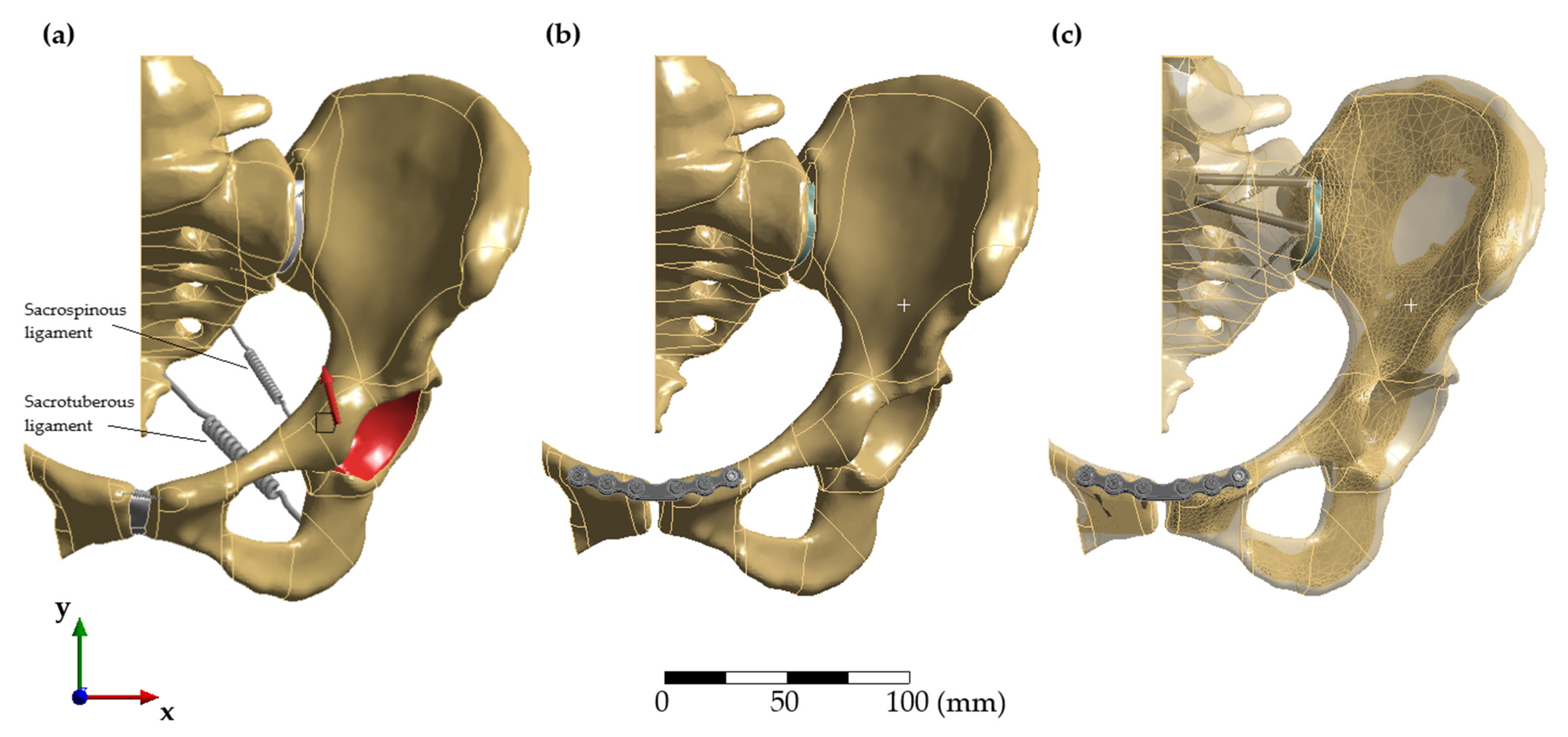
2. Materials and Methods
3. Results
3.1. Convergence Study and Validation
3.2. Range of Motion of the Sacroiliac Joint and the Pubic Symphysis
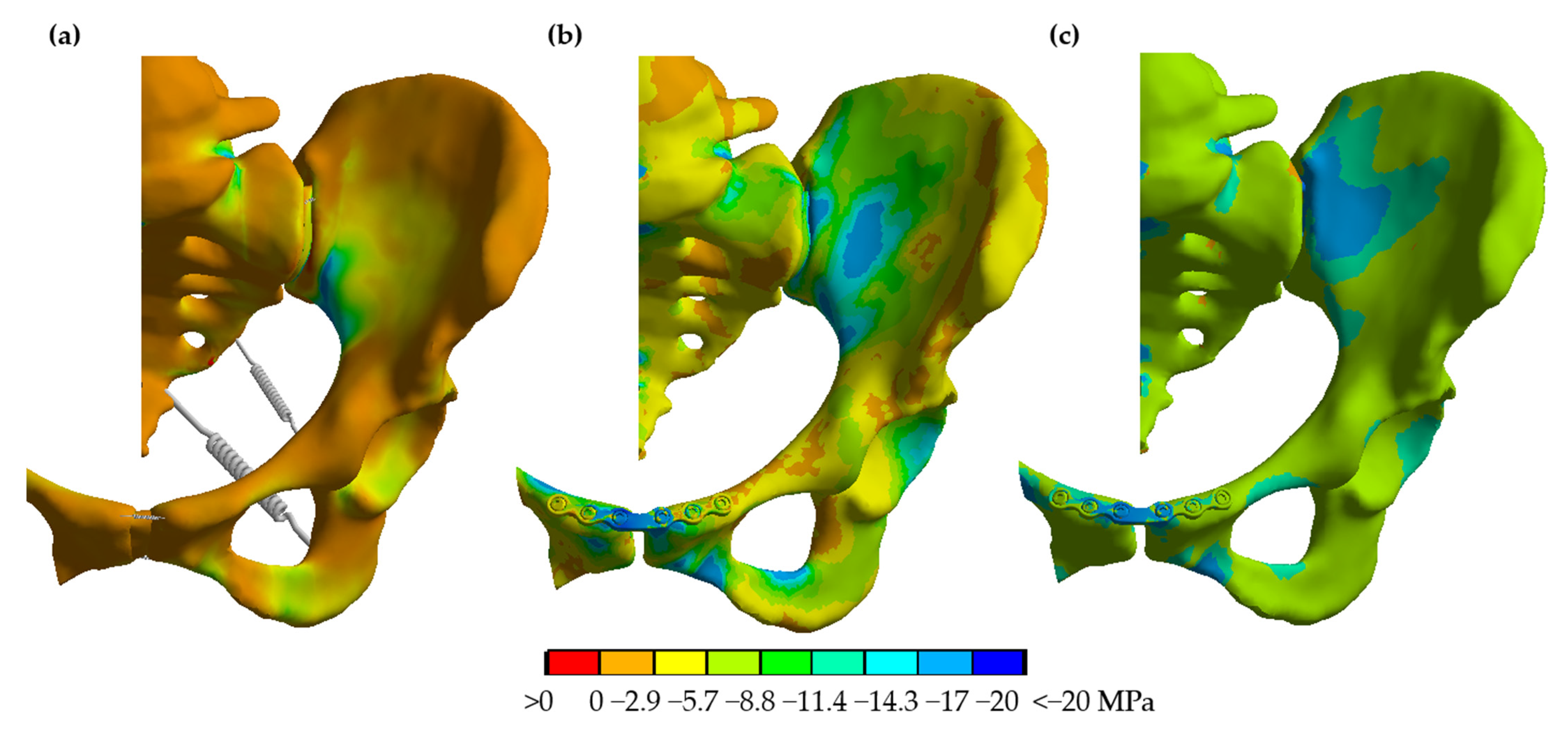
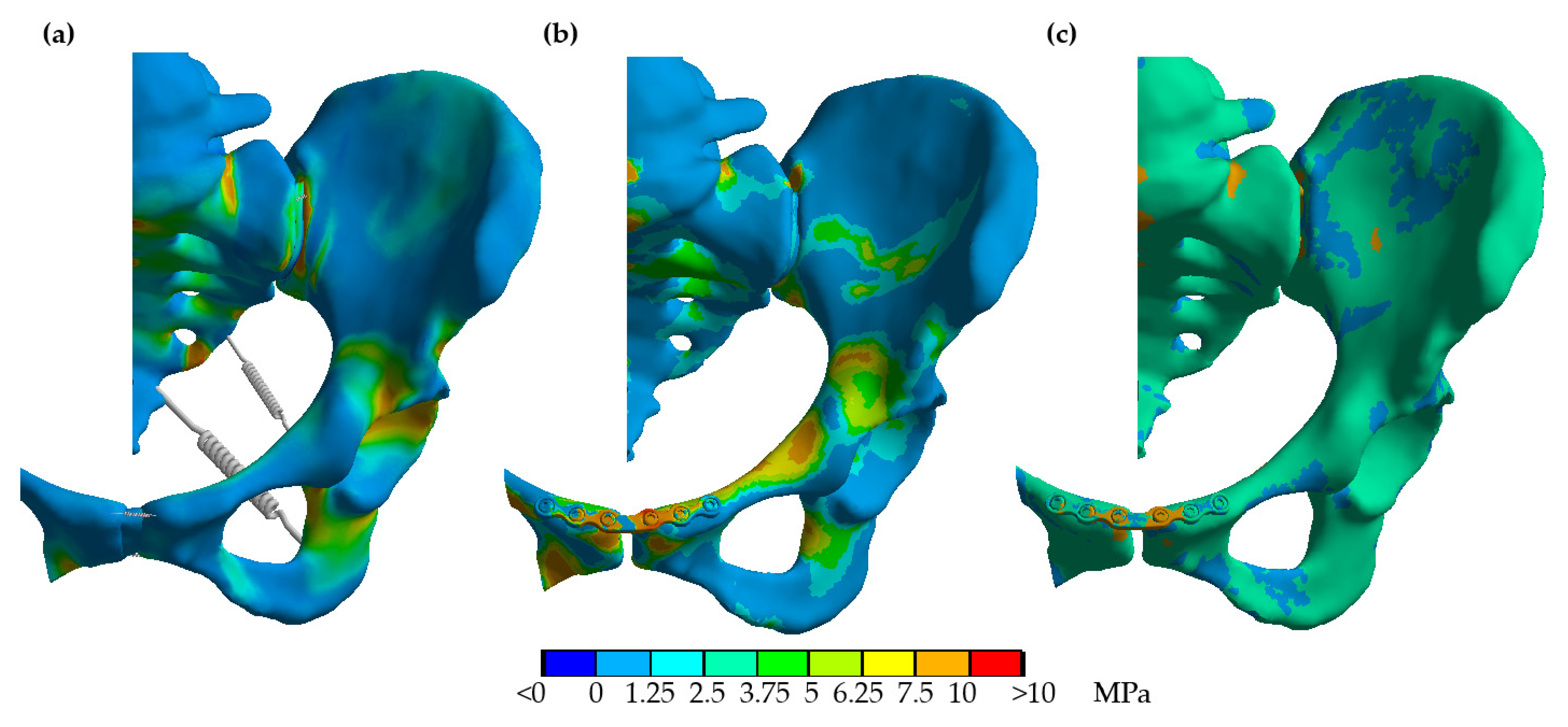
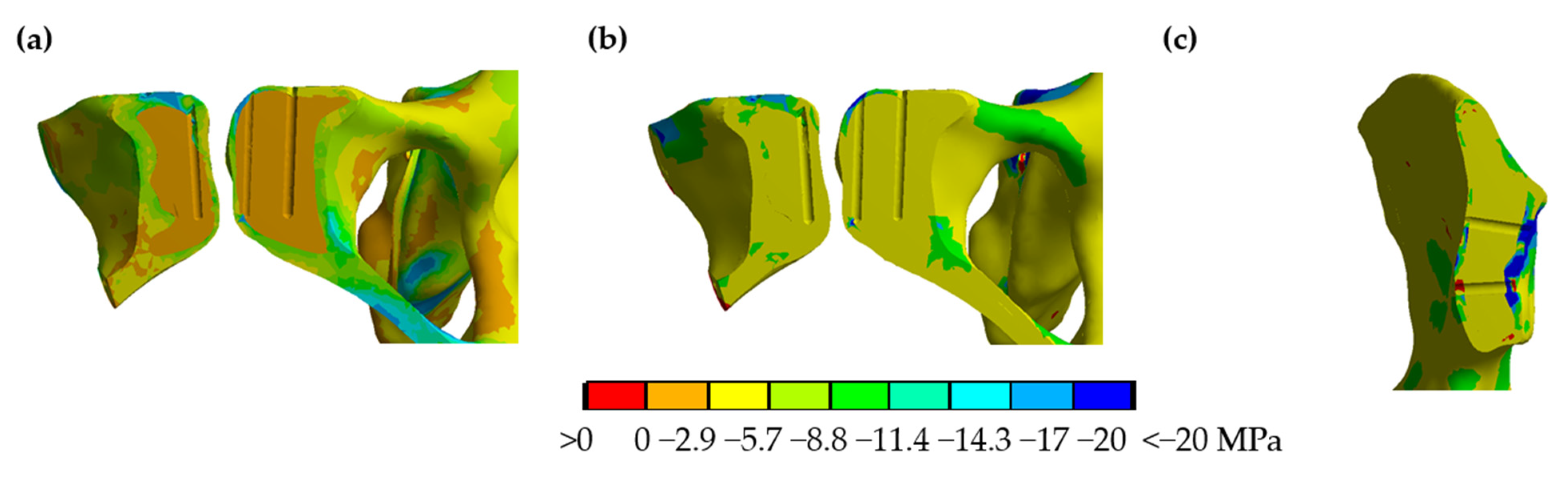
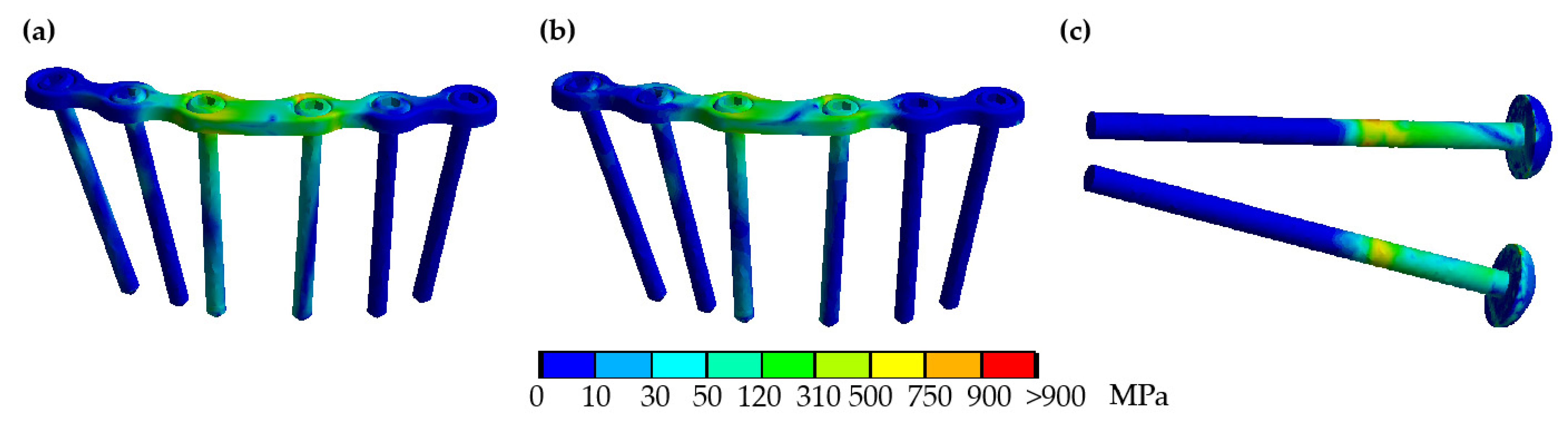
3.3. Implant and Bone Stresses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pohlemann, T.; Tscherne, H.; Baumgärtel, F.; Egbers, H.J.; Euler, E.; Maurer, F.; Fell, M.; Mayr, E.; Quirini, W.W.; Schlickewei, W.; et al. Beckenverletzungen: Epidemiologie, Therapie und Langzeitverlauf. Übersicht über die multizentrische Studie der Arbeitsgruppe Becken. Unfallchirurg 1996, 99, 160–167. [Google Scholar]
- Hauschild, O.; Strohm, P.C.; Culemann, U.; Pohlemann, T.; Suedkamp, N.P.; Koestler, W.; Schmal, H. Mortality in patients with pelvic fractures: Results from the German pelvic injury register. J. Trauma 2008, 64, 449–455. [Google Scholar] [CrossRef]
- Culemann, U.; Oestern, H.J.; Pohlemann, T. Aktuelle Behandlung der Beckenringfraktur. Unfallchirurg 2014, 117, 145–159. [Google Scholar] [CrossRef] [PubMed]
- Hermans, E.; Edwards, M.J.R.; Goslings, J.C.; Biert, J. Open pelvic fracture: The killing fracture? J. Orthop. Surg. Res. 2018, 13, 83. [Google Scholar] [CrossRef]
- Durkin, A.; Sagi, H.C.; Durham, R.; Flint, L. Contemporary management of pelvic fractures. Am. J. Surg. 2006, 192, 211–223. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, D.P.; Luchette, F.A.; Pereira, S.J.; Lim, E.; Seeskin, C.S.; James, L.; Miller, S.; Davis, K.; Hurst, J.M.; Johannigman, J.A.; et al. Pelvic fracture in the elderly is associated with increased mortality. Surgery 2002, 132, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.R.; Eastridge, B.J.; Young, J.W.; Ellison, T.S.; Ellison, P.S.; Poka, A.; Bathon, G.H.; Brumback, R.J. Pelvic ring disruptions: Effective classification system and treatment protocols. J. Trauma 1990, 30, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Tile, M. Fractures of the Pelvis. In The Rationale of Operative Fracture Care, 3rd ed.; Schatzker, J., Tile, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 239–290. [Google Scholar]
- Abdelfattah, A.; Moed, B.R. Ligamentous contributions to pelvic stability in a rotationally unstable open-book injury: A cadaver study. Injury 2014, 45, 1599–1603. [Google Scholar] [CrossRef]
- Stuby, F.M.; Lenz, M.; Doebele, S.; Agarwal, Y.; Skulev, H.; Ochs, B.G.; Zwingmann, J.; Gueorguiev, B. Symphyseal fixation in open book injuries cannot fully compensate anterior SI joint injury-A biomechanical study in a two-leg alternating load model. PLoS ONE 2017, 12, e0184000. [Google Scholar] [CrossRef]
- Dujardin, F.H.; Roussignol, X.; Hossenbaccus, M.; Thomine, J.M. Experimental study of the sacroiliac joint micromotion in pelvic disruption. J. Orthop. Trauma 2002, 16, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Simonian, P.T.; Routt, M.L.; Harrington, R.M.; Mayo, K.A.; Tencer, A.F. Biomechanical simulation of the anteroposterior compression injury of the pelvis. An understanding of instability and fixation. Clin. Orthop. Relat. Res. 1994, 309, 245–256. [Google Scholar]
- Moed, B.R.; Barla, J.; Israel, H.A.; Tovar, S.; Joeris, A. Current Trends in the Surgical Treatment of Open-Book Pelvic Ring Injuries: An International Survey Among Experienced Trauma Surgeons. J. Orthop. Trauma 2019, 33, 61–65. [Google Scholar] [CrossRef]
- Metz, R.M.; Bledsoe, J.G.; Moed, B.R. Does Posterior Fixation of Partially Unstable Open-Book Pelvic Ring Injuries Decrease Symphyseal Plate Failure? A Biomechanical Study. J. Orthop. Trauma 2018, 32, 18–24. [Google Scholar] [CrossRef]
- Avilucea, F.R.; Whiting, P.S.; Mir, H. Posterior fixation of APC-2 pelvic ring injuries decreases rates of anterior plate failure and malunion. J. Bone Jt. Surg. Am. 2016, 98, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Van Loon, P.; Kuhn, S.; Hofmann, A.; Hessmann, M.H.; Rommens, P.M. Radiological analysis, operative management and functional outcome of open book pelvic lesions: A 13-year cohort study. Injury 2011, 42, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Meyhoff, C.S.; Thomsen, C.H.; Rasmussen, L.S.; Nielsen, P.R. High incidence of chronic pain following surgery for pelvic fracture. Clin. J. Pain 2006, 22, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Quade, J.; Busel, G.; Beebe, M.; Auston, D.; Shah, A.R.; Infante, A.; Maxson, B.; Watson, D.; Sanders, R.W.; Mir, H.R. Symptomatic Iliosacral Screw Removal After Pelvic Trauma-Incidence and Clinical Impact. J. Orthop. Trauma 2019, 33, 351–353. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Chalidis, B.E.; Roberts, C.S. Internal fixation of traumatic diastasis of pubic symphysis: Is plate removal essential? Arch. Orthop. Trauma Surg. 2008, 128, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Labitzke, R.; Witzel, U. Plattenfreie Synthese der ligamentären Beckenringverletzung (Malgaigne-Luxation). Langenbecks Arch. Chiv. 1983, 361, 781. [Google Scholar] [CrossRef][Green Version]
- Jordan, M.C.; Jäckle, V.; Scheidt, S.; Gilbert, F.; Hölscher-Doht, S.; Ergün, S.; Meffert, R.H.; Heintel, T.M. Trans-obturator cable fixation of open book pelvic injuries. Sci. Rep. 2021, 11, 13463. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti Kußmaul, A.; Schwaabe, F.; Kistler, M.; Gennen, C.; Andreß, S.; Becker, C.A.; Böcker, W.; Greiner, A. Novel minimally invasive tape suture osteosynthesis for instabilities of the pubic symphysis: A biomechanical study. Arch. Orthop. Trauma Surg. 2021, 1–9, Epub ahead of print. [Google Scholar] [CrossRef]
- Kim, J.W.; Oh, C.W.; Oh, J.K.; Kyung, H.S.; Park, K.H.; Yoon, S.D.; Yoon, S.H. The incidence of and factors affecting iliosacral screw loosening in pelvic ring injury. Arch. Orthop. Trauma Surg. 2016, 136, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Collinge, C.; Archdeacon, M.T.; Dulaney-Cripe, E.; Moed, B.R. Radiographic changes of implant failure after plating for pubic symphysis diastasis: An underappreciated reality? Clin. Orthop. Relat. Res. 2012, 470, 2148–2153. [Google Scholar] [CrossRef] [PubMed]
- Witzel, U. Generelle Systematik und Beurteilung temporärer Implantate aus biomechanischer Sicht. In Generelle Beurteilungskriterien Für Die Wirksamkeit Temporärer Implantate, Proceedings of the DVM, Berlin, Germany; Deutscher Verband für Materialforschung: Berlin, Germany, 21 November 1989. [Google Scholar]
- Salo, Z.; Kreder, H.; Whyne, C.M. The Impact of an Open-Book Pelvic Ring Injury on Bone Strain: Validation of a Finite Element Model and Analysis Within the Gait Cycle. J. Biomech. Eng. 2021, 143, 071005. [Google Scholar] [CrossRef] [PubMed]
- Böhme, J.; Steinke, H.; Huelse, R.; Hammer, N.; Klink, T.; Slowik, V.; Josten, C. Komplexe ligamentäre Instabilitäten nach “open book“-Verletzungen des Beckenrings-Finite-Elemente-Computersimulation und Bruchversuch. Z. Orthop. Unf. 2011, 149, 83–89. [Google Scholar] [CrossRef]
- Ricci, P.L.; Maas, S.; Kelm, J.; Gerich, T. Finite element analysis of the pelvis including gait muscle forces: An investigation into the effect of rami fractures on load transmission. J. Exp. Orthop. 2018, 5, 33. [Google Scholar] [CrossRef]
- Hu, P.; Wu, T.; Wang, H.Z.; Qi, X.Z.; Yao, J.; Cheng, X.D.; Chen, W.; Zhang, Y.Z. Biomechanical Comparison of Three Internal Fixation Techniques for Stabilizing Posterior Pelvic Ring Disruption: A 3D Finite Element Analysis. Orthop. Surg. 2019, 11, 195–203. [Google Scholar] [CrossRef]
- Shim, V.; Höch, A.; Grunert, R.; Peldschus, S.; Böhme, J. Development of a Patient-Specific Finite Element Model for Predicting Implant Failure in Pelvic Ring Fracture Fixation. Comput. Math. Methods Med. 2017, 2017, 9403821. [Google Scholar]
- Kurz, S.; Pieroh, P.; Lenk, M.; Josten, C.; Böhme, J. Three-dimensional reduction and finite element analysis improves the treatment of pelvic malunion reconstructive surgery: A case report. Medicine 2017, 96, e8136. [Google Scholar] [CrossRef]
- Yu, K.H.; Hong, J.J.; Guo, X.S.; Zhou, D.S. Comparison of reconstruction plate screw fixation and percutaneous cannulated screw fixation in treatment of Tile B1 type pubic symphysis diastasis: A finite element analysis and 10-year clinical experience. J. Orthop. Surg. Res. 2015, 10, 151. [Google Scholar] [CrossRef]
- García, J.M.; Doblaré, M.; Seral, B.; Seral, F.; Palanca, D.; Gracia, L. Three-dimensional finite element analysis of several internal and external pelvis fixations. J. Biomech. Eng. 2000, 122, 516–522. [Google Scholar] [CrossRef]
- Carniel, E.L.; Toniolo, I.; Fontanella, C.G. Computational Biomechanics: In-Silico Tools for the Investigation of Surgical Procedures and Devices. Bioengineering 2020, 7, 48. [Google Scholar] [CrossRef]
- Rubio-Pérez, I.; Díaz Lantada, A. Surgical Planning of Sacral Nerve Stimulation Procedure in Presence of Sacral Anomalies by Using Personalized Polymeric Prototypes Obtained with Additive Manufacturing Techniques. Polymers 2020, 12, 581. [Google Scholar] [CrossRef] [PubMed]
- Bakhshayesh, P.; Zaghloul, A.; Sephton, B.M.; Enocson, A. A novel 3D technique to assess symmetry of hemi pelvises. Sci. Rep. 2020, 10, 18789. [Google Scholar] [CrossRef]
- Ead, M.S.; Duke, K.K.; Jaremko, J.L.; Westover, L. Investigation of pelvic symmetry using CAD software. Med. Biol. Eng. Comput. 2020, 58, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Bachtar, F.; Chen, X.; Hisada, T. Finite element contact analysis of the hip joint. Med. Bio. Eng. Comput. 2006, 44, 643–651. [Google Scholar] [CrossRef]
- Salzar, R.S.; Genovese, D.; Bass, C.R.; Bolton, J.R.; Guillemot, H.; Damon, A.M.; Crandall, J.R. Load path distribution within the pelvic structure under lateral loading. Int. J. Crashworth. 2009, 14, 99–110. [Google Scholar] [CrossRef]
- Watson, P.J.; Dostanpor, A.; Fagan, M.J.; Dobson, C.A. The effect of boundary conditions on finite element modelling of the human pelvis. Med. Eng. Phys. 2017, 43, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Dalstra, M.; Huiskes, R. Load transfer across the pelvic bone. J. Biomech. 1995, 28, 715–724. [Google Scholar] [CrossRef]
- Li, Z.; Alonso, J.E.; Kim, J.E.; Davidson, J.S.; Etheridge, B.S.; Eberhardt, A.W. Three-dimensional finite element models of the human pubic symphysis with viscohyperelastic soft tissues. Ann. Biomed. Eng. 2006, 34, 1452–1462. [Google Scholar] [CrossRef]
- Xu, Z.; Li, Y.; Zhang, S.; Liao, L.; Wu, K.; Feng, Z.; Li, D. A finite element analysis of sacroiliac joint displacements and ligament strains in response to three manipulations. BMC Musculoskelet. Disord. 2020, 21, 709. [Google Scholar] [CrossRef]
- Hayes, W.C.; Mockros, L.F. Viscoelastic properties of human articular cartilage. J. Appl. Physiol. 1971, 31, 562–568. [Google Scholar] [CrossRef] [PubMed]
- ASTM F1295-16. Standard Specification for Wrought Titanium-6 Aluminum-7 Niobium Alloy for Surgical Implant Applications (UNS R56700); ASTM International: West Conshohocken, PA, USA, 2016. [Google Scholar]
- Phillips, A.T.; Pankaj, P.; Howie, C.R.; Usmani, A.S.; Simpson, A.H. Finite element modelling of the pelvis: Inclusion of muscular and ligamentous boundary conditions. Med. Eng. Phys. 2007, 29, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Shi, D.; Wang, F.; Wang, D.; Li, X.; Wang, Q. 3-D finite element analysis of the influence of synovial condition in sacroiliac joint on the load transmission in human pelvic system. Med. Eng. Phys. 2014, 36, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; He, Y.; Qian, H.; Zhou, D.; Li, Q. Comparison of Biomechanical Characteristics and Pelvic Ring Stability Using Different Fixation Methods to Treat Pubic Symphysis Diastasis: A Finite Element Study. Medicine 2015, 94, e2207. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, S.; Sun, T.; Wang, D.; Lian, W.; Tan, J.; Zou, D.; Zhao, Y. Mechanical comparison between lengthened and short sacroiliac screws in sacral fracture fixation: A finite element analysis. Orthop. Traumatol. Surg. Res. 2013, 99, 601–606. [Google Scholar] [CrossRef]
- Miller, J.A.; Schultz, A.B.; Andersson, G.B. Load-displacement behavior of sacroiliac joints. J. Orthop. Res. 1987, 5, 92–101. [Google Scholar] [CrossRef]
- Bergmann, G.; Deuretzbacher, G.; Heller, M.; Graichen, F.; Rohlmann, A.; Strauss, J.; Duda, G.N. Hip contact forces and gait patterns from routine activities. J. Biomech. 2001, 34, 859–871. [Google Scholar] [CrossRef]
- Ghosh, R.; Pal, B.; Ghosh, D.; Gupta, S. Finite element analysis of a hemi-pelvis: The effect of inclusion of cartilage layer on acetabular stresses and strain. Comput. Methods Biomech. Biomed. Eng. 2015, 18, 697–710. [Google Scholar] [CrossRef]
- Böhme, J.; Hülse, R.; Slowik, V.; Hammer, N.; Steinke, H.; Josten, C. Computersimulation von ligamentären Instabilitäten bei anterior-posterioren Kompressionsverletzungen des Beckens. In Proceedings of the ANSYS Conference & 27th CADFEM Users’ Meeting, Leipzig, Germany, 18–20 November 2009. [Google Scholar]
- MacAvoy, M.C.; McClellan, R.T.; Goodman, S.B.; Chien, C.R.; Allen, W.A.; van der Meulen, M.C. Stability of open-book pelvic fractures using a new biomechanical model of single-limb stance. J. Orthop. Trauma 1997, 11, 590–593. [Google Scholar] [CrossRef]
- AO Surgery Reference. Available online: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/pelvic-ring/pubic-symphysis/orif-pubic-symphysis-plate (accessed on 30 October 2021).
- Gill, J.R.; Murphy, C.; Quansah, B.; Carrothers, A. Management of the open book APC II pelvis: Survey results from pelvic and acetabular surgeons in the United Kingdom. J. Orthop. 2017, 14, 530–536. [Google Scholar] [CrossRef]
- Witzel, U. Virtual synthesis of the skull in neanderthals by FESS. In Continuity and Discontinuity in the Peopling of Europe; Condemi, S., Weniger, G.C., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 203–212. [Google Scholar]
- Frietman, B.; Verbeek, J.; Biert, J.; Frölke, J.P. The Effect of Implant Failure After Symphyseal Plating on Functional Outcome and General Health. J. Orthop. Trauma 2016, 30, 336–339. [Google Scholar] [PubMed]
- Banierink, H.; Reininga, I.H.F.; Heineman, E.; Wendt, K.W.; Ten Duis, K.; IJpma, F.F.A. Long-term physical functioning and quality of life after pelvic ring injuries. Arch. Orthop. Trauma Surg. 2019, 139, 1225–1233. [Google Scholar] [CrossRef]
- Bakhtiarinejad, M.; Farvardin, A.; Murphy, R.J.; Grupp, R.B.; Tis, J.E.; Sponseller, P.D.; Armand, M. Comparative Biomechanical Study of Screw Fixation Techniques in Periacetabular Osteotomy. Biomechanics 2021, 1, 131–144. [Google Scholar] [CrossRef]
- Sverdlova, N.S.; Witzel, U. Principles of determination and verification of muscle forces in the human musculoskeletal system: Muscle forces to minimise bending stress. J. Biomech. 2010, 43, 387–396. [Google Scholar] [CrossRef]
- Witzel, U. Eine neue Methode zur virtuellen Schädelsynthese am Beispiel Camarasaurus. Hallesches Jahrb. Für Geowiss. 2007, 23, 73–78. [Google Scholar]
| Direction of Displacement | Superior | Inferior | Anterior | Posterior |
|---|---|---|---|---|
| in vitro Model [44] | 0.28 mm | 0.26 mm | 0.48 mm | 0.53 mm |
| FE model using ligament stiffness by Shi et al. [41] | 0.25 mm | 0.34 mm | 0.32 mm | 0.37 mm |
| FE model using ligament stiffness by Yao et al. [42] | 0.26 mm | 0.48 mm | 0.35 mm | 0.35 mm |
| FE model using ligament stiffness by Zhao et al. [43] | 0.26 mm | 0.5 mm | 0.49 mm | 0.48 mm |
| Direction of Displacement | Sacroiliac Joint | Pubic Symphysis | ||||
|---|---|---|---|---|---|---|
| Healthy pelvis | Symphyseal plating | Symphyseal plating andiliosacral screw fixation | Healthy pelvis | Symphyseal plating | Symphyseal plating andiliosacral screw fixation | |
| Mediolateral | 0.07 mm | −0.03 mm | 0.07 mm | 0.0135 mm | 0.35 mm | 0.165 mm |
| Craniocaudal | 0.39 mm | 0.12 mm | 0.005 mm | 1.44 mm | 0.33 mm | 0.105 mm |
| Anterio-posterior | −0.235 mm | 0.078 mm | 0.03 mm | 1.05 mm | 0.365 mm | 0.34 mm |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lipphaus, A.; Klimek, M.; Witzel, U. Comparative Finite Element Analysis of Fixation Techniques for APC II Open-Book Injuries of the Pelvis. Biomechanics 2021, 1, 321-333. https://doi.org/10.3390/biomechanics1030027
Lipphaus A, Klimek M, Witzel U. Comparative Finite Element Analysis of Fixation Techniques for APC II Open-Book Injuries of the Pelvis. Biomechanics. 2021; 1(3):321-333. https://doi.org/10.3390/biomechanics1030027
Chicago/Turabian StyleLipphaus, Andreas, Matthias Klimek, and Ulrich Witzel. 2021. "Comparative Finite Element Analysis of Fixation Techniques for APC II Open-Book Injuries of the Pelvis" Biomechanics 1, no. 3: 321-333. https://doi.org/10.3390/biomechanics1030027
APA StyleLipphaus, A., Klimek, M., & Witzel, U. (2021). Comparative Finite Element Analysis of Fixation Techniques for APC II Open-Book Injuries of the Pelvis. Biomechanics, 1(3), 321-333. https://doi.org/10.3390/biomechanics1030027







